Recent from talks
Nothing was collected or created yet.
Tumor necrosis factor receptor 2
View on Wikipedia
Tumor necrosis factor receptor 2 (TNFR2), also known as tumor necrosis factor receptor superfamily member 1B (TNFRSF1B) and CD120b, is one of two membrane receptors that binds tumor necrosis factor-alpha (TNFα).[5][6] Like its counterpart, tumor necrosis factor receptor 1 (TNFR1), the extracellular region of TNFR2 consists of four cysteine-rich domains which allow for binding to TNFα.[7][8] TNFR1 and TNFR2 possess different functions when bound to TNFα due to differences in their intracellular structures, such as TNFR2 lacking a death domain (DD).[7]
Function
[edit]The protein encoded by this gene is a member of the tumor necrosis factor receptor superfamily, which also contains TNFRSF1A. This protein and TNF-receptor 1 form a heterocomplex that mediates the recruitment of two anti-apoptotic proteins, c-IAP1 and c-IAP2, which possess E3 ubiquitin ligase activity. The function of IAPs in TNF-receptor signalling is unknown, however, c-IAP1 is thought to potentiate TNF-induced apoptosis by the ubiquitination and degradation of TNF-receptor-associated factor 2 (TRAF2), which mediates anti-apoptotic signals. Knockout studies in mice also suggest a role of this protein in protecting neurons from apoptosis by stimulating antioxidative pathways.[9]
Clinical significance
[edit]CNS
[edit]At least partly because TNFR2 has no intracellular death domain, TNFR2 is neuroprotective.[10]
Patients with schizophrenia have increased levels of soluble tumor necrosis factor receptor 2 (sTNFR2).[11]
Cancer
[edit]Targeting of TNFR2 in tumor cells is associated with increased tumor cell death and decreased progression of tumor cell growth.[8]
Increased expression of TNFR2 is found in breast cancer, cervical cancer, colon cancer, and renal cancer.[8] A link between the expression of TNFR2 in tumor cells and late-stage cancer has been discovered.[8] TNFR2 plays a significant role in tumor cell growth as it has been found that the loss of TNFR2 expression is linked with increased death of associated tumor cells and a significant standstill of further growth.[8] There is therapeutic potential in the targeting of TNFR2 for cancer treatments through TNFR2 inhibition.[12]
Systemic Lupus Erythematous (SLE)
[edit]A small scale study of 289 Japanese patients suggested a minor increased predisposition from an amino acid substitution of the 196 allele at exon 6. Genomic testing of 81 SLE patients and 207 healthy patients in a Japanese study showed 37% of SLE patients had a polymorphism on position 196 of exon 6 compared to 18.8% of healthy patients. The TNFR2 196R allele polymorphism suggests that even one 196R allele results in increased risk for SLE.[13]
Interactions
[edit]References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000028137 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000028599 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Schall TJ, Lewis M, Koller KJ, Lee A, Rice GC, Wong GH, et al. (April 1990). "Molecular cloning and expression of a receptor for human tumor necrosis factor". Cell. 61 (2): 361–370. doi:10.1016/0092-8674(90)90816-W. PMID 2158863. S2CID 36187863.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Santee SM, Owen-Schaub LB (August 1996). "Human tumor necrosis factor receptor p75/80 (CD120b) gene structure and promoter characterization". The Journal of Biological Chemistry. 271 (35): 21151–21159. doi:10.1074/jbc.271.35.21151. PMID 8702885.
- ^ a b Wang J, Al-Lamki RS (2013-11-17). "Tumor necrosis factor receptor 2: its contribution to acute cellular rejection and clear cell renal carcinoma". BioMed Research International. 2013 821310. doi:10.1155/2013/821310. PMC 3848079. PMID 24350291.
- ^ a b c d e Sheng Y, Li F, Qin Z (2018). "TNF Receptor 2 Makes Tumor Necrosis Factor a Friend of Tumors". Frontiers in Immunology. 9 1170. doi:10.3389/fimmu.2018.01170. PMC 5985372. PMID 29892300.
- ^ "Entrez Gene: TNFRSF1B tumor necrosis factor receptor superfamily, member 1B". Retrieved 8 May 2017.
- ^ Chadwick W, Magnus T, Martin B, Keselman A, Mattson MP, Maudsley S (October 2008). "Targeting TNF-alpha receptors for neurotherapeutics". Trends in Neurosciences. 31 (10): 504–511. doi:10.1016/j.tins.2008.07.005. PMC 2574933. PMID 18774186.
