Recent from talks
Nothing was collected or created yet.
Symphysiotomy
View on Wikipedia| Symphysiotomy | |
|---|---|
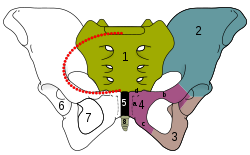
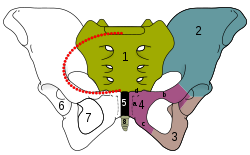 The black area marked by a "5" is the pubic symphysis, which is divided during the procedure | |
| ICD-9-CM | 73.94 |
Symphysiotomy is a surgical procedure in which the cartilage of the pubic symphysis is divided to widen the pelvis allowing childbirth when the baby has difficulty fitting through the pelvis (obstructed labour). It is also known as pelviotomy[1] and synchondrotomy.[1] It has largely been supplanted by C-sections, with the exception of certain rare obstetric emergencies or in resource poor settings. It is different from pubiotomy, where the pelvic bone itself is cut in two places, rather than cutting through the symphysis pubis joint.[2]
Introduction
[edit]Symphysiotomy was advocated in 1597 by Severin Pineau after his description of a diastasis of the pubis on a hanged pregnant woman.[3] Thus symphysiotomies became a routine surgical procedure for women experiencing an obstructed labour.[citation needed] They became less frequent in the late 20th century after the risk of maternal death from caesarean section decreased (due to improvement in techniques, hygiene, and clinical practice).[4]
Indications
[edit]The most common indications are a trapped head of a breech baby,[5][6] shoulder dystocia which does not resolve with routine manoeuvres, and obstructed labor at full cervical dilation, especially with failed vacuum extraction.[5] Use for shoulder dystocia is controversial.[5]
Currently the procedure is rarely performed in developed countries, but is still performed in "rural areas and resource-poor settings of developing countries"[7] where caesarean sections are not available, or where obstetricians may not be available to deliver subsequent pregnancies.[8] Current practice guidelines in Canada recommend symphysiotomy for trapped head during vaginal delivery of a breech birth.[9]
A 2016 meta-analysis found that in low and middle income countries, there was no difference between maternal and perinatal mortality following either symphysiotomy or C-section.[10] There was a lower risk of infection following symphysiotomy, but a higher risk of fistula, compared to C-section.[10]
Procedure
[edit]
Symphysiotomy results in a temporary increase in pelvic diameter (up to 2 centimetres (0.79 in)) by surgically dividing the ligaments of the symphysis under local anaesthesia. This procedure should be carried out only in combination with vacuum extraction.[11] Symphysiotomy can be a life-saving procedure in areas of the world where caesarean section is not feasible or immediately available as it does not require an operating theatre or "advanced" surgical skills.[5] Since this procedure does not scar the uterus, the concern of future uterine rupture that exists with cesarean section is not a factor.[12]
The procedure carries the risks of urethral and bladder injury, fistulas,[10] infection, pain, and long-term walking difficulty.[11] Symphysiotomy should, therefore, be carried out only when there is no safe alternative.[11] It is advised that this procedure should not be repeated due to the risk of gait problems and continual pain.[11] Abduction of the thighs more than 45 degrees from the midline may cause tearing of the urethra and bladder. If long-term walking difficulties and pain are reported, the patient's condition generally improves with physical therapy.[11]
Controversial practices in Ireland
[edit]In 2002 an advocacy group called Survivors of Symphysiotomy (SoS) was set up alleging religiously motivated symphysiotomies were performed without consent and against best medical practice in Ireland between 1944 and 1987.[13][14] In 2014 Ireland agreed to pay women who received the procedure compensation without admitting liability.[15]
References
[edit]- ^ a b "symphysiotomy". The American Heritage Stedman's Medical Dictionary. Archived from the original on 2014-01-07. Retrieved March 22, 2012 – via Dictionary.com.
- ^ "pubiotomy". Oxford English Dictionary (Online ed.). Oxford University Press. (Subscription or participating institution membership required.)
- ^ Dumont M: La longue et laborieuse naissance de la symphyséotomie ou de Séverin Pineau à Jean-René Sigault. J Gynecol Obstet Biol Reprod 1989;18:11-21
- ^ Bergström, S.; Lublin, H.; Molin, A. (1994). "Value of symphysiotomy in obstructed labour management and follow-up of 31 cases". Gynecologic and Obstetric Investigation. 38 (1): 31–35. doi:10.1159/000292441. ISSN 0378-7346. PMID 7959323.
