Recent from talks
Nothing was collected or created yet.
Estrogen
View on Wikipedia
| Estrogen | |
|---|---|
| Drug class | |
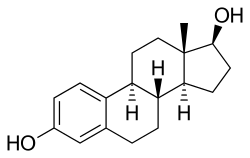
 Estradiol, the major estrogen sex hormone in humans and a widely used medication | |
| Class identifiers | |
| Use | Contraception, menopause, hypogonadism, transgender women, prostate cancer, breast cancer, others |
| ATC code | G03C |
| Biological target | Estrogen receptors (ERα, ERβ, mERs (e.g., GPER, others)) |
| External links | |
| MeSH | D004967 |
| Legal status | |
| In Wikidata | |
Estrogen (also spelled oestrogen in British English; see spelling differences) is a category of sex hormone responsible for the development and regulation of the female reproductive system and secondary sex characteristics.[1][2] There are three major endogenous estrogens that have estrogenic hormonal activity: estrone (E1), estradiol (E2), and estriol (E3).[1][3] Estradiol, an estrane, is the most potent and prevalent.[1] Another estrogen called estetrol (E4) is produced only during pregnancy.
Estrogens are synthesized in all vertebrates[4] and some insects.[5] Quantitatively, estrogens circulate at lower levels than androgens in both men and women.[6] While estrogen levels are significantly lower in males than in females, estrogens nevertheless have important physiological roles in males.[7]
Like all steroid hormones, estrogens readily diffuse across the cell membrane. Once inside the cell, they bind to and activate estrogen receptors (ERs) which in turn modulate the expression of many genes.[8] Additionally, estrogens bind to and activate rapid-signaling membrane estrogen receptors (mERs),[9][10] such as GPER (GPR30).[11]
In addition to their role as natural hormones, estrogens are used as medications, for instance in menopausal hormone therapy, hormonal birth control and feminizing hormone therapy for transgender women, intersex people, and nonbinary people.
Synthetic and natural estrogens have been found in the environment and are referred to as xenoestrogens. Estrogens are among the wide range of endocrine-disrupting compounds and can cause health issues and reproductive dysfunction in both wildlife and humans.[12][13]
Types and examples
[edit]The four major naturally occurring estrogens in women are estrone (E1), estradiol (E2), estriol (E3), and estetrol (E4). Estradiol (E2) is the predominant estrogen during reproductive years both in terms of absolute serum levels as well as in terms of estrogenic activity. During menopause, estrone is the predominant circulating estrogen and during pregnancy estriol is the predominant circulating estrogen in terms of serum levels. Given by subcutaneous injection in mice, estradiol is about 10-fold more potent than estrone and about 100-fold more potent than estriol.[14] Thus, estradiol is the most important estrogen in non-pregnant females who are between the menarche and menopause stages of life. However, during pregnancy this role shifts to estriol, and in postmenopausal women estrone becomes the primary form of estrogen in the body. Another type of estrogen called estetrol (E4) is produced only during pregnancy. All of the different forms of estrogen are synthesized from androgens, specifically testosterone and androstenedione, by the enzyme aromatase.[citation needed]
Minor endogenous estrogens, the biosyntheses of which do not involve aromatase, include 27-hydroxycholesterol, dehydroepiandrosterone (DHEA), 7-oxo-DHEA, 7α-hydroxy-DHEA, 16α-hydroxy-DHEA, 7β-hydroxyepiandrosterone, androstenedione (A4), androstenediol (A5), 3α-androstanediol, and 3β-androstanediol.[15][16] Some estrogen metabolites, such as the catechol estrogens 2-hydroxyestradiol, 2-hydroxyestrone, 4-hydroxyestradiol, and 4-hydroxyestrone, as well as 16α-hydroxyestrone, are also estrogens with varying degrees of activity.[17] The biological importance of these minor estrogens is not entirely clear.
Biological function
[edit]
The actions of estrogen are mediated by the estrogen receptor (ER), a dimeric nuclear protein that binds to DNA and controls gene expression. Like other steroid hormones, estrogen enters passively into the cell where it binds to and activates the estrogen receptor. The estrogen:ER complex binds to specific DNA sequences called a hormone response element to activate the transcription of target genes (in a study using an estrogen-dependent breast cancer cell line as model, 89 such genes were identified).[19] Since estrogen enters all cells, its actions are dependent on the presence of the ER in the cell. The ER is expressed in specific tissues including the ovary, uterus and breast. The metabolic effects of estrogen in postmenopausal women have been linked to the genetic polymorphism of the ER.[20]
While estrogens are present in both men and women, they are usually present at significantly higher levels in biological females of reproductive age. They promote the development of female secondary sexual characteristics, such as breasts, darkening and enlargement of nipples,[21] and thickening of the endometrium and other aspects of regulating the menstrual cycle. In males, estrogen regulates certain functions of the reproductive system important to the maturation of sperm[22][23][24] and may be necessary for a healthy libido.[25]
| Ligand | Other names | Relative binding affinities (RBA, %)a | Absolute binding affinities (Ki, nM)a | Action | ||
|---|---|---|---|---|---|---|
| ERα | ERβ | ERα | ERβ | |||
| Estradiol | E2; 17β-Estradiol | 100 | 100 | 0.115 (0.04–0.24) | 0.15 (0.10–2.08) | Estrogen |
| Estrone | E1; 17-Ketoestradiol | 16.39 (0.7–60) | 6.5 (1.36–52) | 0.445 (0.3–1.01) | 1.75 (0.35–9.24) | Estrogen |
| Estriol | E3; 16α-OH-17β-E2 | 12.65 (4.03–56) | 26 (14.0–44.6) | 0.45 (0.35–1.4) | 0.7 (0.63–0.7) | Estrogen |
| Estetrol | E4; 15α,16α-Di-OH-17β-E2 | 4.0 | 3.0 | 4.9 | 19 | Estrogen |
| Alfatradiol | 17α-Estradiol | 20.5 (7–80.1) | 8.195 (2–42) | 0.2–0.52 | 0.43–1.2 | Metabolite |
| 16-Epiestriol | 16β-Hydroxy-17β-estradiol | 7.795 (4.94–63) | 50 | ? | ? | Metabolite |
| 17-Epiestriol | 16α-Hydroxy-17α-estradiol | 55.45 (29–103) | 79–80 | ? | ? | Metabolite |
| 16,17-Epiestriol | 16β-Hydroxy-17α-estradiol | 1.0 | 13 | ? | ? | Metabolite |
| 2-Hydroxyestradiol | 2-OH-E2 | 22 (7–81) | 11–35 | 2.5 | 1.3 | Metabolite |
| 2-Methoxyestradiol | 2-MeO-E2 | 0.0027–2.0 | 1.0 | ? | ? | Metabolite |
| 4-Hydroxyestradiol | 4-OH-E2 | 13 (8–70) | 7–56 | 1.0 | 1.9 | Metabolite |
| 4-Methoxyestradiol | 4-MeO-E2 | 2.0 | 1.0 | ? | ? | Metabolite |
| 2-Hydroxyestrone | 2-OH-E1 | 2.0–4.0 | 0.2–0.4 | ? | ? | Metabolite |
| 2-Methoxyestrone | 2-MeO-E1 | <0.001–<1 | <1 | ? | ? | Metabolite |
| 4-Hydroxyestrone | 4-OH-E1 | 1.0–2.0 | 1.0 | ? | ? | Metabolite |
| 4-Methoxyestrone | 4-MeO-E1 | <1 | <1 | ? | ? | Metabolite |
| 16α-Hydroxyestrone | 16α-OH-E1; 17-Ketoestriol | 2.0–6.5 | 35 | ? | ? | Metabolite |
| 2-Hydroxyestriol | 2-OH-E3 | 2.0 | 1.0 | ? | ? | Metabolite |
| 4-Methoxyestriol | 4-MeO-E3 | 1.0 | 1.0 | ? | ? | Metabolite |
| Estradiol sulfate | E2S; Estradiol 3-sulfate | <1 | <1 | ? | ? | Metabolite |
| Estradiol disulfate | Estradiol 3,17β-disulfate | 0.0004 | ? | ? | ? | Metabolite |
| Estradiol 3-glucuronide | E2-3G | 0.0079 | ? | ? | ? | Metabolite |
| Estradiol 17β-glucuronide | E2-17G | 0.0015 | ? | ? | ? | Metabolite |
| Estradiol 3-gluc. 17β-sulfate | E2-3G-17S | 0.0001 | ? | ? | ? | Metabolite |
| Estrone sulfate | E1S; Estrone 3-sulfate | <1 | <1 | >10 | >10 | Metabolite |
| Estradiol benzoate | EB; Estradiol 3-benzoate | 10 | ? | ? | ? | Estrogen |
| Estradiol 17β-benzoate | E2-17B | 11.3 | 32.6 | ? | ? | Estrogen |
| Estrone methyl ether | Estrone 3-methyl ether | 0.145 | ? | ? | ? | Estrogen |
| ent-Estradiol | 1-Estradiol | 1.31–12.34 | 9.44–80.07 | ? | ? | Estrogen |
| Equilin | 7-Dehydroestrone | 13 (4.0–28.9) | 13.0–49 | 0.79 | 0.36 | Estrogen |
| Equilenin | 6,8-Didehydroestrone | 2.0–15 | 7.0–20 | 0.64 | 0.62 | Estrogen |
| 17β-Dihydroequilin | 7-Dehydro-17β-estradiol | 7.9–113 | 7.9–108 | 0.09 | 0.17 | Estrogen |
| 17α-Dihydroequilin | 7-Dehydro-17α-estradiol | 18.6 (18–41) | 14–32 | 0.24 | 0.57 | Estrogen |
| 17β-Dihydroequilenin | 6,8-Didehydro-17β-estradiol | 35–68 | 90–100 | 0.15 | 0.20 | Estrogen |
| 17α-Dihydroequilenin | 6,8-Didehydro-17α-estradiol | 20 | 49 | 0.50 | 0.37 | Estrogen |
| Δ8-Estradiol | 8,9-Dehydro-17β-estradiol | 68 | 72 | 0.15 | 0.25 | Estrogen |
| Δ8-Estrone | 8,9-Dehydroestrone | 19 | 32 | 0.52 | 0.57 | Estrogen |
| Ethinylestradiol | EE; 17α-Ethynyl-17β-E2 | 120.9 (68.8–480) | 44.4 (2.0–144) | 0.02–0.05 | 0.29–0.81 | Estrogen |
| Mestranol | EE 3-methyl ether | ? | 2.5 | ? | ? | Estrogen |
| Moxestrol | RU-2858; 11β-Methoxy-EE | 35–43 | 5–20 | 0.5 | 2.6 | Estrogen |
| Methylestradiol | 17α-Methyl-17β-estradiol | 70 | 44 | ? | ? | Estrogen |
| Diethylstilbestrol | DES; Stilbestrol | 129.5 (89.1–468) | 219.63 (61.2–295) | 0.04 | 0.05 | Estrogen |
| Hexestrol | Dihydrodiethylstilbestrol | 153.6 (31–302) | 60–234 | 0.06 | 0.06 | Estrogen |
| Dienestrol | Dehydrostilbestrol | 37 (20.4–223) | 56–404 | 0.05 | 0.03 | Estrogen |
| Benzestrol (B2) | – | 114 | ? | ? | ? | Estrogen |
| Chlorotrianisene | TACE | 1.74 | ? | 15.30 | ? | Estrogen |
| Triphenylethylene | TPE | 0.074 | ? | ? | ? | Estrogen |
| Triphenylbromoethylene | TPBE | 2.69 | ? | ? | ? | Estrogen |
| Tamoxifen | ICI-46,474 | 3 (0.1–47) | 3.33 (0.28–6) | 3.4–9.69 | 2.5 | SERM |
| Afimoxifene | 4-Hydroxytamoxifen; 4-OHT | 100.1 (1.7–257) | 10 (0.98–339) | 2.3 (0.1–3.61) | 0.04–4.8 | SERM |
| Toremifene | 4-Chlorotamoxifen; 4-CT | ? | ? | 7.14–20.3 | 15.4 | SERM |
| Clomifene | MRL-41 | 25 (19.2–37.2) | 12 | 0.9 | 1.2 | SERM |
| Cyclofenil | F-6066; Sexovid | 151–152 | 243 | ? | ? | SERM |
| Nafoxidine | U-11,000A | 30.9–44 | 16 | 0.3 | 0.8 | SERM |
| Raloxifene | – | 41.2 (7.8–69) | 5.34 (0.54–16) | 0.188–0.52 | 20.2 | SERM |
| Arzoxifene | LY-353,381 | ? | ? | 0.179 | ? | SERM |
| Lasofoxifene | CP-336,156 | 10.2–166 | 19.0 | 0.229 | ? | SERM |
| Ormeloxifene | Centchroman | ? | ? | 0.313 | ? | SERM |
| Levormeloxifene | 6720-CDRI; NNC-460,020 | 1.55 | 1.88 | ? | ? | SERM |
| Ospemifene | Deaminohydroxytoremifene | 0.82–2.63 | 0.59–1.22 | ? | ? | SERM |
| Bazedoxifene | – | ? | ? | 0.053 | ? | SERM |
| Etacstil | GW-5638 | 4.30 | 11.5 | ? | ? | SERM |
| ICI-164,384 | – | 63.5 (3.70–97.7) | 166 | 0.2 | 0.08 | Antiestrogen |
| Fulvestrant | ICI-182,780 | 43.5 (9.4–325) | 21.65 (2.05–40.5) | 0.42 | 1.3 | Antiestrogen |
| Propylpyrazoletriol | PPT | 49 (10.0–89.1) | 0.12 | 0.40 | 92.8 | ERα agonist |
| 16α-LE2 | 16α-Lactone-17β-estradiol | 14.6–57 | 0.089 | 0.27 | 131 | ERα agonist |
| 16α-Iodo-E2 | 16α-Iodo-17β-estradiol | 30.2 | 2.30 | ? | ? | ERα agonist |
| Methylpiperidinopyrazole | MPP | 11 | 0.05 | ? | ? | ERα antagonist |
| Diarylpropionitrile | DPN | 0.12–0.25 | 6.6–18 | 32.4 | 1.7 | ERβ agonist |
| 8β-VE2 | 8β-Vinyl-17β-estradiol | 0.35 | 22.0–83 | 12.9 | 0.50 | ERβ agonist |
| Prinaberel | ERB-041; WAY-202,041 | 0.27 | 67–72 | ? | ? | ERβ agonist |
| ERB-196 | WAY-202,196 | ? | 180 | ? | ? | ERβ agonist |
| Erteberel | SERBA-1; LY-500,307 | ? | ? | 2.68 | 0.19 | ERβ agonist |
| SERBA-2 | – | ? | ? | 14.5 | 1.54 | ERβ agonist |
| Coumestrol | – | 9.225 (0.0117–94) | 64.125 (0.41–185) | 0.14–80.0 | 0.07–27.0 | Xenoestrogen |
| Genistein | – | 0.445 (0.0012–16) | 33.42 (0.86–87) | 2.6–126 | 0.3–12.8 | Xenoestrogen |
| Equol | – | 0.2–0.287 | 0.85 (0.10–2.85) | ? | ? | Xenoestrogen |
| Daidzein | – | 0.07 (0.0018–9.3) | 0.7865 (0.04–17.1) | 2.0 | 85.3 | Xenoestrogen |
| Biochanin A | – | 0.04 (0.022–0.15) | 0.6225 (0.010–1.2) | 174 | 8.9 | Xenoestrogen |
| Kaempferol | – | 0.07 (0.029–0.10) | 2.2 (0.002–3.00) | ? | ? | Xenoestrogen |
| Naringenin | – | 0.0054 (<0.001–0.01) | 0.15 (0.11–0.33) | ? | ? | Xenoestrogen |
| 8-Prenylnaringenin | 8-PN | 4.4 | ? | ? | ? | Xenoestrogen |
| Quercetin | – | <0.001–0.01 | 0.002–0.040 | ? | ? | Xenoestrogen |
| Ipriflavone | – | <0.01 | <0.01 | ? | ? | Xenoestrogen |
| Miroestrol | – | 0.39 | ? | ? | ? | Xenoestrogen |
| Deoxymiroestrol | – | 2.0 | ? | ? | ? | Xenoestrogen |
| β-Sitosterol | – | <0.001–0.0875 | <0.001–0.016 | ? | ? | Xenoestrogen |
| Resveratrol | – | <0.001–0.0032 | ? | ? | ? | Xenoestrogen |
| α-Zearalenol | – | 48 (13–52.5) | ? | ? | ? | Xenoestrogen |
| β-Zearalenol | – | 0.6 (0.032–13) | ? | ? | ? | Xenoestrogen |
| Zeranol | α-Zearalanol | 48–111 | ? | ? | ? | Xenoestrogen |
| Taleranol | β-Zearalanol | 16 (13–17.8) | 14 | 0.8 | 0.9 | Xenoestrogen |
| Zearalenone | ZEN | 7.68 (2.04–28) | 9.45 (2.43–31.5) | ? | ? | Xenoestrogen |
| Zearalanone | ZAN | 0.51 | ? | ? | ? | Xenoestrogen |
| Bisphenol A | BPA | 0.0315 (0.008–1.0) | 0.135 (0.002–4.23) | 195 | 35 | Xenoestrogen |
| Endosulfan | EDS | <0.001–<0.01 | <0.01 | ? | ? | Xenoestrogen |
| Kepone | Chlordecone | 0.0069–0.2 | ? | ? | ? | Xenoestrogen |
| o,p'-DDT | – | 0.0073–0.4 | ? | ? | ? | Xenoestrogen |
| p,p'-DDT | – | 0.03 | ? | ? | ? | Xenoestrogen |
| Methoxychlor | p,p'-Dimethoxy-DDT | 0.01 (<0.001–0.02) | 0.01–0.13 | ? | ? | Xenoestrogen |
| HPTE | Hydroxychlor; p,p'-OH-DDT | 1.2–1.7 | ? | ? | ? | Xenoestrogen |
