Recent from talks
Nothing was collected or created yet.
MYD88
View on Wikipedia
Myeloid differentiation primary response 88 (MYD88) is a protein that, in humans, is encoded by the MYD88 gene.[5][6] originally discovered in the laboratory of Dan A. Liebermann (Lord et al. Oncogene 1990) as a Myeloid differentiation primary response gene.
Function
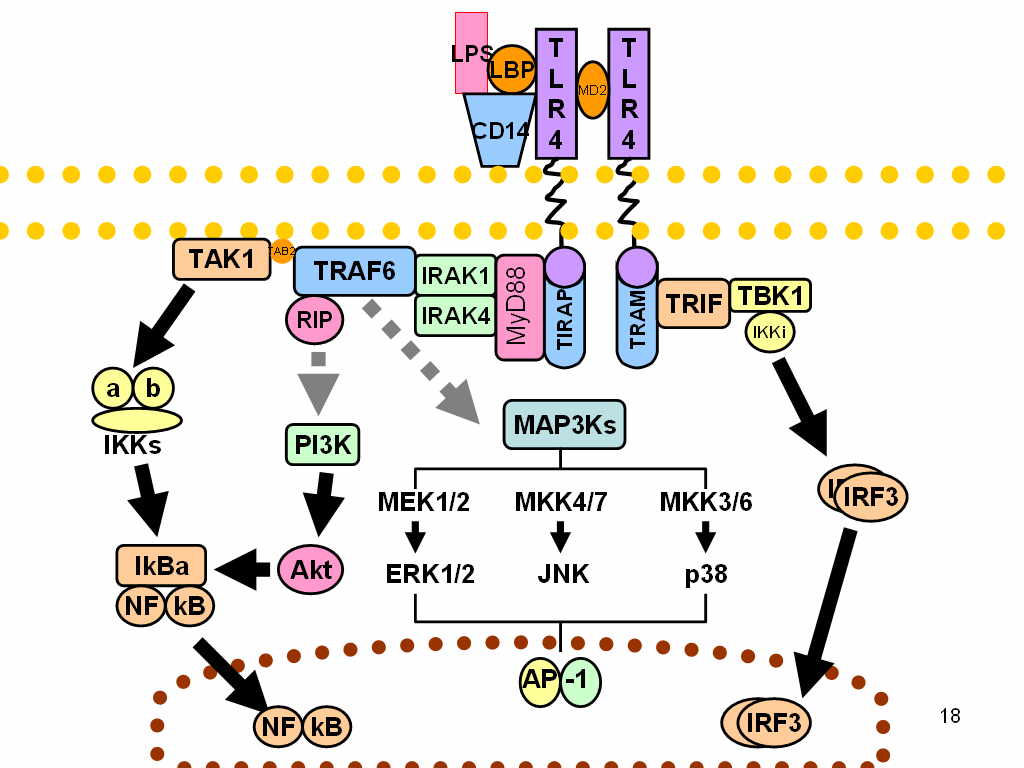
[edit]The MYD88 gene provides instructions for making a protein involved in signaling within immune cells. The MyD88 protein acts as an adapter, connecting proteins that receive signals from outside the cell to the proteins that relay signals inside the cell.
In innate immunity, the MyD88 plays a pivotal role in immune cell activation through Toll-like receptors (TLRs), which belong to large group of pattern recognition receptors (PRR). In general, these receptors sense common patterns which are shared by various pathogens – Pathogen-associated molecular pattern (PAMPs), or which are produced/released during cellular damage – damage-associated molecular patterns (DAMPs).[7]
TLRs are homologous to Toll receptors, which were first described in the ontogenesis of fruit flies Drosophila, being responsible for dorso-ventral development. Hence, TLRs have been proved in all animals from insects to mammals. TLRs are located either on the cellular surface (TLR1, TLR2, TLR4, TLR5, TLR6) or within endosomes (TLR3, TLR7, TLR8, TLR9) sensing extracellular or phagocytosed pathogens, respectively. TLRs are integral membrane glycoproteins with typical semicircular-shaped extracellular parts containing leucine-rich repeats responsible for ligand binding, and Intracellular parts containing Toll-Interleukin receptor (TIR) domain.[8]
After ligand binding, all TLRs, apart from TLR3, interact with adaptor protein MyD88. Another adaptor protein, which is activated by TLR3 and TLR4, is called TIR domain-containing adapter-inducing IFN-β (TRIF). Subsequently, these proteins activate two important transcription factors:
- NF-κB is a dimeric protein responsible for expression of various inflammatory cytokines, chemokines and adhesion and costimulatory molecules, which in turn triggers acute inflammation and stimulation of adaptive immunity
- IRFs is a group of proteins responsible for expression of type I interferons setting the so-called antiviral state of a cell.
