Recent from talks
Be the first to start a discussion here.
Be the first to start a discussion here.
Be the first to start a discussion here.
Be the first to start a discussion here.
Contribute something
Welcome to the community hub built to collect knowledge and have discussions related to Oxolamine.
Nothing was collected or created yet.
Oxolamine
View on Wikipediafrom Wikipedia
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | International Drug Names |
| ATC code | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.012.267 |
| Chemical and physical data | |
| Formula | C14H19N3O |
| Molar mass | 245.326 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Oxolamine is a cough suppressant[1] that is available as a generic drug in many jurisdictions.[2]
Oxolamine also has anti-inflammatory activity, which causes a reduction in irritation of the nerve receptors of the respiratory tract.[3]
It is mainly used for the treatment of pharyngitis, tracheitis, bronchitis, bronchiectasis and pertussis.[3]
Oxolamine is not approved in the USA, it may be marketed elsewhere internationally as a cough suppressant. It is listed as a prescription drug in New Zealand legislation. Oxolamine is also approved in Taiwan for the treatment of respiratory tract inflammation.[4]
References
[edit]- ^ de Groot AC (2022). "3.357 Oxolamine". Systemic Drugs. Monographs in Contact Allergy. Vol. 4 (First ed.). CRC Press. p. 712. ISBN 978-1-00-054991-1.
- ^ "Oxolamine". drugs.com. 19 April 2015. Archived from the original on 20 September 2018. Retrieved 23 January 2018.
- ^ a b "NCATS Inxight Drugs — OXOLAMINE CITRATE". drugs.ncats.io. Archived from the original on 2022-09-26. Retrieved 2022-09-26.
- ^ "Oxolamine". go.drugbank.com. Archived from the original on 2022-09-26. Retrieved 2022-09-26.
Oxolamine
View on Grokipediafrom Grokipedia
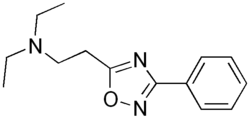
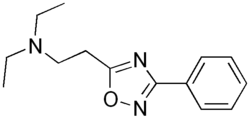
Oxolamine is a synthetic non-opioid antitussive agent primarily used for the symptomatic relief of cough associated with upper respiratory tract inflammation and infections.[1] It belongs to the class of 1,2,4-oxadiazole derivatives and acts predominantly through peripheral mechanisms to suppress cough reflexes, particularly in response to bronchial irritation rather than central neural stimulation.[2]
Chemically known as 5-[2-(diethylamino)ethyl]-3-phenyl-1,2,4-oxadiazole, oxolamine has the molecular formula C14H19N3O and a molecular weight of 245.32 g/mol.[3] Beyond its antitussive effects, it exhibits additional pharmacological properties including analgesic, anti-inflammatory, local anesthetic, and antispasmodic actions.[2] These properties contribute to its utility in conditions like laryngitis, pharyngitis, sinusitis, and tonsillitis when combined with other agents such as propyphenazone.[1] It is administered orally in forms such as syrups, tablets, or capsules, with typical dosing around 200 mg four times daily, though sustained-release formulations have been developed to reduce gastrointestinal side effects like nausea and vomiting.[4]
Oxolamine demonstrates low acute and chronic toxicity in experimental studies, with no significant side effects observed in preclinical trials, though post-marketing reports have linked it to rare hallucinations in children when used in cough mixtures.[2][5] Clinical evidence for its efficacy is limited, primarily relying on older single-blind or observational studies rather than robust randomized controlled trials.[6] It is not approved by the U.S. Food and Drug Administration but is available as a prescription medication in countries including New Zealand and Taiwan as of 2025, classified under ATC code R05DB07 for other cough suppressants.[1]
Medical Uses
Indications
Oxolamine is primarily indicated as an antitussive for the symptomatic relief of dry, non-productive coughs associated with upper and lower respiratory tract infections.[1] It is particularly effective in suppressing irritative coughs without promoting expectoration, making it suitable for acute conditions where cough productivity is not desired. Specific indications include pharyngitis, tracheitis, bronchitis, bronchiectasis, pertussis, and acute respiratory inflammation.[7] These applications target inflammatory and irritative processes in the respiratory system, where oxolamine helps alleviate cough symptoms stemming from irritation of the bronchial mucosa or upper airways.[8] Typical oral dosages for adults range from 50 to 100 mg three to four times daily, or 5 to 10 mL of 10 mg/mL syrup every 4 to 6 hours, not exceeding 400 mg per day; pediatric doses are weight-adjusted (e.g., 7.5 mg/kg/day divided into three doses for children over 4 months), with treatment limited to 5-7 days to avoid prolonged use.[9] Clinical studies support its efficacy in reducing cough frequency and severity in respiratory infections; for instance, a randomized, placebo-controlled trial in patients with chronic obstructive pulmonary disease (COPD) demonstrated that oxolamine significantly lowered cough reflex sensitivity to inhaled capsaicin, with corresponding reductions in subjective cough severity scores, though overall symptom improvements were not always statistically significant across all measures.[10] Earlier investigations have similarly confirmed its antitussive action in acute tracheobronchitis, highlighting decreased cough episodes compared to baseline.[11]Contraindications and Precautions