- ^ a b c d Hofmeyr, G Justus; Shweni, P Mike (2012-10-17). Cochrane Pregnancy and Childbirth Group (ed.). "Symphysiotomy for feto-pelvic disproportion". Cochrane Database of Systematic Reviews. 10 (10) CD005299. doi:10.1002/14651858.CD005299.pub3. PMC 7390327. PMID 23076913.
- ^ Kotaska, Andrew; Menticoglou, Savas (August 2019). "No. 384-Management of Breech Presentation at Term". Journal of Obstetrics and Gynaecology Canada. 41 (8): 1193–1205. doi:10.1016/j.jogc.2018.12.018. PMID 31331608.
- ^ Monjok, Emmanuel; Okokon, Ita B.; Opiah, Margaret M.; Ingwu, Justin A.; Ekabua, John E.; Essien, Ekere J. (September 2012). "Obstructed labour in resource-poor settings: the need for revival of symphysiotomy in Nigeria". African Journal of Reproductive Health. 16 (3): 94–101. ISSN 1118-4841. PMID 23437503.
- ^ Verkuyl, Douwe Arie Anne (2007-03-27). "Think globally act locally: the case for symphysiotomy". PLOS Medicine. 4 (3) e71. doi:10.1371/journal.pmed.0040071. ISSN 1549-1676. PMC 1831724. PMID 17388656.
- ^ Hofmeyr, G. Justus; Shweni, P. Mike (2012-10-17). "Symphysiotomy for feto-pelvic disproportion". The Cochrane Database of Systematic Reviews. 10 (10) CD005299. doi:10.1002/14651858.CD005299.pub3. ISSN 1469-493X. PMC 7390327. PMID 23076913.
- ^ a b c Wilson, A; Truchanowicz, Eg; Elmoghazy, D; MacArthur, C; Coomarasamy, A (August 2016). "Symphysiotomy for obstructed labour: a systematic review and meta-analysis". BJOG: An International Journal of Obstetrics & Gynaecology. 123 (9): 1453–1461. doi:10.1111/1471-0528.14040. ISSN 1470-0328. PMID 27126671.
- ^ a b c d e Mathai, Matthews, ed. (2003). Managing complications in pregnancy and childbirth: a guide for midwives and doctors. Integrated management of pregnancy and childbirth (1st ed.). Geneva: WHO, RHR Department of Reproductive Health and Research. ISBN 978-92-4-154587-7. Archived from the original on 2002-08-09.
- ^ van Roosmalen, Jos (July 1990). "Safe motherhood: cesarean section or symphysiotomy?". American Journal of Obstetrics and Gynecology. 163 (1 Pt 1): 1–4. doi:10.1016/S0002-9378(11)90653-X. ISSN 0002-9378. PMID 2375330.
- ^ "SOS Ireland - survivors of symphysiotomy". Survivors of Symphysiotomy ireland. Retrieved 2018-04-16.
- ^ "Draft Report on Symphysiotomy in Ireland 1944 - 1987, Dr Oonagh Walsh"
- ^ "Symphysiotomy compensation agreed in Republic of Ireland". BBC News. 2014-07-01. Retrieved 2024-08-10.
Symphysiotomy
View on GrokipediaSymphysiotomy is an obstetric surgical procedure in which the fibrocartilaginous disc of the pubic symphysis is partially incised to enable separation of the pubic bones, thereby enlarging the pelvic outlet by about 2 cm to facilitate vaginal delivery during obstructed labor caused by feto-pelvic disproportion.[1][2] The technique, which avoids the need for general anesthesia and can be performed rapidly by trained providers, has been utilized historically in resource-constrained settings where timely cesarean section is unavailable, potentially reducing maternal mortality risks associated with prolonged labor or destructive fetal procedures.[3] While symphysiotomy confers a permanent pelvic enlargement that may benefit subsequent deliveries, empirical data from cohort studies indicate higher rates of postpartum complications such as urinary incontinence, pelvic pain, and sacroiliac joint issues compared to cesarean delivery, though vital maternal outcomes like death or severe infection appear comparable or improved in select low-resource contexts.[4][1] Long-term follow-up reveals risks of osteoarthritis and gait abnormalities in some patients, contributing to its obsolescence in high-income countries with reliable surgical infrastructure.[5] Despite these drawbacks, meta-analyses of 20th-century cases, including over 5,000 procedures, support its cautious application in emergencies where cesarean access poses greater logistical hazards, emphasizing operator skill and immediate stabilization to mitigate morbidity.[6] The procedure remains a subject of debate in global obstetrics, with advocates highlighting its life-saving potential grounded in causal mechanisms of pelvic mechanics over ideological preferences for surgical alternatives.[1][3]