Recent from talks
Nothing was collected or created yet.
Pancuronium bromide
View on Wikipedia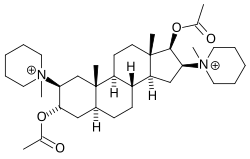 | |
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | NA |
| Protein binding | 77 to 91% |
| Metabolism | Hepatic |
| Elimination half-life | 1.5 to 2.7 hours |
| Excretion | Renal and biliary |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII |
|
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.035.923 |
| Chemical and physical data | |
| Formula | C35H60N2O4 |
| Molar mass | 572.875 g·mol−1 |
| |
| | |
Pancuronium (trademarked as Pavulon) is an aminosteroid muscle relaxant with various medical uses.[1] It is used in euthanasia and is used in some states as the second of three drugs administered during lethal injections in the United States.
Mechanism of action
[edit]Pancuronium is a typical non-depolarizing curare-mimetic muscle relaxant. It competitively inhibits the nicotinic acetylcholine receptor at the neuromuscular junction by blocking the binding of acetylcholine. It has slight vagolytic activity, causing an increase in heart rate, but no ganglioplegic (i.e., blocking ganglions) activity. It is a very potent muscle relaxant drug, with an ED95 (i.e., the dose that causes 95% depression of muscle twitch response) of only 60 μg/kg body weight. Onset of action is relatively slow compared to other similar drugs, in part due to its low dose: an intubating dose takes 3–6 minutes for full effect. Clinical effects (muscle activity lower than 25% of physiological) last for about 100 minutes. The time needed for full (over 90% muscle activity) recovery after single administration is about 120–180 minutes in healthy adults.
The effects of pancuronium can be at least partially reversed by anticholinesterasics, such as neostigmine, pyridostigmine, and edrophonium.
Development
[edit]Workers at Organon were inspired by the structure of the aminosteroid alkaloid malouetine to develop a series of aminosteroid neuromuscular blockers based on an androstane nucleus, culminating in the development of pancuronium bromide.[2][3][4]
Pancuronium is designed to mimic the action of two molecules of acetylcholine with the quaternary nitrogen atoms spaced rigidly apart by the steroid rings at a distance of ten atoms (interonium distance). Decamethonium and suxamethonium also have this same interonium distance.
Uses in medicine
[edit]Pancuronium is used with general anesthesia in surgery for muscle relaxation and as an aid to intubation or ventilation. It does not have sedative or analgesic effects.
Side-effects include moderately raised heart rate and thereby arterial pressure and cardiac output, excessive salivation, apnea and respiratory depression, rashes, flushing, and sweating.[medical citation needed] The muscular relaxation can be dangerous in the seriously ill and it can accumulate leading to extended weakness. Pancuronium is not preferable in long-term use in ICU-ventilated patients.
In Belgium and the Netherlands, pancuronium is recommended in the protocol for euthanasia. After administering sodium thiopental to induce coma, pancuronium is delivered in order to stop breathing.[5]
Uses in execution
[edit]Procedure
[edit]Pancuronium is also used as one component of a lethal injection in administration of the death penalty in some parts of the United States.[6]
Controversy
[edit]Like all non-depolarising muscle relaxants, pancuronium has no effect on level of consciousness. Therefore, if the anaesthetic used is insufficient, the individual may be awake but unable to cry out or move due to the effect of the pancuronium. There have been several civil lawsuits alleging similar failures of adequate anaesthesia during general surgical procedures. These have been largely due to improper or insufficient dosages of anaesthetic in concert with normal dosages of muscle relaxants such as pancuronium.
In 2007, Michael Munro, a Scottish neonatologist at Aberdeen Maternity Hospital, was cleared of malpractice by the General Medical Council Fitness to Practice panel after giving 23 times the standard dose of pancuronium to two dying neonates. Terminally ill, both dying babies were suffering from agonal gasping and violent body spasms, which was highly distressing for the parents to witness. Munro then administered pancuronium to the babies after advising the parents that this would ease their suffering and could also hasten death.[7][8] It was on record that neither of the children's parents were unhappy with Munro's treatment.[9]
Amnesty International has objected to its use in lethal injections on the grounds that it "may mask the condemned prisoner's suffering during the execution,"[10] thereby leading observers to conclude that lethal injection is painless, or less cruel than other forms of execution.
