Recent from talks
Nothing was collected or created yet.
Menopause
View on Wikipedia
| Menopause | |
|---|---|
| Other names | Climacteric |
 | |
| Specialty | Gynecology |
| Symptoms | No menstrual periods for a year[1] |
| Duration | 5-15 years |
| Causes | Usually a natural change. Can also be caused by surgery that removes both ovaries, and some types of chemotherapy.[1] |
| Treatment | None, lifestyle changes[2] |
| Medication | Menopausal hormone therapy, clonidine, gabapentin, selective serotonin reuptake inhibitors[2][3] |

Menopause is the time when menstrual periods permanently stop, marking the end of the reproductive stage for the female human.[1][4][5] It typically occurs between the ages of 45 and 55, although the exact timing can vary.[6] Menopause is usually a natural change related to a decrease in circulating blood estrogen levels.[1] It can occur earlier in those who smoke tobacco.[1][7] Other causes include surgery that removes both ovaries, some types of chemotherapy, or anything that leads to a decrease in hormone levels.[8][1] At the physiological level, menopause happens because of a decrease in the ovaries' production of the hormones estrogen and progesterone.[1] While typically not needed, measuring hormone levels in the blood or urine can confirm a diagnosis.[9] Menopause is the opposite of menarche, the time when periods start.[10]
In the years before menopause, a woman's periods typically become irregular,[11][12] which means that periods may be longer or shorter in duration, or be lighter or heavier in the amount of flow.[11] During this time, women often experience hot flashes; these typically last from 30 seconds to ten minutes and may be associated with shivering, night sweats, and reddening of the skin.[11] Hot flashes can recur for four to five years.[4] Other symptoms may include vaginal dryness,[13] trouble sleeping, and mood changes.[11][14] The severity of symptoms varies between women.[4] Menopause before the age of 45 years is considered to be "early menopause", and ovarian failure or surgical removal of the ovaries before the age of 40 years is termed "premature ovarian insufficiency".[15]
In addition to symptoms (hot flushes/flashes, night sweats, mood changes, arthralgia and vaginal dryness), the physical consequences of menopause include bone loss, increased central abdominal fat, and adverse changes in a woman's cholesterol profile and vascular function.[15] These changes predispose postmenopausal women to increased risks of osteoporosis and bone fracture, and of cardio-metabolic disease (diabetes and cardiovascular disease).[15]
Medical professionals often define menopause as having occurred when a woman has not had any menstrual bleeding for a year.[1] It may also be defined by a decrease in hormone production by the ovaries.[16] In those who have had surgery to remove their uterus but still have functioning ovaries, menopause is not considered to have yet occurred.[15] Following the removal of the uterus, symptoms of menopause typically occur earlier.[17] Iatrogenic menopause occurs when both ovaries are surgically removed (oophorectomy) along with the uterus for medical reasons.
Medical treatment of menopause is primarily to ameliorate symptoms and prevent bone loss.[18] Mild symptoms may be improved with treatment. With respect to hot flashes, avoiding nicotine, caffeine, and alcohol is often recommended; sleeping naked in a cool room and using a fan may help. The most effective treatment for menopausal symptoms is menopausal hormone therapy (MHT).[13][18] Non-hormonal therapies for hot flashes include cognitive-behavioral therapy, clinical hypnosis, gabapentin, fezolinetant or selective serotonin reuptake inhibitors.[19][20] These will not improve symptoms such as joint pain or vaginal dryness, which affect over 55% of women.[18] Exercise may help with sleeping problems. Many of the concerns about the use of MHT raised by older studies are no longer considered barriers to MHT in healthy women.[18] High-quality evidence for the effectiveness of alternative medicine has not been found.[4]
Signs and symptoms
[edit]
During early menopause transition, the menstrual cycles remain regular but the interval between cycles begins to lengthen. Hormone levels begin to fluctuate. Ovulation may not occur with each cycle.[21]
The term menopause refers to a point in time that follows one year after the last menstruation.[21] During the menopausal transition and after menopause, women can experience a range of symptoms.[11] However, for women who enter the menopause transition without having regular menstrual cycles (due to prior surgery, other medical conditions or ongoing hormonal contraception) the menopause cannot be identified by bleeding patterns and is defined as the permanent loss of ovarian function.[18]
Vagina, uterus and bladder (urogenital tract)
[edit]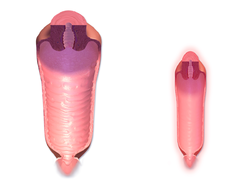
During the transition to menopause, menstrual patterns can show shorter cycling (by 2–7 days);[21] longer cycles remain possible.[21] There may be irregular bleeding (lighter, heavier, spotting).[11][21] Dysfunctional uterine bleeding is often experienced by women approaching menopause due to the hormonal changes that accompany the menopause transition. Spotting or bleeding may simply be related to vaginal atrophy, a benign sore (polyp or lesion), or may be a functional endometrial response. The European Menopause and Andropause Society has released guidelines for assessment of the endometrium, which is usually the main source of spotting or bleeding.[22]
In post-menopausal women, however, any unscheduled vaginal bleeding is of concern and requires an appropriate investigation to rule out the possibility of malignant diseases.
Urogenital symptoms may appear during menopause and continue through postmenopause and include painful intercourse, vaginal dryness and atrophic vaginitis (thinning of the membranes of the vulva, the vagina, the cervix and the outer urinary tract). There may also be considerable shrinking and loss in elasticity of all of the outer and inner genital areas. Urinary urgency may also occur and urinary incontinence in some women.[21][23]
Other physical effects
[edit]
The most common physical symptoms of menopause are heavy night sweats, and hot flashes (also known as vasomotor symptoms).[24] Sleeping problems and insomnia are also common.[25] Other physical symptoms may be reported that are not specific to menopause but may be exacerbated by it, such as lack of energy, joint soreness, stiffness, back pain, breast enlargement, breast pain, heart palpitations, headache, dizziness, dry, itchy skin, thinning of the skin, tingling skin, rosacea, weight gain.[21][26]
Mood and memory effects
[edit]Psychological symptoms are often reported but they are not specific to menopause and can be caused by other factors.[27][28] They include anxiety, poor memory, inability to concentrate, depressive mood, irritability, mood swings, and less interest in sexual activity.[21][29][11]
Menopause-related cognitive impairment can be confused with the mild cognitive impairment that precedes dementia.[30] There is evidence of small decreases in verbal memory, on average, which may be caused by the effects of declining estrogen levels on the brain,[31] or perhaps by reduced blood flow to the brain during hot flashes.[32] However, these tend to resolve for most women during the postmenopause. Subjective reports of memory and concentration problems are associated with several factors, such as lack of sleep, and stress.[28][27]
Long-term effects
[edit]Cardiovascular health
[edit]Exposure to endogenous estrogen during reproductive years provides women with protection against cardiovascular disease, which is lost around 10 years after the onset of menopause. The menopausal transition is associated with an increase in fat mass (predominantly in visceral fat), an increase in insulin resistance, dyslipidaemia, and endothelial dysfunction.[33] Women with vasomotor symptoms during menopause seem to have an especially unfavorable cardiometabolic profile,[34] as well as women with premature onset of menopause (before 45 years of age).[35] These risks can be reduced by managing risk factors, such as tobacco smoking, hypertension, increased blood lipids and body weight.[36][37]
Bone health
[edit]The annual rates of bone mineral density loss are highest starting one year before the final menstrual period and continuing through the two years after it.[38] Thus, post menopausal women are at increased risk of osteopenia, osteoporosis and fractures.
Causes
[edit]Menopause is a normal event in a woman's life and a natural part of aging.[23] Menopause can also be induced early.[39] Induced menopause occurs as a result of medical treatment such as chemotherapy, radiotherapy, oophorectomy, or complications of tubal ligation, hysterectomy, unilateral or bilateral salpingo-oophorectomy or leuprorelin usage.[40]
Age
[edit]Menopause typically occurs at some point between 47 and 54 years of age.[6] According to various data, more than 95% of women have their last period between the ages of 44–56 (median 49–50). 2% of women under the age of 40, 5% between the ages of 40–45 and the same number between the ages of 55–58 have their last bleeding.[41] The average age of the last period in the United States is 51 years, in Russia is 50 years, in Greece is 49 years, in Turkey is 47 years, in Egypt is 47 years and in India is 46 years.[42] Beyond the influence of genetics, these differences are also due to early-life environmental conditions[43] and associated with epigenetic effects.[44] The menopausal transition or perimenopause leading up to menopause usually lasts 3–4 years (sometimes as long as 5–14 years).[1][12]
Undiagnosed and untreated coeliac disease is a risk factor for early menopause. Coeliac disease can present with several non-gastrointestinal symptoms, in the absence of gastrointestinal symptoms, and most cases escape timely recognition and go undiagnosed, leading to a risk of long-term complications. A strict gluten-free diet reduces the risk. Women with early diagnosis and treatment of coeliac disease present a normal duration of fertile life span.[45][46]
Women who have undergone hysterectomy with ovary conservation go through menopause on average 1.5 years earlier than the expected age.[18]
Premature ovarian insufficiency
[edit]In rare cases, a woman's ovaries stop working at a very early age, ranging anywhere from the age of puberty to age 40. This is known as premature ovarian failure or premature ovarian insufficiency (POI) and affects 1 to 2% of women by age 40.[47][48][49] It is diagnosed or confirmed by high blood levels of follicle stimulating hormone (FSH) and luteinizing hormone (LH) on at least three occasions at least four weeks apart.[50]
Premature ovarian insufficiency may be related to an auto immune disorder and therefore might co-occur with other autoimmune disorders such as thyroid disease, [adrenal insufficiency], and diabetes mellitus.[49] Other causes include chemotherapy, being a carrier of the fragile X syndrome gene, and radiotherapy.[49] However, in about 50–80% of cases of premature ovarian insufficiency, the cause is unknown, i.e., it is generally idiopathic.[48][50]
Early menopause can be related to cigarette smoking, higher body mass index, racial and ethnic factors, illnesses, and the removal of the uterus.[51]
Surgical menopause
[edit]Menopause can be surgically induced by bilateral oophorectomy (removal of ovaries),[39] which is often, but not always, done in conjunction with removal of the fallopian tubes (salpingo-oophorectomy) and uterus (hysterectomy).[52] Cessation of menses as a result of removal of the ovaries is called "surgical menopause". Surgical treatments, such as the removal of ovaries, might cause periods to stop altogether.[53] The sudden and complete drop in hormone levels may produce extreme withdrawal symptoms such as hot flashes, etc. The symptoms of early menopause may be more severe.[53]
Removal of the uterus without removal of the ovaries does not directly cause menopause, although pelvic surgery of this type can often precipitate a somewhat earlier menopause, perhaps because of a compromised blood supply to the ovaries.[medical citation needed] The time between surgery and possible early menopause is due to the fact that ovaries are still producing hormones.[53]
Mechanism
[edit]
The menopausal transition, and postmenopause itself, is a natural change, not usually a disease state or a disorder. The main cause of this transition is the natural depletion and aging of the finite amount of oocytes (ovarian reserve). This process is sometimes accelerated by other conditions and is known to occur earlier after a wide range of gynecologic procedures such as hysterectomy (with and without ovariectomy), endometrial ablation and uterine artery embolisation. The depletion of the ovarian reserve causes an increase in circulating follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels because there are fewer oocytes and follicles responding to these hormones and producing estrogen.[citation needed]
The transition has a variable degree of effects.[54]
The stages of the menopause transition have been classified according to a woman's reported bleeding pattern, supported by changes in the pituitary follicle-stimulating hormone (FSH) levels.[55]
In younger women, during a normal menstrual cycle the ovaries produce estradiol, testosterone and progesterone in a cyclical pattern under the control of FSH and luteinizing hormone (LH), which are both produced by the pituitary gland. During perimenopause (approaching menopause), estradiol levels and patterns of production remain relatively unchanged or may increase compared to young women, but the cycles become frequently shorter or irregular.[56] The often observed increase in estrogen is presumed to be in response to elevated FSH levels that, in turn, is hypothesized to be caused by decreased feedback by inhibin.[57] Similarly, decreased inhibin feedback after hysterectomy is hypothesized to contribute to increased ovarian stimulation and earlier menopause.[58][59]
The menopausal transition is characterized by marked, and often dramatic, variations in FSH and estradiol levels. Because of this, measurements of these hormones are not considered to be reliable guides to a woman's exact menopausal status.[57]
Menopause occurs because of the sharp decrease of estradiol and progesterone production by the ovaries. After menopause, estrogen continues to be produced mostly by aromatase in fat tissues and is produced in small amounts in many other tissues such as ovaries, bone, blood vessels, and the brain where it acts locally.[60] The substantial fall in circulating estradiol levels at menopause impacts many tissues, from brain to skin.
In contrast to the sudden fall in estradiol during menopause, the levels of total and free testosterone, as well as dehydroepiandrosterone sulfate (DHEAS) and androstenedione appear to decline more or less steadily with age. An effect of natural menopause on circulating androgen levels has not been observed.[61] Thus specific tissue effects of natural menopause cannot be attributed to loss of androgenic hormone production.[62]
Hot flashes and other vasomotor and body symptoms accompanying the menopausal transition are associated with estrogen insufficiency and changes that occur in the brain, primarily the hypothalamus and involve complex interplay between the neurotransmitters kisspeptin, neurokinin B, and dynorphin, which are found in KNDy neurons in the infundibular nucleus.[63]
Ovarian aging
[edit]Decreased inhibin feedback after hysterectomy is hypothesized to contribute to increased ovarian stimulation and earlier menopause. Hastened ovarian aging has been observed after endometrial ablation. While it is difficult to prove that these surgeries are causative, it has been hypothesized that the endometrium may be producing endocrine factors contributing to the endocrine feedback and regulation of the ovarian stimulation. Elimination of these factors contributes to faster depletion of the ovarian reserve. Reduced blood supply to the ovaries that may occur as a consequence of hysterectomy and uterine artery embolisation has been hypothesized to contribute to this effect.[58][59]
Impaired DNA repair mechanisms may contribute to earlier depletion of the ovarian reserve during aging.[64] As women age, double-strand breaks accumulate in the DNA of their primordial follicles. Primordial follicles are immature primary oocytes surrounded by a single layer of granulosa cells. An enzyme system is present in oocytes that ordinarily accurately repairs DNA double-strand breaks. This repair system is called "homologous recombinational repair", and it is especially effective during meiosis. Meiosis is the general process by which germ cells are formed in all sexual eukaryotes; it appears to be an adaptation for efficiently removing damages in germ line DNA.[65]
Human primary oocytes are present at an intermediate stage of meiosis, termed prophase I (see Oogenesis). Expression of four key DNA repair genes that are necessary for homologous recombinational repair during meiosis (BRCA1, MRE11, Rad51, and ATM) decline with age in oocytes.[64] This age-related decline in ability to repair DNA double-strand damages can account for the accumulation of these damages, that then likely contributes to the depletion of the ovarian reserve.
Diagnosis
[edit]Ways of assessing the impact on women of some of these menopause effects, include the Greene climacteric scale questionnaire,[66] the Cervantes scale[67] and the Menopause rating scale.[68]
Perimenopause
[edit]The term "perimenopause", which literally means "around the menopause", refers to the menopause transition years before the date of the final episode of flow.[1][12][69][70] According to the North American Menopause Society, this transition can last for four to eight years.[71] The Centre for Menstrual Cycle and Ovulation Research describes it as a six- to ten-year phase ending 12 months after the last menstrual period.[72]
During perimenopause, estrogen levels average about 20–30% higher than during premenopause, often with wide fluctuations.[72] These fluctuations cause many of the physical changes during perimenopause as well as menopause, especially during the last 1–2 years of perimenopause (before menopause).[69][73] Some of these changes are hot flashes, night sweats, difficulty sleeping, mood swings, vaginal dryness or atrophy, incontinence, osteoporosis, and heart disease.[72] Perimenopause is also associated with a higher likelihood of depression (affecting from 45 percent to 68 percent of perimenopausal women), which is twice as likely to affect those with a history of depression.[74][75]
During this period, fertility diminishes but is not considered to reach zero until the official date of menopause. The official date is determined retroactively, once 12 months have passed after the last appearance of menstrual blood.
The menopause transition typically begins between 40 and 50 years of age (average 47.5).[76][77] The duration of perimenopause may be for up to eight years.[77] Women will often, but not always, start these transitions (perimenopause and menopause) about the same time as their mother did.[78]
Some research appears to show that melatonin supplementation in perimenopausal women can improve thyroid function and gonadotropin levels, as well as restoring fertility and menstruation and preventing depression associated with menopause.[79]
Postmenopause
[edit]The term "postmenopausal" describes women who have not experienced any menstrual flow for a minimum of 12 months, assuming that they have a uterus and are not pregnant or lactating.[52] The reason for this delay in declaring postmenopause is that periods are usually erratic during menopause. Therefore, a reasonably long stretch of time is necessary to be sure that the cycling has ceased. At this point a woman is considered infertile; however, the possibility of becoming pregnant has usually been very low (but not quite zero) for a number of years before this point is reached.[citation needed]
In women with or without a uterus, menopause or postmenopause can also be identified by a blood test showing a very high follicle-stimulating hormone level, greater than 25 IU/L in a random blood draw; it rises as ovaries become inactive.[52] FSH continues to rise, as its counterpart estradiol continues to drop for about 2 years after the last menstrual period, after which the levels of each of these hormones stabilize. The stabilization period after the begin of early postmenopause has been estimated to last 3 to 6 years, so early postmenopause lasts altogether about 5 to 8 years, during which hormone withdrawal effects such as hot flashes disappear.[52] Finally, late postmenopause has been defined as the remainder of a woman's lifespan, when reproductive hormones do not change any more.[citation needed]
A period-like flow during postmenopause, even spotting, may be a sign of endometrial cancer.
Management
[edit]Perimenopause is a natural stage of life. It is not a disease or a disorder. Therefore, it does not automatically require any kind of medical treatment. However, in those cases where the physical, mental, and emotional effects of perimenopause are strong enough that they significantly disrupt the life of the woman experiencing them, palliative medical therapy may sometimes be appropriate.
