Recent from talks
Nothing was collected or created yet.
CALCRL
View on WikipediaCalcitonin receptor-like (CALCRL), also known as the calcitonin receptor-like receptor (CRLR), is a human protein; it is a receptor for calcitonin gene-related peptide.[5]
Function
[edit]The protein encoded by the CALCRL gene is a G protein-coupled receptor related to the calcitonin receptor. CALCRL is linked to one of three single transmembrane domain receptor activity-modifying proteins (RAMPs) that are essential for functional activity.
The association of CALCRL with different RAMP proteins produces different receptors:[6][7]
- with RAMP1: produces a CGRP receptor
- with RAMP2: produces an adrenomedullin (AM) receptor, designated AM1[8]
- with RAMP3: produces a dual CGRP/AM receptor designated AM2
These receptors are linked to the G protein Gs,[9] which activates adenylate cyclase and activation results in the generation of intracellular cyclic adenosine monophosphate (cAMP).
CGRP receptors are found throughout the body, suggesting that the protein may modulate a variety of physiological functions in all major systems (e.g., respiratory, endocrine, gastrointestinal, immune, and cardiovascular).[10]
Wounds
[edit]In wounds, CGRP receptors found in nerve cells deactivate the immune system, to prevent collateral damage in case of a clean wound (common case). In very preliminary research, nerve blockers like e.g. lidocaine or botox have been demonstrated to block CGRP cascade, thereby allowing immune system involvement and control of pathogens, resulting in complete control and recovery.[11]
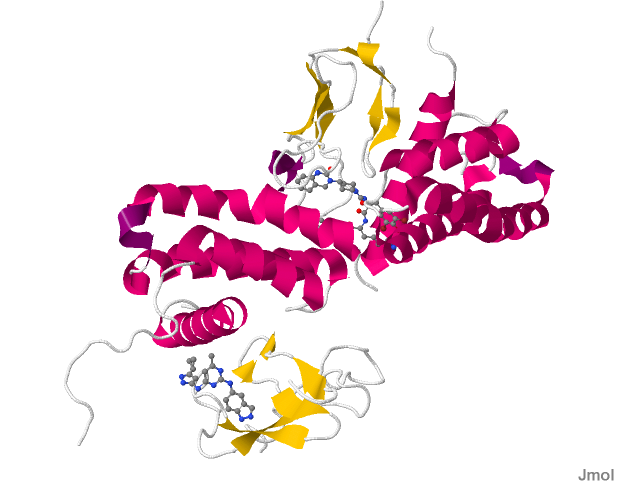
Structure
[edit]CALCRL associated with RAMP1 produces the CGRP receptor which is a trans-membrane protein receptor that is made up of four chains. Two of the four chains contain unique sequences. It is a heterodimer protein composed of two polypeptide chains differing in composition of their amino acid residues. The sequence reveals multiple hydrophobic and hydrophilic regions throughout the four chains in the protein.[12]
The CGRP family of receptors including CALCRL can couple to G-protein Gαs, Gαi and Gαq subunits to transduce their signals. Furthermore binding of ligands to CALCRL can bias coupling to these G-protein.[13] Peptide agonist bind to the extracellular loops of CALCRL. This binding in turn causes TM5 (transmembrane helix 5) and TM6 to pivot around TM3 which in turn facilitates Gαs binding.[14]
Adrenomedullin receptor
[edit]This section is empty. You can help by adding to it. (November 2017) |
Expression
[edit]The RNA expression charts show a high level in fetal lung.
This section needs expansion. You can help by adding to it. (November 2017) |
Clinical significance
[edit]Calcitonin gene-related peptide receptor antagonists are approved for the treatment of migraine.
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000064989 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000059588 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Aiyar N, Rand K, Elshourbagy NA, Zeng Z, Adamou JE, Bergsma DJ, Li Y (May 1996). "A cDNA encoding the calcitonin gene-related peptide type 1 receptor". J. Biol. Chem. 271 (19): 11325–9. doi:10.1074/jbc.271.19.11325. PMID 8626685.
- ^ McLatchie LM, Fraser NJ, Main MJ, Wise A, Brown J, Thompson N, Solari R, Lee MG, Foord SM (May 1998). "RAMPs regulate the transport and ligand specificity of the calcitonin-receptor-like receptor". Nature. 393 (6683): 333–9. Bibcode:1998Natur.393..333M. doi:10.1038/30666. PMID 9620797. S2CID 4364526.
- ^ Foord SM, Marshall FH (May 1999). "RAMPs: accessory proteins for seven transmembrane domain receptors". Trends Pharmacol. Sci. 20 (5): 184–7. doi:10.1016/S0165-6147(99)01347-4. PMID 10354609.