| Testosterone | T; 4-Androstenolone | <0.0001–<0.01 | <0.002–0.040 | >5000 | >5000 | Androgen |
| Dihydrotestosterone | DHT; 5α-Androstanolone | 0.01 (<0.001–0.05) | 0.0059–0.17 | 221–>5000 | 73–1688 | Androgen |
| Nandrolone | 19-Nortestosterone; 19-NT | 0.01 | 0.23 | 765 | 53 | Androgen |
| Dehydroepiandrosterone | DHEA; Prasterone | 0.038 (<0.001–0.04) | 0.019–0.07 | 245–1053 | 163–515 | Androgen |
| 5-Androstenediol | A5; Androstenediol | 6 | 17 | 3.6 | 0.9 | Androgen |
| 4-Androstenediol | – | 0.5 | 0.6 | 23 | 19 | Androgen |
| 4-Androstenedione | A4; Androstenedione | <0.01 | <0.01 | >10000 | >10000 | Androgen |
| 3α-Androstanediol | 3α-Adiol | 0.07 | 0.3 | 260 | 48 | Androgen |
| 3β-Androstanediol | 3β-Adiol | 3 | 7 | 6 | 2 | Androgen |
| Androstanedione | 5α-Androstanedione | <0.01 | <0.01 | >10000 | >10000 | Androgen |
| Etiocholanedione | 5β-Androstanedione | <0.01 | <0.01 | >10000 | >10000 | Androgen |
| Methyltestosterone | 17α-Methyltestosterone | <0.0001 | ? | ? | ? | Androgen |
| Ethinyl-3α-androstanediol | 17α-Ethynyl-3α-adiol | 4.0 | <0.07 | ? | ? | Estrogen |
| Ethinyl-3β-androstanediol | 17α-Ethynyl-3β-adiol | 50 | 5.6 | ? | ? | Estrogen |
| Progesterone | P4; 4-Pregnenedione | <0.001–0.6 | <0.001–0.010 | ? | ? | Progestogen |
| Norethisterone | NET; 17α-Ethynyl-19-NT | 0.085 (0.0015–<0.1) | 0.1 (0.01–0.3) | 152 | 1084 | Progestogen |
| Norethynodrel | 5(10)-Norethisterone | 0.5 (0.3–0.7) | <0.1–0.22 | 14 | 53 | Progestogen |
| Tibolone | 7α-Methylnorethynodrel | 0.5 (0.45–2.0) | 0.2–0.076 | ? | ? | Progestogen |
| Δ4-Tibolone | 7α-Methylnorethisterone | 0.069–<0.1 | 0.027–<0.1 | ? | ? | Progestogen |
| 3α-Hydroxytibolone | – | 2.5 (1.06–5.0) | 0.6–0.8 | ? | ? | Progestogen |
| 3β-Hydroxytibolone | – | 1.6 (0.75–1.9) | 0.070–0.1 | ? | ? | Progestogen |
| Footnotes: a = (1) Binding affinity values are of the format "median (range)" (# (#–#)), "range" (#–#), or "value" (#) depending on the values available. The full sets of values within the ranges can be found in the Wiki code. (2) Binding affinities were determined via displacement studies in a variety of in-vitro systems with labeled estradiol and human ERα and ERβ proteins (except the ERβ values from Kuiper et al. (1997), which are rat ERβ). Sources: See template page. | ||||||
| Estrogen | Relative binding affinities (%) | ||||||
|---|---|---|---|---|---|---|---|
| ER | AR | PR | GR | MR | SHBG | CBG | |
| Estradiol | 100 | 7.9 | 2.6 | 0.6 | 0.13 | 8.7–12 | <0.1 |
| Estradiol benzoate | ? | ? | ? | ? | ? | <0.1–0.16 | <0.1 |
| Estradiol valerate | 2 | ? | ? | ? | ? | ? | ? |
| Estrone | 11–35 | <1 | <1 | <1 | <1 | 2.7 | <0.1 |
| Estrone sulfate | 2 | 2 | ? | ? | ? | ? | ? |
| Estriol | 10–15 | <1 | <1 | <1 | <1 | <0.1 | <0.1 |
| Equilin | 40 | ? | ? | ? | ? | ? | 0 |
| Alfatradiol | 15 | <1 | <1 | <1 | <1 | ? | ? |
| Epiestriol | 20 | <1 | <1 | <1 | <1 | ? | ? |
| Ethinylestradiol | 100–112 | 1–3 | 15–25 | 1–3 | <1 | 0.18 | <0.1 |
| Mestranol | 1 | ? | ? | ? | ? | <0.1 | <0.1 |
| Methylestradiol | 67 | 1–3 | 3–25 | 1–3 | <1 | ? | ? |
| Moxestrol | 12 | <0.1 | 0.8 | 3.2 | <0.1 | <0.2 | <0.1 |
| Diethylstilbestrol | ? | ? | ? | ? | ? | <0.1 | <0.1 |
| Notes: Reference ligands (100%) were progesterone for the PR, testosterone for the AR, estradiol for the ER, dexamethasone for the GR, aldosterone for the MR, dihydrotestosterone for SHBG, and cortisol for CBG. Sources: See template. | |||||||
| Estrogen | Other names | RBA (%)a | REP (%)b | |||
|---|---|---|---|---|---|---|
| ER | ERα | ERβ | ||||
| Estradiol | E2 | 100 | 100 | 100 | ||
| Estradiol 3-sulfate | E2S; E2-3S | ? | 0.02 | 0.04 | ||
| Estradiol 3-glucuronide | E2-3G | ? | 0.02 | 0.09 | ||
| Estradiol 17β-glucuronide | E2-17G | ? | 0.002 | 0.0002 | ||
| Estradiol benzoate | EB; Estradiol 3-benzoate | 10 | 1.1 | 0.52 | ||
| Estradiol 17β-acetate | E2-17A | 31–45 | 24 | ? | ||
| Estradiol diacetate | EDA; Estradiol 3,17β-diacetate | ? | 0.79 | ? | ||
| Estradiol propionate | EP; Estradiol 17β-propionate | 19–26 | 2.6 | ? | ||
| Estradiol valerate | EV; Estradiol 17β-valerate | 2–11 | 0.04–21 | ? | ||
| Estradiol cypionate | EC; Estradiol 17β-cypionate | ?c | 4.0 | ? | ||
| Estradiol palmitate | Estradiol 17β-palmitate | 0 | ? | ? | ||
| Estradiol stearate | Estradiol 17β-stearate | 0 | ? | ? | ||
| Estrone | E1; 17-Ketoestradiol | 11 | 5.3–38 | 14 | ||
| Estrone sulfate | E1S; Estrone 3-sulfate | 2 | 0.004 | 0.002 | ||
| Estrone glucuronide | E1G; Estrone 3-glucuronide | ? | <0.001 | 0.0006 | ||
| Ethinylestradiol | EE; 17α-Ethynylestradiol | 100 | 17–150 | 129 | ||
| Mestranol | EE 3-methyl ether | 1 | 1.3–8.2 | 0.16 | ||
| Quinestrol | EE 3-cyclopentyl ether | ? | 0.37 | ? | ||
| Footnotes: a = Relative binding affinities (RBAs) were determined via in-vitro displacement of labeled estradiol from estrogen receptors (ERs) generally of rodent uterine cytosol. Estrogen esters are variably hydrolyzed into estrogens in these systems (shorter ester chain length -> greater rate of hydrolysis) and the ER RBAs of the esters decrease strongly when hydrolysis is prevented. b = Relative estrogenic potencies (REPs) were calculated from half-maximal effective concentrations (EC50) that were determined via in-vitro β‐galactosidase (β-gal) and green fluorescent protein (GFP) production assays in yeast expressing human ERα and human ERβ. Both mammalian cells and yeast have the capacity to hydrolyze estrogen esters. c = The affinities of estradiol cypionate for the ERs are similar to those of estradiol valerate and estradiol benzoate (figure). Sources: See template page. | ||||||
| Estrogen | ER RBA (%) | Uterine weight (%) | Uterotrophy | LH levels (%) | SHBG RBA (%) |
|---|---|---|---|---|---|
| Control | – | 100 | – | 100 | – |
| Estradiol (E2) | 100 | 506 ± 20 | +++ | 12–19 | 100 |
| Estrone (E1) | 11 ± 8 | 490 ± 22 | +++ | ? | 20 |
| Estriol (E3) | 10 ± 4 | 468 ± 30 | +++ | 8–18 | 3 |
| Estetrol (E4) | 0.5 ± 0.2 | ? | Inactive | ? | 1 |
| 17α-Estradiol | 4.2 ± 0.8 | ? | ? | ? | ? |
| 2-Hydroxyestradiol | 24 ± 7 | 285 ± 8 | +b | 31–61 | 28 |
| 2-Methoxyestradiol | 0.05 ± 0.04 | 101 | Inactive | ? | 130 |
| 4-Hydroxyestradiol | 45 ± 12 | ? | ? | ? | ? |
| 4-Methoxyestradiol | 1.3 ± 0.2 | 260 | ++ | ? | 9 |
| 4-Fluoroestradiola | 180 ± 43 | ? | +++ | ? | ? |
| 2-Hydroxyestrone | 1.9 ± 0.8 | 130 ± 9 | Inactive | 110–142 | 8 |
| 2-Methoxyestrone | 0.01 ± 0.00 | 103 ± 7 | Inactive | 95–100 | 120 |
| 4-Hydroxyestrone | 11 ± 4 | 351 | ++ | 21–50 | 35 |
| 4-Methoxyestrone | 0.13 ± 0.04 | 338 | ++ | 65–92 | 12 |
| 16α-Hydroxyestrone | 2.8 ± 1.0 | 552 ± 42 | +++ | 7–24 | <0.5 |
| 2-Hydroxyestriol | 0.9 ± 0.3 | 302 | +b | ? | ? |
| 2-Methoxyestriol | 0.01 ± 0.00 | ? | Inactive | ? | 4 |
| Notes: Values are mean ± SD or range. ER RBA = Relative binding affinity to estrogen receptors of rat uterine cytosol. Uterine weight = Percentage change in uterine wet weight of ovariectomized rats after 72 hours with continuous administration of 1 μg/hour via subcutaneously implanted osmotic pumps. LH levels = Luteinizing hormone levels relative to baseline of ovariectomized rats after 24 to 72 hours of continuous administration via subcutaneous implant. Footnotes: a = Synthetic (i.e., not endogenous). b = Atypical uterotrophic effect which plateaus within 48 hours (estradiol's uterotrophy continues linearly up to 72 hours). Sources: [26][27][28][29][30][31][32][33][34] | |||||
Overview of actions
[edit]- Musculoskeletal
- Anabolic: Increases muscle mass and strength, speed of muscle regeneration, and bone density, increased sensitivity to exercise, protection against muscle damage, stronger collagen synthesis, increases the collagen content of connective tissues, tendons, and ligaments, but also decreases stiffness of tendons and ligaments (especially during menstruation). Decreased stiffness of tendons gives women much lower predisposition to muscle strains but soft ligaments are much more prone to injuries (ACL tears are 2-8x more common among women than men).[35][36][37][38]
- Reduce bone resorption, increase bone formation[39][40]
- In mice, estrogen has been shown to increase the proportion of the fastest-twitch (type IIX) muscle fibers by over 40%.[41]
- Metabolic
- Anti-inflammatory properties
- Accelerate metabolism
- Gynoid fat distribution: increased fat storage or estrogenic fat in some body parts such as breasts, buttocks, and legs but decreased abdominal and visceral fat (androgenic obesity).[42][43][44]
- Estradiol also regulates energy expenditure, body weight homeostasis, and seems to have much stronger anti-obesity effects than testosterone in general.[45]
- Inhibition of ferroptosis by hydroxyoestradiol derivatives.[46]
- Other structural
- Maintenance of vessels and skin
- Protein synthesis
- Increase hepatic production of binding proteins
- Increase production of the hepatokine adropin.[47]
- Suppress the transcription of ether-lipid pathway proteins.[46]
- Coagulation
- Increase circulating level of factors 2, 7, 9, 10, plasminogen
- Decrease antithrombin III
- Increase platelet adhesiveness
- Increase vWF (estrogen -> Angiotensin II -> Vasopressin)
- Increase PAI-1 and PAI-2 also through Angiotensin II
- Lipid
- Increase HDL, triglyceride
- Decrease LDL, fat deposition
- Fluid balance
- Melanin
- Estrogen is known to cause darkening of skin, especially in the face and areolae.[50] Pale skinned women will develop browner and yellower skin during pregnancy, as a result of the increase of estrogen, known as the "mask of pregnancy".[51] Estrogen may explain why women have darker eyes than men, and also a lower risk of skin cancer than men; a European study found that women generally have darker skin than men.[52][53]
- Lung function
- Kidney function
- Protects from acute kidney injury in females.[46]
- Sexual
- Mediate formation of female secondary sex characteristics
- Stimulate endometrial growth
- Increase uterine growth
- Increase vaginal lubrication
- Thicken the vaginal wall
- Uterus lining
- Estrogen together with progesterone promotes and maintains the uterus lining in preparation for implantation of fertilized egg and maintenance of uterus function during gestation period, also upregulates oxytocin receptor in myometrium
- Ovulation
- Surge in estrogen level induces the release of luteinizing hormone, which then triggers ovulation by releasing the egg from the Graafian follicle in the ovary.
- Sexual behavior
- Estrogen is required for female mammals to engage in lordosis behavior during estrus (when animals are "in heat").[55][56] This behavior is required for sexual receptivity in these mammals and is regulated by the ventromedial nucleus of the hypothalamus.[57]
- Sex drive is dependent on androgen levels[58] only in the presence of estrogen. Without estrogen, free testosterone level actually decreases sexual desire (instead of increasing sex drive), as demonstrated for those women who have hypoactive sexual desire disorder, and the sexual desire in these women can be restored by administration of estrogen (using oral contraceptive).[59]
Female pubertal development
[edit]Estrogens are responsible for the development of female secondary sexual characteristics during puberty, including breast development, widening of the hips, and female fat distribution. Conversely, androgens are responsible for pubic and body hair growth, as well as acne and axillary odor.
Breast development
[edit]Estrogen, in conjunction with growth hormone (GH) and its secretory product insulin-like growth factor 1 (IGF-1), is critical in mediating breast development during puberty, as well as breast maturation during pregnancy in preparation of lactation and breastfeeding.[60][61] Estrogen is primarily and directly responsible for inducing the ductal component of breast development,[62][63][64] as well as for causing fat deposition and connective tissue growth.[62][63] It is also indirectly involved in the lobuloalveolar component, by increasing progesterone receptor expression in the breasts[62][64][65] and by inducing the secretion of prolactin.[66][67] Allowed for by estrogen, progesterone and prolactin work together to complete lobuloalveolar development during pregnancy.[63][68]
Androgens such as testosterone powerfully oppose estrogen action in the breasts, such as by reducing estrogen receptor expression in them.[69][70]
Female reproductive system
[edit]Estrogens are responsible for maturation and maintenance of the vagina and uterus, and are also involved in ovarian function, such as maturation of ovarian follicles. In addition, estrogens play an important role in regulation of gonadotropin secretion. For these reasons, estrogens are required for female fertility.[citation needed]
Neuroprotection and DNA repair
[edit]Estrogen regulated DNA repair mechanisms in the brain have neuroprotective effects.[71] Estrogen regulates the transcription of DNA base excision repair genes as well as the translocation of the base excision repair enzymes between different subcellular compartments.
Brain and behavior
[edit]Sex drive
[edit]Estrogens are involved in libido (sex drive) in both women and men.
