Recent from talks
Nothing was collected or created yet.
Serotonin–norepinephrine reuptake inhibitor
View on Wikipedia
| Serotonin–norepinephrine reuptake inhibitor | |
|---|---|
| Drug class | |
 Duloxetine, an example of an SNRI. | |
| Class identifiers | |
| Synonyms | Selective Serotonin–noradrenaline reuptake inhibitor; SNaRI |
| Use | Depression; Anxiety; Pain; Obesity; Menopausal symptoms |
| Biological target | Serotonin transporter; Norepinephrine transporter |
| External links | |
| MeSH | D000068760 |
| Legal status | |
| In Wikidata | |
Serotonin–norepinephrine reuptake inhibitors (SNRIs) are a class of antidepressant medications used to treat major depressive disorder (MDD), anxiety disorders, social phobia, chronic neuropathic pain, fibromyalgia syndrome (FMS), and menopausal symptoms. Off-label uses include treatments for attention-deficit hyperactivity disorder (ADHD), and obsessive–compulsive disorder (OCD).[1] SNRIs are monoamine reuptake inhibitors; specifically, they inhibit the reuptake of serotonin and norepinephrine. These neurotransmitters are thought to play an important role in mood regulation. SNRIs can be contrasted with the selective serotonin reuptake inhibitors (SSRIs) and norepinephrine reuptake inhibitors (NRIs), which act upon single neurotransmitters.[2]
The human serotonin transporter (SERT) and noradrenaline transporter (NAT) are membrane transport proteins that are responsible for the reuptake of serotonin and noradrenaline from the synaptic cleft back into the presynaptic nerve terminal. Dual inhibition of serotonin and noradrenaline reuptake can offer advantages over other antidepressant drugs by treating a wider range of symptoms.[3] They can be especially useful in concomitant chronic or neuropathic pain.[4]
SNRIs, along with SSRIs and NRIs, are second-generation antidepressants. Since their introduction in the late 1980s, second-generation antidepressants have largely replaced first-generation antidepressants, such as tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs), as the drugs of choice for the treatment of MDD due to their improved tolerability and safety profile.[5]
Medications
[edit]
There are eight FDA approved SNRIs in the United States, with venlafaxine being the first drug to be developed in 1993 and levomilnacipran being the latest drug to be developed in 2013. The drugs vary by their other medical uses, chemical structure, adverse effects, and efficacy.[6]
| Medication | Brand name | FDA Indications | Approval Year | Chemical structure | Notes |
|---|---|---|---|---|---|
| Desvenlafaxine[7] | Pristiq
Khedezla (ER) |
|
2007 |  |
The active metabolite of venlafaxine. It is believed to work in a similar manner, though some evidence suggests lower response rates compared to venlafaxine and duloxetine. It was introduced by Wyeth in May 2008 and was then the third approved SNRI.[8] |
| Duloxetine[9] | Cymbalta
Irenka |
|
2004 |  |
Approved for the treatment of depression and neuropathic pain in August 2004. Duloxetine is contraindicated in patients with heavy alcohol use or chronic liver disease, as duloxetine can increase the levels of certain liver enzymes that can lead to acute hepatitis or other diseases in certain at risk patients. The risk of liver damage appears to be only for patients already at risk, unlike the antidepressant nefazodone, which, though rare, can spontaneously cause liver failure in healthy patients.[13] Duloxetine is also approved for major depressive disorder (MDD), generalized anxiety disorder (GAD), diabetic neuropathy, chronic musculoskeletal pain, including chronic osteoarthritis pain and chronic low back pain.[11] Duloxetine also undergoes hepatic metabolism and has been shown to cause inhibition of the hepatic cytochrome P450 enzyme CYP 2D6.[14] Caution should be taken when taking Duloxetine with other medications that are metabolized by CYP 2D6 as this may precipitate a potential drug-drug interaction.[14] |
| Levomilnacipran | Fetzima |
|
2013 | 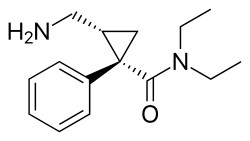 |
The levorotating isomer of milnacipran. Under development for the treatment of depression in the United States and Canada, it was approved by the FDA for treatment of MDD in July 2013. |
| Milnacipran | Ixel Savella Impulsor |
|
1996 |  |
Shown to be significantly effective in the treatment of depression and fibromyalgia.[15] The Food and Drug Administration (FDA) approved milnacipran for treatment of fibromyalgia in the United States in January 2009, however it is not approved for depression in that country.[citation needed] Milnacipran has been commercially available in Europe and Asia for several years.[citation needed] It was first introduced in France in 1996.[citation needed] |
| Sibutramine | Meridia | 1997 |  |
An SNRI, which, instead of being developed for the treatment of depression, was widely marketed as an appetite suppressant for weight loss purposes. Sibutramine was the first drug for the treatment of obesity to be approved in 30 years.[17] It has been associated with increased cardiovascular events and strokes and has been withdrawn from the market in several countries and regions including the United States in 2010.[18] | |
| Tramadol | Ultram |
|
1977 |  |
A dual weak opioid and SNRI. It was approved by the FDA in 1995, though it has been marketed in Germany since 1977. The drug is used to treat acute and chronic pain. It has shown effectiveness in the treatment of fibromyalgia, though it is not specifically approved for this purpose. The drug is also under investigation as an antidepressant and for the treatment of neuropathic pain. It is related in chemical structure to venlafaxine. Due to being an opioid, there is risk of abuse and addiction, but it does have less abuse potential, respiratory depression, and constipation compared to other opioids (hydrocodone, oxycodone, etc.).[19] |
| Venlafaxine | Effexor | 1994 |  |
The first and most commonly used SNRI. It was introduced by Wyeth in 1994. The reuptake effects of venlafaxine are dose-dependent. At low doses (<150 mg/day), it acts only on serotonergic transmission. At moderate doses (>150 mg/day), it acts on serotonergic and noradrenergic systems, whereas at high doses (>300 mg/day), it also affects dopaminergic neurotransmission.[22] At small doses, venlafaxine has also been shown to be effective in treating vasomotor symptoms (hot flashes and night sweats) of menopause.[21] |
History
[edit]In 1952, iproniazid, an antimycobacterial agent, was discovered to have psychoactive properties while researched as a possible treatment for tuberculosis. Researchers noted that patients given iproniazid became cheerful, more optimistic, and more physically active. Soon after its development, iproniazid and related substances were shown to slow enzymatic breakdown of serotonin, dopamine, and norepinephrine via inhibition of the enzyme monoamine oxidase. For this reason, this class of drugs became known as monoamine oxidase inhibitors, or MAOIs. During this time development of distinctively different antidepressant agents was also researched. Imipramine became the first clinically useful tricyclic antidepressant (TCA). Imipramine was found to affect numerous neurotransmitter systems and to block the reuptake of norepinephrine and serotonin from the synapse, therefore increasing the levels of these neurotransmitters. Use of MAOIs and TCAs gave major advances in treatment of depression but their use was limited by unpleasant side effects and significant safety and toxicity issues.[23]
Throughout the 1960s and 1970s, the catecholamine hypothesis of emotion and its relation to depression was of wide interest and that the decreased levels of certain neurotransmitters, such as norepinephrine, serotonin, and dopamine might play a role in the pathogenesis of depression. This led to the development of fluoxetine, the first SSRI. The improved safety and tolerability profile of the SSRIs in patients with MDD, compared with TCAs and MAOIs, represented yet another important advance in the treatment of depression.[23]
Since the late 1980s, SSRIs have dominated the antidepressant drug market. Today, there is increased interest in antidepressant drugs with broader mechanisms of action that may offer improvements in efficacy and tolerability. In 1993, a new drug was introduced to the US market called venlafaxine, a serotonin–norepinephrine reuptake inhibitor.[20] Venlafaxine was the first compound described in a new class of antidepressant substances called phenylethylamines. These substances are unrelated to TCA and other SSRIs. Venlafaxine blocks the neuronal reuptake of serotonin, noradrenaline and, to a lesser extent, dopamine in the central nervous system. In contrast with several other antidepressant drugs, venlafaxine can induce a rapid onset of action mainly due to a subsequent norepinephrine reuptake inhibition.[24] See timeline in figure 1.

Mechanism of action
[edit]Monoamines are connected to the pathophysiology of depression. Symptoms may occur because concentrations of neurotransmitters, such as norepinephrine and serotonin, are insufficient, leading to downstream changes.[10][25] Medications for depression affect the transmission of serotonin, norepinephrine, and dopamine.[10] Older and less selective antidepressants like TCAs and MAOIs inhibit the reuptake or metabolism of norepinephrine and serotonin in the brain, which results in higher concentrations of neurotransmitters.[25] Antidepressants that have dual mechanisms of action inhibit the reuptake of both serotonin and norepinephrine and, in some cases, inhibit with weak effect the reuptake of dopamine.[10] Antidepressants affect variable neuronal receptors such as muscarinic cholinergic, α1- and α2-adrenergic, H1-histaminergic, and sodium channels in the cardiac muscle, leading to decreased cardiac conduction and cardiotoxicity associated particularly with TCAs, and to a lesser extent with SSRIs.[26] Selectivity of antidepressant agents are based on the neurotransmitters that are thought to influence symptoms of depression.[27] Drugs that selectively block the reuptake of serotonin and norepinephrine effectively treat depression and are better tolerated than TCAs. TCAs have comprehensive effects on various neurotransmitters receptors, which leads to lack of tolerability and increased risk of toxicity.[2]
Tricyclic antidepressants
[edit]
TCAs were the first medications that had dual mechanism of action. The mechanism of action of tricyclic secondary amine antidepressants is only partly understood. TCAs have dual inhibition effects on norepinephrine reuptake transporters and serotonin reuptake transporters. Increased norepinephrine and serotonin concentrations are obtained by inhibiting both of these transporter proteins. TCAs have substantially more affinity for norepinephrine reuptake proteins than the SSRIs. This is because of a formation of secondary amine TCA metabolites.[28][29]
In addition, the TCAs interact with adrenergic receptors. This interaction seems to be critical for increased availability of norepinephrine in or near the synaptic clefts. Actions of imipramine-like tricyclic antidepressants have complex, secondary adaptions to their initial and sustained actions as inhibitors of norepinephrine transport and variable blockade of serotonin transport.
Norepinephrine interacts with postsynaptic α and β adrenergic receptor subtypes and presynaptic α2 autoreceptors. The α2 receptors include presynaptic autoreceptors which limit the neurophysiological activity of noradrenergic neurons in the central nervous system. Formation of norepinephrine is reduced by autoreceptors through the rate-limiting enzyme tyrosine hydroxylase, an effect mediated by decreased cyclic AMP-mediated phosphorylation-activation of the enzyme.[29] α2 receptors also cause decreased intracellular cyclic AMP expression which results in smooth muscle relaxation or decreased secretion.[30]
TCAs activate a negative feedback mechanism through their effects on presynaptic receptors. One probable explanation for the effects on decreased neurotransmitter release is that, as the receptors activate, inhibition of neurotransmitter release occurs (including suppression of voltage-gated Ca2+ currents and activation of G protein-coupled receptor-operated K+ currents). Repeated exposure of agents with this type of mechanism leads to inhibition of neurotransmitter release, but repeated administration of TCAs finally leads to decreased responses by α2 receptors. The desensitization of these responses may be due to increased exposure to endogenous norepinephrine or from the prolonged occupation of the norepinephrine transport mechanisms (via an allosteric effect). The adaptation allows the presynaptic synthesis and secretion of norepinephrine to return to, or even exceed, normal levels of norepinephrine in the synaptic clefts. Overall, inhibition of norepinephrine reuptake induced by TCAs leads to decreased rates of neuron firing (mediated through α2 autoreceptors), metabolic activity, and release of neurotransmitters.[29]
TCAs do not block dopamine transport directly but might facilitate dopaminergic effects indirectly by inhibiting dopamine transport into noradrenergic terminals of the cerebral cortex.[29] Because they affect so many different receptors, TCAs have adverse effects, poor tolerability, and an increased risk of toxicity.[2]
Selective serotonin reuptake inhibitors
[edit]Selective serotonin reuptake inhibitors (SSRIs) selectively inhibit the reuptake of serotonin and are a widely used group of antidepressants.[31] With increased receptor selectivity compared to TCAs, undesired effects such as poor tolerability are avoided.[29] Serotonin is synthesized from an amino acid called L-tryptophan. Active transport system regulates the uptake of tryptophan across the blood–brain barrier. Serotonergic pathways are classified into two main ways in the brain: the ascending projections from the medial and dorsal raphe and the descending projections from the caudal raphe into the spinal cord.
Selective norepinephrine reuptake inhibitors
[edit]Noradrenergic neurons are located in two major regions in the brain, the locus coeruleus and lateral tegmental. With administration of SNRIs, neuronal activity in the locus coeruleus is induced because of increased concentration of norepinephrine in the synaptic cleft. This results in activation of α2 adrenergic receptors,[25] as discussed previously.
