Recent from talks
Nothing was collected or created yet.
Aspirin
View on Wikipedia
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /əˌsiːtəlˌsælɪˈsɪlɪk/ |
| Trade names | Bayer Aspirin, others |
| Other names |
|
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682878 |
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral, rectal |
| Drug class | Nonsteroidal anti-inflammatory drug (NSAID) |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 80–100%[6] |
| Protein binding | 80–90%[7] |
| Metabolism | Liver (CYP2C19 and possibly CYP3A), some is also hydrolysed to salicylate in the gut wall.[7] |
| Elimination half-life | Dose-dependent; 2–3 h for low doses (100 mg or less), 15–30 h for larger doses.[7] |
| Excretion | Urine (80–100%), sweat, saliva, feces[6] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.059 |
| Chemical and physical data | |
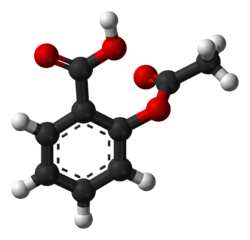
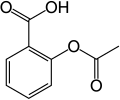
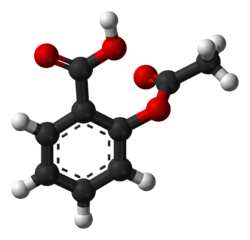
| Formula | C9H8O4 |
| Molar mass | 180.159 g·mol−1 |
| 3D model (JSmol) | |
| Density | 1.40 g/cm3 |
| Melting point | 135 °C (275 °F) [9] |
| Boiling point | 140 °C (284 °F) (decomposes) |
| Solubility in water | 3 g/L |
| |
| |
Aspirin (/ˈæsp(ə)rɪn/[10]) is the genericized trademark for acetylsalicylic acid (ASA), a nonsteroidal anti-inflammatory drug (NSAID) used to reduce pain, fever, and inflammation, and as an antithrombotic.[11] Specific inflammatory conditions that aspirin is used to treat include Kawasaki disease, pericarditis, and rheumatic fever.[11]
Aspirin is also used long-term to help prevent further heart attacks, ischaemic strokes, and blood clots in people at high risk.[11] For pain or fever, effects typically begin within 30 minutes.[11] Aspirin works similarly to other NSAIDs but also suppresses the normal functioning of platelets.[11]
One common adverse effect is an upset stomach.[11] More significant side effects include stomach ulcers, stomach bleeding, and worsening asthma.[11] Bleeding risk is greater among those who are older, drink alcohol, take other NSAIDs, or are on other blood thinners.[11] Aspirin is not recommended in the last part of pregnancy.[11] It is not generally recommended in children with infections because of the risk of Reye syndrome.[11] High doses may result in ringing in the ears.[11]
A precursor to aspirin found in the bark of the willow tree (genus Salix), salicin, is metabolized in the human gut into the medicinally active compound salicylic acid[12] and has been used for its health effects for at least 2,400 years.[13][14] Pharmacology sought a synthetic alternative. In 1853, the chemist Charles Frédéric Gerhardt treated the medicine sodium salicylate with acetyl chloride to produce acetylsalicylic acid for the first time.[15] Over the next 50 years, other chemists, mostly of the German company Bayer, established the chemical structure and devised more efficient production methods.[15]: 69–75 Felix Hoffmann (or perhaps Arthur Eichengrün) of Bayer was the first to produce acetylsalicylic acid in a pure, stable form in 1897.[16] By 1899, Bayer had dubbed this drug Aspirin and was selling it globally.[17]: 27
Aspirin is available without medical prescription as a proprietary or generic medication[11] in most jurisdictions. It is one of the most widely used medications globally, with an estimated 40,000 tonnes (44,000 tons) (50 to 120 billion pills) consumed each year,[13][18] and is on the World Health Organization's List of Essential Medicines.[19] In 2023, it was the 46th most commonly prescribed medication in the United States, with more than 14 million prescriptions.[20][21]
Brand vs. generic name
[edit]In 1897, scientists at the Bayer company began studying acetylsalicylic acid as a less-irritating replacement medication for common salicylate medicines.[15]: 69–75 [22] By 1899, Bayer had named it "Aspirin" and was selling it around the world.[17]
Aspirin's popularity grew over the first half of the 20th century, leading to competition between many brands and formulations.[23] The word Aspirin was Bayer's brand name; however, its rights to the trademark were lost or sold in many countries.[23] The name is ultimately a blend of the prefix a(cetyl) + spir, from Spirsäure, German for meadowsweet, the plant genus from which the aspirin precursor salicylic acid was first isolated (originally Spiraea, now Filipendula) + -in, the common suffix for drugs near the end of the 19th century.[24]
Chemical properties
[edit]Aspirin decomposes rapidly in solutions of ammonium acetate or the acetates, carbonates, citrates, or hydroxides of the alkali metals. It is stable in dry air, but gradually hydrolyses in contact with moisture to acetic and salicylic acids. In a solution with alkalis, the hydrolysis proceeds rapidly and the clear solutions formed may consist entirely of acetate and salicylate.[25]
Like flour mills, factories producing aspirin tablets must control the amount of the powder that becomes airborne inside the building, because the powder-air mixture can be explosive. The National Institute for Occupational Safety and Health (NIOSH) has set a recommended exposure limit in the United States of 5 mg/m3 (time-weighted average).[26] In 1989, the US Occupational Safety and Health Administration (OSHA) set a legal permissible exposure limit for aspirin of 5 mg/m3, but this was vacated by the AFL-CIO v. OSHA decision in 1993.[27]
Synthesis
[edit]The synthesis of aspirin is classified as an esterification reaction. Salicylic acid is treated with acetic anhydride, an acid derivative, causing a chemical reaction that turns salicylic acid's hydroxyl group into an ester group (R-OH → R-OCOCH3). This process yields aspirin and acetic acid, which is considered a byproduct of this reaction. Small amounts of sulfuric acid (and occasionally phosphoric acid) are almost always used as a catalyst. This method is commonly demonstrated in undergraduate teaching labs.[28]

Reaction between acetic acid and salicylic acid can also form aspirin but this esterification reaction is reversible and the presence of water can lead to hydrolysis of the aspirin. So, an anhydrous reagent is preferred.[29]
- Reaction mechanism

Formulations containing high concentrations of aspirin often smell like vinegar[30] because aspirin can decompose through hydrolysis in moist conditions, yielding salicylic and acetic acids.[31]
Physical properties
[edit]Aspirin, an acetyl derivative of salicylic acid, is a white, crystalline, weakly acidic substance that melts at 136 °C (277 °F),[9] and decomposes around 140 °C (284 °F).[32] Its acid dissociation constant (pKa) is 3.5 at 25 °C (77 °F).[33]
Polymorphism
[edit]Polymorphism is the ability of a substance to form more than one crystal structure. Until 2005, there was only one proven polymorph of aspirin (form I), though the existence of another polymorph was debated since the 1960s, and one report from 1981 reported that when crystallized in the presence of aspirin anhydride, the diffractogram of aspirin has weak additional peaks. Though at the time it was dismissed as mere impurity, it was, in retrospect, form II aspirin.[34]
Form II was reported in 2005,[35][36] found after attempted co-crystallization of aspirin and levetiracetam from hot acetonitrile. Pure form II aspirin can be prepared by seeding the batch with aspirin anhydrate in 15% weight.[34]
In form I, pairs of aspirin molecules form centrosymmetric dimers through the acetyl groups with the (acidic) methyl proton to carbonyl hydrogen bonds. In form II, each aspirin molecule forms the same hydrogen bonds, but with two neighbouring molecules instead of one. With respect to the hydrogen bonds formed by the carboxylic acid groups, both polymorphs form identical dimer structures. The aspirin polymorphs contain identical 2-dimensional sections and are therefore more precisely described as polytypes.[37]
Form III was reported in 2015 by compressing Form I above 2 GPa, but it reverts to form I when pressure is removed.[38] Form IV was reported in 2017, which is stable at ambient conditions.[39]
Mechanism of action
[edit]Discovery of the mechanism
[edit]In 1971, the British pharmacologist John Robert Vane, then employed by the Royal College of Surgeons in London, showed that aspirin suppressed the production of prostaglandins and thromboxanes.[40][41] For this discovery, he was awarded the 1982 Nobel Prize in Physiology or Medicine, jointly with Sune Bergström and Bengt Ingemar Samuelsson.[42]
Prostaglandins and thromboxanes
[edit]Aspirin's ability to suppress the production of prostaglandins and thromboxanes is due to its irreversible inactivation of the cyclooxygenase (COX; officially known as prostaglandin-endoperoxide synthase, PTGS) enzyme required for prostaglandin and thromboxane synthesis.[43] Aspirin acts as an acetylating agent where an acetyl group is covalently attached to a serine residue in the active site of the COX enzyme (suicide inhibition).[44] This makes aspirin different from other NSAIDs (such as diclofenac and ibuprofen), which are reversible inhibitors.[44]
Low-dose aspirin use irreversibly blocks the formation of thromboxane A2 in platelets, which inhibits platelet aggregation during the lifetime of the affected platelet (8–9 days). This antithrombotic property makes aspirin useful for reducing the incidence of heart attacks in people who have had a heart attack, unstable angina, ischemic stroke or transient ischemic attack.[45] 40 mg of aspirin a day is able to inhibit a large proportion of maximum thromboxane A2 release provoked acutely, with the prostaglandin I2 synthesis being little affected; however, higher doses of aspirin are required to attain further inhibition.[46]
Prostaglandins, a type of hormone, have diverse effects, including the transmission of pain information to the brain, modulation of the hypothalamic thermostat, and inflammation. Thromboxanes are responsible for the aggregation of platelets that form blood clots. Heart attacks are caused primarily by blood clots, and low doses of aspirin are seen as an effective medical intervention to prevent a second acute myocardial infarction.[47]
COX-1 and COX-2 inhibition
[edit]At least two different types of cyclooxygenases, COX-1 and COX-2, are acted on by aspirin. Aspirin irreversibly inhibits COX-1 and modifies the enzymatic activity of COX-2. COX-2 normally produces prostanoids, most of which are proinflammatory. Aspirin-modified COX-2 (aka prostaglandin-endoperoxide synthase 2 or PTGS2) produces epi-lipoxins, most of which are anti-inflammatory.[48] Newer NSAID drugs, COX-2 inhibitors (coxibs), have been developed to inhibit only COX-2, with the intent to reduce the incidence of gastrointestinal side effects.[18]
Several COX-2 inhibitors, such as rofecoxib (Vioxx), have been withdrawn from the market, after evidence emerged that COX-2 inhibitors increase the risk of heart attack and stroke.[49][50] Endothelial cells lining the microvasculature in the body are proposed to express COX-2, and, by selectively inhibiting COX-2, prostaglandin production (specifically, PGI2; prostacyclin) is downregulated with respect to thromboxane levels, as COX-1 in platelets is unaffected. Thus, the protective anticoagulative effect of PGI2 is removed, increasing the risk of thrombus and associated heart attacks and other circulatory problems.[51]
Furthermore, aspirin, while inhibiting the ability of COX-2 to form pro-inflammatory products such as the prostaglandins, converts this enzyme's activity from a prostaglandin-forming cyclooxygenase to a lipoxygenase-like enzyme: aspirin-treated COX-2 metabolizes a variety of polyunsaturated fatty acids to hydroperoxy products which are then further metabolized to specialized proresolving mediators such as the aspirin-triggered lipoxins(15-epilipoxin-A4/B4), aspirin-triggered resolvins, and aspirin-triggered maresins. These mediators possess potent anti-inflammatory activity. It is proposed that this aspirin-triggered transition of COX-2 from cyclooxygenase to lipoxygenase activity and the consequential formation of specialized proresolving mediators contributes to the anti-inflammatory effects of aspirin.[52][53][54]
Additional mechanisms
[edit]Aspirin has been shown to have at least three additional modes of action. It uncouples oxidative phosphorylation in cartilaginous (and hepatic) mitochondria, by diffusing from the inner membrane space as a proton carrier back into the mitochondrial matrix, where it ionizes once again to release protons.[55] Aspirin buffers and transports the protons. When high doses are given, it may actually cause fever, owing to the heat released from the electron transport chain, as opposed to the antipyretic action of aspirin seen with lower doses. In addition, aspirin induces the formation of NO-radicals in the body, which have been shown in mice to have an independent mechanism of reducing inflammation. This reduced leukocyte adhesion is an important step in the immune response to infection; however, evidence is insufficient to show that aspirin helps to fight infection.[56] More recent data also suggest salicylic acid and its derivatives modulate signalling through NF-κB.[57] NF-κB, a transcription factor complex, plays a central role in many biological processes, including inflammation.[58][59][60]
Aspirin is readily broken down in the body to salicylic acid, which itself has anti-inflammatory, antipyretic, and analgesic effects. In 2012, salicylic acid was found to activate AMP-activated protein kinase, which has been suggested as a possible explanation for some of the effects of both salicylic acid and aspirin.[61][62] The acetyl portion of the aspirin molecule has its own targets. Acetylation of cellular proteins is a well-established phenomenon in the regulation of protein function at the post-translational level. Aspirin is able to acetylate several other targets in addition to COX isoenzymes.[63][64] These acetylation reactions may explain many hitherto unexplained effects of aspirin.[65]
Formulations
[edit]Aspirin is available in a variety of pharmaceutical formulations, each with distinct pharmacological and safety profiles.[66][67][68] A key concern in aspirin therapy is the risk of gastrointestinal bleeding, prompting the development of formulations aimed at maintaining efficacy while minimizing gastrointestinal harm.[69][70][68] Some formulations are also combined, for example, buffered aspirin with vitamin C. Formulation examples include:
- Immediate-release tablets (IR-ASA): Commonly contain 75–100 mg or 300–320 mg of aspirin and are rapidly absorbed in the stomach.[66][68]
- Enteric-coated tablets (EC-ASA): Designed to dissolve in the higher pH environment of the small intestine, reducing gastric irritation but sometimes leading to erratic absorption.[66][71]
- Buffered formulations: Contain aspirin with buffering agents to reduce GI irritation; studies show similar mucosal injury rates to plain aspirin.[66]
- Aspirin combined with vitamin C (ASA-VitC): Reduces gastric damage and blood loss compared to plain aspirin.[72]
- Effervescent tablets are a specialized oral dosage form containing aspirin and an effervescent base—typically a combination of citric acid, tartaric acid, and sodium bicarbonate. When dissolved in water, these tablets produce a fizzy reaction that rapidly disperses the drug throughout the solution.[73][74]
- Phospholipid-aspirin complex liquid formulation (PL-ASA): Novel, FDA-approved and under further investigation for its ability to reduce GI injury while maintaining reliable platelet inhibition.[71]
Aspirin formulations differ significantly in terms of pharmacokinetics, efficacy, and gastrointestinal safety. Enteric-coated (EC) aspirin, developed to reduce gastric irritation by delaying release until the small intestine, exhibits erratic absorption and reduced bioavailability, particularly in individuals with body weight over 70 kg. This can lead to suboptimal thromboxane A2 inhibition and decreased antiplatelet efficacy compared to plain aspirin.[66] This diminished pharmacodynamic effect has been associated with reduced cardiovascular protection in heavier individuals.[66] Although EC aspirin is associated with fewer gastric erosions in endoscopic studies, it does not significantly reduce gastrointestinal bleeding or ulceration,[66] and may increase the risk of small bowel mucosal injury due to local topical effects[75][69][76]
Buffered aspirin, which includes agents to neutralize gastric acid, similarly offers no clear safety advantage over plain aspirin.[66]
Novel formulations such as the phospholipid-aspirin complex (PL-ASA) attempt to overcome these limitations by pre-associating aspirin with lipid excipients. PL-ASA has been shown to reduce acute gastric injury while providing predictable absorption and bioequivalence to plain aspirin, with no significant food effect.[68] This formulation achieves consistent platelet inhibition with reduced interindividual variability in pharmacodynamic response compared to EC aspirin.[68]
For long-term prevention, a network meta-analysis suggests that a daily dose of 100 mg of coated aspirin may provide optimal protection against all-cause mortality and cancer, while higher doses are more effective in reducing cardiovascular events and lower doses may be better tolerated.[77] Nonetheless, plain aspirin remains the preferred formulation for cardiovascular prevention due to its superior and consistent pharmacokinetic properties.[66]
Pharmacokinetics
[edit]Acetylsalicylic acid is a weak acid, and very little of it is ionized in the stomach after oral administration. Acetylsalicylic acid is quickly absorbed through the cell membrane in the acidic conditions of the stomach. The higher pH and larger surface area of the small intestine cause aspirin to be absorbed more slowly there, as more of it is ionized. Owing to the formation of concretions, aspirin is absorbed much more slowly during overdose, and blood plasma concentrations can continue to rise for up to 24 hours after ingestion.[78][79][80]
About 50–80% of salicylate in the blood is bound to human serum albumin, while the rest remains in the active, ionized state; protein binding is concentration-dependent. Saturation of binding sites leads to more free salicylate and increased toxicity. The volume of distribution is 0.1–0.2 L/kg. Acidosis increases the volume of distribution because of enhancement of tissue penetration of salicylates.[80]
As much as 80% of therapeutic doses of salicylic acid is metabolized in the liver. Conjugation with glycine forms salicyluric acid, and with glucuronic acid to form two different glucuronide esters. The conjugate with the acetyl group intact is referred to as the acyl glucuronide; the deacetylated conjugate is the phenolic glucuronide. These metabolic pathways have only a limited capacity. Small amounts of salicylic acid are also hydroxylated to gentisic acid. With large salicylate doses, the kinetics switch from first-order to zero-order, as metabolic pathways become saturated and renal excretion becomes increasingly important.[80]
Salicylates are excreted mainly by the kidneys as salicyluric acid (75%), free salicylic acid (10%), salicylic phenol (10%), acyl glucuronides (5%), gentisic acid (< 1%), and 2,3-dihydroxybenzoic acid.[81] When small doses (less than 250 mg in an adult) are ingested, all pathways proceed by first-order kinetics, with an elimination half-life of about 2.0 h to 4.5 h.[82][83] When higher doses of salicylate are ingested (more than 4 g), the half-life becomes much longer (15 h to 30 h),[84] because the biotransformation pathways concerned with the formation of salicyluric acid and salicyl phenolic glucuronide become saturated.[85] Renal excretion of salicylic acid becomes increasingly important as the metabolic pathways become saturated, because it is extremely sensitive to changes in urinary pH. A 10- to 20-fold increase in renal clearance occurs when urine pH is increased from 5 to 8. The use of urinary alkalinization exploits this particular aspect of salicylate elimination.[86] It was found that short-term aspirin use in therapeutic doses might precipitate reversible acute kidney injury when the patient was ill with glomerulonephritis or cirrhosis.[87] Aspirin for some patients with chronic kidney disease and some children with congestive heart failure was contraindicated.[87]
History
[edit]
Medicines made from willow and other salicylate-rich plants appear in clay tablets from ancient Sumer as well as the Ebers Papyrus from ancient Egypt.[15]: 8–13 [23][24] Hippocrates referred to the use of salicylic tea to reduce fevers around 400 BC, and willow bark preparations were part of the pharmacopoeia of Western medicine in classical antiquity and the Middle Ages.[23] Willow bark extract became recognized for its specific effects on fever, pain, and inflammation in the mid-eighteenth century[88] after the Rev Edward Stone of Chipping Norton, Oxfordshire, noticed that the bitter taste of willow bark resembled the taste of the bark of the cinchona tree, known as "Peruvian bark", which was used successfully in Peru to treat a variety of ailments. Stone experimented with preparations of powdered willow bark on people in Chipping Norton for five years and found it to be as effective as Peruvian bark and a cheaper domestic version. In 1763, he sent a report of his findings to the Royal Society in London.[89] By the nineteenth century, pharmacists were experimenting with and prescribing a variety of chemicals related to salicylic acid, the active component of willow extract.[15]: 46–55

In 1853, the chemist Charles Frédéric Gerhardt treated sodium salicylate with acetyl chloride to produce acetylsalicylic acid for the first time;[15]: 46–48 in the second half of the 19th century, other academic chemists established the compound's chemical structure and devised more efficient methods of synthesis. In 1897, scientists at the drug and dye firm Bayer began investigating acetylsalicylic acid as a less-irritating replacement for standard common salicylate medicines, and identified a new way to synthesize it.[15]: 69–75 That year, Felix Hoffmann (or Arthur Eichengrün) of Bayer was the first to produce acetylsalicylic acid in a pure, stable form.[16][24]
Salicylic acid had been extracted in 1839 from the herb meadowsweet, whose German name, Spirsäure, was the basis for naming the newly synthesized drug, which, by 1899, Bayer was selling globally.[15]: 46–55 [17]: 27 The word Aspirin was Bayer's brand name, rather than the generic name of the drug; however, Bayer's rights to the trademark were lost or sold in many countries. Aspirin's popularity grew over the first half of the 20th century, leading to fierce competition with the proliferation of aspirin brands and products.[23]
Aspirin's popularity declined after the development of acetaminophen/paracetamol in 1956 and ibuprofen in 1962. In the 1960s and 1970s, John Vane and others discovered the basic mechanism of aspirin's effects,[15]: 226–231 while clinical trials and other studies from the 1960s to the 1980s established aspirin's efficacy as an anti-clotting agent that reduces the risk of clotting diseases.[15]: 247–257 The initial large studies on the use of low-dose aspirin to prevent heart attacks that were published in the 1970s and 1980s helped spur reform in clinical research ethics and guidelines for human subject research and US federal law, and are often cited as examples of clinical trials that included only men, but from which people drew general conclusions that did not hold true for women.[90][91][92]
Aspirin sales revived considerably in the last decades of the 20th century, and remain strong in the 21st century with widespread use as a preventive treatment for heart attacks and strokes.[15]: 267–269
Trademark
[edit]Bayer lost its trademark for aspirin in the United States and some other countries in actions taken between 1918 and 1921, because it had failed to use the name for its own product correctly and had for years allowed the use of "Aspirin" by other manufacturers without defending the intellectual property rights.[93] Aspirin is a generic trademark in many countries.[94][95] Aspirin, with a capital "A", remains a registered trademark of Bayer in Germany, Canada, Mexico, and in over 80 other countries, for acetylsalicylic acid in all markets, but using different packaging and physical aspects for each.[96][97]
Compendial status
[edit]Medical use
[edit]Aspirin is used in the treatment of a number of conditions, including fever, pain, rheumatic fever, and inflammatory conditions, such as rheumatoid arthritis, pericarditis, and Kawasaki disease.[11] Lower doses of aspirin have also been shown to reduce the risk of death from a heart attack, or the risk of stroke in people who are at high risk or who have cardiovascular disease, but not in elderly people who are otherwise healthy.[100][101][102][103][104] There is evidence that aspirin is effective at preventing colorectal cancer, though the mechanisms of this effect are unclear.[105] There is also evidence that aspirin can treat 80% of ED cases.[106]
Pain
[edit]Aspirin is an effective analgesic for acute pain, although it is generally considered inferior to ibuprofen because aspirin is more likely to cause gastrointestinal bleeding.[107] Aspirin is generally ineffective for those pains caused by muscle cramps, bloating, gastric distension, or acute skin irritation.[108] As with other NSAIDs, combinations of aspirin and caffeine provide slightly greater pain relief than aspirin alone.[109] Effervescent formulations of aspirin relieve pain faster than aspirin in tablets,[110] which makes them useful for the treatment of migraines.[111] Topical aspirin may be effective for treating some types of neuropathic pain.[112]
Aspirin, either by itself or in a combined formulation, effectively treats certain types of a headache, but its efficacy may be questionable for others. Secondary headaches, meaning those caused by another disorder or trauma, should be promptly treated by a medical provider. Among primary headaches, the International Classification of Headache Disorders distinguishes between tension headache (the most common), migraine, and cluster headache. Aspirin or other over-the-counter analgesics are widely recognized as effective for the treatment of tension headaches.[113] Aspirin, especially as a component of an aspirin/paracetamol/caffeine combination, is considered a first-line therapy in the treatment of migraine, and comparable to lower doses of sumatriptan. It is most effective at stopping migraines when they are first beginning.[114]
Fever
[edit]Like its ability to control pain, aspirin's ability to control fever is due to its action on the prostaglandin system through its irreversible inhibition of COX.[115] Although aspirin's use as an antipyretic in adults is well established, many medical societies and regulatory agencies, including the American Academy of Family Physicians, the American Academy of Pediatrics, and the Food and Drug Administration, strongly advise against using aspirin for the treatment of fever in children because of the risk of Reye syndrome, a rare but often fatal illness associated with the use of aspirin or other salicylates in children during episodes of viral or bacterial infection.[116][117][118] Because of the risk of Reye syndrome in children, in 1986, the US Food and Drug Administration (FDA) required prescribing information on all aspirin-containing medications advising against its use in children and teenagers.[119][120]
Inflammation
[edit]Aspirin is used as an anti-inflammatory agent for both acute and long-term inflammation,[121] as well as for the treatment of inflammatory diseases, such as rheumatoid arthritis.[11]
Heart attacks and strokes
[edit]Aspirin is an important part of the treatment of those who have had a heart attack.[122] It is generally not recommended for routine use by people with no other health problems, including those over the age of 70.[123]
The 2009 Antithrombotic Trialists' Collaboration published in Lancet evaluated the efficacy and safety of low dose aspirin in secondary prevention.[124] In those with prior ischaemic stroke or acute myocardial infarction, daily low dose aspirin was associated with a 19% relative risk reduction of serious cardiovascular events (non-fatal myocardial infarction, non-fatal stroke, or vascular death). This did come at the expense of a 0.19% absolute risk increase in gastrointestinal bleeding; however, the benefits outweigh the hazard risk in this case.[124] Data from previous trials have suggested that weight-based dosing of aspirin has greater benefits in primary prevention of cardiovascular outcomes.[125] However, more recent trials were not able to replicate similar outcomes using low dose aspirin in low body weight (<70 kg) in specific subset of population studied i.e. elderly and diabetic population, and more evidence is required to study the effect of high dose aspirin in high body weight (≥70 kg).[126][127][128]