- ^ Kudo N, Yamamori H, Ishima T, Nemoto K, Yasuda Y, Fujimoto M, et al. (July 2018). "Plasma Levels of Soluble Tumor Necrosis Factor Receptor 2 (sTNFR2) Are Associated with Hippocampal Volume and Cognitive Performance in Patients with Schizophrenia". The International Journal of Neuropsychopharmacology. 21 (7): 631–639. doi:10.1093/ijnp/pyy013. PMC 6031046. PMID 29529289.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Medler J, Wajant H (April 2019). "Tumor necrosis factor receptor-2 (TNFR2): an overview of an emerging drug target". Expert Opinion on Therapeutic Targets. 23 (4): 295–307. doi:10.1080/14728222.2019.1586886. PMID 30856027. S2CID 75139844.
- ^ Komata T, Tsuchiya N, Matsushita M, Hagiwara K, Tokunaga K (June 1999). "Association of tumor necrosis factor receptor 2 (TNFR2) polymorphism with susceptibility to systemic lupus erythematosus". Tissue Antigens. 53 (6): 527–533. doi:10.1034/j.1399-0039.1999.530602.x. PMID 10395102.
- ^ Bouwmeester T, Bauch A, Ruffner H, Angrand PO, Bergamini G, Croughton K, et al. (February 2004). "A physical and functional map of the human TNF-alpha/NF-kappa B signal transduction pathway". Nature Cell Biology. 6 (2): 97–105. doi:10.1038/ncb1086. PMID 14743216. S2CID 11683986.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Song HY, Donner DB (August 1995). "Association of a RING finger protein with the cytoplasmic domain of the human type-2 tumour necrosis factor receptor". The Biochemical Journal. 309 (3): 825–829. doi:10.1042/bj3090825. PMC 1135706. PMID 7639698.
- ^ Takeuchi M, Rothe M, Goeddel DV (August 1996). "Anatomy of TRAF2. Distinct domains for nuclear factor-kappaB activation and association with tumor necrosis factor signaling proteins". The Journal of Biological Chemistry. 271 (33): 19935–19942. doi:10.1074/jbc.271.33.19935. PMID 8702708.
- ^ Hostager BS, Bishop GA (April 2002). "Role of TNF receptor-associated factor 2 in the activation of IgM secretion by CD40 and CD120b". Journal of Immunology. 168 (7): 3318–3322. doi:10.4049/jimmunol.168.7.3318. PMID 11907088.
- ^ Rothe M, Xiong J, Shu HB, Williamson K, Goddard A, Goeddel DV (August 1996). "I-TRAF is a novel TRAF-interacting protein that regulates TRAF-mediated signal transduction". Proceedings of the National Academy of Sciences of the United States of America. 93 (16): 8241–8246. Bibcode:1996PNAS...93.8241R. doi:10.1073/pnas.93.16.8241. PMC 38654. PMID 8710854.
- ^ Marsters SA, Ayres TM, Skubatch M, Gray CL, Rothe M, Ashkenazi A (May 1997). "Herpesvirus entry mediator, a member of the tumor necrosis factor receptor (TNFR) family, interacts with members of the TNFR-associated factor family and activates the transcription factors NF-kappaB and AP-1". The Journal of Biological Chemistry. 272 (22): 14029–14032. doi:10.1074/jbc.272.22.14029. PMID 9162022.
- ^ Carpentier I, Coornaert B, Beyaert R (October 2008). "Smurf2 is a TRAF2 binding protein that triggers TNF-R2 ubiquitination and TNF-R2-induced JNK activation". Biochemical and Biophysical Research Communications. 374 (4): 752–757. Bibcode:2008BBRC..374..752C. doi:10.1016/j.bbrc.2008.07.103. PMID 18671942.
- ^ Pype S, Declercq W, Ibrahimi A, Michiels C, Van Rietschoten JG, Dewulf N, et al. (June 2000). "TTRAP, a novel protein that associates with CD40, tumor necrosis factor (TNF) receptor-75 and TNF receptor-associated factors (TRAFs), and that inhibits nuclear factor-kappa B activation". The Journal of Biological Chemistry. 275 (24): 18586–18593. doi:10.1074/jbc.M000531200. PMID 10764746.
{{cite journal}}: CS1 maint: overridden setting (link)
Further reading
[edit]- Kollias G, Kontoyiannis D (2003). "Role of TNF/TNFR in autoimmunity: specific TNF receptor blockade may be advantageous to anti-TNF treatments". Cytokine & Growth Factor Reviews. 13 (4–5): 315–321. doi:10.1016/S1359-6101(02)00019-9. PMID 12220546.
- Holtmann MH, Schuchmann M, Zeller G, Galle PR, Neurath MF (2003). "The emerging distinct role of TNF-receptor 2 (p80) signaling in chronic inflammatory disorders". Archivum Immunologiae et Therapiae Experimentalis. 50 (4): 279–288. PMID 12371624.