Assays have shown that SNRIs have insignificant penchant for mACh, α1 and α2 adrenergic, or H1 receptors.[27]
Dual serotonin and norepinephrine reuptake inhibitors
[edit]Agents with dual serotonin and norepinephrine reuptake inhibition (SNRIs) are sometimes called non-tricyclic serotonin and norepinephrine reuptake inhibitors. Clinical studies suggest that compounds that increase the concentration in the synaptic cleft of both norepinephrine and serotonin are more successful than single acting agents in the treatment of depression, but the data is not conclusive whether SNRIs are a more effective treatment option over SSRIs for depression.[32][33][34]
The non-tricyclic SNRIs have several important differences that are based on pharmacokinetics, metabolism to active metabolites, inhibition of CYP isoforms, effect of drug-drug interactions, and the half-life of the nontricyclic SNRIs.[28][35]
Combination of mechanisms of action in a single active agent is an important development in psychopharmacology.[35]
Structure activity relationship
[edit]Aryloxypropanamine scaffold
[edit]Several reuptake inhibitors contain an aryloxypropanamine scaffold. This structural motif has potential for high affinity binding to biogenic amine transports.[35] Drugs containing an aryloxypropanamine scaffold have selectivity profile for norepinephrine and serotonin transporters that depends on the substitution pattern of the aryloxy ring. Selective NRIs contain a substituent in 2' position of the aryloxy ring but SSRIs contain a substituent in 4' position of the aryloxy ring. Atomoxetine, nisoxetine and reboxetine all have a substitution group in the 2' position and are selective NRIs while compounds that have a substitution group in the 4' position (like fluoxetine and paroxetine) are SSRIs. Duloxetine contains a phenyl group fused at the 2' and 3' positions, therefore it has dual selective norepinephrine and serotonin reuptake inhibitory effects and has similar potencies for both transporters.[36] The nature of the aromatic substituent also has a significant influence on the activity and selectivity of the compounds as inhibitors of the serotonin or the norepinephrine transporters.[35]

Cycloalkanol ethylamine scaffold
[edit]Venlafaxine and desvenlafaxine contain a cycloalkanol ethylamine scaffold. Increasing the electron-withdrawing nature of the aromatic ring provides a more potent inhibitory effect of norepinephrine uptake and improves the selectivity for norepinephrine over the serotonin transporter.[36] Effects of chloro, methoxy and trifluoromethyl substituents in the aromatic ring of cycloalkanol ethylamine scaffold were tested. The results showed that the strongest electron-withdrawing m-trifluoromethyl analogue exhibited the most potent inhibitory effect of norepinephrine and the most selectivity over serotonin uptake.[36] WY-46824, a piperazine-containing derivative, has shown norepinephrine and dopamine reuptake inhibition. Further synthesis and testing identified WAY-256805, a potent norepinephrine reuptake inhibitor that exhibited excellent selectivity and was efficacious in animal models of depression, pain, and thermoregulatory dysfunction.[37]

Milnacipran
[edit]
Milnacipran is structurally different from other SNRIs.[28] The structure activity relationship of milnacipran derivatives at the transporter level is still largely unclear and is based on in vivo efficacy that was reported in 1987. N-methylation of milnacipran in substituent group R4 and R5 reduces the norepinephrine and serotonin activity.[38] Researches on different secondary amides in substitution groups R6 and R7 showed that π electrons play an important role in the interaction between transporters and ligands. A phenyl group in substituent R6 showed effect on norepinephrine transporters. Substituent groups in R6 and R7 with allylic double bond showed significant improved effect on both norepinephrine and serotonin transporters.[38] Studies show that introducing a 2-methyl group in substituent R3, the potency at norepinephrine and serotonin transporters are almost abolished. Methyl groups in substituent groups R1 and R2 also abolish the potency at norepinephrine and serotonin transporters. Researchers found that replacing one of the ethyl groups of milnacipran with an allyl moiety increases the norepinephrine potency.[39] The pharmacophore of milnacipran derivatives is still largely unclear.[38]
The conformation of milnacipran is an important part of its pharmacophore. Changing its stereochemistry affects the norepinephrine and serotonin concentration. Milnacipran is marketed as a racemic mixture. Effects of milnacipran reside in the (1S,2R)-isomer and substitution of the phenyl group in the (1S,2R)-isomer has negative impact on norepinephrine concentration.[39] Milnacipran has low molecular weight and low lipophilicity. Because of these properties, milnacipran exhibits almost ideal pharmacokinetics in humans such as high bioavailability, low inter-subject variability, limited liver enzyme interaction, moderate tissue distribution and a reasonably long elimination half-life. Milnacipran's lack of drug-drug interactions via cytochrome P450 enzymes is thought to be an attractive feature because many of the central nervous system drugs are highly lipophilic and are mainly eliminated by liver enzymes.[39]
Future development of structure activity relationship
[edit]The application of an aryloxypropanamine scaffold has generated a number of potent MAOIs.[40] Before the development of duloxetine, the exploration of aryloxypropanamine structure activity relationships resulted in the identification of fluoxetine and atomoxetine. The same motif can be found in reboxetine where it is constrained in a morpholine ring system. Some studies have been made where the oxygen in reboxetine is replaced by sulfur to give arylthiomethyl morpholine. Some of the arylthiomethyl morpholine derivatives maintain potent levels of serotonin and norepinephrine reuptake inhibition. Dual serotonin and norepinephrine reuptake inhibition resides in different enantiomers for arylthiomethyl morpholine scaffold.[41] Possible drug candidates with dual serotonin and norepinephrine reuptake inhibitory activity have also been derived from piperazine, 3-amino-pyrrolidine and benzylamine templates.[42]
Clinical trials
[edit]Depression
[edit]Several studies have shown that antidepressant drugs which have combined serotonergic and noradrenergic activity are generally more effective than SSRIs, which act upon serotonin reuptake by itself. Serotonergic-noradrenergic antidepressant drugs may have a modest efficacy advantage compared to SSRIs in treating major depressive disorder (MDD),[43] but are slightly less well tolerated.[44] Further research is needed to examine the possible differences of efficacy in specific MDD sub-populations or for specific MDD symptoms, between these classes of antidepressant drugs.
Analgesic
[edit]Data from clinical trials have indicated that SNRIs might have pain relieving properties. Although the perception and transmission of pain stimuli in the central nervous system have not been fully elucidated, extensive data support a role for serotonin and norepinephrine in the modulation of pain. Findings from clinical trials in humans have shown these antidepressants can help to reduce pain and functional impairment in central and neuropathic pain conditions. This property of SNRIs might be used to reduce doses of other pain relieving medication and lower the frequency of safety, limited efficacy and tolerability issues.[45] Clinical research data have shown in patients with GAD that the SNRI duloxetine is significantly more effective than placebo in reducing pain-related symptoms of GAD, after short-term and long-term treatment. However, findings suggested that such symptoms of physical pain reoccur in relapse situations, which indicates a need for ongoing treatment in patients with GAD and concurrent painful physical symptoms.[46]
Indications
[edit]SNRIs have been tested for treatment of the following conditions:
Pharmacology
[edit]Route of administration
[edit]
SNRIs are delivered orally, usually in the form of capsules or tablets. It is recommended to take SNRIs in the morning with breakfast, which does not affect drug levels, but may help with certain side effects.[48] Norepinephrine has activating effects in the body and therefore can cause insomnia in some patients if taken at bedtime.[49] SNRIs can also cause nausea, which is usually mild and goes away within a few weeks of treatment, but taking the medication with food can help alleviate this.[50]
Mode of action
[edit]The condition for which SNRIs are mostly indicated, major depressive disorder, was thought to be mainly caused by decreased levels of serotonin and norepinephrine in the synaptic cleft, causing erratic signaling. This theory, however, has been refuted.[51] Based on the monoamine hypothesis of depression, which asserts that decreased concentrations of monoamine neurotransmitters leads to depressive symptoms, the following relations were determined: "Norepinephrine may be related to alertness and energy as well as anxiety, attention, and interest in life; [lack of] serotonin to anxiety, obsessions, and compulsions; and dopamine to attention, motivation, pleasure, and reward, as well as interest in life."[52] SNRIs work by inhibiting the reuptake of the neurotransmitters serotonin and norepinephrine. This results in increased extracellular concentrations of serotonin and norepinephrine and, consequently, an increase in neurotransmission. Most SNRIs including venlafaxine, desvenlafaxine, and duloxetine, are several fold more selective for serotonin over norepinephrine, while milnacipran is three times more selective for norepinephrine than serotonin. Elevation of norepinephrine levels is thought to be necessary for an antidepressant to be effective against neuropathic pain, a property shared with the older tricyclic antidepressants (TCAs), but not with the SSRIs.[53]
Recent studies have shown that depression may be linked to increased inflammatory response,[54] thus attempts at finding an additional mechanism for SNRIs have been made. Studies have shown that SNRIs as well as SSRIs have significant anti-inflammatory action on microglia[55] in addition to their effect on serotonin and norepinephrine levels. As such, it is possible that an additional mechanism of these drugs that acts in combination with the previously understood mechanism exist. The implication behind these findings suggests use of SNRIs as potential anti-inflammatories following brain injury or any other disease where swelling of the brain is an issue. However, regardless of the mechanism, the efficacy of these drugs in treating the diseases for which they have been indicated has been proven, both clinically and in practice.[improper synthesis?]
Pharmacodynamics
[edit]Most SNRIs function alongside primary metabolites and secondary metabolites in order to inhibit reuptake of serotonin, norepinepherine, and marginal amounts of dopamine. For example, venlafaxine works alongside its primary metabolite O-desmethylvenlafaxine to strongly inhibit serotonin and norepinephrine reuptake in the brain. The evidence also suggests that dopamine and norepinephrine behave in a co-transportational manner, due to the inactivation of dopamine by norepinephrine reuptake in the frontal cortex, an area of the brain largely lacking in dopamine transporters. This effect of SNRIs results in increased dopamine neurotransmission, in addition to the increases in serotonin and norepinephrine activity.[56] Furthermore, because SNRIs are extremely selective, they have no measurable effects on other, unintended receptors, in contrast to monoamine oxidase inhibition.[57] Pharmaceutical tests have determined that use of both SNRIs or SSRIs can generate significant anti-inflammatory action on microglia, as well.[55][16][58][59][11][60]
Activity profiles
[edit]| Compound | SERT | NET | ~Ratio (5-HT : NE) | ||
|---|---|---|---|---|---|
| Ki | IC50 | Ki | IC50 | ||
| Venlafaxine | 7.8 | 145 | 1920 | 1420 | ~30:1 |
| Desvenlafaxine | 40.2 | 47.3 | 558.4 | 531.3 | 11.2:1 |
| Duloxetine | 0.07 | 3.7 | 1.17 | 20 | 5.4:1 |
| Atomoxetine | 87[62] | 5.4[62] | 0.06:1 (= 1:16) | ||
| Milnacipran | 8.44 | 151 | 22 | 68 | 2:1[64] |
| Levomilnacipran | 11.2 | 19.0 | 92.2 | 10.5 | 0.55:1 (= 1:1.8) |
| All of the Ki and IC50 values are nM. The 5-HT/NE ratio is based on IC50 values for the SERT and NET.[61] | |||||
Pharmacokinetics
[edit]The half-life of venlafaxine is about 5 hours, and with once-daily dosing, steady-state concentration is achieved after about 3 days, though its active metabolite desvenlafaxine lasts longer.[59] The half-life of desvenlafaxine is about 11 hours, and steady-state concentrations are achieved after 4 to 5 days.[58] The half-life of duloxetine is about 12 hours (range: 8–17 hours), and steady-state is achieved after about 3 days.[11] Milnacipran has a half-life of about 6 to 8 hours, and steady-state levels are reached within 36 to 48 hours.[60]
Contraindications
[edit]SNRIs are contraindicated in patients taking MAOIs within the last two weeks due to the increased risk of serotonin syndrome, which can be life-threatening.[65] Other drugs and substances that should be avoided due to increased risk of serotonin syndrome when combined with an SNRI include: other anti-depressants, anti-convulsants, analgesics, antiemetic agents, anti-migraine medications, methylene blue, linezolid, Lithium, St. John's wort, ecstasy, and LSD.[65] Signs and symptoms of serotonin syndrome include: hyperthermia, rigidity, myoclonus, autonomic instability with fluctuating vital signs, and mental status changes that include extreme agitation progressing to delirium and coma.[11]
Due to the effects of increased norepinephrine levels and, therefore, higher noradrenergic activity, pre-existing hypertension should be controlled before treatment with SNRIs and blood pressure periodically monitored throughout treatment.[66] Duloxetine has also been associated with cases of liver failure and should not be prescribed to patients with chronic alcohol use or liver disease. Studies have found that Duloxetine can increase liver function tests three times above their upper normal limit.[67] Patients with coronary artery disease should caution the use of SNRIs.[68] Furthermore, due to some SNRIs' actions on obesity, patients with major eating disorders such as anorexia nervosa or bulimia should not be prescribed SNRIs.[16] Duloxetine and milnacipran are also contraindicated in patients with uncontrolled narrow-angle glaucoma, as they have been shown to increase incidence of mydriasis.[11][60]
SNRIs should not be used to treat depressive episodes in Bipolar disorder I and should only be used to treat depression in Bipolar disorder II with caution and accompanied by mood stabilizers to avoid hypomania.[69]
Side effects
[edit]Since SNRIs and SSRIs act in similar ways to elevate serotonin levels, they share many side effects, though to varying degrees. Some common side effects include nausea, dry mouth, dizziness, sweating, increased blood pressure, loss of appetite, headache, increase in suicidal thoughts, and sexual dysfunction.[70] Elevation of norepinephrine levels can sometimes cause anxiety, mildly elevated pulse, and elevated blood pressure. However, norepinephrine-selective antidepressants, such as reboxetine and desipramine, have successfully treated anxiety disorders.[71] People at risk for hypertension and heart disease should monitor their blood pressure.[16][58][59][11][60]
Sexual Dysfunction
[edit]SNRIs, similarly to SSRIs, can cause several types of sexual dysfunction, such as erectile dysfunction, decreased libido, sexual anhedonia, and anorgasmia.[11][59][72] The two common sexual side effects are diminished interest in sex (libido) and difficulty reaching climax (anorgasmia), which are usually somewhat milder with SNRIs compared to SSRIs.[73] To manage sexual dysfunction, studies have shown that switching to or augmenting with bupropion or adding a PDE5 Inhibitor have decreased symptoms of sexual dysfunction.[74] Studies have shown that PDE5 Inhibitors, such as sildenafil (Viagra), tadalafil (Cialis), vardenafil (Levitra), and avanafil (Stendra), have sometimes been helpful to decrease the sexual dysfunction, including erectile dysfunction, although they have been shown to be more effective in men than women.[74]
Serotonin Syndrome
[edit]A serious, but rare, side effect of SNRIs is serotonin syndrome, which is caused by an excess of serotonin in the body. Serotonin syndrome can be caused by taking multiple serotonergic drugs, such as SSRIs or SNRIs. Other drugs that contribute to serotonin syndrome include MAO inhibitors, linezolid, tedizolid, methylene blue, procarbazine, amphetamines, clomipramine, and more.[75] Early symptoms of serotonin syndrome may include nausea, vomiting, diarrhea, sweating, agitation, confusion, muscle rigidity, dilated pupils, hyperthermia, rigidity, and goose bumps. More severe symptoms include fever, seizures, irregular heartbeat, delirium, and coma.[76][77][11] If signs or symptoms arise, discontinue treatment with serotonergic agents immediately.[76] It is recommended to washout 4 to 5 half-lives of the serotonergic agent before using an MAO inhibitor.[78]
Bleeding
[edit]Some studies suggest there are risks of upper gastrointestinal bleeding, especially venlafaxine, due to impairment of platelet aggregation and depletion of platelet serotonin levels.[79][80] Similarly to SSRIs, SNRIs may interact with anticoagulants, like warfarin. There is more evidence of SSRIs having higher risk of bleeding than SNRIs.[79] Studies have suggested caution when using SNRIs or SSRIs with high doses of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen due to an increased risk of upper GI bleeding.[34]
Visual problems
[edit]
Similarly to other antidepressants, SNRI medications have been found to cause visual snow syndrome, a condition characterized by visual static, palinopsia (negative after image), nyctalopia (poor vision at night), and photophobia (brighter presentation of lights or highlighted colors). Evidence shows that 8.9% of those taking SNRIs experienced visual snow, 10.5% experienced palinopsia, 15.3% experienced photophobia, and 17.7% experienced nyctolopia as the result of SNRI prescription intake. Amitriptyline, and citalopram have also been reported to worsen or cause symptoms of VSS.[81]
Precautions
[edit]Starting an SNRI regimen
[edit]Due to the extreme changes in noradrenergic activity produced from norepinephrine and serotonin reuptake inhibition, patients that are just starting an SNRI regimen are usually given lower doses than their expected final dosing to allow the body to acclimate to the drug's effects. As the patient continues along at low doses without any side-effects, the dose is incrementally increased until the patient sees improvement in symptoms without detrimental side-effects.[82]
Discontinuation syndrome
[edit]As with SSRIs, the abrupt discontinuation of an SNRI usually leads to withdrawal, or "discontinuation syndrome", which could include states of anxiety and other symptoms. Therefore, it is recommended that users seeking to discontinue an SNRI slowly taper the dose under the supervision of a professional. Discontinuation syndrome has been reported to be markedly worse for venlafaxine when compared to other SNRIs. As such, as tramadol is related to venlafaxine, the same conditions apply.[83] This is likely due to venlafaxine's relatively short half-life and therefore rapid clearance upon discontinuation. In some cases, switching from venlafaxine to fluoxetine, a long-acting SSRI, and then tapering off fluoxetine, may be recommended to reduce discontinuation symptoms.[84][85] Signs and symptoms of withdrawal from abrupt cessation of an SNRI include dizziness, anxiety, insomnia, nausea, sweating, and flu-like symptoms, such as lethargy and malaise.[85]
Overdose
[edit]Causes
[edit]Overdosing on SNRIs can be caused by either drug combinations or excessive amounts of the drug itself. Venlafaxine is marginally more toxic in overdose than duloxetine or the SSRIs.[16][58][59][11][60][86]
Symptoms
[edit]Symptoms of SNRI overdose, whether it be a mixed drug interaction or the drug alone, vary in intensity and incidence based on the amount of medicine taken and the individuals sensitivity to SNRI treatment. Possible symptoms may include:[11]
- Somnolence
- Coma
- Serotonin syndrome
- Seizures
- Syncope
- Tachycardia
- Hypotension
- Hypertension
- Hyperthermia
- Vomiting
Management
[edit]Overdose is usually treated symptomatically, especially in the case of serotonin syndrome, which requires treatment with cyproheptadine and temperature control based on the progression of the serotonin toxicity.[87] Patients are often monitored for vitals and airways cleared to ensure that they are receiving adequate levels of oxygen. Another option is to use activated carbon in the GI tract in order to absorb excess neurotransmitter.[11]
Comparison to SSRIs
[edit]Because SNRIs were developed more recently than SSRIs, there are relatively few of them. However, the SNRIs are among the most widely used antidepressants today. In 2009, Cymbalta and Effexor were the 11th- and 12th-most-prescribed branded drugs in the United States, respectively. This translates to the 2nd- and 3rd-most-common antidepressants, behind Lexapro (escitalopram), an SSRI.[88] In some studies, SNRIs demonstrated slightly higher antidepressant efficacy than the SSRIs (response rates 63.6% versus 59.3%).[43] However, in one study escitalopram had a superior efficacy profile to venlafaxine.[89]
Special populations
[edit]Pregnancy
[edit]No antidepressants are FDA approved during pregnancy.[90][failed verification] Use of antidepressants during pregnancy may result in fetus abnormalities affecting functional development of the brain and behavior.[90][dubious – discuss] Studies have shown correlations between pregnant women treated with SNRIs and risk of hypertensive disorders,[91] preeclampsia,[92] miscarriage,[93] seizures in children,[94] and many other adverse affects.[citation needed]
Pediatrics
[edit]SSRIs and SNRIs have been shown to be effective in treating major depressive disorder and anxiety in pediatric populations.[95] However, differences in metabolism, renal function, and total percentage of body water and body fat can influence the pharmacokinetics of medications in youths as compared to adults.[96] Additionally, there is a risk of increased suicidality in pediatric populations for treatment of major depressive disorder, especially with venlafaxine.[95] Fluoxetine and Escitalopram are the only antidepressants that are approved for child/adolescent major depressive disorder.[96] A literature review by Castagna, et. al from 2023 shows indications of efficacy treating pediatric generalized anxiety disorder. Currently, Duloxetine, an SNRI, is the only FDA-approved medication for pediatric GAD, despite the fact that SSRIs are typically first-line treatment.[96][97] It is suggested that these medications be combined with psychotherapy to maximize effectiveness.[98][96]
Geriatrics
[edit]Most antidepressants, including SNRIs, are safe and effective in the geriatric population. The geriatric population is at greater risk for adverse effects relating to drug interaction as they are more likely to experience polypharmacy.[99] Decisions are often based on co-morbid conditions, drug interactions, and patient tolerance. Due to differences in body composition and metabolism, starting doses are often half that of the recommended dose for younger adults.[100] Studies show that these factors also put the geriatric population at increased risk of adverse effects when treated with SNRIs but not with SSRIs.[101][102]
Research
[edit]A systematic review that looked at the efficacy of antidepressants for pain relief concludes that only 11 of 42 comparisons showed evidence of efficacy. Seven of the eleven comparisons belong to the SNRI drug class.[103]
See also
[edit]References
[edit]- ^ Cleveland Clinic medical professional (2023-03-05). "SNRIs". Cleveland Clinic. Retrieved 2024-01-09.