TLR7 and TLR9 activate both NF-κB and IRF3 through MyD88-dependent and TRIF-independent pathway, respectively.[8]
The human ortholog MYD88 seems to function similarly to mice, since the immunological phenotype of human cells deficient in MYD88 is similar to cells from MyD88 deficient mice. However, available evidence suggests that MYD88 is dispensable for human resistance to common viral infections and to all but a few pyogenic bacterial infections, demonstrating a major difference between mouse and human immune responses.[9] Mutation in MYD88 at position 265 leading to a change from leucine to proline have been identified in many human lymphomas including ABC subtype of diffuse large B-cell lymphoma[10] and Waldenström's macroglobulinemia.[11]
Interactions
[edit]Myd88 has been shown to interact with:
Gene polymorphisms
[edit]Various single nucleotide polymorphisms (SNPs) of the MyD88 have been identified. and for some of them an association with susceptibility to various infectious diseases[22] and to some autoimmune diseases like ulcerative colitis was found.[23]
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000172936 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000032508 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Entrez Gene: MYD88 Myeloid differentiation primary response gene (88)".
- ^ Bonnert TP, Garka KE, Parnet P, Sonoda G, Testa JR, Sims JE (January 1997). "The cloning and characterization of human MyD88: a member of an IL-1 receptor related family". FEBS Letters. 402 (1): 81–4. doi:10.1016/S0014-5793(96)01506-2. PMID 9013863. S2CID 44843127.
- ^ Deguine J, Barton GM (2014-11-04). "MyD88: a central player in innate immune signaling". F1000Prime Reports. 6: 97. doi:10.12703/P6-97. PMC 4229726. PMID 25580251.
- ^ a b Abbas A, Lichtman AH, Pillai S (10 March 2017). Cellular and molecular immunology (Ninth ed.). Philadelphia, PA. ISBN 978-0-323-52323-3. OCLC 973917896.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ von Bernuth H, Picard C, Jin Z, Pankla R, Xiao H, Ku CL, et al. (August 2008). "Pyogenic bacterial infections in humans with MyD88 deficiency". Science. 321 (5889): 691–6. Bibcode:2008Sci...321..691V. doi:10.1126/science.1158298. PMC 2688396. PMID 18669862.
- ^ Ngo VN, Young RM, Schmitz R, Jhavar S, Xiao W, Lim KH, et al. (February 2011). "Oncogenically active MYD88 mutations in human lymphoma". Nature. 470 (7332): 115–9. Bibcode:2011Natur.470..115N. doi:10.1038/nature09671. PMC 5024568. PMID 21179087.
- ^ Treon SP, Xu L, Yang G, Zhou Y, Liu X, Cao Y, et al. (August 2012). "MYD88 L265P somatic mutation in Waldenström's macroglobulinemia". The New England Journal of Medicine. 367 (9): 826–33. doi:10.1056/NEJMoa1200710. PMID 22931316.
- ^ a b c Fitzgerald KA, Palsson-McDermott EM, Bowie AG, Jefferies CA, Mansell AS, Brady G, et al. (September 2001). "Mal (MyD88-adapter-like) is required for Toll-like receptor-4 signal transduction". Nature. 413 (6851): 78–83. Bibcode:2001Natur.413...78F. doi:10.1038/35092578. PMID 11544529. S2CID 4333764.
- ^ a b Wesche H, Gao X, Li X, Kirschning CJ, Stark GR, Cao Z (July 1999). "IRAK-M is a novel member of the Pelle/interleukin-1 receptor-associated kinase (IRAK) family". The Journal of Biological Chemistry. 274 (27): 19403–10. doi:10.1074/jbc.274.27.19403. PMID 10383454.
- ^ Chen BC, Wu WT, Ho FM, Lin WW (July 2002). "Inhibition of interleukin-1beta -induced NF-kappa B activation by calcium/calmodulin-dependent protein kinase kinase occurs through Akt activation associated with interleukin-1 receptor-associated kinase phosphorylation and uncoupling of MyD88". The Journal of Biological Chemistry. 277 (27): 24169–79. doi:10.1074/jbc.M106014200. PMID 11976320.
- ^ Li S, Strelow A, Fontana EJ, Wesche H (April 2002). "IRAK-4: a novel member of the IRAK family with the properties of an IRAK-kinase". Proceedings of the National Academy of Sciences of the United States of America. 99 (8): 5567–72. Bibcode:2002PNAS...99.5567L. doi:10.1073/pnas.082100399. PMC 122810. PMID 11960013.
- ^ a b Muzio M, Ni J, Feng P, Dixit VM (November 1997). "IRAK (Pelle) family member IRAK-2 and MyD88 as proximal mediators of IL-1 signaling". Science. 278 (5343): 1612–5. Bibcode:1997Sci...278.1612M. doi:10.1126/science.278.5343.1612. PMID 9374458.