Cognition
[edit]Verbal memory scores are frequently used as one measure of higher level cognition. These scores vary in direct proportion to estrogen levels throughout the menstrual cycle, pregnancy, and menopause. Furthermore, estrogens when administered shortly after natural or surgical menopause prevents decreases in verbal memory. In contrast, estrogens have little effect on verbal memory if first administered years after menopause.[72] Estrogens also have positive influences on other measures of cognitive function.[73] However the effect of estrogens on cognition is not uniformly favorable and is dependent on the timing of the dose and the type of cognitive skill being measured.[74]
The protective effects of estrogens on cognition may be mediated by estrogen's anti-inflammatory effects in the brain.[75] Studies have also shown that the Met allele gene and level of estrogen mediates the efficiency of prefrontal cortex dependent working memory tasks.[76][77] Researchers have urged for further research to illuminate the role of estrogen and its potential for improvement on cognitive function.[78]
Mental health
[edit]Estrogen is considered to play a significant role in women's mental health. Sudden estrogen withdrawal, fluctuating estrogen, and periods of sustained low estrogen levels correlate with a significant lowering of mood. Clinical recovery from postpartum, perimenopause, and postmenopause depression has been shown to be effective after levels of estrogen were stabilized and/or restored.[79][80][81] Menstrual exacerbation (including menstrual psychosis) is typically triggered by low estrogen levels,[82] and is often mistaken for premenstrual dysphoric disorder.[83]
Compulsions in male lab mice, such as those in obsessive-compulsive disorder (OCD), may be caused by low estrogen levels. When estrogen levels were raised through the increased activity of the enzyme aromatase in male lab mice, OCD rituals were dramatically decreased. Hypothalamic protein levels in the gene COMT are enhanced by increasing estrogen levels which are believed to return mice that displayed OCD rituals to normal activity. Aromatase deficiency is ultimately suspected which is involved in the synthesis of estrogen in humans and has therapeutic implications in humans having obsessive-compulsive disorder.[84]
Local application of estrogen in the rat hippocampus has been shown to inhibit the re-uptake of serotonin. Contrarily, local application of estrogen has been shown to block the ability of fluvoxamine to slow serotonin clearance, suggesting that the same pathways which are involved in SSRI efficacy may also be affected by components of local estrogen signaling pathways.[85]
Parenthood
[edit]Studies have also found that fathers had lower levels of cortisol and testosterone but higher levels of estrogen (estradiol) than did non-fathers.[86]
Binge eating
[edit]Estrogen may play a role in suppressing binge eating. Hormone replacement therapy using estrogen may be a possible treatment for binge eating behaviors in females. Estrogen replacement has been shown to suppress binge eating behaviors in female mice.[87] The mechanism by which estrogen replacement inhibits binge-like eating involves the replacement of serotonin (5-HT) neurons. Women exhibiting binge eating behaviors are found to have increased brain uptake of neuron 5-HT, and therefore less of the neurotransmitter serotonin in the cerebrospinal fluid.[88] Estrogen works to activate 5-HT neurons, leading to suppression of binge like eating behaviors.[87]
It is also suggested that there is an interaction between hormone levels and eating at different points in the female menstrual cycle. Research has predicted increased emotional eating during hormonal flux, which is characterized by high progesterone and estradiol levels that occur during the mid-luteal phase. It is hypothesized that these changes occur due to brain changes across the menstrual cycle that are likely a genomic effect of hormones. These effects produce menstrual cycle changes, which result in hormone release leading to behavioral changes, notably binge and emotional eating. These occur especially prominently among women who are genetically vulnerable to binge eating phenotypes.[89]
Binge eating is associated with decreased estradiol and increased progesterone.[90] Klump et al.[91] Progesterone may moderate the effects of low estradiol (such as during dysregulated eating behavior), but that this may only be true in women who have had clinically diagnosed binge episodes (BEs). Dysregulated eating is more strongly associated with such ovarian hormones in women with BEs than in women without BEs.[91]
The implantation of 17β-estradiol pellets in ovariectomized mice significantly reduced binge eating behaviors and injections of GLP-1 in ovariectomized mice decreased binge-eating behaviors.[87]
The associations between binge eating, menstrual-cycle phase and ovarian hormones correlated.[90][92][93]
Masculinization in rodents
[edit]In rodents, estrogens (which are locally aromatized from androgens in the brain) play an important role in psychosexual differentiation, for example, by masculinizing territorial behavior;[94] the same is not true in humans.[95] In humans, the masculinizing effects of prenatal androgens on behavior (and other tissues, with the possible exception of effects on bone) appear to act exclusively through the androgen receptor.[96] Consequently, the utility of rodent models for studying human psychosexual differentiation has been questioned.[97]
Skeletal system
[edit]Estrogens are responsible for both the pubertal growth spurt, which causes an acceleration in linear growth, and epiphyseal closure, which limits height and limb length, in both females and males. In addition, estrogens are responsible for bone maturation and maintenance of bone mineral density throughout life. Due to hypoestrogenism, the risk of osteoporosis increases during menopause.[98]
Cardiovascular system
[edit]Women are less impacted by heart disease due to vasculo-protective action of estrogen which helps in preventing atherosclerosis.[99] It also helps in maintaining the delicate balance between fighting infections and protecting arteries from damage thus lowering the risk of cardiovascular disease.[100] During pregnancy, high levels of estrogens increase coagulation and the risk of venous thromboembolism. Estrogen has been shown to upregulate the peptide hormone adropin.[47]
| Absolute incidence of first VTE per 10,000 person–years during pregnancy and the postpartum period | ||||||||
|---|---|---|---|---|---|---|---|---|
| Swedish data A | Swedish data B | English data | Danish data | |||||
| Time period | N | Rate (95% CI) | N | Rate (95% CI) | NФВяы | Rate (95% CI) | N | Rate (95% CI) |
| Outside pregnancy | 1105 | 4.2 (4.0–4.4) | 1015 | 3.8 (?) | 1480 | 3.2 (3.0–3.3) | 2895 | 3.6 (3.4–3.7) |
| Antepartum | 995 | 20.5 (19.2–21.8) | 690 | 14.2 (13.2–15.3) | 156 | 9.9 (8.5–11.6) | 491 | 10.7 (9.7–11.6) |
| Trimester 1 | 207 | 13.6 (11.8–15.5) | 172 | 11.3 (9.7–13.1) | 23 | 4.6 (3.1–7.0) | 61 | 4.1 (3.2–5.2) |
| Trimester 2 | 275 | 17.4 (15.4–19.6) | 178 | 11.2 (9.7–13.0) | 30 | 5.8 (4.1–8.3) | 75 | 5.7 (4.6–7.2) |
| Trimester 3 | 513 | 29.2 (26.8–31.9) | 340 | 19.4 (17.4–21.6) | 103 | 18.2 (15.0–22.1) | 355 | 19.7 (17.7–21.9) |
| Around delivery | 115 | 154.6 (128.8–185.6) | 79 | 106.1 (85.1–132.3) | 34 | 142.8 (102.0–199.8) | –
| |
| Postpartum | 649 | 42.3 (39.2–45.7) | 509 | 33.1 (30.4–36.1) | 135 | 27.4 (23.1–32.4) | 218 | 17.5 (15.3–20.0) |
| Early postpartum | 584 | 75.4 (69.6–81.8) | 460 | 59.3 (54.1–65.0) | 177 | 46.8 (39.1–56.1) | 199 | 30.4 (26.4–35.0) |
| Late postpartum | 65 | 8.5 (7.0–10.9) | 49 | 6.4 (4.9–8.5) | 18 | 7.3 (4.6–11.6) | 319 | 3.2 (1.9–5.0) |
| Incidence rate ratios (IRRs) of first VTE during pregnancy and the postpartum period | ||||||||
| Swedish data A | Swedish data B | English data | Danish data | |||||
| Time period | IRR* (95% CI) | IRR* (95% CI) | IRR (95% CI)† | IRR (95% CI)† | ||||
| Outside pregnancy | Reference (i.e., 1.00)
| |||||||
| Antepartum | 5.08 (4.66–5.54) | 3.80 (3.44–4.19) | 3.10 (2.63–3.66) | 2.95 (2.68–3.25) | ||||
| Trimester 1 | 3.42 (2.95–3.98) | 3.04 (2.58–3.56) | 1.46 (0.96–2.20) | 1.12 (0.86–1.45) | ||||
| Trimester 2 | 4.31 (3.78–4.93) | 3.01 (2.56–3.53) | 1.82 (1.27–2.62) | 1.58 (1.24–1.99) | ||||
| Trimester 3 | 7.14 (6.43–7.94) | 5.12 (4.53–5.80) | 5.69 (4.66–6.95) | 5.48 (4.89–6.12) | ||||
| Around delivery | 37.5 (30.9–44.45) | 27.97 (22.24–35.17) | 44.5 (31.68–62.54) | –
| ||||
| Postpartum | 10.21 (9.27–11.25) | 8.72 (7.83–9.70) | 8.54 (7.16–10.19) | 4.85 (4.21–5.57) | ||||
| Early postpartum | 19.27 (16.53–20.21) | 15.62 (14.00–17.45) | 14.61 (12.10–17.67) | 8.44 (7.27–9.75) | ||||
| Late postpartum | 2.06 (1.60–2.64) | 1.69 (1.26–2.25) | 2.29 (1.44–3.65) | 0.89 (0.53–1.39) | ||||
| Notes: Swedish data A = Using any code for VTE regardless of confirmation. Swedish data B = Using only algorithm-confirmed VTE. Early postpartum = First 6 weeks after delivery. Late postpartum = More than 6 weeks after delivery. * = Adjusted for age and calendar year. † = Unadjusted ratio calculated based on the data provided. Source: [101] | ||||||||
Immune system
[edit]The effect of estrogen on the immune system is in general described as Th2 favoring, rather than suppressive, as is the case of the effect of male sex hormone – testosterone.[102] Indeed, women respond better to vaccines, infections and are generally less likely to develop cancer, the tradeoff of this is that they are more likely to develop an autoimmune disease.[103] The Th2 shift manifests itself in a decrease of cellular immunity and increase in humoral immunity (antibody production) shifts it from cellular to humoral by downregulating cell-mediated immunity and enhancing Th2 immune response by stimulating IL-4 production and Th2 differentiation.[102][104] Type 1 and type 17 immune responses are downregulated, likely to be at least partially due to IL-4, which inhibits Th1. Effect of estrogen on different immune cells' cell types is in line with its Th2 bias. Activity of basophils, eosinophils, M2 macrophages and is enhanced, whereas activity of NK cells is downregulated. Conventional dendritic cells are biased towards Th2 under the influence of estrogen, whereas plasmacytoid dendritic cells, key players in antiviral defence, have increased IFN-g secretion.[104] Estrogen also influences B cells by increasing their survival, proliferation, differentiation and function, which corresponds with higher antibody and B cell count generally detected in women.[105]
On a molecular level estrogen induces the above-mentioned effects on cell via acting on intracellular receptors termed ER α and ER β, which upon ligation form either homo or heterodimers. The genetic and nongenetic targets of the receptors differ between homo and heterodimers.[106] Ligation of these receptors allows them to translocate to the nucleus and act as transcription factors either by binding estrogen response elements (ERE) on DNA or binding DNA together with other transcriptional factors e.g. Nf-kB or AP-1, both of which result in RNA polymerase recruitment and further chromatin remodelation.[106] A non-transcriptional response to oestrogen stimulation was also documented (termed membrane-initiated steroid signalling, MISS). This pathway stimulates the ERK and PI3K/AKT pathways, which are known to increase cellular proliferation and affect chromatin remodelation.[106]
Associated conditions
[edit]Researchers have implicated estrogens in various estrogen-dependent conditions, such as ER-positive breast cancer, as well as a number of genetic conditions involving estrogen signaling or metabolism, such as estrogen insensitivity syndrome, aromatase deficiency, and aromatase excess syndrome.[citation needed]
High estrogen can amplify stress-hormone responses in stressful situations.[107]
Biochemistry
[edit]Biosynthesis
[edit]
Estrogens, in females, are produced primarily by the ovaries, and during pregnancy, the placenta.[109] Follicle-stimulating hormone (FSH) stimulates the ovarian production of estrogens by the granulosa cells of the ovarian follicles and corpora lutea. Some estrogens are also produced in smaller amounts by other tissues such as the liver, pancreas, bone, adrenal glands, skin, brain, adipose tissue,[110] and the breasts.[111] These secondary sources of estrogens are especially important in postmenopausal women.[112] The pathway of estrogen biosynthesis in extragonadal tissues is different. These tissues are not able to synthesize C19 steroids, and therefore depend on C19 supplies from other tissues[112] and the level of aromatase.[113]
In females, synthesis of estrogens starts in theca interna cells in the ovary, by the synthesis of androstenedione from cholesterol. Androstenedione is a substance of weak androgenic activity which serves predominantly as a precursor for more potent androgens such as testosterone as well as estrogen. This compound crosses the basal membrane into the surrounding granulosa cells, where it is converted either immediately into estrone, or into testosterone and then estradiol in an additional step. The conversion of androstenedione to testosterone is catalyzed by 17β-hydroxysteroid dehydrogenase (17β-HSD), whereas the conversion of androstenedione and testosterone into estrone and estradiol, respectively is catalyzed by aromatase, enzymes which are both expressed in granulosa cells. In contrast, granulosa cells lack 17α-hydroxylase and 17,20-lyase, whereas theca cells express these enzymes and 17β-HSD but lack aromatase. Hence, both granulosa and theca cells are essential for the production of estrogen in the ovaries.[citation needed]
Estrogen levels vary through the menstrual cycle, with levels highest near the end of the follicular phase just before ovulation.
Note that in males, estrogen is also produced by the Sertoli cells when FSH binds to their FSH receptors.
| Sex | Sex hormone | Reproductive phase |
Blood production rate |
Gonadal secretion rate |
Metabolic clearance rate |
Reference range (serum levels) | |
|---|---|---|---|---|---|---|---|
| SI units | Non-SI units | ||||||
| Men | Androstenedione | –
|
2.8 mg/day | 1.6 mg/day | 2200 L/day | 2.8–7.3 nmol/L | 80–210 ng/dL |
| Testosterone | –
|
6.5 mg/day | 6.2 mg/day | 950 L/day | 6.9–34.7 nmol/L | 200–1000 ng/dL | |
| Estrone | –
|
150 μg/day | 110 μg/day | 2050 L/day | 37–250 pmol/L | 10–70 pg/mL | |
| Estradiol | –
|
60 μg/day | 50 μg/day | 1600 L/day | <37–210 pmol/L | 10–57 pg/mL | |
| Estrone sulfate | –
|
80 μg/day | Insignificant | 167 L/day | 600–2500 pmol/L | 200–900 pg/mL | |
| Women | Androstenedione | –
|
3.2 mg/day | 2.8 mg/day | 2000 L/day | 3.1–12.2 nmol/L | 89–350 ng/dL |
| Testosterone | –
|
190 μg/day | 60 μg/day | 500 L/day | 0.7–2.8 nmol/L | 20–81 ng/dL | |
| Estrone | Follicular phase | 110 μg/day | 80 μg/day | 2200 L/day | 110–400 pmol/L | 30–110 pg/mL | |
| Luteal phase | 260 μg/day | 150 μg/day | 2200 L/day | 310–660 pmol/L | 80–180 pg/mL | ||
| Postmenopause | 40 μg/day | Insignificant | 1610 L/day | 22–230 pmol/L | 6–60 pg/mL | ||
| Estradiol | Follicular phase | 90 μg/day | 80 μg/day | 1200 L/day | <37–360 pmol/L | 10–98 pg/mL | |
| Luteal phase | 250 μg/day | 240 μg/day | 1200 L/day | 699–1250 pmol/L | 190–341 pg/mL | ||
| Postmenopause | 6 μg/day | Insignificant | 910 L/day | <37–140 pmol/L | 10–38 pg/mL | ||
| Estrone sulfate | Follicular phase | 100 μg/day | Insignificant | 146 L/day | 700–3600 pmol/L | 250–1300 pg/mL | |
| Luteal phase | 180 μg/day | Insignificant | 146 L/day | 1100–7300 pmol/L | 400–2600 pg/mL | ||
| Progesterone | Follicular phase | 2 mg/day | 1.7 mg/day | 2100 L/day | 0.3–3 nmol/L | 0.1–0.9 ng/mL | |
| Luteal phase | 25 mg/day | 24 mg/day | 2100 L/day | 19–45 nmol/L | 6–14 ng/mL | ||
Notes and sources
Notes: "The concentration of a steroid in the circulation is determined by the rate at which it is secreted from glands, the rate of metabolism of precursor or prehormones into the steroid, and the rate at which it is extracted by tissues and metabolized. The secretion rate of a steroid refers to the total secretion of the compound from a gland per unit time. Secretion rates have been assessed by sampling the venous effluent from a gland over time and subtracting out the arterial and peripheral venous hormone concentration. The metabolic clearance rate of a steroid is defined as the volume of blood that has been completely cleared of the hormone per unit time. The production rate of a steroid hormone refers to entry into the blood of the compound from all possible sources, including secretion from glands and conversion of prohormones into the steroid of interest. At steady state, the amount of hormone entering the blood from all sources will be equal to the rate at which it is being cleared (metabolic clearance rate) multiplied by blood concentration (production rate = metabolic clearance rate × concentration). If there is little contribution of prohormone metabolism to the circulating pool of steroid, then the production rate will approximate the secretion rate." Sources: See template. | |||||||
Distribution
[edit]Estrogens are plasma protein bound to albumin and/or sex hormone-binding globulin in the circulation.
Metabolism
[edit]Estrogens are metabolized via hydroxylation by cytochrome P450 enzymes such as CYP1A1 and CYP3A4 and via conjugation by estrogen sulfotransferases (sulfation) and UDP-glucuronyltransferases (glucuronidation). In addition, estradiol is dehydrogenated by 17β-hydroxysteroid dehydrogenase into the much less potent estrogen estrone. These reactions occur primarily in the liver, but also in other tissues.[citation needed]
Estrogen metabolism in humans
|
Excretion
[edit]Estrogens are inactivated primarily by the kidneys and liver and excreted via the gastrointestinal tract[114] in the form of conjugates, found in feces, bile, and urine.[115]
Medical use
[edit]Estrogens are used as medications, mainly in hormonal contraception, hormone replacement therapy,[116] and to treat gender dysphoria in transgender women and other transfeminine individuals as part of feminizing hormone therapy.[117]
Chemistry
[edit]The estrogen steroid hormones are estrane steroids.[citation needed]
History
[edit]In 1929, Adolf Butenandt and Edward Adelbert Doisy independently isolated and purified estrone, the first estrogen to be discovered.[118] Then, estriol and estradiol were discovered in 1930 and 1933, respectively. Shortly following their discovery, estrogens, both natural and synthetic, were introduced for medical use. Examples include estriol glucuronide (Emmenin, Progynon), estradiol benzoate, conjugated estrogens (Premarin), diethylstilbestrol, and ethinylestradiol.
The word estrogen derives from Ancient Greek. It is derived from "oestros"[119] (a periodic state of sexual activity in female mammals), and genos (generating).[119] It was first published in the early 1920s and referenced as "oestrin".[120] With the years, American English adapted the spelling of estrogen to fit with its phonetic pronunciation.
Society and culture
[edit]Etymology
[edit]The name estrogen is derived from the Greek οἶστρος (oîstros), literally meaning "verve" or "inspiration" but figuratively sexual passion or desire,[121] and the suffix -gen, meaning "producer of".
Environment
[edit]A range of synthetic and natural substances that possess estrogenic activity have been identified in the environment and are referred to xenoestrogens.[122]
- Synthetic substances such as bisphenol A as well as metalloestrogens (e.g., cadmium).