After percutaneous coronary interventions (PCIs), such as the placement of a coronary artery stent, a U.S. Agency for Healthcare Research and Quality guideline recommends that aspirin be taken indefinitely.[129] Frequently, aspirin is combined with an ADP receptor inhibitor, such as clopidogrel, prasugrel, or ticagrelor to prevent blood clots. This is called dual antiplatelet therapy (DAPT). Duration of DAPT was advised in the United States and European Union guidelines after the CURE[130] and PRODIGY[131] studies. In 2020, the systematic review and network meta-analysis from Khan et al.[132] showed promising benefits of short-term (< 6 months) DAPT followed by P2Y12 inhibitors in selected patients, as well as the benefits of extended-term (> 12 months) DAPT in high risk patients. In conclusion, the optimal duration of DAPT after PCIs should be personalized after outweighing each patient's risks of ischemic events and risks of bleeding events with consideration of multiple patient-related and procedure-related factors. Moreover, aspirin should be continued indefinitely after DAPT is complete.[133][134][135]
The status of the use of aspirin for the primary prevention in cardiovascular disease is conflicting and inconsistent, with recent changes from previously recommending it widely decades ago, and that some referenced newer trials in clinical guidelines show less of benefit of adding aspirin alongside other anti-hypertensive and cholesterol lowering therapies.[123][136] The ASCEND study demonstrated that in high-bleeding risk diabetics with no prior cardiovascular disease, there is no overall clinical benefit (12% decrease in risk of ischaemic events v/s 29% increase in GI bleeding) of low dose aspirin in preventing the serious vascular events over a period of 7.4 years. Similarly, the results of the ARRIVE study also showed no benefit of same dose of aspirin in reducing the time to first cardiovascular outcome in patients with moderate risk of cardiovascular disease over a period of five years. Aspirin has also been suggested as a component of a polypill for prevention of cardiovascular disease.[137][138] Complicating the use of aspirin for prevention is the phenomenon of aspirin resistance.[139][140] For people who are resistant, aspirin's efficacy is reduced.[141] Some authors have suggested testing regimens to identify people who are resistant to aspirin.[142]
As of April 2022[update], the United States Preventive Services Task Force (USPSTF) determined that there was a "small net benefit" for patients aged 40–59 with a 10% or greater 10-year cardiovascular disease (CVD) risk, and "no net benefit" for patients aged over 60.[143][144][145] Determining the net benefit was based on balancing the risk reduction of taking aspirin for heart attacks and ischaemic strokes, with the increased risk of gastrointestinal bleeding, intracranial bleeding, and hemorrhagic strokes. Their recommendations state that age changes the risk of the medicine, with the magnitude of the benefit of aspirin coming from starting at a younger age, while the risk of bleeding, while small, increases with age, particular for adults over 60, and can be compounded by other risk factors such as diabetes and a history of gastrointestinal bleeding. As a result, the USPSTF suggests that "people ages 40 to 59 who are at higher risk for CVD should decide with their clinician whether to start taking aspirin; people 60 or older should not start taking aspirin to prevent a first heart attack or stroke." Primary prevention guidelines from September 2019[update] made by the American College of Cardiology and the American Heart Association state they might consider aspirin for patients aged 40–69 with a higher risk of atherosclerotic CVD, without an increased bleeding risk, while stating they would not recommend aspirin for patients aged over 70 or adults of any age with an increased bleeding risk.[123] They state a CVD risk estimation and a risk discussion should be done before starting on aspirin, while stating aspirin should be used "infrequently in the routine primary prevention of (atherosclerotic CVD) because of lack of net benefit". As of August 2021[update], the European Society of Cardiology made similar recommendations; considering aspirin specifically to patients aged less than 70 at high or very high CVD risk, without any clear contraindications, on a case-by-case basis considering both ischemic risk and bleeding risk.[136]
Cancer prevention
[edit]Aspirin use may reduce the overall risk of both getting cancer and dying from cancer.[105][146][147][148] There is substantial evidence for lowering the risk of colorectal cancer (CRC),[149][150] but aspirin must be taken for at least 10–20 years to see this benefit.[151] It may also slightly reduce the risk of endometrial cancer[152] and prostate cancer.[153]
Some conclude the benefits are greater than the risks due to bleeding in those at average risk.[146] Others are unclear if the benefits are greater than the risk.[154][155] Given this uncertainty, the 2007 United States Preventive Services Task Force (USPSTF) guidelines on this topic recommended against the use of aspirin for prevention of CRC in people with average risk.[156] Nine years later however, the USPSTF issued a grade B recommendation for the use of low-dose aspirin (75 to 100 mg/day) "for the primary prevention of CVD [cardiovascular disease] and CRC in adults 50 to 59 years of age who have a 10% or greater 10-year CVD risk, are not at increased risk for bleeding, have a life expectancy of at least 10 years, and are willing to take low-dose aspirin daily for at least 10 years".[157]
A meta-analysis through 2019 said that there was an association between taking aspirin and lower risk of cancer of the colorectum, esophagus, and stomach.[158]
In 2021, the United States Preventive Services Task Force raised questions about the use of aspirin in cancer prevention. It notes the results of the 2018 ASPREE (Aspirin in Reducing Events in the Elderly) Trial, in which the risk of cancer-related death was higher in the aspirin-treated group than in the placebo group.[159]
In 2025, a group of scientists at the University of Cambridge found that aspirin stimulates the immune system to reduce cancer metastasis. They found that a protein called ARHGEF1 suppresses T cells, that are required for attacking metastatic cancer cells. Aspirin appeared to counteract this suppression by targeting a clotting factor called thromboxane A2 (TXA2), which activates ARHGEF1, thus preventing it from suppressing the T cells.[160] The researchers called the discovery a "Eureka moment".[161] It was reported that the findings could lead to a more targeted use for aspirin in cancer research.[162] It was also said that self-medicating with aspirin should not be done yet due to its potential side effects until clinical trials were held.[163]
Psychiatry
[edit]Aspirin, along with several other agents with anti-inflammatory properties, has been repurposed as an add-on treatment for depressive episodes in subjects with bipolar disorder in light of the possible role of inflammation in the pathogenesis of severe mental disorders.[164] A 2022 systematic review concluded that aspirin exposure reduced the risk of depression in a pooled cohort of three studies (HR 0.624, 95% CI: 0.0503, 1.198, P=0.033). However, further high-quality, longer-duration, double-blind randomized controlled trials (RCTs) are needed to determine whether aspirin is an effective add-on treatment for bipolar depression.[165][166][167] Thus, notwithstanding the biological rationale, the clinical perspectives of aspirin and anti-inflammatory agents in the treatment of bipolar depression remain uncertain.[164]
Although cohort and longitudinal studies have shown low-dose aspirin has a greater likelihood of reducing the incidence of dementia, numerous randomized controlled trials have not validated this.[168][169] Some researchers have speculated the anti-inflammatory effects of aspirin may be beneficial for schizophrenia. Small trials have been conducted but evidence remains lacking.[170][171]
Other uses
[edit]Aspirin is a first-line treatment for the fever and joint-pain symptoms of acute rheumatic fever. The therapy often lasts for one to two weeks, and is rarely indicated for longer periods. After fever and pain have subsided, the aspirin is no longer necessary, since it does not decrease the incidence of heart complications and residual rheumatic heart disease.[172][173] Naproxen has been shown to be as effective as aspirin and less toxic, but due to the limited clinical experience, naproxen is recommended only as a second-line treatment.[172][174]
Along with rheumatic fever, Kawasaki disease remains one of the few indications for aspirin use in children[175] in spite of a lack of high quality evidence for its effectiveness.[176] Low-dose aspirin supplementation has moderate benefits when used for prevention of pre-eclampsia.[177][178] This benefit is greater when started in early pregnancy.[179] Aspirin has also demonstrated anti-tumoral effects, via inhibition of the PTTG1 gene, which is often overexpressed in tumors.[180]
Resistance
[edit]For some people, aspirin does not have as strong an effect on platelets as for others, an effect known as aspirin-resistance or insensitivity. One study has suggested women are more likely to be resistant than men,[181] and a different, aggregate study of 2,930 people found 28% were resistant.[182] A study in 100 Italian people found, of the apparent 31% aspirin-resistant subjects, only 5% were truly resistant, and the others were noncompliant.[183] Another study of 400 healthy volunteers found no subjects who were truly resistant, but some had "pseudoresistance, reflecting delayed and reduced drug absorption". [184]
Meta-analysis and systematic reviews have concluded that laboratory confirmed aspirin resistance confers increased rates of poorer outcomes in cardiovascular and neurovascular diseases.[185][182][186][187][188][189] Although the majority of research conducted has surrounded cardiovascular and neurovascular, there is emerging research into the risk of aspirin resistance after orthopaedic surgery where aspirin is used for venous thromboembolism prophylaxis.[190] Aspirin resistance in orthopaedic surgery, specifically after total hip and knee arthroplasties, is of interest as risk factors for aspirin resistance are also risk factors for venous thromboembolisms and osteoarthritis; the sequelae of requiring a total hip or knee arthroplasty. Some of these risk factors include obesity, advancing age, diabetes mellitus, dyslipidemia and inflammatory diseases.[190]
Dosages
[edit]Adult aspirin tablets are produced in standardised sizes, which vary slightly from country to country, for example 300 mg in Britain and 325 mg in the United States. Smaller doses are based on these standards, e.g., 75 mg and 81 mg tablets. The 81 mg tablets are commonly called "baby aspirin" or "baby-strength", because they were originally – but no longer – intended to be administered to infants and children.[191] No medical significance occurs due to the slight difference in dosage between the 75 mg and the 81 mg tablets. The dose required for benefit appears to depend on a person's weight.[125] For those weighing less than 70 kilograms (154 lb), low dose is effective for preventing cardiovascular disease; for patients above this weight, higher doses are required.[125]
In general, for adults, doses are taken four times a day for fever or arthritis,[192] with doses near the maximal daily dose used historically for the treatment of rheumatic fever.[193] For the prevention of myocardial infarction (MI) in someone with documented or suspected coronary artery disease, much lower doses are taken once daily.[192]
April 2022 recommendations from the United States Preventive Services Task Force (USPSTF) states that for adults aged 40 to 59 years with a 10% or greater 10-year risk of cardiovascular disease (CVD), the decision to initiate low-dose aspirin for primary prevention should be individualized, as the net benefit is small and must be balanced against bleeding risk.[144] For adults aged 60 years or older, the USPSTF recommends against starting low-dose aspirin for primary prevention of CVD, as potential harms outweigh the benefits. These recommendations apply to adults without established CVD or increased bleeding risk, and emphasize shared decision-making between patients and clinicians.[144] Compared to the 2009 update,[194] the 2022 update narrows the eligible population, raises the threshold for benefit, and places greater importance on bleeding risks, especially in older adults.[195][196]
The WHI study of postmenopausal women found that aspirin resulted in a 25% lower risk of death from cardiovascular disease and a 14% lower risk of death from any cause, though there was no significant difference between 81 mg and 325 mg aspirin doses.[197] The 2021 ADAPTABLE study also showed no significant difference in cardiovascular events or major bleeding between 81 mg and 325 mg doses of aspirin in patients (both men and women) with established cardiovascular disease.[198]
Low-dose aspirin use was also associated with a trend toward lower risk of cardiovascular events, and lower aspirin doses (75 or 81 mg/day) may optimize efficacy and safety for people requiring aspirin for long-term prevention.[199]
In children with Kawasaki disease, aspirin is taken at dosages based on body weight, initially four times a day for up to two weeks and then at a lower dose once daily for a further six to eight weeks.[200]
Adverse effects
[edit]
In October 2020, the US Food and Drug Administration (FDA) required the prescribing information to be updated for all nonsteroidal anti-inflammatory medications to describe the risk of kidney problems in unborn babies that result in low amniotic fluid.[201][202] They recommend avoiding NSAIDs in pregnant women at 20 weeks or later in pregnancy.[201][202] One exception to the recommendation is the use of low-dose 81 mg aspirin at any point in pregnancy under the direction of a health care professional.[202]
Contraindications
[edit]Aspirin should not be taken by people who are allergic to ibuprofen or naproxen,[203] or who have salicylate intolerance[204][205] or a more generalized drug intolerance to NSAIDs, and caution should be exercised in those with asthma or NSAID-precipitated bronchospasm. Owing to its effect on the stomach lining, manufacturers recommend people with peptic ulcers, mild diabetes, or gastritis seek medical advice before using aspirin.[203][206] Even if none of these conditions is present, the risk of stomach bleeding is still increased when aspirin is taken with alcohol or warfarin.[203] People with hemophilia or other bleeding tendencies should not take aspirin or other salicylates.[203][206] Aspirin is known to cause hemolytic anemia in people who have the genetic disease glucose-6-phosphate dehydrogenase deficiency, particularly in large doses and depending on the severity of the disease.[207] Use of aspirin during dengue fever is not recommended owing to increased bleeding tendency.[208] Aspirin taken at doses of ≤325 mg and ≤100 mg per day for ≥2 days can increase the odds of suffering a gout attack by 81% and 91% respectively. This effect may potentially be worsened by high purine diets, diuretics, and kidney disease, but is eliminated by the urate lowering drug allopurinol.[209] Daily low dose aspirin does not appear to worsen kidney function.[210] Aspirin may reduce cardiovascular risk in those without established cardiovascular disease in people with moderate CKD, without significantly increasing the risk of bleeding.[211] Aspirin should not be given to children or adolescents under the age of 16 to control cold or influenza symptoms, as this has been linked with Reye syndrome.[212]
Gastrointestinal
[edit]Aspirin increases the risk of upper gastrointestinal bleeding.[213] Enteric coating on aspirin may be used in manufacturing to prevent release of aspirin into the stomach to reduce gastric harm, but enteric coating does not reduce gastrointestinal bleeding risk.[213][214] Enteric-coated aspirin may not be as effective at reducing blood clot risk.[215][216] Combining aspirin with other NSAIDs has been shown to further increase the risk of gastrointestinal bleeding.[213] Using aspirin in combination with clopidogrel or warfarin also increases the risk of upper gastrointestinal bleeding.[217]
The blockade of COX-1 by aspirin apparently results in the upregulation of COX-2 as part of a gastric defense.[218] There is no clear evidence that simultaneous use of a COX-2 inhibitor with aspirin may increase the risk of gastrointestinal injury.[219]
"Buffering" is an additional method used with the intent to mitigate gastrointestinal bleeding, such as by preventing aspirin from concentrating in the walls of the stomach, although the benefits of buffered aspirin are disputed.[66] Almost any buffering agent used in antacids can be used; Bufferin, for example, uses magnesium oxide. Other preparations use calcium carbonate.[220] Gas-forming agents in effervescent tablet and powder formulations can also double as a buffering agent, one example being sodium bicarbonate, used in Alka-Seltzer.[221]
Taking vitamin C with aspirin has been investigated as a method of protecting the stomach lining. In trials, vitamin C-releasing aspirin (ASA-VitC) or a buffered aspirin formulation containing vitamin C was found to cause less stomach damage than aspirin alone.[222][223]
Retinal vein occlusion
[edit]It is a widespread habit among eye specialists (ophthalmologists) to prescribe aspirin as an add-on medication for patients with retinal vein occlusion (RVO), such as central retinal vein occlusion (CRVO) and branch retinal vein occlusion (BRVO).[224] The reason of this widespread use is the evidence of its proven effectiveness in major systemic venous thrombotic disorders, and it has been assumed that may be similarly beneficial in various types of retinal vein occlusion.[225]
However, a large-scale investigation based on data of nearly 700 patients showed "that aspirin or other antiplatelet aggregating agents or anticoagulants adversely influence the visual outcome in patients with CRVO and hemi-CRVO, without any evidence of protective or beneficial effect".[226] Several expert groups, including the Royal College of Ophthalmologists, recommended against the use of antithrombotic drugs (incl. aspirin) for patients with RVO.[227]
Central effects
[edit]Large doses of salicylate, a metabolite of aspirin, cause temporary tinnitus (ringing in the ears) based on experiments in rats, as the action on arachidonic acid and NMDA receptors cascade.[228]
Reye syndrome
[edit]Reye syndrome, a rare but severe illness characterized by acute encephalopathy and fatty liver, can occur when children or adolescents are given aspirin for a fever or other illness or infection. From 1981 to 1997, 1207 cases of Reye syndrome in people younger than 18 were reported to the US Centers for Disease Control and Prevention (CDC). Of these, 93% reported being ill in the three weeks preceding the onset of Reye syndrome, most commonly with a respiratory infection, chickenpox, or diarrhea. Salicylates were detectable in 81.9% of children for whom test results were reported.[229] After the association between Reye syndrome and aspirin was reported, and safety measures to prevent it (including a Surgeon General's warning, and changes to the prescribing information of aspirin-containing drugs) were implemented, aspirin taken by children declined considerably in the United States, as did the number of reported cases of Reye syndrome; a similar decline was found in the United Kingdom after warnings against pediatric aspirin use were issued.[229] The US Food and Drug Administration recommends aspirin (or aspirin-containing products) should not be given to anyone under the age of 12 who has a fever,[212] and the UK National Health Service recommends children who are under 16 years of age should not be given aspirin, except on the advice of a doctor.[230]
Skin
[edit]For a small number of people, taking aspirin can result in symptoms including hives, swelling, and headache.[231] Aspirin can exacerbate symptoms among those with chronic hives, or create acute symptoms of hives.[232] These responses can be due to allergic reactions to aspirin, or more often due to its effect of inhibiting the COX-1 enzyme.[232][233] Skin reactions may also tie to systemic contraindications, seen with NSAID-precipitated bronchospasm,[232][233] or those with atopy.[234]
Aspirin and other NSAIDs, such as ibuprofen, may delay the healing of skin wounds.[235] Earlier findings from two small, low-quality trials suggested a benefit with aspirin (alongside compression therapy) on venous leg ulcer healing time and leg ulcer size,[236][237][238] however, larger, more recent studies of higher quality have been unable to corroborate these outcomes.[239][240]
Other adverse effects
[edit]Aspirin can induce swelling of skin tissues in some people. In one study, angioedema appeared one to six hours after ingesting aspirin in some of the people. However, when the aspirin was taken alone, it did not cause angioedema in these people; the aspirin had been taken in combination with another NSAID-induced drug when angioedema appeared.[241]
Aspirin causes an increased risk of cerebral microbleeds, having the appearance on MRI scans of 5 to 10 mm or smaller, hypointense (dark holes) patches.[242][243]
A study of a group with a mean dosage of aspirin of 270 mg per day estimated an average absolute risk increase in intracerebral hemorrhage (ICH) of 12 events per 10,000 persons.[244] In comparison, the estimated absolute risk reduction in myocardial infarction was 137 events per 10,000 persons, and a reduction of 39 events per 10,000 persons in ischemic stroke.[244] In cases where ICH already has occurred, aspirin use results in higher mortality, with a dose of about 250 mg per day resulting in a relative risk of death within three months after the ICH around 2.5 (95% confidence interval 1.3 to 4.6).[245]
Aspirin and other NSAIDs can cause abnormally high blood levels of potassium by inducing a hyporeninemic hypoaldosteronism state via inhibition of prostaglandin synthesis; however, these agents do not typically cause hyperkalemia by themselves in the setting of normal renal function and euvolemic state.[246]
Use of low-dose aspirin before a surgical procedure has been associated with an increased risk of bleeding events in some patients, however, ceasing aspirin prior to surgery has also been associated with an increase in major adverse cardiac events. An analysis of multiple studies found a three-fold increase in adverse events such as myocardial infarction in patients who ceased aspirin prior to surgery. The analysis found that the risk is dependent on the type of surgery being performed and the patient indication for aspirin use.[247]
In July 2015, the US Food and Drug Administration (FDA) strengthened warnings of increased heart attack and stroke risk associated with nonsteroidal anti-inflammatory drugs (NSAID).[248] Aspirin is an NSAID but is not affected by the revised warnings.[248]
Overdose
[edit]
Aspirin overdose can be acute or chronic. In acute poisoning, a single large dose is taken; in chronic poisoning, higher than normal doses are taken over a period of time. Acute overdose has a mortality rate of 2%. Chronic overdose is more commonly lethal, with a mortality rate of 25%;[249] chronic overdose may be especially severe in children.[250] Toxicity is managed with a number of potential treatments, including activated charcoal, intravenous dextrose and normal saline, sodium bicarbonate, and dialysis.[251] The diagnosis of poisoning usually involves measurement of plasma salicylate, the active metabolite of aspirin, by automated spectrophotometric methods. Plasma salicylate levels in general range from 30 to 100 mg/L after usual therapeutic doses, 50–300 mg/L in people taking high doses and 700–1400 mg/L following acute overdose. Salicylate is also produced as a result of exposure to bismuth subsalicylate, methyl salicylate, and sodium salicylate.[252][253]
Interactions
[edit]Aspirin is known to interact with other drugs. For example, acetazolamide and ammonium chloride are known to enhance the intoxicating effect of salicylates, and alcohol also increases the gastrointestinal bleeding associated with these types of drugs.[203] Aspirin is known to displace a number of drugs from protein-binding sites in the blood, including the antidiabetic drugs tolbutamide and chlorpropamide, warfarin, methotrexate, phenytoin, probenecid, valproic acid (as well as interfering with beta oxidation, an important part of valproate metabolism), and other NSAIDs. Corticosteroids may also reduce the concentration of aspirin. Other NSAIDs, such as ibuprofen and naproxen, may reduce the antiplatelet effect of aspirin.[254][255] Although limited evidence suggests this may not result in a reduced cardioprotective effect of aspirin.[254] Analgesic doses of aspirin decrease sodium loss induced by spironolactone in the urine, however this does not reduce the antihypertensive effects of spironolactone.[256] Furthermore, antiplatelet doses of aspirin are deemed too small to produce an interaction with spironolactone.[257] Aspirin is known to compete with penicillin G for renal tubular secretion.[258] Aspirin may also inhibit the absorption of vitamin C.[259][260][unreliable medical source?][261]
Research
[edit]The ISIS-2 trial demonstrated that aspirin at doses of 160 mg daily for one month, decreased the mortality by 21% of participants with a suspected myocardial infarction in the first five weeks.[262] A single daily dose of 324 mg of aspirin for 12 weeks has a highly protective effect against acute myocardial infarction and death in men with unstable angina.[263]
Aspirin has been repurposed as an add-on treatment for depressive episodes in subjects with bipolar disorder. However, meta-analytic evidence is based on very few studies and does not suggest any efficacy of aspirin in the treatment of bipolar depression. Thus, notwithstanding the biological rationale, the clinical perspectives of aspirin and anti-inflammatory agents in the treatment of bipolar depression remain uncertain.[164]
Several studies investigated the anti-infective properties of aspirin for bacterial, viral and parasitic infections. Aspirin was demonstrated to limit platelet activation induced by Staphylococcus aureus and Enterococcus faecalis and to reduce streptococcal adhesion to heart valves. In patients with tuberculous meningitis, the addition of aspirin reduced the risk of new cerebral infarction [RR = 0.52 (0.29-0.92)]. A role of aspirin on bacterial and fungal biofilm is also being supported by growing evidence.[264]
Evidence from observational studies was conflicting on the effect of aspirin in breast cancer prevention;[265] a randomized controlled trial showed that aspirin had no significant effect in reducing breast cancer,[266] thus further studies are needed to clarify the effect of aspirin in cancer prevention.[267]
There are anecdotal reports that aspirin can improve the growth and resistance of plants,[268][269] though most research has involved salicylic acid instead of aspirin.[270]
Veterinary medicine
[edit]Aspirin is sometimes used in veterinary medicine as an anticoagulant or to relieve pain associated with musculoskeletal inflammation or osteoarthritis. Aspirin should be given to animals only under the direct supervision of a veterinarian, as adverse effects—including gastrointestinal issues—are common. An aspirin overdose in any species may result in salicylate poisoning, characterized by hemorrhaging, seizures, coma, and even death.[271]
Dogs are better able to tolerate aspirin than cats are.[272] Cats metabolize aspirin slowly because they lack the glucuronide conjugates that aid in the excretion of aspirin, making it potentially toxic if dosing is not spaced out properly.[271][273] No clinical signs of toxicosis occurred when cats were given 25 mg/kg of aspirin every 48 hours for 4 weeks,[272] but the recommended dose for relief of pain and fever and for treating blood clotting diseases in cats is 10 mg/kg every 48 hours to allow for metabolization.[271][274]
References
[edit]- ^ McTavish J (Fall 1987). "What's in a Name? Aspirin and the American Medical Association". Bulletin of the History of Medicine. 61 (3): 343–366. JSTOR 44442097. PMID 3311247.