- Horiuchi T, Kiyohara C, Tsukamoto H, Sawabe T, Furugo I, Yoshizawa S, et al. (March 2007). "A functional M196R polymorphism of tumour necrosis factor receptor type 2 is associated with systemic lupus erythematosus: a case-control study and a meta-analysis". Annals of the Rheumatic Diseases. 66 (3): 320–324. doi:10.1136/ard.2006.058917. PMC 1856025. PMID 17028114.
{{cite journal}}: CS1 maint: overridden setting (link)
External links
[edit]- CD120b+Antigen at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
Tumor necrosis factor receptor 2
View on GrokipediaMolecular Biology
Gene Characteristics
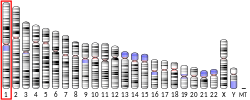
The TNFRSF1B gene, which encodes tumor necrosis factor receptor 2 (TNFR2), is located on the short arm of human chromosome 1 at cytogenetic band p36.22, spanning genomic coordinates 12,166,991–12,209,220 (GRCh38 assembly), a region of approximately 42 kb.[1] The orthologous gene in mice, Tnfrsf1b, resides on chromosome 4 at positions 144,940,033–144,973,440 (GRCm39 assembly).[6] The gene consists of 10 exons in its canonical transcript (ENST00000376259.9), encoding a 461-amino-acid precursor protein that includes a signal peptide, extracellular domains, a transmembrane region, and an intracellular signaling domain. Alternative splicing of TNFRSF1B transcripts can produce soluble isoforms of TNFR2 (sTNFR2), which lack the transmembrane and cytoplasmic domains and function as decoy receptors to modulate TNF signaling.[7] TNFRSF1B exhibits constitutive low-level expression across most human tissues, with higher baseline levels in placenta, lung, and immune cells such as T lymphocytes and endothelial cells. Its expression is upregulated by inflammatory cytokines including TNF-α, IL-1β, and IFN-γ, which bind to promoter regions and activate distal enhancers to drive transcription in response to immune challenges.[8] Tissue-specific patterns are regulated by cis-regulatory elements, including NF-κB-responsive promoters and inducible enhancers that integrate signals from the inflammatory microenvironment.[9] Evolutionary conservation of TNFRSF1B is evident across vertebrates, with over 300 orthologs identified, reflecting its fundamental role in inflammation and immune regulation; for example, human and mouse proteins share approximately 62% amino acid sequence identity, with higher similarity (>80%) in the extracellular cysteine-rich domains critical for ligand binding.[10]Protein Structure
Tumor necrosis factor receptor 2 (TNFR2), also known as TNFRSF1B, is a type I transmembrane glycoprotein composed of 439 amino acids in its mature form following cleavage of the N-terminal signal peptide, with an approximate molecular weight of 75 kDa due to extensive glycosylation.[11] The protein's architecture is divided into three principal regions: an extracellular ligand-binding domain, a transmembrane-spanning segment, and an intracellular signaling domain. This organization facilitates TNFR2's role in transducing signals from the cytokine tumor necrosis factor alpha (TNF-α), encoded by the TNFRSF1B gene (see Gene Characteristics).[12] The extracellular domain encompasses the first 235 amino acids and is characterized by four tandem cysteine-rich domains (CRDs 1–4), each approximately 40 amino acids long and stabilized by disulfide bonds formed by conserved cysteine residues. CRD1 and CRD4 contribute to overall structural integrity and ligand positioning, while CRD2 and CRD3 are essential for conferring specificity and high-affinity binding to membrane-bound TNF-α homotrimers, enabling TNFR2's preferential activation by transmembrane forms of the ligand over soluble TNF-α (see Ligand Binding and Activation).[4] The domain also contains multiple N-linked glycosylation sites, which promote protein stability, prevent aggregation, and modulate ligand accessibility.[13] The transmembrane domain consists of a single α-helical stretch of about 30 hydrophobic amino acids that anchors TNFR2 in the plasma membrane, facilitating signal transmission across the lipid bilayer.[14] In contrast, the intracellular domain comprises the C-terminal 174 amino acids and notably lacks a death domain, unlike its counterpart TNFR1, which precludes direct activation of caspase-dependent apoptosis pathways.[11] Instead, this region is enriched with motifs for adaptor protein recruitment, including multiple TRAF-binding sites conforming to the consensus sequence PXQXT/S (where X is any amino acid), particularly prominent near the membrane-proximal area, which selectively engage TRAF2 to initiate non-canonical NF-κB and MAPK signaling.[15] Prior to ligand engagement, TNFR2 assembles into constitutive dimers via interactions in the pre-ligand assembly domain (PLAD) within CRD1, maintaining a poised state on the cell surface.[16] Ligand binding induces higher-order trimerization, clustering three receptor dimers around a single TNF-α trimer and stabilizing the signaling complex through conformational changes in the transmembrane and intracellular domains.[16] This dynamic oligomerization is crucial for amplifying downstream signals, with glycosylation further enhancing receptor half-life and functional integrity.[13]Mechanism of Action