Menopausal hormone therapy
[edit]In the context of the menopause, menopausal hormone therapy (MHT) is the use of estrogen in women without a uterus and estrogen plus progestogen in women who have an intact uterus.[80]
MHT may be reasonable for the treatment of menopausal symptoms, such as hot flashes.[81] It is the most effective treatment option, especially when delivered as a skin patch.[82][83] Its use, however, appears to increase the risk of strokes and blood clots.[84] When used for menopausal symptoms the global recommendation is MHT should be prescribed for as long as there are defined treatment effects and goals for the individual woman.[18]
MHT is also effective for preventing bone loss and osteoporotic fracture,[85] but it is generally recommended only for women at significant risk for whom other therapies are unsuitable.[86]
MHT may be unsuitable for some women, including those at increased risk of cardiovascular disease, increased risk of thromboembolic disease (such as those with obesity or a history of venous thrombosis) or increased risk of some types of cancer.[86] There is some concern that this treatment increases the risk of breast cancer.[87] Women at increased risk of cardiometabolic disease and VTE may be able to use transdermal estradiol which does not appear to increase risks in low to moderate doses.[18]
Adding testosterone to hormone therapy has a positive effect on sexual function in postmenopausal women, although it may be accompanied by hair growth or acne if used in excess. Transdermal testosterone therapy in appropriate dosing is generally safe.[88]
Selective estrogen receptor modulators
[edit]SERMs are a category of drugs, either synthetically produced or derived from a botanical source, that act selectively as agonists or antagonists on the estrogen receptors throughout the body. The most commonly prescribed SERMs are raloxifene and tamoxifen. Raloxifene exhibits oestrogen agonist activity on bone and lipids, and antagonist activity on breast and the endometrium.[89] Tamoxifen is in widespread use for treatment of hormone sensitive breast cancer. Raloxifene prevents vertebral fractures in postmenopausal, osteoporotic women and reduces the risk of invasive breast cancer.[90]
Other medications
[edit]Some of the SSRIs and SNRIs appear to provide some relief from vasomotor symptoms.[20][19] The most effective SSRIs and SNRIs are paroxetine, escitalopram, citalopram, venlafaxine, and desvenlafaxine.[19] They may, however, be associated with appetite and sleeping problems, constipation and nausea.[20][91]
Gabapentin or fezolinetant can also improve the frequency and severity of vasomotor symptoms.[20][19] Side effects of using gabapentin include drowsiness and headaches.[20][91]
Therapy
[edit]Cognitive behavioural therapy and clinical hypnosis can decrease the amount women are affected by hot flashes.[19] Mindfulness is not yet proven to be effective in easing vasomotor symptoms.[92][93][19]
Lifestyle and exercise
[edit]Exercise has been thought to reduce postmenopausal symptoms through the increase of endorphin levels, which decrease as estrogen production decreases.[94] However, there is insufficient evidence to suggest that exercise helps with the symptoms of menopause.[19] Similarly, yoga has not been shown to be useful as a treatment for vasomotor symptoms.[19]
However a high BMI is a risk factor for vasomotor symptoms in particular. Weight loss may help with symptom management.[95][19]
There is no strong evidence that cooling techniques such as using specific clothing or environment control tools (for example fans) help with symptoms.[19] Paced breathing and relaxation are not effective in easing symptoms.[19]
Research suggests that, as hormones and gut microbiome are intertwined in some ways, hormone fluctuations during menopause can alter the gut environment and microbial activity.[96] This can contribute to menopausal symptoms, including weight gain and mood swings.[97] Diet can support a healthy gut microbiome, and avoiding things like alcohol and added sugar, which can disrupt this environment, could mitigate symptoms.[98][99][100]
Dietary supplements
[edit]There is no evidence of consistent benefit of taking any dietary supplements or herbal products for menopausal symptoms.[19][101][102] These widely marketed but ineffective supplements include soy isoflavones, pollen extracts, black cohosh, omega-3 among many others.[19][103][104]
Alternative medicine
[edit]There is no evidence of consistent benefit of alternative therapies for menopausal symptoms despite their popularity.[102][19]
As of 2023, there is no evidence to support the efficacy of acupuncture as a management for menopausal symptoms.[19][105][102] The Cochrane review found not enough evidence in 2016 to show a difference between Chinese herbal medicine and placebo for the vasomotor symptoms.[106]
Other efforts
[edit]- Lack of lubrication is a common problem during and after perimenopause. Vaginal moisturizers can help women with overall dryness, and lubricants can help with lubrication difficulties that may be present during intercourse. It is worth pointing out that moisturizers and lubricants are different products for different issues: some women complain that their genitalia are uncomfortably dry all the time, and they may do better with moisturizers. Those who need only lubricants do well using them only during intercourse.
- Low-dose prescription vaginal estrogen products such as estrogen creams are generally a safe way to use estrogen topically, to help vaginal thinning and dryness problems (see vaginal atrophy) while only minimally increasing the levels of estrogen in the bloodstream.
- Individual counseling or support groups can sometimes be helpful to handle sad, depressed, anxious or confused feelings women may be having as they pass through what can be for some a very challenging transition time.
- Osteoporosis can be minimized by smoking cessation, adequate vitamin D intake and regular weight-bearing exercise. The bisphosphonate drug alendronate may decrease the risk of a fracture, in women that have both bone loss and a previous fracture and less so for those with just osteoporosis.[107]
- A surgical procedure where a part of one of the ovaries is removed earlier in life and frozen and then over time thawed and returned to the body (ovarian tissue cryopreservation) has been tried. While at least 11 women have undergone the procedure and paid over £6,000, there is no evidence it is safe or effective.[108]
Society and culture
[edit]Attitudes and experiences
[edit]The menopause transition is a process, involving hormonal, menstrual, and typically vasomotor changes. However, the experience of the menopause as a whole is very much influenced by psychological and social factors, such as past experience, lifestyle, social and cultural meanings of menopause, and a woman's social and material circumstances. Menopause has been described as a biopsychosocial experience, with social and cultural factors playing a prominent role in the way menopause is experienced and perceived.[109]
The paradigm within which a woman considers menopause influences the way she views it: women who understand menopause as a medical condition rate it significantly more negatively than those who view it as a life transition or a symbol of aging.[110] There is some evidence that negative attitudes and expectations, held before the menopause, predict symptom experience during the menopause,[111] and beliefs and attitudes toward menopause tend to be more positive in postmenopausal than in premenopausal women.[112] Women with more negative attitudes towards the menopause report more symptoms during this transition.[111]
Though there has been a shift towards more public conversations around menopause, it is often still seen as a private process and is predominantly understood through the medical paradigm.[113] Despite these growing conversations, the embodied experience of menopause is often reduced to biological symptoms rather than understood as a complex social and cultural process.[114] Hot flashes are one of the most common symptoms of menopause.[115] They are also associated with psychological symptoms such as anxiety[115] and embarrassment.[116] Heat and emotionality are frequently linked, which can socially associate hot flashes with a breakdown of emotional and physical regulation.[116] This can be partially understood as hot flashes breaking down barriers between private, internal bodily processes and the external world, physically manifesting menopause. Observers of menopause have sometimes interpreted it as a complete loss of the ability to regulate emotions, an interpretation frequently at odds with how it is actually experienced by the individual.[116] Victorian medical understandings — which positioned women's health as primarily controlled by the reproductive system — could have influenced ideas around hot flashes as revealing the dominance of reproductive control over the individual. Feminist critiques of medical treatment of menopause, however, have framed it as part of a broader social and political system "that attempts to control the effects of the aging of the female body, which loses its social significance with the loss of reproductive capacity".[113] This tension between medicalisation and feminist perspectives highlights how menopause has been framed less as a natural life stage and more as a site of social regulation and control.
Menopause is a stage of life experienced in different ways. It can be characterized by personal challenges, changes in personal roles within the family and society. Women's approaches to changes during menopause are influenced by their personal, family and sociocultural background.[117] Women from different regions and countries also have different attitudes. Postmenopausal women had more positive attitudes toward menopause compared with peri- or premenopausal women. Other influencing factors of attitudes toward menopause include age, menopausal symptoms, psychological and socioeconomical status, and profession and ethnicity.[118]
Ethnicity and geography play roles in the experience of menopause. American women of different ethnicities report significantly different types of menopausal effects. One major study found Caucasian women most likely to report what are sometimes described as psychosomatic symptoms, while African-American women were more likely to report vasomotor symptoms.[119]
There may be variations in experiences of women from different ethnic backgrounds regarding menopause and care. Immigrant women reported more vasomotor symptoms and other physical symptoms and poorer mental health than non-immigrant women and were mostly dissatisfied with the care they had received. Self-management strategies for menopausal symptoms were also influenced by culture.[120]
Two multinational studies of Asian women, found that hot flushes were not the most commonly reported symptoms, instead body and joint aches, memory problems, sleeplessness, irritability and migraines were.[121] In another study comparing experiences of menopause amongst White Australian women and women in Laos, Australian women reported higher rates of depression, as well as fears of aging, weight gain and cancer – fears not reported by Laotian women, who positioned menopause as a positive event.[122] Japanese women experience menopause effects, or kōnenki (更年期), in a different way from American women.[123] Japanese women report lower rates of hot flashes and night sweats; this can be attributed to a variety of factors, both biological and social. Historically, kōnenki was associated with wealthy middle-class housewives in Japan, i.e., it was a "luxury disease" that women from traditional, inter-generational rural households did not report. Menopause in Japan was viewed as a symptom of the inevitable process of aging, rather than a "revolutionary transition", or a "deficiency disease" in need of management.[123] As of 2005, in Japanese culture, reporting of vasomotor symptoms has been on the increase, with research finding that of 140 Japanese participants, hot flashes were prevalent in 22.1%.[124] This was almost double that of 20 years prior.[125] Whilst the exact cause for this is unknown, possible contributing factors include dietary changes, increased medicalisation of middle-aged women and increased media attention on the subject.[125] However, reporting of vasomotor symptoms is still "significantly" lower than in North America.[126]
Additionally, while most women in the United States apparently have a negative view of menopause as a time of deterioration or decline, some studies seem to indicate that women from some Asian cultures have an understanding of menopause that focuses on a sense of liberation and celebrates the freedom from the risk of pregnancy.[127] Diverging from these conclusions, one study appeared to show that many American women "experience this time as one of liberation and self-actualization".[128]
Recent biosocial and anthropological scholarship cautions against interpreting ethnic or national differences in menopausal timing and symptom burden as innate racial biology. A 2024 U.S. scoping review synthesizing fifteen studies reported that African American women, on average, reach natural menopause earlier than White women and report vasomotor symptoms more frequently. The review links these patterns to cumulative psychosocial stressors—including racial discrimination, lower income, and heavy caregiving demands—rather than to genetic difference. It also reports associations between intimate partner violence and childhood abuse with greater symptom severity, as well as higher hormone therapy use among women veterans, patterns interpreted as markers of heightened chronic stress exposure.[129] These findings highlight how experiences of inequality and trauma can become biologically embedded, shaping health outcomes across the life course. Anthropological syntheses likewise emphasize "local biologies," showing that symptom profiles vary across societies as labor rhythms, diet, clinical discourse, and life-course endocrinology interact. For example, Japanese women commonly report chilliness rather than hot flushes, and symptom labeling and expectations differ accordingly.[130] This underscores that menopause is not only a physiological transition but also a socially mediated experience that reflects broader cultural environments. Together, these sources suggest that apparent disparities are best understood as embodied effects of unequal social conditions and culturally specific meanings. Explanations focused only on attitudes or estrogen may overlook wider social determinants and limit clinical care.[130]
In some women, menopause may bring about a sense of loss related to the end of fertility. In addition, this change often aligns with other stressors, such as the responsibility of looking after elderly parents or dealing with the emotional challenges of "empty nest syndrome" when children move out of the family home. This situation can be accentuated in cultures where being older is negatively perceived.
LGBTQIA+ experiences
[edit]The experience of menopause for non-binary and transgender people can be especially difficult in relation to gender, as menopause is heavily defined as a feminine experience.[131] Menopause is typically defined as the discontinuation of menstrual periods, the conclusion of fertility, and the finalisation of ovarian function — all of which are deeply connected to traditional understandings of gender and femininity.[132] One study, published in the International Journal of Transgender Health, reported that non-binary individuals experienced menopause as having an impact on their gender identity, either positively or negatively, and that many also struggled to find supportive resources and spaces to share their experiences.[132] Some participants further highlighted broader societal prejudices that undermined their sense of security — especially as menopause is still largely framed through traditional ideas of gender, hormones, and the female body.[132] They also emphasised that many medical professionals lacked adequate understanding of menopause in relation to non-binary and transgender people. This lack of awareness often created barriers to accessing essential health services that recognised and met their needs.[132] A 2021 UK GP Patient Survey found that while trans and non‑binary adults reported similar access to primary care as the general population, they were significantly less likely to feel involved in decisions about their treatment (85.0% versus 93.7%) and less likely to feel their needs were met overall (88.1% versus 95.2%).[133]
Menopause across cultures
[edit]Menopause is both viewed and experienced differently in cultures around the globe. From a Western perspective, focus on menopause tends to be more scientific, with an emphasis on the management of symptoms.
In post-war (modern) Japan, there has been a sharp increase in the medicalisation of menopause. Anthropologist Margaret Lock explores the cultural construction of the 'menopausal syndrome' present in Japanese rhetoric.[134] Whilst symptoms of 'headaches, shoulder stiffness, and dizziness' are viewed as usual menopause symptoms, 'changes in endocrine function and in the autonomic nervous system' are classified as menopausal.[134] The menopausal syndrome is perpetrated as being more common in housewives. This is because as they age, "their traditional role [as a housewife] is in jeopardy", creating larger susceptibility to stress.[134] Menopausal syndrome is highly stigmatised and associated with being selfish, pleasure driven, and deficient in willpower.[134] However, there is a significant difference between the rhetoric and statistical results. Lock reports that housewives do not experience higher menopausal symptoms. In her sample, 53% of women reported going through menopause, yet only 12% reported visiting the gynaecologist in the past two years, and only 2% had taken prescribed estrogen replacement therapy.[134] A curation of the societal role of women, increasing medicalisation, economic concern, and the 'usefulness' of middle-aged women has led to this increasing debate over menopause in Japan. However, while both symptoms and rhetoric grow, so does the 'political consciousness' of Japanese middle-aged women.[134]
Throughout Mayan history, the cultural perception of menopause is primarily understood as a biological transitioning, rather than bearing any medical or societal significance. An article written by Yewoubdar Beyen delves into the experiences of menopause by Mayan women in Yucatan.[135] Discoveries made by this study promote the cultural construction of menopause as "unmarked" by stigma, rituals or significance. The emphasis of menopause in Western societies differentiated from the Mayan perception, where it is beheld as a natural part of development, holding no substantiating symbolic importance. Beyen found that 68.2% of Mayan women reported no distressing health changes, which may suggest that the absence of medicalisation leads to a reduction of symptom reporting.[135] Similar results were evident in Donna Stewart's investigation on Highland Guatemalan Mayan women who welcomed their symptoms and perceived them positively.[136] Some Mayan women express a sense of liberation after menopause; free from menstruation and childbearing. Cross-cultural research affirms this, discovering that feelings around menopause varies through cultural interpretation.[137] The absence of negative cultural connotations enables Mayan women for a more normalised transition to an older stage of life. Collectively, these discoveries challenge the Western model of menopause by exploring how neutral cultural beliefs shape experiences of menopause.
A study conducted at Monash University saw 74% of post-menopausal Australian women under the age of 55 suffer from vasomotor symptoms, with 28% reporting them as "severely bothersome".[138] It is statistics like this which have promoted the use of Hormone Replacement Therapy (HRT), also known as Menopausal Hormone Therapy (MHT) in Australia. These ongoing studies have proven that for symptomatic women, non-hormonal remedies are significantly "less effective than MHT".[138] This in turn has opened the floor for conversations surrounding menopause and its various symptoms, leading to further education for health professionals and women alike, through public health campaigns promoting evidence-based education.[138]
Along with menopausal education in Australia, the importance of biocultural research in this area is being explored. An examination conducted by a team of female anthropologists at BMC Women's Health denotes that there is extensive research for Australian women as a collective while only two reports relating to the Indigenous population. Through this the anthropological team highlight the importance of understanding "culture, social disadvantage"[139] and suggest that this would aid the population and improve "management and support for Indigenous Australian women".1
Impact on work
[edit]Midlife is typically a life stage when men and women may be dealing with demanding life events and responsibilities, such as work, health problems, and caring roles. For example, in 2018 in the UK women aged 45–54 report more work-related stress than men or women of any other age group.[140] Hot flashes are often reported to be particularly distressing at work and lead to embarrassment and worry about potential stigmatisation.[141] A June 2023 study by the Mayo Clinic estimated an annual loss of $1.8 billion in the United States due to workdays missed as a result of menopause symptoms.[142] This was one of the largest studies to date examining the impact of menopause symptoms on work outcomes. The research concluded there was a strong need to improve medical treatment for menopausal women and make the workplace environment more supportive to avoid such productivity losses.
Etymology
[edit]Menopause literally means the "end of monthly cycles" (the end of monthly periods or menstruation), from the Greek word pausis ("pause") and mēn ("month"). This is a medical coinage; the Greek word for menses is actually different. In Ancient Greek, the menses were described in the plural, ta emmēnia ("the monthlies"), and its modern descendant has been clipped to ta emmēna. The Modern Greek medical term is emmenopausis in Katharevousa or emmenopausi in Demotic Greek. The Ancient Greeks did not produce medical concepts about any symptoms associated with end of menstruation and did not use a specific word to refer to this time of a woman's life. The word menopause was invented by French doctors at the beginning of the nineteenth century. Greek etymology was reconstructed at this time and it was the Parisian student doctor Charles-Pierre-Louis de Gardanne who invented a variation of the word in 1812, which was edited to its final French form in 1821.[143]
Some of them noted that peasant women had no complaints about the end of menses, while urban middle-class women had many troubling symptoms. Doctors at this time considered the symptoms to be the result of urban lifestyles of sedentary behaviour, alcohol consumption, too much time indoors, and over-eating, with a lack of fresh fruit and vegetables.[144]
The word "menopause" was coined specifically for female humans, where the end of fertility is traditionally indicated by the permanent stopping of monthly menstruations. However, menopause exists in some other animals, many of which do not have monthly menstruation;[145] in this case, the term means a natural end to fertility that occurs before the end of the natural lifespan.