- ^ a b c Stahl SM, Grady MM, Moret C, Briley M (September 2005). "SNRIs: their pharmacology, clinical efficacy, and tolerability in comparison with other classes of antidepressants". CNS Spectrums. 10 (9): 732–747. doi:10.1017/S1092852900019726. PMID 16142213.
- ^ Cashman JR, Ghirmai S (October 2009). "Inhibition of serotonin and norepinephrine reuptake and inhibition of phosphodiesterase by multi-target inhibitors as potential agents for depression". Bioorganic & Medicinal Chemistry. 17 (19): 6890–6897. doi:10.1016/j.bmc.2009.08.025. PMID 19740668.
- ^ Wright ME, Rizzolo D (March 2017). "An update on the pharmacologic management and treatment of neuropathic pain". JAAPA. 30 (3): 13–17. doi:10.1097/01.JAA.0000512228.23432.f7. PMID 28151738. S2CID 205396280.
- ^ Spina E, Santoro V, D'Arrigo C (July 2008). "Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update". Clinical Therapeutics. 30 (7): 1206–1227. doi:10.1016/S0149-2918(08)80047-1. PMID 18691982.
- ^ Hillhouse TM, Porter JH (February 2015). "A brief history of the development of antidepressant drugs: from monoamines to glutamate". Experimental and Clinical Psychopharmacology. 23 (1): 1–21. doi:10.1037/a0038550. PMC 4428540. PMID 25643025.
- ^ a b Deecher DC, Beyer CE, Johnston G, Bray J, Shah S, Abou-Gharbia M, et al. (August 2006). "Desvenlafaxine succinate: A new serotonin and norepinephrine reuptake inhibitor". The Journal of Pharmacology and Experimental Therapeutics. 318 (2): 657–665. doi:10.1124/jpet.106.103382. PMID 16675639. S2CID 15063064.
- ^ a b Perry R, Cassagnol M (June 2009). "Desvenlafaxine: a new serotonin-norepinephrine reuptake inhibitor for the treatment of adults with major depressive disorder". Clinical Therapeutics. 31 (1): 1374–1404. doi:10.1016/j.clinthera.2009.07.012. PMID 19698900.
- ^ Iyengar S, Webster AA, Hemrick-Luecke SK, Xu JY, Simmons RM (November 2004). "Efficacy of duloxetine, a potent and balanced serotonin-norepinephrine reuptake inhibitor in persistent pain models in rats". The Journal of Pharmacology and Experimental Therapeutics. 311 (2): 576–584. doi:10.1124/jpet.104.070656. PMID 15254142. S2CID 18022449.
- ^ a b c d Hunziker ME, Suehs BT, Bettinger TL, Crismon ML (August 2005). "Duloxetine hydrochloride: a new dual-acting medication for the treatment of major depressive disorder". Clinical Therapeutics. 27 (8): 1126–1143. doi:10.1016/j.clinthera.2005.08.010. PMID 16199241.
- ^ a b c d e f g h i j k l "Cymbalta- duloxetine hydrochloride capsule, delayed release". DailyMed. 20 September 2021. Retrieved 12 February 2023.
- ^ "Yentreve (duloxetine hydrochloride) Hard Gastro-Resistant Capsules. Summary of Product Characteristics" (PDF). European Medicines Agency. Archived from the original (PDF) on 26 June 2016. Retrieved 29 August 2016.
- ^ "Nefazodone hydrochloride tablet". DailyMed. 16 November 2021. Retrieved 12 February 2023.
- ^ a b Frampton JE, Plosker GL (2007). "Duloxetine: a review of its use in the treatment of major depressive disorder". CNS Drugs. 21 (7): 581–609. doi:10.2165/00023210-200721070-00004. PMID 17579500. S2CID 22242897.
- ^ a b Morishita S, Arita S (February 2003). "The clinical use of milnacipran for depression". European Psychiatry. 18 (1): 34–35. doi:10.1016/S0924-9338(02)00003-2. PMID 12648895. S2CID 5978467.
- ^ a b c d e "Meridia (sibutramine hydrochloride monohydrate) Capsules C-IV. Full Prescribing Information (archived label)". Abbott Laboratories, North Chicago, IL 60064, USA. Retrieved 2 September 2016.
- ^ Luque CA, Rey JA (April 2002). "The discovery and status of sibutramine as an anti-obesity drug". European Journal of Pharmacology. 440 (2–3): 119–128. doi:10.1016/S0014-2999(02)01423-1. PMID 12007530.
- ^ Rockoff JD, Dooren JC (October 8, 2010). "Abbott Pulls Diet Drug Meridia Off US Shelves". The Wall Street Journal. Archived from the original on 11 October 2010. Retrieved 8 October 2010.
- ^ Keating GM (2006). "Tramadol sustained-release capsules". Drugs. 66 (2): 223–230. doi:10.2165/00003495-200666020-00006. PMID 16451094. S2CID 22620947.
- ^ a b Gutierrez MA, Stimmel GL, Aiso JY (August 2003). "Venlafaxine: a 2003 update". Clinical Therapeutics. 25 (8): 2138–2154. doi:10.1016/s0149-2918(03)80210-2. PMID 14512125.
- ^ a b Joffe H, Guthrie KA, LaCroix AZ, Reed SD, Ensrud KE, Manson JE, et al. (July 2014). "Low-dose estradiol and the serotonin-norepinephrine reuptake inhibitor venlafaxine for vasomotor symptoms: a randomized clinical trial". JAMA Internal Medicine. 174 (7): 1058–1066. doi:10.1001/jamainternmed.2014.1891. PMC 4179877. PMID 24861828.
- ^ Redrobe JP, Bourin M, Colombel MC, Baker GB (July 1998). "Dose-dependent noradrenergic and serotonergic properties of venlafaxine in animal models indicative of antidepressant activity". Psychopharmacology. 138 (1): 1–8. doi:10.1007/s002130050638. PMID 9694520. S2CID 35064471.
- ^ a b Lieberman JA (2003). "History of the Use of Antidepressants in Primary Care" (PDF). Primary Care Companion J Clin Psychiatry. 5 (S7): 6–10. Archived from the original (PDF) on 2014-06-11. Retrieved 2014-03-05.
- ^ Ruelas EG, Diaz-Martinez A, Ruiz RM, Study TV, Group C (1997). "An open assessment of the acceptability, efficacy, and tolerance of venlafaxine in usual care settings". Current Therapeutic Research. 58 (9): 609–630. doi:10.1016/S0011-393X(97)80088-4.
- ^ a b c Grandoso L, Pineda J, Ugedo L (May 2004). "Comparative study of the effects of desipramine and reboxetine on locus coeruleus neurons in rat brain slices". Neuropharmacology. 46 (6): 815–823. doi:10.1016/j.neuropharm.2003.11.033. PMID 15033341. S2CID 13228862.
- ^ Pacher P, Kecskemeti V (2004). "Cardiovascular side effects of new antidepressants and antipsychotics: new drugs, old concerns?". Current Pharmaceutical Design. 10 (20): 2463–2475. doi:10.2174/1381612043383872. PMC 2493295. PMID 15320756.
- ^ a b Brunello N, Mendlewicz J, Kasper S, Leonard B, Montgomery S, Nelson J, et al. (October 2002). "The role of noradrenaline and selective noradrenaline reuptake inhibition in depression". European Neuropsychopharmacology. 12 (5): 461–475. doi:10.1016/s0924-977x(02)00057-3. hdl:11380/307479. PMID 12208564. S2CID 7989883.
- ^ a b c Lemke TL, Williams DA, Roche VF, Zito SW (2008). Foye's principles of medicinal chemistry (6th ed.). USA: Lippincott Williams & Wilkins. pp. 547–67, 581–582.
- ^ a b c d e Brunton LL, Lazo JS, Parker KL, eds. (2006). Goodman & Gilman's: The Pharmacological Basis of Therapeutics (11 ed.). New York: McGraw-Hill.
- ^ Silverthorn DU, ed. (2007). Human Physiology (4 ed.). San Francisco: Pearson. pp. 383–384.
- ^ Nutt DJ, Forshall S, Bell C, Rich A, Sandford J, Nash J, et al. (July 1999). "Mechanisms of action of selective serotonin reuptake inhibitors in the treatment of psychiatric disorders". European Neuropsychopharmacology. 9 (Suppl 3): S81 – S86. doi:10.1016/S0924-977X(99)00030-9. PMID 10523062. S2CID 23634771.
- ^ Santarsieri D, Schwartz TL (2015). "Antidepressant efficacy and side-effect burden: a quick guide for clinicians". Drugs in Context. 4 212290. doi:10.7573/dic.212290. PMC 4630974. PMID 26576188.
- ^ Clevenger SS, Malhotra D, Dang J, Vanle B, IsHak WW (January 2018). "The role of selective serotonin reuptake inhibitors in preventing relapse of major depressive disorder". Therapeutic Advances in Psychopharmacology. 8 (1): 49–58. doi:10.1177/2045125317737264. PMC 5761909. PMID 29344343.
- ^ a b Zeind C, Carvalho MG (2018). Applied Therapeutics: The Clinical Use of Drugs, 11e. Wolters Kluwer. pp. 1813–1833. ISBN 978-1-4963-1829-9.
- ^ a b c d Boot J, Cases M, Clark BP, Findlay J, Gallagher PT, Hayhurst L, et al. (February 2005). "Discovery and structure-activity relationships of novel selective norepinephrine and dual serotonin/norepinephrine reuptake inhibitors". Bioorganic & Medicinal Chemistry Letters. 15 (3): 699–703. doi:10.1016/j.bmcl.2004.11.025. PMID 15664840.
- ^ a b c Mahaney PE, Vu AT, McComas CC, Zhang P, Nogle LM, Watts WL, et al. (December 2006). "Synthesis and activity of a new class of dual acting norepinephrine and serotonin reuptake inhibitors: 3-(1H-indol-1-yl)-3-arylpropan-1-amines". Bioorganic & Medicinal Chemistry. 14 (24): 8455–8466. doi:10.1016/j.bmc.2006.08.039. PMID 16973367.
- ^ Mahaney PE, Gavrin LK, Trybulski EJ, Stack GP, Vu TA, Cohn ST, et al. (July 2008). "Structure-activity relationships of the cycloalkanol ethylamine scaffold: discovery of selective norepinephrine reuptake inhibitors". Journal of Medicinal Chemistry. 51 (13): 4038–4049. doi:10.1021/jm8002262. PMID 18557608.
- ^ a b c Chen C, Dyck B, Fleck BA, Foster AC, Grey J, Jovic F, et al. (February 2008). "Studies on the SAR and pharmacophore of milnacipran derivatives as monoamine transporter inhibitors". Bioorganic & Medicinal Chemistry Letters. 18 (4): 1346–1349. doi:10.1016/j.bmcl.2008.01.011. PMID 18207394.
- ^ a b c Tamiya J, Dyck B, Zhang M, Phan K, Fleck BA, Aparicio A, et al. (June 2008). "Identification of 1S,2R-milnacipran analogs as potent norepinephrine and serotonin transporter inhibitors". Bioorganic & Medicinal Chemistry Letters. 18 (11): 3328–3332. doi:10.1016/j.bmcl.2008.04.025. PMID 18445525.
- ^ Vu AT, Cohn ST, Terefenko EA, Moore WJ, Zhang P, Mahaney PE, et al. (May 2009). "3-(Arylamino)-3-phenylpropan-2-olamines as a new series of dual norepinephrine and serotonin reuptake inhibitors". Bioorganic & Medicinal Chemistry Letters. 19 (9): 2464–2467. doi:10.1016/j.bmcl.2009.03.054. PMID 19329313.
- ^ Boot JR, Brace G, Delatour CL, Dezutter N, Fairhurst J, Findlay J, et al. (November 2004). "Benzothienyloxy phenylpropanamines, novel dual inhibitors of serotonin and norepinephrine reuptake". Bioorganic & Medicinal Chemistry Letters. 14 (21): 5395–5399. doi:10.1016/j.bmcl.2004.08.005. PMID 15454233.
