Recent from talks
Nothing was collected or created yet.
Axis (anatomy)
View on Wikipedia| Axis | |
|---|---|
 Position of axis (shown in red) | |
 Second cervical vertebra, or epistropheus, from above | |
| Details | |
| Identifiers | |
| Latin | axis, vertebra cervicalis II |
| MeSH | D001368 |
| TA98 | A02.2.02.201 |
| TA2 | 1050 |
| FMA | 12520 |
| Anatomical terms of bone | |
In anatomy, the axis (from Latin axis, "axle") is the second cervical vertebra (C2) of the spine, immediately inferior to the atlas, upon which the head rests. The spinal cord passes through the axis.
The defining feature of the axis is its strong bony protrusion known as the dens, which rises from the superior aspect of the bone.
Structure
[edit]The body is deeper in front or in the back and is prolonged downward anteriorly to overlap the upper and front part of the third vertebra.
It presents a median longitudinal ridge in front, separating two lateral depressions for the attachment of the longus colli muscles.

Dens
[edit]The dens, also called the odontoid process, or the peg, is the most pronounced projecting feature of the axis. The dens exhibits a slight constriction where it joins the main body of the vertebra. The condition where the dens is separated from the body of the axis is called os odontoideum and may cause nerve and circulation compression syndrome.[1] On its anterior surface is an oval or nearly circular facet for articulation with that on the anterior arch of the atlas. On the back of the neck, and frequently extending on to its lateral surfaces, is a shallow groove for the transverse atlantal ligament which retains the process in position. The apex is pointed and gives attachment to the apical odontoid ligament. Below the apex, the process is somewhat enlarged and presents on either side a rough impression for the attachment of the alar ligament; these ligaments connect the process to the occipital bone.
The internal structure of the odontoid process is more compact than that of the body. The odontoid peg is the ascension of the atlas fused to the ascension of the axis. The peg has an articular facet at its front and forms part of a joint with the anterior arch of the atlas. It is a non-weight bearing joint. The alar ligaments, together with the apical ligaments, are attached from the sloping upper edge of the odontoid peg to the margins of the foramen magnum. The inner ligaments limit rotation of the head and are very strong. The weak apical ligament lies in front of the upper longitudinal bone of the cruciform ligament and joins the apex of the deltoid peg to the anterior margin of the foramen magnum. It is the fibrous remnant of the notochord.
Other features
[edit]The pedicles are broad and strong, especially in the front, where they coalesce with the sides of the body and the root of the odontoid process. They are covered above by the superior articular surfaces.
The laminae are thick and strong. They play a large role in the stability of the cervical spine alongside the laminae of C7.[2]
The vertebral foramen is large, but smaller than the atlas.
The transverse processes are very small, and each ends in a single tubercle. Each process is perforated by the transverse foramen, which is directed obliquely upward and laterally.
The superior articular surfaces are round, slightly convex, directed upward and laterally, and are supported on the body, pedicles, and transverse processes.
The inferior articular surfaces have the same direction as those of the other cervical vertebrae.
The superior vertebral notches are very shallow, and lie behind the articular processes. The inferior vertebral notches lie in front of the articular processes, as in the other cervical vertebrae.
The spinous process is large, very strong, deeply channelled on its under surface, and presents a bifurcated extremity.
Variation
[edit]Contact sports are contraindicated for individuals with anomalous dens, as any violent impact may result in a catastrophic injury.[3] This is because a malformed odontoid process may lead to instability between the atlas and axis (the C1 and C2 cervical vertebrae).
Development
[edit]
The axis is ossified from five primary and two secondary centres.
The body and vertebral arch are ossified in the same manner as the corresponding parts in the other vertebrae, viz., one centre for the body, and two for the vertebral arch.
The centres for the arch appear about the seventh or eighth week of fetal life, while the centres for the body appear in about the fourth or fifth month.
The dens, or odontoid process, consists originally of a continuation upward of the cartilaginous mass, in which the lower part of the body is formed.
