Recent from talks
All channels
Be the first to start a discussion here.
Be the first to start a discussion here.
Be the first to start a discussion here.
Be the first to start a discussion here.
Welcome to the community hub built to collect knowledge and have discussions related to RANKL.
Nothing was collected or created yet.
RANKL
View on Wikipediafrom Wikipedia
Not found
RANKL
View on Grokipediafrom Grokipedia
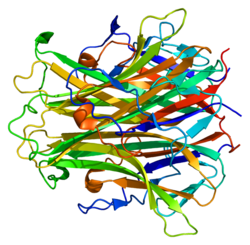
RANKL (Receptor Activator of Nuclear Factor Kappa-B Ligand), also known as TNFSF11, is a cytokine belonging to the tumor necrosis factor (TNF) superfamily that exists as a type II transmembrane protein and a soluble form, encoded by a gene on chromosome 13q14.11 and consisting of 317 amino acids that form a homotrimeric structure essential for its biological activity.[1][2] Discovered in the late 1990s initially as TNF-related activation-induced cytokine (TRANCE) for its role in T-cell activation of dendritic cells, RANKL primarily functions by binding to its receptor RANK on the surface of osteoclast precursors and mature osteoclasts, thereby regulating bone homeostasis through osteoclast differentiation, activation, and survival.[1][3]
In bone metabolism, RANKL is predominantly expressed by osteoblasts, osteocytes, and bone marrow stromal cells, where its expression is upregulated by factors such as parathyroid hormone (PTH) and interleukins during inflammatory conditions, leading to enhanced bone resorption critical for skeletal remodeling and repair.[1][3] The binding of RANKL to RANK triggers intracellular signaling via adaptor protein TRAF6, activating pathways including NF-κB, JNK, and NFATc1, which collectively drive the fusion of monocyte-macrophage precursors into multinucleated osteoclasts capable of degrading bone matrix.[3] Dysregulation of RANKL contributes to pathological conditions like osteoporosis, where elevated levels accelerate bone loss, and rheumatoid arthritis, where synovial fibroblasts and activated T cells overexpress RANKL to promote joint destruction.[1][3] Its activity is tightly controlled by osteoprotegerin (OPG), a decoy receptor that sequesters RANKL and prevents excessive osteoclastogenesis.[3]
Beyond bone, RANKL exerts diverse functions in the immune system, including the development and organization of lymphoid tissues such as the thymus and lymph nodes, where it supports medullary thymic epithelial cell expansion and T-cell maturation.[1] Expressed at high levels in lymphoid organs like lymph nodes and thymus, as well as in activated immune cells, RANKL facilitates dendritic cell survival and enhances interactions between T cells and antigen-presenting cells during immune responses.[1][3] Additionally, RANKL influences extraskeletal processes, such as mammary gland development during lactation through osteoclast-mediated remodeling, regulation of fever via hypothalamic signaling, vascular calcification, and even tumorigenesis in cancers like multiple myeloma and breast cancer, where it promotes bone metastasis.[1] These multifaceted roles underscore RANKL's importance as a therapeutic target, exemplified by denosumab, a monoclonal antibody that inhibits RANKL to treat osteoporosis and bone metastases.[1]