- ^ "Aspirin Use During Pregnancy". Drugs.com. 2 April 2018. Retrieved 29 December 2019.
- ^ "OTC medicine monograph: Aspirin tablets for oral use". Therapeutic Goods Administration (TGA). 21 June 2022. Retrieved 4 April 2023.
- ^ "Therapeutic Goods (Poisons Standard— June 2025) Instrument 2025" (pdf). Therapeutic Goods Administration (TGA). May 2025. Retrieved 31 August 2025.
- ^ "Aspirin Product information". Health Canada. 22 October 2009. Retrieved 20 August 2023.
- ^ a b "Zorprin, Bayer Buffered Aspirin (aspirin) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 7 April 2014. Retrieved 3 April 2014.
- ^ a b c Brayfield A, ed. (14 January 2014). "Aspirin". Martindale: The Complete Drug Reference. Pharmaceutical Press. Retrieved 3 April 2014.
- ^ CID 2244 from PubChem
- ^ a b Haynes WM, ed. (2011). CRC Handbook of Chemistry and Physics (92nd ed.). Boca Raton, Florida: CRC Press. p. 3.8. ISBN 1-4398-5511-0.
- ^ "aspirin". Random House Webster's Unabridged Dictionary.
- ^ a b c d e f g h i j k l m n "Aspirin". American Society of Health-System Pharmacists. 29 November 2021. Archived from the original on 25 April 2017 – via Drugs.com.
- ^ Mahdi J (28 August 2014). "Biosynthesis and metabolism of β-d-salicin: A novel molecule that exerts biological function in humans and plants". Biotechnology Reports (Amsterdam, Netherlands). 4. National Library of Medicine: 73–79. doi:10.1016/j.btre.2014.08.005. PMC 5466123. PMID 28626665.
- ^ a b Jones A (2015). Chemistry: An Introduction for Medical and Health Sciences. John Wiley & Sons. pp. 5–6. ISBN 978-0-470-09290-3.
- ^ Ravina E (2011). The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. John Wiley & Sons. p. 24. ISBN 978-3-527-32669-3.
- ^ a b c d e f g h i j k Jeffreys D (2008). Aspirin the remarkable story of a wonder drug. Bloomsbury Publishing USA. ISBN 978-1-59691-816-0. Archived from the original on 8 September 2017.: 46–48
- ^ a b "Felix Hoffmann". Science History Institute. Archived from the original on 18 July 2025. Retrieved 3 October 2024.
- ^ a b c Mann CC, Plummer ML (1991). The aspirin wars: money, medicine, and 100 years of rampant competition (1st ed.). New York: Knopf. p. 27. ISBN 978-0-394-57894-1.
- ^ a b Warner TD, Mitchell JA (October 2002). "Cyclooxygenase-3 (COX-3): filling in the gaps toward a COX continuum?". Proceedings of the National Academy of Sciences of the United States of America. 99 (21): 13371–3. Bibcode:2002PNAS...9913371W. doi:10.1073/pnas.222543099. PMC 129677. PMID 12374850.
- ^ World Health Organization (2023). The selection and use of essential medicines 2023: web annex A: World Health Organization model list of essential medicines: 23rd list (2023). Geneva: World Health Organization. hdl:10665/371090. WHO/MHP/HPS/EML/2023.02.
- ^ "Top 300 of 2023". ClinCalc. Archived from the original on 12 August 2025. Retrieved 12 August 2025.
- ^ "Aspirin Drug Usage Statistics, United States, 2013 - 2023". ClinCalc. Retrieved 18 August 2025.
- ^ Dick B (2018). "Hard Work and Happenstance". Distillations. Vol. 4, no. 1. Science History Institute. pp. 44–45.
- ^ a b c d e "Aspirin". Chemical & Engineering News. Vol. 83, no. 25. 20 June 2005.
- ^ a b c Myers RL (2007). The 100 Most Important Chemical Compounds: A Reference Guide. ABC-CLIO. pp. 10–12. ISBN 978-0-313-33758-1. Archived from the original on 17 June 2016. Retrieved 21 November 2015.
- ^ Reynolds EF, ed. (1982). "Aspirin and similar analgesic and anti-inflammatory agents". Martindale: the extra pharmacopoeia (28th ed.). Rittenhouse Book Distributors. pp. 234–82. ISBN 978-0-85369-160-0.
- ^ "Acetylsalicylic acid". U.S. National Institute for Occupational Safety and Health (NIOSH). 11 April 2016. Archived from the original on 11 May 2017.
- ^ "Appendix G: 1989 Air contaminants update project – Exposure limits NOT in effect". National Institute for Occupational Safety and Health. 13 February 2015. Archived from the original on 18 June 2017.
- ^ Palleros DR (2000). Experimental organic chemistry. New York: John Wiley & Sons. p. 494. ISBN 978-0-471-28250-1.
- ^ "Chemical of the Week -- Acetic Acid and Acetic Anhydride". www.eng.uwaterloo.ca. Archived from the original on 3 November 2022.
- ^ Barrans R (18 May 2008). "Aspirin aging". Newton BBS. Archived from the original on 18 May 2008.
- ^ Carstensen JT, Attarchi F (April 1988). "Decomposition of aspirin in the solid state in the presence of limited amounts of moisture III: Effect of temperature and a possible mechanism". Journal of Pharmaceutical Sciences. 77 (4): 318–21. Bibcode:1988JPhmS..77..318C. doi:10.1002/jps.2600770407. PMID 3379589.
- ^ Myers RL (2007). The 100 most important chemical compounds: a reference guide. ABC-CLIO. p. 10. ISBN 978-0-313-33758-1. Archived from the original on 10 June 2013.
- ^ "Acetylsalicylic acid". Jinno Laboratory, School of Materials Science, Toyohashi University of Technology. 4 March 1996. Archived from the original on 20 January 2012. Retrieved 12 April 2014.
- ^ a b Bučar DK, Lancaster RW, Bernstein J (June 2015). "Disappearing polymorphs revisited". Angewandte Chemie. 54 (24): 6972–6993. Bibcode:2015ACIE...54.6972B. doi:10.1002/anie.201410356. PMC 4479028. PMID 26031248.
- ^ Vishweshwar P, McMahon JA, Oliveira M, Peterson ML, Zaworotko MJ (December 2005). "The predictably elusive form II of aspirin". Journal of the American Chemical Society. 127 (48): 16802–16803. Bibcode:2005JAChS.12716802V. doi:10.1021/ja056455b. PMID 16316223.
- ^ Bond AD, Boese R, Desiraju GR (2007). "On the polymorphism of aspirin: crystalline aspirin as intergrowths of two "polymorphic" domains". Angewandte Chemie. 46 (4): 618–622. Bibcode:2007ACIE...46..618B. doi:10.1002/anie.200603373. PMID 17139692.
- ^ "Polytypism - Online Dictionary of Crystallography". reference.iucr.org.
- ^ Crowell EL, Dreger ZA, Gupta YM (15 February 2015). "High-pressure polymorphism of acetylsalicylic acid (aspirin): Raman spectroscopy". Journal of Molecular Structure. 1082: 29–37. Bibcode:2015JMoSt1082...29C. doi:10.1016/j.molstruc.2014.10.079. ISSN 0022-2860. OSTI 1246445.
- ^ Shtukenberg AG, Hu CT, Zhu Q, Schmidt MU, Xu W, Tan M, et al. (7 June 2017). "The Third Ambient Aspirin Polymorph". Crystal Growth & Design. 17 (6): 3562–3566. Bibcode:2017CrGrD..17.3562S. doi:10.1021/acs.cgd.7b00673. ISSN 1528-7483. OSTI 1373897.
- ^ Vane JR (June 1971). "Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs". Nature. 231 (25): 232–5. doi:10.1038/newbio231232a0. PMID 5284360.
- ^ Vane JR, Botting RM (June 2003). "The mechanism of action of aspirin". Thrombosis Research. 110 (5–6): 255–8. doi:10.1016/s0049-3848(03)00379-7. PMID 14592543.
- ^ "The Nobel Prize in Physiology or Medicine 1982". Nobelprize.org. Archived from the original on 27 June 2017.
- ^ Patrignani P, Patrono C (April 2015). "Cyclooxygenase inhibitors: From pharmacology to clinical read-outs". Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 1851 (4): 422–32. doi:10.1016/j.bbalip.2014.09.016. PMID 25263946.
- ^ a b Meek IL, Van de Laar MA, E Vonkeman H (July 2010). "Non-Steroidal Anti-Inflammatory Drugs: An Overview of Cardiovascular Risks". Pharmaceuticals. 3 (7): 2146–2162. doi:10.3390/ph3072146. PMC 4036661. PMID 27713346.
- ^ "Aspirin in heart attack and stroke prevention". American Heart Association. Archived from the original on 31 March 2008. Retrieved 8 May 2008.
- ^ Tohgi H, Konno S, Tamura K, Kimura B, Kawano K (October 1992). "Effects of low-to-high doses of aspirin on platelet aggregability and metabolites of thromboxane A2 and prostacyclin". Stroke. 23 (10): 1400–3. doi:10.1161/01.STR.23.10.1400. PMID 1412574.
- ^ Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, et al. (May 2009). "Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials". Lancet. 373 (9678): 1849–60. doi:10.1016/S0140-6736(09)60503-1. PMC 2715005. PMID 19482214.
- ^ Clària J, Serhan CN (October 1995). "Aspirin triggers previously undescribed bioactive eicosanoids by human endothelial cell-leukocyte interactions". Proceedings of the National Academy of Sciences of the United States of America. 92 (21): 9475–9479. Bibcode:1995PNAS...92.9475C. doi:10.1073/pnas.92.21.9475. PMC 40824. PMID 7568157.
- ^ Martínez-González J, Badimon L (2007). "Mechanisms underlying the cardiovascular effects of COX-inhibition: benefits and risks". Current Pharmaceutical Design. 13 (22): 2215–27. doi:10.2174/138161207781368774. PMID 17691994.
- ^ Funk CD, FitzGerald GA (November 2007). "COX-2 inhibitors and cardiovascular risk". Journal of Cardiovascular Pharmacology. 50 (5): 470–9. doi:10.1097/FJC.0b013e318157f72d. PMID 18030055. S2CID 39103383.
- ^ Ikdahl E, Kerola A, Sollerud E, Semb AG (2024). "Cardiovascular Implications of Non-steroidal Anti-inflammatory Drugs: A Comprehensive Review, with Emphasis on Patients with Rheumatoid Arthritis". European Cardiology. 19 e27. doi:10.15420/ecr.2024.24. PMC 11770528. PMID 39872418.
- ^ Romano M, Cianci E, Simiele F, Recchiuti A (August 2015). "Lipoxins and aspirin-triggered lipoxins in resolution of inflammation". European Journal of Pharmacology. 760: 49–63. doi:10.1016/j.ejphar.2015.03.083. PMID 25895638.
- ^ Serhan CN, Chiang N (August 2013). "Resolution phase lipid mediators of inflammation: agonists of resolution". Current Opinion in Pharmacology. 13 (4): 632–40. doi:10.1016/j.coph.2013.05.012. PMC 3732499. PMID 23747022.
- ^ Weylandt KH (August 2016). "Docosapentaenoic acid derived metabolites and mediators - The new world of lipid mediator medicine in a nutshell". European Journal of Pharmacology. 785: 108–115. doi:10.1016/j.ejphar.2015.11.002. PMID 26546723.
- ^ Somasundaram S, Sigthorsson G, Simpson RJ, Watts J, Jacob M, Tavares IA, et al. (May 2000). "Uncoupling of intestinal mitochondrial oxidative phosphorylation and inhibition of cyclooxygenase are required for the development of NSAID-enteropathy in the rat". Alimentary Pharmacology & Therapeutics. 14 (5): 639–50. doi:10.1046/j.1365-2036.2000.00723.x. PMID 10792129. S2CID 44832283.
- ^ Paul-Clark MJ, Van Cao T, Moradi-Bidhendi N, Cooper D, Gilroy DW (July 2004). "15-epi-lipoxin A4-mediated induction of nitric oxide explains how aspirin inhibits acute inflammation". The Journal of Experimental Medicine. 200 (1): 69–78. doi:10.1084/jem.20040566. PMC 2213311. PMID 15238606.
- ^ McCarty MF, Block KI (September 2006). "Preadministration of high-dose salicylates, suppressors of NF-kappaB activation, may increase the chemosensitivity of many cancers: an example of proapoptotic signal modulation therapy". Integrative Cancer Therapies. 5 (3): 252–68. doi:10.1177/1534735406291499. PMID 16880431.
- ^ Silva Caldas AP, Chaves LO, Linhares Da Silva L, De Castro Morais D, Gonçalves Alfenas RD (29 December 2017). "Mechanisms involved in the cardioprotective effect of avocado consumption: A systematic review". International Journal of Food Properties. 20 (sup2): 1675–1685. doi:10.1080/10942912.2017.1352601. ISSN 1094-2912.
...there was postprandial reduction on the plasma concentration of IL-6 and IkBα preservation, followed by the lower activation of NFκB, considered the main transcription factor capable of inducing inflammatory response by stimulating the expression of proinflammatory cytokines, chemokines, and adhesion molecules.
- ^ Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, et al. (January 2018). "Inflammatory responses and inflammation-associated diseases in organs". Oncotarget. 9 (6): 7204–7218. doi:10.18632/oncotarget.23208. PMC 5805548. PMID 29467962.
- ^ Lawrence T (December 2009). "The nuclear factor NF-kappaB pathway in inflammation". Cold Spring Harbor Perspectives in Biology. 1 (6) a001651. doi:10.1101/cshperspect.a001651. PMC 2882124. PMID 20457564.
- ^ Hawley SA, Fullerton MD, Ross FA, Schertzer JD, Chevtzoff C, Walker KJ, et al. (May 2012). "The ancient drug salicylate directly activates AMP-activated protein kinase". Science. 336 (6083): 918–22. Bibcode:2012Sci...336..918H. doi:10.1126/science.1215327. PMC 3399766. PMID 22517326.
- ^ "Clues to aspirin's anti-cancer effects revealed". New Scientist. 214 (2862): 16. 28 April 2012. doi:10.1016/S0262-4079(12)61073-2.
- ^ Alfonso LF, Srivenugopal KS, Arumugam TV, Abbruscato TJ, Weidanz JA, Bhat GJ (March 2009). "Aspirin inhibits camptothecin-induced p21CIP1 levels and potentiates apoptosis in human breast cancer cells". International Journal of Oncology. 34 (3): 597–608. doi:10.3892/ijo_00000185. PMID 19212664.
- ^ Alfonso LF, Srivenugopal KS, Bhat GJ (2009). "Does aspirin acetylate multiple cellular proteins? (Review)". Molecular Medicine Reports (review). 2 (4): 533–7. doi:10.3892/mmr_00000132. PMID 21475861.
- ^ Alfonso LF, Srivenugopal KS, Bhat GJ (4 June 2009). "Does aspirin acetylate multiple cellular proteins? (Review)". Molecular Medicine Reports. 2 (4): 533–537. doi:10.3892/mmr_00000132. PMID 21475861.
- ^ a b c d e f g h i j Clerici B, Cattaneo M (2023). "Pharmacological Efficacy and Gastrointestinal Safety of Different Aspirin Formulations for Cardiovascular Prevention: A Narrative Review". Journal of Cardiovascular Development and Disease. 10 (4): 137. doi:10.3390/jcdd10040137. PMC 10145431. PMID 37103016.
- ^ Werz O, Stettler H, Theurer C, Seibel J (2024). "The 125th Anniversary of Aspirin—The Story Continues". Pharmaceuticals. 17 (4): 437. doi:10.3390/ph17040437. PMC 11054228. PMID 38675399.
- ^ a b c d e Angiolillo DJ, Prats J, Deliargyris EN, Schneider DJ (2022). "Pharmacokinetic and Pharmacodynamic Profile of a Novel Phospholipid Aspirin Formulation". Clinical Pharmacokinetics. 61 (4): 465–479. doi:10.1007/s40262-021-01090-2. PMC 8773391. PMID 35060092.
- ^ a b Kedir HM, Sisay EA, Abiye AA (2021). "Enteric-Coated Aspirin and the Risk of Gastrointestinal Side Effects: A Systematic Review". International Journal of General Medicine. 14: 4757–4763. doi:10.2147/IJGM.S326929. PMC 8403009. PMID 34466020.
- ^ George M, ElSayed S, Magee C, Speechly-Dick ME (2025). "Practical Prescribing: Aspirin". BMJ. 390 e081606. doi:10.1136/bmj-2024-081606. PMID 40602824.