Export limitations
[edit]The United Kingdom bans the export of pancuronium bromide to the United States due to its use in lethal injections, but not to the Netherlands or Belgium.[11]
Uses in crime
[edit]Pancuronium was used in Efren Saldivar's killing spree.[12] It was also used by the Skin Hunters to kill patients in the Polish city of Łódź. Pavulon was also used by Richard Angelo in 1987 to kill at least ten patients under his care at the Good Samaritan Hospital in New York.
See also
[edit]References
[edit]- ^ Das GN, Sharma P, Maani CV (January 2021). "Pancuronium". StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. PMID 30855929.
- ^ Lewis JJ, Martin-Smith M, Muir TC, Ross HH (August 1967). "Steroidal monoquaternary ammonium salts with non-depolarizing neuromuscular blocking activity". The Journal of Pharmacy and Pharmacology. 19 (8): 502–508. doi:10.1111/j.2042-7158.1967.tb09579.x. PMID 4382437. S2CID 2938040.
- ^ Buckett WR, Hewett CL, Savage DS (October 1973). "Pancuronium bromide and other steroidal neuromuscular blocking agents containing acetylcholine fragments". Journal of Medicinal Chemistry. 16 (10): 1116–1124. doi:10.1021/jm00268a011. PMID 4356139.
- ^ McKenzie AG (June 2000). "Prelude to pancuronium and vecuronium". Anaesthesia. 55 (6): 551–556. doi:10.1046/j.1365-2044.2000.01423.x. PMID 10866718. S2CID 22476701.
- ^ "Administration and Compounding Of Euthanasic Agents". The Hague: Royal Dutch Society for the Advancement of Pharmacy. Archived from the original on 7 June 2008. Retrieved 15 July 2008 – via ERGO!.
- ^ "US court backs lethal injection". BBC News. 16 April 2008.
- ^ "Baby doctor cleared of misconduct". BBC News. 11 July 2007. Retrieved 2010-05-21.
- ^ "Doctor cleared over baby deaths". The Guardian. 11 July 2007.
- ^ "Doctor felt babies were suffering". BBC News. 9 July 2007. Retrieved 2010-05-21.
- ^ "UA 44/04 Death penalty". Amnesty International. 6 February 2004. Archived from the original on 17 May 2004.
- ^ "Provisions supplementing "the torture Regulation"". Article 4A of Export Control Order 2008, UK Statutory Instruments 2008 No. 3231 PART 2 Article 9. UK Legislation.
- ^ Ramsland K (9 April 2005). "Dark Rumors". Crimelibrary. Archived from the original on 9 April 2005.
Pancuronium bromide
View on GrokipediaChemical and Pharmacological Properties
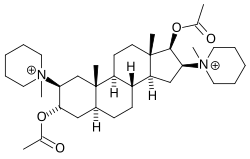
Chemical Structure and Classification
Pancuronium bromide is a synthetic aminosteroid compound with the molecular formula C₃₅H₆₀Br₂N₂O₄ and a molecular weight of 732.67 g/mol.[12] It consists of two bromide ions paired with a pancuronium dication, which features a quaternary ammonium structure.[12] The chemical designation is 2β,16β-dipiperidino-5α-androstane-3α,17β-diol diacetate dimethobromide, reflecting its derivation from the androstane steroid skeleton modified with piperidino groups at the 2 and 16 positions and acetate esters at the 3 and 17 positions.[3] Pancuronium bromide is classified as a non-depolarizing neuromuscular blocking agent, acting as a competitive antagonist at nicotinic acetylcholine receptors.[2] As a bis-quaternary aminosteroid, it belongs to a subclass of synthetic curare-mimetic muscle relaxants designed for prolonged blockade of neuromuscular transmission without initial depolarization.[13] This classification distinguishes it from depolarizing agents like succinylcholine and from earlier benzylisoquinolinium non-depolarizers like tubocurarine.[2]Mechanism of Action
Pancuronium bromide is classified as a long-acting, non-depolarizing neuromuscular blocking agent of the aminosteroid type, acting primarily through competitive antagonism of acetylcholine at postjunctional nicotinic receptors in the neuromuscular junction.[1] It binds to the alpha subunits of these receptors, inducing a conformational change that closes the ion channel and prevents sodium influx, thereby inhibiting end-plate depolarization and skeletal muscle contraction without eliciting initial fasciculations.[1][2] This mechanism results in dose-dependent flaccid paralysis, with potency enhanced by its bis-quaternary ammonium structure that electrostatically mimics acetylcholine's cationic properties for receptor affinity.[14] The drug's large molecular size may also contribute to channel occlusion, further blocking ion flow.[1] In addition to its nicotinic effects, pancuronium demonstrates weak antagonism at muscarinic acetylcholine receptors, particularly M2 subtypes in cardiac tissue, leading to vagolytic actions such as tachycardia and hypertension due to unopposed sympathetic tone.[2] Reversal of the neuromuscular blockade occurs via cholinesterase inhibitors (e.g., neostigmine), which elevate acetylcholine concentrations to competitively displace pancuronium, often administered with anticholinergics to mitigate muscarinic side effects.[1][2]Pharmacokinetics and Dosage