During about the sixth month of fetal life, two centres make their appearance in the base of this process: they are placed laterally, and join before birth to form a conical bilobed mass deeply cleft above; the interval between the sides of the cleft and the summit of the process is formed by a wedge-shaped piece of cartilage.
The base of the process is separated from the body by a cartilaginous disk, which gradually becomes ossified at its circumference, but remains cartilaginous in its center until advanced age.
In this cartilage, rudiments of the lower epiphyseal plate of the atlas, and the upper epiphyseal plate of the axis may sometimes be found.
The apex of the dens has a separate centre that appears in the second and joins about the twelfth year; this is the upper epiphyseal plate of the atlas.
In addition to these, there is a secondary centre for a thin epiphyseal plate on the undersurface of the body of the bone.
Clinical significance
[edit]Fractures
[edit]
A fracture of both pedicles of the axis is termed a Hangman's fracture.
Fractures of the dens are classified into three categories according to the Anderson Alonso system:
- Type I fracture - Extends through the tip of the dens. This type is usually stable.
- Type II fracture - Extends through the base of the dens. It is the most commonly encountered fracture for this region of the axis. This type is unstable and has a high rate of non-union.
- Type III fracture - Extends through the vertebral body of the axis. This type can be stable or unstable and may require surgery.[1]
-
A fracture of the base of the dens as seen on plain X-ray
-
A fracture of the base of the dens as seen on CT
-
Type 3 odontoid fracture
-
Type 2 dens fracture
Additional images
[edit]-
Its shape and position (shown in red) from above. The skull is shown in semi-transparent.
-
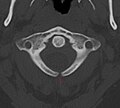
Axis seen from above
-
3D image
-
Posterior atlantooccipital membrane and atlantoaxial ligament; the axis is visible at center.
-
Median sagittal section through the occipital bone and first three cervical vertebra
-
Sagittal section of nose mouth, pharynx, and larynx
-
Axis on X-ray taken through an open mouth, teeth visible
-
Unfused arch of atlas at CT
See also
[edit]References
[edit]![]() This article incorporates text in the public domain from page 99 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 99 of the 20th edition of Gray's Anatomy (1918)
- ^ Jumah, Fareed; Alkhdour, Saja; Mansour, Shaden; He, Puhan; Hroub, Ali; Adeeb, Nimer; Hanif, Rimal; Mortazavi, Martin M; Tubbs, R. Shane; Nanda, Anil (2017). "Os Odontoideum: A Comprehensive Clinical and Surgical Review". Cureus. 9 (8) e1551. doi:10.7759/cureus.1551. ISSN 2168-8184. PMC 5630463. PMID 29018648.
- ^ Pal, G. P.; Routal, R. V. (April 1996). "The role of the vertebral laminae in the stability of the cervical spine". Journal of Anatomy. 188 ( Pt 2) (Pt 2): 485–489. ISSN 0021-8782. PMC 1167584. PMID 8621347.
- ^ Schenck, Robert C., ed. (1999). Athletic Training and Sports Medicine (3 ed.). American Academy of Orthopaedic Surgeons. ISBN 978-0-89203-172-6.