Ligand Binding and Activation
Tumor necrosis factor receptor 2 (TNFR2) primarily interacts with tumor necrosis factor-alpha (TNF-α) as its main ligand, binding both membrane-bound and soluble forms, with a dissociation constant (K_d) of approximately 0.42 nM for soluble TNF-α, which represents lower affinity compared to TNFR1 but higher affinity for the membrane-bound form.[17] TNFR2 also binds lymphotoxin-α (LT-α) homotrimers.[4] TNFR2 also binds progranulin, which acts as an antagonist to TNF-α signaling.[18] The binding mechanism involves the trimeric TNF-α ligand engaging three TNFR2 molecules simultaneously, which induces a conformational change in the receptor extracellular domains and promotes receptor clustering on the cell surface.[19] This interaction primarily occurs through cysteine-rich domains (CRDs) 2 and 3 of TNFR2, while CRD4 contributes to affinity and CRD1 serves to stabilize the complex but is not essential for achieving high-affinity binding.[4] Upon ligand binding, TNFR2 undergoes trimerization that exposes its intracellular signaling domain, initiating activation; however, TNFR2 can also exhibit low-level constitutive signaling through pre-formed dimers mediated by the pre-ligand assembly domain (PLAD) within CRD1.[20] Additionally, activation can be regulated by ectodomain shedding, where the metalloproteinase ADAM17 (also known as TACE) cleaves the extracellular portion of TNFR2, generating a soluble form that acts as a decoy receptor to sequester TNF-α and attenuate signaling.[21] TNFR2 demonstrates selectivity by preferentially binding membrane-bound TNF-α over the soluble form, in contrast to TNFR1 which favors soluble TNF-α, thereby enabling context-specific activation in cell-cell interactions.[22]Downstream Signaling Pathways
Upon ligand-induced trimerization, TNFR2 recruits adaptor proteins TRAF2 and TRAF5 through specific intracellular binding motifs, initiating intracellular signaling without involvement of RIPK1 due to the absence of a death domain.[4] This recruitment assembles a signaling complex that activates the canonical NF-κB pathway, where TRAF2 associates with cIAP1/2 to mediate K63-linked ubiquitination of downstream effectors, leading to phosphorylation and activation of the IKK complex.[23] The activated IKK phosphorylates IκBα, resulting in its degradation and nuclear translocation of p65/RelA-p50 dimers to drive transcription of pro-survival and inflammatory genes.[4] Additionally, TNFR2 promotes non-canonical NF-κB activation by facilitating TRAF2-cIAP1/2 degradation via K48-linked ubiquitination, which stabilizes NIK and enables IKKα-mediated processing of p100 to p52, culminating in RelB-p52 dimer translocation.[23] TNFR2 signaling branches into pro-survival pathways, including activation of the MAPK cascade through TRAF2, which stimulates ERK, JNK, and p38 kinases to promote cell proliferation and cytokine production.[23] The PI3K/Akt pathway is also engaged downstream of TNFR2, enhancing cell survival, migration, and metabolic reprogramming via phosphorylation of Akt and downstream targets like mTOR.[4] Furthermore, the TRAF2-cIAP1/2 complex exerts anti-apoptotic effects by ubiquitinating and degrading pro-apoptotic substrates, such as caspases and RIPK1, while upregulating anti-apoptotic proteins like cFLIP; the lack of a death domain in TNFR2 precludes caspase-8 recruitment and activation, reinforcing survival signals.[24] These mechanisms collectively inhibit extrinsic apoptosis and support tissue repair. Crosstalk between TNFR2 and TNFR1 occurs through shared TRAF2 and cIAP1/2 adaptors, where TNFR2 can amplify TNFR1-mediated canonical NF-κB signaling under co-stimulation but also deplete TRAFs to modulate cell fate.[4] Outcomes are context-dependent: in regulatory T cells (Tregs), TNFR2 drives proliferation and suppressive function via NF-κB and PI3K/Akt, whereas in macrophages, it can promote inflammatory responses through MAPK and NF-κB activation.[25]Biological Roles
Immune System Regulation
TNFR2 plays a pivotal role in modulating T cell responses, particularly through its selective expression on regulatory T cells (Tregs), where it promotes their expansion, survival, and suppressive function. TNFR2 signaling prevents DNA methylation at the Foxp3 promoter, thereby stabilizing Foxp3 expression and enabling Tregs to resolve inflammation while preventing dedifferentiation.[26] In TNFR2-deficient models, Tregs exhibit reduced Foxp3 stability and impaired suppressive capacity, underscoring TNFR2's necessity for Treg homeostasis.[27] TNF-α binding to TNFR2 activates these CD4⁺Foxp3⁺TNFR2⁺ Tregs, which represent a highly suppressive subset comprising about 40% of peripheral Tregs in mice, enhancing their proliferation via non-canonical NF-κB pathways that support IL-2-induced expansion.