In popular culture, law and politics
[edit]In the 21st century, celebrities have spoken out about their experiences of the menopause, which has led to it becoming less of a taboo as it has boosted awareness of the debilitating symptoms. Subsequently, TV shows have been running features on the menopause to help women experiencing symptoms. In the UK Lorraine Kelly has been an advocate for getting women to speak about their experiences including sharing her own. This has led to an increase in women seeking treatment such as HRT.[146] Davina McCall also led an awareness campaign based on a documentary on Channel 4.[147]
In the UK, Carolyn Harris sponsored the Menopause (Support and Services) Bill in June 2021. It was to exempt hormone replacement therapy from National Health Service prescription charges and to make provisions about menopause support and services, including public education and communication in supporting perimenopausal and post-menopausal women, and to raise awareness of menopause and its effects. The bill was withdrawn on 29 October 2021.[148]
In the US, David McKinley, Republican from West Virginia introduced the Menopause Research Act in September 2022 for $100 million in 2023 and 2024, but it stalled.[149]
Other animals
[edit]The majority of mammal species reach menopause when they cease the production of ovarian follicles, which contain eggs (oocytes), between one-third and two-thirds of their maximum possible lifespan.[150] However, few live long enough in the wild to reach this point. Humans are joined by a limited number of other species in which females live substantially longer than their ability to reproduce. Examples of others include cetaceans: beluga whales,[151] narwhals,[151] orcas,[152] false killer whales[153] and short-finned pilot whales.[154]
Menopause has been reported in a variety of other vertebrate species, but these examples tend to be from captive individuals, and thus are not necessarily representative of what happens in natural populations in the wild. Menopause in captivity has been observed in several species of nonhuman primates,[145] including rhesus macaques[155] and chimpanzees.[156] Some research suggests that wild chimpanzees do not experience menopause, as their fertility declines are associated with declines in overall health.[157] Menopause has been reported in elephants in captivity[158] and guppies.[159] Dogs do not experience menopause; the canine estrus cycle simply becomes irregular and infrequent. Although older female dogs are not considered good candidates for breeding, offspring have been produced by older animals, see Canine reproduction. Similar observations have been made in cats.[160]
Life histories show a varying degree of senescence; rapid senescing organisms (e.g., Pacific salmon and annual plants) do not have a post-reproductive life-stage. Gradual senescence is exhibited by all placental mammalian life histories.[original research?]
Evolution
[edit]There are various theories on the origin and process of the evolution of the menopause. These attempt to suggest evolutionary benefits to the human species stemming from the cessation of women's reproductive capability before the end of their natural lifespan. It is conjectured that in highly social groups natural selection favors females that stop reproducing and devote that post-reproductive life span to continuing to care for existing offspring, both their own and those of others to whom they are related, especially their granddaughters and grandsons.[161]
See also
[edit]References
[edit]- ^ a b c d e f g h i j "Menopause Basics". United States Deputy Secretary of Health and Human Services. 13 March 2025. Retrieved 15 March 2025.
- ^ a b "What are the treatments for other symptoms of menopause?". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 28 June 2013. Archived from the original on 20 March 2015. Retrieved 8 March 2015.
- ^ Krause MS, Nakajima ST (March 2015). "Hormonal and nonhormonal treatment of vasomotor symptoms". Obstetrics and Gynecology Clinics of North America. 42 (1): 163–179. doi:10.1016/j.ogc.2014.09.008. PMID 25681847.
- ^ a b c d Menopause: Overview. Institute for Quality & Efficiency in Health Care. 2 July 2020. Retrieved 20 October 2022 – via National Library of Medicine - Bookshelf.
- ^ Angelou K, Grigoriadis T, Diakosavvas M, Zacharakis D, Athanasiou S (8 April 2020). "The Genitourinary Syndrome of Menopause: An Overview of the Recent Data". Cureus. 12 (4) e7586. doi:10.7759/cureus.7586. ISSN 2168-8184. PMC 7212735. PMID 32399320.
- ^ a b Takahashi TA, Johnson KM (May 2015). "Menopause". The Medical Clinics of North America. 99 (3): 521–534. doi:10.1016/j.mcna.2015.01.006. PMID 25841598.
- ^ Warren M, Soares CN, eds. (2009). The menopausal transition: interface between gynecology and psychiatry ([Online-Ausg.] ed.). Basel: Karger. p. 73. ISBN 978-3-8055-9101-0.
- ^ "Menopause & Chemotherapy - Managing Side Effects - Chemocare". chemocare.com. Archived from the original on 21 November 2012. Retrieved 20 October 2022.
- ^ "How do health care providers diagnose menopause?". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 6 May 2013. Archived from the original on 2 April 2015. Retrieved 8 March 2015.
- ^ Wood J. "9". Dynamics of Human Reproduction: Biology, Biometry, Demography. Transaction Publishers. p. 401. ISBN 978-0-202-36570-1. Archived from the original on 10 September 2017.
- ^ a b c d e f g "Menopause Symptoms and Relief". Office on Women's Health. 22 February 2021. Retrieved 20 October 2022.
- ^ a b c "What Is Menopause?". National Institute on Aging. 30 September 2021. Archived from the original on 28 July 2017. Retrieved 20 October 2022.
- ^ a b Mark JK, Samsudin S, Looi I, Yuen KH (3 May 2024). "Vaginal dryness: a review of current understanding and management strategies". Climacteric. 27 (3): 236–244. doi:10.1080/13697137.2024.2306892. ISSN 1369-7137. PMID 38318859.
- ^ Marino JM (November 2021). "Genitourinary Syndrome of Menopause". Journal of Midwifery & Women's Health. 66 (6): 729–739. doi:10.1111/jmwh.13277. ISSN 1526-9523. PMID 34464022.
- ^ a b c d Davis SR, Lambrinoudaki I, Lumsden M, Mishra GD, Pal L, Rees M, et al. (April 2015). "Menopause". Nature Reviews. Disease Primers. 1 (1) 15004. doi:10.1038/nrdp.2015.4. PMID 27188659.
- ^ Sievert LL (2006). Menopause: a biocultural perspective ([Online-Ausg.] ed.). New Brunswick, N.J.: Rutgers University Press. p. 81. ISBN 978-0-8135-3856-3. Archived from the original on 10 September 2017.
- ^ International position paper on women's health and menopause: a comprehensive approach. DIANE Publishing. 2002. p. 36. ISBN 978-1-4289-0521-4. Archived from the original on 10 September 2017.
- ^ a b c d e f g h Davis SR, Baber RJ (August 2022). "Treating menopause - MHT and beyond". Nature Reviews. Endocrinology. 18 (8): 490–502. doi:10.1038/s41574-022-00685-4. PMID 35624141. S2CID 249069157.
- ^ a b c d e f g h i j k l m n o "The 2023 nonhormone therapy position statement of The North American Menopause Society". Menopause. 30 (6): 573–590. 21 June 2023. doi:10.1097/GME.0000000000002200. ISSN 1072-3714. PMID 37252752. S2CID 258969337.
- ^ a b c d e Krause MS, Nakajima ST (March 2015). "Hormonal and nonhormonal treatment of vasomotor symptoms". Obstetrics and Gynecology Clinics of North America. 42 (1): 163–179. doi:10.1016/j.ogc.2014.09.008. PMID 25681847.
- ^ a b c d e f g h Hoffman B (2012). Williams Gynecology. New York: McGraw-Hill Medical. pp. 555–56. ISBN 978-0-07-171672-7.
- ^ Dreisler E, Poulsen LG, Antonsen SL, Ceausu I, Depypere H, Erel CT, Lambrinoudaki I, Pérez-López FR, Simoncini T, Tremollieres F, Rees M, Ulrich LG (June 2013). "EMAS clinical guide: assessment of the endometrium in peri and postmenopausal women". Maturitas. 75 (2): 181–90. doi:10.1016/j.maturitas.2013.03.011. PMID 23619009.
- ^ a b Allafi AH, Al-Johani AS, Babukur RM, Fikri J, Alanazi RR, Ali SD, Alkathiry A, Alfozan AM, Mayoof KI, Abualhamael MA (2024). "The Link Between Menopause and Urinary Incontinence: A Systematic Review". Cureus. 16 (10) e71260. doi:10.7759/cureus.71260. ISSN 2168-8184. PMC 11550778. PMID 39525118.
- ^ Crandall CJ, Mehta JM, Manson JE (February 2023). "Management of Menopausal Symptoms: A Review". JAMA. 329 (5): 405–420. doi:10.1001/jama.2022.24140. PMID 36749328. S2CID 256628900.
- ^ Santoro N, Epperson CN, Mathews SB (September 2015). "Menopausal Symptoms and Their Management". Endocrinology and Metabolism Clinics of North America. 44 (3): 497–515. doi:10.1016/j.ecl.2015.05.001. PMC 4890704. PMID 26316239.
- ^ "Red in the Face". NIH News in Health. 27 June 2017. Retrieved 31 March 2021.
- ^ a b Hogervorst E, Craig J, O'Donnell E (1 May 2022). "Cognition and mental health in menopause: A review". Best Practice & Research Clinical Obstetrics & Gynaecology. Menopause Management. 81: 69–84. doi:10.1016/j.bpobgyn.2021.10.009. ISSN 1521-6934. PMID 34969617. S2CID 244805452.
- ^ a b Kilpi F, Soares AL, Fraser A, Nelson SM, Sattar N, Fallon SJ, Tilling K, Lawlor DA (14 August 2020). "Changes in six domains of cognitive function with reproductive and chronological ageing and sex hormones: a longitudinal study in 2411 UK mid-life women". BMC Women's Health. 20 (1): 177. doi:10.1186/s12905-020-01040-3. ISSN 1472-6874. PMC 7427852. PMID 32795281.
- ^ Llaneza P, García-Portilla MP, Llaneza-Suárez D, Armott B, Pérez-López FR (February 2012). "Depressive disorders and the menopause transition". Maturitas. 71 (2): 120–30. doi:10.1016/j.maturitas.2011.11.017. hdl:10651/6519. PMID 22196311.
- ^ Panay N, Briggs P, Kovacs G (20 August 2015). "Memory and Mood in the Menopause". Managing the Menopause: 21st Century Solutions. Cambridge University Press. ISBN 978-1-316-35271-7.
- ^ Birkhaeuser M, Genazzani AR (30 January 2018). Pre-Menopause, Menopause and Beyond: Volume 5: Frontiers in Gynecological Endocrinology. Springer. pp. 38–39. ISBN 978-3-319-63540-8.
- ^ Papadakis MA, McPhee SJ, Rabow MW (11 September 2017). Current Medical Diagnosis and Treatment 2018, 57th Edition. McGraw Hill Professional. p. 1212. ISBN 978-1-259-86149-9.
- ^ Nappi RE, Chedraui P, Lambrinoudaki I, Simoncini T (June 2022). "Menopause: a cardiometabolic transition". The Lancet. Diabetes & Endocrinology. 10 (6): 442–456. doi:10.1016/S2213-8587(22)00076-6. PMID 35525259. S2CID 248561432.
- ^ Thurston RC (April 2018). "Vasomotor symptoms: natural history, physiology, and links with cardiovascular health". Climacteric. 21 (2): 96–100. doi:10.1080/13697137.2018.1430131. PMC 5902802. PMID 29390899.
- ^ Stevenson JC, Collins P, Hamoda H, Lambrinoudaki I, Maas AH, Maclaran K, Panay N (October 2021). "Cardiometabolic health in premature ovarian insufficiency". Climacteric. 24 (5): 474–480. doi:10.1080/13697137.2021.1910232. hdl:2066/238753. PMID 34169795. S2CID 235634591.
- ^ Souza HC, Tezini GC (September 2013). "Autonomic Cardiovascular Damage during Post-menopause: the Role of Physical Training". Aging and Disease. 4 (6): 320–328. doi:10.14336/AD.2013.0400320. PMC 3843649. PMID 24307965.
- ^ ESHRE Capri Workshop Group (2011). "Perimenopausal risk factors and future health". Human Reproduction Update. 17 (5): 706–717. doi:10.1093/humupd/dmr020. hdl:11380/665246. PMID 21565809.
- ^ Warming L, Hassager C, Christiansen C (1 February 2002). "Changes in bone mineral density with age in men and women: a longitudinal study". Osteoporosis International. 13 (2): 105–112. doi:10.1007/s001980200001. PMID 11905520. S2CID 618576.
- ^ a b "Early or premature menopause | Office on Women's Health". www.womenshealth.gov. Retrieved 21 October 2022.
- ^ "Gynaecologic Problems: Menopausal Problems". Health on the Net Foundation. Archived from the original on 25 February 2021. Retrieved 22 February 2012.
- ^ Morabia A, Costanza MC (December 1998). "International variability in ages at menarche, first livebirth, and menopause. World Health Organization Collaborative Study of Neoplasia and Steroid Contraceptives". American Journal of Epidemiology. 148 (12): 1195–205. doi:10.1093/oxfordjournals.aje.a009609. PMID 9867266.
- ^ Ringa V (2000). "Menopause and treatments". Quality of Life Research. 9 (6): 695–707. doi:10.1023/A:1008913605129. JSTOR 4036942. S2CID 22496307.
- ^ Begum K, Muttukrishna S, Sievert LL, Sharmeen T, Murphy L, Chowdhury O, Kasim A, Gunu R, Bentley GR (March 2016). "Ethnicity or environment: effects of migration on ovarian reserve among Bangladeshi women in the United Kingdom". Fertility and Sterility. 105 (3): 744–754.e1. doi:10.1016/j.fertnstert.2015.11.024. PMID 26706133.
- ^ Bar-Sadeh B, Rudnizky S, Pnueli L, Bentley GR, Stöger R, Kaplan A, Melamed P (15 September 2020). "Unravelling the role of epigenetics in reproductive adaptations to early-life environment". Nature Reviews Endocrinology. 16 (9): 519–533. doi:10.1038/s41574-020-0370-8. ISSN 1759-5029. PMID 32620937.
- ^ Tersigni C, Castellani R, de Waure C, Fattorossi A, De Spirito M, Gasbarrini A, Scambia G, Di Simone N (2014). "Celiac disease and reproductive disorders: meta-analysis of epidemiologic associations and potential pathogenic mechanisms". Human Reproduction Update. 20 (4): 582–93. doi:10.1093/humupd/dmu007. hdl:10807/56796. PMID 24619876.
- ^ Lasa JS, Zubiaurre I, Soifer LO (2014). "Risk of infertility in patients with celiac disease: a meta-analysis of observational studies". Arquivos de Gastroenterologia. 51 (2): 144–50. doi:10.1590/S0004-28032014000200014. PMID 25003268.
- ^ Podfigurna-Stopa A, Czyzyk A, Grymowicz M, Smolarczyk R, Katulski K, Czajkowski K, Meczekalski B (September 2016). "Premature ovarian insufficiency: the context of long-term effects". Journal of Endocrinological Investigation. 39 (9): 983–90. doi:10.1007/s40618-016-0467-z. PMC 4987394. PMID 27091671.
- ^ a b Laissue P (August 2015). "Aetiological coding sequence variants in non-syndromic premature ovarian failure: From genetic linkage analysis to next generation sequencing". Molecular and Cellular Endocrinology (Review). 411: 243–57. doi:10.1016/j.mce.2015.05.005. PMID 25960166.
- ^ a b c Fenton AJ (2015). "Premature ovarian insufficiency: Pathogenesis and management". Journal of Mid-Life Health (Review). 6 (4): 147–53. doi:10.4103/0976-7800.172292. PMC 4743275. PMID 26903753.
- ^ a b Kalantaridou SN, Davis SR, Nelson LM (December 1998). "Premature ovarian failure". Endocrinology and Metabolism Clinics of North America. 27 (4): 989–1006. doi:10.1016/s0889-8529(05)70051-7. PMID 9922918.
- ^ Bucher, et al. 1930
- ^ a b c d Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, Sherman S, Sluss PM, de Villiers TJ (April 2012). "Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging". Fertility and Sterility. 97 (4): 843–51. doi:10.1016/j.fertnstert.2012.01.128. PMC 3340904. PMID 22341880.
- ^ a b c "Early or premature menopause". Womenshealth.gov. 12 July 2017. Retrieved 7 November 2018.
- ^ Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL (April 2006). "Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles". Archives of General Psychiatry. 63 (4): 385–90. doi:10.1001/archpsyc.63.4.385. PMID 16585467.
- ^ Soules MR, Sherman S, Parrott E, Rebar R, Santoro N, Utian W, Woods N (December 2001). "Executive summary: Stages of Reproductive Aging Workshop (STRAW)". Climacteric. 4 (4): 267–72. doi:10.1080/cmt.4.4.267.272. PMID 11770182. S2CID 28673617.
- ^ Prior JC (August 1998). "Perimenopause: the complex endocrinology of the menopausal transition". Endocrine Reviews. 19 (4): 397–428. doi:10.1210/edrv.19.4.0341. PMID 9715373.
- ^ a b Burger HG (January 1994). "Diagnostic role of follicle-stimulating hormone (FSH) measurements during the menopausal transition—an analysis of FSH, oestradiol and inhibin". European Journal of Endocrinology. 130 (1): 38–42. doi:10.1530/eje.0.1300038. PMID 8124478.
- ^ a b Nahás E, Pontes A, Traiman P, NahásNeto J, Dalben I, De Luca L (April 2003). "Inhibin B and ovarian function after total abdominal hysterectomy in women of reproductive age". Gynecological Endocrinology. 17 (2): 125–31. doi:10.1080/713603218. PMID 12737673.
- ^ a b Petri Nahás EA, Pontes A, Nahas-Neto J, Borges VT, Dias R, Traiman P (February 2005). "Effect of total abdominal hysterectomy on ovarian blood supply in women of reproductive age". Journal of Ultrasound in Medicine. 24 (2): 169–74. doi:10.7863/jum.2005.24.2.169. hdl:11449/224482. PMID 15661947. S2CID 30259666.
- ^ Simpson ER, Davis SR (November 2001). "Minireview: aromatase and the regulation of estrogen biosynthesis—some new perspectives". Endocrinology. 142 (11): 4589–94. doi:10.1210/endo.142.11.8547. PMID 11606422.
- ^ Davison SL, Bell R, Donath S, Montalto JG, Davis SR (July 2005). "Androgen levels in adult females: changes with age, menopause, and oophorectomy". The Journal of Clinical Endocrinology and Metabolism. 90 (7): 3847–53. doi:10.1210/jc.2005-0212. PMID 15827095.
- ^ Fogle RH, Stanczyk FZ, Zhang X, Paulson RJ (August 2007). "Ovarian androgen production in postmenopausal women". The Journal of Clinical Endocrinology and Metabolism. 92 (8): 3040–3. doi:10.1210/jc.2007-0581. PMID 17519304.
- ^ Skorupskaite K, George JT, Anderson RA (2014). "The kisspeptin-GnRH pathway in human reproductive health and disease". Human Reproduction Update. 20 (4): 485–500. doi:10.1093/humupd/dmu009. PMC 4063702. PMID 24615662.
- ^ a b Titus S, Li F, Stobezki R, Akula K, Unsal E, Jeong K, Dickler M, Robson M, Moy F, Goswami S, Oktay K (February 2013). "Impairment of BRCA1-related DNA double-strand break repair leads to ovarian aging in mice and humans". Science Translational Medicine. 5 (172): 172ra21. doi:10.1126/scitranslmed.3004925. PMC 5130338. PMID 23408054.
- ^ Brandl E, Mirzaghaderi G (September 2016). "The evolution of meiotic sex and its alternatives". Proceedings of the Royal Society B: Biological Sciences. 283 (1838). Proc Biol Sci. doi:10.1098/rspb.2016.1221. PMC 5031655. PMID 27605505.