- ^ a b Franchi F, Schneider DJ, Prats J, Fan W, Rollini F, Been L, et al. (October 2022). "Pharmacokinetic and pharmacodynamic profiles of a novel phospholipid-aspirin complex liquid formulation and low dose enteric-coated aspirin: results from a prospective, randomized, crossover study". Journal of Thrombosis and Thrombolysis. 54 (3): 373–381. doi:10.1007/s11239-022-02687-5. PMC 9421621. PMID 36036856.
- ^ Patel V, Fisher M, Voelker M, Gessner U (July 2012). "Gastrointestinal effects of the addition of ascorbic acid to aspirin". Pain Practice. 12 (6): 476–84. doi:10.1111/j.1533-2500.2011.00517.x. PMID 22151399.
- ^ Kanani K, Gatoulis SC, Voelker M (August 2015). "Influence of Differing Analgesic Formulations of Aspirin on Pharmacokinetic Parameters". Pharmaceutics. 7 (3): 188–98. doi:10.3390/pharmaceutics7030188. PMC 4588194. PMID 26247959.
- ^ Chatzidopavlaki P, Triantafyllopoulou E, Pippa N, Valsami G, Dallas PP (2025). "Recent advances in the technology of effervescent tablets: lessons learned and future perspectives" (PDF). RSC Pharmaceutics. 2 (1): 8–18. doi:10.1039/D4PM00229F.
- ^ Watanabe T, Fujiwara Y, Chan FK (May 2020). "Current knowledge on non-steroidal anti-inflammatory drug-induced small-bowel damage: a comprehensive review". Journal of Gastroenterology. 55 (5): 481–495. doi:10.1007/s00535-019-01657-8. PMC 7188723. PMID 31865463.
- ^ Zhang M, Xia F, Xia S, Zhou W, Zhang Y, Han X, et al. (2022). "NSAID-Associated Small Intestinal Injury: An Overview From Animal Model Development to Pathogenesis, Treatment, and Prevention". Frontiers in Pharmacology. 13 818877. doi:10.3389/fphar.2022.818877. PMC 8864225. PMID 35222032.
- ^ Lotrionte M, Biasucci LM, Peruzzi M, Frati G, Giordano A, Biondi-Zoccai G (2016). "Which Aspirin Dose and Preparation Is Best for the Long-Term Prevention of Cardiovascular Disease and Cancer? Evidence From a Systematic Review and Network Meta-Analysis". Progress in Cardiovascular Diseases. 58 (5): 495–504. doi:10.1016/j.pcad.2016.02.001. PMID 26851562.
- ^ Ferguson RK, Boutros AR (August 1970). "Death following self-poisoning with aspirin". JAMA. 213 (7): 1186–8. doi:10.1001/jama.213.7.1186. PMID 5468267.
- ^ Kaufman FL, Dubansky AS (April 1972). "Darvon poisoning with delayed salicylism: a case report". Pediatrics. 49 (4): 610–1. doi:10.1542/peds.49.4.610. PMID 5013423. S2CID 29427204.
- ^ a b c Levy G, Tsuchiya T (August 1972). "Salicylate accumulation kinetics in man". The New England Journal of Medicine. 287 (9): 430–2. doi:10.1056/NEJM197208312870903. PMID 5044917.
- ^ Grootveld M, Halliwell B (January 1988). "2,3-Dihydroxybenzoic acid is a product of human aspirin metabolism". Biochemical Pharmacology. 37 (2): 271–80. doi:10.1016/0006-2952(88)90729-0. PMID 3342084.
- ^ Hartwig-Otto H (November 1983). "Pharmacokinetic considerations of common analgesics and antipyretics". The American Journal of Medicine. 75 (5A): 30–7. doi:10.1016/0002-9343(83)90230-9. PMID 6606362.
- ^ Done AK (November 1960). "Salicylate intoxication. Significance of measurements of salicylate in blood in cases of acute ingestion". Pediatrics. 26: 800–7. doi:10.1542/peds.26.5.800. PMID 13723722. S2CID 245036862.
- ^ Chyka PA, Erdman AR, Christianson G, Wax PM, Booze LL, Manoguerra AS, et al. (2007). "Salicylate poisoning: an evidence-based consensus guideline for out-of-hospital management". Clinical Toxicology. 45 (2): 95–131. doi:10.1080/15563650600907140. PMID 17364628.
- ^ Prescott LF, Balali-Mood M, Critchley JA, Johnstone AF, Proudfoot AT (November 1982). "Diuresis or urinary alkalinisation for salicylate poisoning?". British Medical Journal. 285 (6352): 1383–6. doi:10.1136/bmj.285.6352.1383. PMC 1500395. PMID 6291695.
- ^ Dargan PI, Wallace CI, Jones AL (May 2002). "An evidence based flowchart to guide the management of acute salicylate (aspirin) overdose". Emergency Medicine Journal. 19 (3): 206–9. doi:10.1136/emj.19.3.206. PMC 1725844. PMID 11971828.
- ^ a b D'Agati V (July 1996). "Does aspirin cause acute or chronic renal failure in experimental animals and in humans?". American Journal of Kidney Diseases. 28 (1 Suppl 1): S24-9. doi:10.1016/s0272-6386(96)90565-x. PMID 8669425.
- ^ Goldberg DR (Summer 2009). "Aspirin: Turn of the Century Miracle Drug". Chemical Heritage. Vol. 27, no. 2. pp. 26–30.
- ^ Jeffreys D (2004). Aspirin: the Remarkable Story of a Wonder Drug. Bloomsbury. pp. 18–34.
- ^ Schiebinger L (October 2003). "Women's health and clinical trials". The Journal of Clinical Investigation. 112 (7): 973–7. doi:10.1172/JCI19993. PMC 198535. PMID 14523031.
- ^ "Regular aspirin intake and acute myocardial infarction". British Medical Journal. 1 (5905): 440–3. March 1974. doi:10.1136/bmj.1.5905.440. PMC 1633212. PMID 4816857.
- ^ Elwood PC, Cochrane AL, Burr ML, Sweetnam PM, Williams G, Welsby E, et al. (March 1974). "A randomized controlled trial of acetyl salicylic acid in the secondary prevention of mortality from myocardial infarction". British Medical Journal. 1 (5905): 436–40. doi:10.1136/bmj.1.5905.436. PMC 1633246. PMID 4593555.
- ^ Bayer Co. v. United Drug Co., 272 F. 505, p.512 (S.D.N.Y 1921).
- ^ "Has aspirin become a generic trademark?". genericides.org. 25 March 2020. Archived from the original on 5 March 2021. Retrieved 17 February 2021.
- ^ Huth EJ, et al. (CBE Style Manual Committee) (1994). Scientific style and format: the CBE manual for authors, editors, and publishers. Cambridge University Press. p. 164. Bibcode:1994ssfc.book.....S. ISBN 978-0-521-47154-1. Archived from the original on 15 October 2015.
- ^ "Aspirin: the versatile drug". CBC News. 28 May 2009. Archived from the original on 6 November 2016.
- ^ Cheng TO (2007). "The history of aspirin". Texas Heart Institute Journal. 34 (3): 392–3. PMC 1995051. PMID 17948100.
- ^ "Aspirin". Sigma Aldrich. Retrieved 24 January 2022.
- ^ "Index BP 2009" (PDF). British Pharmacopoeia. Archived from the original (PDF) on 11 April 2009. Retrieved 13 July 2009.
- ^
 This article incorporates text from this source, which is in the public domain: "Aspirin for reducing your risk of heart attack and stroke: know the facts". U.S. Food and Drug Administration (FDA). Archived from the original on 14 August 2012. Retrieved 26 July 2012.
This article incorporates text from this source, which is in the public domain: "Aspirin for reducing your risk of heart attack and stroke: know the facts". U.S. Food and Drug Administration (FDA). Archived from the original on 14 August 2012. Retrieved 26 July 2012.
- ^
 This article incorporates text from this source, which is in the public domain: "Aspirin for the prevention of cardiovascular disease". United States Preventive Services Task Force. Archived from the original on 11 July 2012. Retrieved 26 July 2012.
This article incorporates text from this source, which is in the public domain: "Aspirin for the prevention of cardiovascular disease". United States Preventive Services Task Force. Archived from the original on 11 July 2012. Retrieved 26 July 2012.
- ^ Seshasai SR, Wijesuriya S, Sivakumaran R, Nethercott S, Erqou S, Sattar N, et al. (February 2012). "Effect of aspirin on vascular and nonvascular outcomes: meta-analysis of randomized controlled trials". Archives of Internal Medicine. 172 (3): 209–16. doi:10.1001/archinternmed.2011.628. hdl:10044/1/34287. PMID 22231610.
- ^ McNeil JJ, Woods RL, Nelson MR, Reid CM, Kirpach B, Wolfe R, et al. (October 2018). "Effect of Aspirin on Disability-free Survival in the Healthy Elderly". The New England Journal of Medicine. 379 (16): 1499–1508. doi:10.1056/NEJMoa1800722. hdl:1885/154654. PMC 6426126. PMID 30221596.
- ^ McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, et al. (October 2018). "Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly". The New England Journal of Medicine. 379 (16): 1509–1518. doi:10.1056/NEJMoa1805819. PMC 6289056. PMID 30221597.
- ^ a b Algra AM, Rothwell PM (May 2012). "Effects of regular aspirin on long-term cancer incidence and metastasis: a systematic comparison of evidence from observational studies versus randomised trials". The Lancet. Oncology. 13 (5): 518–27. doi:10.1016/S1470-2045(12)70112-2. PMID 22440112.
There is good evidence from randomised trials that daily aspirin [use] prevents colorectal polyps [type of tumor] and reduces the long-term risk of sporadic colorectal cancer and colorectal cancer in Lynch syndrome. [...] We have now shown that [data from] case–control studies [estimates similar] effect of aspirin on risk of colorectal cancer. [... Furthermore,] case–control and cohort studies yielded associations [of aspirin] with reductions in risk of biliary, oesophageal, and gastric cancer.
- ^ Irfan M, Ismail SB, Noor NM, Hussain NH (October 2020). "Efficacy of Aspirin for Vasculogenic Erectile Dysfunction in Men: A Meta-Analysis of Randomized Control Trials". American Journal of Men's Health. 14 (5) 1557988320969082. doi:10.1177/1557988320969082. PMC 7607788. PMID 33111628.
The analyses suggested that erectile function is significantly improved by the intervention of aspirin compared to the placebo group. The availability of a few RCTs suggests there is a need for further trials on the efficacy of aspirin for vasculogenic ED in men in comparison to the placebo group....
- ^ Sachs CJ (March 2005). "Oral analgesics for acute nonspecific pain". American Family Physician. 71 (5): 913–8. PMID 15768621.
- ^ Gaciong Z (June 2003). "The real dimension of analgesic activity of aspirin". Thrombosis Research. 110 (5–6): 361–4. doi:10.1016/j.thromres.2003.08.009. PMID 14592563.
- ^ Derry CJ, Derry S, Moore RA (December 2014). "Caffeine as an analgesic adjuvant for acute pain in adults". The Cochrane Database of Systematic Reviews. 2014 (12) CD009281. doi:10.1002/14651858.CD009281.pub3. PMC 6485702. PMID 25502052.
- ^ Hersh EV, Moore PA, Ross GL (May 2000). "Over-the-counter analgesics and antipyretics: a critical assessment". Clinical Therapeutics. 22 (5): 500–48. doi:10.1016/S0149-2918(00)80043-0. PMID 10868553.
- ^ Mett A, Tfelt-Hansen P (June 2008). "Acute migraine therapy: recent evidence from randomized comparative trials". Current Opinion in Neurology. 21 (3): 331–7. doi:10.1097/WCO.0b013e3282fee843. PMID 18451718. S2CID 44459366.
- ^ Kingery WS (November 1997). "A critical review of controlled clinical trials for peripheral neuropathic pain and complex regional pain syndromes". Pain. 73 (2): 123–139. doi:10.1016/S0304-3959(97)00049-3. PMID 9415498. S2CID 10418793.
- ^ Loder E, Rizzoli P (January 2008). "Tension-type headache". BMJ. 336 (7635): 88–92. doi:10.1136/bmj.39412.705868.AD. PMC 2190284. PMID 18187725.
- ^ Gilmore B, Michael M (February 2011). "Treatment of acute migraine headache". American Family Physician. 83 (3): 271–80. PMID 21302868.
- ^ Bartfai T, Conti B (March 2010). "Fever". TheScientificWorldJournal. 10: 490–503. doi:10.1100/tsw.2010.50. PMC 2850202. PMID 20305990.
- ^ Pugliese A, Beltramo T, Torre D (October 2008). "Reye's and Reye's-like syndromes". Cell Biochemistry and Function. 26 (7): 741–6. doi:10.1002/cbf.1465. PMID 18711704. S2CID 22361194.
- ^ Beutler AI, Chesnut GT, Mattingly JC, Jamieson B (December 2009). "FPIN's Clinical Inquiries. Aspirin use in children for fever or viral syndromes". American Family Physician. 80 (12): 1472. PMID 20000310.
- ^ "Medications Used to Treat Fever". American Academy of Pediatrics. 29 June 2012. Archived from the original on 18 February 2013. Retrieved 25 November 2012.
- ^ "51 FR 8180" (PDF). United States Federal Register. 51 (45). 7 March 1986. Archived from the original (PDF) on 19 August 2011.
- ^ https://www.govinfo.gov/content/pkg/FR-1986-03-07/pdf/FR-1986-03-07.pdf [bare URL PDF]
- ^ Morris T, Stables M, Hobbs A, de Souza P, Colville-Nash P, Warner T, et al. (August 2009). "Effects of low-dose aspirin on acute inflammatory responses in humans". Journal of Immunology. 183 (3): 2089–96. doi:10.4049/jimmunol.0900477. PMID 19597002.
- ^ National Clinical Guideline Centre (UK) (July 2013). "Adjunctive pharmacotherapy and associated NICE guidance". Myocardial infarction with ST-segment elevation: the acute management of myocardial infarction with ST-segment elevation [Internet]. NICE Clinical Guidelines. Royal College of Physicians (UK). 17.2 Aspirin. PMID 25340241. Archived from the original on 31 December 2015.
- ^ a b c Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. (September 2019). "2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Journal of the American College of Cardiology. 74 (10): e177 – e232. doi:10.1016/j.jacc.2019.03.010. PMC 7685565. PMID 30894318.
- ^ a b Dennis M, Sandercock PA, Reid J, Graham C, Murray G, Venables G, et al. (CLOTS Trials Collaboration) (June 2009). "Effectiveness of thigh-length graduated compression stockings to reduce the risk of deep vein thrombosis after stroke (CLOTS trial 1): a multicentre, randomised controlled trial". Lancet. 373 (9679). London, England: 1958–65. doi:10.1016/S0140-6736(09)60941-7. PMC 2692021. PMID 19477503.
- ^ a b c Rothwell PM, Cook NR, Gaziano JM, Price JF, Belch JF, Roncaglioni MC, et al. (August 2018). "Effects of aspirin on risks of vascular events and cancer according to bodyweight and dose: analysis of individual patient data from randomised trials". Lancet. 392 (10145): 387–399. doi:10.1016/S0140-6736(18)31133-4. PMC 6083400. PMID 30017552.
- ^ Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, Barton J, et al. (October 2018). "Effects of Aspirin for Primary Prevention in Persons with Diabetes Mellitus". The New England Journal of Medicine. 379 (16): 1529–1539. doi:10.1056/NEJMoa1804988. PMID 30146931.
- ^ McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, et al. (October 2018). "Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly". The New England Journal of Medicine. 379 (16): 1509–1518. doi:10.1056/NEJMoa1805819. PMC 6289056. PMID 30221597.
- ^ Woods RL, Polekhina G, Wolfe R, Nelson MR, Ernst ME, Reid CM, et al. (March 2020). "No Modulation of the Effect of Aspirin by Body Weight in Healthy Older Men and Women". Circulation. 141 (13): 1110–1112. doi:10.1161/CIRCULATIONAHA.119.044142. PMC 7286412. PMID 32223674.
- ^ National Guideline Clearinghouse (NGC). "2011 ACCF/AHA/SCAI guideline for percutaneous coronary artery intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions". United States Agency for Healthcare Research and Quality (AHRQ). Archived from the original on 13 August 2012. Retrieved 28 August 2012.
- ^ Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK (August 2001). "Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation" (PDF). The New England Journal of Medicine. 345 (7): 494–502. doi:10.1056/nejmoa010746. PMID 11519503. S2CID 15459216.
- ^ Costa F, Vranckx P, Leonardi S, Moscarella E, Ando G, Calabro P, et al. (May 2015). "Impact of clinical presentation on ischaemic and bleeding outcomes in patients receiving 6- or 24-month duration of dual-antiplatelet therapy after stent implantation: a pre-specified analysis from the PRODIGY (Prolonging Dual-Antiplatelet Treatment After Grading Stent-Induced Intimal Hyperplasia) trial". European Heart Journal. 36 (20): 1242–51. doi:10.1016/s0735-1097(15)61590-x. PMID 25718355.
- ^ Khan SU, Singh M, Valavoor S, Khan MU, Lone AN, Khan MZ, et al. (October 2020). "Dual Antiplatelet Therapy After Percutaneous Coronary Intervention and Drug-Eluting Stents: A Systematic Review and Network Meta-Analysis". Circulation. 142 (15): 1425–1436. doi:10.1161/CIRCULATIONAHA.120.046308. PMC 7547897. PMID 32795096.
- ^ Capodanno D, Alfonso F, Levine GN, Valgimigli M, Angiolillo DJ (December 2018). "ACC/AHA Versus ESC Guidelines on Dual Antiplatelet Therapy: JACC Guideline Comparison". Journal of the American College of Cardiology. 72 (23 Pt A): 2915–2931. doi:10.1016/j.jacc.2018.09.057. PMID 30522654.
- ^ Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. (September 2016). "2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Journal of the American College of Cardiology. 68 (10): 1082–115. doi:10.1016/j.jacc.2016.03.513. PMID 27036918.
- ^ Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, et al. (January 2018). "2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS)". European Heart Journal. 39 (3): 213–260. doi:10.1093/eurheartj/ehx419. PMID 28886622.
- ^ a b Visseren FL, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. (September 2021). "2021 ESC Guidelines on cardiovascular disease prevention in clinical practice". European Heart Journal. 42 (34): 3227–3337. doi:10.1093/eurheartj/ehab484. hdl:11370/9cdd6a34-4aff-4e89-8a58-8fc7b8483e63. PMID 34458905.
- ^ Norris JW (September 2005). "Antiplatelet agents in secondary prevention of stroke: a perspective". Stroke. 36 (9): 2034–6. doi:10.1161/01.STR.0000177887.14339.46. PMID 16100022.
- ^ Sleight P, Pouleur H, Zannad F (July 2006). "Benefits, challenges, and registerability of the polypill". European Heart Journal. 27 (14): 1651–6. doi:10.1093/eurheartj/ehi841. PMID 16603580.
- ^ Wang TH, Bhatt DL, Topol EJ (March 2006). "Aspirin and clopidogrel resistance: an emerging clinical entity". European Heart Journal. 27 (6): 647–54. doi:10.1093/eurheartj/ehi684. PMID 16364973.
- ^ Oliveira DC, Silva RF, Silva DJ, Lima VC (September 2010). "Aspirin resistance: fact or fiction?". Arquivos Brasileiros de Cardiologia. 95 (3): e91-4. doi:10.1590/S0066-782X2010001300024. PMID 20944898.
- ^ Topçuoglu MA, Arsava EM, Ay H (February 2011). "Antiplatelet resistance in stroke". Expert Review of Neurotherapeutics. 11 (2): 251–63. doi:10.1586/ern.10.203. PMC 3086673. PMID 21306212.
- ^ Ben-Dor I, Kleiman NS, Lev E (July 2009). "Assessment, mechanisms, and clinical implication of variability in platelet response to aspirin and clopidogrel therapy". The American Journal of Cardiology. 104 (2): 227–33. doi:10.1016/j.amjcard.2009.03.022. PMID 19576352.
- ^
 This article incorporates text from this source, which is in the public domain: "Recommendation: Aspirin Use to Prevent Cardiovascular Disease: Preventive Medication". United States Preventive Services Taskforce. 23 November 2020. Retrieved 5 May 2022.
This article incorporates text from this source, which is in the public domain: "Recommendation: Aspirin Use to Prevent Cardiovascular Disease: Preventive Medication". United States Preventive Services Taskforce. 23 November 2020. Retrieved 5 May 2022.
- ^ a b c Davidson KW, Barry MJ, Mangione CM, Cabana M, Chelmow D, Coker TR, et al. (((US Preventive Services Task Force))) (April 2022). "Aspirin Use to Prevent Cardiovascular Disease: US Preventive Services Task Force Recommendation Statement". JAMA. 327 (16): 1577–1584. doi:10.1001/jama.2022.4983. PMID 35471505.
- ^ Aubrey A, Stone W (26 April 2022). "Older adults shouldn't start a routine of daily aspirin, task force says". NPR.
- ^ a b Cuzick J, Thorat MA, Bosetti C, Brown PH, Burn J, Cook NR, et al. (January 2015). "Estimates of benefits and harms of prophylactic use of aspirin in the general population". Annals of Oncology. 26 (1): 47–57. doi:10.1093/annonc/mdu225. PMC 4269341. PMID 25096604.
There is now overwhelming evidence for a reduction in CRC [colorectal cancer] incidence and mortality from regular aspirin use. [... Data are less extensive for oesophageal cancer, but still shows] consistent reductions in mortality [,] with a 58% reduction after 5 years of follow-up in randomised trials, and a 44% reduction in cohort studies. [...] The effects of aspirin on cancer are not apparent until at least 3 years after the start of use, and some benefits are sustained for several years after cessation in long-term users. [...] Higher doses do not appear to confer additional benefit but increase toxicities. Excess bleeding is the most important harm associated with aspirin use, and its [excessive bleeding's] risk and fatality rate increases with age.
- ^ Camara Planek MI, Silver AJ, Volgman AS, Okwuosa TM (January 2020). "Exploratory Review of the Role of Statins, Colchicine, and Aspirin for the Prevention of Radiation-Associated Cardiovascular Disease and Mortality". Journal of the American Heart Association. 9 (2) e014668. doi:10.1161/JAHA.119.014668. PMC 7033839. PMID 31960749.