Pancuronium bromide is administered intravenously, with no significant oral bioavailability due to its quaternary ammonium structure, which prevents gastrointestinal absorption.[1] Onset of neuromuscular blockade occurs within 2 to 5 minutes following intravenous injection, with peak effect in approximately 4 minutes.[15] [1] Distribution is rapid into extracellular fluid, with a volume of distribution of 0.24 to 0.28 L/kg and protein binding of 77% to 91%.[2] [16] Its low lipid solubility limits penetration of the blood-brain barrier, though it crosses the placenta to a minor extent.[1] Metabolism occurs minimally via hepatic deacetylation, producing 3-desacetylpancuronium (approximately 30% to 50% as potent as the parent drug) and weaker metabolites such as 17-desacetyl and 3,17-dihydroxy forms; overall, hepatic metabolism accounts for about 10% of clearance.[1] [16] Elimination is primarily renal, with 60% to 80% excreted unchanged in urine, alongside minor biliary excretion (about 10%) and the remainder as metabolites.[1] Plasma clearance ranges from 1.1 to 1.9 mL/min/kg.[2] The elimination half-life is 1.5 to 2.7 hours in healthy adults, though it prolongs to over 3 hours in renal or hepatic impairment, leading to extended duration of action (60 to 90 minutes for return to 25% twitch recovery with standard doses).[2] [16] [1] Dosage must be individualized based on patient response, anesthesia type, and organ function, with monitoring via peripheral nerve stimulator recommended. For adjunctive use in balanced anesthesia, an initial intravenous dose of 0.04 to 0.1 mg/kg provides skeletal muscle relaxation; for rapid tracheal intubation, 0.06 to 0.1 mg/kg (with ED95 of 0.07 mg/kg) is typical, achieving maximal blockade in 3 to 5 minutes.[16] [1] [17] Maintenance doses of 0.01 to 0.02 mg/kg are administered at 25- to 60-minute intervals or as continuous infusion at 0.7 to 2 mcg/kg/min, titrated to clinical effect.[1] [16] In patients with renal failure, doses should be reduced by 30% to 50% and intervals extended due to prolonged half-life.[16]History and Development
Discovery and Synthesis
Pancuronium bromide, a synthetic aminosteroid neuromuscular blocking agent, was first prepared in 1964 by David S. Savage and colleagues at Organon Laboratories in Newstead, Scotland, under the direction of C. L. Hewett.[18] [1] The compound emerged from research aimed at developing potent, non-depolarizing muscle relaxants inspired by the structure of natural aminosteroid alkaloids like malouetine, which exhibited neuromuscular blocking effects.[18] This work built on earlier efforts to modify steroid scaffolds to mimic the bis-quaternary ammonium structure of acetylcholine for enhanced receptor affinity at the neuromuscular junction. The synthesis proceeded from a 5α-androstane steroid precursor, specifically 3α,17β-diacetoxy-2β,16β-bis(piperidino)-5α-androstane, which was quaternized at the piperidine nitrogens using methyl bromide to form the bis(1-methylpiperidinium) dibromide salt.[19] This key step introduced the charged onium centers essential for competitive antagonism at nicotinic acetylcholine receptors, while the rigid steroid core provided selectivity and potency over flexible synthetic relaxants like succinylcholine.[20] [21] Pharmacological screening, directed by W. R. Buckett, identified pancuronium's long-acting profile and cardiovascular stability, distinguishing it from prior agents.[18]Clinical Trials and Regulatory Approval
Pancuronium bromide underwent initial clinical evaluation in 1967, when Baird and Reid administered varying doses to six patients undergoing surgery under general anesthesia, reporting effective neuromuscular blockade with a duration of action approximately twice that of gallamine, and minimal cardiovascular effects at standard doses.[22] Subsequent preliminary trials expanded to 50 patients, confirming its potency as a non-depolarizing muscle relaxant, with an effective dose for 95% twitch suppression (ED95) of 0.07 mg/kg, rapid onset within 2-3 minutes, and blockade lasting 45-60 minutes, alongside advantages such as lack of histamine release and stability under anesthesia.[21] These early studies, conducted primarily in the United Kingdom, emphasized its superiority over prior agents like d-tubocurarine in terms of potency and reduced side effects, paving the way for broader testing.[5] Further clinical trials in the late 1960s and early 1970s validated pancuronium's safety and efficacy for facilitating endotracheal intubation, maintaining muscle relaxation during surgery, and supporting mechanical ventilation, with data from hundreds of patients showing low incidence of adverse reactions, primarily transient tachycardia in about 30% of cases at higher doses.