- Plant products with estrogenic activity are called phytoestrogens (e.g., coumestrol, daidzein, genistein, miroestrol).
- Those produced by fungi are known as mycoestrogens (e.g., zearalenone).
Estrogens are among the wide range of endocrine-disrupting compounds because they have high estrogenic potency. When an endocrine-disrupting compound makes its way into the environment, it may cause male reproductive dysfunction to wildlife and humans.[12][13] The estrogen excreted from farm animals makes its way into fresh water systems.[123][124] During the germination period of reproduction the fish are exposed to low levels of estrogen which may cause reproductive dysfunction to male fish.[125][126]
Cosmetics
[edit]Some hair shampoos on the market include estrogens and placental extracts; others contain phytoestrogens. In 1998, there were case reports of four prepubescent African-American girls developing breasts after exposure to these shampoos.[127] In 1993, the FDA determined that not all over-the-counter topically applied hormone-containing drug products for human use are generally recognized as safe and effective and are misbranded. An accompanying proposed rule deals with cosmetics, concluding that any use of natural estrogens in a cosmetic product makes the product an unapproved new drug and that any cosmetic using the term "hormone" in the text of its labeling or in its ingredient statement makes an implied drug claim, subjecting such a product to regulatory action.[128]
In addition to being considered misbranded drugs, products claiming to contain placental extract may also be deemed to be misbranded cosmetics if the extract has been prepared from placentas from which the hormones and other biologically active substances have been removed and the extracted substance consists principally of protein. The FDA recommends that this substance be identified by a name other than "placental extract" and describing its composition more accurately because consumers associate the name "placental extract" with a therapeutic use of some biological activity.[128]
See also
[edit]References
[edit]- ^ a b c Huether SE, McCance KL (2019). Understanding Pathophysiology. Elsevier Health Sciences. p. 767. ISBN 978-0-32-367281-8.
Estrogen is a generic term for any of three similar hormones derived from cholesterol: estradiol, estrone, and estriol.
- ^ Satoskar RS, Rege N, Bhandarkar SD (2017). Pharmacology and Pharmacotherapeutics. Elsevier Health Sciences. p. 943. ISBN 978-8-13-124941-3.
The natural estrogens are steroids. However, typical estrogenic activity is also shown by chemicals which are not steroids. Hence, the term 'estrogen' is used as a generic term to describe all the compounds having estrogenic activity.
- ^ Delgado BJ, Lopez-Ojeda W (20 December 2021). "Estrogen". StatPearls [Internet]. StatPearls Publishing. PMID 30855848.
Estrogen is a steroid hormone associated with the female reproductive organs and is responsible for the development of female sexual characteristics. Estrogen is often referred to as estrone, estradiol, and estriol. ... Synthetic estrogen is also available for clinical use, designed to increase absorption and effectiveness by altering the estrogen chemical structure for topical or oral administration. Synthetic steroid estrogens include ethinyl estradiol, estradiol valerate, estropipate, conjugate esterified estrogen, and quinestrol.
- ^ Ryan KJ (August 1982). "Biochemistry of aromatase: significance to female reproductive physiology". Cancer Research. 42 (8 Suppl): 3342s – 3344s. PMID 7083198.
- ^ Mechoulam R, Brueggemeier RW, Denlinger DL (September 2005). "Estrogens in insects". Cellular and Molecular Life Sciences. 40 (9): 942–944. doi:10.1007/BF01946450. S2CID 31950471.
- ^ Burger HG (April 2002). "Androgen production in women". Fertility and Sterility. 77 (Suppl 4): S3 – S5. doi:10.1016/S0015-0282(02)02985-0. PMID 12007895.
- ^ Lombardi G, Zarrilli S, Colao A, Paesano L, Di Somma C, Rossi F, et al. (June 2001). "Estrogens and health in males". Molecular and Cellular Endocrinology. 178 (1–2): 51–55. doi:10.1016/S0303-7207(01)00420-8. PMID 11403894. S2CID 36834775.
- ^ Whitehead SA, Nussey S (2001). Endocrinology: an integrated approach. Oxford: BIOS: Taylor & Francis. ISBN 978-1-85996-252-7. PMID 20821847.
- ^ Soltysik K, Czekaj P (April 2013). "Membrane estrogen receptors – is it an alternative way of estrogen action?". Journal of Physiology and Pharmacology. 64 (2): 129–142. PMID 23756388.
- ^ Micevych PE, Kelly MJ (2012). "Membrane estrogen receptor regulation of hypothalamic function". Neuroendocrinology. 96 (2): 103–110. doi:10.1159/000338400. PMC 3496782. PMID 22538318.
- ^ Prossnitz ER, Arterburn JB, Sklar LA (February 2007). "GPR30: A G protein-coupled receptor for estrogen". Molecular and Cellular Endocrinology. 265–266: 138–142. doi:10.1016/j.mce.2006.12.010. PMC 1847610. PMID 17222505.
- ^ a b Wang S, Huang W, Fang G, Zhang Y, Qiao H (2008). "Analysis of steroidal estrogen residues in food and environmental samples". International Journal of Environmental Analytical Chemistry. 88 (1): 1–25. Bibcode:2008IJEAC..88....1W. doi:10.1080/03067310701597293. S2CID 93975613.
- ^ a b Korach KD (1998). Reproductive and developmental toxicology. New York: Marcel Dekker. ISBN 0-585-15807-X. OCLC 44957536.
- ^ A. Labhart (6 December 2012). Clinical Endocrinology: Theory and Practice. Springer Science & Business Media. pp. 548–. ISBN 978-3-642-96158-8.
- ^ Baker ME (March 2013). "What are the physiological estrogens?". Steroids. 78 (3): 337–340. doi:10.1016/j.steroids.2012.12.011. PMID 23313336. S2CID 11803629.
- ^ Miller KK, Al-Rayyan N, Ivanova MM, Mattingly KA, Ripp SL, Klinge CM, et al. (January 2013). "DHEA metabolites activate estrogen receptors alpha and beta". Steroids. 78 (1): 15–25. doi:10.1016/j.steroids.2012.10.002. PMC 3529809. PMID 23123738.
- ^ Bhavnani BR, Nisker JA, Martin J, Aletebi F, Watson L, Milne JK (2000). "Comparison of pharmacokinetics of a conjugated equine estrogen preparation (premarin) and a synthetic mixture of estrogens (C.E.S.) in postmenopausal women". Journal of the Society for Gynecologic Investigation. 7 (3): 175–183. doi:10.1016/s1071-5576(00)00049-6. PMID 10865186.
- ^ Häggström M (2014). "Reference ranges for estradiol, progesterone, luteinizing hormone and follicle-stimulating hormone during the menstrual cycle". WikiJournal of Medicine. 1 (1). doi:10.15347/wjm/2014.001. ISSN 2002-4436.
- ^ Lin CY, Ström A, Vega VB, Kong SL, Yeo AL, Thomsen JS, et al. (2004). "Discovery of estrogen receptor alpha target genes and response elements in breast tumor cells". Genome Biology. 5 (9) R66. doi:10.1186/gb-2004-5-9-r66. PMC 522873. PMID 15345050.
- ^ Darabi M, Ani M, Panjehpour M, Rabbani M, Movahedian A, Zarean E (2011). "Effect of estrogen receptor β A1730G polymorphism on ABCA1 gene expression response to postmenopausal hormone replacement therapy". Genetic Testing and Molecular Biomarkers. 15 (1–2): 11–15. doi:10.1089/gtmb.2010.0106. PMID 21117950.
- ^ Lauwers J, Shinskie D (2004). Counseling the Nursing Mother: A Lactation Consultant's Guide. Jones & Bartlett Learning, LLC. p. 93. ISBN 978-0-7637-2765-9. Retrieved 12 October 2023.
- ^ Raloff J (6 December 1997). "Science News Online (12/6/97): Estrogen's Emerging Manly Alter Ego". Science News. Retrieved 4 March 2008.
- ^ Hess RA, Bunick D, Lee KH, Bahr J, Taylor JA, Korach KS, et al. (December 1997). "A role for oestrogens in the male reproductive system". Nature. 390 (6659): 509–512. Bibcode:1997Natur.390..509H. doi:10.1038/37352. PMC 5719867. PMID 9393999.
- ^ "Estrogen Linked To Sperm Count, Male Fertility". Science Blog. Archived from the original on 7 May 2007. Retrieved 4 March 2008.
- ^ Hill RA, Pompolo S, Jones ME, Simpson ER, Boon WC (December 2004). "Estrogen deficiency leads to apoptosis in dopaminergic neurons in the medial preoptic area and arcuate nucleus of male mice". Molecular and Cellular Neurosciences. 27 (4): 466–476. doi:10.1016/j.mcn.2004.04.012. PMID 15555924. S2CID 25280077.
- ^ Martucci C, Fishman J (March 1976). "Uterine estrogen receptor binding of catecholestrogens and of estetrol (1,3,5(10)-estratriene-3,15alpha,16alpha,17beta-tetrol)". Steroids. 27 (3): 325–333. doi:10.1016/0039-128x(76)90054-4. PMID 178074. S2CID 54412821.
- ^ Martucci C, Fishman J (December 1977). "Direction of estradiol metabolism as a control of its hormonal action--uterotrophic activity of estradiol metabolites". Endocrinology. 101 (6): 1709–1715. doi:10.1210/endo-101-6-1709. PMID 590186.
- ^ Fishman J, Martucci C (December 1978). "Differential biological activity of estradiol metabolites". Pediatrics. 62 (6 Pt 2): 1128–1133. doi:10.1542/peds.62.6.1128. PMID 724350. S2CID 29609115.
- ^ Martucci CP, Fishman J (December 1979). "Impact of continuously administered catechol estrogens on uterine growth and luteinizing hormone secretion". Endocrinology. 105 (6): 1288–1292. doi:10.1210/endo-105-6-1288. PMID 499073.
- ^ Fishman J, Martucci CP (1980). "New Concepts of Estrogenic Activity: the Role of Metabolites in the Expression of Hormone Action". In Pasetto N, Paoletti R, Ambrus JL (eds.). The Menopause and Postmenopause. pp. 43–52. doi:10.1007/978-94-011-7230-1_5. ISBN 978-94-011-7232-5.
- ^ Fishman J, Martucci C (September 1980). "Biological properties of 16 alpha-hydroxyestrone: implications in estrogen physiology and pathophysiology". The Journal of Clinical Endocrinology and Metabolism. 51 (3): 611–615. doi:10.1210/jcem-51-3-611. PMID 7190977.
- ^ Martucci CP (July 1983). "The role of 2-methoxyestrone in estrogen action". Journal of Steroid Biochemistry. 19 (1B): 635–638. doi:10.1016/0022-4731(83)90229-7. PMID 6310247.
- ^ Fishman J, Martucci C (1980). "Dissociation of biological activities in metabolites of estradiol". In McLachlan JA (ed.). Estrogens in the Environment: Proceedings of the Symposium on Estrogens in the Environment, Raleigh, North Carolina, U.S.A., September 10-12, 1979. Elsevier. pp. 131–145. ISBN 9780444003720.
- ^ Kuhl H (August 2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- ^ Chidi-Ogbolu N, Baar K (2018). "Effect of Estrogen on Musculoskeletal Performance and Injury Risk". Frontiers in Physiology. 9 1834. doi:10.3389/fphys.2018.01834. PMC 6341375. PMID 30697162.
- ^ Lowe DA, Baltgalvis KA, Greising SM (April 2010). "Mechanisms behind estrogen's beneficial effect on muscle strength in females". Exercise and Sport Sciences Reviews. 38 (2): 61–67. doi:10.1097/JES.0b013e3181d496bc. PMC 2873087. PMID 20335737.
- ^ Max SR (December 1984). "Androgen-estrogen synergy in rat levator ani muscle: glucose-6-phosphate dehydrogenase". Molecular and Cellular Endocrinology. 38 (2–3): 103–107. doi:10.1016/0303-7207(84)90108-4. PMID 6510548. S2CID 24198956.
- ^ Koot RW, Amelink GJ, Blankenstein MA, Bär PR (1991). "Tamoxifen and oestrogen both protect the rat muscle against physiological damage". The Journal of Steroid Biochemistry and Molecular Biology. 40 (4–6): 689–695. doi:10.1016/0960-0760(91)90292-d. PMID 1958566. S2CID 44446541.
- ^ Gavali S, Gupta MK, Daswani B, Wani MR, Sirdeshmukh R, Khatkhatay MI (2019). "LYN, a key mediator in estrogen-dependent suppression of osteoclast differentiation, survival, and function". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1865 (3): 547–557. doi:10.1016/j.bbadis.2018.12.016. PMID 30579930.
- ^ Gavali S, Gupta MK, Daswani B, Wani MR, Sirdeshmukh R, Khatkhatay MI (2019). "Estrogen enhances human osteoblast survival and function via promotion of autophagy". Biochimica et Biophysica Acta (BBA) - Molecular Cell Research. 1866 (9): 1498–1507. doi:10.1016/j.bbamcr.2019.06.014. PMID 31255720.
- ^ Haizlip KM, Harrison BC, Leinwand LA (January 2015). "Sex-based differences in skeletal muscle kinetics and fiber-type composition". Physiology. 30 (1): 30–39. doi:10.1152/physiol.00024.2014. PMC 4285578. PMID 25559153. "Supplementation with estrogen increases the type-IIX percentage composition in the plantaris back to 42%. (70)"
- ^ Frank AP, de Souza Santos R, Palmer BF, Clegg DJ (October 2019). "Determinants of body fat distribution in humans may provide insight about obesity-related health risks". Journal of Lipid Research. 60 (10): 1710–1719. doi:10.1194/jlr.R086975. PMC 6795075. PMID 30097511.
- ^ Brown LM, Gent L, Davis K, Clegg DJ (September 2010). "Metabolic impact of sex hormones on obesity". Brain Research. 1350: 77–85. doi:10.1016/j.brainres.2010.04.056. PMC 2924463. PMID 20441773.
- ^ Janssen I, Powell LH, Kazlauskaite R, Dugan SA (March 2010). "Testosterone and visceral fat in midlife women: the Study of Women's Health Across the Nation (SWAN) fat patterning study". Obesity. 18 (3): 604–610. doi:10.1038/oby.2009.251. PMC 2866448. PMID 19696765.
- ^ Rubinow KB (2017). "Estrogens and Body Weight Regulation in Men". Sex and Gender Factors Affecting Metabolic Homeostasis, Diabetes and Obesity. Advances in Experimental Medicine and Biology. Vol. 1043. Springer. pp. 285–313. doi:10.1007/978-3-319-70178-3_14. ISBN 978-3-319-70177-6. PMC 5835337. PMID 29224100.
- ^ a b c Tonnus W, Maremonti F, Gavali S, Schlecht MN, Gembardt F, Belavgeni A, et al. (September 2025). "Multiple oestradiol functions inhibit ferroptosis and acute kidney injury". Nature. 645 (8082): 1011–1019. Bibcode:2025Natur.645.1011T. doi:10.1038/s41586-025-09389-x. ISSN 1476-4687. PMC 12460175. PMID 40804518.
- ^ a b Stokar J, Gurt I, Cohen-Kfir E, Yakubovsky O, Hallak N, Benyamini H, et al. (June 2022). "Hepatic adropin is regulated by estrogen and contributes to adverse metabolic phenotypes in ovariectomized mice". Molecular Metabolism. 60 101482. doi:10.1016/j.molmet.2022.101482. PMC 9044006. PMID 35364299.
- ^ Frysh P. "Reasons Why Your Face Looks Swollen". WebMD.
- ^ Stachenfeld NS (July 2008). "Sex hormone effects on body fluid regulation". Exercise and Sport Sciences Reviews. 36 (3): 152–159. doi:10.1097/JES.0b013e31817be928. PMC 2849969. PMID 18580296.
- ^ Pawlina W (2023). Histology: A Text and Atlas: With Correlated Cell and Molecular Biology. Wolters Kluwer Health. p. 1481. ISBN 978-1-9751-8152-9. Retrieved 12 October 2023.
- ^ Greenberg J, Bruess C, Oswalt S (2014). "Conception, Pregnancy, and Birth". Exploring the Dimensions of Human Sexuality. Jones & Bartlett Learning. p. 248. ISBN 978-1-4496-4851-0. Retrieved 12 October 2023.
- ^ "Researchers discover genetic causes of higher melanoma risk in men". ScienceDaily.
- ^ Hernando B, Ibarrola-Villava M, Fernandez LP, Peña-Chilet M, Llorca-Cardeñosa M, Oltra SS, et al. (18 March 2016). "Sex-specific genetic effects associated with pigmentation, sensitivity to sunlight, and melanoma in a population of Spanish origin". Biology of Sex Differences. 7 (1) 17. doi:10.1186/s13293-016-0070-1. PMC 4797181. PMID 26998216. "The results of this study suggest that there are indeed sex-specific genetic effects in human pigmentation, with larger effects for darker pigmentation in females compared to males. A plausible cause might be the differentially expressed melanogenic genes in females due to higher oestrogen levels. These sex-specific genetic effects would help explain the presence of darker eye and skin pigmentation in females, as well as the well-known higher melanoma risk displayed by males."
- ^ Massaro D, Massaro GD (December 2004). "Estrogen regulates pulmonary alveolar formation, loss, and regeneration in mice" (PDF). American Journal of Physiology. Lung Cellular and Molecular Physiology. 287 (6): L1154 – L1159. doi:10.1152/ajplung.00228.2004. PMID 15298854. S2CID 24642944. Archived from the original (PDF) on 25 February 2019.
- ^ Christensen A, Bentley GE, Cabrera R, Ortega HH, Perfito N, Wu TJ, et al. (July 2012). "Hormonal regulation of female reproduction". Hormone and Metabolic Research. 44 (8): 587–591. doi:10.1055/s-0032-1306301. PMC 3647363. PMID 22438212.