[28][29] In myeloid cells, TNFR2 drives anti-inflammatory polarization and functional maturation. For macrophages, TNFR2 activation by progranulin (PGRN) or granulin (GRN) upregulates M2-like phenotypes, promoting tissue repair and dampening excessive inflammation in contexts such as pulmonary tuberculosis and periodontal disease.[30][31] This shift involves enhanced expression of anti-inflammatory markers and reduced pro-inflammatory cytokine output, balancing immune responses. In dendritic cells (DCs), TNFR2 contributes to survival and modulates cytokine production, including IL-6 and IL-10, which support tolerogenic functions and prevent overactivation during immune challenges.[32] TNFR2 also influences B cell dynamics, particularly in supporting antibody production. Expression of TNFR2 on proliferating B cells and plasma blasts correlates with increased IL-10 secretion and enhanced cell viability, facilitating humoral immunity without excessive inflammation.[33] This receptor identifies IL-10-producing regulatory B cells, which help maintain immune tolerance.[34] Overall, TNFR2 balances pro- and anti-inflammatory responses by preferentially activating immunosuppressive populations, making it critical for peripheral tolerance induction. Recent studies highlight its role in allergen tolerance, where TNFR2 signaling on immune cells promotes resolution of allergic inflammation and sustains long-term unresponsiveness to antigens.[35] This regulatory function ensures immune homeostasis, preventing autoimmunity while allowing adaptive responses.Tissue Protection and Homeostasis
TNFR2 plays a critical role in endothelial function by promoting angiogenesis and maintaining vascular integrity, particularly in response to ischemic conditions. In endothelial cells, TNFR2 activation upregulates survival and migration pathways through TRAF2-NF-κB signaling and Bmx/Etk transactivation of VEGF receptor 2, enhancing vessel maturation and perfusion recovery post-ischemia.[36] This receptor also protects against ischemia-reperfusion injury in the myocardium by mediating STAT3, SOCS3, and VEGF expression, which limits JNK activation and inflammatory cytokine release like IL-1β, thereby improving cardiac functional recovery.[37] Furthermore, TNFα priming of endothelial progenitor cells via TNFR2 boosts their immunosuppressive properties and pro-angiogenic capacity, supporting vascular homeostasis by suppressing T-cell activation and promoting endothelial repair without excessive inflammation.[38] In epithelial tissues, TNFR2 supports barrier function and maintenance in both the gut and skin. Physiological levels of TNFα acting through TNFR2 enhance intestinal epithelial cell migration via Src-dependent FAK phosphorylation, facilitating wound closure and preserving mucosal integrity independent of proliferation or apoptosis.[39] During colitis-induced injury, upregulated TNFR2 in colonic epithelium terminates excessive regenerative signaling, such as Ly6a-mediated hyperproliferation, to promote ulcer healing and restore secretory cell differentiation essential for barrier repair.[40] In the skin, TNFR2 signaling in keratinocytes confers anti-apoptotic protection against oxidative stress, reducing neutrophil infiltration and supporting tissue homeostasis during injury.[41] TNFR2 contributes to neuronal support through neuroprotective signaling in glial cells, aiding homeostasis during development and injury. In astrocytes, TNFR2 activation promotes myelin regeneration via cytokine induction, counteracting neuroinflammation.[42] Microglial TNFR2 similarly modulates inflammatory responses post-central nervous system injury, enhancing neuroprotection through regulation of immune signaling.[42] These glial mechanisms support neuronal survival and cerebrovascular maturation, as seen in Hmgb1-mediated astrocyte regulation.[43] In metabolic regulation, TNFR2 modulates insulin sensitivity in adipocytes by reflecting TNFα activity and influencing pro-inflammatory pathways. Elevated soluble TNFR2 levels correlate positively with insulin resistance (HOMA-IR), independent of adiposity, through interactions with adipokines like resistin and adiponectin that alter lipid flux and glucose uptake in adipose tissue.[44] This signaling prevents excessive inflammation by balancing TNFα effects, though TNFR2's role is less dominant than TNFR1 in directly impairing insulin pathways, contributing to overall metabolic homeostasis in obesity.[45]Protein Interactions
Key Binding Partners