[23] Trials also assessed reversibility with anticholinesterases like neostigmine, achieving adequate recovery in most cases within 30-60 minutes post-administration.[6] Developed by Organon researchers under W.R. Buckett, who synthesized it in 1964 and refined analogs, the drug progressed through phased evaluations focusing on dose-response curves, hemodynamic stability, and compatibility with volatile anesthetics.[1] Regulatory approval followed successful trials, with initial marketing authorizations granted in Europe by the late 1960s, enabling commercial launch as Pavulon by Organon, a Dutch firm, for use in anesthesia.[5] In the United States, the Food and Drug Administration approved pancuronium bromide in 1972 under the trade name Pavulon for indications including skeletal muscle relaxation during surgery and assisted ventilation, based on submitted clinical data demonstrating predictable pharmacokinetics and a favorable risk-benefit profile compared to earlier neuromuscular blockers.[12] Approvals in other jurisdictions, such as Canada and Australia, occurred concurrently in the early 1970s, with labeling emphasizing intravenous administration, contraindications in myasthenia gravis, and need for controlled reversal.[16] Post-approval surveillance has since monitored rare hypersensitivity reactions, but initial regulatory decisions rested on trial evidence of reliable blockade without significant ganglionic or vagolytic effects at therapeutic doses.[1]Medical Uses
Applications in Anesthesia and Surgery
Pancuronium bromide functions as a non-depolarizing neuromuscular blocking agent administered intravenously as an adjunct to general anesthesia, enabling rapid endotracheal intubation and sustained skeletal muscle relaxation essential for surgical immobility.[24][1] It competitively antagonizes nicotinic acetylcholine receptors at the neuromuscular junction, preventing depolarization and muscle contraction without intrinsic anesthetic, analgesic, or amnestic effects, thus requiring co-administration of hypnotics, opioids, or inhalational agents for comprehensive anesthesia.[1] This application is particularly valued in procedures demanding prolonged paralysis, such as intra-abdominal, thoracic, or orthopedic surgeries, where its long duration—typically 60 to 90 minutes for an initial dose—reduces the frequency of redosing compared to shorter-acting agents.[1][16] Standard dosing begins with a bolus of 0.06 to 0.1 mg/kg for intubation, achieving maximal blockade within 2 to 5 minutes under balanced anesthesia, followed by incremental maintenance doses of 0.01 to 0.015 mg/kg every 30 to 60 minutes or as guided by clinical response.[25][16] Lower initial doses (0.04 to 0.06 mg/kg) suffice when potentiated by volatile anesthetics or prior succinylcholine, while continuous infusion at 0.7 to 2 mcg/kg/min supports extended operations.[1] In cesarean sections, equivalent dosing facilitates relaxation without altering the standard regimen, though delivery should occur promptly after induction to limit transplacental transfer, and concurrent magnesium sulfate may necessitate dose reduction.[16] Neuromuscular function must be monitored using peripheral nerve stimulation, such as train-of-four ratio, to titrate doses, avert overdose, and ensure reversal with anticholinesterases like neostigmine prior to extubation.[1][24] Its vagolytic properties often induce mild tachycardia, offering hemodynamic stability advantageous in hypovolemic or cardiac patients, though this requires vigilant cardiovascular monitoring during use.[1] Despite declining favor due to availability of intermediate-acting alternatives, pancuronium remains effective for scenarios prioritizing duration over rapid offset.[1]Use in Intensive Care and Ventilation
Pancuronium bromide, a long-acting non-depolarizing neuromuscular blocking agent, is utilized in intensive care units (ICUs) primarily to facilitate mechanical ventilation in patients with severe acute respiratory failure, such as acute respiratory distress syndrome (ARDS), by inducing skeletal muscle paralysis.[26] This blockade eliminates spontaneous respiratory efforts, thereby improving patient-ventilator synchrony, reducing oxygen consumption, and minimizing ventilator-induced lung injury through optimized tidal volumes and pressures.[27] Early reports from 1975 documented its efficacy in six ARDS patients, where it enhanced ventilation compliance without immediate complications.[26] Administration typically involves an initial intravenous bolus of 0.06–0.1 mg/kg, followed by intermittent maintenance boluses of 0.01–0.02 mg/kg every 30–60 minutes or a continuous infusion starting at 0.05–0.1 mg/kg/hour, titrated based on clinical response and ideal body weight.