External links
[edit]- Netter, Frank. Atlas of Human Anatomy Archived 2017-11-20 at the Wayback Machine, "High Cervical Spine: C1-C2"
Axis (anatomy)
View on GrokipediaGross anatomy
Vertebral body and dens
The vertebral body of the axis (second cervical vertebra, or C2) is notably short and broad compared to typical cervical vertebrae, serving primarily as a stable base for the projecting dens while bearing significant load from the skull above. Unlike other vertebrae, it lacks a typical intervertebral disc on its superior surface, as this articulation with the atlas (C1) occurs via the dens rather than a disc interface, allowing for enhanced rotational mobility at the atlantoaxial joint.[1][5] The dens, also known as the odontoid process, is a distinctive peg-like bony projection that arises superiorly from the center of the vertebral body, forming a key pivot for head rotation. It features a narrow neck at its base, where it fuses seamlessly with the body, and tapers to a slightly conical apex that provides attachment for the apical ligament of the dens. The dens measures approximately 12-15 mm in height and 8-10 mm in diameter on average, with its superior tip facilitating precise alignment within the atlas ring. The dens is derived embryonically from the centrum of the atlas.[1][5][6][7] Blood supply to the dens is critical for its stability and is derived from ascending and descending branches originating from the vertebral arteries, forming an arcade that enters at the base and apex to nourish the structure. Sensory innervation of the dens arises from branches of the C2 spinal nerve, contributing to proprioception and pain signaling in the upper cervical region.[8][9][10]Arches and processes
The neural arch of the axis vertebra (C2) consists of paired pedicles and laminae that form the posterior boundary of the vertebral foramen, enclosing and protecting the spinal cord. The pedicles are short, robust bony projections that extend posteriorly from the superior aspect of the vertebral body, connecting it to the laminae and transverse processes while featuring superior and inferior vertebral notches that contribute to the intervertebral foramina for spinal nerve passage.[11] The laminae are broad, flattened plates that unite the pedicles dorsally, creating a robust posterior arch distinct from the more delicate laminae of lower cervical vertebrae; they fuse early in development, typically by age 2-3 years, to provide structural integrity.[12][11] The transverse processes of the axis are short and extend laterally from the junction of the pedicles and laminae, each containing a transverse foramen that transmits the vertebral artery, vertebral vein, and sympathetic plexus toward the cranium—a feature unique to the cervical vertebrae. These processes bear anterior and posterior tubercles: the anterior tubercle serves as an attachment site for muscles such as the longus capitis and longus colli, while the posterior tubercle provides anchorage for deeper posterior neck muscles like the splenius cervicis and levator scapulae.[1][11] This configuration supports vascular passage and muscle leverage without extending as prominently as in the atlas (C1). The spinous process of the axis is short, projects posteriorly and slightly inferiorly from the midline fusion of the laminae, and is bifid (Y-shaped) at its tip, similar to C3-C6 but less elongated than in lower vertebrae. It functions primarily as an attachment point for the nuchal ligament superiorly and posterior neck muscles, including the semispinalis capitis, rectus capitis posterior major, and obliquus capitis inferior, which aid in head extension and rotation.[11][12][13] The inferior articular processes arise from the posterolateral junctions of the pedicles and laminae, projecting downward to form convex, oval-shaped facets that articulate with the superior articular processes of the third cervical vertebra (C3). These processes are oriented at approximately 45 degrees to the transverse plane, facilitating flexion, extension, and lateral bending at the C2-C3 joint while contributing to overall cervical stability.[1][12]Articular surfaces and ligaments
The superior articular facets of the axis are located on the superior aspect of the vertebral body, lateral to the dens, and exhibit a sloping orientation that extends over the pedicles, forming bilateral gliding synovial joints with the inferior articular facets of the atlas (C1).[14] These facets are covered in hyaline cartilage and are kidney-shaped or saddle-like, enabling smooth rotational and gliding movements at the lateral atlanto-axial joints.[5] In contrast, the dens of the axis features an anterior articular surface that contacts the fovea dentis, a smooth facet on the anterior arch of the atlas, establishing the anterior aspect of the median atlanto-axial pivot joint.[15] Posteriorly, the dens is held against the anterior arch of the atlas by the transverse atlantal ligament, which arches across the dens to form the pivot mechanism of this joint.