- ^ Handa RJ, Ogawa S, Wang JM, Herbison AE (January 2012). "Roles for oestrogen receptor β in adult brain function". Journal of Neuroendocrinology. 24 (1): 160–173. doi:10.1111/j.1365-2826.2011.02206.x. PMC 3348521. PMID 21851428.
- ^ Kow LM, Pfaff DW (May 1998). "Mapping of neural and signal transduction pathways for lordosis in the search for estrogen actions on the central nervous system". Behavioural Brain Research. 92 (2): 169–180. doi:10.1016/S0166-4328(97)00189-7. PMID 9638959. S2CID 28276218.
- ^ Warnock JK, Swanson SG, Borel RW, Zipfel LM, Brennan JJ (2005). "Combined esterified estrogens and methyltestosterone versus esterified estrogens alone in the treatment of loss of sexual interest in surgically menopausal women". Menopause. 12 (4): 374–384. doi:10.1097/01.GME.0000153933.50860.FD. PMID 16037752. S2CID 24557071.
- ^ Heiman JR, Rupp H, Janssen E, Newhouse SK, Brauer M, Laan E (May 2011). "Sexual desire, sexual arousal and hormonal differences in premenopausal US and Dutch women with and without low sexual desire". Hormones and Behavior. 59 (5): 772–779. doi:10.1016/j.yhbeh.2011.03.013. PMID 21514299. S2CID 20807391.
- ^ Brisken C, O'Malley B (December 2010). "Hormone action in the mammary gland". Cold Spring Harbor Perspectives in Biology. 2 (12) a003178. doi:10.1101/cshperspect.a003178. PMC 2982168. PMID 20739412.
- ^ Kleinberg DL (February 1998). "Role of IGF-I in normal mammary development". Breast Cancer Research and Treatment. 47 (3): 201–208. doi:10.1023/a:1005998832636. PMID 9516076. S2CID 30440069.
- ^ a b c Johnson LR (2003). Essential Medical Physiology. Academic Press. p. 770. ISBN 978-0-12-387584-6.
- ^ a b c Norman AW, Henry HL (30 July 2014). Hormones. Academic Press. p. 311. ISBN 978-0-08-091906-5.
- ^ a b Coad J, Dunstall M (2011). Anatomy and Physiology for Midwives, with Pageburst online access,3: Anatomy and Physiology for Midwives. Elsevier Health Sciences. p. 413. ISBN 978-0-7020-3489-3.
- ^ Haslam SZ, Osuch JR (1 January 2006). Hormones and Breast Cancer in Post-Menopausal Women. IOS Press. p. 69. ISBN 978-1-58603-653-9.
- ^ Silbernagl S, Despopoulos A (1 January 2011). Color Atlas of Physiology. Thieme. pp. 305–. ISBN 978-3-13-149521-1.
- ^ Fadem B (2007). High-yield Comprehensive USMLE Step 1 Review. Lippincott Williams & Wilkins. pp. 445–. ISBN 978-0-7817-7427-7.
- ^ Blackburn S (14 April 2014). Maternal, Fetal, & Neonatal Physiology. Elsevier Health Sciences. pp. 146–. ISBN 978-0-323-29296-2.
- ^ Strauss JF, Barbieri RL (13 September 2013). Yen and Jaffe's Reproductive Endocrinology. Elsevier Health Sciences. pp. 236–. ISBN 978-1-4557-2758-2.
- ^ Wilson CB, Nizet V, Maldonado Y, Remington JS, Klein JO (24 February 2015). Remington and Klein's Infectious Diseases of the Fetus and Newborn Infant. Elsevier Health Sciences. pp. 190–. ISBN 978-0-323-24147-2.
- ^ Zárate S, Stevnsner T, Gredilla R (2017). "Role of Estrogen and Other Sex Hormones in Brain Aging. Neuroprotection and DNA Repair". Frontiers in Aging Neuroscience. 9 430. doi:10.3389/fnagi.2017.00430. PMC 5743731. PMID 29311911.
- ^ Sherwin BB (February 2012). "Estrogen and cognitive functioning in women: lessons we have learned". Behavioral Neuroscience. 126 (1): 123–127. doi:10.1037/a0025539. PMC 4838456. PMID 22004260.
- ^ Hara Y, Waters EM, McEwen BS, Morrison JH (July 2015). "Estrogen Effects on Cognitive and Synaptic Health Over the Lifecourse". Physiological Reviews. 95 (3): 785–807. doi:10.1152/physrev.00036.2014. PMC 4491541. PMID 26109339.
- ^ Korol DL, Pisani SL (August 2015). "Estrogens and cognition: Friends or foes?: An evaluation of the opposing effects of estrogens on learning and memory". Hormones and Behavior. 74: 105–115. doi:10.1016/j.yhbeh.2015.06.017. PMC 4573330. PMID 26149525.
- ^ Au A, Feher A, McPhee L, Jessa A, Oh S, Einstein G (January 2016). "Estrogens, inflammation and cognition". Frontiers in Neuroendocrinology. 40: 87–100. doi:10.1016/j.yfrne.2016.01.002. PMID 26774208.
- ^ Jacobs E, D'Esposito M (April 2011). "Estrogen shapes dopamine-dependent cognitive processes: implications for women's health". The Journal of Neuroscience. 31 (14): 5286–5293. doi:10.1523/JNEUROSCI.6394-10.2011. PMC 3089976. PMID 21471363.
- ^ Colzato LS, Hommel B (1 January 2014). "Effects of estrogen on higher-order cognitive functions in unstressed human females may depend on individual variation in dopamine baseline levels". Frontiers in Neuroscience. 8: 65. doi:10.3389/fnins.2014.00065. PMC 3985021. PMID 24778605.
- ^ Hogervorst E (March 2013). "Estrogen and the brain: does estrogen treatment improve cognitive function?". Menopause International. 19 (1): 6–19. doi:10.1177/1754045312473873. PMID 27951525. S2CID 10122688.
- ^ Douma SL, Husband C, O'Donnell ME, Barwin BN, Woodend AK (2005). "Estrogen-related mood disorders: reproductive life cycle factors". ANS. Advances in Nursing Science. 28 (4): 364–375. doi:10.1097/00012272-200510000-00008. PMID 16292022. S2CID 9172877.
- ^ Osterlund MK, Witt MR, Gustafsson JA (December 2005). "Estrogen action in mood and neurodegenerative disorders: estrogenic compounds with selective properties-the next generation of therapeutics". Endocrine. 28 (3): 235–242. doi:10.1385/ENDO:28:3:235. PMID 16388113. S2CID 8205014.
- ^ Lasiuk GC, Hegadoren KM (October 2007). "The effects of estradiol on central serotonergic systems and its relationship to mood in women". Biological Research for Nursing. 9 (2): 147–160. doi:10.1177/1099800407305600. PMID 17909167. S2CID 37965502.
- ^ Grigoriadis S, Seeman MV (June 2002). "The role of estrogen in schizophrenia: implications for schizophrenia practice guidelines for women". Canadian Journal of Psychiatry. 47 (5): 437–442. doi:10.1177/070674370204700504. PMID 12085678.
- ^ "PMDD/PMS". The Massachusetts General Hospital Center for Women's Mental Health. Retrieved 12 January 2019.
- ^ Hill RA, McInnes KJ, Gong EC, Jones ME, Simpson ER, Boon WC (February 2007). "Estrogen deficient male mice develop compulsive behavior". Biological Psychiatry. 61 (3): 359–366. doi:10.1016/j.biopsych.2006.01.012. PMID 16566897. S2CID 22669945.
- ^ Benmansour S, Weaver RS, Barton AK, Adeniji OS, Frazer A (April 2012). "Comparison of the effects of estradiol and progesterone on serotonergic function". Biological Psychiatry. 71 (7): 633–641. doi:10.1016/j.biopsych.2011.11.023. PMC 3307822. PMID 22225849.
- ^ Berg SJ, Wynne-Edwards KE (June 2001). "Changes in testosterone, cortisol, and estradiol levels in men becoming fathers". Mayo Clinic Proceedings. 76 (6): 582–592. doi:10.4065/76.6.582. PMID 11393496.
- ^ a b c Cao X, Xu P, Oyola MG, Xia Y, Yan X, Saito K, et al. (October 2014). "Estrogens stimulate serotonin neurons to inhibit binge-like eating in mice". The Journal of Clinical Investigation. 124 (10): 4351–4362. doi:10.1172/JCI74726. PMC 4191033. PMID 25157819.
- ^ Jimerson DC, Lesem MD, Kaye WH, Hegg AP, Brewerton TD (September 1990). "Eating disorders and depression: is there a serotonin connection?". Biological Psychiatry. 28 (5): 443–454. doi:10.1016/0006-3223(90)90412-u. PMID 2207221. S2CID 31058047.
- ^ Klump KL, Keel PK, Racine SE, Burt SA, Burt AS, Neale M, et al. (February 2013). "The interactive effects of estrogen and progesterone on changes in emotional eating across the menstrual cycle". Journal of Abnormal Psychology. 122 (1): 131–137. doi:10.1037/a0029524. PMC 3570621. PMID 22889242.
- ^ a b Edler C, Lipson SF, Keel PK (January 2007). "Ovarian hormones and binge eating in bulimia nervosa". Psychological Medicine. 37 (1): 131–141. doi:10.1017/S0033291706008956. PMID 17038206. S2CID 36609028.
- ^ a b Klump KL, Racine SE, Hildebrandt B, Burt SA, Neale M, Sisk CL, et al. (September 2014). "Ovarian Hormone Influences on Dysregulated Eating: A Comparison of Associations in Women with versus without Binge Episodes". Clinical Psychological Science. 2 (4): 545–559. doi:10.1177/2167702614521794. PMC 4203460. PMID 25343062.
- ^ Klump KL, Keel PK, Culbert KM, Edler C (December 2008). "Ovarian hormones and binge eating: exploring associations in community samples". Psychological Medicine. 38 (12): 1749–1757. doi:10.1017/S0033291708002997. PMC 2885896. PMID 18307829.
- ^ Lester NA, Keel PK, Lipson SF (January 2003). "Symptom fluctuation in bulimia nervosa: relation to menstrual-cycle phase and cortisol levels". Psychological Medicine. 33 (1): 51–60. doi:10.1017/s0033291702006815. PMID 12537036. S2CID 21497515.
- ^ Wu MV, Manoli DS, Fraser EJ, Coats JK, Tollkuhn J, Honda S, et al. (October 2009). "Estrogen masculinizes neural pathways and sex-specific behaviors". Cell. 139 (1): 61–72. doi:10.1016/j.cell.2009.07.036. PMC 2851224. PMID 19804754.
- ^ Rochira V, Carani C (October 2009). "Aromatase deficiency in men: a clinical perspective". Nature Reviews. Endocrinology. 5 (10): 559–568. doi:10.1038/nrendo.2009.176. hdl:11380/619320. PMID 19707181. S2CID 22116130.
- ^ Wilson JD (September 2001). "Androgens, androgen receptors, and male gender role behavior" (PDF). Hormones and Behavior. 40 (2): 358–366. doi:10.1006/hbeh.2001.1684. PMID 11534997. S2CID 20480423. Archived from the original (PDF) on 26 February 2019.
- ^ Baum MJ (November 2006). "Mammalian animal models of psychosexual differentiation: when is 'translation' to the human situation possible?". Hormones and Behavior. 50 (4): 579–588. doi:10.1016/j.yhbeh.2006.06.003. PMID 16876166. S2CID 7465192.
- ^ Cheng CH, Chen LR, Chen KH (25 January 2022). "Osteoporosis Due to Hormone Imbalance: An Overview of the Effects of Estrogen Deficiency and Glucocorticoid Overuse on Bone Turnover". International Journal of Molecular Sciences. 23 (3): 1376. doi:10.3390/ijms23031376. ISSN 1422-0067. PMC 8836058. PMID 35163300.
- ^ Rosano GM, Panina G (1999). "Oestrogens and the heart". Therapie. 54 (3): 381–385. PMID 10500455.
- ^ Nadkarni S, Cooper D, Brancaleone V, Bena S, Perretti M (November 2011). "Activation of the annexin A1 pathway underlies the protective effects exerted by estrogen in polymorphonuclear leukocytes". Arteriosclerosis, Thrombosis, and Vascular Biology. 31 (11): 2749–2759. doi:10.1161/ATVBAHA.111.235176. PMC 3357483. PMID 21836070.
- ^ Abdul Sultan A, West J, Stephansson O, Grainge MJ, Tata LJ, Fleming KM, et al. (November 2015). "Defining venous thromboembolism and measuring its incidence using Swedish health registries: a nationwide pregnancy cohort study". BMJ Open. 5 (11) e008864. doi:10.1136/bmjopen-2015-008864. PMC 4654387. PMID 26560059.
- ^ a b Foo YZ, Nakagawa S, Rhodes G, Simmons LW (February 2017). "The effects of sex hormones on immune function: a meta-analysis" (PDF). Biological Reviews of the Cambridge Philosophical Society. 92 (1): 551–571. doi:10.1111/brv.12243. PMID 26800512. S2CID 37931012.
- ^ Taneja V (27 August 2018). "Sex Hormones Determine Immune Response". Frontiers in Immunology. 9 1931. doi:10.3389/fimmu.2018.01931. PMC 6119719. PMID 30210492.
- ^ a b Roved J, Westerdahl H, Hasselquist D (February 2017). "Sex differences in immune responses: Hormonal effects, antagonistic selection, and evolutionary consequences". Hormones and Behavior. 88: 95–105. doi:10.1016/j.yhbeh.2016.11.017. PMID 27956226. S2CID 9137227.
- ^ Khan D, Ansar Ahmed S (6 January 2016). "The Immune System Is a Natural Target for Estrogen Action: Opposing Effects of Estrogen in Two Prototypical Autoimmune Diseases". Frontiers in Immunology. 6: 635. doi:10.3389/fimmu.2015.00635. PMC 4701921. PMID 26779182.
- ^ a b c Kovats S (April 2015). "Estrogen receptors regulate innate immune cells and signaling pathways". Cellular Immunology. 294 (2): 63–69. doi:10.1016/j.cellimm.2015.01.018. PMC 4380804. PMID 25682174.
- ^
Prior JC (2018). Estrogen's Storm Season: stories of perimenopause. Vancouver, British Columbia: CeMCOR (Centre for Menstrual Cycle and Ovulation Research). ISBN 978-0-9738275-2-1. Retrieved 24 July 2021.
[...] high estrogen amplifies your stress hormone responses to stressful things [...]
- ^ Häggström M, Richfield D (2014). "Diagram of the pathways of human steroidogenesis". WikiJournal of Medicine. 1 (1). doi:10.15347/wjm/2014.005. ISSN 2002-4436.
- ^ Marieb E (2013). Anatomy & physiology. Benjamin-Cummings. p. 903. ISBN 978-0-321-88760-3.
- ^ Hemsell DL, Grodin JM, Brenner PF, Siiteri PK, MacDonald PC (March 1974). "Plasma precursors of estrogen. II. Correlation of the extent of conversion of plasma androstenedione to estrone with age". The Journal of Clinical Endocrinology and Metabolism. 38 (3): 476–479. doi:10.1210/jcem-38-3-476. PMID 4815174.
- ^ Barakat R, Oakley O, Kim H, Jin J, Ko CJ (September 2016). "Extra-gonadal sites of estrogen biosynthesis and function". BMB Reports. 49 (9): 488–496. doi:10.5483/BMBRep.2016.49.9.141. PMC 5227141. PMID 27530684.
- ^ a b Nelson LR, Bulun SE (September 2001). "Estrogen production and action". Journal of the American Academy of Dermatology. 45 (3 Suppl): S116 – S124. doi:10.1067/mjd.2001.117432. PMID 11511861.
- ^ Labrie F, Bélanger A, Luu-The V, Labrie C, Simard J, Cusan L, et al. (1998). "DHEA and the intracrine formation of androgens and estrogens in peripheral target tissues: its role during aging". Steroids. 63 (5–6): 322–328. doi:10.1016/S0039-128X(98)00007-5. PMID 9618795. S2CID 37344052.
- ^ Schreinder WE (2012). "The Ovary". In Trachsler A, Thorn G, Labhart A, Bürgi H, Dodsworth-Phillips J, Constam G, Courvoisier B, Fischer JA, Froesch ER, Grob P (eds.). Clinical Endocrinology: Theory and Practice. Springer Berlin Heidelberg. p. 530. ISBN 978-3-642-96158-8. Retrieved 12 October 2023.
- ^ Fuentes N, Silveyra P (2019). "Estrogen receptor signaling mechanisms". Advances in Protein Chemistry and Structural Biology. Vol. 116. Elsevier. pp. 135–170. doi:10.1016/bs.apcsb.2019.01.001. ISBN 978-0-12-815561-5. ISSN 1876-1623. PMC 6533072. PMID 31036290.
Physiologically, the metabolic conversion of estrogens allows their excretion from the body via urine, feces, and/or bile, along with the production of estrogen analogs, which have been shown to present antiproliferative effects (Tsuchiya et al., 2005).
- ^ Kuhl H (August 2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric. 8 (Suppl 1): 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- ^ Wesp LM, Deutsch MB (March 2017). "Hormonal and Surgical Treatment Options for Transgender Women and Transfeminine Spectrum Persons". The Psychiatric Clinics of North America. 40 (1): 99–111. doi:10.1016/j.psc.2016.10.006. PMID 28159148.
- ^ Tata JR (June 2005). "One hundred years of hormones". EMBO Reports. 6 (6): 490–496. doi:10.1038/sj.embor.7400444. PMC 1369102. PMID 15940278.
- ^ a b "Origin in Biomedical Terms: oestrogen or oestrogen". Bioetymology. Retrieved 24 January 2018.