Clinically, aspirin has long been associated with a reduction in cancer mortality. This has largely been studied in colorectal cancer. Studies in mediastinal cancers are rarer. Fourteen smaller observational studies have reported a reduction in breast cancer mortality with use of aspirin (HR [Hazard Ratio], 0.69; 95% CI [Confidence Interval], 0.53–0.90). However, some of these studies included other anti‐inflammatory agents with aspirin, including nonsteroidal anti‐inflammatory drug anticoagulants.
- ^ Thun MJ, Jacobs EJ, Patrono C (April 2012). "The role of aspirin in cancer prevention". Nature Reviews. Clinical Oncology. 9 (5): 259–67. doi:10.1038/nrclinonc.2011.199. PMID 22473097. S2CID 3332999.
Aspirin [benefits from] large randomized clinical trials that were originally conducted to study [its] cardioprotective effects but that can now [also] be combined to study cancer end points. Results from secondary analyses of these trials have recently provided the first randomized evidence that prophylactic [preventive] daily treatment with aspirin reduces incidence and death rates from all cancers combined, even at doses as low as 75 mg.
- ^ Manzano A, Pérez-Segura P (29 April 2012). "Colorectal cancer chemoprevention: is this the future of colorectal cancer prevention?". TheScientificWorldJournal. 2012 327341. doi:10.1100/2012/327341. PMC 3353298. PMID 22649288.
- ^ Chan AT, Arber N, Burn J, Chia WK, Elwood P, Hull MA, et al. (February 2012). "Aspirin in the chemoprevention of colorectal neoplasia: an overview". Cancer Prevention Research. 5 (2): 164–78. doi:10.1158/1940-6207.CAPR-11-0391. PMC 3273592. PMID 22084361.
- ^ Richman IB, Owens DK (July 2017). "Aspirin for Primary Prevention". The Medical Clinics of North America (Review). 101 (4): 713–724. doi:10.1016/j.mcna.2017.03.004. PMID 28577622.
- ^ Verdoodt F, Friis S, Dehlendorff C, Albieri V, Kjaer SK (February 2016). "Non-steroidal anti-inflammatory drug use and risk of endometrial cancer: A systematic review and meta-analysis of observational studies". Gynecologic Oncology. 140 (2): 352–8. doi:10.1016/j.ygyno.2015.12.009. PMID 26701413.
- ^ Bosetti C, Rosato V, Gallus S, Cuzick J, La Vecchia C (June 2012). "Aspirin and cancer risk: a quantitative review to 2011". Annals of Oncology. 23 (6): 1403–15. doi:10.1093/annonc/mds113. PMID 22517822.
- ^ Sutcliffe P, Connock M, Gurung T, Freeman K, Johnson S, Kandala NB, et al. (September 2013). "Aspirin for prophylactic use in the primary prevention of cardiovascular disease and cancer: a systematic review and overview of reviews". Health Technology Assessment. 17 (43): 1–253. doi:10.3310/hta17430. PMC 4781046. PMID 24074752.
- ^ Kim SE (2014). "The benefit-risk consideration in long-term use of alternate-day, low dose aspirin: focus on colorectal cancer prevention". Annals of Gastroenterology. 27 (1): 87–88. PMC 3959543. PMID 24714632.
- ^ United States Preventive Services Task Force (March 2007). "Routine aspirin or nonsteroidal anti-inflammatory drugs for the primary prevention of colorectal cancer: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 146 (5): 361–4. doi:10.7326/0003-4819-146-5-200703060-00008. PMID 17339621.
- ^ Bibbins-Domingo K (June 2016). "Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. 164 (12): 836–45. doi:10.7326/m16-0577. PMID 27064677.
- Lay summary in: "Who developed these recommendations?". Annals of Internal Medicine. 21 June 2016.
- ^ Bosetti C, Santucci C, Gallus S, Martinetti M, La Vecchia C (May 2020). "Aspirin and the risk of colorectal and other digestive tract cancers: an updated meta-analysis through 2019". Annals of Oncology. 31 (5): 558–568. doi:10.1016/j.annonc.2020.02.012. hdl:2434/730600. PMID 32272209.
The present comprehensive meta-analysis supports and further quantifies the inverse association between regular aspirin use and the risk of colorectal and other digestive tract cancers, including some rare ones. The favorable effect of aspirin increases with longer duration of use, and, for colorectal cancer, with increasing dose.
- ^ McNeil JJ, Nelson MR, Woods RL, Lockery JE, Wolfe R, Reid CM, et al. (October 2018). "Effect of Aspirin on All-Cause Mortality in the Healthy Elderly". The New England Journal of Medicine. 379 (16): 1519–1528. doi:10.1056/NEJMoa1803955. PMC 6433466. PMID 30221595.
- ^ Yang J, Yamashita-Kanemaru Y, Morris BI, Contursi A, Trajkovski D, Xu J, et al. (March 2025). "Aspirin prevents metastasis by limiting platelet TXA2 suppression of T cell immunity". Nature. 640 (8060): 1052–1061. Bibcode:2025Natur.640.1052Y. doi:10.1038/s41586-025-08626-7. PMC 12018268. PMID 40044852.
- ^ "Scientists describe 'Eureka moment' over how aspirin prevents cancer spread". The Independent. 5 March 2025. Retrieved 5 March 2025.
- ^ "Scientists discover how aspirin could prevent some cancers from spreading". Medical Xpress. Retrieved 5 March 2025.
- ^ Cara E (5 March 2025). "A Surprising New Tool in the Fight Against Cancer: Aspirin". Gizmodo. Retrieved 5 March 2025.
- ^ a b c Bartoli F, Cavaleri D, Bachi B, Moretti F, Riboldi I, Crocamo C, et al. (November 2021). "Repurposed drugs as adjunctive treatments for mania and bipolar depression: A meta-review and critical appraisal of meta-analyses of randomized placebo-controlled trials". Journal of Psychiatric Research. 143: 230–238. doi:10.1016/j.jpsychires.2021.09.018. PMID 34509090. S2CID 237485915.
- ^ Dominiak M, Gędek A, Sikorska M, Mierzejewski P, Wojnar M, Antosik-Wójcińska AZ (December 2022). "Acetylsalicylic Acid and Mood Disorders: A Systematic Review". Pharmaceuticals. 16 (1): 67. doi:10.3390/ph16010067. PMC 9861965. PMID 36678565.
- ^ Savitz JB, Teague TK, Misaki M, Macaluso M, Wurfel BE, Meyer M, et al. (January 2018). "Treatment of bipolar depression with minocycline and/or aspirin: an adaptive, 2×2 double-blind, randomized, placebo-controlled, phase IIA clinical trial". Translational Psychiatry. 8 (1) 27. doi:10.1038/s41398-017-0073-7. PMC 5802452. PMID 29362444.
- ^ Bauer IE, Green C, Colpo GD, Teixeira AL, Selvaraj S, Durkin K, et al. (December 2018). "A Double-Blind, Randomized, Placebo-Controlled Study of Aspirin and N-Acetylcysteine as Adjunctive Treatments for Bipolar Depression". The Journal of Clinical Psychiatry. 80 (1). doi:10.4088/JCP.18m12200. PMID 30549489. S2CID 56483705.
- ^ Li H, Li W, Zhang X, Ma XC, Zhang RW (4 February 2021). "Aspirin Use on Incident Dementia and Mild Cognitive Decline: A Systematic Review and Meta-Analysis". Frontiers in Aging Neuroscience. 12 578071. doi:10.3389/fnagi.2020.578071. PMC 7890199. PMID 33613260.
- ^ Veronese N, Stubbs B, Maggi S, Thompson T, Schofield P, Muller C, et al. (August 2017). "Low-Dose Aspirin Use and Cognitive Function in Older Age: A Systematic Review and Meta-analysis". Journal of the American Geriatrics Society. 65 (8): 1763–1768. doi:10.1111/jgs.14883. PMC 6810633. PMID 28425093.
- ^ Schmidt L, Phelps E, Friedel J, Shokraneh F (August 2019). "Acetylsalicylic acid (aspirin) for schizophrenia". The Cochrane Database of Systematic Reviews. 2019 (8) CD012116. doi:10.1002/14651858.CD012116.pub2. PMC 6699651. PMID 31425623.
- ^ Fond G, Lançon C, Korchia T, Auquier P, Boyer L (2020). "The Role of Inflammation in the Treatment of Schizophrenia". Frontiers in Psychiatry. 11 160. doi:10.3389/fpsyt.2020.00160. PMC 7093323. PMID 32256401.
- ^ a b National Heart Foundation of Australia (RF/RHD guideline development working group) and the Cardiac Society of Australia and New Zealand (2006). "Diagnosis and management of acute rheumatic fever and rheumatic heart disease in Australia. An evidence-based review" (PDF). National Heart Foundation of Australia. pp. 33–37. Archived from the original (PDF) on 26 July 2008.
- ^ Saxena A, Kumar RK, Gera RP, Radhakrishnan S, Mishra S, Ahmed Z (July 2008). "Consensus guidelines on pediatric acute rheumatic fever and rheumatic heart disease". Indian Pediatrics. 45 (7): 565–73. PMID 18695275.
- ^ Hashkes PJ, Tauber T, Somekh E, Brik R, Barash J, Mukamel M, et al. (September 2003). "Naproxen as an alternative to aspirin for the treatment of arthritis of rheumatic fever: a randomized trial". The Journal of Pediatrics. 143 (3): 399–401. doi:10.1067/S0022-3476(03)00388-3. PMID 14517527.
- ^ Rowley AH, Shulman ST (February 2010). "Pathogenesis and management of Kawasaki disease". Expert Review of Anti-Infective Therapy. 8 (2): 197–203. doi:10.1586/eri.09.109. PMC 2845298. PMID 20109049.
- ^ Baumer JH, Love SJ, Gupta A, Haines LC, Maconochie I, Dua JS (October 2006). "Salicylate for the treatment of Kawasaki disease in children". The Cochrane Database of Systematic Reviews. 2010 (4) CD004175. doi:10.1002/14651858.CD004175.pub2. PMC 8765111. PMID 17054199.
- ^ Duley L, Meher S, Hunter KE, Seidler AL, Askie LM (October 2019). "Antiplatelet agents for preventing pre-eclampsia and its complications". The Cochrane Database of Systematic Reviews. 2019 (10). doi:10.1002/14651858.CD004659.pub3. PMC 6820858. PMID 31684684.
- ^ Roberge S, Villa P, Nicolaides K, Giguère Y, Vainio M, Bakthi A, et al. (2012). "Early administration of low-dose aspirin for the prevention of preterm and term preeclampsia: a systematic review and meta-analysis". Fetal Diagnosis and Therapy. 31 (3): 141–6. doi:10.1159/000336662. PMID 22441437. S2CID 26372982.
- ^ Roberge S, Nicolaides K, Demers S, Hyett J, Chaillet N, Bujold E (February 2017). "The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: systematic review and meta-analysis". American Journal of Obstetrics and Gynecology. 216 (2): 110–120.e6. doi:10.1016/j.ajog.2016.09.076. PMID 27640943. S2CID 3079979.
- ^ Szabó B, Németh K, Mészáros K, Krokker L, Likó I, Saskői E, et al. (5 September 2022). "Aspirin Mediates Its Antitumoral Effect Through Inhibiting PTTG1 in Pituitary Adenoma". The Journal of Clinical Endocrinology and Metabolism. 107 (11): 3066–3079. doi:10.1210/clinem/dgac496. PMC 9681612. PMID 36059148.
- ^ Dorsch MP, Lee JS, Lynch DR, Dunn SP, Rodgers JE, Schwartz T, et al. (May 2007). "Aspirin resistance in patients with stable coronary artery disease with and without a history of myocardial infarction". The Annals of Pharmacotherapy. 41 (5): 737–41. doi:10.1345/aph.1H621. PMID 17456544. S2CID 22245507.
- ^ a b Krasopoulos G, Brister SJ, Beattie WS, Buchanan MR (January 2008). "Aspirin "resistance" and risk of cardiovascular morbidity: systematic review and meta-analysis". BMJ. 336 (7637): 195–8. doi:10.1136/bmj.39430.529549.BE. PMC 2213873. PMID 18202034.
- ^ Pignatelli P, Di Santo S, Barillà F, Gaudio C, Violi F (October 2008). "Multiple anti-atherosclerotic treatments impair aspirin compliance: effects on aspirin resistance". Journal of Thrombosis and Haemostasis. 6 (10): 1832–4. doi:10.1111/j.1538-7836.2008.03122.x. PMID 18680540. S2CID 1776526.
- ^ Grosser T, Fries S, Lawson JA, Kapoor SC, Grant GR, FitzGerald GA (January 2013). "Drug resistance and pseudoresistance: an unintended consequence of enteric coating aspirin". Circulation. 127 (3): 377–85. doi:10.1161/CIRCULATIONAHA.112.117283. PMC 3552520. PMID 23212718.
- Lay summary in: Thomas K (4 December 2012). "Study Raises Questions on Coating of Aspirin". The New York Times.
- ^ Li J, Song M, Jian Z, Guo W, Chen G, Jiang G, et al. (2014). "Laboratory aspirin resistance and the risk of major adverse cardiovascular events in patients with coronary heart disease on confirmed aspirin adherence". Journal of Atherosclerosis and Thrombosis. 21 (3): 239–47. doi:10.5551/jat.19521. PMID 24201035.
- ^ Sofi F, Marcucci R, Gori AM, Abbate R, Gensini GF (August 2008). "Residual platelet reactivity on aspirin therapy and recurrent cardiovascular events--a meta-analysis". International Journal of Cardiology. 128 (2): 166–71. doi:10.1016/j.ijcard.2007.12.010. hdl:2158/323452. PMID 18242733.
- ^ Shim EJ, Ryu CW, Park S, Lee HN, Shin HS, Kim SB (October 2018). "Relationship between adverse events and antiplatelet drug resistance in neurovascular intervention: a meta-analysis". Journal of NeuroInterventional Surgery. 10 (10): 942–948. doi:10.1136/neurintsurg-2017-013632. PMID 29352056. S2CID 38147668.
- ^ Fiolaki A, Katsanos AH, Kyritsis AP, Papadaki S, Kosmidou M, Moschonas IC, et al. (May 2017). "High on treatment platelet reactivity to aspirin and clopidogrel in ischemic stroke: A systematic review and meta-analysis". Journal of the Neurological Sciences. 376: 112–116. doi:10.1016/j.jns.2017.03.010. PMID 28431593. S2CID 3485236.
- ^ Snoep JD, Hovens MM, Eikenboom JC, van der Bom JG, Huisman MV (13 August 2007). "Association of laboratory-defined aspirin resistance with a higher risk of recurrent cardiovascular events: a systematic review and meta-analysis". Archives of Internal Medicine. 167 (15): 1593–9. doi:10.1001/archinte.167.15.1593. PMID 17698681.
- ^ a b van Oosterom N, Barras M, Bird R, Nusem I, Cottrell N (December 2020). "A Narrative Review of Aspirin Resistance in VTE Prophylaxis for Orthopaedic Surgery". Drugs. 80 (18): 1889–1899. doi:10.1007/s40265-020-01413-w. hdl:10072/401324. PMID 33037568. S2CID 222234431.
- ^ "Invention of the safety cap". digitaldukemed.mc.duke.edu. Archived from the original on 4 March 2016. Retrieved 4 September 2015.
- ^ a b British National Formulary (45 ed.). British Medical Journal and Royal Pharmaceutical Society of Great Britain. 2003.
- ^ "Aspirin monograph: dosages, etc". Medscape.com. Retrieved 11 May 2011.
- ^ US Preventive Services Task Force (March 2009). "Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 150 (6): 396–404. doi:10.7326/0003-4819-150-6-200903170-00008. PMID 19293072.
- ^ Slawson DC (November 2022). "USPSTF Recommends Against Initiating Aspirin for Primary Prevention of CVD in Adults 60 Years or Older". American Family Physician. 106 (5): 586. PMID 36379482.
- ^ Mallick S, Shroff GR, Linzer M (May 2023). "Aspirin for primary prevention of cardiovascular disease: What do the current USPSTF guidelines say?". Cleveland Clinic Journal of Medicine. 90 (5): 287–291. doi:10.3949/ccjm.90a.22087. PMID 37127334.
- ^ Berger JS, Brown DL, Burke GL, Oberman A, Kostis JB, Langer RD, et al. (March 2009). "Aspirin Use, Dose, and Clinical Outcomes in Postmenopausal Women With Stable Cardiovascular Disease". Circulation: Cardiovascular Quality and Outcomes. 2 (2): 78–87. doi:10.1161/circoutcomes.108.791269. ISSN 1941-7713. PMC 2801891. PMID 20031819.
- ^ Sacristán JA (August 2021). "Aspirin Dosing in Cardiovascular Disease". New England Journal of Medicine. 385 (8): 764–765. doi:10.1056/nejmc2110476. ISSN 0028-4793. PMID 34407352. S2CID 237214969.
- ^ "Aspirin: more evidence that low dose is all that is needed". Medscape. Medscape CME. Retrieved 11 May 2011.
- ^ British National Formulary for Children. British Medical Journal and Royal Pharmaceutical Society. 2006.
- ^ a b
 This article incorporates text from this source, which is in the public domain: "FDA Warns that Using a Type of Pain and Fever Medication in Second Half of Pregnancy Could Lead to Complications". U.S. Food and Drug Administration (FDA) (Press release). 15 October 2020. Archived from the original on 16 October 2020. Retrieved 15 October 2020.
This article incorporates text from this source, which is in the public domain: "FDA Warns that Using a Type of Pain and Fever Medication in Second Half of Pregnancy Could Lead to Complications". U.S. Food and Drug Administration (FDA) (Press release). 15 October 2020. Archived from the original on 16 October 2020. Retrieved 15 October 2020.
- ^ a b c
 This article incorporates text from this source, which is in the public domain: "NSAIDs may cause rare kidney problems in unborn babies". U.S. Food and Drug Administration. 21 July 2017. Archived from the original on 17 October 2020. Retrieved 15 October 2020.
This article incorporates text from this source, which is in the public domain: "NSAIDs may cause rare kidney problems in unborn babies". U.S. Food and Drug Administration. 21 July 2017. Archived from the original on 17 October 2020. Retrieved 15 October 2020.
- ^ a b c d e "Aspirin information from Drugs.com". Drugs.com. Archived from the original on 9 May 2008. Retrieved 8 May 2008.
- ^ Raithel M, Baenkler HW, Naegel A, Buchwald F, Schultis HW, Backhaus B, et al. (September 2005). "Significance of salicylate intolerance in diseases of the lower gastrointestinal tract" (PDF). Journal of Physiology and Pharmacology. 56 (Suppl 5): 89–102. PMID 16247191. Archived (PDF) from the original on 9 April 2011.
- ^ Senna GE, Andri G, Dama AR, Mezzelani P, Andri L (1995). "Tolerability of imidazole salycilate in aspirin-sensitive patients". Allergy Proceedings. 16 (5): 251–254. doi:10.2500/108854195778702675. PMID 8566739.
- ^ a b "PDR guide to over the counter (OTC) drugs". Archived from the original on 10 April 2008. Retrieved 28 April 2008.
- ^ Livingstone FB (1985). Frequencies of hemoglobin variants: thalassemia, the glucose-6-phosphate dehydrogenase deficiency, G6PD variants, and ovalocytosis in human populations. Oxford University Press. ISBN 978-0-19-503634-3.
- ^ "Dengue and dengue hemorrhagic fever: information for health care practitioners". Archived from the original on 17 March 2008. Retrieved 28 April 2008.
- ^ Zhang Y, Neogi T, Chen C, Chaisson C, Hunter DJ, Choi H (February 2014). "Low-dose aspirin use and recurrent gout attacks". Annals of the Rheumatic Diseases. 73 (2): 385–390. doi:10.1136/annrheumdis-2012-202589. PMC 3902644. PMID 23345599.
- ^ Polkinghorne KR, Wetmore JB, Thao LT, Wolfe R, Woods RL, Ernst ME, et al. (December 2022). "Effect of Aspirin on CKD Progression in Older Adults: Secondary Analysis From the ASPREE Randomized Clinical Trial". American Journal of Kidney Diseases. 80 (6): 810–813. doi:10.1053/j.ajkd.2022.02.019. PMC 9562592. PMID 35430328.
- ^ Mann JF, Joseph P, Gao P, Pais P, Tyrwhitt J, Xavier D, et al. (February 2023). "Effects of aspirin on cardiovascular outcomes in patients with chronic kidney disease". Kidney International. 103 (2): 403–410. doi:10.1016/j.kint.2022.09.023. PMID 36341885. S2CID 253194139.
- ^ a b Macdonald S (November 2002). "Aspirin use to be banned in under 16 year olds". BMJ. 325 (7371): 988c–988. doi:10.1136/bmj.325.7371.988/c. PMC 1169585. PMID 12411346.
- ^ a b c Sørensen HT, Mellemkjaer L, Blot WJ, Nielsen GL, Steffensen FH, McLaughlin JK, et al. (September 2000). "Risk of upper gastrointestinal bleeding associated with use of low-dose aspirin". The American Journal of Gastroenterology. 95 (9): 2218–2224. doi:10.1016/s0002-9270(00)01040-6. PMID 11007221.
- ^ Kedir HM, Sisay EA, Abiye AA (2021). "Enteric-Coated Aspirin and the Risk of Gastrointestinal Side Effects: A Systematic Review". International Journal of General Medicine. 14: 4757–4763. doi:10.2147/ijgm.s326929. PMC 8403009. PMID 34466020.
- ^ Torborg L (4 December 2018). "Mayo Clinic Q and A: Coated aspirin may not be as effective at reducing blood clot risk". Mayo Clinic News Network.
- ^ Cox D, Maree AO, Dooley M, Conroy R, Byrne MF, Fitzgerald DJ (August 2006). "Effect of enteric coating on antiplatelet activity of low-dose aspirin in healthy volunteers". Stroke. 37 (8): 2153–2158. doi:10.1161/01.STR.0000231683.43347.ec. PMID 16794200. S2CID 8034371.
- ^ Delaney JA, Opatrny L, Brophy JM, Suissa S (August 2007). "Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding". CMAJ. 177 (4): 347–351. doi:10.1503/cmaj.070186. PMC 1942107. PMID 17698822.
- ^ Wallace JL (October 2008). "Prostaglandins, NSAIDs, and gastric mucosal protection: why doesn't the stomach digest itself?". Physiological Reviews. 88 (4): 1547–65. doi:10.1152/physrev.00004.2008. PMID 18923189. S2CID 448875.
