Recent from talks
Nothing was collected or created yet.
Anoscopy
View on WikipediaThis article needs additional citations for verification. (January 2021) |
| Anoscopy | |
|---|---|
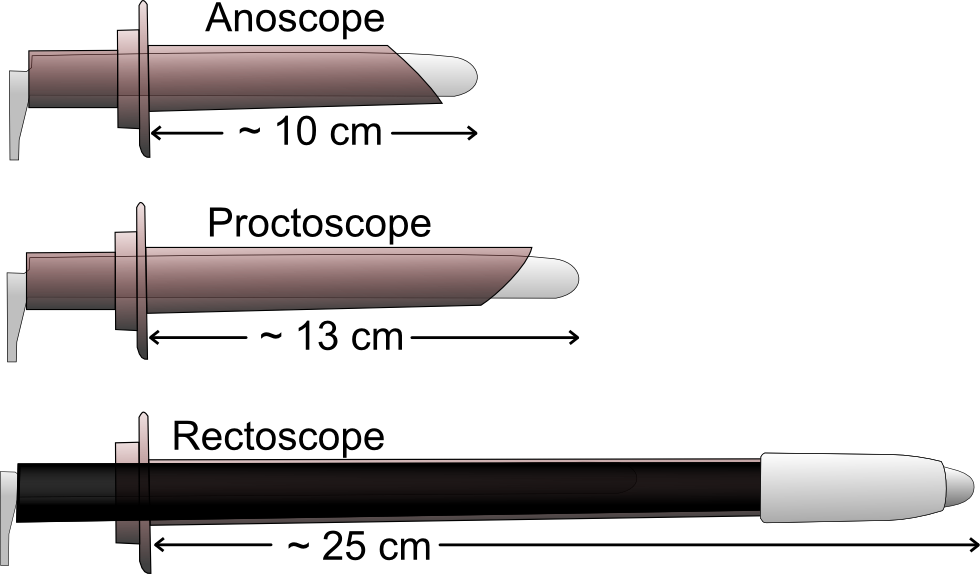
 An anoscope, a proctoscope and a rectoscope, and their approximate lengths. | |
| ICD-9-CM | 49.21 |
| MedlinePlus | 003890 |
An anoscopy is a medical examination using a small, rigid, tubular instrument called an anoscope (also called a rectal speculum). This is inserted a few centimeters into the anus in order to evaluate problems of the anal canal. Anoscopy is used to diagnose hemorrhoids, anal fissures (tears in the lining of the anus), and some cancers.[1][2]
Process
[edit]This test is usually done in a doctor's office. The patient is required to remove their underwear, and must either lie on their side on top of an examining table, with their knees bent up towards the chest, or bend forward over the table. The anoscope is 50 to 100 mm long and 8 to 25 mm in diameter. The doctor will coat the anoscope with a lubricant and then gently push it into the anus and rectum. The doctor may ask the patient to "bear down" or push as if they were going to have a bowel movement, and then relax. This helps the doctor insert the anoscope more easily and identify any bulges along the lining of the rectum.
By shining a light into this tube, the doctor will have a clear view of the lining of the lower rectum and anus. The anoscope is pulled out slowly once the test is finished.
The patient will feel pressure during the examination, and the anoscope will make one feel as if they were about to have a bowel movement. This is normal, however, and many patients do not feel pain from anoscopy.
-
The use of the anoscope for internal inspection of the lower rectum.
Conditions visible to anoscopy
[edit]- Hemorrhoids
- Anal fissures
- Fistulas
- Abscesses
- Inflammation
- Perianal/rectal tumors
- Some types of rectal or mucosal prolapses
- Rectal cancer
- Other anorectal problems
Anoscopy will permit biopsies to be taken, and is used when ligating prolapsed hemorrhoids. It is used in the treatment of warts produced by HPV.
The procedure is done on an outpatient basis.
References
[edit]- ^ London, Shawn; Hoilat, Gilles J.; Tichauer, Matthew B. (2020). "Anoscopy". StatPearls. StatPearls Publishing. PMID 29083587. Retrieved 9 January 2021.
- ^ Isaacs, Kim L. (2005). "9. Anoscopy and rigid sigmoidoscopy". In Drossman, Douglas A.; Grimm, Ian S.; Shaheen, Nicholas J. (eds.). Handbook of Gastroenterologic Procedures (4th ed.). Lippincott Williams & Wilkins. pp. 64–71. ISBN 978-0-7817-5008-0.