[16] The inferior articular facets of the axis arise from the inferior surface of the vertebral body and extend over the pedicles, facing anteroinferiorly in a plane orientation typical of cervical vertebrae, where they articulate with the superior articular facets of the third cervical vertebra (C3) to form standard facet joints.[14] These facets contribute to the overall alignment of the subaxial cervical spine but are distinct from the specialized superior articulations.[5] Several key ligaments stabilize the axis and its articulations with the atlas and occiput. The transverse atlantal ligament, a strong band connecting the lateral masses of the atlas, passes behind the dens to secure it firmly against the anterior arch, preventing anterior displacement.[15] The paired alar ligaments extend from the lateral aspects of the dens to the medial tubercles of the occipital condyles, providing lateral stability to the atlanto-occipital joint.[5] The apical ligament runs from the apex of the dens to the anterior margin of the foramen magnum, offering supplementary tensile support.[14] Collectively, these form part of the cruciform ligament complex, which includes longitudinal bands from the posterior surface of the axis body to the basion of the occiput, enhancing overall craniocervical stability.[15] The capsules of the atlanto-axial joints are fibrous reinforcements surrounding the synovial articulations, with the lateral joint capsules being relatively loose to permit flexion and extension while the median joint capsule integrates with the transverse ligament for rotational pivot action.[16]Development and variation
Embryological origins
The axis vertebra, or C2, exhibits a distinctive embryological origin compared to typical vertebrae, which derive from paired somites of the paraxial mesoderm. Instead, it incorporates contributions from four occipital somites and the first cervical somite, reflecting its transitional role at the craniocervical junction. The proatlas, derived from the fourth occipital somite and the cranial half of the fifth somite, plays a key role in this process, while the caudal half of the sixth somite and the cranial half of the seventh somite form the primary C2 sclerotome.[17][18] The dens, or odontoid process, arises from multiple sclerotomal elements, underscoring its composite nature. Its basal portion develops from the first cervical centrum, contributed by the caudal half of the fifth somite and the cranial half of the sixth somite, while the apical region originates from the proatlas.[17][18] The neural arch of the axis forms from the lateral zones of the second cervical sclerotome, involving both neural crest-derived cells and paraxial mesoderm. These elements migrate around the neural tube and fuse dorsally by the eighth week of gestation, enclosing the spinal cord and establishing the posterior vertebral elements.[17][18] Development begins in the membranous phase around 4 to 5 weeks of gestation, with sclerotomal cells condensing around the notochord and neural tube. Chondrification initiates by 6 weeks, marking the transition to cartilage models, during which the dens temporarily separates from the vertebral body as a distinct entity before reapproximating.[17][18] Disruptions in these processes can lead to developmental anomalies, such as os odontoideum, where incomplete fusion of the dens components results in a separate ossicle, potentially predisposing to atlantoaxial instability.[17][18]Ossification process
The ossification of the axis (C2 vertebra) begins in utero with five primary ossification centers. One center forms in the vertebral body and the base of the dens during the fourth to fifth month of fetal development, while two centers develop in the neural arches during the seventh to eighth week of gestation. An additional two primary centers appear bilaterally in the dens around the sixth month of gestation and fuse with each other in the midline before birth, contributing to the inferior portion of the dens. These primary centers establish the foundational bony structure present at birth.[14][19] Secondary ossification centers emerge postnatally to complete the skeletal maturation. The tip of the dens ossifies from a secondary center between 3 and 6 years of age, fusing to the main body of the dens by approximately 12 years. The inferior epiphysis of the vertebral body develops as another secondary center, appearing around 6 to 8 years and contributing to the lower surface; it fully integrates by early adulthood. These secondary centers ensure the final shaping and strengthening of the axis.[14][20] Fusion of the primary ossification centers follows a specific timeline to achieve structural integrity. The neural arches unite posteriorly by 3 to 6 years of age, while the dens fuses to the vertebral body through the neurocentral synchondroses between 3 and 7 years. Complete skeletal maturity, including the integration of all secondary centers and growth plates, occurs by around 25 years. The neurocentral synchondroses serve as growth plates for lateral expansion of the body and dens, whereas the inferior epiphyseal plate facilitates vertical elongation of the vertebral body during development.[19][20][21] Compared to the atlas (C1), the axis displays a more intricate ossification pattern due to the dens, involving additional primary centers and delayed secondary fusions that accommodate its unique role in rotation and stability.[14]Anatomical variations
