Recent from talks
Nothing was collected or created yet.
Superficial temporal vein
View on Wikipedia| Superficial temporal vein | |
|---|---|
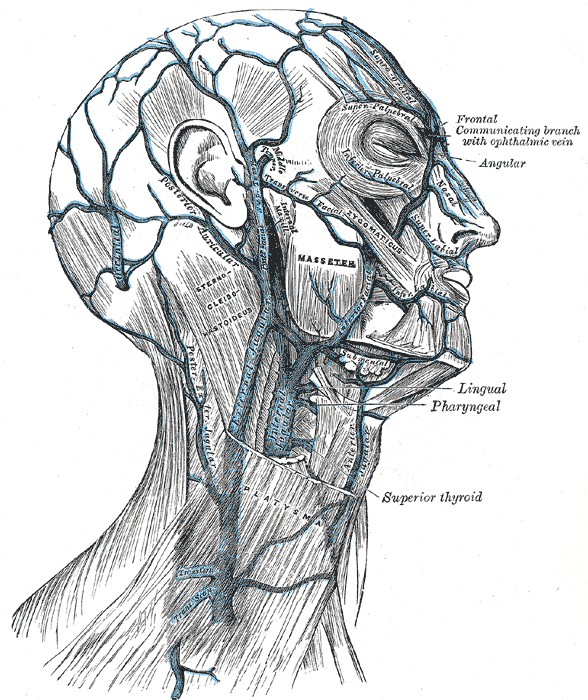
 Veins of the head and neck. ("Sup. Temp." labeled at center, anterior to the ear.) | |
 Bloodvessels of the eyelids, front view. (13, at left, is branch of the superficial temporal vein.) | |
| Details | |
| Drains from | Temple, scalp |
| Drains to | Retromandibular vein |
| Artery | Superficial temporal artery |
| Identifiers | |
| Latin | venae temporales superficiales |
| TA98 | A12.3.05.032 |
| TA2 | 4832 |
| FMA | 70849 |
| Anatomical terminology | |
The superficial temporal vein is a vein of the side of the head which collects venous blood from the region of the temple.[1]: 355 It arises from an anastomosing venous plexus on the side and top of the head. The superficial temporal vein terminates within the substance of the parotid gland[citation needed] by uniting with the maxillary vein to form the retromandibular vein.[1]: 364
Structure
[edit]It begins on the side and vertex of the skull in a network (plexus) which communicates with the frontal vein and supraorbital vein, with the corresponding vein of the opposite side, and with the posterior auricular vein and occipital vein.
From this network frontal and parietal branches arise, and join above the zygomatic arch to form the trunk of the vein, which is joined by the middle temporal vein emerging from the temporalis muscle.
It then crosses the posterior root of the zygomatic arch, enters the substance of the parotid gland where it unites with the internal maxillary vein to form the posterior facial vein.
Tributaries
[edit]Tributaries of the superficial temporal vein drain venous blood from the temple.[2]
Tributaries of the superficial temporal vein include:
- some parotid veins
- articular veins of the temporomandibular joint
- anterior auricular veins from the auricula
- the transverse facial vein from the side of the face
References
[edit]![]() This article incorporates text in the public domain from page 645 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 645 of the 20th edition of Gray's Anatomy (1918)
- ^ a b Sinnatamby, Chummy S. (2011). Last's Anatomy (12th ed.). ISBN 978-0-7295-3752-0.
- ^ Sinnatamby, Chummy S. (2011). Last's Anatomy (12th ed.). ISBN 978-0-7295-3752-0.