- ^ Greene JG (May 1998). "Constructing a standard climacteric scale". Maturitas. 29 (1): 25–31. doi:10.1016/s0378-5122(98)00025-5. PMID 9643514.
- ^ Monterrosa-Castro A, Romero-Pérez I, Marrugo-Flórez M, Fernández-Alonso AM, Chedraui P, Pérez-López FR (August 2012). "Quality of life in a large cohort of mid-aged Colombian women assessed using the Cervantes Scale". Menopause. 19 (8): 924–30. doi:10.1097/gme.0b013e318247908d. PMID 22549166. S2CID 19201297.
- ^ Chedraui P, Pérez-López FR, Mendoza M, Leimberg ML, Martínez MA, Vallarino V, Hidalgo L (January 2010). "Factors related to increased daytime sleepiness during the menopausal transition as evaluated by the Epworth sleepiness scale". Maturitas. 65 (1): 75–80. doi:10.1016/j.maturitas.2009.11.003. PMID 19945237.
- ^ a b "What Is Perimenopause?". WebMD. Retrieved 6 October 2018.
- ^ "Perimenopause – Symptoms and causes". Mayo Clinic. Retrieved 6 October 2018.
- ^ "Menopause 101". A primer for the perimenopausal. The North American Menopause Society. Archived from the original on 10 April 2013. Retrieved 11 April 2013.
- ^ a b c Prior J. "Perimenopause". Centre for Menstrual Cycle and Ovulation Research (CeMCOR). Archived from the original on 25 February 2013. Retrieved 10 May 2013.
- ^ Chichester M, Ciranni P (August–September 2011). "Approaching menopause (but not there yet!): caring for women in midlife". Nursing for Women's Health. 15 (4): 320–4. doi:10.1111/j.1751-486X.2011.01652.x. PMID 21884497.
- ^ Silver DN (2023). "Mood Changes During Perimenopause Are Real. Here's What to Know". www.acog.org. Retrieved 27 March 2025.
- ^ Gilbert N (27 January 2022). "When depression sneaks up on menopause". Knowable Magazine. doi:10.1146/knowable-012722-1. Retrieved 17 May 2022.
- ^ Hurst BS (2011). Disorders of menstruation. Chichester, West Sussex: Wiley-Blackwell. ISBN 978-1-4443-9181-7.
- ^ a b McNamara M, Batur P, DeSapri KT (February 2015). "In the clinic. Perimenopause". Annals of Internal Medicine. 162 (3): ITC1–15. doi:10.7326/AITC201502030. PMID 25643316. S2CID 216041116.
- ^ Kessenich C. "Inevitable Menopause". Archived from the original on 2 November 2013. Retrieved 11 April 2013.
- ^ Bellipanni G, DI Marzo F, Blasi F, Di Marzo A (December 2005). "Effects of melatonin in perimenopausal and menopausal women: our personal experience". Annals of the New York Academy of Sciences. 1057 (1): 393–402. Bibcode:2005NYASA1057..393B. doi:10.1196/annals.1356.030. PMID 16399909. S2CID 25213110.
- ^ The Woman's Health Program Monash University, Oestrogen and Progestin as Hormone Therapy Archived 11 July 2012 at the Wayback Machine
- ^ North American Menopause Society (March 2010). "Estrogen and progestogen use in postmenopausal women: 2010 position statement of The North American Menopause Society". Menopause. 17 (2): 242–255. doi:10.1097/gme.0b013e3181d0f6b9. PMID 20154637. S2CID 24806751.
- ^ North American Menopause Society (March 2012). "The 2012 hormone therapy position statement of: The North American Menopause Society". Menopause. 19 (3): 257–71. doi:10.1097/GME.0000000000000921. PMC 3443956. PMID 22367731.
- ^ Sarri G, Pedder H, Dias S, Guo Y, Lumsden MA (September 2017). "Vasomotor symptoms resulting from natural menopause: a systematic review and network meta-analysis of treatment effects from the National Institute for Health and Care Excellence guideline on menopause" (PDF). BJOG. 124 (10): 1514–1523. doi:10.1111/1471-0528.14619. PMID 28276200. S2CID 206909766.
- ^ Boardman HM, Hartley L, Eisinga A, Main C, Roqué i Figuls M, Bonfill Cosp X, Gabriel Sanchez R, Knight B (March 2015). "Hormone therapy for preventing cardiovascular disease in post-menopausal women". The Cochrane Database of Systematic Reviews. 2015 (3) CD002229. doi:10.1002/14651858.CD002229.pub4. hdl:20.500.12105/9999. PMC 10183715. PMID 25754617.
- ^ de Villiers TJ, Stevenson JC (June 2012). "The WHI: the effect of hormone replacement therapy on fracture prevention". Climacteric. 15 (3): 263–6. doi:10.3109/13697137.2012.659975. PMID 22612613. S2CID 40340985.
- ^ a b Marjoribanks J, Farquhar C, Roberts H, Lethaby A, Lee J (January 2017). "Long-term hormone therapy for perimenopausal and postmenopausal women". The Cochrane Database of Systematic Reviews. 1 (1) CD004143. doi:10.1002/14651858.CD004143.pub5. PMC 6465148. PMID 28093732.
- ^ Chlebowski RT, Anderson GL (April 2015). "Menopausal hormone therapy and breast cancer mortality: clinical implications". Therapeutic Advances in Drug Safety. 6 (2): 45–56. doi:10.1177/2042098614568300. PMC 4406918. PMID 25922653.
- ^ Davis SR, Baber R, Panay N, Bitzer J, Cerdas Perez S, Islam RM, et al. (October 2019). "Global Consensus Position Statement on the Use of Testosterone Therapy for Women". Climacteric. 22 (5): 429–434. doi:10.1080/13697137.2019.1637079. hdl:2158/1176450. PMID 31474158. S2CID 201713094.
- ^ Davis SR, Dinatale I, Rivera-Woll L, Davison S (May 2005). "Postmenopausal hormone therapy: from monkey glands to transdermal patches". The Journal of Endocrinology. 185 (2): 207–22. doi:10.1677/joe.1.05847. PMID 15845914.
- ^ Bevers TB (September 2007). "The STAR trial: evidence for raloxifene as a breast cancer risk reduction agent for postmenopausal women". Journal of the National Comprehensive Cancer Network. 5 (8): 719–24. doi:10.6004/jnccn.2007.0073. PMID 17927929.
- ^ a b Potter B, Schrager S, Dalby J, Torell E, Hampton A (December 2018). "Menopause". Primary Care. Women's Health. 45 (4): 625–641. doi:10.1016/j.pop.2018.08.001. PMID 30401346. S2CID 239485855.
- ^ Goldstein KM, Shepherd-Banigan M, Coeytaux RR, McDuffie JR, Adam S, Befus D, et al. (April 2017). "Use of mindfulness, meditation and relaxation to treat vasomotor symptoms". Climacteric. 20 (2): 178–182. doi:10.1080/13697137.2017.1283685. PMID 28286985. S2CID 10446084.
- ^ van Driel CM, Stuursma A, Schroevers MJ, Mourits MJ, de Bock GH (February 2019). "Mindfulness, cognitive behavioural and behaviour-based therapy for natural and treatment-induced menopausal symptoms: a systematic review and meta-analysis". BJOG. 126 (3): 330–339. doi:10.1111/1471-0528.15153. PMC 6585818. PMID 29542222.
- ^ Hickey M, Szabo RA, Hunter MS (November 2017). "Non-hormonal treatments for menopausal symptoms". BMJ. 359 j5101. doi:10.1136/bmj.j5101. PMID 29170264. S2CID 46856968.
- ^ Moore TR, Franks RB, Fox C (May 2017). "Review of Efficacy of Complementary and Alternative Medicine Treatments for Menopausal Symptoms". Journal of Midwifery & Women's Health. 62 (3): 286–297. doi:10.1111/jmwh.12628. PMID 28561959. S2CID 4756342.
- ^ Peters, Brandilyn A, et al. (10 August 2022). "Spotlight on the Gut Microbiome in Menopause: Current Insights". International Journal of Women's Health. 14: 1059–1072. doi:10.2147/IJWH.S340491. PMC 9379122. PMID 35983178.
- ^ Yu, S, et al. (2025). "Deciphering the influence of gut and oral microbiomes on menopause". Journal of Genetics and Genomics. 52 (5): 601–614. doi:10.1016/j.jgg.2024.11.010. PMID 39577767. Retrieved 15 October 2025.
- ^ Zhang, P, et al. (24 August 2022). "Influence of Foods and Nutrition on the Gut Microbiome and Implications for Intestinal Health". [International Journal of Molecular Sciences]. 23 (17): 9588. doi:10.3390/ijms23179588. PMC 9455721. PMID 36076980.
- ^ British Dietetic Association, et al. (April 2025). "Eating well for the perimenopause and menopause". British Dietetic Association. Retrieved 15 October 2025.
- ^ Barton, Fionnuala (21 July 2025). "Your Gut Microbiome in Menopause". Field Doctor. Retrieved 15 October 2025.
- ^ Clement YN, Onakpoya I, Hung SK, Ernst E (March 2011). "Effects of herbal and dietary supplements on cognition in menopause: a systematic review". Maturitas. 68 (3): 256–63. doi:10.1016/j.maturitas.2010.12.005. PMID 21237589.
- ^ a b c Nedrow A, Miller J, Walker M, Nygren P, Huffman LH, Nelson HD (July 2006). "Complementary and alternative therapies for the management of menopause-related symptoms: a systematic evidence review". Archives of Internal Medicine. 166 (14): 1453–65. doi:10.1001/archinte.166.14.1453. PMID 16864755.
- ^ Franco OH, Chowdhury R, Troup J, Voortman T, Kunutsor S, Kavousi M, et al. (June 2016). "Use of Plant-Based Therapies and Menopausal Symptoms: A Systematic Review and Meta-analysis". JAMA. 315 (23): 2554–2563. doi:10.1001/jama.2016.8012. PMID 27327802.
- ^ Leach MJ, Moore V (September 2012). "Black cohosh (Cimicifuga spp.) for menopausal symptoms". The Cochrane Database of Systematic Reviews. 9 (9) CD007244. doi:10.1002/14651858.CD007244.pub2. PMC 6599854. PMID 22972105.
- ^ Dodin S, Blanchet C, Marc I, Ernst E, Wu T, Vaillancourt C, Paquette J, Maunsell E (July 2013). "Acupuncture for menopausal hot flushes". The Cochrane Database of Systematic Reviews. 7 (7) CD007410. doi:10.1002/14651858.CD007410.pub2. PMC 6544807. PMID 23897589.
- ^ Zhu X, Liew Y, Liu ZL (March 2016). "Chinese herbal medicine for menopausal symptoms". The Cochrane Database of Systematic Reviews. 3 (5) CD009023. doi:10.1002/14651858.CD009023.pub2. PMC 4951187. PMID 26976671.
- ^ Wells GA, Cranney A, Peterson J, Boucher M, Shea B, Robinson V, Coyle D, Tugwell P (January 2008). "Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women". The Cochrane Database of Systematic Reviews (1) CD001155. doi:10.1002/14651858.CD001155.pub2. PMID 18253985.
- ^ "Concerns over new 'menopause delay' procedure". BBC News. 28 January 2020.
- ^ Evans S (2024). "The need for biopsychosocial menopause care: a narrative review". Menopause (New York, N.Y.). 31 (12): 1090–1096. doi:10.1097/GME.0000000000002441. PMID 39470610.
- ^ Gannon L, Ekstrom B (1993). "Attitudes toward menopause: The influence of sociocultural paradigms". Psychology of Women Quarterly. 17 (3): 275–88. doi:10.1111/j.1471-6402.1993.tb00487.x. hdl:2286/R.I.44298. S2CID 144546258.
- ^ a b Ayers B, Forshaw M, Hunter MS (January 2010). "The impact of attitudes towards the menopause on women's symptom experience: a systematic review". Maturitas. 65 (1): 28–36. doi:10.1016/j.maturitas.2009.10.016. PMID 19954900. S2CID 486661.
- ^ Brown L, Brown V, Judd F, Bryant C (2 October 2018). "It's not as bad as you think: menopausal representations are more positive in postmenopausal women". Journal of Psychosomatic Obstetrics & Gynecology. 39 (4): 281–288. doi:10.1080/0167482X.2017.1368486. ISSN 0167-482X. PMID 28937311. S2CID 24085899.
- ^ a b Voicu, Ilona. "The social construction of menopause as disease: A literature review." Journal of Comparative Research in Anthropology and Sociology, vol. 9, no. 2 (Winter 2018): 71–82. ISSN 2068-0317. http://compaso.eu/wpd/wp-content/uploads/2019/02/Voicu_Journal-of-Comparative-Research-in-Anthropology-and-Sociology_vol9_issue2.pdf
- ^ Williams M (2024). "Culturally responsive care for menopausal women". Maturitas. 185 107995. doi:10.1016/j.maturitas.2024.107995. PMID 38663163.
- ^ a b Bansal, Ramandeep, and Neelam Aggarwal. "Menopausal Hot Flashes: A Concise Review." Journal of Mid-Life Health 10, no. 1 (2019): 6–13. Available via EBSCO.
- ^ a b c Martin, Emily. The Woman in the Body: A Cultural Analysis of Reproduction. Boston, MA: Beacon Press, 1987. Available via Alexander Street
- ^ Hoga L, Rodolpho J, Gonçalves B, Quirino B (September 2015). "Women's experience of menopause: a systematic review of qualitative evidence". JBI Database of Systematic Reviews and Implementation Reports. 13 (8): 250–337. doi:10.11124/jbisrir-2015-1948. PMID 26455946. S2CID 21908463.
- ^ Dashti S, Bahri N, Fathi Najafi T, Amiridelui M, Latifnejad Roudsari R (September 2021). "Influencing factors on women's attitudes toward menopause: a systematic review". Menopause. 28 (10): 1192–1200. doi:10.1097/GME.0000000000001833. PMID 34520416. S2CID 237516036.
- ^ Avis N, Stellato RC, Bromberger J, Gan P, Cain V, Kagawa-Singer M (2001). "Is there a menopausal syndrome? Menopausal status and symptoms across racial/ethnic group". Social Science & Medicine. 52 (3): 345–56. doi:10.1016/S0277-9536(00)00147-7. PMID 11330770.
- ^ Stanzel KA, Hammarberg K, Fisher J (April 2018). "Experiences of menopause, self-management strategies for menopausal symptoms and perceptions of health care among immigrant women: a systematic review". Climacteric. 21 (2): 101–110. doi:10.1080/13697137.2017.1421922. PMID 29345497. S2CID 3653549.
- ^ Haines CJ, Xing SM, Park KH, Holinka CF, Ausmanas MK (November 2005). "Prevalence of menopausal symptoms in different ethnic groups of Asian women and responsiveness to therapy with three doses of conjugated estrogens/medroxyprogesterone acetate: the Pan-Asia Menopause (PAM) study". Maturitas. 52 (3–4): 264–276. doi:10.1016/j.maturitas.2005.03.012. PMID 15921865.
- ^ Sayakhot P, Vincent A, Teede H (December 2012). "Cross-cultural study: experience, understanding of menopause, and related therapies in Australian and Laotian women". Menopause. 19 (12): 1300–1308. doi:10.1097/gme.0b013e31825fd14e. PMID 22929035. S2CID 205613667.
- ^ a b Lock M (1998). "Menopause: lessons from anthropology". Psychosomatic Medicine. 60 (4): 410–9. doi:10.1097/00006842-199807000-00005. PMID 9710286. S2CID 38878080.
- ^ Melby MK (2005). "Factor analysis of climacteric symptoms in Japan". Maturitas. 52 (3–4): 205–22. doi:10.1016/j.maturitas.2005.02.002. PMID 16154301.
- ^ a b Lock M, Nguyen V (2010). "Chapter 4: Local Biologies and Human Difference". An Anthropology of Biomedicine. West Sussex: Wiley-Blackwell. pp. 84–89.
- ^ Gold EB, Block G, Crawford S, Lachance L, FitzGerald G, Miracle H, Sherman S (June 2004). "Lifestyle and demographic factors in relation to vasomotor symptoms: baseline results from the Study of Women's Health Across the Nation". American Journal of Epidemiology. 159 (12): 1189–99. doi:10.1093/aje/kwh168. PMID 15191936.
- ^ Maoz B, Dowty N, Antonovsky A, Wisjenbeck H (1970). "Female attitudes to menopause". Social Psychiatry. 5: 35–40. doi:10.1007/BF01539794. S2CID 30147685.
- ^ Stotland NL (August 2002). "Menopause: social expectations, women's realities". Archives of Women's Mental Health. 5 (1): 5–8. doi:10.1007/s007370200016. PMID 12503068. S2CID 9248759.
- ^ Blackson EA, McCarthy C, Bell C, Ramirez S, Bazzano AN (2024). "Experiences of menopausal transition among populations exposed to chronic psychosocial stress in the United States: A scoping review". BMC Women's Health. 24 (1) 487. doi:10.1186/s12905-024-03329-z. PMC 11373288. PMID 39232712.
- ^ a b Melby MK, Lampl M (2011). "Menopause, A Biocultural Perspective". Annual Review of Anthropology. 40: 53–70. doi:10.1146/annurev-anthro-081309-145641.
- ^ Mohamed S, Hunter MS (2019). "Transgender women's experiences and beliefs about hormone therapy through and beyond mid-age: An exploratory UK study". International Journal of Transgenderism. 20 (1): 98–107. doi:10.1080/15532739.2018.1493626. PMC 6831003. PMID 32999597.
- ^ a b c d Toze M, Westwood S (2025). "Experiences of menopause among non-binary and trans people". International Journal of Transgender Health. 26 (2): 447–458. doi:10.1080/26895269.2024.2389924. PMC 12016236. PMID 40276004.
- ^ University of Cambridge. (2023, 7 February). GP survey reveals health and healthcare inequalities of trans and non-binary adults. Retrieved from https://www.cam.ac.uk/research/news/gp-survey-reveals-health-and-healthcare-inequalities-of-trans-and-non-binary-adults
- ^ a b c d e f Lock M (1988). "new Japanese mythologies: faltering discipline and the ailing housewife". American Ethnologist. 15 (1): 43–61. doi:10.1525/ae.1988.15.1.02a00040. ISSN 1548-1425.
- ^ a b Beyene Y (1986). "Cultural significance and physiological manifestations of menopause a biocultural analysis". Culture, Medicine and Psychiatry. 10 (1): 47–71. doi:10.1007/BF00053262. PMID 3698649. Retrieved 8 August 2025.
- ^ Stewart DE (2003). "Menopause in highland Guatemala Mayan women". Maturitas. 44 (4): 293–297. doi:10.1016/s0378-5122(03)00036-7. PMID 12697370. Retrieved 8 August 2025.