[17] [28] Neuromuscular function must be monitored using peripheral nerve stimulation, such as train-of-four (TOF) testing, to maintain one to two twitches and prevent excessive blockade, with daily interruptions recommended to assess ongoing need and weaning potential.[27] Its duration of action, approximately 60–100 minutes after bolus dosing, suits scenarios requiring sustained relaxation but necessitates caution in renal impairment due to 45–70% renal excretion, leading to potential accumulation.[28] [29] Despite these applications, prolonged pancuronium use in ICUs has been associated with critical illness myopathy and polyneuropathy, particularly when co-administered with corticosteroids, as evidenced by clusters of seven patients developing severe weakness and prolonged ventilation dependence after 5–16 days of therapy.[30] Surveys indicate higher utilization in surgical ICUs compared to medical ones, where shorter-acting agents like vecuronium predominate to mitigate risks of extended mechanical ventilation and ICU length of stay.[31] Current guidelines advocate restrictive use, reserving it for refractory cases unresponsive to sedation alone, given evidence linking continuous neuromuscular blockade to increased ICU-acquired weakness incidence.[29] [32]Pediatric and Special Populations
In pediatric patients, pancuronium bromide dosing generally mirrors adult regimens for children over 1 month of age, with an initial intravenous dose of 0.04 to 0.1 mg/kg followed by maintenance increments of 0.01 to 0.1 mg/kg every 30 to 60 minutes or continuous infusion at 0.1 mg/kg/hour, adjusted based on ideal body weight and neuromuscular monitoring.[25] [17] Neonates and premature infants require heightened caution, as certain formulations contain benzyl alcohol, which is contraindicated due to risks of metabolic acidosis and kernicterus; however, preservative-free preparations have been used safely for muscle relaxation during neonatal anesthesia and mechanical ventilation, with test doses of 0.02 mg/kg recommended to assess responsiveness.[16] [33] Dose requirements per effective dose (ED95) are higher in neonates (0.6 mg/kg) and infants (0.7 mg/kg) compared to older children (0.4 mg/kg) and adults (0.3 mg/kg), reflecting immature neuromuscular junction sensitivity, with onset in 70-90% of cases within 150 seconds at 100 mcg/kg.[34] [35] For special populations, renal impairment prolongs pancuronium's elimination half-life by approximately twofold and reduces clearance by 50-67%, necessitating dose reductions, prolonged monitoring, and avoidance of accumulation through extended intervals or lower infusion rates to prevent prolonged paralysis.[36] [37] Hepatic dysfunction or biliary obstruction similarly extends duration by increasing volume of distribution and impairing biliary excretion (which accounts for 10-40% of elimination), requiring cautious titration and neuromuscular function assessment.[36] [35] In elderly patients, effects exhibit greater variability with age-related declines in organ function, elevating the risk of postoperative residual neuromuscular blockade; standard adult dosing applies but with enhanced vigilance for tachycardia and incomplete reversal.[38] [39] Overall, use in debilitated individuals or those with myasthenia gravis demands peripheral nerve stimulation to guide dosing and minimize overdose risks across these groups.[40]Non-Therapeutic Applications
Role in Capital Punishment Protocols
Pancuronium bromide serves as the paralytic agent in the traditional three-drug lethal injection protocol employed for capital punishment in several U.S. states. Administered after an initial barbiturate anesthetic such as sodium thiopental or pentobarbital to induce unconsciousness, it functions by competitively blocking nicotinic acetylcholine receptors at the neuromuscular junction, thereby paralyzing skeletal muscles, halting respiration, and preventing visible convulsions or movement during the execution process.[9] [8] This immobilization ensures that the inmate's body remains still, which protocol designers have cited as a means to maintain composure among witnesses and execution personnel, though critics argue it primarily conceals potential signs of distress if anesthesia is inadequate.[41] The sequence concludes with potassium chloride to induce cardiac arrest by disrupting myocardial electrical activity. Typical dosages in state protocols have included 100 mg of pancuronium bromide, administered intravenously via sequential syringes or a single infusion line, with execution times generally ranging from 5 to 15 minutes from injection to death declaration.[8] [42] This regimen originated from veterinary euthanasia practices adapted for human application and was first utilized in the United States on December 7, 1982, when Texas executed Charles Brooks Jr., marking the debut of lethal injection as a method of capital punishment following its proposal in Oklahoma in 1977.