Tumor necrosis factor receptor 2 (TNFR2) primarily interacts with intracellular adaptor proteins from the tumor necrosis factor receptor-associated factor (TRAF) family to initiate signaling. The key adaptor is TRAF2, which binds directly to the intracellular tail of TNFR2 via a conserved PXQXT motif, enabling recruitment and activation of downstream pathways such as NF-κB.[46] TRAF2 is essential for TNFR2-mediated NF-κB activation and plays a central role in promoting cell survival and proliferation.[47] TRAF1 and TRAF3 also bind directly to TNFR2 via similar motifs; TRAF1 forms heterodimers with TRAF2 to enhance survival signaling, while TRAF3 contributes to non-canonical NF-κB activation.[47] Members of the inhibitor of apoptosis protein (IAP) family, specifically cIAP1 and cIAP2, are recruited to TNFR2 indirectly through their association with TRAF2. These proteins function as E3 ubiquitin ligases, adding K63-linked ubiquitin chains to signaling components, which amplifies NF-κB signaling and enhances signal transduction efficiency.[47] This ubiquitination activity is critical for the non-degradative modification that sustains TNFR2-dependent cellular responses. TNFR2 signaling also involves indirect interactions with IKKγ (also known as NEMO), which is part of the IKK complex recruited via TRAF2 to facilitate canonical NF-κB activation.[47] NEMO recognizes polyubiquitin chains generated by TRAF2 and cIAPs, thereby linking TNFR2 to the kinase complex that phosphorylates IκB for its degradation. Additionally, TNFR2 exhibits potential cross-talk with TNFR1 through shared ligands like TNF-α, but maintains distinct binding partners that prevent overlap in primary signaling complexes.[48] As a soluble modulator, TNF-α-converting enzyme (TACE), also known as ADAM17, interacts with the extracellular domain of TNFR2 to cleave and release its ectodomain, generating a soluble form that regulates ligand availability and attenuates membrane-bound signaling.[47] This shedding mechanism helps fine-tune TNFR2 activity in response to inflammatory cues.Signaling Complex Assembly
Upon ligand binding, tumor necrosis factor receptor 2 (TNFR2) assembles into a primary signaling complex as a homotrimer bound to trimeric TNF-α, recruiting tumor necrosis factor receptor-associated factor 2 (TRAF2) and cellular inhibitors of apoptosis 1 and 2 (cIAP1/2) to its intracellular domains via conserved TRAF-binding motifs.[49] This TRAF2-cIAP1/2 platform facilitates non-canonical NF-κB activation by stabilizing NIK through reduced ubiquitination and degradation, while cIAP1/2 mediate K63-linked ubiquitination on TRAF2 lysine residues, creating docking sites for the TAK1 kinase complex to propagate downstream signals.[4][50] The assembly occurs rapidly post-ligand engagement, with TRAF2 binding directly to the receptor's cytoplasmic tail, followed by cIAP recruitment that enhances complex stability without involving death domain adaptors like TRADD, distinguishing it from TNFR1 complexes.[49] Heterocomplexes form when TNFR2 associates with TNFR1 in trans, often via membrane-bound TNF on adjacent cells, enabling cooperative signaling that modulates pro-survival outcomes such as enhanced NF-κB and MAPK activation.[51] This interaction depletes shared adaptors like TRAF2 from TNFR1 complexes, shifting TNFR1 toward pro-apoptotic signaling while amplifying TNFR2-mediated cytoprotection.[52] Localization to lipid rafts further potentiates these heterocomplexes, concentrating TNFR2 and associated TRAF2 in cholesterol-enriched domains to boost MAPK pathway activation, including JNK and p38, essential for inflammatory and proliferative responses.[53] Complex assembly is dynamically regulated by post-translational modifications, including phosphorylation of TRAF2 by kinases like PKC, which fine-tunes IKK recruitment and signal duration.[54] Disassembly is controlled by deubiquitinases such as CYLD, which removes K63-linked ubiquitin chains from TRAF2 and receptor-proximal components, terminating signaling and preventing excessive inflammation. These regulatory steps ensure transient complex formation, with phosphorylation promoting assembly and deubiquitination facilitating rapid turnover. Soluble variants of TNFR2, generated by proteolytic shedding or alternative splicing, form non-signaling complexes that act as decoys, binding free TNF-α trimers with high affinity to sequester ligand and inhibit membrane TNFR activation without intracellular transduction.[19] These soluble TNFR2 (sTNFR2) complexes circulate systemically, modulating TNF bioavailability and contributing to immune homeostasis by neutralizing soluble TNF while sparing membrane-bound forms that preferentially activate TNFR2.Clinical Relevance
Neurological Disorders
In schizophrenia, elevated levels of soluble TNFR2 in serum have been observed, correlating with greater symptom severity as measured by clinical scales such as the Positive and Negative Syndrome Scale.[55] Genetic variants in the TNFRSF1B gene encoding TNFR2, such as the rs1061622 polymorphism, are associated with increased susceptibility to schizophrenia, potentially through altered inflammatory responses in the central nervous system.[56] TNFR2 plays a protective role in neuroinflammation, as demonstrated in experimental models of multiple sclerosis where selective agonism of TNFR2 reduces demyelination, limits excessive microglial activation, and attenuates proinflammatory cytokine release in the brain.