External links
[edit]- lesson4 at The Anatomy Lesson by Wesley Norman (Georgetown University) (parotid2)
- Diagram at Tufts.edu
- Diagram at stchas.edu
Superficial temporal vein
View on GrokipediaAnatomy
Origin
The superficial temporal vein arises from an anastomosing venous plexus situated on the lateral aspect of the head, encompassing the side and vertex of the skull over the temple and scalp regions.[2] This plexus collects deoxygenated blood from the superficial tissues of the temporal and parietal scalp, facilitating drainage from the superficial layers of the integument.[3] The network extends across the temporal fossa toward the superior auricular region, providing extensive interconnections among superficial veins of the scalp.[4] The vein proper forms through the union of its frontal and parietal branches, which emerge from the aforementioned plexus and converge to establish the main trunk.[2] These branches drain the anterior (frontal) and posterior (parietal) portions of the temporal scalp, respectively, ensuring comprehensive venous return from the superficial temporal area.[4] This origin plexus communicates with the frontal vein system via the supratrochlear and supraorbital veins, located at the medial forehead, allowing for collateral flow across the midline of the scalp.[2] Such anastomoses enhance the robustness of superficial venous drainage in the head.[4]Course
The superficial temporal vein forms its main trunk through the union of its frontal and parietal branches above the zygomatic arch. From this point, the vein descends vertically along the anterior aspect of the auricle.[5][2] It crosses the posterior root of the zygomatic arch superficially and runs parallel to, and often superficial to, the superficial temporal artery during its descent.[2][5][6] The vein maintains this trajectory until it reaches the parotid region, where it enters the substance of the parotid gland and shifts from a superficial to a deeper position within the gland.[5][2][3] The course from the union of the branches to entry into the parotid gland measures a mean harvestable length of 6.5 cm. Its diameter shows interindividual variation, with a median of 1.3 mm and a range of 0.5–2 mm.[7]Tributaries
The superficial temporal vein receives several key tributaries that augment its collection of venous blood from the temporal and periauricular regions, maintaining its superficial drainage pathway. The primary tributary is the middle temporal vein, which drains the temporalis muscle and the lateral aspect of the temporal scalp.[6][3] Additional inputs include the anterior auricular veins, which collect blood from the anterior portion of the external ear, and small emissary veins emerging from the temporal bone foramina, providing valveless connections to the intracranial dural venous sinuses such as the superior sagittal sinus via the parietal emissary pathway.[3][1] The vein's formation from the frontoparietal venous plexus on the side and vertex of the skull incorporates indirect drainage from the lateral aspects of the frontal and parietal emissary networks, enhancing regional scalp venous return without direct deep connections.[3][1] Notably, the superficial temporal vein lacks major deep tributaries, relying instead on these primarily superficial sources to support its essential role in draining the scalp, temple, and superficial temporal structures.[6][1]Termination
The superficial temporal vein terminates by uniting with the maxillary vein within the substance of the parotid gland to form the retromandibular vein.[8][9][10] This union occurs posterior to the ramus of the mandible and deep to the parotid fascia, integrating the superficial temporal drainage into the deeper venous network of the face.[8][11] The newly formed retromandibular vein descends through the parotid gland, superficial to the external carotid artery and deep to the facial nerve branches.[8][9] At the inferior pole of the parotid gland, it typically bifurcates into an anterior division and a posterior division.[8][9] The anterior division joins the facial vein to form the common facial vein, which drains into the internal jugular vein.[8][9] The posterior division unites with the posterior auricular vein to contribute to the external jugular vein, which ultimately empties into the subclavian vein; in some variations, the posterior division may drain directly into the external jugular vein.[8][9] This dual drainage pathway ensures efficient return of venous blood from the temporal scalp, lateral face, and parotid region to the central venous system.[12]Relations
To arteries
The superficial temporal vein runs parallel to the superficial temporal artery along its course from the zygomatic arch to the parotid gland, maintaining a close anatomical proximity that forms part of a neurovascular bundle essential for surgical navigation in the temporal region.[13][14] This parallelism is evident in the temporal fascia, where the vein and artery are closely associated, facilitating shared drainage and supply to the scalp and face.[14] The vein typically lies superficial to the artery, which underscores the need for precise dissection to avoid vascular injury during procedures like temporal artery biopsy.[14] At the zygomatic arch crossing, this configuration aids in identifying the structures during preauricular incisions.[13] This bundled arrangement includes the auriculotemporal nerve posterior to both vessels.[13] In the parotid region, the vein accompanies the superficial temporal artery.[1]To other structures