- ^ Melby MK (2005). "Culture and Symptom Reporting At Menopause". Human Reproduction Update. 11 (5): 495–512. doi:10.1093/humupd/dmi018. PMID 15919681. Retrieved 8 August 2025.
- ^ a b c Davis SR, Magraith K (19 June 2023). "Advancing menopause care in Australia: barriers and opportunities". Medical Journal of Australia. 218 (11): 500–502. doi:10.5694/mja2.51981. ISSN 0025-729X. PMID 37330995.
- ^ Jones EK, Jurgenson JR, Katzenellenbogen JM, Thompson SC (12 December 2012). "Menopause and the influence of culture: another gap for Indigenous Australian women?". BMC Women's Health. 12 43. doi:10.1186/1472-6874-12-43. ISSN 1472-6874. PMC 3554544. PMID 23234340.
- ^ "Work related stress, depression or anxiety" (PDF). Health and Safety Executive (HSE). 31 October 2018.
- ^ Griffiths A, S Hunter M (2015). "Psychosocial factors and menopause: The impact of menopause on personal and working life". In C Davies S (ed.). Annual Report of the Chief Medical Officer, 2014, The Health of the 51%: Women (PDF). Department of Health.
- ^ Faubion SS, Enders F, Hedges MS, Chaudhry R, Kling JM, Shufelt CL, Saadedine M, Mara K, Griffin JM, Kapoor E (1 June 2023). "Impact of Menopause Symptoms on Women in the Workplace". Mayo Clinic Proceedings. 98 (6): 833–845. doi:10.1016/j.mayocp.2023.02.025. ISSN 0025-6196. PMID 37115119. S2CID 258367393.
- ^ Moore ADM |2022|The French Invention of Menopause and the Medicalisation of Women's Ageing, A History|Oxford University Press |page 85
- ^ Moore AM (2018). "Conceptual Layers in the Invention of Menopause in Nineteenth-Century France". French History. 32 (2): 226–248. doi:10.1093/fh/cry006.
- ^ a b Walker ML, Herndon JG (September 2008). "Menopause in nonhuman primates?". Biology of Reproduction. 79 (3): 398–406. doi:10.1095/biolreprod.108.068536. PMC 2553520. PMID 18495681.
- ^ "'Breakthrough moment': how Lorraine Kelly helped shift the menopause debate". The Guardian. 29 April 2022. Retrieved 2 August 2022.
- ^ "Davina McCall: Sex, Myths and the Menopause". www.channel4.com. Retrieved 3 July 2023.
- ^ House of Commons (27 October 2021). "Menopause (Support and Services) Bill, House of Commons, Session 2021-22".
- ^ McKinley, David B. (6 September 2022). "H.R.8774 - Menopause Research Act of 2022".
- ^ Winkler I, Goncalves A (October 2023). "Do mammals have menopause?". Cell. 186 (22): 4729–4733. doi:10.1016/j.cell.2023.09.026. PMID 37890455.
- ^ a b Ellis S, Franks DW, Nattrass S, Currie TE, Cant MA, Giles D, Balcomb KC, Croft DP (August 2018). "Analyses of ovarian activity reveal repeated evolution of post-reproductive lifespans in toothed whales". Scientific Reports. 8 (1) 12833. Bibcode:2018NatSR...812833E. doi:10.1038/s41598-018-31047-8. PMC 6110730. PMID 30150784.
- ^ Brent LJ, Franks DW, Foster EA, Balcomb KC, Cant MA, Croft DP (March 2015). "Ecological knowledge, leadership, and the evolution of menopause in killer whales". Current Biology. 25 (6): 746–750. Bibcode:2015CBio...25..746B. doi:10.1016/j.cub.2015.01.037. hdl:10871/32919. PMID 25754636.
- ^ Article | Reuters - Why did menopause evolve? New study of whales gives some clues
- ^ Marsh H, Kasuya T (1986). "Evidence for reproductive senescence in female cetaceans" (PDF). Reports of the International Whaling Commission. pp. 57–74. Archived from the original (PDF) on 21 September 2020. Retrieved 9 June 2018.
- ^ Walker ML (1995). "Menopause in female rhesus monkeys". American Journal of Primatology. 35 (1): 59–71. doi:10.1002/ajp.1350350106. PMC 10590078. PMID 31924061. S2CID 83848539.
- ^ Bowden DM, Williams DD (1984). "Aging". Research on Nonhuman Primates. Advances in Veterinary Science and Comparative Medicine. Vol. 28. pp. 305–341. doi:10.1016/b978-0-12-039228-5.50015-2. ISBN 978-0-12-039228-5. PMID 6395674.
- ^ Emery Thompson M, Jones JH, Pusey AE, Brewer-Marsden S, Goodall J, Marsden D, et al. (December 2007). "Aging and fertility patterns in wild chimpanzees provide insights into the evolution of menopause". Current Biology. 17 (24): 2150–6. Bibcode:2007CBio...17.2150E. doi:10.1016/j.cub.2007.11.033. PMC 2190291. PMID 18083515.
- ^ Sukumar R (1992). The Asian Elephant. Cambridge University Press. ISBN 978-0-521-43758-5. Archived from the original on 12 May 2016.
- ^ Reznick D, Bryant M, Holmes D (January 2006). "The evolution of senescence and post-reproductive lifespan in guppies (Poecilia reticulata)". PLOS Biology. 4 (1) e7. doi:10.1371/journal.pbio.0040007. PMC 1318473. PMID 16363919.
- ^ "How long is a cat in heat?". Animal Planet. 15 May 2012. Archived from the original on 14 November 2015. Retrieved 12 June 2018.
- ^ Almansa JC (16 November 2022). "The evolutionary origins of menopause explained". The Conversation. Retrieved 20 September 2023.
Further reading
[edit]- Rebecca Mead, "If You Can't Stand the Heat: Why menopause never gets old", The New Yorker, 10 March 2025, pp. 28–31. "If you've got ovaries, you'll go through it. Why do so many feel so blindsided?" (p. 28.)
External links
[edit]- Menopause: MedlinePlus
- What Is Menopause?, National Institute on Aging
- Menopause & Me, The North American Menopause Society
Menopause
View on GrokipediaDefinition and Stages
Definition
Menopause is defined as the permanent cessation of menstrual cycles resulting from the loss of ovarian follicular function and the attendant decline in ovarian hormone production, particularly estrogen and progesterone.[3][1] This physiological event marks the end of a woman's natural reproductive capability, as the ovaries no longer release eggs and menstrual periods cease.[4] Clinically, menopause is retrospectively diagnosed after 12 consecutive months without menses, in the absence of pathological conditions, surgical interventions, or other causes that could explain the amenorrhea.[5][6] The average age of natural menopause worldwide is approximately 51 years, though it typically occurs between ages 45 and 55, with variations influenced by genetic, environmental, and lifestyle factors.[1][3] In populations of European descent, the mean age is around 51 years, while it may be slightly earlier in some other ethnic groups, such as African American women at about 49 years.[1] Menopause represents a universal biological milestone in female aging, distinct from perimenopause (the transitional phase preceding it) and postmenopause (the period following), though the term is sometimes used more broadly to encompass the entire climacteric transition.[4][5] Premature menopause, occurring before age 40, or early menopause before age 45, affects a smaller subset of women and may stem from autoimmune disorders, genetic conditions like fragile X syndrome, or medical treatments such as chemotherapy, but these are exceptions to the normative process driven by ovarian follicle depletion over time.[1][3] The diagnosis relies on clinical history rather than laboratory tests alone, as hormone levels like follicle-stimulating hormone (FSH) fluctuate and are not definitive until the 12-month criterion is met.[5][6]Perimenopause
Perimenopause is the transitional phase immediately preceding menopause, defined by the onset of irregular menstrual cycles due to declining ovarian follicle reserve and associated hormonal fluctuations. This stage reflects the gradual diminution of ovarian function, leading to reduced ovulatory cycles and eventual cessation of menses. It is distinguished from menopause proper, which is retrospectively diagnosed after 12 consecutive months of amenorrhea in the absence of other causes.[7][8] The onset typically occurs between ages 40 and 44, with a median age of 47 years in the United States, though variability exists influenced by factors such as genetics, smoking, and body mass index. Duration averages four years but can extend from several months to 10 years or more, with longer phases often correlating with greater symptom severity; one longitudinal study reported a mean duration of 3.8 to 6.25 years. Perimenopause is subdivided into early and late stages per the STRAW+10 criteria: early perimenopause features persistent cycle shortening or skipping, while late perimenopause involves amenorrhea of 60 days or longer but less than 12 months.[9][10][11] Hormonally, perimenopause involves erratic elevations in follicle-stimulating hormone (FSH) as feedback from diminishing ovarian estrogen production weakens, alongside fluctuating estradiol levels that can surge before progressive decline, and reduced progesterone due to anovulatory cycles. These changes drive symptoms including vasomotor instability (hot flashes, night sweats), sleep disruption, mood variability, and menstrual irregularities such as heavier or lighter flows and cycle lengths varying by seven days or more. Urogenital effects like vaginal dryness may emerge early, linked to falling estrogen. Symptom onset and intensity vary, with evidence indicating that higher premenopausal body mass index predicts more severe vasomotor symptoms.[7][12][13] Diagnosis relies primarily on clinical history—age-appropriate menstrual irregularity and symptoms—rather than biomarkers, as FSH levels fluctuate widely and lack specificity; elevated FSH exceeding 30 IU/L on a single measurement supports ovarian insufficiency but is neither necessary nor sufficient for confirmation, with guidelines advising against routine testing in women over 45. Differential diagnosis excludes pregnancy, thyroid dysfunction, or hyperprolactinemia via targeted labs when indicated. Fertility declines markedly, though conception remains possible until menopause, necessitating contraception until amenorrhea persists for one year.[14][15][16]Menopause
Menopause is defined as the permanent cessation of menstrual cycles resulting from the loss of ovarian follicular function and confirmed retrospectively after 12 consecutive months of amenorrhea in the absence of pathological or physiological causes.[1][17] This anchor point, known as the final menstrual period (FMP), marks the end of the menopausal transition and the onset of postmenopause.[18] In the Stages of Reproductive Aging Workshop +10 (STRAW+10) staging system, menopause corresponds to stage +0, following the late menopausal transition (stage -1), during which irregular cycles and symptoms intensify before the FMP.[19][20] The diagnosis of menopause is typically clinical and retrospective, relying on the absence of menses for one year without requiring laboratory confirmation in women over age 45, though elevated follicle-stimulating hormone (FSH) levels above 30 IU/L in the early follicular phase can support it if needed.[1] It differs from perimenopause, which encompasses variable cycle lengths and bleeding leading up to the FMP, and postmenopause, the years following the FMP characterized by sustained hypoestrogenism.[21] Natural menopause excludes cases induced by surgery, chemotherapy, or radiation, which can occur prematurely.[22] Globally, the average age at natural menopause ranges from 45 to 55 years, with a median around 49 to 51 years depending on ethnicity and region; for instance, it is approximately 51 years in North America and Europe, lower in Latin America (around 48.6 years), and varies within Asia (around 51 years overall).[3][23][24] In the United States, trends show an increase from 48.4 years in the early 1960s to 49.9 years by 2015-2018, potentially linked to improved health and nutrition.[25] Factors influencing timing include genetics, smoking (which advances onset by 1-2 years), parity, and socioeconomic status, though no universal predictors exist beyond these.[26][27]Postmenopause
Postmenopause is defined as the phase of a woman's life that follows menopause, commencing 12 months after the final menstrual period and continuing for the remainder of her lifespan. During this period, ovarian function has ceased, with negligible production of estrogen and progesterone, leading to sustained hypoestrogenic states that influence multiple physiological systems.[4][1][28] Hormonal profiles in postmenopause reflect the culmination of ovarian aging, characterized by persistently low circulating levels of estradiol (typically below 20-30 pg/mL) and elevated follicle-stimulating hormone (FSH) concentrations exceeding 30 IU/L. These changes arise from follicular depletion, rendering the ovaries unresponsive to gonadotropins, and contribute to altered metabolism, including shifts in lipid profiles with increased low-density lipoprotein cholesterol and decreased high-density lipoprotein in some women.[28][29] Many symptoms from the menopausal transition diminish over time in postmenopause, but vasomotor symptoms such as hot flashes persist in a subset of women, with a median duration of 4.5 years after the final menstrual period among those experiencing them, though up to 10-20% report symptoms lasting beyond 10 years or even into the seventh decade of life. Genitourinary symptoms, including vaginal dryness and urinary urgency, often endure or emerge due to urogenital atrophy from estrogen deficiency, affecting quality of life in up to 50% of postmenopausal women without intervention. Cognitive and mood disturbances may also continue, linked to hormonal fluctuations and sleep disruption, though evidence for direct causality remains correlative rather than definitive.[30][31][32] Long-term health risks escalate in postmenopause due to estrogen's protective roles in vascular, skeletal, and metabolic homeostasis. Osteoporosis risk rises markedly, with postmenopausal women facing a 2-3 fold increase in fracture incidence compared to premenopausal counterparts, driven by accelerated bone resorption exceeding formation; vertebral, hip, and wrist fractures predominate, contributing to morbidity in over 20% of women by age 80. Cardiovascular disease incidence surges, becoming the leading cause of death, as estrogen withdrawal promotes endothelial dysfunction, atherogenesis, and adverse lipid changes, with relative risk elevation of 2-4 times within 10 years post-menopause in observational cohorts. These risks are modulated by factors like age at menopause onset, with earlier transition (before age 45) amplifying hazards via prolonged hypoestrogenism.[33][34][35] Lifestyle and pharmacological interventions, such as bisphosphonates for bone density or selective estrogen receptor modulators, can mitigate these effects, but their efficacy varies by individual risk profiles and timing relative to menopause onset. Empirical data underscore the need for personalized assessment, as randomized trials like the Women's Health Initiative indicate that hormone therapy initiated near menopause may confer cardiovascular benefits in select low-risk groups, though absolute risks of stroke and thrombosis persist.[36][37]Physiology and Causes
Ovarian Aging and Hormonal Changes
Ovarian aging is characterized by the irreversible depletion of the primordial follicle pool, which begins in fetal life and continues throughout reproductive years without replenishment. Females are born with an estimated 1 to 2 million primordial follicles, which represent the lifelong reserve of potential oocytes. By the onset of puberty, this number has declined to approximately 300,000 to 400,000 due to continuous atresia and minimal recruitment into growth phases. The process accelerates post-puberty, driven by both passive loss and active follicle activation, culminating in menopause when fewer than 1,000 primordial follicles remain, insufficient to sustain regular ovulatory cycles.[38][39][40] This follicle exhaustion disrupts ovarian steroidogenesis, leading to profound hormonal shifts. In the perimenopausal transition, reduced follicle numbers result in erratic gonadotropin stimulation, with follicle-stimulating hormone (FSH) levels rising due to diminished inhibin B and estrogen-mediated negative feedback on the pituitary. Estrogen production fluctuates markedly—sometimes surging from fewer but hyper-responsive follicles—while progesterone declines owing to shortened luteal phases and increased anovulation. By menopause, ovarian estrogen (primarily estradiol) falls to low levels (<20–30 pg/mL), progesterone becomes negligible outside of peripheral sources, and FSH persistently elevates above 30 mIU/mL, reflecting the loss of ovarian feedback. Luteinizing hormone (LH) also rises but to a lesser extent than FSH.[41][42][1] These changes stem causally from the finite nature of the follicle reserve and age-related oocyte quality decline, including increased chromosomal aneuploidy and mitochondrial dysfunction, which impair follicular maturation. Postmenopause, residual ovarian stromal cells produce androgens that undergo peripheral conversion to estrogens, but overall hypoestrogenism persists, driving systemic effects. Empirical studies confirm that follicle density correlates inversely with age, with mathematical models predicting exponential depletion rates that align with average menopausal onset around age 51 in populations without interventions.[43][44][45]Premature Ovarian Insufficiency
Premature ovarian insufficiency (POI), also known as primary ovarian insufficiency, refers to the loss of ovarian follicular function before age 40, leading to oligo- or amenorrhea for at least four months and elevated follicle-stimulating hormone (FSH) levels above 25 IU/L on two separate occasions at least one month apart, alongside low estradiol concentrations.[46] This condition results in premature cessation of ovarian estrogen production, mimicking menopausal hormonal profiles but occurring in reproductive-age women, with approximately 1% prevalence among females under 40 years.[47] Unlike natural menopause, POI often presents with intermittent ovarian activity, allowing for sporadic ovulation in up to 5-10% of cases, though fertility remains severely impaired.[48] The primary physiological mechanism involves accelerated depletion of the ovarian follicle reserve, driven by follicular atresia or impaired folliculogenesis, leading to diminished granulosa cell function and reduced ovarian steroidogenesis.[46] Causes are multifactorial, with 70-90% classified as idiopathic, lacking identifiable etiology despite evaluation.[49] Genetic factors account for 20-30% of cases, including chromosomal abnormalities such as Turner syndrome (45,X) or X-chromosome mosaicism, and monogenic mutations in genes like FMR1 (premutation carriers), FOXL2, or BMP15, which disrupt oocyte development or survival.[50] Autoimmune etiologies contribute in 10-20% of instances, often linked to polyglandular autoimmune syndromes involving anti-ovarian antibodies targeting steroidogenic cells, with associated conditions like Hashimoto's thyroiditis or Addison's disease increasing risk.[51] Iatrogenic causes, responsible for 5-10% of cases, stem from gonadotoxic therapies such as alkylating chemotherapy agents (e.g., cyclophosphamide) or pelvic radiation, which induce direct follicular apoptosis, or surgical oophorectomy.[52] Familial aggregation elevates risk, with first-degree relatives of affected women showing a 5-10-fold higher incidence, underscoring heritable components.[53] Diagnosis requires exclusion of secondary hypogonadism via clinical evaluation, including menstrual history, symptom assessment for vasomotor instability, and laboratory confirmation of hypergonadotropic hypogonadism (FSH >25 IU/L, estradiol <50 pg/mL), supplemented by low anti-Müllerian hormone (AMH) levels and transvaginal ultrasound revealing small ovaries with reduced antral follicle count.[54] Karyotyping, FMR1 testing, and adrenal autoantibody screening are recommended to identify treatable or genetic causes, as up to 13% of POI cases harbor FMR1 premutations.[48] Untreated POI confers elevated long-term risks, including osteoporosis (due to hypoestrogenism-induced bone loss, with fracture rates 2-3 times higher), cardiovascular disease (e.g., coronary artery disease and stroke, with hazard ratios up to 1.5-2.0), and overall mortality from endocrine deficiencies.[55] Hormone replacement therapy (HRT) with estrogen and progestin until age 50-51 (approximate natural menopause) mitigates these sequelae, preserving bone density and cardiovascular health without increased breast cancer risk in this population, per observational data from cohorts like the Danish POI registry.[56] Fertility preservation via oocyte cryopreservation prior to gonadotoxic exposure or egg donation post-diagnosis represents standard management for reproductive goals.[48]Surgical or Induced Menopause
Surgical menopause results from the bilateral surgical removal of the ovaries (bilateral salpingo-oophorectomy), which immediately eliminates ovarian production of estrogen and progesterone, inducing a state of hypoestrogenism akin to postmenopause but without preceding perimenopausal fluctuations. This procedure is frequently performed concurrently with hysterectomy to address conditions such as ovarian cysts, endometriosis, or uterine cancer, or prophylactically in women with genetic predispositions like BRCA1/2 mutations to reduce ovarian cancer risk. In the United States, an estimated 55-80% of the approximately 600,000 annual hysterectomies in premenopausal women include oophorectomy, contributing to surgical menopause in a substantial proportion of cases.[57][58] The abrupt hormonal cessation in surgical menopause contrasts with natural menopause's gradual decline, leading to more intense and sudden onset of symptoms including vasomotor instability and urogenital atrophy, alongside elevated long-term risks for osteoporosis—particularly in women under 45 years—and cardiovascular disease due to unmitigated estrogen deficiency. Elevated follicle-stimulating hormone (FSH) levels confirm ovarian failure, often exceeding 30 IU/L post-surgery. Current guidelines from organizations like the British Menopause Society recommend initiating hormone replacement therapy (HRT) immediately post-oophorectomy in women under 45 (or until age 51, the average natural menopause age) to counteract bone density loss and cardiometabolic risks, unless contraindicated by conditions such as hormone-sensitive cancers.[58][59][60] Induced menopause, distinct from surgical causes, stems from medical treatments like chemotherapy or pelvic radiation that inflict direct toxicity on ovarian follicles, accelerating atresia and precipitating premature ovarian insufficiency. Alkylating agents (e.g., cyclophosphamide) and high-dose radiation to the pelvis are primary culprits, with ovarian damage risk correlating inversely with age: women over 40 face near-certain permanent failure, while younger patients may experience transient amenorrhea or delayed menopause. This results in variable but often rapid hypoestrogenism, with FSH surges indicating depleted follicular reserve; long-term sequelae mirror surgical menopause, including heightened infertility and endocrine disruption persisting years post-treatment.[61][62][63] In both surgical and induced forms, the underlying physiology involves irreversible loss of granulosa cell function, halting estradiol synthesis and feedback inhibition on the hypothalamic-pituitary axis, thereby sustaining hypergonadotropic hypogonadism. Population studies indicate surgical menopause accounts for 10-15% of all menopause cases in Western cohorts, with induced cases varying by cancer incidence and treatment protocols. Management emphasizes individualized HRT assessment to balance symptom relief against potential thrombotic or neoplastic risks, prioritizing estrogen-only therapy post-hysterectomy where feasible.[64][65][66]Symptoms and Effects