- ^ Fish PV, Deur C, Gan X, Greene K, Hoople D, Mackenny M, et al. (April 2008). "Design and synthesis of morpholine derivatives. SAR for dual serotonin & noradrenaline reuptake inhibition". Bioorganic & Medicinal Chemistry Letters. 18 (8): 2562–2566. doi:10.1016/j.bmcl.2008.03.050. PMID 18387300.
- ^ a b Papakostas GI, Thase ME, Fava M, Nelson JC, Shelton RC (December 2007). "Are antidepressant drugs that combine serotonergic and noradrenergic mechanisms of action more effective than the selective serotonin reuptake inhibitors in treating major depressive disorder? A meta-analysis of studies of newer agents". Biological Psychiatry. 62 (11): 1217–1227. doi:10.1016/j.biopsych.2007.03.027. PMID 17588546. S2CID 45621773.
- ^ Nemeroff CB, Thase ME (2007). "A double-blind, placebo-controlled comparison of venlafaxine and fluoxetine treatment in depressed outpatients". Journal of Psychiatric Research. 41 (3–4): 351–359. doi:10.1016/j.jpsychires.2005.07.009. PMID 16165158.
- ^ Marks DM, Shah MJ, Patkar AA, Masand PS, Park GY, Pae CU (December 2009). "Serotonin-norepinephrine reuptake inhibitors for pain control: premise and promise". Current Neuropharmacology. 7 (4): 331–336. doi:10.2174/157015909790031201. PMC 2811866. PMID 20514212.
- ^ Beesdo K, Hartford J, Russell J, Spann M, Ball S, Wittchen HU (December 2009). "The short- and long-term effect of duloxetine on painful physical symptoms in patients with generalized anxiety disorder: results from three clinical trials". Journal of Anxiety Disorders. 23 (8): 1064–1071. doi:10.1016/j.janxdis.2009.07.008. PMID 19643572.
- ^ Sansone RA, Sansone LA (June 2011). "SNRIs pharmacological alternatives for the treatment of obsessive compulsive disorder?". Innovations in Clinical Neuroscience. 8 (6): 10–14. PMC 3140892. PMID 21779536.
- ^ Troy SM, Parker VP, Hicks DR, Pollack GM, Chiang ST (October 1997). "Pharmacokinetics and effect of food on the bioavailability of orally administered venlafaxine". Journal of Clinical Pharmacology. 37 (10): 954–961. doi:10.1002/j.1552-4604.1997.tb04270.x. PMID 9505987. S2CID 33518952.
- ^ Wichniak A, Wierzbicka A, Walęcka M, Jernajczyk W (August 2017). "Effects of Antidepressants on Sleep". Current Psychiatry Reports. 19 (9) 63. doi:10.1007/s11920-017-0816-4. PMC 5548844. PMID 28791566.
- ^ "Helpful for chronic pain in addition to depression". Mayo Clinic. Retrieved 2019-10-24.
- ^ Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA (August 2023). "The serotonin theory of depression: a systematic umbrella review of the evidence". Molecular Psychiatry. 28 (8): 3243–3256. doi:10.1038/s41380-022-01661-0. PMC 10618090. PMID 35854107. S2CID 250646781.
- ^ Nutt DJ (2008). "Relationship of neurotransmitters to the symptoms of major depressive disorder". The Journal of Clinical Psychiatry. 69: 4–7. PMID 18494537.
- ^ Sindrup SH, Otto M, Finnerup NB, Jensen TS (June 2005). "Antidepressants in the treatment of neuropathic pain". Basic & Clinical Pharmacology & Toxicology. 96 (6): 399–409. doi:10.1111/j.1742-7843.2005.pto_96696601.x. PMID 15910402.
- ^ Shelton RC, Miller AH (2011). "Inflammation in depression: is adiposity a cause?". Dialogues in Clinical Neuroscience. 13 (1): 41–53. doi:10.31887/DCNS.2011.13.1/rshelton. PMC 3181969. PMID 21485745.
- ^ a b Tynan RJ, Weidenhofer J, Hinwood M, Cairns MJ, Day TA, Walker FR (March 2012). "A comparative examination of the anti-inflammatory effects of SSRI and SNRI antidepressants on LPS stimulated microglia". Brain, Behavior, and Immunity. 26 (3): 469–479. doi:10.1016/j.bbi.2011.12.011. PMID 22251606. S2CID 39281923.
- ^ "Cambridge University Press - Service Announcement".
- ^ Lambert O, Bourin M (November 2002). "SNRIs: mechanism of action and clinical features". Expert Review of Neurotherapeutics. 2 (6): 849–858. doi:10.1586/14737175.2.6.849. PMID 19810918. S2CID 37792842.
- ^ a b c d "Pristiq Extended-Release- desvenlafaxine succinate tablet, extended release". DailyMed. 25 March 2022. Retrieved 12 February 2023.
- ^ a b c d e "Effexor XR- venlafaxine hydrochloride capsule, extended release". DailyMed. 29 August 2022. Retrieved 12 February 2023.
- ^ a b c d e "Savella- milnacipran hydrochloride tablet, film coated Savella- milnacipran hydrochloride kit". DailyMed. 23 December 2022. Retrieved 12 February 2023.
- ^ a b Raouf M, Glogowski AJ, Bettinger JJ, Fudin J (August 2017). "Serotonin-norepinephrine reuptake inhibitors and the influence of binding affinity (Ki) on analgesia". Journal of Clinical Pharmacy and Therapeutics. 42 (4): 513–517. doi:10.1111/jcpt.12534. PMID 28503727.
- ^ a b c Upadhyaya HP, Desaiah D, Schuh KJ, Bymaster FP, Kallman MJ, Clarke DO, et al. (March 2013). "A review of the abuse potential assessment of atomoxetine: a nonstimulant medication for attention-deficit/hyperactivity disorder". Psychopharmacology. 226 (2). Springer Nature: 189–200. doi:10.1007/s00213-013-2986-z. PMC 3579642. PMID 23397050.
- ^ Roth BL, Driscol J (Dec 2012). "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 7 July 2018.
- ^ Takano A, Halldin C, Farde L (2013-03-01). "SERT and NET occupancy by venlafaxine and milnacipran in nonhuman primates: a PET study". Psychopharmacology. 226 (1): 147–153. doi:10.1007/s00213-012-2901-z. ISSN 1432-2072. PMID 23090625.
- ^ a b Boyer EW, Shannon M (March 2005). "The serotonin syndrome". The New England Journal of Medicine. 352 (11): 1112–1120. doi:10.1056/NEJMra041867. PMID 15784664. S2CID 37959124.
- ^ Zhong Z, Wang L, Wen X, Liu Y, Fan Y, Liu Z (November 2017). "A meta-analysis of effects of selective serotonin reuptake inhibitors on blood pressure in depression treatment: outcomes from placebo and serotonin and noradrenaline reuptake inhibitor controlled trials". Neuropsychiatric Disease and Treatment. 13: 2781–2796. doi:10.2147/NDT.S141832. PMC 5683798. PMID 29158677.
- ^ McIntyre RS et al. The hepatic safety profile of duloxetine: a review. Expert Opin Drug Metab Toxicol. 2008;4(3):281–285.
- ^ Mladěnka P, Applová L, Patočka J, Costa VM, Remiao F, Pourová J, et al. (July 2018). "Comprehensive review of cardiovascular toxicity of drugs and related agents". Medicinal Research Reviews. 38 (4): 1332–1403. doi:10.1002/med.21476. PMC 6033155. PMID 29315692.
- ^ Chris Aiken: Antidepressants in Bipolar II Disorder, May 14, 2019. In: psychiatrictimes.com
- ^ "SNRI Antidepressants". poison.org. Retrieved 2019-10-21.
- ^ Versiani M, Cassano G, Perugi G, Benedetti A, Mastalli L, Nardi A, et al. (January 2002). "Reboxetine, a selective norepinephrine reuptake inhibitor, is an effective and well-tolerated treatment for panic disorder". The Journal of Clinical Psychiatry. 63 (1): 31–37. doi:10.4088/jcp.v63n0107. PMID 11838623.
- ^ Olivier JD, Olivier B (2019-09-01). "Antidepressants and Sexual Dysfunctions: a Translational Perspective". Current Sexual Health Reports. 11 (3): 156–166. doi:10.1007/s11930-019-00205-y.
- ^ Clayton AH, Montejo AL (2006). "Major depressive disorder, antidepressants, and sexual dysfunction". The Journal of Clinical Psychiatry. 67 (Suppl 6): 33–37. PMID 16848675.
- ^ a b Jing E, Straw-Wilson K (July 2016). "Sexual dysfunction in selective serotonin reuptake inhibitors (SSRIs) and potential solutions: A narrative literature review". The Mental Health Clinician. 6 (4): 191–196. doi:10.9740/mhc.2016.07.191. PMC 6007725. PMID 29955469.
- ^ "Serotonin syndrome: Preventing, recognizing, and treating it". www.mdedge.com. Retrieved 2019-11-21.
- ^ a b Frank C (July 2008). "Recognition and treatment of serotonin syndrome". Canadian Family Physician. 54 (7): 988–992. PMC 2464814. PMID 18625822.
- ^ "SNRI Antidepressants". poison.org. Retrieved 2019-10-23.
- ^ Tint A, Haddad PM, Anderson IM (May 2008). "The effect of rate of antidepressant tapering on the incidence of discontinuation symptoms: a randomised study". Journal of Psychopharmacology. 22 (3): 330–332. doi:10.1177/0269881107081550. PMID 18515448. S2CID 145217439.
- ^ a b Cochran KA, Cavallari LH, Shapiro NL, Bishop JR (August 2011). "Bleeding incidence with concomitant use of antidepressants and warfarin". Therapeutic Drug Monitoring. 33 (4): 433–438. doi:10.1097/FTD.0b013e318224996e. PMC 3212440. PMID 21743381.
- ^ Cheng YL, Hu HY, Lin XH, Luo JC, Peng YL, Hou MC, et al. (November 2015). "Use of SSRI, But Not SNRI, Increased Upper and Lower Gastrointestinal Bleeding: A Nationwide Population-Based Cohort Study in Taiwan". Medicine. 94 (46) e2022. doi:10.1097/MD.0000000000002022. PMC 4652818. PMID 26579809.
- ^ Curr Neurol, Neurosci Rep. (2022). "Visual Snow: Updates on Pathology". Current Neurology and Neuroscience Reports. 22 (3). National Institutes of Health: 209–217. doi:10.1007/s11910-022-01182-x. PMC 8889058. PMID 35235167.
- ^ "Duloxetine: Drug Information". UpToDate. Retrieved 28 June 2012.
- ^ Perahia DG, Pritchett YL, Kajdasz DK, Bauer M, Jain R, Russell JM, et al. (January 2008). "A randomized, double-blind comparison of duloxetine and venlafaxine in the treatment of patients with major depressive disorder". Journal of Psychiatric Research. 42 (1): 22–34. doi:10.1016/j.jpsychires.2007.01.008. PMID 17445831.
- ^ Wilson E, Lader M (December 2015). "A review of the management of antidepressant discontinuation symptoms". Therapeutic Advances in Psychopharmacology. 5 (6): 357–368. doi:10.1177/2045125315612334. PMC 4722507. PMID 26834969.
- ^ a b Fava GA, Benasi G, Lucente M, Offidani E, Cosci F, Guidi J (2018). "Withdrawal Symptoms after Serotonin-Noradrenaline Reuptake Inhibitor Discontinuation: Systematic Review" (PDF). Psychotherapy and Psychosomatics. 87 (4): 195–203. doi:10.1159/000491524. PMID 30016772.
- ^ Taylor D, Lenox-Smith A, Bradley A (June 2013). "A review of the suitability of duloxetine and venlafaxine for use in patients with depression in primary care with a focus on cardiovascular safety, suicide and mortality due to antidepressant overdose". Therapeutic Advances in Psychopharmacology. 3 (3): 151–161. doi:10.1177/2045125312472890. PMC 3805457. PMID 24167687.
- ^ Simon LV, Hashmi MF, Keenaghan M (2019). "Serotonin Syndrome". StatPearls. StatPearls Publishing. PMID 29493999. Retrieved 2019-11-21.
- ^ "2009 Top 200 branded drugs by total prescriptions" (PDF). SDI/Verispan, VONA, full year 2009. www.drugtopics.com. Archived from the original (PDF) on 14 July 2011. Retrieved 6 April 2011.
- ^ Llorca PM, Fernandez JL (April 2007). "Escitalopram in the treatment of major depressive disorder: clinical efficacy, tolerability and cost-effectiveness vs. venlafaxine extended-release formulation". International Journal of Clinical Practice. 61 (4): 702–710. doi:10.1111/j.1742-1241.2007.01335.x. PMID 17394446.
- ^ a b Dubovicky M, Belovicova K, Csatlosova K, Bogi E (September 2017). "Risks of using SSRI / SNRI antidepressants during pregnancy and lactation". Interdisciplinary Toxicology. 10 (1): 30–34. doi:10.1515/intox-2017-0004. PMC 6096863. PMID 30123033.
- ^ Benevent J, Araujo M, Karki S, Delarue-Hurault C, Waser J, Lacroix I, et al. (July 2023). "Risk of Hypertensive Disorders of Pregnancy in Women Treated With Serotonin-Norepinephrine Reuptake Inhibitors: A Comparative Study Using the EFEMERIS Database". The Journal of Clinical Psychiatry. 84 (4): 47872. doi:10.4088/JCP.22m14734. PMID 37437238.
- ^ Tran YH, Huynh HK, Faas MM, de Vos S, Groen H (February 2022). "Antidepressant use during pregnancy and development of preeclampsia: A focus on classes of action and specific transporters/receptors targeted by antidepressants". Journal of Psychiatric Research. 146: 92–101. doi:10.1016/j.jpsychires.2021.12.038. PMID 34959164.
- ^ Smith S, Martin F, Rai D, Forbes H (January 2024). "Association between antidepressant use during pregnancy and miscarriage: a systematic review and meta-analysis". BMJ Open. 14 (1) e074600. doi:10.1136/bmjopen-2023-074600. PMC 10824002. PMID 38272551.
- ^ Wiggs KK, Sujan AC, Rickert ME, Quinn PD, Larsson H, Lichtenstein P, et al. (June 2022). "Maternal Serotonergic Antidepressant Use in Pregnancy and Risk of Seizures in Children". Neurology. 98 (23): e2329 – e2336. doi:10.1212/WNL.0000000000200516. PMC 9202527. PMID 35545445.
- ^ a b Strawn JR, Mills JA, Sauley BA, Welge JA (April 2018). "The Impact of Antidepressant Dose and Class on Treatment Response in Pediatric Anxiety Disorders: A Meta-Analysis". Journal of the American Academy of Child and Adolescent Psychiatry. 57 (4): 235–244.e2. doi:10.1016/j.jaac.2018.01.015. PMC 5877120. PMID 29588049.
- ^ a b c d Strawn JR, Vaughn S, Ramsey LB (April 2022). "Pediatric Psychopharmacology for Depressive and Anxiety Disorders". Focus. 20 (2): 184–190. doi:10.1176/appi.focus.20210036. PMC 10153505. PMID 37153132.
- ^ Strawn JR, Prakash A, Zhang Q, Pangallo BA, Stroud CE, Cai N, et al. (April 2015). "A randomized, placebo-controlled study of duloxetine for the treatment of children and adolescents with generalized anxiety disorder". Journal of the American Academy of Child and Adolescent Psychiatry. 54 (4): 283–293. doi:10.1016/j.jaac.2015.01.008. PMID 25791145.
- ^ Castagna PJ, Farahdel E, Potenza MN, Crowley MJ (May 2023). "The current state-of-the-art in pharmacotherapy for pediatric generalized anxiety disorder". Expert Opinion on Pharmacotherapy. 24 (7): 835–847. doi:10.1080/14656566.2023.2199921. PMC 10197951. PMID 37074259.
