Recent from talks
Nothing was collected or created yet.
Fenofibrate
View on Wikipedia
 | |
| Clinical data | |
|---|---|
| Trade names | Tricor, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a601052 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 99% |
| Metabolism | glucuronidation |
| Elimination half-life | 20 h |
| Excretion | urine (60%), feces (25%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.051.234 |
| Chemical and physical data | |
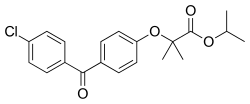
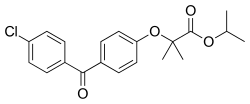
| Formula | C20H21ClO4 |
| Molar mass | 360.83 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 80 to 81 °C (176 to 178 °F) |
| |
| |
| (verify) | |
Fenofibrate, sold under the brand name Tricor among others, is an oral medication of the fibrate class used to treat abnormal blood lipid levels.[4] It is less commonly used compared to statins because it treats a different type of cholesterol abnormality to statins. While statins have strong evidence for reducing heart disease and death, there is evidence to suggest that fenofibrate also reduces the risk of heart disease and death. However, this seems only to apply to specific populations of people with elevated triglyceride levels and reduced high-density lipoprotein (HDL) cholesterol.[4][5][6] Its use is recommended together with dietary changes.[4]
Common side effects include liver problems, breathing problems, abdominal pain, muscle problems, and nausea.[4] Serious side effects may include toxic epidermal necrolysis, rhabdomyolysis, gallstones, and pancreatitis.[4] Use during pregnancy and breastfeeding is not recommended.[7][8] It works by multiple mechanisms.[4]
It was patented in 1969, and came into medical use in 1975.[9] It is available as a generic medication.[7] In 2023, it was the 83rd most commonly prescribed medication in the United States, with more than 8 million prescriptions.[10][11]
Medical uses
[edit]Fenofibrate continues to be one of the most effective medicine in reducing serum triglycerides levels in people living with metabolic dysfunction associated fatty liver disease (MASLD), previously known as non-alcoholic fatty liver disease (NAFLD), commonly seen in people with obesity and/or diabetes. In a meta-analysis involving data from 5 randomized controlled trials, fenofibrate was found to be safe to use in people with MASLD, as was superior to pioglitazone, omega-3 fatty acids and atorvastatin with regards to serum triglycerides reduction.[12]
Fenofibrate is mainly used for primary hypercholesterolemia or mixed dyslipidemia. Fenofibrate may slow the progression of diabetic retinopathy and the need for invasive treatment such as laser therapy in patients with type 2 diabetes with pre-existing retinopathy.[13][14][15] It was initially indicated for diabetic retinopathy in patients with type 2 diabetes and diabetic retinopathy in Australia.[16] The large scale, international FIELD and ACCORD-Eye trials found that fenofibrate therapy reduced required laser treatment for diabetic retinopathy by 1.5% over 5 years, as well as reducing progression by 3.7% over 4 years. [13][14][15][17] Further studies looking at the role of fenofibrate in the progression of diabetic retinopathy as the primary outcome is warranted to understand its role in this condition. Although no statistically significant cardiovascular risk benefits were identified in these trials, benefits may accrue to add on therapy to patients with high triglyceride dyslipidaemia currently taking statin medications.[18][19]
Fenofibrate appears to reduce the risk of below ankle amputations in patients with Type 2 diabetes without microvascular disease.[20] The FIELD study reported that fenofibrate at doses of 200 mg daily, reduced the risk for any amputation by 37% independent of glycaemic control, presence or absence of dyslipidaemia and its lipid-lowering mechanism of action.[20][21] However, the cohort of participants who underwent amputations were more likely to have had previous cardiovascular disease (e.g. angina, myocardial infarction), longer duration of diabetes and had baseline neuropathy.[20][21]
Fenofibrate has an off-label use as an added therapy of high blood uric acid levels in people who have gout.[22]
It is used in addition to diet to reduce elevated low-density lipoprotein cholesterol (LDL), total cholesterol, triglycerides (TG), and apolipoprotein B (apo B), and to increase high-density lipoprotein cholesterol (HDL) in adults with primary hypercholesterolemia or mixed dyslipidemia.[3]
Severe hypertriglyceridemia type IV or V
[edit]It is used in tandem with diet for treatment of adults with severe hypertriglyceridemia. Improving glycemic control in diabetics showing fasting chylomicronemia usually reduces the need for pharmacologic intervention.[3]