[57] In Alzheimer's disease, TNFR2 exhibits a dual function: while chronic activation can contribute to pro-amyloidogenic processes and synaptic potentiation deficits in hippocampal neurons of disease models, targeted TNFR2 stimulation decreases amyloid-β production rates and mitigates neuropathological features like plaque burden.[58][59] During ischemic stroke, TNFR2 deficiency, particularly in microglia, exacerbates outcomes in preclinical models, leading to larger infarct volumes, heightened neuroinflammation, and worsened motor and cognitive recovery, especially in females.[60] Conversely, TNFR2 agonism enhances neuronal survival post-stroke by promoting antioxidative mechanisms, including the activation of the Nrf2 pathway to counteract oxidative stress and support tissue repair.[61][62] Recent investigations as of 2025 highlight TNFR2's role in hippocampal function, where astroglial TNFR2 signaling regulates synaptic plasticity in a sex-dependent manner, potentially relevant to neuropsychiatric conditions.[63][64][65] This modulation underscores TNFR2's neuroprotective potential in mitigating symptoms linked to central imbalances.Cancer
Tumor necrosis factor receptor 2 (TNFR2) is frequently overexpressed in various solid tumors, including breast, colon, cervical, and renal cancers, where it contributes to oncogenic signaling. In breast cancer, elevated TNFR2 expression correlates with larger tumor size and advanced clinical stage, promoting cell survival and resistance to apoptosis. Similarly, in colon cancer, TNFR2 overexpression enhances tumor cell proliferation and colony formation through activation of the PI3K/AKT pathway. In cervical and renal cancers, TNFR2 is expressed on malignant cells, facilitating survival signals that support tumor progression. A key mechanism underlying this pro-tumorigenic effect involves TNFR2-mediated activation of the non-canonical NF-κB pathway, which drives proliferation and inhibits apoptosis in tumor cells across multiple solid malignancies. Within the tumor microenvironment, TNFR2 exacerbates immune evasion by enhancing regulatory T cell (Treg) infiltration and promoting M2-like polarization of tumor-associated macrophages (TAMs). TNFR2 expression on Tregs sustains their immunosuppressive function, leading to increased tumor-infiltrating Tregs that suppress anti-tumor CD8+ T cell responses, as observed in pancreatic ductal adenocarcinoma and colorectal cancer models. Concurrently, TNFR2 signaling in macrophages induces M2 polarization, characterized by elevated IL-10 production and reduced pro-inflammatory cytokine release, further dampening immune surveillance. This dual action fosters an immunosuppressive niche conducive to tumor growth. Additionally, TNFR2 on endothelial cells activates pathways that promote metastasis by enhancing vascular permeability and adhesion molecule expression, facilitating tumor cell extravasation in breast and colorectal cancers. TNFR2 also drives angiogenesis by upregulating vascular endothelial growth factor (VEGF) and matrix metalloproteinases (MMPs) in the stromal compartment. Activation of TNFR2 in stromal cells, including fibroblasts and endothelial cells, induces VEGF expression via HIF-1α stabilization and NF-κB signaling, promoting neovascularization essential for nutrient supply in hypoxic tumors. MMPs, such as MMP-9, are similarly elevated through TNFR2-dependent pathways, enabling extracellular matrix remodeling to support vessel sprouting in colorectal and breast cancers. High TNFR2 expression serves as a negative prognostic indicator in solid tumors, correlating with reduced overall survival and poorer outcomes in patients with breast, colorectal, and renal cancers. Meta-analyses across multiple cohorts confirm that elevated TNFR2 levels in tumor tissues or serum predict advanced disease stages and increased recurrence risk. In contrast, TNFR2 does not exhibit a prominent pro-tumorigenic role in hematological cancers, where its signaling more often sensitizes malignant cells to apoptosis-inducing therapies.Autoimmune Diseases
Tumor necrosis factor receptor 2 (TNFR2) has been implicated in the pathogenesis of systemic lupus erythematosus (SLE), where genetic variations in its gene, TNFRSF1B, influence disease susceptibility. Specifically, the 196R allele polymorphism of TNFRSF1B is associated with increased risk of SLE in Japanese populations, with a frequency of 37% in patients compared to 18.8% in healthy controls.[66] Additionally, elevated levels of soluble TNFR2 (sTNFR2) serve as a biomarker for disease activity and renal involvement in SLE, correlating with lupus nephritis progression and long-term outcomes.[67] In rheumatoid arthritis (RA), TNFR2 expressed on synovial fibroblasts contributes to the amplification of inflammation by promoting proinflammatory gene expression through pathways like STAT1, exacerbating joint damage during active disease phases.[68] Conversely, TNFR2 signaling on regulatory T cells (Tregs) exerts protective effects by enhancing Treg expansion and suppressive function, aiding in the resolution of inflammation in later stages.