Oxolamine is contraindicated in patients with known hypersensitivity to the drug or any of its components, as this may lead to allergic reactions.[12] It is also absolutely contraindicated in individuals with severe hepatic impairment due to the risk of exacerbated toxicity from impaired metabolism.[13] Caution is advised in patients with severe renal impairment due to potential reduced clearance, which could prolong exposure and increase adverse effects; no routine dose adjustment is required, but close monitoring is recommended.[14] Relative contraindications include use during pregnancy, where oxolamine should only be administered if the potential benefits outweigh the risks, as limited data exist on fetal safety; it is not classified under a specific FDA category but aligns with cautious use similar to Category C recommendations.[13] During lactation, it is relatively contraindicated unless deemed necessary by a physician, given potential excretion into breast milk and unknown effects on infants.[15] Oxolamine is contraindicated in children under 2 years of age due to insufficient safety and efficacy data in this population.[13] Precautions are advised in elderly patients, where monitoring for excessive sedation is essential due to age-related increases in sensitivity to central nervous system effects.[13] Concurrent use with alcohol or other CNS depressants should be avoided to prevent additive drowsiness and impaired psychomotor function.[16] Drug interactions necessitate caution with monoamine oxidase inhibitors (MAOIs), tricyclic antidepressants, and other antitussives, as oxolamine may potentiate their effects, leading to enhanced sedation or serotonin-related risks.[12] In patients with renal or hepatic dysfunction, recommendations for dose adjustment are limited; while no specific modifications are typically required based on available pharmacokinetic data showing no described need for alterations, close monitoring is recommended to account for potential changes in elimination half-life and clearance.[13]Pharmacology
Mechanism of Action
Oxolamine exerts its antitussive effects predominantly through a peripheral mechanism of action, targeting receptors in the respiratory tract to suppress the cough reflex. Experimental studies in animals demonstrated that oxolamine is more effective at inhibiting cough elicited by diffuse bronchial stimulation, such as via citric acid aerosol, compared to cough induced by central electrical stimulation of the superior laryngeal nerve, indicating primary action at peripheral sites in the airways rather than the brainstem.[17] The compound's local anesthetic properties play a key role in reducing bronchial irritation by desensitizing sensory nerve endings in the respiratory mucosa, thereby diminishing the stimuli that trigger coughing. Additionally, oxolamine exhibits analgesic and anti-inflammatory effects that alleviate inflammation in the bronchial tree, contributing to overall cough suppression in conditions involving airway irritation. These anti-inflammatory actions have been observed in animal models of respiratory inflammation.[17][2] Oxolamine also inhibits cytochrome P450 enzymes CYP2B1 and CYP2B2, which can influence the metabolism of co-administered drugs. In male rats, this inhibition significantly increases the area under the curve (AUC) of warfarin and phenytoin, substrates of these enzymes, potentially leading to altered pharmacokinetics and elevated drug levels. No such effect was observed in female rats, highlighting a gender-specific interaction.[18]Pharmacokinetics