Statins remain the first line for treatment of blood cholesterol. AHA guidelines from 2013 did not find evidence for routine use of additional medications.[23]
Additionally, in 2016, the FDA filed "Withdrawal of Approval of Indications Related to the Coadministration With Statins in Applications for Niacin Extended-Release Tablets and Fenofibric Acid Delayed Release Capsules" noting "the Agency has concluded that the totality of the scientific evidence no longer supports the conclusion that a drug-induced reduction in triglyceride levels and/or increase in HDL cholesterol levels in statin-treated patients results in a reduction in the risk of cardiovascular events. Consistent with this conclusion, FDA has determined that the benefits of niacin ER tablets and fenofibric acid DR capsules for coadministration with statins no longer outweigh the risks, and the approvals for this indication should be withdrawn."[24]
Contraindications
[edit]Fenofibrate is contraindicated in:[3]
- Patients with severe renal impairment, including those receiving dialysis (2.7-fold increase in exposure, and increased accumulation during chronic dosing in patients with estimated glomerular filtration rate < 30 mL/min)
- Patients with active liver disease, including those with primary biliary cirrhosis and unexplained persistent liver function test abnormalities
- Patients with preexisting gallbladder disease
- Nursing mothers
- Hypothyroidism
- Patients with known hypersensitivity to fenofibrate or fenofibric acid
Adverse effects
[edit]The most common adverse events (>3% of patients with coadministered statins) are[25]
- Headache
- Back pain
- Nasopharyngitis
- Nausea
- Myalgia
- Joint pain or arthralgia
- Diarrhea
- Upper respiratory tract infection
- Calculi (Kidney Stones)
Precautions
[edit]When fenofibrate and a statin are given as combination therapy, it is recommended that fenofibrate be given in the morning and the statin at night, so that the peak dosages do not overlap.[26]
Musculoskeletal
- Myopathy and rhabdomyolysis; increased risk when coadminstered with a statin, particularly in the elderly and patients with diabetes, kidney failure, hypothyroidism[25]
Hepatotoxicity
- Can increase serum transaminases; liver tests should be monitored periodically[25]
Nephrotoxicity
- Can increase serum creatinine levels; renal function should be monitored periodically in patients with chronic kidney disease[25]
Biliary
- Can increase cholesterol excretion into the bile, leading to risk of cholelithiasis; if suspected, gallbladder studies are indicated. See "Interaction" section under Bile acid sequestrant[25]
Coagulation/Bleeding
Overdose
[edit]"There is no specific treatment for overdose with fenofibric acid delayed-release capsules. General supportive care is indicated, including monitoring of vital signs and observation of clinical status". Additionally, hemodialysis should not be considered as an overdose treatment option because fenofibrate heavily binds to plasma proteins and does not dialyze well.[25]
Interactions
[edit]These drug interactions with fenofibrate are considered major and may need therapy modifications:
- Bile acid sequestrants (e.g. cholestyramine, colestipol, etc.): If taken together, bile acid resins may bind to fenofibrate, resulting in a decrease in fenofibrate absorption. To maximize absorption, patients need to separate administration by at least 1 h before or 4 h to 6 h after taking the bile acid sequestrant.[25][27]
- Immunosuppressants (e.g. ciclosporin or tacrolimus): An increased risk of renal dysfunction exists with concomitant use of immunosuppressants and fenofibrate. Approach with caution when coadministering additional medications that decrease renal function.[28]
- Vitamin K antagonists (e.g. warfarin): As previously mentioned, fenofibrate interacts with coumadin anticoagulants to increase the risk of bleeding. Dosage adjustment of vitamin K antagonist may be necessary.[25]
- Statins: Combination of statins and fenofibrate may increase the risk of rhabdomyolysis or myopathy.[29]
Mechanism of action
[edit]"In summary, enhanced catabolism of triglyceride-rich particles and reduced secretion of VLDL underlie the hypotriglyceridemic effect of fibrates, whereas their effect on HDL metabolism is associated with changes in HDL apolipoprotein expression."[30]
Fenofibrate is a fibrate derivative, a prodrug comprising fenofibric acid linked to an isopropyl ester. It lowers lipid levels by activating peroxisome proliferator-activated receptor alpha (PPARα). PPARα activates lipoprotein lipase and reduces apoprotein CIII, which increases lipolysis and elimination of triglyceride-rich particles from plasma.[30]
PPARα also increases apoproteins AI and AII, reduces VLDL- and LDL-containing apoprotein B, and increases HDL-containing apoprotein AI and AII.