The axis vertebra (C2) exhibits several anatomical variations that occur within the normal population range, primarily affecting the dens, posterior arch, and processes. These variations can influence stability at the atlantoaxial joint and are often asymptomatic but may predispose individuals to hypermobility or require consideration during imaging or surgical planning. Variations arise from incomplete ossification or fusion during development, though they are distinct from pathological conditions. Dens variations include os odontoideum, characterized by a separate, well-corticated ossicle at the superior aspect of the C2 body, with the dens base appearing hypoplastic. This variant is rare and often incidental but can lead to atlantoaxial hypermobility due to ligamentous laxity. Dens hypoplasia, involving a shortened or underdeveloped dens (typically less than 4 mm in height), is uncommon and may contribute to subtle instability without overt symptoms. Hypermobile variants of the dens, often associated with os odontoideum, result in increased atlantoaxial translation. Posterior arch variations of the axis are less common but include non-fusion of the laminae, a form of spina bifida occulta, which manifests as a midline defect in the lamina without meningeal protrusion. This occurs rarely at C2, with an estimated prevalence below 1% in the cervical spine, compared to higher rates in lumbosacral regions. Ponticulus posticus, or arcuate foramen formation, is primarily described in the atlas (C1), but analogous partial bony bridging over the vertebral artery groove has been noted in C2 arches in isolated reports, though specific prevalence data for C2 remains limited to case studies. Process variations encompass elongated transverse processes, potentially altering muscle attachments or vascular relations. The spinous process, normally bifid, shows asymmetry or shape variations such as inverted-V, inverted-U, M-shaped, or non-bifid forms, affecting palpation landmarks. Gender differences in axis morphology include slightly larger dens dimensions in males and greater overall vertebral body width, reflecting sexual dimorphism in cervical spine size. Ethnic variations demonstrate morphometric differences in lamina thickness and process length. Computed tomography (CT) is the gold standard for identifying these variations, revealing corticated margins and smooth contours that distinguish benign variants from fractures or erosions, such as the rounded ossicle in os odontoideum versus irregular fracture lines. Magnetic resonance imaging (MRI) complements CT by assessing soft tissue implications, like ligament integrity in hypermobile cases, with T2-weighted sequences highlighting any associated edema or instability without radiation exposure.Function and biomechanics
Role in cervical motion
The axis vertebra (C2) serves as the primary pivot point for cervical rotation through the atlanto-axial joint, where its dens acts as a fulcrum enabling approximately 50% of the total rotational range of the cervical spine. This joint accounts for 40-70 degrees of axial rotation overall, facilitating essential head-turning movements such as the "no" gesture.[22][23] In terms of kinematics, the dens of the axis provides a stable central axis around which the atlas (C1) rotates, with the lateral atlanto-axial facet joints allowing the atlas's lateral masses to glide and translate slightly during motion; coupled flexion-extension at this level remains minimal, typically under 10 degrees, to prioritize pure rotation.[1][23] Key muscles controlling this motion include the suboccipital group, particularly the obliquus capitis inferior for ipsilateral rotation and the rectus capitis posterior major for stabilization during turns, while the splenius capitis contributes to extension coupled with rotation. The alar ligaments, which connect the dens to the occiput, primarily limit excessive axial rotation to prevent overextension.[23] The range of motion at the atlanto-axial joint is approximately 40-70 degrees of axial rotation total, significantly greater than the 10-15 degrees per level observed at C3-C7 segments, where rotation is more distributed and coupled with other motions.[23][24]Stability mechanisms