[9] By the early 2000s, over 30 states had adopted variations of this protocol, with Texas conducting more than 500 executions using it until shifts in drug availability prompted modifications.[43] Although pharmaceutical manufacturers like Hospira ceased supplying pancuronium for lethal injections around 2011 due to ethical concerns and European export restrictions, some states retained it in authorized protocols or as an alternative paralytic (e.g., alongside rocuronium bromide).[44] For instance, as of 2023, protocols in states like Alabama and Missouri permitted its use in multi-drug combinations, though single-drug pentobarbital regimens have increasingly supplanted the three-drug approach amid sourcing challenges and legal scrutiny.[45] The drug's inclusion persists in part because it provides rapid, reliable paralysis without requiring specialized equipment beyond standard IV setup, aligning with state corrections departments' emphasis on procedural efficiency over single-agent simplicity.[11]Involvement in Criminal Cases
Pancuronium bromide has been used illicitly in homicides, particularly by medical personnel exploiting its paralytic effects to cause respiratory failure without obvious external trauma. In such cases, detection often relies on forensic toxicology, as the drug metabolizes rapidly and requires specialized analysis in postmortem tissues.[46] The most prominent example involves Efren Saldivar, a respiratory therapist employed at Glendale Adventist Medical Center in California from 1988 to 1998. Saldivar confessed in January 1998 to deliberately injecting approximately 50 terminally ill or unconscious patients with overdoses of pancuronium bromide or succinylcholine chloride, paralyzing their respiratory muscles and hastening death under the guise of euthanasia or mercy killing.[47] Estimates of total victims reached up to 200, targeting those unlikely to be closely monitored.[48] Initial investigations stalled due to the drug's degradation in embalmed bodies, but advanced forensic testing at Lawrence Livermore National Laboratory in 2000 confirmed pancuronium residues in exhumed tissues from six victims, leading to Saldivar's indictment on six counts of first-degree murder in February 2001.[46] He pleaded guilty to two murders and received a sentence of six years to life, with additional charges limited by statutes of limitations.[49] In a separate incident documented in forensic literature, a nurse attempted to murder her anesthesiologist husband on two occasions by intravenously administering pancuronium bromide, aiming to induce paralysis and simulate a medical emergency.[50] The attempts failed due to timely intervention and low dosing relative to the victim's body weight, but toxicological evidence substantiated the intent, resulting in criminal charges. This case highlights the drug's accessibility to healthcare workers and the challenges in proving intent without overt symptoms.[50]Controversies and Debates
Claims of Inhumane Effects in Executions
Critics of lethal injection protocols employing pancuronium bromide argue that the drug's paralytic effects render executions potentially inhumane by concealing signs of consciousness and suffering. As a non-depolarizing neuromuscular blocker, pancuronium induces rapid paralysis of skeletal muscles, including those of the diaphragm and chest wall, leading to respiratory arrest without alleviating pain or awareness. If the preceding anesthetic, such as sodium thiopental, proves insufficient—due to inadequate dosing, improper administration, or individual variability—the inmate may remain conscious while experiencing the corrosive pain of potassium chloride, which disrupts cardiac function and produces a severe burning sensation equivalent to liquid fire along veins. This paralysis prevents outward manifestations of distress, such as convulsions or vocalization, creating an illusion of a peaceful death primarily for the benefit of witnesses and execution personnel rather than mitigating the inmate's experience.[41][8] Medical experts and analyses have highlighted the risk of aware suffocation under pancuronium's influence, drawing parallels to prohibited practices in veterinary euthanasia. At least 30 U.S. states ban paralytic agents like pancuronium in animal killings without confirmed unconsciousness, citing the ethical concern of undetectable agony from asphyxiation. Anesthesiologist Mark Dershwitz has acknowledged that pancuronium serves to suppress visible movement, thereby "enhancing the dignity" of the process for observers, but does not address potential internal torment if anesthesia lapses. Studies of execution data, including autopsy toxicology, reveal inconsistencies in anesthetic levels; for instance, postmortem thiopental concentrations in some cases fell below therapeutic ranges for deep sedation, suggesting possible awareness during paralysis. Execution logs further indicate prolonged breathing post-anesthetic but pre-paralytic, implying windows of potential consciousness.