Formulations
[edit]Fenofibrate is available in several formulations and is sold under several brand names. The formulations may differ in terms of pharmacokinetic properties, particularly bioavailability; some must be taken with meals, whereas others may be taken without regard to food.[31]
The choline salt of fenofibrate is available in the United States, sold as Trilipix, and may be taken without regard to meals.[25][32]
Environmental presence
[edit]Fenofibric acid was one of the 12 compounds identified in sludge samples taken from 12 wastewater treatment plants in California that were associated with estrogenic activity in in vitro.[33]
History
[edit]Fenofibrate was first synthesized in 1974, as a derivative of clofibrate, and was initially offered in France. It was initially known as procetofen, and was later renamed fenofibrate to comply with World Health Organization International Nonproprietary Name guidelines.[34]
Fenofibrate was developed by Groupe Fournier SA of France.[citation needed]
Society and culture
[edit]In the United States, Tricor was reformulated in 2005. This reformulation was controversial, seen as an attempt to stifle competition from generic equivalents,[35] and was the subject of antitrust litigation by Teva.[35]
Brand names
[edit]- Tricor by AbbVie
- Lipofen by Kowa Pharmaceuticals America Inc
- Lofibra by Teva
- Lipanthyl, Lipidil, Lipantil micro and Supralip by Abbott Laboratories
- Fenocor-67 by Ordain Health Care
- Fenogal by SMB Laboratories
- Antara by Oscient Pharmaceuticals
- Tricheck by Zydus (CND)
- Atorva TG by Zydus Medica
- Golip by GolgiUSA
- Stanlip by Sun Pharma (India)
Research
[edit]A systematic review and meta-analysis found that fenofibrate might be a safe adjunct to neonatal phototherapy. However, the certainty of evidence was very low.[36]
References
[edit]- ^ "Prescription medicines: registration of new generic medicines and biosimilar medicines, 2017". Therapeutic Goods Administration (TGA). 21 June 2022. Retrieved 30 March 2024.
- ^ "Fenofibrate 267mg Capsules - Summary of Product Characteristics (SmPC)". (emc). 12 February 2020. Retrieved 13 April 2020.
- ^ a b c d "Tricor- fenofibrate tablet". DailyMed. 14 November 2024. Retrieved 2 May 2025.
- ^ a b c d e f "Fenofibric Acid/Fenofibrate Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 3 March 2019.
- ^ Ginsberg HN, Elam MB, Lovato LC, Crouse JR, Leiter LA, Linz P, et al. (April 2010). "Effects of combination lipid therapy in type 2 diabetes mellitus". The New England Journal of Medicine. 362 (17): 1563–1574. doi:10.1056/NEJMoa1001282. PMC 2879499. PMID 20228404.
- ^ Kim NH, Han KH, Choi J, Lee J, Kim SG (September 2019). "Use of fenofibrate on cardiovascular outcomes in statin users with metabolic syndrome: propensity matched cohort study". BMJ. 366 l5125. doi:10.1136/bmj.l5125. PMC 6763755. PMID 31562117. S2CID 203580658.