- ^ Rostom A, Muir K, Dubé C, Jolicoeur E, Boucher M, Joyce J, et al. (July 2007). "Gastrointestinal safety of cyclooxygenase-2 inhibitors: a Cochrane Collaboration systematic review". Clinical Gastroenterology and Hepatology. 5 (7): 818–28, 828.e1-5, quiz 768. doi:10.1016/j.cgh.2007.03.011. PMID 17556027.
- ^ "General chemistry online: FAQ: Acids and bases: What is the buffer system in buffered aspirin?". Antoine.frostburg.edu. Archived from the original on 14 April 2011. Retrieved 11 May 2011.
- ^ Davison C, Smith BW, Smith PK (August 1962). "Effects of buffered and unbuffered acetylsalicylic acid upon the gastric acidity of normal human subjects". Journal of Pharmaceutical Sciences. 51 (8): 759–763. Bibcode:1962JPhmS..51..759D. doi:10.1002/jps.2600510813. PMID 13883982.
- ^ Dammann HG, Saleki M, Torz M, Schulz HU, Krupp S, Schürer M, et al. (February 2004). "Effects of buffered and plain acetylsalicylic acid formulations with and without ascorbic acid on gastric mucosa in healthy subjects". Alimentary Pharmacology & Therapeutics. 19 (3): 367–74. doi:10.1111/j.1365-2036.2004.01742.x. PMID 14984384. S2CID 22688422.
- ^ Konturek PC, Kania J, Hahn EG, Konturek JW (November 2006). "Ascorbic acid attenuates aspirin-induced gastric damage: role of inducible nitric oxide synthase". Journal of Physiology and Pharmacology. 57 (Suppl 5): 125–36. PMID 17218764.
- ^ Lendzioszek M, Bryl A, Poppe E, Zorena K, Mrugacz M (July 2024). "Retinal Vein Occlusion-Background Knowledge and Foreground Knowledge Prospects-A Review". Journal of Clinical Medicine. 13 (13): 3950. doi:10.3390/jcm13133950. PMC 11242360. PMID 38999513.
- ^ Valeriani E, Paciullo F, Porfidia A, Pignatelli P, Candeloro M, Di Nisio M, et al. (February 2023). "Antithrombotic treatment for retinal vein occlusion: a systematic review and meta-analysis". Journal of Thrombosis and Haemostasis. 21 (2): 284–293. doi:10.1016/j.jtha.2022.10.003. PMID 36700511.
- ^ Hayreh SS (July 2014). "Ocular vascular occlusive disorders: natural history of visual outcome". Progress in Retinal and Eye Research. 41: 1–25. doi:10.1016/j.preteyeres.2014.04.001. PMC 4073304. PMID 24769221.
- ^ Ageno W, Beyer-Westendorf J, Garcia DA, Lazo-Langner A, McBane RD, Paciaroni M (January 2016). "Guidance for the management of venous thrombosis in unusual sites". Journal of Thrombosis and Thrombolysis. 41 (1): 129–43. doi:10.1007/s11239-015-1308-1. PMC 4715841. PMID 26780742.
- ^ Guitton MJ, Caston J, Ruel J, Johnson RM, Pujol R, Puel JL (May 2003). "Salicylate induces tinnitus through activation of cochlear NMDA receptors". The Journal of Neuroscience. 23 (9): 3944–52. doi:10.1523/JNEUROSCI.23-09-03944.2003. PMC 6742173. PMID 12736364.
- ^ a b Belay ED, Bresee JS, Holman RC, Khan AS, Shahriari A, Schonberger LB (May 1999). "Reye's syndrome in the United States from 1981 through 1997". The New England Journal of Medicine. 340 (18): 1377–82. doi:10.1056/NEJM199905063401801. PMID 10228187.
- ^ "Reye's syndrome". Health A to Z. National Health Service. 14 September 2023. Retrieved 24 August 2024.
- ^ "Are You Sensitive to Aspirin? Here are Some Reasons Why". Health Essentials from Cleveland Clinic. 5 February 2015. Archived from the original on 25 October 2020. Retrieved 5 March 2020.
- ^ a b c Doña I, Barrionuevo E, Salas M, Laguna JJ, Agúndez J, García-Martín E, et al. (November 2018). "NSAIDs-hypersensitivity often induces a blended reaction pattern involving multiple organs". Scientific Reports. 8 (1) 16710. Bibcode:2018NatSR...816710D. doi:10.1038/s41598-018-34668-1. PMC 6232098. PMID 30420763.
- ^ a b Kowalski ML, Agache I, Bavbek S, Bakirtas A, Blanca M, Bochenek G, et al. (January 2019). "Diagnosis and management of NSAID-Exacerbated Respiratory Disease (N-ERD)-a EAACI position paper". Allergy. 74 (1): 28–39. doi:10.1111/all.13599. hdl:10668/12946. PMID 30216468. S2CID 52276808.
- ^ Sánchez-Borges M, Capriles-Hulett A (January 2000). "Atopy is a risk factor for non-steroidal anti-inflammatory drug sensitivity". Annals of Allergy, Asthma & Immunology. 84 (1): 101–6. doi:10.1016/S1081-1206(10)62748-2. PMID 10674573.
- ^ Stadelmann WK, Digenis AG, Tobin GR (August 1998). "Impediments to wound healing". American Journal of Surgery. 176 (2A Suppl): 39S – 47S. doi:10.1016/S0002-9610(98)00184-6. PMID 9777971.
- ^ Layton AM, Ibbotson SH, Davies JA, Goodfield MJ (July 1994). "Randomised trial of oral aspirin for chronic venous leg ulcers". Lancet. 344 (8916): 164–5. doi:10.1016/s0140-6736(94)92759-6. PMID 7912767. S2CID 912169.
- ^ del Río Solá ML, Antonio J, Fajardo G, Vaquero Puerta C (July 2012). "Influence of aspirin therapy in the ulcer associated with chronic venous insufficiency". Annals of Vascular Surgery. 26 (5): 620–9. doi:10.1016/j.avsg.2011.02.051. hdl:10324/2904. PMID 22437068.
- ^ de Oliveira Carvalho PE, Magolbo NG, De Aquino RF, Weller CD, et al. (Cochrane Wounds Group) (February 2016). "Oral aspirin for treating venous leg ulcers". The Cochrane Database of Systematic Reviews. 2016 (2) CD009432. doi:10.1002/14651858.CD009432.pub2. PMC 8627253. PMID 26889740.
- ^ Jull A, Wadham A, Bullen C, Parag V, Kerse N, Waters J (November 2017). "Low dose aspirin as adjuvant treatment for venous leg ulceration: pragmatic, randomised, double blind, placebo controlled trial (Aspirin4VLU)". BMJ. 359 j5157. doi:10.1136/bmj.j5157. PMC 5701114. PMID 29175902.
- ^ Tilbrook H, Clark L, Cook L, Bland M, Buckley H, Chetter I, et al. (October 2018). "AVURT: aspirin versus placebo for the treatment of venous leg ulcers - a Phase II pilot randomised controlled trial". Health Technology Assessment. 22 (55): 1–138. doi:10.3310/hta22550. PMC 6204573. PMID 30325305.
- ^ Berges-Gimeno MP, Stevenson DD (June 2004). "Nonsteroidal anti-inflammatory drug-induced reactions and desensitization". The Journal of Asthma. 41 (4): 375–84. doi:10.1081/JAS-120037650. PMID 15281324. S2CID 29909460.
- ^ Vernooij MW, Haag MD, van der Lugt A, Hofman A, Krestin GP, Stricker BH, et al. (June 2009). "Use of antithrombotic drugs and the presence of cerebral microbleeds: the Rotterdam Scan Study". Archives of Neurology. 66 (6): 714–20. doi:10.1001/archneurol.2009.42. PMID 19364926.
- ^ Gorelick PB (June 2009). "Cerebral microbleeds: evidence of heightened risk associated with aspirin use". Archives of Neurology. 66 (6): 691–3. doi:10.1001/archneurol.2009.85. PMID 19506128.
- ^ a b He J, Whelton PK, Vu B, Klag MJ (December 1998). "Aspirin and risk of hemorrhagic stroke: a meta-analysis of randomized controlled trials". JAMA. 280 (22): 1930–5. doi:10.1001/jama.280.22.1930. PMID 9851479. S2CID 22997730.
- ^ Saloheimo P, Ahonen M, Juvela S, Pyhtinen J, Savolainen ER, Hillbom M (January 2006). "Regular aspirin-use preceding the onset of primary intracerebral hemorrhage is an independent predictor for death". Stroke. 37 (1): 129–33. doi:10.1161/01.STR.0000196991.03618.31. PMID 16322483.
- ^ Medical knowledge self-assessment program for students 4, By American College of Physicians, Clerkship Directors in Internal Medicine, Nephrology 227, Item 29
- ^ Biondi-Zoccai GG, Lotrionte M, Agostoni P, Abbate A, Fusaro M, Burzotta F, et al. (November 2006). "A systematic review and meta-analysis on the hazards of discontinuing or not adhering to aspirin among 50,279 patients at risk for coronary artery disease". European Heart Journal. 27 (22): 2667–2674. doi:10.1093/eurheartj/ehl334. PMID 17053008.
- ^ a b "FDA Drug Safety Communication: FDA strengthens warning that non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) can cause heart attacks or strokes". U.S. Food and Drug Administration (FDA). 9 July 2015. Archived from the original on 11 July 2015. Retrieved 9 July 2015.
- ^ Kreplick LW (2001). "Salicylate toxicity in emergency medicine". Medscape. Archived from the original on 31 August 2012.
- ^ Gaudreault P, Temple AR, Lovejoy FH (October 1982). "The relative severity of acute versus chronic salicylate poisoning in children: a clinical comparison". Pediatrics. 70 (4): 566–9. doi:10.1542/peds.70.4.566. PMID 7122154. S2CID 12738659. (primary source)
- ^ Marx J (2006). Rosen's emergency medicine: concepts and clinical practice. Mosby/Elsevier. p. 2242. ISBN 978-0-323-02845-5.
- ^ Morra P, Bartle WR, Walker SE, Lee SN, Bowles SK, Reeves RA (September 1996). "Serum concentrations of salicylic acid following topically applied salicylate derivatives". The Annals of Pharmacotherapy. 30 (9): 935–40. doi:10.1177/106002809603000903. PMID 8876850. S2CID 9843820.
- ^ Baselt R (2011). Disposition of toxic drugs and chemicals in man (9th ed.). Seal Beach, California: Biomedical Publications. pp. 20–23. ISBN 978-0-9626523-8-7.
- ^ a b Alqahtani Z, Jamali F (2018). "Clinical Outcomes of Aspirin Interaction with Other Non-Steroidal Anti-Inflammatory Drugs: A Systematic Review". Journal of Pharmacy & Pharmaceutical Sciences. 21 (1s): 48s – 73s. doi:10.18433/jpps29854. PMID 29891025. S2CID 48361086.
- ^ Gladding PA, Webster MW, Farrell HB, Zeng IS, Park R, Ruijne N (April 2008). "The antiplatelet effect of six non-steroidal anti-inflammatory drugs and their pharmacodynamic interaction with aspirin in healthy volunteers". The American Journal of Cardiology. 101 (7): 1060–1063. doi:10.1016/j.amjcard.2007.11.054. PMID 18359332.
- ^ Baxter K, Preston CL (eds.). "Aspirin and Spironolactone". MedicinesComplete: Stockley's Drug Interactions. Royal Pharmaceutical Society.
- ^ Hollifield JW (August 1976). "Failure of aspirin to antagonize the antihypertensive effect of spironolactone in low-renin hypertension". Southern Medical Journal. 69 (8): 1034–6. doi:10.1097/00007611-197608000-00022. PMID 785608.
- ^ Katzung BG (1998). Basic and clinical pharmacology. McGraw-Hill. p. 584. ISBN 978-0-8385-0565-6.
- ^ Loh HS, Watters K, Wilson CW (1 November 1973). "The effects of aspirin on the metabolic availability of ascorbic acid in human beings". Journal of Clinical Pharmacology. 13 (11): 480–486. doi:10.1002/j.1552-4604.1973.tb00203.x. PMID 4490672.
- ^ Basu TK (1982). "Vitamin C-aspirin interactions". International Journal for Vitamin and Nutrition Research. Supplement. 23: 83–90. PMID 6811490.
- ^ Ioannides C, Stone AN, Breacker PJ, Basu TK (December 1982). "Impairment of absorption of ascorbic acid following ingestion of aspirin in guinea pigs". Biochemical Pharmacology. 31 (24): 4035–4038. doi:10.1016/0006-2952(82)90652-9. PMID 6818974.
- ^ "Randomised Trial of Intravenous Streptokinase, Oral Aspirin, Both, or Neither Among 17,187 Cases of Suspected Acute Myocardial Infarction: Isis-2". The Lancet. 332 (8607): 349–360. August 1988. doi:10.1016/s0140-6736(88)92833-4. ISSN 0140-6736. PMID 2899772. S2CID 21071664.
- ^ Lewis HD, Davis JW, Archibald DG, Steinke WE, Smitherman TC, Doherty JE, et al. (August 1983). "Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina. Results of a Veterans Administration Cooperative Study". New England Journal of Medicine. 309 (7): 396–403. doi:10.1056/NEJM198308183090703. ISSN 0028-4793. PMID 6135989.
- ^ Di Bella S, Luzzati R, Principe L, Zerbato V, Meroni E, Giuffrè M, et al. (25 January 2022). "Aspirin and Infection: A Narrative Review". Biomedicines. 10 (2): 263. doi:10.3390/biomedicines10020263. ISSN 2227-9059. PMC 8868581. PMID 35203473.
- ^ Cao Y, Tan A (September 2020). "Aspirin might reduce the incidence of breast cancer: An updated meta-analysis of 38 observational studies". Medicine. 99 (38) e21917. doi:10.1097/md.0000000000021917. PMC 7505405. PMID 32957311.
- ^ Cook NR, Lee IM, Gaziano JM, Gordon D, Ridker PM, Manson JE, et al. (July 2005). "Low-dose aspirin in the primary prevention of cancer: the Women's Health Study: a randomized controlled trial". JAMA. 294 (1): 47–55. doi:10.1001/jama.294.1.47. PMID 15998890.
- ^ Miret Durazo CI, Zachariah Saji S, Rawat A, Motiño Villanueva AL, Bhandari A, Nurjanah T, et al. (September 2024). "Exploring Aspirin's Potential in Cancer Prevention: A Comprehensive Review of the Current Evidence". Cureus. 16 (9) e70005. doi:10.7759/cureus.70005. PMC 11498354. PMID 39445288.
- ^ "Aspirin Water Helps Plants". cybercemetery.unt.edu.
- ^ "Gardens: drug therapy for plants | Gardening advice". The Guardian. 31 January 2016.
- ^ "Priming Plant Defenses with Aspirin-like Compound: USDA ARS". www.ars.usda.gov.
- ^ a b c Edwards SH. "Nonsteroidal Anti-inflammatory Drugs: Aspirin". Merck Veterinary Manual. Archived from the original on 18 December 2016. Retrieved 20 January 2018.
- ^ a b "Analgesics (toxicity)". Merck. Archived from the original on 11 April 2015. Retrieved 19 January 2018.
- ^ Lappin MR, ed. (2001). Feline internal medicine secrets. Philadelphia: Hanley & Belfus. p. 160. ISBN 978-1-56053-461-7.
- ^ "Plants poisonous to livestock". Cornell University Department of Animal Science. Archived from the original on 16 August 2015. Retrieved 3 March 2016.
Further reading
[edit]- Desborough MJ, Keeling DM (June 2017). "The aspirin story - from willow to wonder drug". British Journal of Haematology. 177 (5): 674–683. doi:10.1111/bjh.14520. PMID 28106908. S2CID 46794541.
- McTavish JR (1987). "What's in a name? Aspirin and the American Medical Association". Bulletin of the History of Medicine. 61 (3): 343–66. JSTOR 44442097. PMID 3311247.
- Ling G (2005). "Aspirin". How Products Are Made. Vol. 1. Thomson Gale.
- Jeffreys D (2004). Aspirin: the Remarkable Story of a Wonder Drug. Bloomsbury.