Vasomotor Symptoms
Vasomotor symptoms (VMS), commonly manifesting as hot flashes and night sweats, involve sudden episodes of intense heat sensation, typically originating in the face, neck, and chest, accompanied by peripheral vasodilation, perspiration, and sometimes chills or palpitations upon cooling. These symptoms arise from dysregulation in the hypothalamus, where declining estrogen levels during the menopausal transition narrow the thermoneutral zone, prompting inappropriate activation of heat-loss effectors like sweating and skin vasodilation even without elevated core temperature.[67] [68] This central thermoregulatory instability is linked to altered activity in kisspeptin/neurokinin B/dynorphin (KNDy) neurons and neurotransmitter systems, including serotonin and norepinephrine, rather than solely peripheral vascular changes.[67] VMS affect 60-80% of women during the menopausal transition, with prevalence peaking in late perimenopause and early postmenopause, often beginning before the final menstrual period.[68] The median duration is approximately 7-10 years from onset, though some women experience symptoms for over a decade, particularly if starting early in perimenopause.[67] Frequency varies, with episodes lasting 1-5 minutes and occurring from several times a day to nightly, contributing to sleep disruption and reduced quality of life.[67] Racial and ethnic variations influence VMS prevalence and persistence, with African American women reporting the highest rates (up to 80-90% lifetime prevalence) and longest duration (median 10.1 years), followed by Hispanic women, while Japanese and Chinese women experience the lowest (around 20-30%).[68] [67] Key risk factors include smoking (60% increased odds), obesity (BMI >30 kg/m² associated with frequent VMS), low socioeconomic status, negative affect or anxiety, and lower endogenous estrogen levels, independent of age or menopausal stage.[68] These disparities persist after adjusting for socioeconomic and lifestyle confounders, suggesting genetic or cultural influences beyond traditional risk profiles.[68]Urogenital and Sexual Effects
Genitourinary syndrome of menopause (GSM) refers to a collection of symptoms and signs affecting the vulva, vagina, and lower urinary tract due to estrogen deficiency during perimenopause and postmenopause.[69] This hypoestrogenic state leads to structural changes including thinning of the vaginal epithelium, reduced vascularity, and increased pH, which impair tissue resilience and lubrication.[70] Prevalence of GSM varies widely, estimated at 13% to 87% among postmenopausal women, with factors such as age, time since menopause, and symptom assessment methods contributing to the range.[71] Symptoms often emerge gradually, with vaginal dryness reported in up to 50% of cases and many affected women not seeking treatment due to underrecognition or normalization of discomfort.[72] Urogenital manifestations include vulvovaginal dryness, irritation, burning, and pruritus, alongside urinary symptoms such as urgency, frequency, dysuria, nocturia, recurrent urinary tract infections, and incontinence.[70] Estrogen depletion causes atrophy of the vaginal mucosa, reducing its thickness from approximately 3-4 mm premenopausally to 1 mm or less, which heightens susceptibility to trauma and infection.[73] Urinary symptoms arise from analogous changes in the urethral and bladder epithelium, leading to weakened pelvic floor support and altered bladder function; for instance, stress urinary incontinence affects nearly 50% of postmenopausal women in some cohorts.[74] These effects can significantly impair daily activities and quality of life, though severity varies individually based on baseline estrogen sensitivity and comorbidities.[75] Sexual effects encompass dyspareunia, reduced lubrication, and diminished arousal, often exacerbated by vaginal atrophy and dryness during intercourse.[76] Decreased libido occurs in a substantial subset of menopausal women, with estrogen decline contributing to decreased desire, difficulty achieving orgasm, vaginal dryness, or pain during intercourse in 10-50% of women; however, experiences vary, and some report enhanced desire post-menopause due to factors such as absence of pregnancy concerns, increased privacy, and greater confidence.[77] Declining levels of estrogen and testosterone contribute to reduced arousal, vaginal dryness, pain during sex, fatigue from hot flashes and night sweats, and mood changes—alongside associated health issues including joint pain, medications, chronic diseases, stress, depression, and anxiety; partner-related factors such as male erectile dysfunction; and psychological or relationship elements like long-term routine and shifting priorities where sex is no longer central.[78][79] Many affected women recover sexual function through lifestyle adjustments including regular physical exercise, lubricants, vaginal moisturizers, or hormone therapy. Indirect contributors like vasomotor symptoms, sleep disruption, and mood alterations further compound these effects.[79] Studies indicate arousal difficulties as the most prevalent sexual dysfunction, reported by over 40% in some postmenopausal populations, with painful sex correlating directly to GSM severity.[80] These changes stem from hypoestrogenism's impact on genital blood flow and neural sensitivity, reducing clitoral and vaginal responsiveness, though psychological factors and partner dynamics can modulate expression.[81] Untreated, such effects may lead to avoidance of sexual activity and relational strain.[82]Cognitive, Mood, and Sleep Disturbances
Cognitive disturbances during the menopausal transition often manifest as subjective complaints of brain fog, including difficulties with memory, concentration, and verbal fluency, which correlate with declining estrogen levels that influence hippocampal and prefrontal cortex function.[83] These symptoms are more prevalent in perimenopause than in postmenopause, with estrogen fluctuations disrupting neurotransmitter systems like serotonin and acetylcholine essential for cognition.[84] Empirical studies indicate that while objective cognitive tests show minimal deficits in most women, self-reported impairments affect up to 60% during this period, potentially exacerbated by sleep loss or vasomotor symptoms rather than direct ovarian failure alone.[85] Mood alterations, particularly depressive symptoms, peak during perimenopause due to erratic estrogen levels disrupting monoamine pathways and hypothalamic-pituitary-adrenal axis regulation, with cohort data from over 9,000 women showing elevated depression risk compared to pre- or postmenopause stages.[86] Irritability and anxiety may occur, but systematic reviews of longitudinal studies find inconsistent evidence for heightened anxiety disorders across the transition, attributing variability to psychosocial factors over hormonal causality.02801-5/abstract) No broad increase in psychosis or bipolar disorder is supported by available data, emphasizing that pre-existing vulnerabilities, not menopause per se, drive severe outcomes in susceptible individuals.02801-5/abstract) Sleep disturbances, including insomnia and frequent awakenings, affect 40-60% of women transitioning through menopause, with prevalence rising from 16-42% in premenopause to 39-47% in perimenopause and higher in postmenopause, often independently of hot flashes via estrogen's role in regulating circadian rhythms and melatonin production.[87] Studies link these issues to reduced slow-wave sleep and increased awakenings, where hormonal shifts alter GABAergic inhibition in the brain, compounding fatigue that indirectly worsens cognitive and mood symptoms.[88] Surgical menopause without hormone replacement elevates risk further, with up to 60% reporting disorders, highlighting estrogen's neuroprotective effects on sleep architecture.[89]Other Physical Manifestations
Joint and muscle aches are prevalent during menopause, affecting up to 65% of women globally according to a 2024 meta-analysis of symptom prevalence.[90] These manifestations arise from estrogen's role in maintaining joint lubrication and muscle integrity; its decline leads to inflammation and stiffness, independent of age-related osteoarthritis exacerbation.[91] Symptoms often include diffuse pain in the back, knees, and hands, worsening during perimenopause and persisting into postmenopause without intervention.[1] Skin alterations constitute another common physical change, with estrogen deficiency accelerating collagen loss by approximately 2% annually post-menopause, resulting in dryness, thinning, increased wrinkling, and reduced elasticity.[92] Epidermal thinning reduces barrier function, heightening pruritus and poor wound healing, while dermal changes manifest as sagging and vascular diminishment.[93] These effects are empirically linked to hypoestrogenism rather than chronological aging alone, as evidenced by reversal with estrogen supplementation in controlled studies.[92] Hair thinning and loss affect up to 40% of menopausal women, driven by estrogen-progesterone imbalance favoring androgenic influences, which miniaturize follicles and prolong telogen phases.[92] Scalp density decreases, often diffusely, contrasting with patterned androgenetic alopecia in men.[93] Body composition shifts toward central adiposity, often termed "estrogen belly," occur in over 60% of women, with declining estrogen levels during perimenopause and menopause shifting fat storage from hips and thighs to abdominal visceral and subcutaneous fat. This primarily represents actual body fat accumulation rather than bloating or water retention, though estrogen fluctuations can separately cause temporary bloating and water retention. Average weight gain of 1-2 kg during transition is attributable to metabolic slowdown from ovarian cessation and reduced lean mass.[91] Estrogen loss promotes visceral fat accumulation via impaired insulin sensitivity and altered fat distribution, independent of caloric intake changes.[1][94]Diagnosis
Clinical History and Symptom Evaluation
The diagnosis of menopause is established primarily through clinical evaluation, focusing on patient age, menstrual history, and characteristic symptoms rather than laboratory confirmation in most cases. For women aged 45 years or older, menopause is diagnosed retrospectively after 12 consecutive months of amenorrhea, provided no other pathological or physiological causes (such as pregnancy, thyroid dysfunction, or medication effects) are identified. Perimenopause, the transitional phase preceding menopause, is identified by irregular menstrual cycles accompanied by vasomotor symptoms, typically beginning in the mid-40s and lasting 4 to 8 years on average. Clinicians assess the timing and pattern of menstrual changes, including cycle length variability, flow volume, and the date of the last menstrual period, while inquiring about current or recent use of hormonal contraceptives, which can mask underlying ovarian changes.[95][1][96] Symptom evaluation centers on the presence, severity, frequency, and impact of estrogen deficiency manifestations, which inform both diagnosis and management decisions. Key symptoms include vasomotor disturbances such as hot flushes and night sweats, affecting 75% to 80% of women and often persisting 1 to 6 years; genitourinary issues like vaginal dryness and urinary urgency, occurring in 50% to 75%; and psychological effects including mood instability or sleep disruption, reported by up to 70%. A comprehensive history explores the onset of these symptoms relative to menstrual alterations, their diurnal patterns (e.g., nocturnal sweats exacerbating insomnia), and associated factors such as triggers or lifestyle influences. Validated tools, such as the Modified Greene Climacteric Scale, may quantify symptom burden across psychological, vasomotor, and somatic domains to guide severity assessment and track response to interventions. Differential diagnoses are excluded through targeted questioning on comorbidities, including endocrine disorders (e.g., hyperthyroidism mimicking vasomotor symptoms) or psychiatric conditions, emphasizing empirical correlation over isolated symptom checklists.[1][96][97] In younger women (under 45), or when symptoms are atypical, history alone may prompt further investigation to rule out secondary amenorrhea causes, but routine hormone assays like follicle-stimulating hormone (FSH) are discouraged due to perimenopausal fluctuations rendering them unreliable for confirmatory diagnosis. Instead, evaluation prioritizes causal attribution to ovarian aging, integrating family history of early menopause and ethnic factors that may lower average age of onset. This approach avoids over-reliance on variable biomarkers, favoring observable clinical patterns supported by longitudinal symptom tracking.[95][96][1]Hormonal and Imaging Tests
Diagnosis of menopause in women over 45 years is typically based on clinical history, including the absence of menses for 12 consecutive months accompanied by vasomotor symptoms, without the need for laboratory confirmation in most cases.[98][99] Hormonal testing is not routinely recommended during the menopausal transition due to fluctuating levels that may not accurately reflect ovarian function; guidelines from organizations such as the American College of Obstetricians and Gynecologists (ACOG) and the Endocrine Society advise against it for standard diagnosis.[100][99] Follicle-stimulating hormone (FSH) measurement in serum is the most commonly considered hormonal test, with levels exceeding 30 international units per liter (IU/L), often in conjunction with estradiol below 20-30 pg/mL, providing supportive evidence of ovarian insufficiency in postmenopausal states.[101][27] However, FSH elevations precede overt menopause and can vary widely during perimenopause due to intermittent ovarian activity, rendering single measurements unreliable for confirming the transition; repeat testing or assessment in the early follicular phase may be needed for precision, though evidence shows limited diagnostic utility overall.[97][96] Estradiol assays are similarly interpretive only when low and paired with elevated FSH, as isolated low levels occur in perimenopause without indicating permanent cessation.[101] In younger women under 40 or those with premature ovarian insufficiency (POI), elevated FSH on two occasions more than one month apart, alongside low estradiol, is used to confirm diagnosis, distinguishing it from transient hypothalamic amenorrhea.[27] Other markers like anti-Müllerian hormone (AMH) or inhibin B assess ovarian reserve but lack specificity for menopause and are not standard for routine evaluation.[96] Imaging tests, primarily transvaginal ultrasound, play a limited role in direct menopause diagnosis but are employed to evaluate structural causes of symptoms or rule out pathology such as endometrial hyperplasia in cases of irregular bleeding.[102] Ovarian ultrasound may reveal reduced follicular activity or small, inactive ovaries in postmenopausal women, with antral follicle counts below 5-7 per ovary supporting diminished reserve, though these findings are correlative rather than diagnostic of menopause itself.[103] Endometrial thickness measurement via ultrasound (typically <4-5 mm in asymptomatic postmenopausal women) helps exclude malignancy but does not confirm hormonal status.[102] Advanced imaging like MRI is reserved for equivocal ultrasound results or suspected masses, not for routine menopause assessment, as empirical data indicate low yield in uncomplicated cases.[104] Overall, both hormonal and imaging modalities are adjunctive, with clinical judgment prioritized to avoid over-testing driven by variability in perimenopausal physiology.[97][105]Long-Term Health Implications
Cardiovascular Risks
The transition through menopause is associated with a marked increase in cardiovascular disease (CVD) risk among women, primarily due to the decline in endogenous estrogen levels, which previously exerted protective effects on vascular endothelium, lipid profiles, and inflammation. Prior to menopause, women exhibit lower rates of CVD compared to age-matched men, but postmenopausal women experience a rapid escalation in incidence, with CVD emerging as the leading cause of death. For instance, the Framingham Heart Study reported a 2.6-fold higher incidence of cardiovascular events in postmenopausal women relative to their premenopausal counterparts, independent of age and other risk factors.[106][34] Mechanistically, estrogen deficiency contributes to endothelial dysfunction, adverse lipid changes (elevated low-density lipoprotein cholesterol and reduced high-density lipoprotein cholesterol), increased visceral adiposity, hypertension, and prothrombotic states, all of which accelerate atherosclerosis. These shifts begin during perimenopause, with evidence of rising blood pressure, oxidative stress, and subclinical atherosclerosis even before full estrogen cessation. Systematic reviews confirm that the menopause transition correlates with heightened risks for coronary heart disease, stroke, and heart failure, with postmenopausal prevalence of traditional risk factors like dyslipidemia and metabolic syndrome exceeding premenopausal levels.[107][108][109] Subgroup analyses highlight amplified risks for early or premature menopause: women experiencing natural menopause before age 45 face a 16% higher total CVD risk, while premature menopause (before age 40) elevates it by 36%, based on longitudinal cohort data with extended follow-up. Conversely, later menopause (after age 51) is linked to reduced CVD incidence, with hazard ratios as low as 0.85 relative to average age at menopause. Vasomotor symptoms during the transition, such as hot flashes, independently predict elevated CVD risk in meta-analyses, potentially reflecting underlying autonomic and vascular instability.[110][111][34]| Menopause Timing | Relative CVD Risk Increase | Source |
|---|---|---|
| Premature (<40 years) | 36% | [110] |
| Early (40-44 years) | 16% | [110] |
| Average (50-51 years) | Reference | [111] |
Skeletal and Metabolic Effects
The decline in estrogen levels following menopause accelerates bone resorption, leading to a net loss of bone mineral density (BMD). In the first 5-7 years post-menopause, the rate of bone loss averages 1-5% annually due to estrogen deficiency.[112] This rapid phase of bone turnover increases the risk of osteoporosis, characterized by reduced bone strength and higher fracture susceptibility. Worldwide, approximately 1 in 3 women over age 50 experiences an osteoporosis-related fracture.[113] In the United States, osteoporosis affects about 30% of Caucasian postmenopausal women based on World Health Organization criteria.[114] Factors influencing BMD loss include body weight, with women in higher body weight tertiles exhibiting 35-55% slower bone loss rates during late peri- and postmenopause compared to those in lower tertiles.[115] Estrogen's protective role on bone health is evident, as its reduction not only diminishes BMD but also impairs bone biomechanical integrity.[116] Postmenopausal osteoporosis arises primarily from this hormonal imbalance disrupting remodeling balance, though androgen deficiency contributes in some cases.[117] Menopause also induces metabolic shifts, including adverse changes in body composition such as increased visceral adiposity and fat mass, which elevate cardiovascular disease risk.[118] Visceral fat accumulation during this transition promotes insulin resistance and central obesity, key components of metabolic syndrome.[119] The prevalence of metabolic syndrome rises post-menopause, partly attributable to estrogen loss affecting lipid metabolism and energy homeostasis, leading to abdominal fat redistribution independent of overall weight gain.[120] [121] These metabolic alterations, including heightened insulin resistance, stem from menopause-related increases in intra-abdominal fat, which correlate with dyslipidemia and glucose dysregulation.[122] Cross-sectional evidence links menopausal status to greater abdominal adiposity and insulin resistance, though longitudinal data show mixed results on diabetes prevalence.[123] Overall, the transition exacerbates cardiometabolic risks through fat redistribution favoring visceral depots over subcutaneous sites.[124]Neurological and Cancer Risks