[41][51] Specific botched executions underscore these claims, such as Florida's 2006 implementation on Angel Diaz, where intravenous access failed, resulting in chemical burns, open eyes, and mouth movements persisting for 24 minutes after pancuronium administration, with evidence of inadequate anesthesia contributing to extended distress. Similar concerns arose in challenges under the Eighth Amendment, where inmates contended that pancuronium exacerbates risks of "superadded" pain beyond necessary for execution, constituting cruel and unusual punishment by prioritizing cosmetic serenity over verifiable unconsciousness. While courts, including in Baze v. Rees (2008), have generally rejected such challenges absent proof of substantial risk, proponents of reform argue the drug's inclusion reflects a flawed protocol prone to human error in non-medical settings.[8][52]Evidence on Efficacy and Safety in Lethal Injection
Pancuronium bromide, administered as the second drug in the standard three-drug lethal injection protocol following a barbiturate anesthetic like sodium thiopental, induces rapid paralysis of skeletal muscles, including the diaphragm, thereby causing respiratory arrest and contributing to death via chemical asphyxiation.[8] Pharmacokinetic modeling and execution data indicate that pancuronium effectively halts voluntary respiration within 1-9 minutes post-injection in documented cases, often preceding the cardiac effects of the subsequent potassium chloride.[8] However, its efficacy in ensuring a swift, humane death depends critically on prior achievement of deep unconsciousness; without it, the drug prevents external signs of distress while permitting internal awareness of suffocation.[8] [53] Scientific analyses, including pharmacokinetic simulations based on human and animal data, reveal that standard thiopental doses (typically 3-5 grams) redistribute rapidly, falling below surgical anesthesia levels (around 10-15 mg/L plasma concentration) within minutes, potentially leaving inmates conscious during pancuronium-induced paralysis.[8] In North Carolina executions from 1998-2005, mean time to death ranged from 9 to 13.5 minutes across protocols, with respiration ceasing before potassium chloride injection in many instances, underscoring pancuronium's dominant role in asphyxiation rather than the intended cardiac arrest.[8] California records similarly showed cardiac flatlining delayed 2-9 minutes after potassium chloride, with low postmortem thiopental levels in multiple cases suggesting inadequate anesthesia.[8] Safety concerns center on the risk of conscious suffering masked by paralysis, as pancuronium blocks neuromuscular transmission without analgesia or sedation, amplifying agony from hypoxia or potassium chloride's burning sensation if anesthesia fails.[8] [53] The 2006 execution of Angel Nieves Diaz in Florida exemplifies protocol vulnerabilities: despite 34 minutes to death, signs of distress (wincing, gasping) occurred due to subcutaneous rather than intravenous delivery, resulting in chemical burns and highlighting inconsistent drug absorption.[53] Eyewitness accounts and autopsy findings from such botched events indicate that pancuronium may prolong awareness of suffocation, with thiopental doses often sub-lethal and insufficient for sustained unconsciousness.[53] These findings, drawn from peer-reviewed modeling and state execution logs, question the protocol's reliability for averting cruel punishment.[8] [53]Regulatory and Supply Restrictions
Pancuronium bromide is classified as a prescription-only medication in the United States, subject to FDA oversight for use as a neuromuscular blocking agent in anesthesia, with administration restricted to or under the direct supervision of experienced clinicians trained in its handling to mitigate risks of respiratory paralysis.[16] It does not fall under the DEA's controlled substances schedules, lacking narcotic or abuse potential classifications that would impose additional federal tracking or quota requirements.[54] Supply restrictions intensified due to the drug's role in multi-drug lethal injection protocols, prompting pharmaceutical manufacturers to limit distribution to prevent diversion for capital punishment. In May 2016, Pfizer announced enforcement of stringent controls on pancuronium bromide (along with other agents like potassium chloride and rocuronium bromide), prohibiting sales to entities intending use in executions and requiring end-user verification to ensure medical-only applications.