- ^ Brender R, Mulsant BH, Blumberger DM (October 2021). "An update on antidepressant pharmacotherapy in late-life depression". Expert Opinion on Pharmacotherapy. 22 (14): 1909–1917. doi:10.1080/14656566.2021.1921736. PMID 33910422.
- ^ Mulsant BH, Blumberger DM, Ismail Z, Rabheru K, Rapoport MJ (August 2014). "A systematic approach to pharmacotherapy for geriatric major depression". Clinics in Geriatric Medicine. 30 (3): 517–534. doi:10.1016/j.cger.2014.05.002. PMC 4122285. PMID 25037293.
- ^ Simon G (October 2019). "Review: In older adults with acute major depression, SNRIs, but not SSRIs, increase adverse events vs placebo". Annals of Internal Medicine. 171 (8): JC39. doi:10.7326/acpj201910150-039. PMID 31610552.
- ^ "More adverse events with SNRIs than placebo in older patients". The Brown University Psychopharmacology Update. 30 (10): 7–8. October 2019. doi:10.1002/pu.30488. ISSN 1068-5308.
- ^ Ferreira GE, Abdel-Shaheed C, Underwood M, Finnerup NB, Day RO, McLachlan A, et al. (February 2023). "Efficacy, safety, and tolerability of antidepressants for pain in adults: overview of systematic reviews". BMJ. 380 e072415. doi:10.1136/bmj-2022-072415. PMC 9887507. PMID 36725015.
Serotonin–norepinephrine reuptake inhibitor
View on GrokipediaDefinition and Classification
Definition
Serotonin–norepinephrine reuptake inhibitors (SNRIs) are a class of pharmacological agents that inhibit the reuptake of serotonin (5-hydroxytryptamine, 5-HT) and norepinephrine (NE) by blocking their respective presynaptic transporters, the serotonin transporter (SERT) and the norepinephrine transporter (NET).[1][2] This dual inhibition prevents the reabsorption of these monoamine neurotransmitters into the presynaptic neuron, thereby increasing their extracellular concentrations in the synaptic cleft.[10][12] By elevating synaptic levels of both 5-HT and NE, SNRIs enhance neurotransmission involving these catecholamines, which differentiates them from selective serotonin reuptake inhibitors (SSRIs) that primarily target SERT or norepinephrine reuptake inhibitors (NRIs) that focus on NET.[1][3] This balanced or selective modulation of monoamine systems is thought to contribute to their therapeutic effects in conditions involving dysregulated serotonin and norepinephrine signaling.[13] SNRIs are primarily classified as antidepressants due to their efficacy in treating major depressive disorder, and they also serve as analgesics for chronic pain management by influencing descending pain inhibitory pathways.[6][8] Within the SNRI class, drugs vary in their potency ratios for SERT versus NET inhibition; for instance, venlafaxine exhibits a serotonin-preferring profile with approximately 30-fold higher affinity for SERT than NET, while others like duloxetine show a more balanced 10-fold selectivity for serotonin reuptake inhibition.[14][15]Classification Within Antidepressants
Serotonin–norepinephrine reuptake inhibitors (SNRIs) are positioned as second-generation antidepressants, emerging after the first-generation tricyclic antidepressants (TCAs) and alongside selective serotonin reuptake inhibitors (SSRIs). This classification reflects their development in the late 1980s and 1990s as an evolution from earlier agents, offering improved tolerability while targeting multiple monoamine systems.[16] Unlike the single-target focus of SSRIs on serotonin reuptake, SNRIs' dual inhibition of both serotonin and norepinephrine reuptake enables a broader neurochemical impact, which is associated with enhanced efficacy in treating major depressive disorder, particularly in cases refractory to SSRIs.[17] SNRIs are further subclassified based on their relative selectivity for the serotonin transporter (SERT) versus the norepinephrine transporter (NET), determined by binding affinity measures such as inhibition constants (Ki values). This subclassification highlights variations in their pharmacological profiles, influencing clinical applications. Serotonin-preferring SNRIs, exemplified by venlafaxine, demonstrate markedly higher affinity for SERT (Ki = 82 nM) than NET (Ki = 2480 nM), yielding a selectivity ratio (NET/SERT) of approximately 30, which results in predominant serotonergic effects at lower doses.[18] In contrast, balanced SNRIs like duloxetine exhibit more equipotent inhibition, with Ki values of 0.8 nM for SERT and 7.5 nM for NET, corresponding to a selectivity ratio of about 9 and allowing concurrent modulation of both neurotransmitters across therapeutic doses.[18] Norepinephrine-preferring SNRIs, such as levomilnacipran, show reduced SERT selectivity (Ki = 11.2 nM for SERT and 92.2 nM for NET, ratio ≈8), providing relatively greater norepinephrine reuptake inhibition compared to serotonin-preferring agents and resembling hybrids with selective norepinephrine reuptake inhibitors like reboxetine.[19]History
Early Development
The development of serotonin–norepinephrine reuptake inhibitors (SNRIs) traces its origins to the tricyclic antidepressants (TCAs), which emerged in the mid-20th century as the first effective pharmacological treatments for depression. Imipramine, synthesized in 1951 and introduced clinically in the late 1950s, represented a breakthrough as the inaugural TCA, discovered serendipitously during research into antipsychotic agents.[20] This compound non-selectively inhibited the reuptake of both serotonin (5-HT) and norepinephrine (NE) at their respective transporters, thereby elevating synaptic levels of these monoamines and alleviating depressive symptoms in patients.[20] Throughout the 1960s, further TCAs such as amitriptyline and desipramine expanded on imipramine's foundation, confirming the therapeutic relevance of dual monoamine reuptake inhibition while highlighting the need for refined selectivity.[21] These early agents laid the groundwork for subsequent antidepressants by establishing the monoamine hypothesis of depression, which posits that deficiencies in 5-HT and NE contribute to mood disorders.[20] A pivotal advancement in the 1970s involved the synthesis of viloxazine, developed by Imperial Chemical Industries as a prototype selective norepinephrine reuptake inhibitor (NRI) for depression treatment.[22] Unlike the broad-spectrum TCAs, viloxazine primarily targeted NE reuptake with minimal impact on other systems, facilitating the transition toward dual-action compounds that balanced 5-HT and NE modulation without excessive non-specificity.[23] Early synthesis efforts for these precursors faced significant challenges, particularly the tricyclic structures' propensity for off-target effects, including potent antihistamine activity at H1 receptors, which contributed to sedation and other adverse reactions.[24] Such interactions complicated clinical utility and spurred research into structurally modified agents to enhance selectivity and reduce unwanted receptor bindings.[24]Key Approvals and Milestones
The development of serotonin–norepinephrine reuptake inhibitors (SNRIs) marked a significant advancement in antidepressant therapy, with the first regulatory approval occurring in 1993. Venlafaxine, first synthesized in the late 1980s by Wyeth, and marketed as Effexor, received U.S. Food and Drug Administration (FDA) approval on December 28, 1993, for the treatment of major depressive disorder (MDD), establishing it as the inaugural SNRI and offering an alternative to selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants with a dual mechanism targeting both serotonin and norepinephrine reuptake.[25][26] Subsequent approvals expanded the class's therapeutic scope beyond depression. Duloxetine, branded as Cymbalta, was approved by the FDA on August 3, 2004, initially for MDD and diabetic peripheral neuropathic pain, later gaining indications for generalized anxiety disorder in 2007, fibromyalgia in 2008, and chronic musculoskeletal pain in 2010, highlighting the SNRI class's efficacy in managing both mood and pain disorders.[27][28] Milnacipran, under the trade name Savella, followed with FDA approval on January 14, 2009, specifically for the management of fibromyalgia, broadening SNRI applications to non-psychiatric chronic pain conditions despite its earlier approval in Europe for depression.[29] Further milestones included the approval of levomilnacipran extended-release capsules (Fetzima) by the FDA on July 25, 2013, for adults with MDD, introducing a more norepinephrine-selective SNRI profile that showed potential advantages in certain depressive symptoms.[30] Desvenlafaxine, the active metabolite of venlafaxine and marketed as Pristiq, had been approved earlier on February 29, 2008, for MDD; clinical studies have supported its off-label use in anxiety disorders, though formal FDA expansion remains pending as of 2025.[31][32]Mechanism of Action
Serotonin Reuptake Inhibition
Serotonin–norepinephrine reuptake inhibitors (SNRIs) primarily block serotonin reuptake by binding to the serotonin transporter (SERT), a sodium-dependent transmembrane protein expressed on presynaptic serotonergic neurons in the central nervous system. This binding occurs at the central substrate-binding site (S1 pocket) of SERT, where SNRIs competitively inhibit the transporter's ability to translocate serotonin (5-HT) from the synaptic cleft back into the presynaptic terminal. As a result, synaptic clearance of 5-HT is reduced, leading to prolonged availability of the neurotransmitter in the extracellular space.[12] The accumulation of extracellular 5-HT enhances serotonergic signaling by stimulating postsynaptic receptors, notably the 5-HT1A autoreceptors and heteroreceptors, as well as 5-HT2A and 5-HT2C subtypes, which modulate neuronal excitability and downstream intracellular pathways such as adenylate cyclase and phospholipase C activation. This receptor activation contributes to the neuroplastic changes associated with antidepressant effects, though the acute increase in 5-HT can initially desensitize presynaptic 5-HT1A autoreceptors over time.[33][34] Affinity for SERT varies among SNRIs, influencing their potency in serotonin reuptake inhibition; for instance, venlafaxine demonstrates a high affinity with a Ki value of 82 nM for human SERT in vitro, enabling effective blockade at clinically relevant doses, while its metabolite desvenlafaxine maintains similar potency. Other SNRIs, such as duloxetine, exhibit even stronger SERT inhibition with a Ki of 0.8 nM, highlighting structural differences that optimize binding interactions within the SERT pocket. These variations underscore the dose-dependent nature of serotonin reuptake blockade in SNRIs, where lower doses predominantly target SERT before norepinephrine effects become prominent.[18][35]Norepinephrine Reuptake Inhibition
Serotonin–norepinephrine reuptake inhibitors (SNRIs) exert their effects on the noradrenergic system primarily through blockade of the norepinephrine transporter (NET), a sodium/chloride-dependent membrane protein that facilitates the reuptake of norepinephrine (NE) from the synaptic cleft back into presynaptic neurons.[1] By binding to NET and inhibiting this reuptake process, SNRIs increase extracellular NE concentrations in key brain regions such as the locus coeruleus and prefrontal cortex, enhancing noradrenergic neurotransmission.[2] This elevation of synaptic NE levels is central to the therapeutic actions of SNRIs in conditions involving noradrenergic dysregulation. The increased synaptic NE resulting from NET inhibition activates various adrenergic receptors, including presynaptic α₂-adrenergic autoreceptors on noradrenergic neurons, which provide negative feedback to modulate NE release.[36] Initially, this activation limits excessive NE efflux, but chronic treatment leads to desensitization of these autoreceptors, ultimately promoting sustained noradrenergic signaling.[37] Postsynaptically, elevated NE stimulates β₁-adrenergic receptors, which are coupled to Gₛ proteins and increase cyclic AMP levels, contributing to enhanced arousal, attention, and vigilance.[38] In the context of pain modulation, noradrenergic enhancement via these pathways inhibits nociceptive transmission in the spinal cord, particularly through α₂-adrenergic mechanisms, providing analgesic effects.[8] Affinity for NET varies among SNRIs, influencing their noradrenergic potency; for instance, duloxetine demonstrates balanced inhibition with an IC₅₀ of approximately 7 nM for human NET, allowing effective NE reuptake blockade at clinically relevant doses. In contrast, serotonin-preferring SNRIs like venlafaxine exhibit weaker NET affinity, with an IC₅₀ around 2,550 nM, resulting in more selective serotonergic effects at lower doses.[39] This differential binding underscores the spectrum of noradrenergic engagement across the class. The combined elevation of NE and serotonin synergistically amplifies antidepressant efficacy beyond isolated monoamine effects.Synergistic Effects
The dual reuptake inhibition characteristic of SNRIs facilitates reciprocal neuroadaptations between serotonergic and noradrenergic systems, particularly through downregulation of key autoreceptors and heteroreceptors. Chronic elevation of synaptic serotonin desensitizes presynaptic 5-HT1A autoreceptors on raphe nuclei neurons, thereby reducing inhibitory feedback and enhancing serotonin release.[33] Concurrently, increased synaptic norepinephrine desensitizes α2-adrenergic autoreceptors on locus coeruleus neurons, promoting norepinephrine release, while also desensitizing α2-heteroreceptors located on serotonergic terminals, which further disinhibits serotonin outflow.[40] This bidirectional interaction results in amplified neurotransmission of both monoamines, exceeding the effects achievable through isolated inhibition of either system.[41] In addition to enhancing acute monoamine signaling, SNRIs contribute to long-term therapeutic benefits by promoting neuroplasticity, largely via upregulation of brain-derived neurotrophic factor (BDNF). Elevated levels of serotonin and norepinephrine activate signaling pathways, such as TrkB receptor phosphorylation, that increase BDNF expression in regions like the hippocampus and prefrontal cortex, fostering dendritic arborization, synaptogenesis, and neuronal survival.[42] This BDNF-mediated plasticity improves overall monoamine efficacy by strengthening circuit connectivity in mood-regulating networks, a process integral to the sustained antidepressant action of SNRIs.[43] Preclinical evidence from animal models underscores the superior efficacy of dual reuptake blockade over single-modality inhibition. In rodent chronic unpredictable stress paradigms, SNRIs like duloxetine elicit greater reductions in depressive-like behaviors—such as immobility in the forced swim test—compared to selective serotonin reuptake inhibitors or norepinephrine reuptake inhibitors alone, attributable to the synergistic enhancement of monoamine tone and neuroplastic adaptations.[44] Similarly, dual inhibitors demonstrate more robust reversal of anhedonia and anxiety-like symptoms in olfactory bulbectomy models, highlighting the additive value of combined serotonergic and noradrenergic modulation.[45]Pharmacology
Pharmacodynamics
Serotonin–norepinephrine reuptake inhibitors (SNRIs) exert their primary pharmacodynamic effects by blocking the presynaptic reuptake of serotonin (5-HT) and norepinephrine (NE), thereby elevating extracellular concentrations of these monoamines in the synaptic cleft and enhancing neurotransmission. This dual inhibition varies in potency across the class; for instance, venlafaxine displays approximately 30-fold higher affinity for the serotonin transporter (SERT; Ki ≈ 80 nM) compared to the norepinephrine transporter (NET; Ki ≈ 2,480 nM), while duloxetine shows more balanced inhibition (SERT Ki ≈ 0.8 nM, NET Ki ≈ 7.5 nM). Levomilnacipran, in contrast, exhibits slightly greater potency for NET inhibition (IC50 ≈ 10.5 nM) over SERT (IC50 ≈ 19 nM). These actions initiate downstream signaling through postsynaptic 5-HT and NE receptors, including 5-HT1A, 5-HT2A, and α1-adrenergic receptors, contributing to mood regulation and antinociceptive effects. Dose-response relationships differ among SNRIs, often shifting from predominantly serotonergic to dual effects at higher doses. Venlafaxine, for example, achieves substantial SERT occupancy (>80%) at doses below 150 mg/day, mimicking selective serotonin reuptake inhibitor (SSRI) activity, but NET occupancy increases dose-dependently thereafter, reaching approximately 45% at 150 mg/day and over 50% at 225–300 mg/day, enhancing noradrenergic effects. This transition correlates with improved efficacy in treatment-resistant depression but also raises risks like dose-dependent hypertension due to NE elevation. Off-target effects are generally minimal but notable in some agents. High doses of venlafaxine (>300 mg/day) can produce weak dopamine reuptake inhibition (DAT Ki ≈ 2,060–7,640 nM), potentially augmenting reward pathways. Levomilnacipran similarly shows weak DAT affinity (IC50 >10 μM), with negligible clinical impact compared to its primary targets. SNRIs also display low-affinity interactions with the sigma-1 receptor (e.g., duloxetine and venlafaxine with Ki >1,000 nM), which may subtly modulate neuroplasticity and chaperone activity without significant contributions to core efficacy. Chronic SNRI administration induces adaptive changes in receptor function, including desensitization of presynaptic autoreceptors that initially limit monoamine release. 5-HT1A autoreceptors in the raphe nuclei desensitize over 2–4 weeks, reducing negative feedback and allowing sustained 5-HT efflux. Similarly, α2-adrenergic autoreceptors on noradrenergic neurons downregulate within the same timeframe, amplifying NE signaling and aligning with the typical 2–6 week onset of therapeutic response. These adaptations are critical for the delayed but robust antidepressant effects observed in clinical use.Pharmacokinetics