- ^ "Council on Pharmacy and Chemistry". Journal of the American Medical Association. 107 (15): 1221–3. 1936. doi:10.1001/jama.1936.02770410043011.
- ^ "Greek Word Study Tool: oistros". Perseus Digital Library. Retrieved 28 December 2011.
- ^ Fang H, Tong W, Shi LM, Blair R, Perkins R, Branham W, et al. (March 2001). "Structure-activity relationships for a large diverse set of natural, synthetic, and environmental estrogens". Chemical Research in Toxicology. 14 (3): 280–294. CiteSeerX 10.1.1.460.20. doi:10.1021/tx000208y. PMID 11258977.
- ^ Wise A, O'Brien K, Woodruff T (January 2011). "Are oral contraceptives a significant contributor to the estrogenicity of drinking water?". Environmental Science & Technology. 45 (1): 51–60. doi:10.1021/es1014482. PMID 20977246.
- ^ Peach S. "Don't Blame The Pill | Latest News". Chemical & Engineering News. Retrieved 22 April 2023.
- ^ Liney KE, Jobling S, Shears JA, Simpson P, Tyler CR (October 2005). "Assessing the sensitivity of different life stages for sexual disruption in roach (Rutilus rutilus) exposed to effluents from wastewater treatment works". Environmental Health Perspectives. 113 (10): 1299–1307. Bibcode:2005EnvHP.113.1299L. doi:10.1289/ehp.7921. PMC 1281270. PMID 16203238.
- ^ Jobling S, Williams R, Johnson A, Taylor A, Gross-Sorokin M, Nolan M, et al. (April 2006). "Predicted exposures to steroid estrogens in U.K. rivers correlate with widespread sexual disruption in wild fish populations". Environmental Health Perspectives. 114 (Suppl 1): 32–39. Bibcode:2006EnvHP.114S..32J. doi:10.1289/ehp.8050. PMC 1874167. PMID 16818244.
- ^ Sanghavi DM (17 October 2006). "Preschool Puberty, and a Search for the Causes". The New York Times. Retrieved 4 June 2008.
- ^ a b FDA (February 1995). "Products containing estrogenic hormones, placental extract or vitamins". Guide to Inspections of Cosmetic Product Manufacturers. Archived from the original on 14 October 2007. Retrieved 24 October 2006.
External links
[edit]- Nussey and Whitehead: Endocrinology, an integrated approach, Taylor and Francis 2001. Free online textbook.
Estrogen
View on GrokipediaEstrogens are a class of steroid hormones that regulate the growth, development, and physiology of the female reproductive system, including the promotion of secondary sex characteristics such as breast development and fat distribution.[1][2] The three principal endogenous estrogens are estrone (E1), estradiol (E2), and estriol (E3), with estradiol representing the most potent and dominant form in premenopausal women, driving cyclic changes in the uterus and ovaries.[3][4] Estrogens exert their effects primarily through binding to two nuclear receptors, estrogen receptor alpha (ERα) and estrogen receptor beta (ERβ), which act as transcription factors to modulate gene expression in responsive tissues.[5][2] Biosynthesized mainly in ovarian granulosa cells via the cytochrome P450 aromatase enzyme's conversion of androgens like testosterone into estrogens, their production is also significant in adipose tissue, the brain, and during pregnancy in the placenta.[6][7] In males, estrogens derived from peripheral aromatization contribute to bone maturation, spermatogenesis regulation, and cardiovascular function, underscoring their roles beyond female physiology.[6][8] Dysregulation of estrogen levels or signaling has been linked to conditions such as osteoporosis, breast cancer, and endometriosis, prompting therapeutic applications including hormone replacement therapy, though long-term use carries risks like increased thromboembolism and malignancy in certain contexts.[8][3]
Overview and Types
Definition and Primary Forms
Estrogens constitute a class of steroid hormones primarily responsible for the development, maturation, and maintenance of female reproductive structures and secondary sex characteristics in mammals.[9] These hormones exert their effects by binding to estrogen receptors, influencing gene transcription in target tissues such as the uterus, breasts, and bones.[10] In humans, the three major endogenous estrogens exhibiting hormonal activity are estrone (E1), estradiol (E2, or 17β-estradiol), and estriol (E3).[9][10] Estradiol represents the most potent and biologically active form, predominating in non-pregnant reproductive-age females where it is chiefly secreted by the ovarian granulosa cells following aromatization of androgens.[10][11] Its potency stems from a chemical structure featuring phenolic hydroxyl groups at the 3-position of the A-ring and the 17β-position of the D-ring on the estrane steroid nucleus, enabling high-affinity binding to estrogen receptors α and β.[10] In contrast, estrone, formed via oxidation of estradiol's 17β-hydroxyl group to a ketone, exhibits approximately one-tenth the potency of estradiol and becomes the primary circulating estrogen after menopause due to diminished ovarian function.[11][12] Estriol, the weakest of the trio with potency about one-hundredth that of estradiol, arises mainly as a metabolite of estrone and estradiol and is produced in large quantities by the placenta during pregnancy, where it supports fetal development without strongly stimulating maternal reproductive tissues.[11][7] These estrogens interconvert through enzymatic processes involving 17β-hydroxysteroid dehydrogenases and are present in varying ratios depending on physiological state, with estradiol-estrone conversion being reversible.[3]Receptor Binding and Classification
Estrogens primarily exert their biological effects by binding to estrogen receptors (ERs), which are ligand-activated transcription factors in the nuclear receptor superfamily. The two main classical subtypes, ERα (encoded by ESR1) and ERβ (encoded by ESR2), share high homology in their DNA-binding domains (approximately 95%) but differ in ligand-binding domains (about 60% homology), leading to variations in ligand affinity and tissue-specific responses.[13] [14] Upon binding 17β-estradiol (E2), the most potent endogenous estrogen, ERα and ERβ undergo conformational changes, dimerize (as homodimers or heterodimers), and translocate to the nucleus to interact with estrogen response elements (EREs) on target DNA, thereby regulating gene transcription through activation function domains AF-1 and AF-2.[2] This genomic pathway typically occurs over hours, contrasting with rapid non-genomic signaling via membrane-associated ERs.[8] Endogenous estrogens bind both ERα and ERβ with high affinity, though potencies vary: E2 exhibits the strongest binding (dissociation constant Kd ≈ 0.1–0.6 nM for ERα and slightly lower for ERβ), followed by estrone (E1) with weaker affinity due to its structural differences, and estriol (E3) as the least potent among major forms.[15] [16] ERα generally shows higher transcriptional activation in response to E2 at low concentrations compared to ERβ, which may act as a modulator or inhibitor in certain contexts, such as in breast tissue where ERβ can attenuate ERα-driven proliferation.[14] Tissue distribution influences functional outcomes: ERα predominates in mammary gland, uterus, bone, and liver, mediating proliferative and protective effects, while ERβ is more abundant in ovary, prostate, lung, gastrointestinal tract, and certain brain regions, often associated with anti-proliferative roles.[13] [17] A third receptor, G protein-coupled estrogen receptor 1 (GPER1, formerly GPR30), operates via membrane-bound mechanisms and binds E2 with nanomolar affinity, triggering rapid signaling cascades like ERK activation and calcium mobilization independent of nuclear ERs.[8] [15] Classification of ERs distinguishes classical nuclear types (ERα and ERβ) from non-classical GPER1, with the former enabling both genomic and non-genomic effects through palmitoylation or association with plasma membrane proteins.[2] Estrogens and ligands are further classified by receptor selectivity: non-selective (e.g., E2 binds both ERα and ERβ equipotently), ERα-preferring (e.g., certain synthetic agonists), or ERβ-selective (e.g., prinonal or genistein, a phytoestrogen), which informs therapeutic targeting in conditions like breast cancer where ERα dominance correlates with hormone responsiveness.[13] [16] Such selectivity arises from structural differences in the ligand-binding pockets, allowing subtype-specific modulation without uniform agonism or antagonism across tissues.[18]Biosynthesis and Metabolism
Synthesis Pathways in Gonads and Adrenals
Estrogen synthesis in the gonads and adrenal glands occurs through steroidogenesis, beginning with cholesterol as the precursor and involving enzymatic conversions to androgens followed by aromatization to estrogens. The primary estrogens produced are estradiol (E2) and estrone (E1), with E2 being the most potent. This process requires the steroidogenic acute regulatory protein (StAR) to facilitate cholesterol transport into mitochondria, initiating the pathway across these tissues.[19][20] In the ovaries, estrogen biosynthesis follows a two-cell model involving theca and granulosa cells. Theca cells convert cholesterol to pregnenolone via CYP11A1, then to progesterone via HSD3B2, and subsequently to androstenedione or testosterone via CYP17A1 with 17α-hydroxylase and 17,20-lyase activities, primarily through the Δ5 pathway. These androgens diffuse to granulosa cells, where CYP19A1 (aromatase) catalyzes their conversion to estrone and estradiol; HSD17B1 further interconverts estrone to the more active estradiol. Ovaries are the principal source of circulating E2 in premenopausal females, with production peaking during the follicular phase under FSH and LH regulation.[21][7] In the testes, estrogen synthesis is minor compared to androgen production but essential for local functions like spermatogenesis. Leydig cells primarily synthesize testosterone from cholesterol via similar initial steps (CYP11A1, HSD3B2, CYP17A1), which is then aromatized to estradiol by CYP19A1 expressed in Sertoli cells or germ cells. Testes contribute approximately 20% of circulating estrogens in males, with the remainder from peripheral conversion; this local estrogen regulates gonadal development and inhibits excessive steroidogenesis.[22][23] The adrenal cortex produces negligible direct estrogens under normal physiology, focusing instead on glucocorticoids, mineralocorticoids, and androgens like DHEA and DHEAS from the zona reticularis via CYP11A1, CYP17A1, and sulfation. These C19 steroids serve as precursors for peripheral aromatization to estrogens in adipose tissue or other sites, contributing significantly post-menopause when ovarian function declines. Direct adrenal estrogen secretion is minimal, with any reported amounts (e.g., estrone) not substantially impacting circulating levels.[24][25]Hormonal Regulation and Feedback Loops
![Estradiol levels during the menstrual cycle][float-right]Estrogen production is primarily regulated by the hypothalamic-pituitary-gonadal (HPG) axis, where gonadotropin-releasing hormone (GnRH) is secreted in pulses from the hypothalamus to stimulate the anterior pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH).[26] FSH acts on ovarian granulosa cells to promote follicular development and aromatization of androgens to estradiol, the predominant estrogen, while LH stimulates theca cells to produce androgens as precursors.[27] In males, a similar HPG axis maintains steady estrogen levels through Leydig and Sertoli cells, though at lower amplitudes.[28] Negative feedback predominates during most of the menstrual cycle and in steady-state conditions, where rising estradiol levels inhibit GnRH pulsatility at the hypothalamus via estrogen receptor α (ERα) signaling in kisspeptin neurons and suppress LH and FSH secretion at the pituitary.[29][30] This loop prevents excessive gonadal stimulation and maintains homeostasis; for instance, in ovariectomized models, estrogen replacement restores suppression of gonadotropins, confirming the pathway's role.[26] Nonclassical ERα signaling contributes to this hypothalamic inhibition, distinct from genomic effects.[31] In males, estrogen similarly exerts negative feedback to regulate spermatogenesis and prevent hyperandrogenism.[28] Positive feedback occurs specifically in females during the late follicular phase, when sustained estradiol elevation (typically >200 pg/mL for 36-48 hours) switches to stimulate a GnRH/LH surge, triggering ovulation.[32] This surge depends on ERα-mediated excitation of kisspeptin neurons in the anteroventral periventricular nucleus, overriding negative signals, with progesterone priming enhancing sensitivity.[33][34] The mechanism involves bimodal estradiol actions: low levels suppress, while high levels induce surge via altered gene expression and neuronal firing patterns.[35] Absence of this positive loop, as in ERα knockout models, abolishes surges, underscoring its necessity for cyclic reproduction.[34] In males, positive feedback is absent, ensuring tonic rather than cyclic gonadotropin release.[36]
Distribution, Metabolism, and Excretion
Estrogens, including estradiol (the predominant endogenous form), are lipophilic molecules that distribute extensively to tissues via the bloodstream, with particular accumulation in estrogen-sensitive sites such as the ovaries, uterus, breasts, and bone due to receptor-mediated uptake.[3] Approximately 97-98% of circulating estradiol is protein-bound, primarily to albumin (about 60%) and sex hormone-binding globulin (SHBG; about 37-38%), leaving only 1.5-2% in the unbound, bioactive fraction that can readily cross cell membranes.[37] Protein binding influences bioavailability, with SHBG-bound estrogen exhibiting slower dissociation and reduced clearance compared to albumin-bound forms.[38] Metabolism of endogenous estrogens occurs mainly in the liver, involving reversible interconversion and oxidative transformations followed by conjugation for inactivation. Estradiol is primarily oxidized to estrone via 17β-hydroxysteroid dehydrogenase (17β-HSD), a reaction catalyzed by isoforms like HSD17B1 in target tissues and HSD17B2 in the liver.[39] Further hepatic cytochrome P450 enzymes (e.g., CYP1A1, CYP1B1, CYP3A4) mediate hydroxylation at C2, C4, or C16 positions, producing metabolites such as 2-hydroxyestrone (a catechol estrogen) or 16α-hydroxyestrone, which may exhibit varying estrogenic or genotoxic activities depending on redox balance.[40] These hydroxylated forms undergo phase II conjugation with glucuronic acid (via UGT enzymes) or sulfate (via SULT1E1), enhancing water solubility; sulfation can prolong circulation half-life, while glucuronidation facilitates rapid elimination.[40] The process is stereoselective and influenced by genetic polymorphisms in metabolizing enzymes, with estradiol's terminal plasma half-life ranging from 1-2 hours post-production, though sustained levels arise from continuous ovarian or peripheral synthesis.[38] Excretion of estrogen metabolites occurs predominantly renally, with over 80-90% recovered in urine as glucuronide and sulfate conjugates within 24-48 hours of formation, and minor fecal elimination (5-10%) via enterohepatic recirculation and biliary secretion.[38] Unconjugated estrogens constitute less than 5% of urinary output, reflecting efficient conjugation.[39] Renal clearance is enhanced during high estrogen states (e.g., pregnancy), but age-related declines in glomerular filtration can prolong exposure in postmenopausal women.[40] Overall, the rapid turnover supports tight physiological regulation, preventing accumulation except in pathological conditions like estrogen-producing tumors.[38]Physiological Functions
Roles in Female Reproduction and Development
Estrogen is essential for the maturation of the female reproductive tract during puberty, where rising levels, primarily estradiol produced by the ovaries, drive the proliferation and differentiation of uterine, vaginal, and fallopian tube tissues, alongside the development of secondary sexual characteristics such as breast glandular tissue expansion and pubic hair growth.[41][42] These changes typically commence around ages 8-13, with peak estrogen surges correlating to Tanner stage progression, where estradiol concentrations increase from basal levels below 20 pg/mL to over 100 pg/mL by mid-puberty, facilitating epiphyseal closure and pelvic widening via estrogen receptor-mediated signaling in target organs.[42][41] In ovarian folliculogenesis, estrogen acts locally within follicles through autocrine and paracrine mechanisms, promoting granulosa cell proliferation, differentiation, and the expression of luteinizing hormone receptors necessary for ovulation; estradiol synthesized by theca and granulosa cells under follicle-stimulating hormone stimulation selects the dominant follicle by suppressing atresia in preovulatory stages, with levels peaking at 200-400 pg/mL just prior to the luteinizing hormone surge.[43][44] Disruptions in estrogen signaling, as observed in estrogen receptor knockout models, result in impaired follicle maturation and reduced ovulation rates, underscoring its causal role in cyclic fertility.[44] During the menstrual cycle's proliferative phase, estrogen from the maturing follicle induces endometrial glandular and stromal hyperplasia, increasing thickness from 1-2 mm to 8-12 mm and enhancing vascularization via upregulation of progesterone receptors, which primes the endometrium for decidualization post-ovulation.[45] This estrogen-driven preparation is critical for implantation, as evidenced by studies showing that estradiol priming restores receptivity in hormone replacement models, with optimal serum levels around 150-250 pg/mL correlating to higher pregnancy success in assisted reproduction.[45][46] In pregnancy maintenance, placental estrogen production escalates dramatically—from 10 ng/mL in early gestation to over 20,000 ng/mL by term—supporting trophoblast invasion, uterine quiescence through suppression of oxytocin receptors, and cervical remodeling, while deficiencies in early pregnancy are linked to increased miscarriage risk due to inadequate endometrial support.[47][48] Estrogen also facilitates mammary alveolar development for lactation, with knockout studies demonstrating halted ductal branching without estrogen receptor alpha activity.[49]Effects on Female Secondary Characteristics and Systemic Health
Estrogen, primarily in the form of estradiol, drives the development of female secondary sex characteristics during puberty by stimulating target tissues via estrogen receptors. Thelarche, typically occurring between ages 8 and 13, marks the initial breast development as estrogen promotes proliferation of mammary ductal epithelium and accumulation of adipose tissue in the breasts.[42] This process is preceded by rising gonadotropins (FSH and LH) that trigger ovarian estradiol production, leading to Tanner stage progression in breast maturation.[42] Estrogen also induces skeletal changes, including pelvic widening through accelerated growth of the iliac crests and ischial tuberosities, resulting in a wider subischial pelvis diameter by approximately 2-3 cm compared to males.[41] It facilitates gynoid fat redistribution to the hips, thighs, and gluteal region, increasing body fat percentage to 22-28% in females versus 12-18% in males, which supports reproductive energy reserves.[42] Additionally, estrogen contributes to the growth and maturation of external genitalia, such as labial development and pubic hair growth in an inverse triangular pattern, though the latter involves androgen-estrogen interactions.[41] In systemic health, estrogen maintains bone mineral density (BMD) by suppressing osteoclast-mediated resorption and enhancing osteoblast activity, with premenopausal women exhibiting peak BMD levels 10-15% higher than age-matched men due to prolonged estrogen exposure.[50] Postmenopausal estrogen decline accelerates trabecular bone loss at rates of 2-3% per year initially, elevating osteoporosis risk, as evidenced by dual-energy X-ray absorptiometry scans showing reduced femoral neck and lumbar spine BMD in estrogen-deficient states.[41] Estrogen exerts cardioprotective effects in premenopausal women, correlating with 2-3 times lower coronary heart disease incidence compared to men, through endothelial nitric oxide production for vasodilation, HDL cholesterol elevation by 10-15%, and LDL reduction.[51] [52] These benefits diminish post-menopause, with observational data linking earlier menopause (before age 45) to 50% higher CVD mortality risk.[53] Estrogen also supports skin integrity by stimulating collagen synthesis types I and III, preserving dermal thickness and elasticity, with postmenopausal drops linked to 30% collagen loss within five years.[41] However, systemic effects include prothrombotic tendencies via increased clotting factors, which may contribute to venous thromboembolism risks in certain contexts.[54]Functions in Males: Spermatogenesis, Libido, and Bone Maintenance