[55] This followed similar refusals by suppliers of pancuronium and related drugs, exacerbating shortages that forced U.S. states to revise protocols away from traditional three-drug combinations involving the agent.[10] Internationally, export bans have further constrained availability for non-therapeutic purposes. The United Kingdom implemented a prohibition in 2011 on exporting pancuronium bromide—alongside pentobarbital and potassium chloride—to the United States, explicitly citing opposition to its application in lethal injections, while permitting shipments to countries without capital punishment like the Netherlands and Belgium.[56] European Union regulations similarly restrict shipments of execution-related pharmaceuticals, contributing to global supply chain disruptions that have persisted into the 2020s and prompted shifts toward alternative execution methods or single-drug regimens in jurisdictions retaining lethal injection.[57] These measures reflect manufacturer and governmental efforts to align distribution with humanitarian concerns over execution efficacy, though they have not halted approved medical uses.Safety Profile and Alternatives
Adverse Effects and Contraindications
Pancuronium bromide, a non-depolarizing neuromuscular blocking agent, primarily induces skeletal muscle paralysis but can cause cardiovascular effects due to its vagolytic properties, including tachycardia and hypertension, particularly in patients with underlying heart conditions or those receiving doses exceeding 0.1 mg/kg.[1] These effects arise from blockade of cardiac muscarinic receptors, leading to unopposed sympathetic activity, with heart rate increases typically moderate (10-20 beats per minute) at standard doses but potentially more pronounced in edematous states or with slower circulation times.[1] Respiratory depression or apnea occurs as an intended effect but risks prolongation if ventilation is inadequate, compounded by residual blockade in cases of overdose or impaired clearance.[24] Hypersensitivity reactions, though infrequent (0.1-1% incidence), include severe anaphylaxis, rash, bronchospasm, and flushing, necessitating immediate discontinuation and supportive care.[58] Local injection site reactions such as pain or burning are reported in 0.1-1% of administrations.[58] In the absence of concurrent sedation, pancuronium use carries psychological risks for aware patients, alongside hazards like undetected ventilator disconnection leading to hypoxia.[59] Prolonged neuromuscular blockade is a significant concern in renal impairment, where elimination half-life doubles due to reduced urinary excretion of the parent drug and its active metabolite, potentially requiring dose reductions or avoidance.[3] Contraindications include known hypersensitivity to pancuronium or bromides, as well as conditions lacking adequate ventilatory support or involving preexisting neuromuscular disorders like myasthenia gravis, where effects may be exaggerated.[60][1] It is also contraindicated in patients with tachycardia or scenarios where even minor heart rate elevations are undesirable, due to its sympathomimetic profile.[40] Relative contraindications encompass severe renal, hepatic, or pulmonary disease, dehydration, electrolyte imbalances (e.g., hypokalemia, hypermagnesemia), and acidosis, all of which potentiate neuromuscular blockade duration and intensity.[1][61] Careful monitoring via train-of-four stimulation is essential to mitigate risks of incomplete reversal.[1]Comparisons with Other Neuromuscular Blockers
Pancuronium bromide, a bis-quaternary aminosteroid non-depolarizing neuromuscular blocking agent, differs from other non-depolarizing agents primarily in its longer duration of action and pronounced vagolytic effects. Its onset of paralysis occurs in 3-5 minutes following an intubating dose of 0.08-0.1 mg/kg, with clinical duration extending 60-90 minutes or longer, owing to dose-dependent renal elimination (approximately 70-80% unchanged). This contrasts with intermediate-acting aminosteroids like vecuronium (onset 3-4 minutes, duration 25-40 minutes) and rocuronium (onset 1-2 minutes at 1 mg/kg doses, duration 30-60 minutes), which exhibit faster recovery and reduced accumulation with repeated dosing due to greater hepatic clearance.[1][62][63][64]| Agent | Structure Class | Onset (minutes) | Clinical Duration (minutes) | Primary Elimination | Cardiovascular Effects |
|---|---|---|---|---|---|
| Pancuronium | Aminosteroid | 3-5 | 60-90 | Renal (70-80%) | Tachycardia, hypertension (vagolysis) |
| Vecuronium | Aminosteroid | 3-4 | 25-40 | Hepatic/biliary | Minimal; possible opioid-potentiated bradycardia |
| Rocuronium | Aminosteroid | 1-2 (high dose) | 30-60 | Hepatic | Mild vagal blockade |
| Atracurium | Benzylisoquinoline | 2-3 | 20-35 | Hofmann (plasma hydrolysis) | Possible hypotension (histamine release) |