- ^ Kamitani S, Asakawa M, Shimekake Y, Kuwasako K, Nakahara K, Sakata T (April 1999). "The RAMP2/CRLR complex is a functional adrenomedullin receptor in human endothelial and vascular smooth muscle cells". FEBS Lett. 448 (1): 111–4. Bibcode:1999FEBSL.448..111K. doi:10.1016/S0014-5793(99)00358-0. PMID 10217420. S2CID 23729715.
- ^ "Receptor properties". SenseLab Project: Membrane properties resource. Yale University. Archived from the original on 2009-02-28. Retrieved 2008-09-28.
- ^ Arulmani, U.; et al. (2004). "Calcitonin gene-related peptide and its role in migraine pathophysiology". Eur J Pharmacol. 500 (1–3): 315–30. doi:10.1016/j.ejphar.2004.07.035. PMID 15464043.
- ^ "How the germ behind flesh-eating disease hijacks neurons to avoid immune destruction".
- ^ PDB: 3N7S; ter Haar E, Koth CM, Abdul-Manan N, Swenson L, Coll JT, Lippke JA, Lepre CA, Garcia-Guzman M, Moore JM (September 2010). "Crystal structure of the ectodomain complex of the CGRP receptor, a class-B GPCR, reveals the site of drug antagonism". Structure. 18 (9): 1083–93. doi:10.1016/j.str.2010.05.014. PMID 20826335.
- ^ Weston C, Winfield I, Harris M, Hodgson R, Shah A, Dowell SJ, Mobarec JC, Woodlock DA, Reynolds CA, Poyner DR, Watkins HA, Ladds G (October 2016). "Receptor Activity-modifying Protein-directed G Protein Signaling Specificity for the Calcitonin Gene-related Peptide Family of Receptors". The Journal of Biological Chemistry. 291 (42): 21925–21944. doi:10.1074/jbc.M116.751362. PMC 5063977. PMID 27566546.
- ^ Woolley MJ, Reynolds CA, Simms J, Walker CS, Mobarec JC, Garelja ML, Conner AC, Poyner DR, Hay DL (July 2017). "Receptor activity-modifying protein dependent and independent activation mechanisms in the coupling of calcitonin gene-related peptide and adrenomedullin receptors to Gs". Biochemical Pharmacology. 17: 30482–3. doi:10.1016/j.bcp.2017.07.005. PMC 5609567. PMID 28705698.
Further reading
[edit]- Born W, Muff R, Fischer JA (2002). "Functional interaction of G protein-coupled receptors of the adrenomedullin peptide family with accessory receptor-activity-modifying proteins (RAMP)". Microsc. Res. Tech. 57 (1): 14–22. doi:10.1002/jemt.10051. PMID 11921352. S2CID 20459079.
- Yallampalli C, Chauhan M, Thota CS, et al. (2003). "Calcitonin gene-related peptide in pregnancy and its emerging receptor heterogeneity". Trends Endocrinol. Metab. 13 (6): 263–9. doi:10.1016/s1043-2760(02)00563-5. PMID 12128288. S2CID 28476322.
- Foord SM, Craig RK (1988). "Isolation and characterisation of a human calcitonin-gene-related-peptide receptor". Eur. J. Biochem. 170 (1–2): 373–9. doi:10.1111/j.1432-1033.1987.tb13710.x. PMID 2826160.
- Skofitsch G, Jacobowitz DM (1986). "Autoradiographic distribution of 125I calcitonin gene-related peptide binding sites in the rat central nervous system". Peptides. 6 (5): 975–86. doi:10.1016/0196-9781(85)90331-6. PMID 3001670. S2CID 19435035.
- Flühmann B, Muff R, Hunziker W, et al. (1995). "A human orphan calcitonin receptor-like structure". Biochem. Biophys. Res. Commun. 206 (1): 341–7. doi:10.1006/bbrc.1995.1047. PMID 7818539.
- Aiyar N, Rand K, Elshourbagy NA, et al. (1996). "A cDNA encoding the calcitonin gene-related peptide type 1 receptor". J. Biol. Chem. 271 (19): 11325–9. doi:10.1074/jbc.271.19.11325. PMID 8626685.
- McLatchie LM, Fraser NJ, Main MJ, et al. (1998). "RAMPs regulate the transport and ligand specificity of the calcitonin-receptor-like receptor". Nature. 393 (6683): 333–9. Bibcode:1998Natur.393..333M. doi:10.1038/30666. PMID 9620797. S2CID 4364526.