In males, estrogen, primarily estradiol derived from the aromatization of testosterone, plays essential roles in reproductive and skeletal physiology despite lower circulating levels compared to females. Aromatase enzyme activity in the testes, particularly in Leydig and Sertoli cells, facilitates local estrogen production critical for germ cell development and maturation.[55] Deficiency states, such as aromatase deficiency or estrogen receptor mutations, underscore estrogen's necessity, as affected individuals exhibit infertility and skeletal abnormalities reversible by estrogen administration.[56] Estrogen supports spermatogenesis by regulating fluid reabsorption in the rete testis, efferent ductules, and epididymis, preventing sperm dilution and ensuring motility. Estrogen receptor alpha (ERα) knockout in mice disrupts spermatid production and spermiogenesis, leading to reduced fertility, while human studies link low estradiol to germ cell apoptosis and impaired sperm parameters.[57] [58] In men with aromatase deficiency, spermatogenesis is arrested at the spermatid stage, with fertility restoration following estradiol therapy, indicating a direct causal role beyond mere androgen mediation.[23] [55] Estradiol modulates male libido through central and peripheral mechanisms, with both hypo- and hyper-estrogenemia associated with sexual dysfunction. High estradiol suppresses libido directly and indirectly by elevating sex hormone-binding globulin (SHBG), thereby reducing free testosterone bioavailability.[59] Low estradiol, such as from aromatase inhibition, markedly decreases libido and causes joint pain and mood disturbances.[60] In testosterone-deficient men, selective aromatase inhibition reduces libido, reversible by estradiol supplementation, suggesting estrogen's independent contribution alongside testosterone.[61] Clinical observations in aromatase-deficient males show profound libido loss alleviated by estrogen treatment, corroborated by rodent models where ERα activation enhances sexual behavior.[62] Population studies report inverse correlations between low serum estradiol and sexual desire scores, though short-term elevations may not acutely boost function, emphasizing balanced levels for homeostasis.[59] [63] Estrogen maintains bone density in males by suppressing osteoclast activity and bone resorption via ERα signaling, independent of testosterone's effects on formation. Longitudinal studies of elderly men demonstrate that estradiol levels below 10-20 pg/mL predict accelerated bone loss and fracture risk, with testosterone showing weaker associations after adjusting for estrogen.[64] [65] In a case of aromatase deficiency treated with estradiol from age 24, bone mineral density increased by up to 70% over two years, confirming estrogen's pivotal role in peak bone mass acquisition and adult maintenance.[66] Mechanistic evidence from cell culture and animal models shows estrogen inhibits RANKL-mediated osteoclastogenesis, preserving trabecular architecture against age-related decline.[67]Sex-Specific Brain and Behavioral Effects
Estrogen exerts organizational effects on the brain during critical developmental periods, establishing sex-specific neural circuits that underlie behavioral dimorphisms. In male mammals, circulating testosterone is locally aromatized to estradiol within the brain, which binds to estrogen receptors to masculinize structures such as the preoptic area and hypothalamus, promoting male-typical behaviors like mounting and aggression.[68] This process occurs perinatally in rodents—around embryonic day 18 to postnatal day 2—and analogously during the second trimester in humans, where disruptions in aromatase activity lead to defeminized or demasculinized behaviors in animal models.[69] In contrast, female brains develop along a default pathway with minimal gonadal estrogen influence due to alpha-fetoprotein binding, which sequesters circulating estradiol, though emerging evidence suggests estradiol contributes to female-typical sexual differentiation in some circuits.[70][71] These organizational effects manifest in structural sex differences, including larger volumes in male-typical regions like the sexually dimorphic nucleus of the preoptic area, mediated by estrogen receptor signaling that regulates gene expression for neuronal survival and connectivity.[72] In estrogen receptor beta knockout mice, male sexual and aggressive behaviors are impaired, underscoring estrogen's necessity beyond testosterone alone.[73] Human neuroimaging correlates these patterns with prenatal hormone exposure proxies, such as digit ratios, linking higher prenatal estrogen (via aromatization) to enhanced spatial cognition typically male-associated.[74] Behavioral outcomes include sex-dimorphic responses: males show estrogen-dependent territorial aggression, while females exhibit estrogen-modulated maternal and affiliative behaviors, as estradiol surges facilitate oxytocin release in the medial preoptic area.[75][76] In adulthood, activational effects of estrogen further accentuate sex differences, with females displaying cyclic fluctuations tied to ovarian estradiol peaks that enhance verbal memory and fine motor skills but increase vulnerability to mood disorders like premenstrual dysphoric disorder.[77] Males, reliant on steady aromatization from testicular androgens, experience estrogen's maintenance of libido and synaptic plasticity in the hippocampus, where deficiency—as in aromatase-deficient men—impairs spatial navigation.[78][79] Sex-specific neuroprotective roles emerge post-injury, with estradiol preconditioning female brains against stroke via anti-apoptotic pathways, whereas male responses involve androgen-estrogen interplay yielding divergent outcomes.[80] Empirical data from longitudinal studies indicate these effects persist, with postmenopausal estrogen decline accelerating cognitive decline more rapidly in women than age-matched men, highlighting enduring sex-dimorphic vulnerabilities.[81] While rodent models dominate mechanistic insights, human applicability is supported by genetic and endocrine disorder evidence, though confounded by psychosocial factors.[82]Impacts on Skeletal, Cardiovascular, and Immune Systems
Estrogen maintains skeletal integrity primarily by inhibiting osteoclast-mediated bone resorption and promoting osteoblast activity, thereby regulating bone turnover and preserving bone mineral density (BMD) in both sexes.[83] [84] Deficiency in estrogen, as occurs post-menopause in females or with hypogonadism in males, accelerates bone loss, increasing fracture risk; for instance, women experience a 2-3% annual BMD decline in the first postmenopausal years due to elevated RANKL/OPG ratios favoring resorption.[84] [85] Hormone replacement therapy (HRT) with estrogen has demonstrated BMD increases of 2-5% at the spine and hip after 9-12 months in frail elderly women, though long-term fracture reduction benefits vary by formulation and timing.[86] In the cardiovascular system, endogenous estrogen confers protection against atherosclerosis and thrombosis via endothelial nitric oxide production, enhanced vasodilation, and reduced low-density lipoprotein oxidation, contributing to lower pre-menopausal coronary heart disease rates in women compared to age-matched men.[87] Early menopause (before age 45) elevates cardiovascular disease risk by 50% due to prolonged estrogen deprivation, underscoring its causal role in vascular health.[87] Exogenous estrogen in menopausal hormone therapy yields mixed outcomes: transdermal or early-initiated forms may preserve benefits without prothrombotic effects, whereas oral conjugated equine estrogens combined with progestins increase venous thromboembolism risk by 1.5-2-fold and, in older women, coronary events per the Women's Health Initiative trial (initiated 1991, primary results 2002).[88] [89] These risks stem from first-pass hepatic effects elevating triglycerides and coagulation factors like fibrinogen.[89] Estrogen modulates the immune system by influencing cytokine production, T-cell differentiation, and B-cell activation, generally enhancing humoral immunity while suppressing excessive inflammation through estrogen receptor signaling in immune cells.[90] In females, higher estrogen levels correlate with increased autoimmune disease prevalence, such as systemic lupus erythematosus (9:1 female:male ratio), via promotion of Th2 responses and reduced Treg function, though this reflects complex dose-dependent effects rather than uniform immunosuppression.[90] [91] Post-menopausal estrogen decline disrupts immune homeostasis, elevating pro-inflammatory markers like IL-6 and TNF-α, which may heighten infection susceptibility or chronic inflammation; selective estrogen receptor modulators can mitigate this by restoring balance in targeted pathways.[92] [93] Empirical data from knockout models confirm estrogen's direct causal role, as ERα-deficient mice exhibit altered antibody responses and heightened autoimmunity.[90]Molecular Mechanisms
Estrogen Receptors and Signaling Pathways
Estrogen receptors (ERs) primarily consist of two nuclear subtypes, ERα (encoded by the ESR1 gene on chromosome 6) and ERβ (encoded by the ESR2 gene on chromosome 14), which function as ligand-activated transcription factors.[94] These receptors exhibit distinct tissue distributions: ERα predominates in reproductive tissues such as the uterus, mammary gland, and ovary, as well as in bone and liver, while ERβ is more abundant in the prostate, ovary, lung, brain, and vascular endothelium.[95] A third receptor, G protein-coupled estrogen receptor (GPER, also known as GPR30), is a seven-transmembrane domain protein localized to the plasma membrane and endoplasmic reticulum, mediating rapid non-genomic effects independent of ERα and ERβ.[96] [97] In the classical genomic pathway, estrogen binding induces a conformational change in ERα or ERβ, promoting receptor dimerization, nuclear translocation (if cytosolic), and recruitment of co-activators or co-repressors.[2] The dimer binds directly to estrogen response elements (EREs)—palindromic DNA sequences (AGGTCAnnnTGACCT)—in promoter or enhancer regions of target genes, thereby modulating transcription through chromatin remodeling and RNA polymerase II recruitment.[98] Alternatively, ERs exert ERE-independent genomic effects by tethering to other transcription factors, such as AP-1 (via Fos/Jun) or Sp1, to regulate genes lacking canonical EREs, influencing processes like cell proliferation and differentiation.[2] These actions typically occur over hours to days and underpin long-term physiological responses, including reproductive development and homeostasis.[94] Non-genomic signaling provides rapid estrogen effects (seconds to minutes) via membrane-associated receptors, bypassing direct transcriptional changes.[98] Palmitoylated forms of ERα and ERβ at the plasma membrane activate Src kinase, leading to downstream phosphorylation of MAPK/ERK, PI3K/Akt, and PKC pathways, which modulate ion channels, cytoskeletal dynamics, and cell survival without nuclear translocation.[99] GPER, coupling primarily to Gβγ subunits or Gαi/o proteins, stimulates phospholipase C (PLC), increasing intracellular Ca²⁺ and inositol trisphosphate (IP3), or inhibits adenylyl cyclase to reduce cAMP; it can also engage Gαs for ERK activation via transactivation of EGFR.[100] These pathways often converge with genomic mechanisms, where rapid signaling phosphorylates nuclear ERs or co-regulators to enhance transcriptional output.[98] Tissue-specific isoform ratios, such as higher ERβ in certain neurons, further modulate signaling outcomes, with ERβ often antagonizing ERα-driven proliferation.[95]Genomic versus Non-Genomic Actions
Estrogen exerts its effects through two primary signaling modalities: genomic actions, which involve direct regulation of gene transcription, and non-genomic actions, which trigger rapid cellular responses independent of transcriptional changes.[101] Genomic actions are mediated by nuclear estrogen receptors ERα and ERβ, which, upon binding estrogen, undergo conformational changes, dissociate from heat shock proteins, dimerize, and translocate to the nucleus to bind estrogen response elements (EREs) on DNA or interact with other transcription factors such as AP-1 (FOS/JUN).[101] This process modulates the expression of target genes, including those encoding IGF1, CCND1 (cyclin D1), and matrix metalloproteinases, leading to alterations in protein synthesis and long-term cellular adaptations.[101] These effects typically manifest over hours to days, reflecting the time required for transcription and translation.[102] In contrast, non-genomic actions occur rapidly, within seconds to minutes, primarily through membrane-associated or extranuclear estrogen receptors.[102] These include palmitoylated variants of ERα and ERβ localized at the plasma membrane, as well as the G protein-coupled receptor GPER (also known as GPR30), which activate intracellular signaling cascades without direct nuclear involvement.[101] Key pathways encompass MAPK/ERK, PI3K/Akt, PKA, and PKC activation, often coupled with ion channel modulation (e.g., voltage-gated calcium channels) and second messenger production like cAMP or calcium influx.[102] Examples include rapid enhancement of endothelial nitric oxide synthase (eNOS) activity via striatin-ERα complexes or EGFR transactivation leading to cell proliferation signals.[103] The distinction between these actions lies in their temporal dynamics and molecular endpoints: genomic signaling drives sustained structural and functional changes, such as synaptic plasticity via CREB-mediated transcription of genes like HOXC10, whereas non-genomic signaling elicits acute responses, including spine density increases through CaMKII phosphorylation or immediate neuroprotection against excitotoxicity.[102] Non-genomic effects can occur independently of classical ERs via receptor-independent mechanisms, such as direct interaction with membrane lipids, but often involve splice variants like ERα-36.[101] Crosstalk between genomic and non-genomic pathways amplifies estrogen's physiological impact, with rapid signaling potentiating transcriptional outcomes—for instance, MAPK activation enhancing ER recruitment to promoters or PI3K/Akt upregulating postsynaptic density protein 95 (PSD-95) expression.[103] Conversely, genomic actions can prime non-genomic responsiveness by inducing expression of signaling components like IGF-1R, which boosts MAPK flux.[103] This integration is evident in contexts like synaptic plasticity, where acute estrogen-induced ERK signaling facilitates long-term potentiation (LTP) while supporting BCL-2 transcription for neuroprotection.[102] Such cooperation underscores estrogen's multifaceted role beyond binary classification, though debates persist on the precise contributions of GPER versus canonical ERs in specific tissues.[101]Medical Uses and Controversies
Hormone Replacement Therapy in Menopause
Hormone replacement therapy (HRT), also termed menopausal hormone therapy (MHT), involves administering estrogen, often combined with progestogen in women with an intact uterus, to alleviate symptoms of menopause such as vasomotor symptoms (hot flashes and night sweats) and genitourinary syndrome, while addressing long-term risks like osteoporosis.[104] Estrogen-only therapy suffices for hysterectomized women to avoid endometrial hyperplasia and cancer risks associated with unopposed estrogen.[105] Transdermal or lower-dose oral formulations may reduce certain adverse effects compared to standard oral conjugated equine estrogens used in early trials.[88] Clinical trials and meta-analyses confirm HRT's superior efficacy over alternatives like SSRIs for vasomotor symptom relief, with reductions of 75-90% in moderate-to-severe cases among women under 60 or within 10 years of menopause onset.[104] For bone health, HRT increases lumbar spine bone mineral density by 3.4-3.7% after 1-2 years and reduces hip fracture risk by 30-40% in randomized trials, including the Women's Health Initiative (WHI), where estrogen plus progestin lowered vertebral fractures by 34%.[106][107] Long-term WHI follow-up (up to 20 years) showed persistent fracture protection without excess mortality from osteoporosis.[108] Cardiovascular outcomes depend on initiation timing per the "timing hypothesis," supported by subgroup analyses: early initiation (within 10 years of menopause) slows atherosclerosis progression and may lower coronary heart disease risk by 20-30% with estrogen alone, whereas later use (average age 63 in WHI) raised events like stroke (by 1.3-fold) and venous thromboembolism (by 2-fold) with combined therapy.[109][110] WHI's 2002 halt of combined HRT arms, based on excess breast cancer (8 additional cases per 10,000 women-years) and strokes, led to a 75% drop in U.S. HRT use by 2020, but extended data revealed estrogen-alone reduced breast cancer incidence by 23% at 20-year follow-up, with no overall mortality increase.[107][111] Recent Danish cohort studies link oral estrogen-progestin to higher heart disease and thromboembolism risks, though absolute increases remain small (e.g., 1-2 extra events per 1,000 users annually).[88] Guidelines from the North American Menopause Society (2022) endorse individualized HRT for symptomatic women under 60, weighing benefits against risks like gallbladder disease and slight dementia associations in older starters, while critiquing overgeneralization of WHI to younger cohorts.[104] Empirical critiques highlight that WHI's older participants and synthetic progestins amplified risks not seen with micronized progesterone or bioidentical options, urging focus on absolute rather than relative risks—e.g., 1 fewer hip fracture per 100 users versus 1 extra breast cancer per 1,000.[112][89] Discontinuation post-therapy restores fracture risk to baseline within years, underscoring HRT's preventive rather than curative role.[113]Contraceptives and Fertility Treatments