- ^ Burns K, Clatworthy J, Martin L, Martinon F, Plumpton C, Maschera B, et al. (June 2000). "Tollip, a new component of the IL-1RI pathway, links IRAK to the IL-1 receptor". Nature Cell Biology. 2 (6): 346–51. doi:10.1038/35014038. PMID 10854325. S2CID 32036101.
- ^ Jefferies C, Bowie A, Brady G, Cooke EL, Li X, O'Neill LA (July 2001). "Transactivation by the p65 subunit of NF-kappaB in response to interleukin-1 (IL-1) involves MyD88, IL-1 receptor-associated kinase 1, TRAF-6, and Rac1". Molecular and Cellular Biology. 21 (14): 4544–52. doi:10.1128/MCB.21.14.4544-4552.2001. PMC 87113. PMID 11416133.
- ^ Chuang TH, Ulevitch RJ (May 2004). "Triad3A, an E3 ubiquitin-protein ligase regulating Toll-like receptors". Nature Immunology. 5 (5): 495–502. doi:10.1038/ni1066. PMID 15107846. S2CID 39773935.
- ^ Doyle SE, O'Connell R, Vaidya SA, Chow EK, Yee K, Cheng G (April 2003). "Toll-like receptor 3 mediates a more potent antiviral response than Toll-like receptor 4". Journal of Immunology. 170 (7): 3565–71. doi:10.4049/jimmunol.170.7.3565. PMID 12646618.
- ^ Rhee SH, Hwang D (November 2000). "Murine TOLL-like receptor 4 confers lipopolysaccharide responsiveness as determined by activation of NF kappa B and expression of the inducible cyclooxygenase". The Journal of Biological Chemistry. 275 (44): 34035–40. doi:10.1074/jbc.M007386200. PMID 10952994.
- ^ Netea MG, Wijmenga C, O'Neill LA (May 2012). "Genetic variation in Toll-like receptors and disease susceptibility". Nature Immunology. 13 (6): 535–42. doi:10.1038/ni.2284. PMID 22610250. S2CID 24438756.
- ^ Matsunaga K, Tahara T, Shiroeda H, Otsuka T, Nakamura M, Shimasaki T, et al. (January 2014). "The *1244 A>G polymorphism of MyD88 (rs7744) is closely associated with susceptibility to ulcerative colitis". Molecular Medicine Reports. 9 (1): 28–32. doi:10.3892/mmr.2013.1769. PMID 24189845.
Further reading
[edit]- Hardiman G, Rock FL, Balasubramanian S, Kastelein RA, Bazan JF (December 1996). "Molecular characterization and modular analysis of human MyD88". Oncogene. 13 (11): 2467–75. PMID 8957090.
- Bonnert TP, Garka KE, Parnet P, Sonoda G, Testa JR, Sims JE (January 1997). "The cloning and characterization of human MyD88: a member of an IL-1 receptor related family". FEBS Letters. 402 (1): 81–4. doi:10.1016/S0014-5793(96)01506-2. PMID 9013863. S2CID 44843127.
- Hardiman G, Jenkins NA, Copeland NG, Gilbert DJ, Garcia DK, Naylor SL, et al. (October 1997). "Genetic structure and chromosomal mapping of MyD88". Genomics. 45 (2): 332–9. doi:10.1006/geno.1997.4940. PMID 9344657.
- Muzio M, Ni J, Feng P, Dixit VM (November 1997). "IRAK (Pelle) family member IRAK-2 and MyD88 as proximal mediators of IL-1 signaling". Science. 278 (5343): 1612–5. Bibcode:1997Sci...278.1612M. doi:10.1126/science.278.5343.1612. PMID 9374458.
- Jaunin F, Burns K, Tschopp J, Martin TE, Fakan S (August 1998). "Ultrastructural distribution of the death-domain-containing MyD88 protein in HeLa cells". Experimental Cell Research. 243 (1): 67–75. doi:10.1006/excr.1998.4131. PMID 9716450.
- Lan X, Han X, Li Q, Li Q, Gao Y, Cheng T, et al. (March 2017). "Pinocembrin protects hemorrhagic brain primarily by inhibiting toll-like receptor 4 and reducing M1 phenotype microglia". Brain, Behavior, and Immunity. 61: 326–339. doi:10.1016/j.bbi.2016.12.012. PMC 5453178. PMID 28007523.
- Wesche H, Gao X, Li X, Kirschning CJ, Stark GR, Cao Z (July 1999). "IRAK-M is a novel member of the Pelle/interleukin-1 receptor-associated kinase (IRAK) family". The Journal of Biological Chemistry. 274 (27): 19403–10. doi:10.1074/jbc.274.27.19403. PMID 10383454.