Oxolamine is rapidly absorbed from the gastrointestinal tract following oral administration. Peak plasma concentrations are attained relatively quickly, supporting its prompt onset of antitussive action.[19] The drug is widely distributed throughout the body, reflecting its moderate lipophilicity. Human pharmacokinetic data is limited, with much of the available information derived from animal studies or small clinical observations.[1][20] Metabolism of oxolamine occurs primarily in the liver, leading to the formation of inactive metabolites; the exact cytochrome P450 isoenzymes involved are unknown. The elimination half-life is relatively short, allowing for dosing intervals that maintain therapeutic levels without excessive accumulation.[18][19] Excretion is predominantly renal, with metabolites eliminated in the urine, alongside minor fecal elimination. Dose adjustments may be recommended in patients with renal impairment to prevent potential accumulation.[20]Chemistry
Chemical Structure and Properties
Oxolamine has the molecular formula C₁₄H₁₉N₃O and a molecular weight of 245.32 g/mol.[1] The chemical structure of oxolamine is N,N-diethyl-2-(3-phenyl-1,2,4-oxadiazol-5-yl)ethanamine, featuring a central 1,2,4-oxadiazole heterocyclic ring substituted with a phenyl group at the 3-position and a 2-(diethylamino)ethyl chain at the 5-position.[21] This structure includes a tertiary amine group and an aromatic phenyl ring, contributing to its pharmacological profile. In its free base form, oxolamine is a colorless to pale yellow solid with a melting point of 25°C and a boiling point of 127°C at 0.4 mmHg.[22] It exhibits moderate lipophilicity, with a calculated logP value of approximately 2.6–2.9.[23] Oxolamine is commonly formulated as the citrate salt to enhance solubility, appearing as a white to off-white crystalline powder with a melting point of 141–143°C. The citrate salt shows improved water solubility compared to the free base, which is sparingly soluble in water, while both forms dissolve well in organic solvents such as methanol and DMSO.[24] Under normal storage conditions (cool, dry, and protected from light), oxolamine and its citrate salt remain stable, with a shelf life exceeding three years when properly handled.[25]Synthesis
The primary synthesis route for oxolamine involves the formation of the 1,2,4-oxadiazole ring from benzamidoxime and a three-carbon acyl chain bearing a leaving group, followed by nucleophilic substitution. Specifically, benzamidoxime is acylated at the oxygen with 3-chloropropionyl chloride under basic conditions to favor O-acylation due to the alkoxide form; the intermediate then undergoes intramolecular cyclization where the amidoxime nitrogen displaces the chloride, yielding 5-(2-chloroethyl)-3-phenyl-1,2,4-oxadiazole. This chloromethyl intermediate is subsequently treated with diethylamine in the presence of a base such as potassium carbonate to effect nucleophilic substitution, affording oxolamine in good yield.[26][27] An alternative synthetic approach utilizes 3-chloropropanoic anhydride instead of the acid chloride for the acylation step, employing HClO4 supported on silica (HClO4-SiO2, 5 mol%) as a heterogeneous catalyst to promote the reaction at 80°C for 8 minutes, followed by treatment with potassium iodide in acetonitrile at room temperature for 30 minutes to facilitate cyclization. The resulting 5-(2-chloroethyl) intermediate is then reacted with diethylamine hydrochloride and potassium carbonate under reflux in acetonitrile for 2.5 hours, providing oxolamine after purification by column chromatography with a hexane/ethyl acetate eluent (7:3 to 8:2 ratio). This method achieves an overall yield of 84% and highlights the use of recyclable catalysts for efficiency.[28] Key reagents in these routes include benzamidoxime (derived from benzonitrile and hydroxylamine), 3-chloropropionyl chloride or anhydride, potassium iodide (in modern variants), diethylamine or its hydrochloride salt, and bases like potassium carbonate; reaction conditions typically involve aprotic solvents such as acetonitrile or ether, with temperatures ranging from room temperature to reflux, and overall yields reported between 70% and 85% depending on purification steps.[28][26] The original synthesis of oxolamine was described in German patent DE 1 097 998, granted to Aziende Chimiche Riunite Angelini Francesco A.C.R.A.F. in 1961, which details the cyclization and substitution steps central to its production.[27]Adverse Effects and Safety
Common Side Effects
Oxolamine is associated with several common mild adverse reactions, primarily affecting the gastrointestinal tract. Gastrointestinal disturbances represent the typical category of side effects, including nausea, vomiting, diarrhea, and mild abdominal discomfort or pain. These symptoms are generally transient and resolve upon discontinuation of the medication. Constipation may also arise, especially with prolonged use.[29][30][4] Headache is an additional occasional complaint. Post-marketing reports indicate rare hallucinations, particularly in children when used in cough mixtures.[5]Toxicity and Overdose