Combined oral contraceptives (COCs), which typically include synthetic estrogens such as ethinylestradiol at doses of 20-35 micrograms, combined with progestins, prevent pregnancy primarily by suppressing gonadotropin release from the pituitary gland, thereby inhibiting follicular development and ovulation.[114] The estrogen component enhances cycle control and bleeding patterns while contributing to the overall efficacy, with perfect-use failure rates below 1% and typical-use rates around 7-9%.[115] However, COCs elevate the risk of venous thromboembolism (VTE) approximately 2- to 4-fold compared to non-users, with absolute risks rising from about 2 to 10-12 events per 10,000 woman-years, particularly in the first year of use and among those with predisposing factors like obesity or smoking.[114] [116] Other documented risks include modest increases in blood pressure, with systolic elevations of 4-5 mmHg on average, and associations with ischemic stroke and myocardial infarction in susceptible populations.[117] [118] In fertility treatments, exogenous estrogen is administered in hormone replacement therapy (HRT) protocols for frozen embryo transfer (FET) to prepare the endometrium by promoting proliferation and receptivity, typically starting in the early follicular phase at doses of 2-6 mg oral estradiol valerate daily until endometrial thickness reaches 7-10 mm.[119] [120] This suppresses endogenous ovulation and induces progesterone receptors, followed by progesterone supplementation; clinical pregnancy rates in HRT-FET cycles range from 40-50%, comparable to natural cycles in some meta-analyses, though direct comparisons show variable outcomes influenced by patient age and protocol.[121] Oral or vaginal routes are used, with vaginal administration potentially yielding higher serum levels and fewer systemic effects.[120] Prior to assisted reproductive technology (ART) initiation, short courses of COCs containing estrogen are employed to synchronize cycles, reduce ovarian cyst formation, and optimize timing, with evidence indicating no long-term detriment to ovarian response when limited to 2-4 weeks.[122] [123] Elevated estradiol levels during ART monitoring correlate with outcomes, but excessive exogenous exposure in HRT may impact placentation or increase risks like ovarian hyperstimulation syndrome in fresh cycles, though data remain inconclusive.[124]Applications in Gender-Affirming Care
Estrogen, primarily in the form of estradiol, is administered to biological males experiencing gender dysphoria who seek feminization as part of medical transition protocols. Typical regimens involve oral, transdermal, or injectable estradiol at doses of 2-6 mg/day orally or equivalent, often combined with anti-androgens such as spironolactone (100-200 mg/day) or cyproterone acetate to suppress endogenous testosterone production.[125] [126] This therapy aims to induce secondary female characteristics, including breast development (typically Tanner stages 2-4 after 1-2 years), redistribution of adipose tissue to hips and thighs, decreased muscle mass, and softer skin texture.[126] However, full suppression of male skeletal features, such as height or shoulder width, does not occur, as these are established post-puberty.[125] Empirical data on psychosocial outcomes remain limited and of low quality, with systematic reviews indicating inconsistent reductions in depressive symptoms and psychological distress but no robust evidence for improved quality of life or resolution of gender dysphoria.[127] The UK's Cass Review, a comprehensive evaluation of evidence for youth gender services published in 2024, highlighted the paucity of high-quality, long-term randomized controlled trials for hormone interventions, noting that observational studies often suffer from confounding factors like concurrent psychotherapy or selection bias.[128] For adults, a 2023 systematic review found gender-affirming hormone therapy associated with modest decreases in anxiety and depression in short-term follow-ups (up to 12 months), but longer-term data (beyond 2 years) are scarce and fail to demonstrate causal alleviation of underlying dysphoria.[127] Swedish cohort studies tracking post-treatment transgender individuals over decades report persistently elevated suicide rates—19 times higher than age-matched controls—suggesting hormones and surgery do not mitigate mental health risks compared to untreated cohorts.[129] Adverse effects are well-documented, particularly cardiovascular and thrombotic risks. Feminizing estrogen therapy elevates the incidence of venous thromboembolism (2-5 fold increase with oral formulations due to first-pass liver effects), myocardial infarction, and stroke in transgender women relative to cisgender females, with risks amplified by smoking, age over 40, or prothrombotic conditions.[130] [131] [132] Bone mineral density may initially decline due to testosterone suppression but stabilizes or improves with adequate estrogen dosing; however, long-term fractures remain a concern in those with suboptimal adherence.[133] Infertility is near-universal after 6-12 months, as spermatogenesis ceases, and prostate cancer screening challenges persist due to estrogen's potential promotional effects on prostatic tissue.[125] Overall mortality in treated transgender cohorts exceeds general population rates, driven by cardiovascular disease, suicide, and neoplasms, underscoring the need for individualized risk assessment over routine endorsement.[134] [129]Risks, Long-Term Outcomes, and Empirical Critiques
Estrogen therapies, including hormone replacement in postmenopausal women and cross-sex hormone administration, carry documented risks of venous thromboembolism (VTE), with oral formulations conferring a 2- to 3-fold increased incidence compared to non-users, particularly when combined with progestins.[135] [88] In the Women's Health Initiative (WHI) randomized controlled trial, estrogen plus progestin therapy elevated stroke risk by 31% and VTE by 94% over 5.6 years, while estrogen alone increased stroke by 39% and VTE similarly, though breast cancer incidence was lower with unopposed estrogen.[136] These cardiovascular hazards stem from estrogen's prothrombotic effects on coagulation factors and endothelial function, exacerbated by oral routes due to first-pass liver metabolism.[137] Cancer risks vary by regimen: combined estrogen-progestin therapy raises breast cancer incidence by 10-19% with prolonged use, as evidenced by meta-analyses showing duration-dependent excess risk persisting up to 14 years post-cessation, whereas unopposed estrogen heightens endometrial cancer odds through hyperplasia promotion.[138] [139] Long-term WHI follow-up through 18-20 years confirmed sustained breast cancer elevation with combined therapy (hazard ratio 1.28) but suggested protective effects against breast cancer mortality with estrogen alone in adherent subgroups, though overall all-cause mortality remained neutral.[140] [108] In oral contraceptives, estrogen components dose-dependently elevate ischemic stroke and myocardial infarction risks, with third- and fourth-generation progestins amplifying VTE odds 2-4 fold relative to second-generation, per large cohort analyses; these effects compound in smokers or those with hypertension.[141] [142] For cross-sex estrogen therapy in biological males, systematic reviews indicate heightened VTE, myocardial infarction, and ischemic stroke incidences—up to 2-5 fold versus cisgender counterparts—alongside potential osteoporosis from androgen suppression, though bone mineral density data remain inconsistent due to short follow-up durations averaging under 5 years.[143] [144] [133] Empirical critiques highlight methodological flaws in affirming paradigms: the UK's Cass Review (2024) assessed 50+ studies on puberty suppression followed by cross-sex hormones in youth, deeming nearly all low-quality due to absence of randomized controls, high dropout rates, and failure to measure core outcomes like dysphoria resolution or regret, with no robust evidence for cognitive, bone, or fertility benefits outweighing harms like infertility and sexual dysfunction.[145] Observational transgender cohort studies report 2-3 fold overall mortality elevation post-hormone initiation, attributed to cardiovascular and neoplastic causes, yet suffer from confounding by mental health comorbidities and selection bias.[146] Broader hormone therapy literature faces scrutiny for early overemphasis on benefits—pre-WHI assumptions of cardioprotection reversed by trial data—revealing publication biases favoring positive short-term symptom relief over long-term morbidity, with calls for stratified risk modeling by age, timing, and genetics to refine causal inferences.[147] [148]Associated Pathologies
Estrogen Deficiency Syndromes
Estrogen deficiency syndromes encompass conditions characterized by hypoestrogenism, leading to disruptions in multiple organ systems due to estrogen's regulatory roles in bone metabolism, vascular function, thermoregulation, and neurocognition. These syndromes primarily manifest in women through ovarian failure but also occur in men via impaired aromatization of androgens to estrogens, contributing to skeletal fragility and metabolic dysregulation. Key etiologies include natural menopause (typically occurring around age 51), premature ovarian insufficiency (POI, affecting approximately 1% of women under 40), surgical oophorectomy, chemotherapy-induced gonadal toxicity, and hypogonadotropic hypogonadism from hypothalamic-pituitary disorders.[149][150][151] In postmenopausal women, estrogen withdrawal triggers rapid bone resorption, with trabecular bone loss accelerating by 2-3% annually in the first 5 years post-menopause, elevating fracture risk; this is compounded by increased osteoclast activity and reduced osteoblast function absent estrogen's anti-resorptive effects. Vasomotor symptoms, including hot flashes and night sweats, afflict 75-85% of women, stemming from hypothalamic dysregulation and altered norepinephrine-serotonin signaling. Urogenital atrophy, part of the genitourinary syndrome of menopause, causes vaginal dryness, dyspareunia, and recurrent urinary tract infections due to thinning of epithelial layers and diminished glycogen content, persisting lifelong without intervention.[83][152][153] Premature ovarian insufficiency exemplifies early-onset deficiency, mimicking menopausal symptoms such as irregular menses, infertility, and hypoestrogenism, with elevated follicle-stimulating hormone levels exceeding 25 IU/L on two occasions; affected women face heightened risks of osteopenia (prevalent in 20-30% at diagnosis) and cardiovascular disease from prolonged exposure to low estrogen before age 40. In men, estrogen deficiency arises secondary to androgen insufficiency, as aromatase converts testosterone to estradiol; clinical studies link low estradiol levels (<20 pg/mL) to reduced bone mineral density and increased osteoporosis incidence, independent of testosterone concentrations. Metabolic consequences include visceral adiposity and insulin resistance, predisposing to type 2 diabetes, as estrogen modulates glucose homeostasis and lipid profiles via central and peripheral receptors.[154][155][151] Neurological impacts involve accelerated brain aging, with estrogen deprivation linked to hippocampal atrophy, verbal memory deficits, and mood disturbances; longitudinal data indicate a 1.5-2-fold increased dementia risk in untreated postmenopausal women. Cardiovascular pathophysiology features endothelial dysfunction and atherogenic lipid shifts, with estrogen deficiency promoting low-density lipoprotein oxidation and plaque formation, though observational biases in early studies overstated protective effects. These syndromes underscore estrogen's causal role in maintaining tissue integrity, with empirical evidence from ovariectomy models and cohort studies confirming symptom attenuation only upon restoration, albeit with nuanced risk-benefit profiles in therapeutic contexts.[156][157][158]Excess Estrogen and Related Disorders
Excess estrogen, clinically termed hyperestrogenism, occurs when circulating levels of estrogens such as estradiol exceed physiological ranges, often due to increased production via aromatase-mediated conversion of androgens, estrogen-secreting tumors, or impaired metabolism in conditions like liver cirrhosis.[159] This imbalance disrupts estrogen-androgen ratios and progesterone opposition, leading to tissue-specific pathologies rather than a generalized "dominance" syndrome lacking robust empirical validation as a distinct entity.[160] Genetic causes include aromatase excess syndrome (AEXS), an autosomal dominant disorder from gain-of-function mutations in CYP19A1 regulatory regions, resulting in upregulated extraglandular aromatase activity and prepubertal estrogen elevation.[161] Affected individuals exhibit accelerated bone age, short adult stature from premature epiphyseal closure, and metabolic perturbations, with treatment involving aromatase inhibitors like anastrozole to normalize growth trajectories over long-term follow-up.[162] In females, unopposed estrogen exposure—without adequate progesterone to induce endometrial shedding—drives endometrial hyperplasia, characterized by glandular proliferation and stromal expansion, with simple hyperplasia progressing in up to 1% of cases annually if untreated, escalating risks for atypical forms.[160] This condition manifests as abnormal uterine bleeding, often in anovulatory states or postmenopausal hormone therapy without progestins, where biopsy-confirmed hyperplasia rates reached 4.5 per 100 woman-months in early cyclic estrogen studies before progestin co-administration became standard.[163] Other associations include uterine fibroids (leiomyomas), where estrogen stimulates myometrial growth, though causality involves multifactorial pathways beyond isolated excess.[160] Symptoms such as heavy menstrual bleeding, pelvic pain, and infertility predominate, with management prioritizing progesterone therapy or hysterectomy for persistent atypical hyperplasia.[160] In males, hyperestrogenism predominantly causes gynecomastia through estrogen receptor stimulation in breast tissue, altering the estrogen-to-testosterone ratio via enhanced aromatization in adipose tissue or pathologic sources like Sertoli cell tumors, which produce excess estrogen in one-third of cases.[159] Pubertal or adult-onset gynecomastia affects up to 65% of adolescent males transiently but persists pathologically in hyperestrogenic states, presenting as tender subareolar glandular enlargement without underlying malignancy in most instances.[159] AEXS exemplifies this in males, with gynecomastia onset as early as age 2-3 years alongside hypogonadism from suppressed gonadotropins.[161] Erectile dysfunction, reduced libido, and infertility may co-occur due to feedback inhibition on the hypothalamic-pituitary-gonadal axis, with selective estrogen receptor modulators or inhibitors offering symptomatic relief.[159]Links to Cancers and Chronic Diseases
Estrogen exposure, particularly through prolonged endogenous production or exogenous administration via menopausal hormone therapy (MHT), elevates the risk of hormone-sensitive cancers. In breast cancer, estrogens promote proliferation in estrogen receptor-positive tumors, with MHT use associated with excess risk that rises with duration; a 2019 analysis of 58 studies found every MHT type except vaginal estrogens increased breast cancer incidence, with relative risks of 1.2-1.3 for short-term use escalating to over 2 for longer durations.31709-X/fulltext)[164] Unopposed estrogen therapy markedly heightens endometrial cancer risk by stimulating unchecked endometrial hyperplasia, with studies reporting 2-10% incidence of atypical hyperplasia or carcinoma among users, especially thin women without progestin co-administration to induce shedding.[165][166] For ovarian cancer, estrogen-only MHT slightly raises risk, persisting post-discontinuation but diminishing over time, whereas combined estrogen-progestin regimens show neutral or lower associations in some trials.[167] In prostate cancer, estrogens exert dual effects but evidence supports a causative role via paracrine signaling in the prostate microenvironment, genomic alterations, and promotion of prostatic intraepithelial neoplasia; epidemiological data link higher circulating estradiol to increased incidence, while laboratory models demonstrate estrogen-driven tumor growth independent of androgens.[168] Estrogen deficiency syndromes contribute to chronic diseases, foremost osteoporosis, where postmenopausal hypoestrogenism triggers rapid bone loss through enhanced osteoclastogenesis, inflammatory cytokine release (e.g., IL-6, TNF-α), and disrupted remodeling balance, resulting in 2-3% annual trabecular bone loss initially.[169][170] This causal link is substantiated by randomized trials showing estrogen therapy preserves bone mineral density, with women using it for 7+ years exhibiting significantly higher lumbar spine and hip density than non-users.[50] Cardiovascular disease risk escalates post-menopause due to estrogen withdrawal's adverse effects on endothelial function, lipid profiles, and vascular inflammation, with meta-analyses confirming metabolic shifts like insulin resistance and dyslipidemia as mediators.[171] Exogenous estrogens' impact varies: early initiation may confer protection, but oral estrogen-progestin MHT in older women associates with heightened coronary heart disease and venous thromboembolism events in recent cohort data.[88] Estrogen deficiency also implicates Alzheimer's disease pathogenesis in women, amplifying neuroinflammation, amyloid-beta accumulation, and hippocampal glucose hypometabolism; observational and translational studies indicate twofold higher risk post-menopause, with estrogen's neuroprotective signaling via receptors mitigating tau pathology and synaptic loss when present.[172] Timing critically influences outcomes: randomized controlled trials in women over 65 show late MHT elevates dementia risk, contrasting potential benefits from perimenopausal initiation.[173]Environmental Estrogens and Endocrine Disruptors
Sources of Xenoestrogens
Xenoestrogens, synthetic compounds that mimic the structure or function of endogenous estrogens, enter the environment primarily through industrial production, agricultural practices, and consumer products. Common industrial sources include bisphenol A (BPA), a monomer used in polycarbonate plastics and epoxy resins for food containers and can linings, which leaches into food and beverages, particularly when heated.[174] Phthalates, plasticizers added to polyvinyl chloride (PVC) for flexibility in packaging, medical tubing, and flooring, are released via volatilization and degradation, contaminating indoor air and dust.[175] Polychlorinated biphenyls (PCBs) and dioxins, persistent byproducts from manufacturing and incineration, bioaccumulate in sediments and fatty tissues through atmospheric deposition and wastewater.[176] Agricultural pesticides represent another major vector, with atrazine, a widely used herbicide in corn production, detected in groundwater and surface water at concentrations up to 2-10 μg/L in agricultural runoff, exhibiting estrogenic activity via aromatase induction.[177] Organophosphates like endosulfan and legacy persistent organic pollutants such as DDT (banned in the U.S. since 1972 but still present in global trade and residues) persist in soil and food chains, with DDT metabolites like DDE binding estrogen receptors.[178] In livestock, synthetic growth hormones and mycotoxins like zearalenone from Fusarium fungi in contaminated grains act as xenoestrogens, transferring via meat, dairy, and feed, with zearalenone levels in corn reaching 1-5 mg/kg in affected crops.[179] Consumer products contribute through direct dermal and inhalation exposure. Parabens, preservatives in cosmetics, shampoos, and lotions (e.g., methylparaben at 0.1-0.4% concentrations), weakly bind estrogen receptors and are absorbed through skin, with urinary levels in populations correlating to usage.[180] Phthalates in fragrances, nail polishes, and sunscreens (e.g., diethyl phthalate) off-gas or migrate, while nonylphenols from detergents enter wastewater and aquatic systems.[181] Food packaging and processing introduce additional exposure, as BPA and phthalates migrate into fatty foods like dairy and poultry, with dietary intake estimated at 0.1-1.5 μg/kg body weight daily for BPA in adults.[175]- Plastics and packaging: BPA in cans and bottles; phthalates in flexible wraps.[174][182]
- Pesticides and herbicides: Atrazine, DDT metabolites, glyphosate formulations with estrogenic impurities.[177][178]
- Personal care items: Parabens, benzophenone-3 in sunscreens, phthalates in perfumes.[180]
- Household and industrial: Flame retardants (e.g., brominated compounds), solvents, and fuels.[183]
- Water and soil: Runoff from treated wastewater and landfills, with phthalates at 1-10 μg/L in rivers near urban areas.[184]