- Burns K, Clatworthy J, Martin L, Martinon F, Plumpton C, Maschera B, et al. (June 2000). "Tollip, a new component of the IL-1RI pathway, links IRAK to the IL-1 receptor". Nature Cell Biology. 2 (6): 346–51. doi:10.1038/35014038. PMID 10854325. S2CID 32036101.
- Aliprantis AO, Yang RB, Weiss DS, Godowski P, Zychlinsky A (July 2000). "The apoptotic signaling pathway activated by Toll-like receptor-2". The EMBO Journal. 19 (13): 3325–36. doi:10.1093/emboj/19.13.3325. PMC 313930. PMID 10880445.
- Rhee SH, Hwang D (November 2000). "Murine TOLL-like receptor 4 confers lipopolysaccharide responsiveness as determined by activation of NF kappa B and expression of the inducible cyclooxygenase". The Journal of Biological Chemistry. 275 (44): 34035–40. doi:10.1074/jbc.M007386200. PMID 10952994.
- Fitzgerald KA, Palsson-McDermott EM, Bowie AG, Jefferies CA, Mansell AS, Brady G, et al. (September 2001). "Mal (MyD88-adapter-like) is required for Toll-like receptor-4 signal transduction". Nature. 413 (6851): 78–83. Bibcode:2001Natur.413...78F. doi:10.1038/35092578. PMID 11544529. S2CID 4333764.
- Tauszig-Delamasure S, Bilak H, Capovilla M, Hoffmann JA, Imler JL (January 2002). "Drosophila MyD88 is required for the response to fungal and Gram-positive bacterial infections". Nature Immunology. 3 (1): 91–7. doi:10.1038/ni747. PMID 11743586. S2CID 30884230.
- Bannerman DD, Tupper JC, Kelly JD, Winn RK, Harlan JM (February 2002). "The Fas-associated death domain protein suppresses activation of NF-kappa B by LPS and IL-1 beta". The Journal of Clinical Investigation. 109 (3): 419–25. doi:10.1172/JCI14774. PMC 150862. PMID 11828002.
- Tamai R, Sakuta T, Matsushita K, Torii M, Takeuchi O, Akira S, et al. (March 2002). "Human gingival CD14(+) fibroblasts primed with gamma interferon increase production of interleukin-8 in response to lipopolysaccharide through up-regulation of membrane CD14 and MyD88 mRNA expression". Infection and Immunity. 70 (3): 1272–8. doi:10.1128/IAI.70.3.1272-1278.2002. PMC 127773. PMID 11854210.
- Radons J, Gabler S, Wesche H, Korherr C, Hofmeister R, Falk W (May 2002). "Identification of essential regions in the cytoplasmic tail of interleukin-1 receptor accessory protein critical for interleukin-1 signaling". The Journal of Biological Chemistry. 277 (19): 16456–63. doi:10.1074/jbc.M201000200. PMID 11880380.
- Janssens S, Burns K, Tschopp J, Beyaert R (March 2002). "Regulation of interleukin-1- and lipopolysaccharide-induced NF-kappaB activation by alternative splicing of MyD88". Current Biology. 12 (6): 467–71. Bibcode:2002CBio...12..467J. doi:10.1016/S0960-9822(02)00712-1. PMID 11909531.
- Li S, Strelow A, Fontana EJ, Wesche H (April 2002). "IRAK-4: a novel member of the IRAK family with the properties of an IRAK-kinase". Proceedings of the National Academy of Sciences of the United States of America. 99 (8): 5567–72. Bibcode:2002PNAS...99.5567L. doi:10.1073/pnas.082100399. PMC 122810. PMID 11960013.
- Medvedev AE, Lentschat A, Wahl LM, Golenbock DT, Vogel SN (November 2002). "Dysregulation of LPS-induced Toll-like receptor 4-MyD88 complex formation and IL-1 receptor-associated kinase 1 activation in endotoxin-tolerant cells". Journal of Immunology. 169 (9): 5209–16. doi:10.4049/jimmunol.169.9.5209. PMID 12391239.
- Raschi E, Testoni C, Bosisio D, Borghi MO, Koike T, Mantovani A, et al. (May 2003). "Role of the MyD88 transduction signaling pathway in endothelial activation by antiphospholipid antibodies". Blood. 101 (9): 3495–500. doi:10.1182/blood-2002-08-2349. PMID 12531807.
- Doyle SE, O'Connell R, Vaidya SA, Chow EK, Yee K, Cheng G (April 2003). "Toll-like receptor 3 mediates a more potent antiviral response than Toll-like receptor 4". Journal of Immunology. 170 (7): 3565–71. doi:10.4049/jimmunol.170.7.3565. PMID 12646618.
External links
[edit]- MyD88+Protein at the U.S. National Library of Medicine Medical Subject Headings (MeSH)