The decline in estrogen levels during menopause is linked to heightened neurological risks, including accelerated cognitive decline and increased incidence of Alzheimer's disease (AD) and dementia. Systematic reviews have identified earlier age at menopause as a contributing factor to AD susceptibility in women, with estrogen depletion exacerbating synaptic dysfunction and amyloid pathology.[125] Women experiencing natural menopause before age 40 face a significantly elevated dementia risk, with pooled analyses of cohort studies showing hazard ratios up to 1.67 compared to later menopause, independent of menopause type.[126] Postmenopausal brain imaging studies reveal structural changes, such as reduced gray matter volume in hippocampus and prefrontal regions, alongside increased beta-amyloid and tau accumulation, supporting estrogen's prior neuroprotective role in mitigating neurodegeneration.[127][128] Overall, women are approximately twice as likely as men to develop AD, with the menopausal transition pinpointed as a critical vulnerability window due to abrupt hormonal shifts.[129] Regarding cancer risks, natural menopause generally confers protection against endometrial cancer by ending unopposed estrogen exposure from ovulatory cycles, reducing incidence compared to premenopausal states.[130] Ovarian cancer risk remains unaffected by the menopausal transition itself but rises with chronological age post-menopause.[131] For breast cancer, the majority of cases (over 75%) occur post-menopause, driven primarily by age and cumulative lifetime estrogen exposure rather than the hypoestrogenic state; late natural menopause (after age 55) elevates risk due to prolonged reproductive years, with meta-analyses estimating 5-10% increased odds per five years of delayed menopause.[132] Conversely, very early natural menopause (before age 40) has been associated in observational data with modestly higher breast and ovarian cancer risks, potentially reflecting shared genetic predispositions like DNA repair deficiencies rather than estrogen loss alone.[133] These patterns underscore that menopause timing modulates cancer susceptibility through duration of endogenous estrogen exposure, with deviations from the typical age of 51 amplifying specific risks.[134]Management Strategies
Hormone Therapy: Evidence-Based Benefits
Menopausal hormone therapy (MHT), consisting of estrogen alone or combined with progestogen, provides substantial relief from vasomotor symptoms (VMS), including hot flashes and night sweats, which affect up to 80% of postmenopausal women. Clinical trials demonstrate reductions in VMS frequency by 75% to 90% and severity by similar margins, outperforming nonhormonal options like antidepressants or gabapentinoids.[135][136] This efficacy holds across delivery routes, with transdermal and oral formulations showing comparable benefits, though individual response varies by baseline symptom intensity and therapy duration.[137] For genitourinary syndrome of menopause (GSM), encompassing vaginal dryness, dyspareunia, and urinary urgency, low-dose topical or systemic estrogen therapies restore vaginal epithelial integrity and moisture, alleviating symptoms in 70% to 90% of users within 12 weeks.[135] Systemic MHT also improves GSM when VMS treatment is indicated, while local therapies minimize systemic exposure for isolated urogenital complaints. Evidence from randomized trials confirms sustained benefits without progression to more severe atrophy when initiated early postmenopause.[136] In skeletal health, MHT prevents postmenopausal bone mineral density (BMD) loss at the hip, spine, and forearm, with meta-analyses of randomized controlled trials showing a 2% to 5% annual preservation compared to placebo. Fracture risk reduction is evident, particularly for hip and vertebral sites, with relative risk decreases of 20% to 40% in women starting therapy near menopause onset. The Women's Health Initiative trial reported a 34% lower hip fracture incidence with estrogen-progestogen versus placebo over 5.2 years.[138][139] Benefits accrue primarily during active treatment, with discontinuation linked to accelerated bone loss approximating natural postmenopausal rates.[140][141] Emerging data indicate MHT may mitigate insulin resistance and prediabetes progression, with a 2024 meta-analysis of 17 trials (n=20,000+) finding significant improvements in HOMA-IR scores for both estrogen-alone and combined regimens, independent of weight changes. Quality-of-life enhancements, including better sleep and reduced VMS-related fatigue, stem from symptom control rather than direct neuroendocrine effects.[142] These benefits are most pronounced when MHT commences within 10 years of menopause or before age 60, aligning with preserved ovarian reserve physiology.[135][143]Hormone Therapy: Risks and Contraindications
Menopausal hormone therapy (MHT), particularly combined estrogen-progestin regimens, has been associated with elevated risks of breast cancer, with meta-analyses indicating a duration-dependent increase; for instance, use beyond five years correlates with relative risks exceeding 1.2 for estrogen-progestin combinations compared to non-users.[144][145] Estrogen-only therapy shows a smaller or negligible increase in some analyses, though long-term use (over 15 years) may raise risk by approximately 30%.[146] These findings stem from large cohort studies and reanalyses of the Women's Health Initiative (WHI), which reported a hazard ratio of 1.24 for invasive breast cancer with combined therapy after 5.6 years of follow-up.[147] Cardiovascular risks vary by age, regimen, and timing; oral estrogen-progestin MHT increases coronary heart disease risk (adjusted hazard ratio around 1.2-1.5 in older women) and ischemic stroke (relative risk 1.23), particularly in those over 60 or more than 10 years post-menopause.[148][37] Transdermal or estrogen-only formulations initiated near menopause onset may confer neutral or reduced risks in younger women (<60 years), with some observational data suggesting lower myocardial infarction and stroke incidence when started in perimenopause.[149] However, the WHI trial demonstrated overall increases in heart disease, stroke, and blood clots with combined therapy in its primary cohort (mean age 63).[147] Venous thromboembolism (VTE) risk rises significantly with oral MHT (relative risk 1.86, 95% CI 1.39-2.50), driven by first-pass liver effects elevating clotting factors, though transdermal routes pose lower absolute risk.[37] Additional harms include gallbladder disease and potential urinary incontinence worsening, while overall mortality shows no significant elevation in systematic reviews.[150][151] Risks are amplified in smokers, obese individuals, or those with preexisting conditions, underscoring individualized assessment over generalized promotion. Absolute contraindications for systemic MHT include known or suspected estrogen-sensitive cancers (e.g., breast or endometrial), active thromboembolic disease or thrombophilias, undiagnosed abnormal vaginal bleeding, and acute severe liver dysfunction.[137][152] Relative contraindications encompass history of stroke or myocardial infarction, uncontrolled hypertension, migraine with aura, and initiation beyond age 60 or 10 years post-menopause, where harm-benefit ratios deteriorate per WHI-derived evidence.[153][136] Guidelines emphasize screening for these factors, as empirical data from randomized trials highlight non-trivial adverse events even in screened populations.[154]Non-Hormonal Medical Options
Non-hormonal pharmacological interventions for vasomotor symptoms (VMS), such as hot flashes and night sweats, include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), gabapentinoids, clonidine, and neurokinin 3 receptor (NK3R) antagonists like fezolinetant.[155] These options provide modest reductions in VMS frequency and severity, typically 30-60% compared to placebo, but generally less effective than hormone therapy.[156] Paroxetine mesylate (Brisdelle), approved by the FDA in 2013 at a low dose of 7.5 mg daily, reduces moderate-to-severe hot flash frequency by a median of 5.9 episodes per day after 12 weeks, with response rates (≥50% reduction) around 40-50% in trials.[157] [158] Other SSRIs/SNRIs, such as venlafaxine (37.5-75 mg daily) or escitalopram, show similar efficacy in reducing VMS by 40-60%, though direct comparisons are limited and side effects like nausea or sexual dysfunction occur in 10-20% of users.[159] [160] Gabapentin, an anticonvulsant, at doses of 900 mg daily (divided) achieves 45-54% reductions in hot flash frequency and composite scores in randomized trials lasting 4-12 weeks, outperforming placebo but with tolerability issues like dizziness in up to 25% of patients.[161] [162] Extended-release formulations maintain efficacy at weeks 4 and 12.[163] Clonidine (0.1 mg patch or oral) and oxybutynin (anticholinergic, 2.5-5 mg) offer smaller benefits, reducing VMS by 20-40%, but are limited by hypotension or dry mouth, respectively, restricting their first-line use.[155] Fezolinetant (45 mg daily), an NK3R antagonist approved by the FDA in 2023, significantly lowers moderate-to-severe VMS frequency by 50-65% over 12 weeks in phase 3 trials, improves sleep disturbances, and demonstrates good tolerability, though one trial showed non-significance versus placebo and endometrial risks warrant monitoring.[164] [165] [166] For genitourinary syndrome of menopause (GSM), including vaginal dryness and dyspareunia, prescription non-hormonal options center on ospemifene (60 mg daily oral selective estrogen receptor modulator), which alleviates painful intercourse in 50-60% of women with moderate-to-severe GSM after 12 weeks, as evidenced by randomized trials.[167] [168] Over-the-counter vaginal moisturizers (e.g., polycarbophil-based) and lubricants provide symptomatic relief for mild cases but lack the targeted efficacy of prescription agents for severe GSM.[168] Herbal supplements commonly marketed for menopausal symptoms, such as evening primrose oil, dong quai, wild yam, ginseng, DHEA, and maca, lack strong evidence of efficacy. In hormone balancing supplements often marketed for menopause or hormonal issues, certain ingredients carry risks and should be avoided or used cautiously, including black cohosh (linked to potential liver toxicity and elevated liver enzymes; lacks strong evidence for effectiveness),[169] phytoestrogens/isoflavones (e.g., from soy; can mimic estrogen and may be unsafe for individuals with a history of estrogen-sensitive cancers),[170] St. John's wort (can cause serious drug interactions with many medications),[171] ginseng (may interfere with cortisol levels and hormonal balance), and excessive doses of certain nutrients like vitamin D or iodine (can disrupt hormonal signaling or thyroid function).[172] These supplements are not well-regulated by the FDA, often lack proven efficacy, and may contain proprietary blends with unclear dosing; consultation with a healthcare provider is recommended before use, especially for those with health conditions or taking medications. St. John's wort may provide some mood benefits but is associated with significant drug interactions. Harvard experts recommend avoiding supplements specifically marketed for menopause due to unproven claims and potential risks.[173] These treatments do not address systemic risks like osteoporosis or cardiovascular changes, necessitating individualized assessment against hormone contraindications.[71] Overall, non-hormonal options suit women with hormone therapy contraindications but require weighing modest benefits against potential adverse effects in clinical decision-making.[174]Lifestyle and Behavioral Interventions
Lifestyle interventions, including regular physical activity, dietary modifications, and behavioral therapies, provide non-pharmacological approaches to alleviate menopausal symptoms such as vasomotor disturbances, mood alterations, and sleep disruptions. Systematic reviews of randomized controlled trials indicate that combined exercise and health education programs reduce perimenopausal symptom severity and improve overall quality of life, with mind-body exercises like yoga showing particular promise for symptom relief.[175] [176] These strategies also support long-term health outcomes, such as preserving bone density and mitigating cardiovascular risks, by addressing causal factors like estrogen decline and metabolic shifts.[177] Exercise InterventionsAerobic and resistance exercises, performed at moderate intensities for at least 150 minutes weekly, correlate with reduced depressive and anxiety symptoms in menopausal women, with meta-analyses reporting significant improvements in psychological well-being.[178] Mind-body practices, including yoga, tai chi, and Pilates, enhance sleep quality, alleviate anxiety, and maintain bone mineral density, as evidenced by pooled data from multiple trials showing moderate effect sizes across these domains.[177] Resistance training specifically diminishes hot flush frequency and severity, though the evidence base exhibits low certainty due to heterogeneity in study designs and participant adherence.[179] Overall, exercise interventions yield functional capacity gains and quality-of-life enhancements, with greater benefits observed in women engaging consistently over 12 weeks or more.[180] Dietary and Weight Management Strategies
Plant-based diets low in refined carbohydrates and fats, supplemented with soy isoflavones, reduce vasomotor symptom frequency by up to 84% and severity in postmenopausal women, per intervention trials tracking daily intake and symptom logs.[181] Adequate intake of calcium (1,200 mg/day) and vitamin D supports skeletal health amid estrogen-related bone loss, while omega-3-rich foods like oily fish may delay menopause onset by modulating hormonal pathways.[182] [183] Anti-inflammatory dietary approaches, akin to the Mediterranean diet, emphasize whole, unprocessed foods such as fruits (e.g., berries), vegetables (e.g., leafy greens, broccoli), whole grains (e.g., oats, quinoa), legumes, nuts, seeds, fatty fish (e.g., salmon for omega-3s), olive oil, and spices like turmeric and ginger, with smaller, frequent meals incorporating gradually increased high-fiber foods and phytoestrogens (e.g., from flaxseeds, soy) to support digestion, hormone balance, weight management, and reduction of bloating and inflammatory pain. Limiting added sugars, processed foods, refined carbohydrates, and high-sodium items further curbs inflammation.[184] For overweight individuals, intentional weight loss of 5-10% body mass through caloric deficit and activity eliminates hot flushes in nearly half of cases, as demonstrated in behavioral programs emphasizing sustainable habits over rapid reduction.[185] [186] These effects stem from reduced adipose tissue-derived estrogen and improved thermoregulation, though long-term adherence remains a limiting factor.[187] Behavioral Therapies
Cognitive behavioral therapy (CBT), delivered in 6-12 sessions focusing on symptom perception and coping skills, decreases hot flash bother by 40-60% and improves insomnia and mood, independent of age or baseline psychological status.[188] [189] Psychosocial interventions targeting anxiety and depression yield robust reductions in non-vasomotor symptoms, with meta-analyses confirming efficacy over waitlist controls.[190] Mindfulness-based stress reduction complements these by lowering perceived symptom intensity through autonomic modulation, though effects on physiological hot flash frequency are inconsistent.[191] For low libido in perimenopausal and postmenopausal women, sex therapy and counseling address psychological and relational factors, improving desire and satisfaction through education, communication techniques, and couples exercises. Vaginal lubricants and moisturizers alleviate dryness to enhance comfort during intercourse, while pelvic floor therapy strengthens muscles to improve sensation and function. Integrating these with lifestyle modifications such as regular exercise, stress reduction, and better sleep hygiene further supports sexual well-being by enhancing mood and vitality.[192][77] Integration of these therapies with lifestyle changes amplifies benefits, particularly for women with comorbid psychological distress.[193]
Controversies and Empirical Critiques
Reassessing Hormone Therapy Guidelines
The Women's Health Initiative (WHI) trials, published in 2002, initially reported increased risks of breast cancer, stroke, and coronary heart disease with combined estrogen-progestin therapy, leading to a sharp decline in hormone therapy (HT) prescriptions and revised guidelines emphasizing caution.[194] Subsequent long-term follow-up analyses of WHI data, extending to 18 years, found no significant increase in all-cause mortality with 5-7 years of HT use and reduced risks of coronary artery calcification and breast cancer after extended observation, particularly challenging the blanket risk perceptions.[195] [196] Reassessments have centered on the "timing hypothesis," which posits that HT confers cardiovascular benefits and lower overall risks when initiated within 10 years of menopause onset or before age 60, due to estrogen's protective effects on vascular endothelium before advanced atherosclerosis develops.[136] Evidence supporting this includes subgroup analyses from WHI showing decreased heart disease and mortality risks in women aged 50-59 (relative risk 0.70 for mortality), contrasted with harms in older cohorts, as well as randomized trials like the ELITE study demonstrating slowed carotid intima-media thickness progression with early oral estradiol but not late initiation.[197] [198] Monkey models further corroborated early intervention's efficacy in halting atherosclerosis progression, aligning with human observational data from meta-regressions linking proximity to menopause with favorable HT outcomes.[199] [200] Updated guidelines reflect these findings, with the North American Menopause Society's 2022 position statement affirming HT as the most effective treatment for vasomotor symptoms and genitourinary syndrome of menopause, with proven fracture prevention and no causal link to dementia, recommending its use for symptomatic women under 60 or within a decade of menopause after individualized risk assessment.[135] The statement notes absolute risks remain low—e.g., one additional breast cancer case per 1,000 women annually with combined HT—outweighed by benefits for severe symptoms, and supports transdermal or micronized progesterone options to minimize venous thromboembolism.[201] [202] Critiques argue current guidelines retain undue caution stemming from WHI's misapplication to younger women, with calls to remove FDA black box warnings added in 2003, as they overemphasize outdated population-level risks and deter appropriate use; for instance, post-2002 HT avoidance correlated with excess mortality in some cohorts, per observational studies.[203] [204] Proponents of further reassessment, including medical societies, highlight that absolute risks for healthy early menopausal women are minimal (e.g., stroke risk increase of 0.3 per 1,000 user-years), urging emphasis on personalized factors like baseline health over generalized fears, while acknowledging persistent contraindications such as active breast cancer or uncontrolled hypertension.[205] [143] This empirical pivot underscores HT's role not as preventive for chronic diseases in all but as targeted symptom relief with net benefits in optimal windows, informed by decades of post-WHI data rather than initial alarmism.[206]Debunking Symptom and Treatment Myths