Oxolamine demonstrates low acute toxicity in animal models, with an oral LD50 of 1650 mg/kg reported in rats.[31] Human overdose symptoms primarily involve nervous system disturbances such as excessive drowsiness, confusion, lethargy, and visual hallucinations (particularly in children), alongside gastrointestinal effects including nausea, vomiting, epigastric pain, and diarrhea, as well as tachycardia.[29] Few documented cases of oxolamine overdose exist in the medical literature, and those reported are typically mild, attributable in part to the drug's short plasma half-life.[19] Oxolamine may enhance the anticoagulant effects of warfarin, potentially leading to prolonged prothrombin time and increased bleeding risk.[32] Chronic exposure risks appear minimal based on preclinical data; long-term administration in rats at doses up to 200 mg/kg/day produced no observable hepatotoxic effects or alterations in liver weight and histology.[33] Overdose management focuses on supportive and symptomatic care in a clinical setting, with no specific antidote available. Activated charcoal may be considered for recent oral ingestions to reduce absorption, while gastric lavage is not routinely recommended. As a non-opioid antitussive, oxolamine does not respond to naloxone reversal.[29] Pharmacokinetic factors, such as rapid elimination, contribute to the generally favorable prognosis in overdose scenarios.[19]History and Availability
Development and Research
Oxolamine, known during development as SKF-9976, was synthesized in the late 1950s by Smith Kline & French Laboratories as a non-narcotic antitussive agent designed to suppress cough associated with respiratory infections.[34] Early pharmacological evaluations established its central and peripheral antitussive mechanisms, distinguishing it from opioid-based suppressants through studies on its impact on cough reflexes in animal models.[35] Key clinical trials in the 1960s demonstrated oxolamine's efficacy as an antitussive in human subjects with respiratory conditions. A 1960 study highlighted its pharmacotherapeutic profile, showing significant cough reduction in patients with acute and chronic cough without notable sedation.[36] Subsequent research, including a 1961 trial on chronic bronchitis, reported improved symptom control and reduced cough frequency in bronchitis models, supporting its role in managing inflammatory cough.[37] A 1964 investigation further confirmed its effectiveness when used alone or combined with antibiotics like tetracycline in chronic respiratory tract disorders, emphasizing its compatibility in combination therapy.[38] These early trials, often small-scale and observational, established oxolamine's clinical utility but were limited by the methodological standards of the era. Modern randomized controlled trials (RCTs) on oxolamine remain scarce, reflecting its long-established status and reliance on historical data for approval in various markets. Comprehensive reviews of antitussive agents, such as a 2016 evidence-based analysis of European therapies, underscore the general paucity of high-quality contemporary RCTs for non-opioid suppressants like oxolamine, prioritizing instead newer agents with robust trial evidence.[39] Recent investigations have expanded beyond antitussive applications, probing oxolamine's anti-inflammatory potential in conditions like asthma and chronic obstructive pulmonary disease (COPD). Animal models have shown oxolamine citrate reduces inflammation in chemically induced respiratory damage; a seminal 1962 guinea pig study demonstrated its ability to mitigate tracheal and bronchial inflammation, suggesting mucolytic and anti-exudative effects.[6] A 2021 patent filing explores oxolamine in combination with beta-2 agonists like terbutaline for treating inflammatory respiratory syndromes, including asthma and COPD exacerbations, by addressing mucosa inflammation, fever, and spastic irritation.[40] Parallel research has examined oxolamine's pharmacokinetic interactions via cytochrome P450 (CYP) inhibition. In rat models, oxolamine selectively inhibits CYP2B1/2 isoforms, prolonging the half-life and increasing the area under the curve (AUC) of substrates like warfarin, with pronounced effects in males due to gender-specific enzyme expression.[18] These findings highlight potential drug-drug interactions but also suggest avenues for oxolamine in modulating CYP-mediated inflammation in respiratory diseases. Despite these advances, notable research gaps persist, including the lack of large-scale pediatric trials and comprehensive long-term safety data. Early pediatric use was documented in a 1961 clinical report, indicating tolerability in children, but no expansive modern RCTs have evaluated dosing, efficacy, or safety in this population.[41] Similarly, long-term studies are absent, with existing evidence confined to short-term acute use; pharmacovigilance analyses of older antitussives emphasize this void, calling for prospective data on chronic administration risks such as dependency or cumulative toxicity.[39]Regulatory Status and Availability