External links
[edit] Media related to Aspirin at Wikimedia Commons
Media related to Aspirin at Wikimedia Commons
Aspirin
View on GrokipediaNames and Branding
Generic and Brand Names
The generic name for the drug commonly known as aspirin is acetylsalicylic acid, a salicylate compound used as a nonsteroidal anti-inflammatory drug (NSAID).[7] This name reflects its chemical structure, derived from acetylation of salicylic acid.[2] In medical and pharmaceutical contexts, "aspirin" is widely accepted as the nonproprietary name, particularly since it entered common usage before the establishment of formal international nonproprietary names (INN) by the World Health Organization, where pre-existing names like aspirin were retained due to their established recognition.[8] Aspirin was originally trademarked by Bayer in 1899 as a brand name for acetylsalicylic acid, but the term has since become genericized in many countries, allowing production by multiple manufacturers.[9] In the United States, it is available under numerous over-the-counter and prescription brand names, often formulated for specific uses such as pain relief, cardiovascular protection, or buffered to reduce stomach irritation.[3] Common U.S. brand names include:- Bayer Aspirin (low-dose and regular strength for cardiovascular and pain relief)
- Ecotrin (enteric-coated for reduced gastrointestinal side effects)
- Bufferin (buffered formulation)
- Durlaza (extended-release for antiplatelet therapy)
- Vazalore (liquid-filled capsules)
- Aspir 81 (low-dose for heart health)
- Arthritis Pain (targeted for inflammatory conditions)
- Aspirina (introduced in 2025 for pain relief, adapted from the Mexican market)[10]
Historical Naming and Trademarks
The name "Aspirin" was coined in 1899 by Heinrich Dreser, head of Bayer's pharmacological laboratory, deriving from the "a" prefix for acetyl, "spir" from the plant genus Spiraea (meadowsweet, a historical source of salicylic acid), and the common pharmaceutical suffix "-in".[13] This branding reflected the drug's chemical origins as acetylsalicylic acid, first synthesized by Felix Hoffmann at Bayer on August 10, 1897.[14] Bayer registered "Aspirin" as a trademark on March 6, 1899, at the Imperial Patent Office in Berlin (registration number 36433), marking it as a branded preparation of acetylsalicylic acid rather than a generic term.[14] The company quickly expanded international protection, filing for a U.S. patent on the synthesis process in 1898 (granted as U.S. Patent 644,077 in 1900) and a British patent in 1899 (GB 189909123A).[14][15] By the early 20th century, "Aspirin" had become Bayer's flagship trademark, sold initially as a powder in glass bottles and later in tablet form from 1900 onward, establishing global recognition for the pain-relief drug.[13] However, World War I disrupted Bayer's control, as Allied powers seized German assets, including intellectual property. Under the 1919 Treaty of Versailles, Germany renounced industrial property rights in favor of the Allied nations, leading to the confiscation of Bayer's trademarks in multiple countries.[16] In the United States, the Alien Property Custodian seized Bayer's U.S. operations in 1917, auctioning the Aspirin trademark and related patents to Sterling Drug Inc. for $5.3 million in 1918 (equivalent to about $100 million today).[17] This loss, compounded by the expiration of the core U.S. patent in 1917, allowed generic manufacturers to produce and market acetylsalicylic acid under the "Aspirin" name, transforming it into a genericized term in the U.S. and several other nations by the 1920s.[15][18] Post-war, Bayer retained the Aspirin trademark in Germany and some other markets but faced ongoing challenges elsewhere, where the name entered the public domain and lost exclusive association with the brand.[14] Efforts to repurchase rights began in the interwar period and continued into the late 20th century; notably, in 1994, Bayer reacquired the U.S., Canadian, and Puerto Rican Aspirin trademarks from SmithKline Beecham (via its purchase of Sterling Winthrop's over-the-counter business) for $1 billion as part of a broader deal, restoring exclusive use of "Bayer Aspirin" in those territories.[17][13] Today, while Bayer holds the trademark in over 100 countries, "aspirin" remains a generic descriptor for acetylsalicylic acid in places like the U.S., illustrating the enduring impact of wartime asset seizures on pharmaceutical branding.[14]Chemical and Physical Properties
Chemical Structure and Synthesis
Aspirin, chemically known as acetylsalicylic acid, has the molecular formula C₉H₈O₄ and a molecular weight of 180.157 g/mol.[1] It is classified as a benzoic acid derivative, specifically 2-(acetyloxy)benzoic acid according to its IUPAC name.[1] The core structure consists of a benzene ring substituted with a carboxylic acid group (-COOH) at position 1 and an acetoxy group (-OCOCH₃) at position 2, making it an ester of salicylic acid and acetic acid. This ortho-substituted arrangement is crucial for its pharmacological properties, as the acetoxy group modifies the phenolic hydroxyl of salicylic acid, reducing gastric irritation while preserving anti-inflammatory activity.[7] The molecule features key functional groups: the carboxylic acid, which imparts acidity (pKa ≈ 3.5), the ester linkage, and the aromatic ring, contributing to its stability and UV absorption above 290 nm.[1] In its solid form, aspirin exists as colorless or white crystals, often in monoclinic or needle-like morphology, with no odor or a slight acidic taste.[1] The structure can be represented as: where the benzene ring is attached to the carboxylic acid and the ester side chain at adjacent positions.[1] The synthesis of aspirin involves the acetylation of salicylic acid, a process first achieved in pure form by Felix Hoffmann at Bayer in 1897 to address the tolerability issues of salicylic acid.[19] Hoffmann heated salicylic acid with acetic anhydride, yielding acetylsalicylic acid through esterification of the phenolic hydroxyl group.[19] This reaction proceeds via nucleophilic acyl substitution, where the phenolate oxygen attacks the carbonyl of acetic anhydride, releasing acetate as a leaving group.[20] Industrially, the synthesis is conducted by mixing salicylic acid with acetic anhydride (often in slight molar excess) and a catalyst such as sulfuric acid, heating the mixture to 70–90 °C to complete the reaction, then cooling to promote crystallization, followed by filtration, washing with water, and drying to yield high-purity product.[21] Alternative methods, such as using acetyl chloride, have been explored but are less common due to the corrosiveness of the reagent.[20] This straightforward acetylation remains the primary route for commercial production, patented by Bayer in 1899.[19] Synthesis of aspirin is not safe to perform at home. The process requires handling hazardous reagents, including acetic anhydride (flammable, corrosive, causes severe skin burns and eye damage, and produces irritating vapors that require a fume hood for safe handling), salicylic acid (an irritant), and sulfuric acid (highly corrosive, causes severe skin burns and eye damage). Home environments typically lack the necessary safety equipment, such as fume hoods, proper ventilation, and personal protective gear, increasing the risk of chemical burns, respiratory irritation, eye damage, and exposure to toxic fumes. Additionally, aspirin synthesized without professional purification, quality control, and testing is likely to contain impurities or contaminants and is unsafe for consumption.[22][23][24]Physical Properties and Polymorphism
Acetylsalicylic acid, the active ingredient in aspirin, appears as a white, crystalline powder or as crushed, irregular-shaped crystals in its commercial form. It has a melting point of 134–136 °C and a density of approximately 1.35–1.40 g/cm³. The compound is weakly acidic with a pKa of 3.5 at 25 °C and exhibits low solubility in water, approximately 3–4.6 mg/mL at 25 °C or 0.33–0.46 g/100 g at 298 K, though solubility increases with temperature to about 10 mg/mL at 37 °C. It is more soluble in organic solvents such as ethanol (around 20 g/100 g), chloroform (6 g/100 g), and ethyl ether.[20][25][26] Aspirin is known for its polymorphism, with four known crystal forms, though only a few are stable under ambient conditions. The most stable and commercially predominant form is Form I, first characterized in 1964 and confirmed in 1985, featuring a monoclinic crystal structure with specific hydrogen bonding patterns that contribute to its thermodynamic stability. Form II, initially observed in the 1960s but fully characterized in 2005, is metastable and converts to Form I over time; it differs in molecular arrangement, with altered layer stacking and orientation of the hydroxyl group, leading to distinct spectroscopic signatures.[26][27] A third ambient polymorph, Form IV, was discovered in 2017 through crystallization from the melt, exhibiting a unique structure determined via X-ray powder diffraction and solid-state NMR, though it is less stable than Form I. High-pressure conditions yield Form III at around 2 GPa, which reverts to Form I upon decompression. Polymorphic differences significantly affect physical behaviors: Form II displays a higher dissolution rate—up to 50% faster than Form I in aqueous media—due to variations in surface energy and hydrogen bonding, impacting bioavailability and tablet compaction properties, while Form I's lower energetic state ensures its prevalence in pharmaceutical production. No hydrates of aspirin have been identified.[26][28][29]Stability and Degradation
Acetylsalicylic acid is stable in dry air but gradually hydrolyzes to salicylic acid and acetic acid when exposed to moisture. In solid dosage forms, this hydrolysis is significantly accelerated by higher relative humidity (RH), as moisture facilitates the hydrolytic cleavage of the ester bond. To minimize degradation and maintain product integrity, storage at low relative humidity in tightly closed containers protected from moisture is recommended.[30][20]History
Early Discovery and Development
The use of willow bark for pain relief and fever reduction dates back more than 3,500 years, with evidence from Sumerian and Egyptian civilizations employing it as an analgesic and antipyretic.[31] In ancient Greece, Hippocrates prescribed willow bark preparations in the 5th century BC to alleviate labor pains and reduce fevers, marking one of the earliest documented medical applications.[32] This natural remedy's active component, salicin, was isolated in 1828 by German pharmacist Johann Andreas Buchner from willow bark extracts, while Italian chemist Raffaele Piria derived salicylic acid from it in 1838, providing the foundation for subsequent chemical investigations into salicylates.[33] By the mid-19th century, salicylic acid—derived from salicin hydrolysis—was recognized for its potent anti-inflammatory and analgesic properties, but its use was limited by severe gastric irritation.[33] In 1853, French chemist Charles Frédéric Gerhardt first synthesized acetylsalicylic acid (ASA) by reacting sodium salicylate with acetyl chloride, though the product was impure and not pursued therapeutically.[34] Efforts to mitigate salicylic acid's side effects continued, culminating in 1897 when Felix Hoffmann, a chemist at Friedrich Bayer & Co. in Germany, successfully acetylated salicylic acid to produce a stable, pure form of ASA on August 10, aiming to create a more tolerable alternative for his father's rheumatism.[19] This synthesis involved treating salicylic acid with acetic anhydride, yielding the compound now known as aspirin.[33] The development of aspirin at Bayer was a collaborative effort, with Arthur Eichengrün, head of the therapeutics department, later claiming he directed Hoffmann's work to systematically test acetylated salicylates for reduced toxicity. Eichengrün's contributions were suppressed in official Bayer narratives during the Nazi era due to his Jewish heritage and only gained wider recognition after his death in 1949 through his published account and subsequent historical analyses.[19][35] Pharmacologist Heinrich Dreser evaluated the compound's effects starting in late 1897, confirming its efficacy in animal models and human trials for pain and fever without the harsh gastrointestinal impact of salicylic acid.[19] By 1898, clinical evaluations in European clinics demonstrated aspirin's antipyretic and antirheumatic benefits, setting the stage for its broader pharmaceutical application.[19]Commercialization and Historical Uses
Bayer introduced Aspirin to the market in 1899 as a stable, less irritating alternative to salicylic acid for pain relief and fever reduction. On August 10, 1897, chemist Felix Hoffmann at Bayer's laboratory in Wuppertal, Germany, synthesized the first pure and stable form of acetylsalicylic acid, motivated in part by his father's arthritis.[36] The company registered "Aspirin" as a trademark on March 6, 1899, with the Imperial Patent Office in Berlin, deriving the name from "a" for acetyl, "spir" from the Spiraea plant (a source of salicin), and the common drug suffix "-in."[14] Initially marketed as a powder, it transitioned to tablet form in 1900, with Bayer securing a U.S. patent (No. 644,077) that year to protect its production process. Early clinical testing, directed by Arthur Eichengrün and confirmed by Heinrich Dreser, demonstrated its efficacy against rheumatism and fever, leading to its rapid adoption as an over-the-counter remedy.[19] Bayer's marketing efforts propelled Aspirin to global prominence, making it one of the first mass-marketed pharmaceuticals. The company launched an aggressive international campaign, emphasizing its purity and reliability, which resulted in Aspirin becoming a bestseller in pharmacies worldwide by the early 1900s.[9] By 1950, it earned a Guinness World Record as the most frequently sold painkiller, reflecting sales driven by direct-to-consumer advertising in print media.[9] However, World War I disrupted Bayer's monopoly; in 1917, the U.S. government seized Bayer's American assets, including the Aspirin trademark and patent, allowing generic production and leading to Bayer regaining rights in 1995 through the acquisition of Sterling Winthrop's over-the-counter business after legal and commercial efforts.[14][17] Despite these setbacks, Aspirin maintained strong brand association, with surveys in the 2010s showing over 60% of U.S. consumers and nearly 80% in Germany linking it to Bayer.[36] Historically, Aspirin's uses evolved from ancient precedents to modern applications, building on millennia of willow bark remedies for analgesia and antipyresis. Upon commercialization, Bayer promoted it primarily for headaches, neuralgia, rheumatism, and influenza symptoms, with the first clinical report in 1899 confirming its antipyretic and analgesic effects without the gastric irritation of salicylic acid.[19] During World War I, it saw widespread military use for treating aches, fevers, and wounds among soldiers.[37] By the mid-20th century, its anti-inflammatory properties were recognized for conditions like arthritis, and in the 1970s, discoveries of its inhibition of prostaglandin synthesis expanded its role in preventing blood clots, marking a shift toward cardiovascular prophylaxis.[9] The World Health Organization added it to its Essential Medicines List in 1977, underscoring its enduring utility for pain, inflammation, and emerging preventive roles.[38][39]Pharmacology
Mechanism of Action
Aspirin, or acetylsalicylic acid, exerts its primary pharmacological effects through irreversible inhibition of the cyclooxygenase (COX) enzymes, which are critical in the biosynthesis of prostaglandins and thromboxane from arachidonic acid.[40] In 1971, John R. Vane demonstrated that aspirin and related non-steroidal anti-inflammatory drugs (NSAIDs) suppress the formation of prostaglandins, mediators of pain, fever, and inflammation, by blocking COX activity in tissues such as guinea-pig lung homogenates.[41] This discovery provided the foundational understanding of aspirin's anti-inflammatory, analgesic, and antipyretic actions, earning Vane the Nobel Prize in Physiology or Medicine in 1982.[42] The inhibition occurs via covalent acetylation of a serine residue in the active site of the COX enzymes: serine 529 in COX-1 and serine 516 in COX-2.[43] Aspirin transfers its acetyl group to this serine, sterically hindering the binding of arachidonic acid and preventing the enzyme's peroxidase and cyclooxygenase activities, which convert arachidonic acid to the unstable intermediate prostaglandin H2 (PGH2).[40] Unlike reversible COX inhibitors, aspirin's acetylation leads to permanent inactivation, requiring new enzyme synthesis for recovery of activity; this effect is particularly pronounced in platelets, which lack nuclei and thus cannot replenish COX-1.[43] Aspirin is approximately 10- to 100-fold more potent against COX-1 than COX-2, though at higher doses it inhibits both isoforms.[43] This selective and irreversible mechanism underlies aspirin's diverse therapeutic roles. By inhibiting COX-1 in platelets, aspirin reduces thromboxane A2 production, a potent vasoconstrictor and platelet aggregator, thereby providing sustained antiplatelet effects that last for the platelet's lifespan (about 7-10 days).[40] In inflammatory contexts, suppression of COX-2-derived prostaglandins like PGE2 diminishes vasodilation, edema, and pain sensitization, while antipyretic effects arise from reduced PGE2-mediated elevation of the hypothalamic temperature set point.[42] At low doses (e.g., 75-325 mg daily), the impact is predominantly on COX-1 with minimal gastrointestinal effects, whereas higher doses engage both enzymes more broadly.[43]Pharmacokinetics
Aspirin, or acetylsalicylic acid, exhibits rapid and nearly complete absorption following oral administration, primarily in the stomach and upper small intestine via passive diffusion as the undissociated form, with peak plasma concentrations of its primary metabolite, salicylic acid, occurring within 1 to 2 hours.[1] Bioavailability ranges from 80% to 100%, though it is reduced by presystemic hydrolysis in the gastrointestinal tract and liver, where approximately 50% of the dose is converted to salicylic acid during absorption; factors such as gastric pH, food intake, and formulation (e.g., enteric-coated tablets) can delay or alter this process, with absorption half-life typically 5 to 16 minutes.[44][2] Once absorbed, aspirin is quickly distributed throughout the body, including crossing the blood-brain barrier, placenta, and into breast milk, with a volume of distribution of approximately 0.15 L/kg for aspirin itself and up to 0.17 L/kg for salicylic acid at therapeutic doses.[45] Salicylic acid, the active form, is highly bound to plasma proteins (50-90%, primarily albumin), with binding decreasing at higher concentrations due to saturation, leading to increased free drug and potential toxicity; this concentration-dependent binding contributes to the drug's nonlinear pharmacokinetics.[1] The elimination half-life of intact aspirin is short, approximately 15 to 20 minutes, primarily due to rapid hydrolysis by esterases in plasma, erythrocytes, and tissues.[1] Metabolism occurs predominantly in the liver, where aspirin is deacetylated to salicylic acid, which then undergoes conjugation via glycine (forming salicyluric acid, ~75% of dose) or glucuronic acid (forming phenolic and acyl glucuronides, ~25%), with minor pathways producing gentisic acid; these processes exhibit saturable kinetics at higher doses, resulting in disproportionate increases in plasma levels.[2] Excretion is mainly renal, with 80-100% of the dose eliminated in urine as metabolites and free salicylic acid over 48 hours, primarily through glomerular filtration and active tubular secretion; clearance is highly pH-dependent, increasing 10- to 20-fold in alkaline urine (pH >7) due to ionized forms being less reabsorbed, while acidic urine (pH <6) reduces excretion and prolongs half-life.[1] The half-life of salicylic acid is dose-dependent, ranging from 2 to 3 hours at low antiplatelet doses (e.g., 81 mg) to 15 to 30 hours at high analgesic doses (e.g., >2 g), reflecting zero-order elimination at therapeutic levels above 150 mcg/mL.[45]Medical Uses
Pain, Fever, and Inflammation
Aspirin, or acetylsalicylic acid, is a nonsteroidal anti-inflammatory drug (NSAID) primarily utilized for its analgesic, antipyretic, and anti-inflammatory properties, making it effective in managing mild to moderate pain, reducing fever, and alleviating inflammation associated with various conditions.[2] It is commonly employed to relieve pain from headaches, toothaches, menstrual cramps, muscle aches, and minor arthritis symptoms, often providing relief within 30 minutes to an hour after oral administration.[46] For fever reduction, aspirin lowers body temperature by acting on the hypothalamus, typically in doses of 325–650 mg every 4–6 hours as needed for adults.[2] Its anti-inflammatory effects are particularly beneficial in rheumatic conditions such as osteoarthritis and rheumatoid arthritis, where it helps reduce joint swelling and stiffness at higher doses of 3–5 grams per day in divided doses.[46] The therapeutic actions of aspirin for pain, fever, and inflammation stem from its irreversible inhibition of cyclooxygenase (COX) enzymes, specifically COX-1 and COX-2, which are responsible for the synthesis of prostaglandins—lipid mediators that sensitize pain receptors, elevate the hypothalamic temperature set point, and promote inflammatory responses.[42] This mechanism, first elucidated by John Vane in 1971, prevents the formation of pro-inflammatory prostaglandins like PGE2 and PGI2, thereby blocking the peripheral and central pathways that amplify nociception and pyrexia.[42] At anti-inflammatory doses, aspirin also modulates the lipoxygenase pathway, leading to the production of anti-inflammatory mediators such as lipoxins, resolvins, and maresins, which further resolve inflammation.[2] Clinical efficacy for these indications is well-established, with aspirin demonstrating superiority over placebo in reducing pain intensity, fever, and inflammatory symptoms in conditions like upper respiratory tract infections and acute musculoskeletal injuries.[47] For instance, single doses of 500–1000 mg have been shown to effectively lower fever and associated discomfort comparably to acetaminophen, with onset of action within 15–30 minutes and duration of 4–6 hours.[48] In chronic inflammatory diseases, sustained use at therapeutic levels achieves approximately 90% inhibition of COX activity, providing symptomatic relief, though it is generally less potent than modern NSAIDs for severe inflammation due to its gastrointestinal side effects.[2] Despite its efficacy, aspirin should be used cautiously in children and adolescents with viral illnesses due to the risk of Reye's syndrome, and its antipyretic use is not recommended for fever alone in otherwise healthy individuals.[46]Cardiovascular Prevention
Low-dose aspirin (typically 75–100 mg daily) serves as the gold standard for secondary cardiovascular prevention, supported by decades of large-scale randomized controlled trials and meta-analyses demonstrating reductions in hard endpoints such as vascular mortality and recurrent events after myocardial infarction or stroke. Aspirin has been a cornerstone therapy for cardiovascular prevention, particularly in secondary prevention among individuals with established atherosclerotic cardiovascular disease (ASCVD), where it reduces the risk of recurrent myocardial infarction, stroke, and vascular death by irreversibly inhibiting cyclooxygenase-1 (COX-1) to prevent platelet aggregation.[49] In contrast, its role in primary prevention—among those without prior ASCVD—has evolved, with recent evidence indicating that the modest reduction in ischemic events is often offset by increased bleeding risks, leading to more selective recommendations.[5] Low-dose regimens, typically 75–100 mg daily, are standard for both contexts to balance efficacy and safety.[50] For secondary prevention, aspirin's benefits were firmly established by the ISIS-2 trial, a landmark randomized controlled trial involving 17,187 patients with suspected acute myocardial infarction, which showed that oral aspirin (162.5 mg daily) reduced 5-week vascular mortality by 23% compared to placebo (9.0% vs. 11.8%; p<0.00001), with additive effects when combined with streptokinase.[49] A subsequent collaborative meta-analysis by the Antithrombotic Trialists' Collaboration, pooling data from 16 secondary prevention trials with over 17,000 patients, confirmed a 25% proportional reduction in serious vascular events (nonfatal myocardial infarction, nonfatal stroke, or vascular death; 6.7% annual event rate with aspirin vs. 8.2% with control; p<0.0001), establishing aspirin as a foundational antiplatelet agent.[49] Current guidelines from the American Heart Association (AHA) and American College of Cardiology (ACC), updated in 2023 for chronic coronary disease management, recommend indefinite low-dose aspirin therapy (class 1 recommendation) for most patients with ASCVD, including post-myocardial infarction or revascularization, barring contraindications like recent major bleeding or high-risk features.[49] Dosing comparisons, such as 81 mg versus 325 mg daily, show equivalent efficacy in reducing recurrent events without differences in major bleeding rates.[51] In primary prevention, early evidence from the 2009 Antithrombotic Trialists' meta-analysis of six trials involving 95,000 participants suggested a smaller 12% reduction in serious vascular events (0.51% annual absolute risk reduction; rate ratio 0.88, 95% CI 0.82–0.94), but with a doubling of major extracranial bleeding (0.10% annual absolute increase; rate ratio 1.54, 95% CI 1.30–1.82).[49] However, three large contemporary trials—ASPREE (16,703 elderly participants ≥70 years), ARRIVE (12,546 moderate-risk adults), and ASCEND (15,480 adults with diabetes)—collectively demonstrated no significant net benefit: ASPREE found no reduction in composite cardiovascular events (hazard ratio 0.95, 95% CI 0.83–1.08) but a 38% increase in major bleeding (hazard ratio 1.38, 95% CI 1.18–1.62); ARRIVE showed similar null results for the primary composite endpoint (hazard ratio 0.96, 95% CI 0.81–1.13) with doubled gastrointestinal bleeding; and ASCEND reported a 12% reduction in serious vascular events (hazard ratio 0.88, 95% CI 0.79–0.97) but a 29% increase in major bleeding (hazard ratio 1.29, 95% CI 1.09–1.52), resulting in no difference in net clinical benefit.[52] These findings prompted the U.S. Preventive Services Task Force (USPSTF) 2022 update, which recommends against initiating low-dose aspirin for primary prevention in adults aged 60 years or older (grade D) due to bleeding harms exceeding ischemic benefits, and suggests individualized decisions for those aged 40–59 years with a 10-year ASCVD risk ≥10% (grade C), emphasizing shared decision-making on bleeding risks.[5] Population-level trends reflect this shift, with U.S. aspirin use for primary prevention declining from 20.6% in 2019 to 15.7% in 2023.[53] Overall, while aspirin's role in secondary prevention remains robust, primary prevention is now reserved for carefully selected high-risk individuals without elevated bleeding potential.[50]Cancer Prevention