The superficial temporal vein lies superficial to the auriculotemporal nerve along much of its course in the temporal region.[1] The auriculotemporal nerve typically crosses posterior to the vein near the zygomatic arch, with superficial intersections (nerve superficial to the vein and accompanying artery) observed in approximately 84% of cases, while deep crossings occur in about 16%.[13] This crossing takes place as the vein descends over the zygomatic arch, as detailed in its overall course. Within the parotid gland, the superficial temporal vein traverses the glandular substance and lies adjacent to branches of the facial nerve, which divide the gland into superficial and deep lobes.[15] The temporal and zygomatic branches of the facial nerve course nearby, separating the vein's entry point superiorly from deeper glandular structures.[1] At the level of the zygomatic arch, the superficial temporal vein relates superiorly to the temporalis fascia, lying superficial to it as it emerges from the temporal fossa.[1] Inferiorly, it positions above the masseter muscle, crossing the arch just anterior to the external auditory meatus and avoiding direct contact with the muscle belly below.[1] During its passage through the parotid gland, the superficial temporal vein maintains a lateral position relative to the parotid duct, which emerges from the anterior gland border.[15]Clinical significance
Surgical relevance
The superficial temporal vein holds significant surgical importance in procedures involving the parotid gland and temporomandibular joint (TMJ) due to its anatomical position within the parotid parenchyma and its crossing over the zygomatic arch. In parotidectomy, particularly deep lobe resections, the vein converges with the maxillary vein to form the retromandibular vein, necessitating ligation to prevent intraoperative hemorrhage during dissection deep to this structure.[16] Similarly, in TMJ surgeries such as arthroscopy or open joint procedures, the vein lies adjacent to the posterior joint capsule, where it is routinely identified, ligated, and divided to minimize bleeding risks during preauricular approaches.[18] In microvascular reconstruction, the superficial temporal vein serves as a preferred recipient vessel for free flap anastomoses in facial and scalp defects, owing to its reliable caliber of approximately 2-3 mm and superficial accessibility above the temporalis fascia.[19][19] This allows for straightforward end-to-end or end-to-side connections with donor veins from flaps like the anterolateral thigh or radial forearm, facilitating successful revascularization in head and neck oncology cases.[20] During rhytidectomy (facelift), the vein's superficial course in the temporal region requires meticulous dissection to avoid vascular injury, which can lead to expanding hematomas—a common postoperative complication.[21] Preservation or ligation of the vein, often encountered during SMAS elevation, helps mitigate hematoma formation rates, which can exceed 7% in males without careful hemostasis. Historically, the superficial temporal vein was described in Gray's Anatomy (1918 edition) as a key landmark for head and neck dissections, running parallel to the superficial temporal artery from the scalp to the parotid gland. In contemporary practice, preoperative ultrasound with Doppler imaging enables precise mapping of the vein's course and patency, aiding surgical planning and reducing complications in vascularly complex regions like the parotid, where it relates superficially to the facial nerve branches.[22]Pathological conditions
Superficial thrombophlebitis of the superficial temporal vein is a rare condition characterized by inflammation and thrombus formation in this superficial vessel, often presenting with localized pain, swelling, and erythema over the temporal region.[23] Risk factors include local trauma, such as prolonged pressure from lying on the ground, or iatrogenic factors like indwelling catheters, as seen in case reports of bilateral thrombosis following carbon monoxide poisoning.[23] Additionally, infections such as acute rhinosinusitis can lead to thrombophlebitis in the temporal vein as an extracranial complication, confirmed by duplex ultrasonography showing thrombotic occlusion.[24] In head and neck superficial vein thrombosis cases, including the superficial temporal vein, there is a potential for extension into deep venous systems, which may propagate to the cavernous sinus via connections like the retromandibular vein, resulting in life-threatening cavernous sinus thrombosis if untreated. This risk underscores the importance of monitoring for septic propagation in facial or sinus infections, where atypical thrombophlebitis patterns can extend intracranially.[25] Iatrogenic injury to the superficial temporal vein can arise during temporal artery biopsies or dermal filler injections in the temporal region, leading to ecchymosis, hematoma formation, or rarely, thrombosis and embolism risk due to vascular puncture.[26][27] Such complications typically manifest as localized bruising and swelling, with vascular occlusion risks heightened by the proximity to superficial temporal vessels during cosmetic procedures.[28]References
- https://www.sciencedirect.com/topics/[neuroscience](/page/Neuroscience)/superficial-temporal-vein