- ^ a b British national formulary: BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 198. ISBN 978-0-85711-338-2.
- ^ "Fenofibrate Pregnancy and Breastfeeding Warnings". Drugs.com. Retrieved 3 March 2019.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 474. ISBN 978-3-527-60749-5.
- ^ "Top 300 of 2023". ClinCalc. Archived from the original on 12 August 2025. Retrieved 12 August 2025.
- ^ "Fenofibrate Drug Usage Statistics, United States, 2013 - 2023". ClinCalc. Retrieved 18 August 2025.
- ^ Kumar M, Awasthi A, Dutta D, Joshi A, Sharma M (28 June 2025). "Fenofibrate in Metabolic Dysfunction-associated Steatotic Liver Disease: A Systematic Review and Meta-analysis". Indian J Endocrinol Metab. 29 (3): 268–275. doi:10.4103/ijem.ijem_528_24. PMC 12274038. PMID 40688627.
- ^ a b Wong TY, Simó R, Mitchell P (July 2012). "Fenofibrate - a potential systemic treatment for diabetic retinopathy?". American Journal of Ophthalmology. 154 (1): 6–12. doi:10.1016/j.ajo.2012.03.013. PMID 22709833.
- ^ a b Keech AC, Mitchell P, Summanen PA, O'Day J, Davis TM, Moffitt MS, et al. (November 2007). "Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial". Lancet. 370 (9600): 1687–1697. doi:10.1016/S0140-6736(07)61607-9. PMID 17988728. S2CID 30479730.
- ^ a b Chew EY, Davis MD, Danis RP, Lovato JF, Perdue LH, Greven C, et al. (December 2014). "The effects of medical management on the progression of diabetic retinopathy in persons with type 2 diabetes: the Action to Control Cardiovascular Risk in Diabetes (ACCORD) Eye Study". Ophthalmology. 121 (12): 2443–2451. doi:10.1016/j.ophtha.2014.07.019. PMC 4252767. PMID 25172198.
- ^ "Australian Public Assessment Report for fenofibrate". TGA. Archived from the original on 29 June 2015. Retrieved 27 June 2015.
- ^ Fazio S (June 2009). "More clinical lessons from the FIELD study". Cardiovascular Drugs and Therapy. 23 (3): 235–241. doi:10.1007/s10557-008-6160-5. PMID 19160032. S2CID 7987660.
- ^ Elam MB, Ginsberg HN, Lovato LC, Corson M, Largay J, Leiter LA, et al. (April 2017). "Association of Fenofibrate Therapy With Long-term Cardiovascular Risk in Statin-Treated Patients With Type 2 Diabetes". JAMA Cardiology. 2 (4): 370–380. doi:10.1001/jamacardio.2016.4828. PMC 5470410. PMID 28030716.
- ^ Kim NH, Han KH, Choi J, Lee J, Kim SG (September 2019). "Use of fenofibrate on cardiovascular outcomes in statin users with metabolic syndrome: propensity matched cohort study". BMJ. 366 l5125. doi:10.1136/bmj.l5125. PMC 6763755. PMID 31562117.
- ^ a b c Rajamani K, Colman PG, Li LP, Best JD, Voysey M, D'Emden MC, et al. (May 2009). "Effect of fenofibrate on amputation events in people with type 2 diabetes mellitus (FIELD study): a prespecified analysis of a randomised controlled trial". Lancet. 373 (9677): 1780–1788. doi:10.1016/S0140-6736(09)60698-X. PMC 2687887. PMID 19465233.
- ^ a b Steiner G (October 2009). "How can we improve the management of vascular risk in type 2 diabetes: insights from FIELD". Cardiovascular Drugs and Therapy. 23 (5): 403–408. doi:10.1007/s10557-009-6190-7. PMID 19757004. S2CID 12747599.