Oxolamine has not been approved by the United States Food and Drug Administration (FDA) for any indication and is classified as an unapproved drug in the USA.[1] It remains available internationally as an antitussive agent in various markets outside the United States.[1] In Europe, oxolamine is authorized through national procedures in countries such as Italy and Portugal, where it has been available since at least the late 20th century for the symptomatic treatment of dry cough.[42][43] It is not centrally authorized by the European Medicines Agency (EMA) and lacks approval in many other European nations, including Spain, Germany, France, and the United Kingdom.[29][43] In Asia, oxolamine is approved in Taiwan for treating respiratory tract inflammation and is listed as a prescription drug in New Zealand.[1] In Latin America, it is marketed in several countries, including Chile, Mexico, Peru, Paraguay, and Venezuela.[42] It is also available in Israel, Turkey, Georgia, and North Macedonia.[42] Oxolamine is generally classified as a prescription-only medicine (POM) when used as an antitussive, particularly in higher doses or for specific indications, as seen in New Zealand and Turkey.[1][43] However, in some markets like Italy and Portugal, low-dose formulations are available over-the-counter (OTC) without a prescription for short-term relief of dry cough in adults and children over certain ages.[43] There have been no major regulatory bans or withdrawals of oxolamine globally due to safety concerns, though its use has declined in some regions in favor of newer antitussive agents with more established efficacy profiles.[43]Society and Culture
Brand Names
Oxolamine is marketed under various brand names in countries where it is approved, primarily as a cough suppressant. In Italy, it is available as Uniplus and Tussibron by Angelini.[42] In Chile, brands include Perebron by Laboratorio Chile and Oxolamina Andromaco by Laboratorios Andromaco. In Venezuela, notable brands are Broxol by Galeno, Perebron by Elmor, and generic Oxolamina. In Taiwan, it is sold as Oxo by Yung Shin and Afuco by Eng City. Other brands include Symphocal by Teva in Israel and Numosol in Peru and Chile.[42][44] It is typically formulated as oral tablets, syrups, or capsules, often as the citrate salt. Tablets commonly contain 200 mg of oxolamine citrate, while syrup concentrations include 10 mg/mL, such as in Angelini Cough Syrup.[1][45] Pediatric formulations are available in some markets. Combination products with expectorants like guaifenesin or bromhexine exist, such as Caltusine in Mexico.[42] Major manufacturers include Angelini Pharma (Italy, Portugal), Teva (Israel), and local firms like Laboratorio Chile and Galeno. Oxolamine is not approved in the UK or USA and is unavailable there, except possibly for research purposes.[42][8]Non-Medical Uses
Oxolamine has been employed as a research tool in preclinical studies to investigate cytochrome P450 (CYP) enzyme interactions, particularly its inhibitory effects on CYP2B1 and CYP2B2 in male rats. This inhibition has been demonstrated to increase the area under the curve (AUC) and prolong the terminal half-life of warfarin, highlighting oxolamine's role in pharmacokinetic drug interaction models.[18] Such applications aid in understanding gender-specific metabolic differences and potential drug-drug interactions involving CYP2B enzymes.[46] In experimental animal models, oxolamine has been explored for its antitussive and anti-inflammatory properties on the respiratory tract, including reductions in edema and leukocyte infiltration in guinea pigs and evaluations of long-term safety in rhesus monkeys at doses up to 200 mg/kg/day.[6][47] These studies, conducted since the 1960s, have contributed to understanding its peripheral actions on bronchial nerve endings and cough reflex suppression, though it is not established as a standard veterinary treatment for cough or respiratory conditions in animals.[17] Reports of misuse for sedative effects are absent in the literature, consistent with its low abuse potential attributed to short duration of action and primary antitussive profile. No documented cases of recreational abuse have been identified, and its pharmacological properties do not prominently feature sedative mechanisms beyond mild, incidental effects observed in therapeutic contexts.[19]References
- https://commons.wikimedia.org/wiki/File:Oxolamine_synthesis.svg