Serotonin–norepinephrine reuptake inhibitors (SNRIs) are typically administered orally and exhibit variable absorption profiles depending on the specific agent. For instance, duloxetine demonstrates an absolute oral bioavailability ranging from 32% to 80% (mean of 50%), largely limited by extensive first-pass metabolism in the liver and gut wall.[46] Venlafaxine has an absolute bioavailability of approximately 45%, reflecting substantial first-pass effects despite high intestinal absorption of at least 92%.[47] In contrast, desvenlafaxine, the active metabolite of venlafaxine, achieves higher absolute oral bioavailability of about 80%, with minimal first-pass impact.[48] Food generally does not significantly alter the overall bioavailability of SNRIs; for venlafaxine and desvenlafaxine, high-fat meals have no meaningful effect on absorption, though they may slightly delay peak plasma concentrations for duloxetine by about 2 hours without requiring dosage adjustments.[47][48][46] Following absorption, SNRIs are widely distributed throughout the body, with steady-state plasma concentrations achieved within 3 to 5 days due to their moderate half-lives.[49] Venlafaxine exhibits a short elimination half-life of 5 ± 2 hours, while its active metabolite desvenlafaxine has a longer half-life of 11 ± 2 hours; duloxetine's half-life is approximately 12 hours (range 8 to 17 hours).[50][46] These agents display linear pharmacokinetics within the therapeutic dose range, meaning plasma concentrations increase proportionally with dose without accumulation beyond expected levels.[46][48][47] Metabolism of SNRIs primarily occurs via hepatic cytochrome P450 (CYP) enzymes, with variations across compounds influencing potential drug interactions. Venlafaxine is predominantly metabolized by CYP2D6 to its active metabolite O-desmethylvenlafaxine (desvenlafaxine), which contributes significantly to its therapeutic effects.[51] Duloxetine undergoes extensive metabolism through CYP1A2 (major) and CYP2D6 pathways, producing multiple inactive metabolites.[52] Desvenlafaxine, however, is minimally metabolized and primarily excreted unchanged, reducing CYP-related variability.[48] Elimination of SNRIs occurs mainly through renal excretion of metabolites, with parent compounds showing dose-proportional clearance in healthy individuals. Approximately 70% of duloxetine is recovered in urine as metabolites, while venlafaxine and its metabolite are eliminated about 87% renally (55% as ODV).[46][47] Pharmacokinetic profiles vary by specific SNRI, with adjustments needed in renal or hepatic impairment to avoid accumulation.[48]Structure-Activity Relationship
Aryloxypropanamine Derivatives
The aryloxypropanamine derivatives form a major structural class within serotonin–norepinephrine reuptake inhibitors (SNRIs), featuring a core phenoxypropanamine scaffold where aryl substitutions on the phenyl ring enhance affinity for the serotonin transporter (SERT) and norepinephrine transporter (NET). This backbone consists of a propanamine chain linked to a substituted phenoxy group, with the aryl ring typically bearing electron-donating groups like methoxy to facilitate hydrophobic interactions in the transporter binding pockets.[53] The cyclohexanol moiety in representative compounds further stabilizes binding through hydrogen bonding, contributing to dual inhibition potency.[1] Key modifications to this scaffold include the introduction of fluorine atoms, as seen in certain analogs of desvenlafaxine, which improve pharmacokinetic properties by increasing metabolic stability and reducing clearance rates without compromising SERT/NET affinity. Structure-activity relationship (SAR) studies reveal that the length of the ethylamine chain significantly influences selectivity; shorter chains enhance SERT inhibition, while extensions promote balanced or NET-preferring activity, allowing fine-tuning for therapeutic profiles.[54] The benzenoid ring substitutions, such as the 4-methoxy group in venlafaxine, play a non-essential role in core binding but affect overall lipophilicity and transporter access.[55] Prominent examples include venlafaxine, the prototypical SNRI with its 4-methoxyphenyl and 1-hydroxycyclohexyl substitutions providing Ki values of approximately 80 nM for SERT and 2500 nM for NET, and desvenlafaxine, its O-demethylated metabolite featuring a 4-hydroxyphenyl group that retains equivalent efficacy while exhibiting 10-fold SERT selectivity over NET and superior pharmacokinetics independent of CYP2D6.[1] Synthesis of these derivatives often involves multi-step processes starting from cyanohydrin intermediates derived from aryl ketones and cyanide addition, followed by reduction of the nitrile to the primary amine and subsequent N,N-dimethylation; challenges include low yields in the stereoselective cyanohydrin formation and purification of the tertiary amine under reductive conditions to avoid over-alkylation.[56]Other Scaffolds
In addition to the predominant aryloxypropanamine derivatives, alternative chemical scaffolds have been explored for serotonin–norepinephrine reuptake inhibitors (SNRIs), offering distinct structural features that influence binding affinity and selectivity. One notable example is the cycloalkanol ethylamine scaffold exemplified by milnacipran, which incorporates a bicyclic cyclopropane core linking a phenyl ring, an N,N-diethylcarboxamide group, and an aminomethyl side chain, enabling balanced inhibition of both serotonin (SERT) and norepinephrine (NET) transporters with Ki values around 100–200 nM for each. This scaffold's rigidity contrasts with more flexible aryloxy structures, potentially contributing to milnacipran's favorable pharmacokinetic profile and reduced affinity for off-target receptors like the dopamine transporter.[57] Milnacipran is administered as a racemic mixture of (1R,2S)- and (1S,2R)-enantiomers, but the (1S,2R)-configuration, marketed as levomilnacipran, demonstrates superior potency compared to the racemate and the (1R,2S)-enantiomer, which has substantially lower affinity for both transporters. In human recombinant systems, levomilnacipran exhibits Ki values of 11 nM for SERT and 92 nM for NET, indicating higher binding affinity for SERT; however, in functional assays, it shows slightly greater potency for NET reuptake inhibition (IC50 10.5 nM) than SERT (IC50 19 nM), resulting in a norepinephrine-preferring profile relative to other SNRIs.[58] This balanced modulation may enhance efficacy in conditions like major depressive disorder where noradrenergic activity is beneficial.[59] Emerging scaffolds for next-generation SNRIs include piperazine-based frameworks, which have gained attention in post-2020 research for their potential to yield dual reuptake inhibitors with improved selectivity and reduced side effects through modular substitutions on the piperazine ring.[60] These structures leverage the piperazine's nitrogen atoms for hydrogen bonding with transporter residues, positioning them as promising candidates for investigational dual inhibitors beyond traditional scaffolds.Approved Medications
Commonly Used SNRIs
Venlafaxine, marketed as Effexor, is a serotonin-preferring SNRI with approximately 30-fold higher affinity for inhibiting serotonin reuptake compared to norepinephrine reuptake, particularly at lower therapeutic doses where serotonergic effects predominate, while higher doses engage more balanced dual inhibition.[1] It is available in extended-release formulations, which allow for once-daily dosing and improved tolerability by reducing peak plasma fluctuations.[61] Venlafaxine is approved for major depressive disorder, generalized anxiety disorder, social anxiety disorder, and panic disorder.[62][63] Duloxetine, known as Cymbalta, exhibits a more balanced profile with about 10-fold selectivity for serotonin over norepinephrine reuptake inhibition, making it effective for conditions involving both neurotransmitters.[1] It is uniquely approved among SNRIs for diabetic peripheral neuropathy in addition to major depressive disorder, generalized anxiety disorder, fibromyalgia, and chronic musculoskeletal pain.[5][64] Duloxetine's dual action supports its use in pain-related disorders, though it requires monitoring for hepatic effects in patients with comorbidities.[65] Milnacipran, available as Savella, is the most equipotent SNRI, inhibiting serotonin and norepinephrine reuptake with nearly equal affinity, which contributes to its efficacy in conditions responsive to noradrenergic enhancement.[1] It is approved specifically for fibromyalgia management in the United States, where it helps alleviate widespread pain and fatigue without sedative properties common in other analgesics.[66] Other SNRIs include desvenlafaxine (Pristiq), the active metabolite of venlafaxine, which shares a similar serotonin-preferring profile with 10-fold higher selectivity for serotonin reuptake and is approved for major depressive disorder with a simpler pharmacokinetic profile due to minimal metabolism.[1] Levomilnacipran (Fetzima) stands out as norepinephrine-preferring, with greater potency for norepinephrine reuptake inhibition (up to 2- to 3-fold over serotonin), offering potential advantages in patients with prominent anhedonia or fatigue in major depressive disorder.[19]Dosage and Administration
Serotonin–norepinephrine reuptake inhibitors (SNRIs) are primarily administered orally, with the majority of approved formulations designed as extended-release capsules or tablets to facilitate once-daily dosing and improve patient compliance.[63][64] Initial dosing typically begins at lower levels to assess tolerability, such as 37.5–75 mg per day for venlafaxine extended-release or 30–60 mg per day for duloxetine.[63][64] Titration schedules are employed to minimize side effects by allowing gradual achievement of therapeutic plasma levels, often increasing the dose in increments of 30–75 mg every 4–7 days based on individual response and tolerance.[63][64] For venlafaxine extended-release, doses may be escalated up to a maximum of 225 mg per day, while duloxetine can reach up to 120 mg per day if needed, though higher doses do not consistently provide additional benefit and may increase adverse events.[63][64] Similar principles apply to other SNRIs, such as desvenlafaxine starting at 50 mg per day with a maximum of 100 mg, and levomilnacipran initiating at 20 mg per day for 2 days followed by titration to 40–120 mg per day.[48][67] Formulation differences significantly influence administration; immediate-release versions, like certain venlafaxine tablets, require divided dosing (twice or three times daily), whereas extended-release options support once-daily regimens, enhancing adherence by reducing pill burden.[68][63] These dosing strategies are informed by pharmacokinetic profiles, where steady-state concentrations are typically reached within 3–5 days, guiding the timing of dose adjustments.[61]Therapeutic Uses
Major Depressive Disorder
Serotonin–norepinephrine reuptake inhibitors (SNRIs) are indicated for the treatment of major depressive disorder (MDD), where they function by inhibiting the reuptake of both serotonin and norepinephrine, thereby enhancing neurotransmission in these key monoaminergic systems to alleviate depressive symptoms.[4] This dual mechanism is particularly beneficial in MDD subtypes characterized by prominent anhedonia, psychomotor retardation, and fatigue, such as melancholic depression, as norepinephrine enhancement addresses motivational and psychomotor deficits more effectively than serotonin-focused agents alone.[69] According to the American Psychiatric Association (APA) guidelines, SNRIs are recommended as first-line pharmacotherapy options alongside SSRIs for moderate to severe MDD, with a switch to an SNRI like venlafaxine or duloxetine advised following inadequate response to SSRIs to optimize outcomes.[70] In monotherapy, SNRIs achieve response rates of approximately 50-60% in adults with MDD, comparable to other second-generation antidepressants, based on comprehensive network meta-analyses of randomized controlled trials.[71] A distinctive advantage of SNRIs in severe MDD cases is their potential for faster onset of antidepressant effects compared to SSRIs, attributed to elevated dopamine levels in the medial prefrontal cortex via norepinephrine modulation, which may accelerate symptom relief in acutely ill patients.[72]Chronic Pain Conditions
Serotonin–norepinephrine reuptake inhibitors (SNRIs) are utilized in the management of specific chronic pain conditions, particularly those involving neuropathic and musculoskeletal components. Duloxetine, a prototypical SNRI, received U.S. Food and Drug Administration (FDA) approval in 2004 for treating neuropathic pain associated with diabetic peripheral neuropathy, based on evidence from randomized controlled trials demonstrating its ability to alleviate pain intensity in affected patients.[73] In 2008, the FDA extended approval to duloxetine for fibromyalgia, recognizing its role in reducing widespread pain and associated symptoms in this syndrome.[74] Milnacipran (Savella) received FDA approval in 2009 for the management of fibromyalgia, with clinical trials showing improvements in pain, fatigue, and physical function.[75] These approvals highlight SNRIs' established position in guidelines for chronic pain refractory to other therapies. The mechanism underlying SNRIs' analgesic effects in chronic pain centers on norepinephrine modulation of descending inhibitory pathways in the spinal cord. By blocking norepinephrine reuptake, SNRIs increase synaptic norepinephrine availability, which activates α2-adrenergic receptors on spinal dorsal horn neurons, thereby inhibiting nociceptive signal transmission from peripheral afferents.[76] This noradrenergic enhancement complements serotonergic actions but is particularly crucial for pain relief, as descending pathways from brainstem nuclei like the locus coeruleus project to the spinal cord to dampen hyperalgesia in neuropathic and fibromyalgia models.[8] Such modulation addresses the central sensitization common in these conditions, distinguishing SNRIs from selective serotonin reuptake inhibitors, which show lesser analgesic potency. Clinical meta-analyses confirm SNRIs' efficacy, with duloxetine typically yielding at least 30% pain reduction in 20-30% more patients than placebo across chronic neuropathic pain and fibromyalgia over 12 weeks, and ≥50% reduction in up to 12-15% additional patients compared to controls.[77] For diabetic peripheral neuropathy, the relative risk for ≥30% pain intensity reduction is approximately 1.43 (95% CI 1.19-1.71), corresponding to a number needed to treat of 11. In fibromyalgia, the relative risk for ≥50% reduction reaches 1.57 (95% CI 1.20-2.06), with a number needed to treat of 8. These outcomes underscore moderate-to-high certainty evidence for pain relief in 30-50% of responders, though benefits vary by dose (typically 60 mg daily) and individual factors.[78]Other Approved Indications
SNRIs have established approvals for treating generalized anxiety disorder (GAD), a condition characterized by excessive, persistent worry and anxiety. Venlafaxine, marketed as Effexor XR, received FDA approval for GAD in adults in 1999, based on clinical trials demonstrating significant reductions in anxiety symptoms compared to placebo. Duloxetine, known as Cymbalta, was approved by the FDA for GAD in February 2007, following evidence from randomized controlled trials showing efficacy in alleviating GAD symptoms over 9-10 months of treatment. Venlafaxine also received FDA approval for social anxiety disorder in 2003 and panic disorder in 2005, supported by trials establishing efficacy in reducing social phobia symptoms and panic attack frequency.[47] These approvals highlight SNRIs' role in modulating both serotonin and norepinephrine to address anxiety beyond depressive states. In addition to anxiety disorders, duloxetine has been approved for stress urinary incontinence (SUI) in women by the European Medicines Agency (EMA) since 2004, under the brand name Yentreve, where it enhances urethral tone and reduces incontinence episodes through noradrenergic effects on the pelvic floor. However, the FDA application for duloxetine in SUI was voluntarily withdrawn in 2005 prior to approval, citing the need for additional data, and it remains unapproved for this indication in the United States.[79] This regional difference underscores varying regulatory assessments of SNRI utility in urological conditions.Clinical Evidence
Efficacy in Depression