The axis vertebra (C2) maintains spinal integrity primarily through ligamentous structures that resist displacement and distribute loads, supplemented by muscular and neural elements for dynamic support. In neutral posture, the dens transmits compressive loads from the head to the body of C3 via associated ligaments, with biomechanical models indicating that ligamentous contributions can account for a variable portion of the total axial load, depending on posture and facet contact.[11] Key ligaments include the transverse ligament, which encircles the dens posteriorly and resists anterior subluxation by holding the dens against the anterior arch of C1; its tensile strength has been measured at approximately 350 N before rupture in cadaveric studies.[25] The paired alar ligaments, extending from the dens apex to the occipital condyles, limit excessive lateral tilt (contralateral lateral flexion) and axial rotation at the atlanto-occipital and atlantoaxial joints, providing secondary stabilization to the craniocervical junction.[26] These ligaments work in concert with articular facets, which offer congruent surfaces for load sharing and initial resistance to shear forces.[11] Muscular contributions to stability come from deep cervical flexors, such as the longus capitis and rectus capitis anterior, and extensors, including the rectus capitis posterior major and minor, which originate from or near C2 and provide dynamic control against translational and rotational perturbations.[27][28] These muscles generate tonic activity to fine-tune posture and counteract gravitational or inertial forces, enhancing overall segmental stability without restricting physiological motion.[29] Proprioceptive feedback from mechanoreceptors in C2 ligaments, joint capsules, and attached muscles, including nerve endings from the C2 spinal nerve, supports position sense and balance by relaying afferent signals to the central nervous system for reflexive adjustments.[30] This sensory input is crucial for maintaining equilibrium during head movements. Instability arises when these mechanisms fail, such as ligamentous laxity increasing the atlanto-dens interval beyond 3 mm on imaging, which signifies potential anterior translation and compromised integrity.[31]Clinical significance
Fractures and trauma
Fractures of the axis vertebra, also known as C2 fractures, represent approximately 20% of all acute cervical spine injuries and are often associated with high-energy trauma. These fractures primarily involve the odontoid process or the pars interarticularis, leading to potential instability at the atlantoaxial joint. Neurological deficits are uncommon, occurring in approximately 5-15% of cases, often due to associated injuries rather than the axis fracture alone, and most axis fractures do not directly compromise the spinal cord due to the large canal diameter at this level.[32][33][34] The main types of axis fractures include odontoid process fractures and hangman's fractures. Odontoid fractures are classified into three types based on location: Type I involves a rare oblique avulsion of the odontoid apex (approximately 5% of cases), Type II is the most common transverse fracture at the base (about 65%), and Type III extends into the vertebral body (around 30%). Hangman's fractures consist of bilateral pedicle fractures through the pars interarticularis, resulting in traumatic spondylolisthesis of C2 on C3.[35][32][36] These injuries typically arise from high-energy mechanisms, with road traffic accidents accounting for roughly 60-65% of cases. Odontoid Type II and III fractures often result from flexion forces combined with axial loading, while hangman's fractures are caused by hyperextension injuries, such as those from sudden deceleration. Falls from height and sports-related impacts represent other common etiologies.[37][38][36] Classification systems guide assessment of stability and management. For odontoid fractures, the Anderson and d'Alonzo system delineates the anatomical subtypes, with Type II fractures being particularly prone to nonunion due to poor vascularity at the base. Recent advancements include the AO Spine Upper Cervical Injury Classification System (2025), which incorporates modifiers for prognostication and treatment planning. Hangman's fractures are classified using the Effendi (or modified Levine-Edwards) scheme, which differentiates stable Type I fractures (minimal displacement <3 mm, no angulation) from unstable Type II (significant anterolisthesis >3 mm with angulation) and Type III (with associated facet dislocation).[35][33][39][40] Diagnosis relies on imaging to delineate fracture morphology and associated soft tissue injuries. Computed tomography (CT) is the gold standard for visualizing fracture lines and alignment, often detecting subtle disruptions missed on plain radiographs. Magnetic resonance imaging (MRI) is indicated to assess ligamentous integrity, particularly the transverse atlantal ligament in odontoid fractures, and to evaluate for cord or vascular compromise in symptomatic patients.[41][33][42] Initial management emphasizes immobilization to promote healing and prevent displacement, with non-operative approaches suitable for most stable fractures. Type I and III odontoid fractures, as well as Type I hangman's fractures, are typically treated conservatively with a rigid cervical collar for 6-12 weeks, achieving union rates over 90% in uncomplicated cases. Halo vest immobilization is reserved for more unstable patterns or elderly patients, providing rigid external fixation during the healing period.[32][33][43]Associated conditions