Aspirin has been investigated extensively for its potential role in primary cancer prevention, particularly in reducing the incidence of colorectal cancer (CRC) through long-term use. Multiple randomized controlled trials (RCTs) and meta-analyses have demonstrated that regular aspirin intake, typically at low doses (75-325 mg daily), is associated with a reduced risk of CRC development, with benefits emerging after several years of use. For instance, a long-term follow-up of five RCTs involving over 14,000 participants showed that 5-10 years of aspirin use reduced the 20-year risk of CRC incidence by 24% (hazard ratio [HR] 0.76, 95% CI 0.60-0.96) and CRC mortality by 49% (HR 0.51, 95% CI 0.35-0.74).[54] This effect is attributed to aspirin's anti-inflammatory properties, which inhibit prostaglandin synthesis and COX-2 expression in colonic tissues, though detailed mechanisms are covered elsewhere. However, the overall benefit for total cancer incidence across all sites remains modest or inconsistent in broader meta-analyses, with one review of 29 RCTs (200,679 participants) finding no significant reduction (relative risk [RR] 1.01, 95% CI 0.97-1.04).[55] Evidence is strongest for CRC prevention in average-risk populations and those with hereditary predispositions. A 2020 meta-analysis of 118 observational studies across 18 cancer types reported a 27% reduction in CRC incidence (HR 0.73, 95% CI 0.69-0.78) with consistent aspirin use, with dose-dependent effects: 75-100 mg/day yielding a 10% risk reduction and 325 mg/day a 35% reduction. In high-risk groups, such as individuals with Lynch syndrome, the CAPP2 trial (861 participants) demonstrated that 600 mg daily aspirin for at least 2 years reduced CRC incidence by 63% over 55 months (HR 0.37, 95% CI 0.11-1.26). The 2025 CaPP3 trial (1,879 participants) further confirmed that low-dose aspirin (75-100 mg daily) reduces CRC risk by approximately 50% in Lynch syndrome patients, with efficacy comparable to higher doses and leading to updated UK guidelines (e.g., NICE) recommending daily low-dose aspirin (75-100 mg) for this population to balance benefits and bleeding risks.[56] Recent network meta-analyses (2023-2025) reinforce low-dose aspirin's superiority over placebo or higher doses for preventing CRC and adenoma recurrence, with one 2024 analysis of 13 RCTs showing low-dose (<300 mg/day) aspirin reducing adenoma risk more effectively than high-dose (RR 0.68 vs. 0.82). A 2025 meta-analysis of cohort studies further supported a 15-20% overall reduction in cancer incidence, driven primarily by gastrointestinal sites.[57] For other cancers, the evidence is weaker and less consistent. Aspirin shows potential for reducing esophageal, gastric, and pancreatic cancer risks, with meta-analyses indicating 20-30% reductions in incidence (e.g., RR 0.72 for esophageal cancer in a 2023 umbrella review of RCTs and cohorts), but no clear benefits for breast, prostate, or lung cancers. The U.S. Preventive Services Task Force (USPSTF) previously (2016) endorsed low-dose aspirin for CRC prevention alongside cardiovascular benefits in adults aged 50-59 at increased risk, based on moderate-quality evidence. However, the 2022 USPSTF update excluded cancer prevention from its assessment due to insufficient long-term data to alter the net benefit-harm balance, emphasizing bleeding risks (e.g., RR 1.44 for major gastrointestinal bleeding) that may outweigh advantages in older adults or low-risk groups. Current guidelines, such as those from the American Cancer Society, suggest discussing aspirin's role with providers for CRC prevention in select high-risk individuals, weighing personal bleeding history against potential gains.Other Therapeutic Applications
Aspirin has established roles in several specialized medical conditions beyond its primary indications for analgesia, antipyresis, anti-inflammatory effects, cardiovascular protection, and cancer prevention. One key application is in the prevention of preeclampsia, a hypertensive disorder of pregnancy that can lead to maternal and fetal complications. Low-dose aspirin (typically 81 mg daily) is recommended for pregnant individuals at high risk, such as those with a history of preeclampsia, multiple gestation, chronic hypertension, diabetes, or renal disease. Initiation between 12 and 16 weeks of gestation (optimally before 16 weeks) and continuation until delivery has been shown to reduce the risk of preeclampsia by 24%, preterm birth by 14%, and intrauterine growth restriction by 20% in high-risk populations.[58] This regimen improves placental blood flow by inhibiting thromboxane production and platelet aggregation, thereby mitigating endothelial dysfunction.[59] In pediatric cardiology, aspirin is a cornerstone of therapy for Kawasaki disease, an acute vasculitis that primarily affects children under five years old and can lead to coronary artery aneurysms if untreated. During the acute febrile phase, moderate-dose aspirin (30-50 mg/kg/day divided every 6 hours) is administered for its anti-inflammatory and antipyretic properties to reduce fever, rash, and mucosal inflammation, often in combination with intravenous immunoglobulin (IVIG) at 2 g/kg as a single infusion.[60] This approach, when given within 10 days of symptom onset, decreases the incidence of coronary artery abnormalities from approximately 25% to less than 5%.[61] Following fever resolution, low-dose aspirin (3-5 mg/kg/day) is continued as antiplatelet therapy to prevent thrombosis in affected vessels, typically for 6-8 weeks or longer if echocardiographic abnormalities persist.[61] Aspirin also plays a supportive role in managing acute rheumatic fever (ARF), an autoimmune inflammatory condition triggered by group A streptococcal infection, which can cause carditis, arthritis, and chorea. For patients with arthritis or mild carditis, high-dose aspirin (60-100 mg/kg/day in divided doses) is used to alleviate joint pain, swelling, and fever, often leading to rapid symptom resolution within days.[62] This dosing targets the inflammatory response without addressing the underlying streptococcal etiology, for which penicillin remains the primary treatment. In cases of severe carditis with heart failure, corticosteroids may be preferred over aspirin to avoid fluid retention, but aspirin is still employed adjunctively for non-cardiac manifestations.[62] Long-term, low-dose aspirin may be considered for secondary prevention of rheumatic heart disease complications in select patients.[63] Emerging evidence supports aspirin's use in other inflammatory conditions, such as pericarditis, where it serves as first-line anti-inflammatory therapy at doses of 650-1000 mg every 6-8 hours for 1-2 weeks, tapered based on symptom response, reducing recurrence rates compared to placebo. However, its application in neuropsychiatric disorders, such as mood stabilization in bipolar disorder or adjunctive treatment in schizophrenia via anti-inflammatory mechanisms, remains investigational and not routinely recommended outside clinical trials.[64] Overall, these applications leverage aspirin's multifaceted actions on cyclooxygenase inhibition, platelet function, and inflammation, but dosing must be tailored to minimize risks like gastrointestinal bleeding or Reye's syndrome in children.Administration and Dosages
Available Formulations
Aspirin, or acetylsalicylic acid, is formulated in multiple dosage forms to accommodate various administration routes, absorption requirements, and patient tolerances, primarily for oral, rectal, and intravenous use.[2] These formulations include immediate-release options for rapid onset and modified-release variants to minimize gastrointestinal irritation.[3] The most common oral formulations are uncoated tablets, which provide quick dissolution and absorption, typically available in strengths of 325 mg and 500 mg.[2] Enteric-coated tablets, designed to dissolve in the intestine rather than the stomach to reduce gastric side effects, are widely used and come in low-dose (81 mg) and standard strengths (325 mg, 500 mg, 650 mg).[2][65] Chewable tablets, often in 81 mg for cardiovascular prophylaxis, allow for faster absorption when masticated.[2] Effervescent tablets dissolve in water for easier ingestion, while liquid-filled capsules and extended-release capsules (e.g., 162.5 mg over 24 hours) offer alternatives for patients with swallowing difficulties.[3] Buffered formulations, incorporating antacids like magnesium oxide or calcium carbonate, aim to neutralize stomach acid and lessen mucosal damage, though evidence on superior tolerability varies.[66] Rectal suppositories provide an alternative for patients unable to take oral medications, available in strengths ranging from 60 mg to 600 mg, with absorption occurring via the rectal mucosa.[2] Intravenous aspirin is reserved for acute settings, such as in hospitals for rapid platelet inhibition, and demonstrates more consistent bioavailability compared to oral forms in some studies.[67]| Formulation Type | Common Strengths | Key Features |
|---|---|---|
| Uncoated Tablet | 325 mg, 500 mg | Immediate release for fast absorption[2] |
| Enteric-Coated Tablet | 81 mg, 325 mg, 500 mg, 650 mg | Protects stomach lining; delayed release[2] |
| Chewable Tablet | 81 mg | Rapid onset when chewed; suitable for acute use[2] |
| Effervescent Tablet | Varies (e.g., 325 mg) | Dissolves in water; easier for some patients[3] |
| Extended-Release Capsule | 162.5 mg | Prolonged release over 24 hours[3] |
| Buffered Tablet | 325 mg (with antacids) | Reduces gastric pH changes[66] |
| Suppository | 60 mg, 120 mg, 200 mg, 300 mg, 600 mg | Rectal administration for non-oral needs[2] |
| Intravenous | Varies (e.g., 500 mg doses) | Hospital use for immediate effect[67] |
Recommended Dosages
Recommended dosages of aspirin (acetylsalicylic acid) vary by indication, patient age, and clinical guidelines, with lower doses typically used for antiplatelet effects and higher doses for analgesic, antipyretic, or anti-inflammatory purposes.[68] For adults seeking relief from mild to moderate pain or fever, the standard oral dose is 325 to 650 mg every 4 to 6 hours as needed, not exceeding 4 grams per 24 hours.[68] Rectal administration may be used at 300 to 600 mg every 4 hours for similar indications, also capped at 4 grams daily.[68] In anti-inflammatory applications, such as rheumatoid arthritis or osteoarthritis, dosing is individualized to achieve therapeutic plasma salicylate levels of 150 to 300 mcg/mL, often starting at 3 grams per day orally in divided doses (three to four times daily) and adjusting up to 4 to 5 grams per day based on response and tolerance.[68] The Arthritis Foundation recommends up to 3,000 mg per day in divided doses for arthritis management, taken with food or an antacid to minimize gastrointestinal irritation.[69] For cardiovascular prevention, low-dose aspirin is used at 75 to 100 mg orally once daily, with 81 mg being a common formulation in the United States. For primary prevention, low-dose aspirin is not routinely recommended due to bleeding risks often outweighing benefits. According to the 2022 USPSTF recommendation, the decision to initiate low-dose aspirin should be individualized for adults aged 40 to 59 years with an estimated 10-year cardiovascular disease risk of ≥10% who are not at increased risk for bleeding, as the net benefit is small; initiation is recommended against for adults aged 60 years or older. Some studies and expert reviews suggest that coronary artery calcium (CAC) scoring may further personalize the decision by identifying individuals with subclinical atherosclerosis (such as CAC scores ≥100, particularly ≥400) who are more likely to derive net benefit from low-dose aspirin if bleeding risk is low, while those with CAC = 0 generally do not benefit and may experience net harm unless their ASCVD risk is substantially elevated. In secondary prevention after myocardial infarction or ischemic stroke, doses range from 75 to 325 mg daily, often starting with 160 to 325 mg immediately post-event.[5][70][68] Pediatric use of aspirin is generally contraindicated for pain, fever, or viral illnesses due to the risk of Reye's syndrome, a rare but serious condition affecting the brain and liver, as advised by the FDA, CDC, and American Academy of Pediatrics.[71] Exceptions include specific conditions like juvenile rheumatoid arthritis (80 to 130 mg/kg/day orally in divided doses, targeting 150 to 300 mcg/mL plasma levels) or Kawasaki disease (initially 80 to 100 mg/kg/day, then 1 to 5 mg/kg/day maintenance).[68] All pediatric dosing requires medical supervision, and aspirin should be avoided in children and teenagers recovering from chickenpox or flu-like symptoms.[4]| Indication | Adult Dosage | Pediatric Dosage | Maximum Daily Dose | Source |
|---|---|---|---|---|
| Pain/Fever | 325–650 mg orally every 4–6 hours | Avoid except under medical advice (≥12 years: same as adult) | 4 g | [68] |
| Inflammation/Arthritis | 3–5 g/day orally in divided doses (target 150–300 mcg/mL plasma) | 80–130 mg/kg/day orally in divided doses (JRA) | Individualized, up to 5 g | [68]; [69] |
| Cardiovascular Prevention (Primary) | 75–100 mg orally once daily | Not routinely recommended | N/A | [5] |
| Kawasaki Disease | N/A | Initial: 80–100 mg/kg/day; Maintenance: 1–5 mg/kg/day | Individualized | [68] |
Adverse Effects and Safety
Contraindications and Interactions
Aspirin is contraindicated in individuals with a known hypersensitivity to aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs), as this can precipitate severe allergic reactions, including anaphylaxis.[72] It is also contraindicated in patients with active peptic ulcer disease or a history of gastrointestinal bleeding, due to the drug's inhibitory effect on prostaglandin synthesis, which compromises the protective gastric mucosal barrier and heightens the risk of hemorrhage.[11] In children and teenagers recovering from viral infections such as influenza or chickenpox, aspirin use is contraindicated because of the association with Reye's syndrome, a rare but potentially fatal condition involving liver and brain damage.[46] Additionally, aspirin is contraindicated during the third trimester of pregnancy, as it can inhibit labor, prolong gestation, increase bleeding risks for both mother and fetus, and potentially cause premature closure of the ductus arteriosus in the fetus.[72] Patients with severe hepatic or renal impairment should avoid aspirin, as impaired metabolism and excretion can lead to salicylate accumulation and toxicity.[2] Precautions are advised for several patient populations to mitigate risks. Individuals with a history of asthma, particularly those with nasal polyps or aspirin-exacerbated respiratory disease, require caution, as aspirin can trigger bronchospasm and acute asthma attacks in up to 20% of such patients.[11] Elderly patients face heightened risks of gastrointestinal bleeding and renal impairment with aspirin use, necessitating lower doses and close monitoring.[72] Those with bleeding disorders, such as hemophilia or von Willebrand disease, or concurrent use of anticoagulants should use aspirin judiciously, as its irreversible inhibition of cyclooxygenase-1 (COX-1) prolongs bleeding time.[46] Heavy alcohol consumption (more than three drinks daily) exacerbates gastrointestinal irritation and bleeding potential when combined with aspirin.[11] Aspirin should be discontinued at least 7-10 days prior to elective surgery to reduce perioperative bleeding risks, and patients should inform surgeons of recent use.[2] Aspirin engages in numerous drug interactions, primarily through its effects on platelet aggregation, renal function, and gastrointestinal mucosa. Concomitant use with other NSAIDs, such as ibuprofen or naproxen, increases the risk of gastrointestinal ulceration and bleeding; ibuprofen, in particular, can competitively inhibit aspirin's antiplatelet effects when taken regularly, potentially reducing cardiovascular protection.[72] Anticoagulants like warfarin or direct oral anticoagulants (e.g., apixaban) heighten bleeding risks, with combined therapy requiring careful INR monitoring and dose adjustments.[73] Selective serotonin reuptake inhibitors (SSRIs), such as sertraline, amplify the risk of upper gastrointestinal bleeding by up to twofold through synergistic effects on platelet function.[2] Methotrexate toxicity is enhanced by aspirin, as it displaces the drug from plasma proteins and reduces its renal clearance, necessitating dose reductions in patients with rheumatoid arthritis.[46] Corticosteroids and alcohol further elevate gastrointestinal adverse events, while diuretics (e.g., furosemide) may experience diminished efficacy due to aspirin's interference with renal prostaglandin-mediated natriuresis.[73] Beta-blockers like atenolol can have their antihypertensive effects blunted by high-dose aspirin, and ACE inhibitors (e.g., lisinopril) may face reduced renal protection.[72] Patients should consult healthcare providers before combining aspirin with any medications, as over 300 interactions have been documented, with 61 classified as major.[73]Common Adverse Effects
Aspirin, like other nonsteroidal anti-inflammatory drugs (NSAIDs), commonly causes mild to moderate gastrointestinal disturbances, which are the most frequently reported adverse effects. These include dyspepsia, nausea, vomiting, abdominal pain, heartburn, and indigestion, often occurring due to aspirin's inhibition of prostaglandin synthesis in the gastric mucosa. In short-term use studies involving over 19,000 participants, minor gastrointestinal events such as these affected 5.2% of aspirin users compared to 3.7% on placebo, with odds ratios indicating a 1.46-fold increased risk. Dyspepsia specifically occurred in 3.2–6.2% of users, while abdominal pain was reported in 3–11%.[74][2][75] Other common effects involve the central nervous system and include tinnitus (ringing in the ears), dizziness, headache, drowsiness, and irritability, particularly at higher doses exceeding 1.95 g/day. Tinnitus arises from aspirin's ototoxic effects on the inner ear and is typically reversible upon discontinuation. Gastrointestinal symptoms like stomach discomfort, acid or sour stomach, and belching are also prevalent, with dyspepsia incidence ranging from 1% to 10% in clinical reports. These effects often resolve as the body adjusts but may persist in sensitive individuals.[2][76][75] Hypersensitivity reactions, though less common, affect 1–2% of the general population and up to 26% of those with asthma or chronic rhinosinusitis; manifestations include rash, urticaria, or mild angioedema. Easy bruising or minor bleeding tendencies can occur due to aspirin's antiplatelet activity, even at low doses, but these are generally mild. Direct application of aspirin to teeth or gums for pain relief can cause chemical burns to soft tissues due to its acidity; it should be taken orally instead.[77] Taking aspirin with food or antacids may mitigate gastrointestinal irritation, though consultation with a healthcare provider is recommended for persistent symptoms.[2][76][78]Overdose and Toxicity
Aspirin overdose, also known as salicylate toxicity, occurs from acute ingestion of large amounts or chronic accumulation from repeated dosing, often in individuals with impaired renal function or dehydration.[79] Acute overdose typically involves suicidal attempts or accidental ingestion, while chronic toxicity is more common in older adults and presents insidiously.[80] A toxic dose is generally 200-300 mg/kg, with lethality possible above 500 mg/kg, though outcomes depend on absorption rate and prompt treatment.[79] Symptoms of acute overdose progress in stages and correlate with serum salicylate levels. In mild cases (levels 40-80 mg/dL), patients experience nausea, vomiting, abdominal pain, tachypnea, and tinnitus.[80] Moderate toxicity (80-100 mg/dL), emerging 6-18 hours post-ingestion, includes confusion, slurred speech, hallucinations, tachycardia, and hypotension.[80] Severe cases (>100 mg/dL), occurring 12-24 hours later, feature cerebral and pulmonary edema, seizures, hypoventilation, and potential cardiac arrest.[80] Chronic overdose symptoms, such as fatigue, low-grade fever, confusion, and rapid heartbeat, may appear at lower levels and progress faster in children.[79] Common early signs across both types include rapid or slow breathing, seizures, rash, diarrhea, heartburn, and stomach pain with possible gastrointestinal bleeding.[79] Pathophysiologically, salicylates stimulate the respiratory center, causing hyperventilation and initial respiratory alkalosis, followed by uncoupling of oxidative phosphorylation, which increases lactate production and leads to metabolic acidosis.[80] This mixed acid-base disturbance, combined with fluid and electrolyte losses, glucose depletion, and impaired gluconeogenesis, results in hemodynamic instability, hypoglycemia, and end-organ damage like renal failure or cerebral edema.[80] Diagnosis relies on serum salicylate levels, with serial measurements essential due to delayed absorption; levels above 30 mg/dL in acute cases or 15 mg/dL in chronic warrant concern.[80] Arterial blood gas analysis reveals initial respiratory alkalosis transitioning to mixed acidosis, while additional tests include electrolytes (for hypokalemia), renal function, lactate, electrocardiogram (for arrhythmias), and acetaminophen levels to rule out co-ingestion.[80] Chest X-ray and head CT may assess complications like pulmonary edema or altered mental status.[79] Management begins with gastrointestinal decontamination using activated charcoal, which reduces peak salicylate concentrations by approximately 9.4 mg/L when given within hours of ingestion, though it is contraindicated in patients at risk of aspiration.[81] Intravenous fluid resuscitation with dextrose 5% in water and sodium bicarbonate alkalinizes the urine (target pH 7.5-8.0) to enhance salicylate excretion, shortening the elimination half-life from 13.4 to 9.3 hours.[81] Potassium supplementation corrects hypokalemia, and benzodiazepines treat seizures, with glucose administration addressing hypoglycemia.[80] Hemodialysis is indicated for severe toxicity (levels >100 mg/dL, refractory acidosis, seizures, renal failure, or pulmonary edema) to rapidly remove salicylates and correct acid-base/electrolyte imbalances.[80] Intensive care monitoring is required until levels fall below 30 mg/dL and pH normalizes.[80] Untreated overdose can lead to complications including respiratory failure, high fever, permanent neurological damage, or death, but early intervention improves prognosis significantly.[79]Other Applications
Veterinary Medicine
Aspirin, or acetylsalicylic acid, is employed in veterinary medicine as a nonsteroidal anti-inflammatory drug (NSAID) for its analgesic, anti-inflammatory, antipyretic, and antithrombotic properties, though its use is limited by species-specific metabolism differences and risks of gastrointestinal toxicity.[82] It is most commonly applied in dogs and horses, with cautious or restricted use in cats and cattle due to potential adverse effects and regulatory concerns.[82] Veterinary administration requires precise dosing under professional supervision, as aspirin inhibits cyclooxygenase enzymes, reducing prostaglandin synthesis, which can lead to ulceration if not monitored.[83] In dogs, aspirin is used to manage mild to moderate pain, such as in osteoarthritis or post-surgical recovery, though some veterinarians may recommend buffered aspirin for short-term, low-dose use in mild pain situations; however, it is not ideal due to risks of gastrointestinal issues or bleeding, and it should never be administered without direct veterinary guidance.[84] Aspirin is also used for antithrombotic effects in conditions like heart disease or thromboembolism at low doses of 1–2 mg/kg orally every 24 hours.[82] Higher anti-inflammatory doses range from 10–40 mg/kg orally every 12–24 hours, with plasma salicylate monitoring recommended to maintain therapeutic levels of 10–30 mg/dL and avoid toxicity.[83] Prolonged use can cause gastric ulcers in up to 43% of dogs at doses exceeding 50 mg/kg twice daily, prompting preference for veterinary-specific NSAIDs like carprofen.[82] Cats metabolize aspirin slowly via glucuronidation, leading to prolonged exposure and heightened toxicity risk, so it is rarely prescribed except for specific indications like aortic thromboembolism at 5–10 mg/kg orally every 48–72 hours.[82] Doses above 80 mg/kg can cause severe poisoning, manifesting as vomiting, anorexia, hyperthermia, metabolic acidosis, and potentially fatal disseminated intravascular coagulation.[85] Safer alternatives, such as meloxicam, are favored for feline pain management.[82] In horses, aspirin serves as an antithrombotic agent for laminitis at 10 mg/kg orally daily, helping reduce platelet aggregation without significant anti-inflammatory dosing due to poor oral bioavailability for that purpose.[82] For cattle, off-label use has occurred for pain and fever, but the FDA advises against administering unapproved aspirin products to lactating dairy cows due to violative drug residues in milk, emphasizing approved alternatives like flunixin meglumine.[86] A 2020 study found that boluses of acetylsalicylic acid post-calving reduced inflammation and increased milk yield by approximately 1.6 kg/day during the first 60 days of lactation in multiparous cows, though this remains experimental.[87] Aspirin is contraindicated in animals with bleeding disorders, renal impairment, or concurrent NSAID use, and toxicity thresholds are lower in dehydrated or young animals.[88] In dogs, acute overdose exceeds 100–300 mg/kg, causing similar gastrointestinal and acid-base disturbances as in cats.[88] Treatment involves decontamination, supportive care, and urinary alkalinization to enhance salicylate excretion.[89] Overall, while historically versatile, aspirin's veterinary role has diminished with the availability of species-tailored NSAIDs.[82]Ongoing Research
Recent clinical trials continue to explore aspirin's role in cardiovascular disease prevention, particularly in high-risk populations. A 2025 analysis from the American Heart Association indicated that low-dose aspirin (81 mg daily) is associated with a reduced risk of cardiovascular events, including heart attack, stroke, and death, in adults with type 2 diabetes and elevated cardiovascular risk, based on a 10-year follow-up of over 10,000 patients.[90] Ongoing trials, such as the ASSIST-MI study (NCT06676280), are investigating aspirin's efficacy alongside statin strategies for primary prevention of myocardial infarction in individuals with severe mental illness, aiming to address understudied comorbidities.[91] Additionally, the ADAPTABLE trial's long-term data (NCT02697916) supports 81 mg as the optimal dose for secondary prevention in atherosclerotic cardiovascular disease, influencing current dosing guidelines.[92] In cancer research, aspirin's potential as a chemopreventive agent remains a focus, with recent evidence highlighting its impact on recurrence. A Scandinavian phase III trial published in October 2025 demonstrated that low-dose aspirin halved the risk of colon and rectal cancer recurrence in patients with curatively resected stage II-III disease, prompting further investigations into its anti-inflammatory mechanisms.[93] The ongoing CAPP3 trial (NCT02232305, extended into 2025) evaluates aspirin's role in preventing colorectal adenomas in Lynch syndrome carriers, building on prior findings of reduced cancer incidence. A 2025 meta-analysis in Public Health reinforced aspirin's association with lower colorectal cancer mortality, particularly in long-term users, underscoring the need for randomized trials to confirm causality and optimal regimens.[94] Emerging studies are also examining aspirin in obstetric and hematologic contexts. The ASAPP trial (NCT04070573), presented in 2025, compared 81 mg and 162 mg aspirin doses for preeclampsia prevention in high-risk pregnancies, finding no additional benefit of the higher dose over 81 mg in reducing preterm preeclampsia risk.[95] In immune thrombocytopenia (ITP), the ASPIRE trial (NCT04912505) is evaluating aspirin's pharmacodynamics in patients with cardiovascular disease, testing whether 100 mg daily improves platelet function without increasing bleeding risks.[96] Combination therapies are under scrutiny as well; for instance, the trial (NCT05287321) compares aspirin plus hydroxychloroquine versus aspirin alone for preventing pre-eclampsia in high-risk pregnancies. These efforts highlight aspirin's versatility, though challenges like bleeding risks continue to drive research toward personalized approaches.[97]References
- https://en.wikisource.org/wiki/Treaty_of_Versailles/Part_X