- ^ Khanna D, Fitzgerald JD, Khanna PP, Bae S, Singh MK, Neogi T, et al. (October 2012). "2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia". Arthritis Care & Research. 64 (10): 1431–1446. doi:10.1002/acr.21772. PMC 3683400. PMID 23024028.
- ^ Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. (June 2014). "2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. 129 (25 Suppl 2): S1-45. doi:10.1161/01.cir.0000437738.63853.7a. PMID 24222016.
- ^ "AbbVie Inc. et al; Withdrawal of Approval of Indications Related to the Coadministration With Statins in Applications for Niacin Extended-Release Tablets and Fenofibric Acid Delayed- Release Capsules" (PDF). Food and Drug Administration. 18 April 2016.
- ^ a b c d e f g h i j Fenofibric Acid FDA Label Prescribing Information"FDA Label Information" (PDF). FDA. Archived from the original (PDF) on 21 April 2014.
- ^ Wierzbicki AS, Mikhailidis DP, Wray R, Schacter M, Cramb R, Simpson WG, et al. (2003). "Statin-fibrate combination: therapy for hyperlipidemia: a review". Current Medical Research and Opinion. 19 (3): 155–168. doi:10.1185/030079903125001668. PMID 12814127. S2CID 35948128.
- ^ Product Information: TriCor(TM), fenofibrate. Abbott Laboratories, North Chicago, IL, 1998.
- ^ Product Information: Sandimmune(R) oral capsules, oral solution, intravenous injection, cyclosporine oral capsules, oral solution, intravenous injection. Novartis Pharmaceuticals Corporation, East Hanover, NJ, 2010.
- ^ Product Information: TRICOR(R) oral tablets, fenofibrate oral tablets. Abbott Laboratories, North Chicago, IL, 2007.
- ^ a b Staels B, Dallongeville J, Auwerx J, Schoonjans K, Leitersdorf E, Fruchart JC (November 1998). "Mechanism of action of fibrates on lipid and lipoprotein metabolism". Circulation. 98 (19): 2088–2093. CiteSeerX 10.1.1.1004.321. doi:10.1161/01.cir.98.19.2088. PMID 9808609. S2CID 5858864.
- ^ Ling H, Luoma JT, Hilleman D (April 2013). "A Review of Currently Available Fenofibrate and Fenofibric Acid Formulations". Cardiology Research. 4 (2): 47–55. doi:10.4021/cr270w. PMC 5358213. PMID 28352420.
- ^ Alagona P (May 2010). "Fenofibric acid: a new fibrate approved for use in combination with statin for the treatment of mixed dyslipidemia". Vascular Health and Risk Management. 6: 351–362. doi:10.2147/vhrm.s6714. PMC 2879297. PMID 20531954.
- ^ Black GP, He G, Denison MS, Young TM (May 2021). "Using Estrogenic Activity and Nontargeted Chemical Analysis to Identify Contaminants in Sewage Sludge". Environmental Science & Technology. 55 (10): 6729–6739. Bibcode:2021EnST...55.6729B. doi:10.1021/acs.est.0c07846. PMC 8378343. PMID 33909413.
- ^ Lalloyer F, Staels B (May 2010). "Fibrates, glitazones, and peroxisome proliferator-activated receptors". Arteriosclerosis, Thrombosis, and Vascular Biology. 30 (5): 894–899. doi:10.1161/ATVBAHA.108.179689. PMC 2997800. PMID 20393155.
- ^ a b "Abbott's request to dismiss the antitrust charge over Tricor was rejected". FDANews, Drug Daily Bulletin. 1 June 2006. Archived from the original on 10 July 2011. Retrieved 31 August 2010.
- ^ Abdellatif M, Abozaid AA, Shah PS, Dhouibi N, Nguyen-Khac T, Khleif R, et al. (April 2024). "Efficacy and safety of fenofibrate in combination with phototherapy for the treatment of neonatal hyperbilirubinemia: a systematic review and meta-analyses". Canadian Journal of Physiology and Pharmacology. 102 (4) cjpp-2023-0213: 242–253. doi:10.1139/cjpp-2023-0213. PMID 38011686.