Atlantoaxial instability is a congenital condition frequently associated with Down syndrome, where ligamentous laxity at the C1-C2 junction predisposes individuals to excessive motion between the atlas and axis vertebrae. This instability affects approximately 10-20% of people with Down syndrome, though most cases remain asymptomatic.[44] In rheumatoid arthritis, a related form of atlantoaxial subluxation can occur due to chronic synovitis, characterized by anterior migration of the dens exceeding 5 mm on imaging, which compromises spinal cord space and may lead to neurological deficits if untreated.[45] Degenerative changes in the axis primarily involve osteoarthritis of the facet joints, which can narrow the spinal canal and contribute to foraminal stenosis. This condition becomes prevalent in over 85% of individuals aged 60 and older, often manifesting as chronic neck pain, reduced range of motion, and radiculopathy from nerve root compression.[46] Inflammatory arthropathies also target the axis, with rheumatoid arthritis commonly leading to pannus formation—a proliferative synovial tissue that erodes the odontoid process and surrounding structures. This erosion occurs in 43-47% of rheumatoid arthritis patients with cervical involvement, potentially causing basilar invagination and myelopathy.[47] Psoriatic arthritis similarly affects the cervical spine, including the axis, in up to 36% of cases with axial disease, resulting in erosions, ankylosis, or instability that mimics ankylosing spondylitis.[48] Tumors involving the axis are rare but significant, such as chordoma originating from notochordal remnants at the C2 level. These slow-growing neoplasms typically present with localized neck pain radiating to the shoulders or arms, progressing to myelopathy with symptoms like gait disturbance, sensory loss, and upper extremity weakness due to spinal cord compression.[49] Diagnosis of these axis-related conditions often relies on dynamic flexion-extension X-rays to assess instability, particularly measuring the atlantodental interval (ADI), where a normal value is less than 3 mm in adults; values exceeding this indicate potential ligamentous compromise requiring further evaluation with MRI.[50]Surgical considerations
Surgical interventions for the axis vertebra are primarily indicated for unstable Type II odontoid fractures, which carry a non-union risk of approximately 30% with conservative management, particularly in patients over 50 years old. Other key indications include irreducible atlantoaxial dislocations with neurologic deficits or instability (e.g., atlanto-dental interval >5 mm) and tumor resection requiring decompression and stabilization. Recent techniques, such as anterior atlantoaxial motion preservation fixation (introduced in 2024), aim to stabilize fractures while preserving rotation.[51][52][53][54] Common surgical approaches for axis-related instability involve posterior C1-C2 fusion techniques, such as the Gallie method, which uses sublaminar wiring under the C1 posterior arch looped around the C2 spinous process with on-lay bone grafting to achieve stability.[55] Instrumentation often employs Magerl transarticular screws for bicortical purchase across the C1-C2 joint, providing robust fixation while allowing bone graft placement for arthrodesis.[56] For select Type II odontoid fractures, an anterior approach with single-screw odontoid fixation is utilized, involving percutaneous or open insertion of a lag screw to compress the fracture site and preserve atlantoaxial motion.[57] Potential complications of these procedures include non-union rates of 10-20%, with higher incidence following anterior odontoid screw fixation compared to posterior methods.[58] Vertebral artery injury occurs in 1-2% of cases during posterior transarticular screw placement due to anatomical variations in the vessel course.[59] The anterior approach is associated with postoperative dysphagia in up to 10% of patients, often transient but requiring careful monitoring.[58] With modern instrumentation like polyaxial screw-rod constructs, fusion rates for posterior C1-C2 procedures reach 94-100%, significantly improving stability over traditional wiring.[60] Rehabilitation typically spans 3-6 months, beginning with immobilization in a cervical collar for 6-8 weeks to promote healing, followed by gradual mobilization and physical therapy to restore function while avoiding excessive axial loading.[61]References
- https://wikimsk.org/wiki/Atlanto-axial_Joint