- Sams A, Jansen-Olesen I (1999). "Expression of calcitonin receptor-like receptor and receptor-activity-modifying proteins in human cranial arteries". Neurosci. Lett. 258 (1): 41–4. doi:10.1016/S0304-3940(98)00844-1. PMID 9876047. S2CID 371196.
- Kamitani S, Asakawa M, Shimekake Y, et al. (1999). "The RAMP2/CRLR complex is a functional adrenomedullin receptor in human endothelial and vascular smooth muscle cells". FEBS Lett. 448 (1): 111–4. Bibcode:1999FEBSL.448..111K. doi:10.1016/S0014-5793(99)00358-0. PMID 10217420. S2CID 23729715.
- Aldecoa A, Gujer R, Fischer JA, Born W (2000). "Mammalian calcitonin receptor-like receptor/receptor activity modifying protein complexes define calcitonin gene-related peptide and adrenomedullin receptors in Drosophila Schneider 2 cells". FEBS Lett. 471 (2–3): 156–60. Bibcode:2000FEBSL.471..156A. doi:10.1016/S0014-5793(00)01387-9. PMID 10767413. S2CID 32098863.
- Frayon S, Cueille C, Gnidéhou S, et al. (2000). "Dexamethasone increases RAMP1 and CRLR mRNA expressions in human vascular smooth muscle cells". Biochem. Biophys. Res. Commun. 270 (3): 1063–7. doi:10.1006/bbrc.2000.2552. PMID 10772950.
- Kuwasako K, Shimekake Y, Masuda M, et al. (2000). "Visualization of the calcitonin receptor-like receptor and its receptor activity-modifying proteins during internalization and recycling". J. Biol. Chem. 275 (38): 29602–9. doi:10.1074/jbc.M004534200. PMID 10882736.
- Evans BN, Rosenblatt MI, Mnayer LO, et al. (2000). "CGRP-RCP, a novel protein required for signal transduction at calcitonin gene-related peptide and adrenomedullin receptors". J. Biol. Chem. 275 (40): 31438–43. doi:10.1074/jbc.M005604200. PMID 10903324.
- Hilairet S, Foord SM, Marshall FH, Bouvier M (2001). "Protein-protein interaction and not glycosylation determines the binding selectivity of heterodimers between the calcitonin receptor-like receptor and the receptor activity-modifying proteins". J. Biol. Chem. 276 (31): 29575–81. doi:10.1074/jbc.M102722200. PMID 11387328.
- Kamitani S, Sakata T (2001). "Glycosylation of human CRLR at Asn123 is required for ligand binding and signaling". Biochim. Biophys. Acta. 1539 (1–2): 131–9. doi:10.1016/S0167-4889(01)00100-8. PMID 11389975.
- Nikitenko LL, Brown NS, Smith DM, et al. (2001). "Differential and cell-specific expression of calcitonin receptor-like receptor and receptor activity modifying proteins in the human uterus". Mol. Hum. Reprod. 7 (7): 655–64. doi:10.1093/molehr/7.7.655. PMID 11420389.
- Hilairet S, Bélanger C, Bertrand J, et al. (2001). "Agonist-promoted internalization of a ternary complex between calcitonin receptor-like receptor, receptor activity-modifying protein 1 (RAMP1), and beta-arrestin". J. Biol. Chem. 276 (45): 42182–90. doi:10.1074/jbc.M107323200. PMID 11535606.
- Aiyar N, Disa J, Pullen M, Nambi P (2002). "Receptor activity modifying proteins interaction with human and porcine calcitonin receptor-like receptor (CRLR) in HEK-293 cells". Mol. Cell. Biochem. 224 (1–2): 123–33. doi:10.1023/A:1011907328682. PMID 11693189. S2CID 26037173.
- Hagner S, Haberberger RV, Overkamp D, et al. (2002). "Expression and distribution of calcitonin receptor-like receptor in human hairy skin". Peptides. 23 (1): 109–16. doi:10.1016/S0196-9781(01)00586-1. PMID 11814625. S2CID 6936664.
- Hill H, Pioszak A (2013). "Bacterial expression and purification of a heterodimeric adrenomedullin receptor extracellular domain complex using DsbC-assisted disulfide shuffling". Protein Expr. Purif. 88 (1): 107–13. doi:10.1016/j.pep.2012.11.019. PMC 3568255. PMID 23247088.
External links
[edit]- "Calcitonin receptors: CALCRL". IUPHAR Database of Receptors and Ion Channels. International Union of Basic and Clinical Pharmacology.
- calcitonin+receptor-like+receptor at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- CALCRL human gene location in the UCSC Genome Browser.
- CALCRL human gene details in the UCSC Genome Browser.