[69] TNFR2 also plays a role in other autoimmune conditions, such as inflammatory bowel disease (IBD), where it disrupts gut homeostasis by altering colonic epithelial cell function and barrier integrity, thereby promoting chronic inflammation.[70] In osteoarthritis, TNFRSF1B mediates TNF-α-induced inhibition of chondrogenic differentiation in stem cells via RELA and OPA1 upregulation, contributing to cartilage degradation through the TNF pathway.[71] Overall, TNFR2 exhibits a dual nature in autoimmune diseases, driving pro-inflammatory responses in early or acute phases while supporting regulatory mechanisms, such as Treg-mediated suppression, during chronic stages to maintain immune balance.[72]Therapeutic Strategies
Therapeutic strategies targeting tumor necrosis factor receptor 2 (TNFR2) focus on modulating its signaling to address diseases where it plays a dual role in inflammation and immune regulation. Antagonists and agonists represent the primary approaches, with small molecules emerging as complementary options to fine-tune TNFR2 activity. These interventions aim to exploit TNFR2's context-specific effects, such as promoting regulatory T cell (Treg) expansion in autoimmunity or inhibiting tumor-supportive functions in cancer, while navigating challenges like off-target impacts on related pathways.[5] Antagonists, including monoclonal antibodies, block TNFR2 to disrupt its pro-tumorigenic or immunosuppressive effects, particularly in oncology. For instance, BI-1808, a human IgG1 monoclonal antibody that prevents TNF-α binding to TNFR2, has advanced to phase 1/2a trials for advanced solid tumors, demonstrating safety and preliminary efficacy when combined with pembrolizumab (NCT04752826). Preclinical studies with other anti-TNFR2 monoclonal antibodies have shown inhibition of Treg proliferation and ovarian cancer cell growth, highlighting their potential in depleting tumor-associated Tregs. Soluble TNFR2-Fc fusion proteins, such as variants of etanercept, sequester TNF ligands to indirectly antagonize TNFR2 signaling and have been explored in inflammatory models, though their broader effects on TNFR1 limit TNFR2 specificity.[73][74][75] Agonists selectively activate TNFR2 to enhance protective functions, such as neuroprotection in neurological disorders and Treg expansion in autoimmune conditions. In cancer, TNFR2 agonists like BI-1910 have entered phase 1 trials for solid tumors, either alone or with pembrolizumab, with 2025 data indicating tolerability and immune modulation (NCT06205706), with Phase 1 data presented at SITC 2025 showing tolerability and immune modulation across a wide dose range (4-900 mg Q3W) as of November 2025.[76][77] Similarly, HFB200301, a first-in-class TNFR2 agonist, completed phase 1 dosing in advanced solid tumors, showing promising pharmacokinetics (NCT05238883). For autoimmunity, TRB-061, a novel TNFR2 agonist, completed IND-enabling studies by late 2024 and initiated first-in-human trials in early 2025 for inflammatory diseases, targeting Treg-mediated immunosuppression. In preclinical models of multiple sclerosis, TNFR2 agonism promoted oligodendrocyte differentiation and reduced inflammation, supporting its neuroprotective potential.[78][79][80][81][82][83] Small molecules offer targeted modulation of TNFR2 downstream signaling or processing. TRAF2 inhibitors disrupt TNFR2-mediated survival signals, with preclinical compounds showing potential to enhance apoptosis in cancer cells by blocking NF-κB activation, though no phase trials were reported as of 2025. ADAM17 modulators, which regulate TNFR2 ectodomain shedding to control membrane-bound receptor levels, have been investigated for inflammatory bowel disease (IBD) in preclinical models; inhibition preserves membrane TNFR2 for anti-inflammatory effects.[84][15][85][84] Key challenges in TNFR2 therapeutics include its context-dependent effects, where agonism may suppress immunity in cancer but exacerbate it in autoimmunity, necessitating disease-specific dosing. Combination strategies, such as pairing TNFR2 agonists with anti-TNF therapies or immune checkpoint inhibitors, are under exploration to mitigate these issues, as seen in ongoing trials for solid tumors (e.g., NCT06205706). As of 2025, phase 1/2 trials for systemic lupus erythematosus (SLE) incorporating TNFR2 agonism for Treg expansion remain preclinical or early-stage, with no dedicated NCT identifiers reported, while cancer trials continue to advance.[5][86][79]| Therapeutic Agent | Type | Target Disease | Trial Phase/Status (as of 2025) | NCT Identifier |
|---|---|---|---|---|
| BI-1808 | Antagonist mAb | Solid tumors | Phase 1/2a, recruiting | NCT04752826 |
| BI-1910 | Agonist mAb | Solid tumors | Phase 1, data presented | NCT06205706 |
| HFB200301 | Agonist mAb | Advanced solids | Phase 1, completed dosing | NCT05238883 |
| TRB-061 | Agonist | Inflammatory diseases | Phase 1, initiated early 2025 | N/A (IND-enabling complete) |