Serotonin–norepinephrine reuptake inhibitors (SNRIs) have demonstrated efficacy as second-line treatments for major depressive disorder (MDD) following inadequate response to selective serotonin reuptake inhibitors (SSRIs). In the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial, a large-scale pragmatic study involving over 4,000 patients, switching to the SNRI venlafaxine extended-release after SSRI failure resulted in a remission rate of 25% based on Hamilton Depression Rating Scale scores, comparable to other switch options like bupropion or sertraline.[80] This positions SNRIs as effective alternatives, contributing to cumulative remission rates of approximately 50% after two treatment steps in real-world settings.[81] Meta-analyses of randomized controlled trials further support the efficacy of SNRIs in acute MDD treatment. The 2018 Cipriani network meta-analysis of 522 trials involving 116,477 participants found that SNRIs such as venlafaxine and duloxetine were more efficacious than placebo in achieving response (odds ratio [OR] 1.78 for venlafaxine; 95% credible interval [CrI] 1.40–2.20) and comparable to SSRIs overall, with all antidepressants showing moderate effect sizes over placebo.[82] Head-to-head trials indicate SNRIs may have a modest advantage over SSRIs in remission rates (48.5% vs. 41.9%; OR 1.27, 95% CI 1.06–1.52 in intention-to-treat analyses), though clinical significance is debated after bias adjustment.[83] Recent analyses, including a 2025 study, confirm that SNRIs significantly improve depressive symptoms, though individual agents like escitalopram (an SSRI) may show earlier effects.[84] Long-term use of SNRIs aids in relapse prevention among patients achieving initial remission. A comprehensive review of 72 maintenance trials (n=14,450) indicated that SNRIs outperformed placebo in 13 of 15 studies, with overall relapse risk reduced by up to 50% compared to placebo across continuation phases averaging 33 weeks.[85] For instance, desvenlafaxine maintenance therapy reduced relapse rates to 29% versus 50% with placebo over six months in responders.[86] These findings underscore the role of SNRIs in sustaining remission, though individual response variability remains a key consideration.[87]Analgesic Trials
Phase III randomized controlled trials (RCTs) of duloxetine for fibromyalgia demonstrated significant analgesic efficacy. In one pivotal 12-week trial involving patients with fibromyalgia, duloxetine at 60 mg once daily resulted in a ≥30% reduction in Brief Pain Inventory (BPI) average pain score for 41% of participants, compared to 26% in the placebo group, while the 60 mg twice-daily dose achieved 50% response versus 26% placebo.[88] Another phase III trial reported response rates of approximately 38% for duloxetine 60 mg twice daily versus 21% for placebo, based on ≥30% pain improvement, establishing duloxetine's role in managing fibromyalgia-associated pain through dual reuptake inhibition. These trials, involving over 1,000 patients across studies, highlighted sustained pain relief and functional improvements, with effect sizes indicating moderate clinical benefit (standardized mean difference ~0.4-0.5 on pain scales).[89] For venlafaxine in neuropathic pain, evidence from smaller RCTs supports moderate efficacy, though trials are fewer and often underpowered compared to those for duloxetine. A Cochrane review of three RCTs (total n=274) found venlafaxine (150-225 mg/day) provided ≥50% pain relief in 28% of patients versus 12% on placebo, yielding a number needed to treat (NNT) of 5.2 (95% CI 2.7-5.9) for moderate or better pain reduction.[90] In diabetic neuropathy specifically, a 6-week RCT (n=244) showed venlafaxine extended-release 150-225 mg achieving 50% pain intensity reduction in 47% of patients versus 28% placebo, with an NNT of 4.5, though higher doses were associated with increased nausea.[91] These studies indicate venlafaxine's utility as an adjunct in central and peripheral neuropathic pain syndromes, with effect sizes similar to tricyclic antidepressants but better tolerability at therapeutic doses.[92] Recent trials (2022-2025) on SNRIs for osteoarthritis pain reveal mixed results, addressing previous gaps in long-term data for this indication. A 2022 multicenter RCT (n=132) in patients with chronic knee or hip osteoarthritis found no additional pain relief from duloxetine 60 mg/day added to usual care (adjusted mean WOMAC pain score difference: -0.58, 95% CI -1.80 to 0.63 at 3 months; p>0.05), suggesting limited benefit in non-neuropathic osteoarthritis.[93] Conversely, a 2022 RCT in end-stage osteoarthritis patients awaiting joint replacement (n=66) reported significant pain reduction with duloxetine 30-60 mg/day (NRS decrease: -2.1 vs. -0.9 placebo; p=0.01) and improved function on the Oxford Hip/Knee Score.[94] Ongoing trials, such as the sequenced strategy study (NCT04504812, completed 2024), continue to evaluate duloxetine's role in knee osteoarthritis, but results remain unpublished, highlighting incomplete integration of post-2022 evidence into clinical guidelines.[95] No major RCTs for venlafaxine in osteoarthritis emerged in this period, underscoring a research focus on duloxetine for musculoskeletal pain.Comparative Studies
Comparative studies have demonstrated that serotonin–norepinephrine reuptake inhibitors (SNRIs) exhibit similar overall efficacy to selective serotonin reuptake inhibitors (SSRIs) in the acute treatment of major depressive disorder, with both classes outperforming placebo in response rates. However, in cases of treatment-resistant depression, SNRIs may offer a modest advantage in achieving remission when patients switch from SSRIs. A meta-analysis of randomized trials involving 1,496 SSRI non-responders found that switching to an SNRI such as venlafaxine resulted in higher remission rates (28% vs. 23.5%; risk ratio 1.29, 95% CI 1.07–1.56) compared to within-class switches to another SSRI.[96] This benefit is attributed to the dual reuptake inhibition mechanism of SNRIs, which may address residual symptoms not fully alleviated by serotonin-focused therapies.[82] In comparisons with tricyclic antidepressants (TCAs), SNRIs show comparable antidepressant efficacy but markedly better tolerability profiles, particularly with reduced anticholinergic burden. TCAs like amitriptyline are associated with higher rates of side effects such as dry mouth, constipation, and orthostatic hypotension due to their non-selective receptor interactions, leading to greater treatment discontinuation. A network meta-analysis of 522 trials indicated that SNRIs, including duloxetine and venlafaxine, had higher acceptability (lower dropout odds ratios relative to placebo: 0.84–0.91) than most TCAs (e.g., 0.84 for amitriptyline but lower for clomipramine at 0.50), supporting their preference in clinical practice for minimizing adverse events.[82] This improved safety is especially relevant for older adults or those with cardiovascular risks, where TCAs pose greater hazards.[97] Recent evidence from a 2024 network meta-analysis highlights SNRIs' efficacy in more severe depression, with venlafaxine showing symptom reduction (standardized mean difference -0.32, 95% CrI -0.43 to -0.22 vs. placebo).[98] This was observed across moderate-to-severe cases, though combined therapies (e.g., SNRIs plus psychotherapy) yielded the broadest benefits.[98]Adverse Effects
Common Side Effects
Common side effects of serotonin–norepinephrine reuptake inhibitors (SNRIs) are typically mild to moderate and often resolve with continued use or dose adjustment, affecting a significant portion of patients during initial treatment. Gastrointestinal disturbances are among the most frequent, with nausea occurring in 20–30% of patients across clinical trials of agents like venlafaxine and desvenlafaxine, often peaking in the first week and diminishing thereafter.[63][99] Dry mouth is also prevalent, reported in 10–15% of users, particularly with duloxetine and venlafaxine.[100][101] Neurological effects commonly include headache and dizziness, each affecting 10–20% of patients, with dizziness more pronounced during dose escalation owing to orthostatic changes from norepinephrine reuptake inhibition.[10][11] Sexual dysfunction, such as delayed orgasm or anorgasmia, arises in 15–25% of individuals, comparable to rates seen with SSRIs but potentially exacerbated by dual reuptake blockade.[102][103] Additional dose-related complaints linked to enhanced noradrenergic tone involve increased sweating (hyperhidrosis) in 10–12% of cases and insomnia in 15–18%, both more noticeable at higher doses of SNRIs like venlafaxine.[63][104]Serious Adverse Events
Serotonin syndrome is a potentially life-threatening condition associated with serotonin–norepinephrine reuptake inhibitors (SNRIs), resulting from excessive serotonergic activity in the central and peripheral nervous systems.[105] Symptoms can include hyperthermia, muscle rigidity, autonomic instability such as tachycardia and hypertension, and altered mental status including agitation and confusion.[106] The risk is particularly elevated when SNRIs are combined with monoamine oxidase inhibitors (MAOIs), where irreversible MAOIs pose the greatest threat due to prolonged effects.[107] Incidence of serotonin syndrome requiring hospitalization is rare, estimated at less than 1% among patients on serotonergic agents, though exact rates for SNRIs alone remain underreported due to diagnostic challenges.[108] Hypertension represents another serious cardiovascular risk with SNRIs, primarily driven by norepinephrine reuptake inhibition leading to increased sympathetic activity and blood pressure elevation.[109] This effect is dose-dependent, with clinically significant sustained increases in diastolic blood pressure observed at higher doses, particularly for venlafaxine exceeding 225 mg per day.[109] Monitoring of blood pressure is recommended in patients with preexisting hypertension or when escalating to such doses to mitigate risks of accelerated hypertension.[61] Case reports have documented severe hypertensive episodes, such as blood pressure reaching 162/110 mm Hg at 150 mg/day of venlafaxine, underscoring the need for vigilant clinical oversight.[110] Rare hepatotoxicity has been reported with duloxetine, an SNRI, including cases of hepatic failure that can present as hepatitis with or without jaundice and, in extreme instances, prove fatal.[111] These events occur idiosyncratically in postmarketing surveillance, with labeling advising against use in heavy alcohol consumers due to heightened risk.[111] Recent 2025 analyses indicate limited evidence for alcohol-related exacerbation of hepatotoxicity, with overall incidence remaining low, emphasizing baseline liver function assessment prior to initiation.[112]Safety Considerations
Contraindications
Serotonin–norepinephrine reuptake inhibitors (SNRIs) are contraindicated in patients receiving concurrent monoamine oxidase inhibitors (MAOIs), including reversible and irreversible forms, due to the high risk of precipitating serotonin syndrome, a potentially fatal condition characterized by autonomic instability, neuromuscular abnormalities, and altered mental status.[113] A washout period of at least 14 days is required after discontinuing an MAOI before initiating SNRI therapy, while the reverse requires 5 to 7 days depending on the specific SNRI, to allow for enzyme recovery and prevent excessive serotonergic activity.[64] This interaction arises from the combined inhibition of serotonin and norepinephrine reuptake, leading to synergistic neurotransmitter accumulation.[47] SNRIs are also contraindicated in individuals with uncontrolled hypertension, as the inhibition of norepinephrine reuptake can elevate systemic blood pressure through enhanced sympathetic activity, potentially exacerbating cardiovascular risk.[114] Similarly, use is prohibited in patients with narrow-angle glaucoma or a history of angle-closure glaucoma, where the noradrenergic effects may induce mydriasis, increasing intraocular pressure and risking acute closure.[115] These contraindications stem directly from the dual reuptake inhibition mechanism, which amplifies adrenergic tone beyond serotonergic effects alone.[116] Hypersensitivity to any SNRI or its excipients represents an absolute contraindication, as it may provoke anaphylactic reactions or severe dermatologic events upon exposure.[113] SNRIs should be used with caution in patients with active or recent pheochromocytoma, a catecholamine-secreting tumor, because norepinephrine reuptake inhibition can intensify hypertensive crises and interfere with diagnostic metanephrine assays, leading to false positives or clinical deterioration.[117] In such cases, close blood pressure monitoring is required, and alternative therapies without noradrenergic activity may be preferred.[118]Drug Interactions
Serotonin–norepinephrine reuptake inhibitors (SNRIs) exhibit both pharmacokinetic and pharmacodynamic interactions with various medications, primarily due to their metabolism via cytochrome P450 (CYP) enzymes and their effects on serotonin and norepinephrine levels. Pharmacokinetic interactions often involve CYP inhibition, leading to altered drug exposure, while pharmacodynamic interactions can amplify serotonergic activity or affect blood pressure regulation. These interactions necessitate careful monitoring and potential dose adjustments to mitigate risks such as toxicity or reduced efficacy.[119] A key pharmacokinetic interaction occurs with CYP2D6 inhibitors, as several SNRIs, including venlafaxine and duloxetine, are substrates for this enzyme. For instance, paroxetine, a potent CYP2D6 inhibitor, significantly increases venlafaxine plasma concentrations while reducing levels of its active metabolite, O-desmethylvenlafaxine, potentially leading to enhanced side effects like nausea or hypertension in extensive metabolizers. Similarly, coadministration of paroxetine with duloxetine elevates duloxetine exposure by approximately 60%, increasing the risk of adverse events such as somnolence or dry mouth. Clinicians should monitor for these effects and consider reducing SNRI doses when strong CYP2D6 inhibitors are used concurrently.[120][119] Pharmacodynamic interactions with other serotonergic agents pose a risk of serotonin syndrome, a potentially life-threatening condition characterized by autonomic instability, neuromuscular abnormalities, and altered mental status. Combining SNRIs with triptans (e.g., sumatriptan for migraine) or tramadol can result in additive serotonergic effects, as both classes enhance serotonin availability in the central nervous system; case reports and postmarketing data indicate rare but serious instances of serotonin syndrome with venlafaxine and rizatriptan or tramadol. Although the overall incidence is low, especially with triptans, close observation for symptoms like agitation or hyperreflexia is recommended during initiation or dose escalation.[47][121][122] SNRIs can also interact with antihypertensives through pharmacodynamic mechanisms, as their norepinephrine reuptake inhibition may elevate blood pressure, potentially counteracting the effects of agents like beta-blockers. Venlafaxine, in particular, is associated with dose-dependent hypertension, which may necessitate increased doses of beta-blockers such as metoprolol or closer blood pressure monitoring in patients on concurrent therapy. This interaction underscores the importance of baseline cardiovascular assessment and regular monitoring in hypertensive individuals.[123][47] Concomitant use with monoamine oxidase inhibitors (MAOIs) is contraindicated due to the risk of severe serotonin syndrome, but this is addressed under broader safety contraindications.[47]Discontinuation Syndrome
Discontinuation syndrome associated with serotonin–norepinephrine reuptake inhibitors (SNRIs) refers to a cluster of physical and psychological symptoms that can emerge upon abrupt cessation or rapid dose reduction of these medications. Recent estimates indicate an incidence of approximately 15-33% for any symptoms following abrupt discontinuation, with higher rates for SNRIs.[124] Symptoms typically onset within 1 to 3 days of discontinuation and resolve within 1 to 2 weeks, though protracted cases may persist longer.[125][126] Common symptoms include flu-like manifestations such as fatigue, chills, muscle aches, and sweating, alongside gastrointestinal issues like nausea and vomiting. Sensory disturbances are prominent, particularly "brain zaps"—described as brief electric shock-like sensations in the head or body—along with dizziness, paresthesia, and imbalance. Psychological symptoms may encompass anxiety, irritability, insomnia, and vivid dreams, while hyperarousal can manifest as agitation or restlessness. These symptoms are often more intense with SNRIs than with selective serotonin reuptake inhibitors (SSRIs) due to the additional noradrenergic effects, leading to a greater prevalence of adrenergically mediated features like tremor, tachycardia, and heightened sensory phenomena such as brain zaps.[125][127][128] Risk factors for developing discontinuation syndrome with SNRIs include abrupt cessation, longer duration of treatment (typically over 6 weeks), and use of agents with shorter half-lives, such as venlafaxine (parent half-life ~5 hours, active metabolite ~11 hours), which exhibits a higher incidence compared to longer-acting SNRIs like duloxetine (half-life 12 hours). Individual patient factors, such as genetic variations in drug metabolism or history of sensitivity to medication changes, may also contribute, though evidence is limited. In contrast to SSRIs, where serotonergic rebound predominates, SNRI withdrawal often involves more pronounced noradrenergic symptoms, potentially exacerbating autonomic instability.[126][129][127] To mitigate discontinuation syndrome, gradual dose tapering over 2 to 4 weeks is recommended, starting with a 25% to 50% reduction every 1 to 2 weeks, adjusted based on symptom emergence and patient tolerance. For short half-life SNRIs like venlafaxine, slower tapers or switching to a longer-acting equivalent (e.g., fluoxetine) may be employed to bridge the transition. If symptoms occur during tapering, resuming the previous dose and reducing more slowly can alleviate them; severe cases may require symptomatic treatment with short-term benzodiazepines for anxiety or antiemetics for nausea. Guidelines emphasize patient education on these risks prior to initiation to facilitate informed discontinuation planning.[130][131][125]Overdose Management