A prevalent myth posits that hot flashes and night sweats, the hallmark vasomotor symptoms of menopause, afflict all women universally and severely, often portrayed as an inevitable and debilitating phase. In reality, prevalence varies widely, with studies indicating that 50-82% of women experience these symptoms during the menopausal transition, influenced by factors such as genetics, ethnicity, body mass index, and lifestyle, rather than being a uniform outcome of estrogen decline alone.[90] Cross-cultural research further reveals that hot flash reporting is lower in non-Western societies, suggesting sociocultural influences on symptom perception alongside physiological triggers like hypothalamic thermoregulatory dysfunction.[207] This variability underscores that while vasomotor symptoms correlate with fluctuating estradiol levels, they are not experienced identically or intensely by every individual, countering the notion of a monolithic "menopausal syndrome."[208] Another misconception holds that menopausal hormone therapy (MHT) poses unacceptable risks, such as elevated breast cancer or cardiovascular disease incidence, for all users, largely stemming from misapplications of the 2002 Women's Health Initiative (WHI) trial results. The WHI involved women averaging 63 years old—many years post-menopause—using oral conjugated equine estrogens plus medroxyprogesterone acetate, yielding small absolute risks (e.g., 8 additional breast cancer cases per 10,000 women-years) that do not generalize to younger perimenopausal women or transdermal estrogen formulations, which show neutral or protective cardiovascular effects when initiated within 10 years of menopause onset.[209] Reanalyses confirm that for women under 60, MHT reduces coronary heart disease risk by up to 50% in some cohorts and alleviates symptoms without proportional harm, prioritizing symptom relief and osteoporosis prevention over blanket avoidance.[202] This selective interpretation, amplified by media, has led to underutilization, depriving many of evidence-based benefits while ignoring individual risk stratification.[210] Claims that compounded bioidentical hormones offer superior safety over FDA-approved MHT lack rigorous support, often promoted without accounting for inconsistent dosing, purity issues, and potential risks like endometrial hyperplasia from unopposed estrogen. Peer-reviewed evaluations highlight that while "bioidentical" refers to molecular mimicry of endogenous hormones, compounded versions evade standardization, showing no proven efficacy advantage and higher adverse event reports compared to regulated therapies.[211] Similarly, the assertion that phytoestrogens from soy or herbs fully mitigate symptoms as natural alternatives ignores clinical trials demonstrating their modest, inconsistent effects—far inferior to MHT for vasomotor symptom reduction—due to weak estrogenic activity and bioavailability limitations.[212] These alternatives may provide placebo-level relief for mild cases but fail to address underlying hormonal deficits causally linked to symptoms, perpetuating undertreatment under the guise of risk aversion. The belief that all perimenopausal mood changes or cognitive fog stem directly from menopause, warranting pharmacological intervention without discernment, overlooks confounding variables like sleep disruption from vasomotor symptoms or concurrent life stressors. Longitudinal data indicate that while estrogen decline can exacerbate affective symptoms in susceptible women, menopause does not independently cause clinical depression or irreversible cognitive impairment; instead, targeted interventions like MHT or cognitive behavioral therapy address modifiable contributors more effectively than attributing everything to hormonal cessation.[213] This myth fosters over-medicalization of normal aging variances, diverting from empirical assessment of symptom causality. A further myth suggests that menopause can be reversed through medical interventions to restore ovarian function and fertility. Current scientific evidence indicates that menopause reversal is not possible; it represents the permanent cessation of menstrual cycles due to irreversible loss of ovarian function, with no established treatment capable of restoring natural hormone production or fertility in postmenopausal women. Hormone therapy alleviates symptoms but does not reverse the underlying process. Experimental techniques, such as ovarian rejuvenation with platelet-rich plasma (PRP) or stem cells, lack robust peer-reviewed validation and are not endorsed by major medical organizations.Over-Medicalization and Individual Variability
Menopause constitutes a natural physiological process denoting the cessation of ovarian function and reproductive capability, typically occurring around age 51, rather than a disease state necessitating routine medical correction.[1][3] Portraying it primarily as an estrogen deficiency amenable to hormone replacement therapy (HRT) risks over-medicalization, whereby lifestyle factors and adaptive changes are overshadowed by pharmaceutical interventions, potentially fostering dependency and amplifying perceived deficits.00462-8/fulltext)[214] This perspective has drawn critique for conflating transient symptoms with pathology, as evidenced by historical shifts post-Women's Health Initiative (WHI) findings in 2002, which curtailed widespread HRT use after revealing risks like breast cancer and thromboembolism without proportional benefits for all women.[215] Empirical reviews emphasize that menopause aligns with healthy aging for most, advocating narrative reframing to prioritize symptom-specific relief over blanket treatments, thereby curbing iatrogenic harms and stigma.[216][217] Substantial inter-individual variability characterizes menopausal experiences, with over 80% of women reporting symptoms yet marked differences in type, severity, duration, and impact.[1] Vasomotor symptoms, such as hot flashes, exhibit wide heterogeneity—prevalent in 75% of cases but ranging from negligible to debilitating, influenced by genetic polymorphisms, body mass index, smoking, and ethnicity, with durations averaging 7-10 years but extending variably.[91][218] Cluster analyses of symptom logs from large cohorts reveal distinct patterns, capturing 90% of variance in principal components tied to vasomotor, somatic, and psychological domains, underscoring non-uniform trajectories across perimenopause, menopause, and postmenopause.[219] Only 54% of symptomatic women pursue medical input, highlighting self-management efficacy for milder cases and the pitfalls of uniform guidelines that may pathologize normative variation.[220] This variability necessitates tailored strategies over generalized medicalization, as randomized trials demonstrate that lifestyle optimizations—exercise, diet, and cognitive behavioral therapy—alleviate symptoms comparably to HRT for many without associated risks.[217] Causal factors like socioeconomic status and environmental exposures further modulate outcomes, with neighborhood vulnerability linked to earlier onset and intensified severity in cohort studies.[221] Prioritizing empirical assessment of individual burden avoids overtreatment, aligning interventions with verifiable morbidity rather than presumptive deficiency models.[222]Evolutionary and Comparative Biology
Adaptive Theories (Grandmother Hypothesis)
The grandmother hypothesis posits that menopause evolved in humans as an adaptive trait, enabling post-reproductive females to enhance their inclusive fitness by provisioning resources to their adult daughters and grandchildren, thereby increasing offspring survival and maternal fertility rates.[223] This theory suggests that ceasing reproduction around age 50 allows women to redirect energy from gestation and lactation toward foraging and childcare, subsidizing daughters to wean infants earlier and bear subsequent children more frequently.[224] Proposed by anthropologist Kristen Hawkes in the late 1980s and formalized in her 1997 work, the hypothesis contrasts with non-adaptive explanations by emphasizing selection pressures favoring extended longevity without prolonged fertility.[225] Empirical support derives from studies of the Hadza, a Tanzanian hunter-gatherer population, where postmenopausal women collect 50-80% of their caloric intake through labor-intensive tuber digging, contributing substantially to family nutrition without competing for resources via reproduction.[226] Hawkes' longitudinal observations showed that Hadza grandmothers' foraging efforts correlate with improved grandchild growth and survival, as their provisions alleviate maternal workloads, enabling higher birth rates—daughters with living mothers wean at around 2.5 years versus later in their absence.[227] Historical demographic records from 18th- and 19th-century Finland and Canada further substantiate this: grandchildren of present grandmothers exhibited 20-30% higher survival to age 15, with maternal grandmothers exerting stronger effects due to sex-biased parental investment.[228] Mathematical models integrating the grandmother effect with the "mother hypothesis" (where maternal survival benefits offspring) demonstrate that such allomaternal provisioning can evolve menopause-like reproductive cessation, predicting human-specific traits like lifespans extending 20-30 years post-menopause, late maturity, and elevated fertility compared to other primates.[223] Simulations indicate that without grandmothering, optimal female lifespan would align fertility cessation with death around age 50-60, but inclusive fitness gains from post-reproductive aid select for decoupled longevity, as seen in no other great ape species where females remain fertile until near death.[229] Genomic analyses of ancient hominin DNA support this, showing relaxed purifying selection on ovarian aging genes post-menopause, consistent with adaptive postmenopausal lifespan extension in Homo sapiens lineages dating back at least 1-2 million years.[230] While the hypothesis accounts for observed variance in human life histories better than male-focused provisioning models, it requires paternal grandmother effects to be minimal, aligning with data where maternal kin provide disproportionate aid.[231]Non-Adaptive and Mechanistic Explanations
Menopause results from the progressive depletion of the ovarian reserve of primordial follicles, a process that begins in fetal life and accelerates with age. Females are born with approximately 1–2 million primordial follicles, which decline to about 300,000–400,000 by the onset of puberty due to atresia, a form of follicular death independent of ovulation.[232] Each menstrual cycle recruits a cohort of follicles, but only one typically ovulates while the others undergo atresia, leading to an exponential loss that culminates in near-total depletion by around age 50, triggering ovarian failure.[43] This exhaustion disrupts folliculogenesis, reducing production of inhibin B and anti-Müllerian hormone, which in turn fails to suppress rising follicle-stimulating hormone (FSH) levels from the pituitary gland.[233] Consequently, estrogen and progesterone synthesis plummets, marking the perimenopausal transition and eventual postmenopausal state with sustained hypergonadotropic hypogonadism.[2] From an evolutionary standpoint, non-adaptive explanations frame menopause not as a positively selected trait but as a byproduct of competing selective pressures favoring early-life reproduction over extended fertility. One such view posits antagonistic pleiotropy, where genetic variants enhance fecundity in younger females but accelerate ovarian senescence later, as natural selection prioritizes traits boosting fitness before the average age of menopause in ancestral environments.[234] Another perspective highlights a mismatch between somatic longevity and reproductive lifespan: human ovaries exhibit disproportionately rapid aging relative to other tissues, likely because evolutionary pressures did not strongly favor mechanisms to prolong oogenesis beyond the point where post-reproductive survival conferred minimal direct reproductive benefits.[235] Empirical data indicate that the age at menopause has remained stable at approximately 50 years across historical and prehistorical populations, predating modern lifespan extensions, suggesting this reproductive-somatic discord arose in Homo sapiens or earlier hominins rather than as an artifact of contemporary longevity alone.[236] These mechanistic and non-adaptive accounts emphasize causal realism over teleological adaptations, attributing menopause to intrinsic physiological limits rather than derived benefits like kin investment. While adaptive hypotheses invoke post-reproductive roles, non-adaptive models align with observations in comparative biology where menopause is rare and often correlates with species exhibiting extended lifespans without equivalent ovarian durability.[2] Critiques of adaptive theories, including limited empirical support for inter-generational reproductive conflict resolution, further bolster byproduct interpretations, though direct genetic evidence for pleiotropic effects on ovarian aging remains indirect and requires longitudinal genomic studies for validation.[237][234]Observations in Other Species
Menopause, characterized by the permanent cessation of ovulation coupled with an extended post-reproductive lifespan, is observed in humans and a limited number of other species, predominantly toothed whales. In killer whales (Orcinus orca), females typically cease reproduction between ages 30 and 40, while average lifespan reaches 80–90 years, yielding a post-reproductive phase spanning decades.[238] This pattern aligns with demographic data showing no births after approximately 40 years in long-term studies of wild populations.[239] Similarly, short-finned pilot whales (Globicephala macrorhynchus) exhibit fertility ending in the early 30s, with lifespans extending to 60 years or more, confirmed through hormonal assays and reproductive records from stranded and observed individuals.[238] Phylogenetic analyses of 17 toothed whale species indicate that menopause has evolved convergently at least five times within the group, including in beluga whales (Delphinapterus leucas), narwhals (Monodon monoceros), and false killer whales (Pseudorca crassidens).[238] In these taxa, post-reproductive females demonstrate elevated survival rates and contributions to group foraging, without extended reproductive spans relative to non-menopausal counterparts. No equivalent phenomenon is reliably documented in baleen whales or other cetacean lineages. Among primates, wild chimpanzees (Pan troglodytes) show hormonal evidence of menopause, with elevated follicle-stimulating hormone levels and ovarian inactivity emerging around age 50, mirroring human timelines.[240] Captive studies corroborate this, noting follicular depletion near age 50, though post-reproductive survival averages only 3–5 years due to shorter overall lifespans (up to 55–60 years in the wild).[241] This contrasts with the prolonged post-reproductive phase in humans and whales, suggesting limited evolutionary decoupling of reproduction from aging in chimpanzees. Observations in other mammals, such as elephants, lack substantiation for menopause; female Asian and African elephants maintain ovarian cyclicity into their 50s–60s, with documented pregnancies at ages exceeding 60 years, and no distinct fertility termination preceding death.[242] A 2023 analysis redefining menopause solely as ovulation cessation—irrespective of lifespan extension—proposed its prevalence across mammalian orders, including in rodents and bats via reanalyzed necropsy data.[243] However, critics argue this conflates ubiquitous reproductive senescence (fertility declining proximate to mortality) with evolved menopause, which requires substantial post-reproductive longevity for potential adaptive utility, as evidenced by the rarity in natural populations. Empirical validation remains pending for most proposed cases beyond cetaceans and humans.Societal Impacts
Cultural and Cross-Cultural Perspectives
Cultural attitudes toward menopause often frame it as a transition to elder status with increased wisdom and social authority in many non-Western societies, contrasting with more medicalized and symptom-focused views in Western contexts. In collectivistic cultures such as those in Asia, menopause symbolizes elevated prestige and freedom from reproductive burdens, with women reporting it as a period of empowerment rather than decline.[244] [245] For instance, in Islamic, Indian, and various African societies, postmenopausal women gain greater social freedoms, unencumbered by menstrual taboos or fertility expectations, allowing participation in public or ritual roles previously restricted.[246] Symptom experiences also differ cross-culturally, with Japanese women consistently reporting fewer vasomotor symptoms like hot flashes and night sweats compared to Western women, at rates as low as 10-20% versus 70-80% in North American cohorts.[247] [248] This disparity persists among Japanese American women, suggesting influences beyond cultural reporting biases, potentially including dietary factors like high soy isoflavone intake or genetic variations in estrogen metabolism.[247] [249] In contrast, Chinese women more frequently cite fatigue and memory issues, while musculoskeletal complaints like shoulder stiffness predominate in Japan over thermoregulatory symptoms.[250] [251] Anthropological studies highlight that these variations stem from cultural constructions of aging and gender roles rather than universal biological determinism, with symptom attribution shaped by local idioms of distress.[252] [207] In rural Iran, women express more negative attitudes than urban counterparts, linked to socioeconomic stressors and limited access to information, underscoring intra-cultural heterogeneity.[251] Cross-cultural surveys confirm that while hormonal changes are invariant, perceptions of menopause as liberating or debilitating correlate with societal valuation of post-reproductive life stages.[253] [254]Effects on Workforce Participation and Productivity
Menopausal symptoms, particularly vasomotor symptoms such as hot flashes and night sweats, alongside sleep disturbances and cognitive complaints, have been associated with reduced workforce participation and productivity among affected women, primarily through increased absenteeism and presenteeism.[255] [256] A 2023 cross-sectional study of over 1,000 women found that severe menopausal symptoms correlated with higher odds of presenteeism (odds ratio 19.71 for severe total symptom scores), where employees attend work but operate at reduced capacity due to symptom interference.[257] Self-reported data indicate that approximately two-thirds of symptomatic women experience diminished work performance, with 38% noting presenteeism impacts in workplace surveys.[255] [258] Absenteeism rates rise notably during perimenopause and early postmenopause, with women aged 45–55 exhibiting a sickness absence rate of 6.0%, compared to 4.1% for men in the same age group, potentially attributable in part to menopausal symptoms like fatigue and mood alterations.[256] Surveys report that 34% of menopausal women have taken time off work due to symptoms, including 18% absent for more than three days per episode, while around 10% resign and 19% reduce working hours as a result.[259] [260] Earlier menopausal transition has been linked prospectively to lower overall work participation in register-based cohort studies.[261] However, not all research identifies a direct tie to menopausal status itself; a 2018 analysis of midlife women found no significant association between menopause stage and outcomes like absence, performance, or turnover after controlling for other factors, suggesting symptom severity rather than transition per se drives effects.[262] Economic analyses quantify these disruptions, estimating annual U.S. productivity losses from menopausal symptoms at $1.8 billion in forgone work time, escalating to $26.6 billion when including associated medical expenditures, based on self-reported symptom interference in large-scale employer data.[263] Systematic reviews confirm consistent patterns of productivity decrements, with symptomatic women reporting up to 12% lower output and additional sick days compared to asymptomatic peers. These costs vary by occupation, with physically demanding or high-stress roles exacerbating symptom impacts, though supportive work environments—such as flexible scheduling—can mitigate reductions in self-rated productivity.[265] Individual variability remains key, as milder symptoms or effective symptom management enable continued full participation for many women, underscoring that broad workforce effects stem from subsets with severe, unmanaged complaints rather than universal menopause-related impairment.[255]Policy, Stigma, and Biological Realism
In the United States, menopause-related policies have gained traction since 2023, with over 20 bills introduced across at least 13 states by April 2025 to enhance care access, including mandates for insurance coverage of treatments and clinician training.[266] As of July 2025, states such as California and Illinois have enacted laws requiring continuing medical education for providers on menopause management, while others like New York and Pennsylvania consider similar measures for symptom relief coverage.[267] Federally, H.R. 6749 (2023-2024) directs the National Institutes of Health to assess ongoing menopause research, and H.R. 219 (2025) mandates a Government Accountability Office review of care for veterans experiencing menopausal symptoms.[268] [269] Workplace policies, lacking dedicated federal menopause leave, often rely on accommodations under the Americans with Disabilities Act for severe symptoms, with recommendations for flexible hours, temperature controls, and employee resource guides to mitigate impacts on productivity.[270] [271] Social stigma surrounding menopause persists, rooted in cultural associations with aging and diminished femininity, leading to underreporting of symptoms and delayed care-seeking. Empirical data indicate that 37.4% of women experience shame tied to menopausal symptoms, correlating with limited knowledge and negative attitudes that leave many unprepared for physiological shifts.[272] [273] This silence exacerbates health risks, as stigma discourages discussions with healthcare providers or employers, with studies showing marginalized groups facing compounded barriers due to knowledge gaps and supernatural attributions in some contexts.[274] [275] Policy responses aim to counter this by promoting awareness, yet mainstream narratives from academia and media—often critiqued for overemphasizing pathology—may inadvertently reinforce stigma by framing menopause as a deficit rather than a normative transition.[276] Biologically, menopause represents the irreversible cessation of ovarian function, defined by 12 consecutive months without menses due to follicular depletion and low estrogen levels, marking the end of natural fertility rather than a pathological state.[3] [2] This process aligns with reproductive aging, where interventions like hormone therapy address symptoms but do not alter the underlying endpoint, underscoring variability in experiences—many women report minimal disruption without medicalization.[277] Realism demands recognizing menopause's causality in heightened risks for conditions like osteoporosis and cardiovascular disease via estrogen decline, yet evidence cautions against universal treatment, as individual factors such as age at onset and genetics dictate outcomes more than blanket policies.[278] [279] Effective stigma reduction and policy thus hinge on this foundation: affirming menopause as an adaptive biological phase in human females, distinct from disease, to prioritize evidence-based support over ideologically driven over-intervention.References
- https://www.[researchgate](/page/ResearchGate).net/publication/366253093_Work_Productivity_Loss_Among_Women_With_Menopausal_Symptoms_A_Systematic_Literature_Review