Clinical Presentation
In cases of serotonin–norepinephrine reuptake inhibitor (SNRI) overdose, clinical presentation varies by severity and ingested dose, often amplifying routine side effects such as nausea and tachycardia. Venlafaxine is particularly noted for its high toxicity in overdose compared to other SNRIs. Mild overdoses typically manifest with gastrointestinal symptoms like nausea and vomiting, alongside sympathomimetic effects including tachycardia (up to 160 beats per minute), hypertension, diaphoresis, tremor, mydriasis, anxiety, and dysphoria.[132][133][134] Severe overdoses can progress to life-threatening manifestations, including seizures (which may be delayed), serotonin syndrome characterized by agitation, hyperreflexia, inducible clonus, hyperthermia, and muscle rigidity, as well as cardiotoxicity including QRS widening on ECG due to sodium channel blockade, ventricular arrhythmias, and in severe cases, hypotension from cardiomyopathy.[132][133][105][134][135] Symptoms generally onset within 2 to 12 hours post-ingestion, with peak effects around 24 hours, though extended-release formulations may delay seizures up to 16 to 19 hours.[133][136] Fatal outcomes are associated with massive ingestions, such as venlafaxine doses exceeding 8 g, which heighten risks of profound cardiotoxicity including cardiogenic shock and refractory arrhythmias.[137][138]Treatment Approaches
The management of serotonin–norepinephrine reuptake inhibitor (SNRI) overdose primarily involves supportive care, as no specific antidote exists.[139] Initial assessment should focus on airway, breathing, and circulation, with continuous monitoring for symptoms such as seizures, cardiac arrhythmias, and serotonin syndrome, which may manifest following acute ingestion.[105] Gastrointestinal decontamination with activated charcoal is recommended if the patient presents within 2 hours of ingestion, particularly for venlafaxine overdoses exceeding 4.5 grams or other significant amounts, to reduce absorption.[132] This intervention has been shown to increase clearance of venlafaxine and mitigate peak serum levels when administered early.[140] Seizures, a common complication in SNRI overdose, should be treated promptly with benzodiazepines such as lorazepam or diazepam, administered intravenously to achieve rapid control.[141] For cardiac toxicity, including QRS prolongation observed in venlafaxine overdose due to sodium channel blockade, sodium bicarbonate (1-2 mEq/kg IV bolus) is indicated to narrow the QRS complex and stabilize membranes, similar to its use in tricyclic antidepressant poisoning.[142] Continuous electrocardiogram (ECG) monitoring is essential to detect and manage arrhythmias, with serial ECGs recommended in symptomatic patients.[136] In cases of serotonin syndrome, reversal with cyproheptadine (initial dose of 12 mg orally or via nasogastric tube, followed by 2 mg every 2 hours if needed) is a key intervention to antagonize serotonergic effects, alongside discontinuation of the offending agent and supportive measures like cooling for hyperthermia.[143] Admission to an intensive care unit is warranted for severe overdoses involving hemodynamic instability or refractory seizures.[144]Comparisons with Other Agents
Versus SSRIs
Serotonin–norepinephrine reuptake inhibitors (SNRIs) and selective serotonin reuptake inhibitors (SSRIs) are both first-line antidepressants, but they differ in their pharmacological profiles and clinical applications. SNRIs inhibit the reuptake of both serotonin and norepinephrine, potentially offering broader neurotransmitter modulation compared to SSRIs, which primarily target serotonin. This dual action can lead to distinct efficacy patterns in treating major depressive disorder (MDD). In terms of efficacy, SNRIs demonstrate superior outcomes for somatic symptoms in depression, such as pain and physical fatigue, due to their norepinephrine-enhancing effects, which may improve energy and motivation more effectively than SSRIs alone. For instance, meta-analyses of randomized controlled trials (RCTs) have shown that SNRIs like venlafaxine and duloxetine achieve higher response rates in patients with melancholic or somatic features of MDD compared to SSRIs such as fluoxetine or sertraline. Conversely, SSRIs often provide faster symptom relief in anxiety disorders, with onset of action within 1-2 weeks for conditions like generalized anxiety disorder (GAD), whereas SNRIs may require longer titration to balance their dual effects without exacerbating initial agitation. Regarding tolerability, SNRIs are associated with higher rates of nausea, dry mouth, and hypertension, particularly at higher doses, owing to their impact on norepinephrine pathways, which can increase sympathetic activity. In comparative studies, gastrointestinal side effects occur in up to 30% of SNRI users versus 20% with SSRIs, and blood pressure elevations are reported in 5-10% of patients on SNRIs like desvenlafaxine. However, SNRIs present sexual dysfunction rates similar to SSRIs, typically affecting 40-60% of users, though the norepinephrine component may mitigate serotonin-induced libido suppression in some cases. Overall dropout rates due to adverse events are similar between the classes, around 10-15% in long-term trials. Switching from SSRIs to SNRIs is a common strategy in treatment-resistant depression, with approximately 30% of patients who fail to respond to SSRIs showing partial or full remission after transitioning to an SNRI. Guidelines from the American Psychiatric Association recommend this augmentation after 4-6 weeks of inadequate SSRI response, often with a cross-taper to minimize withdrawal symptoms. Clinical trials, such as the STAR*D study, support this approach, indicating that SNRIs like venlafaxine provide additional benefit in 25-35% of non-responders without significantly increasing overall side effect burden.Versus TCAs and Other Classes
Serotonin–norepinephrine reuptake inhibitors (SNRIs) exhibit similar efficacy to tricyclic antidepressants (TCAs) in treating major depressive disorder, but demonstrate higher selectivity for serotonin and norepinephrine transporters, resulting in fewer off-target effects.[104] Unlike TCAs, which non-selectively inhibit multiple neurotransmitter systems including histamine, acetylcholine, and adrenergic receptors, SNRIs primarily target monoamine reuptake, leading to reduced anticholinergic side effects such as dry mouth, constipation, and urinary retention.[24] TCAs are associated with greater cardiac risks, including arrhythmias and orthostatic hypotension due to their quinidine-like effects on cardiac sodium channels, whereas SNRIs pose a lower risk of such cardiovascular adverse events in therapeutic doses.[145] Compared to bupropion, a norepinephrine-dopamine reuptake inhibitor (NDRI), SNRIs show superior efficacy in managing anxiety symptoms comorbid with depression, particularly in patients with high baseline anxiety levels, where serotonergic modulation provides additional anxiolytic benefits.[146] In contrast, bupropion is particularly effective for smoking cessation, increasing abstinence rates by 49% to 72% compared to placebo at six months, owing to its dopaminergic effects that mitigate nicotine cravings and withdrawal.[147] Regarding cost-effectiveness, the availability of generic formulations for common SNRIs like venlafaxine and duloxetine has made them preferable to mirtazapine in certain treatment guidelines for moderate to severe depression, especially where SNRIs offer comparable or superior outcomes in severe cases at lower overall healthcare costs.[148] For instance, duloxetine has been found cost-saving relative to mirtazapine in primary care settings for more severe depression, balancing acquisition costs with improved tolerability and adherence.Use in Special Populations
Pregnancy and Lactation
Serotonin–norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine and duloxetine are classified by the FDA as pregnancy category C, indicating that animal reproduction studies have shown an adverse effect on the fetus, but there are no adequate and well-controlled studies in humans, and potential benefits may warrant use despite potential risks.[149] Exposure to SNRIs during the third trimester has been associated with an increased risk of poor neonatal adaptation syndrome (PNAS), also known as neonatal abstinence syndrome, characterized by symptoms such as irritability, respiratory distress, and feeding difficulties in newborns. For example, venlafaxine exposure carries an approximate 30% risk of PNAS in third-trimester-exposed infants. Additionally, recent data indicate an increased risk of persistent pulmonary hypertension of the newborn (PPHN) with SNRI use during pregnancy, similar to that observed with SSRIs (pooled OR approximately 1.5).[150][151][152] During lactation, SNRIs like duloxetine exhibit low transfer into breast milk, with infant exposure estimated at less than 1% of the maternal weight-adjusted dose, suggesting minimal risk to the breastfeeding infant. However, monitoring for potential infant sedation and other adverse effects is recommended when SNRIs are used postpartum.[153] Guidelines emphasize an individualized risk-benefit assessment for SNRI use in pregnancy, recommending avoidance during the first trimester when possible due to limited safety data and potential teratogenic concerns, though no substantial increase in congenital malformations has been consistently observed. For women requiring ongoing treatment, tapering SNRIs over 2–4 weeks prior to delivery is advised to mitigate PNAS risk, with close neonatal monitoring post-birth.[154][151]Pediatrics
The use of serotonin–norepinephrine reuptake inhibitors (SNRIs) in pediatric populations is limited, with no FDA approvals for major depressive disorder (MDD) in children under 18 years old. Duloxetine is the only SNRI with FDA approval for generalized anxiety disorder (GAD) in children and adolescents aged 7 to 17 years, at starting doses of 30 mg daily, potentially increasing to 60 mg after two weeks.[64] For obsessive-compulsive disorder (OCD), SNRIs lack FDA approval and are used off-label primarily as augmentation to selective serotonin reuptake inhibitors (SSRIs) in treatment-resistant cases, supported by meta-analyses indicating modest efficacy over placebo in reducing OCD symptoms.[155] All SNRIs carry an FDA black box warning for increased risk of suicidality in children and adolescents, based on analyses showing elevated suicidal ideation and behavior, particularly in the initial months of treatment, necessitating close monitoring.[156] Due to heightened sensitivity in youth, treatment typically begins at low doses, such as 37.5 mg daily for venlafaxine extended-release in children aged 8–12, with gradual titration to minimize adverse effects like nausea or agitation.[157] Evidence for SNRIs in pediatric depression remains limited, with small randomized controlled trials demonstrating response rates around 40% in adolescents, often not significantly superior to placebo, as seen in studies of duloxetine and venlafaxine.[158] Recent 2023 analyses highlight ongoing gaps, noting mixed efficacy in treatment-resistant cases but emphasizing the need for larger trials to address high placebo responses (up to 60%) and long-term safety in youth.[159]Geriatrics
In geriatric patients, the administration of serotonin–norepinephrine reuptake inhibitors (SNRIs) requires a cautious approach due to age-related physiological changes, such as reduced renal and hepatic function, which can prolong drug clearance and heighten adverse effect risks. The "start low, go slow" principle is standard, initiating therapy at 25% to 50% of the typical adult starting dose and titrating gradually based on tolerance and response. For instance, venlafaxine is often begun at 18.75–37.5 mg daily in older adults, compared to 75 mg in younger patients.[160][113] In cases of renal or hepatic impairment—prevalent in up to 50% of those over 65—a 50% dose reduction is recommended for many SNRIs to mitigate accumulation and toxicity. Duloxetine, for example, starts at 20–30 mg daily in mild impairment, with further adjustments or avoidance in severe cases. SNRIs offer notable benefits in late-life depression, particularly when comorbid chronic pain is present, as dual inhibition of serotonin and norepinephrine enhances analgesic effects; duloxetine has demonstrated efficacy in reducing both depressive symptoms and neuropathic pain in this population. Compared to tricyclic antidepressants (TCAs), SNRIs pose a lower fall risk owing to reduced anticholinergic burden and less pronounced orthostatic effects, making them preferable for frail elderly patients.[113][161][160][162][163][164] Key risks include hyponatremia, induced by SIADH-like mechanisms, with SNRIs carrying a slightly elevated incidence (up to 10–15% in elderly users) compared to SSRIs, necessitating baseline and follow-up sodium monitoring, especially in the first weeks. Orthostatic hypotension, stemming from noradrenergic effects, can exacerbate fall risks in those with preexisting cardiovascular instability or polypharmacy. Per 2025 clinical guidelines, routine assessment of blood pressure, electrolytes, and fall history is emphasized, alongside patient education on symptom recognition and slow positional changes.[165][166][167][168][167]Research and Future Directions
Ongoing Developments
Recent advancements in the serotonin–norepinephrine reuptake inhibitor (SNRI) pipeline include novel candidates aimed at enhancing efficacy for major depressive disorder. Ammoxetine, a selective SNRI, demonstrated promising antidepressant effects in a phase 2 trial completed in 2025, showing significant symptom reduction with a favorable side effect profile compared to existing options.[169] Similarly, liafensine, a triple reuptake inhibitor targeting serotonin, norepinephrine, and dopamine, received FDA fast track designation in October 2024 for treatment-resistant depression, supported by pharmacogenomic biomarkers to optimize patient selection.[170] Formulation improvements focus on improving patient adherence and safety. Preclinical studies have developed transdermal prototypes of duloxetine hydrochloride using drug-in-adhesive patches, which enhance bioavailability and provide steady release to potentially reduce gastrointestinal side effects associated with oral administration.[171] These prototypes incorporate polymers like hydroxypropyl methylcellulose for controlled delivery, with in vitro permeation tests indicating sustained release over 24 hours.[172] Although abuse-deterrent formulations for venlafaxine remain in exploratory stages, research highlights its misuse potential, prompting interest in tamper-resistant designs to deter extraction for non-oral abuse.[173] Patent landscapes for SNRIs continue to evolve, with key expirations facilitating generic competition. Duloxetine's primary patents expired in 2017–2018, leading to widespread generic availability and substantial price reductions of up to 80% in major markets.[174] Venlafaxine generics, introduced following earlier expirations, dominate the market, while formulations like levomilnacipran extended-release saw generic approval in 2023, further driving accessibility.[175] As of 2025, no major SNRI biosimilars are anticipated due to their small-molecule nature, but ongoing generic entries for extended-release variants are expected to sustain cost reductions without impacting therapeutic innovation.[176]Emerging Therapeutic Areas
SNRIs are being investigated for applications beyond their established roles in major depressive disorder, anxiety, and chronic pain conditions, with research focusing on their potential in neurodevelopmental, trauma-related, and neurodegenerative disorders. Recent studies highlight their off-label use in attention-deficit/hyperactivity disorder (ADHD), where agents like venlafaxine demonstrate efficacy in reducing core symptoms such as inattention and hyperactivity, particularly as non-stimulant alternatives for patients intolerant to traditional medications. A 2024 systematic review and meta-analysis found that SNRIs significantly improved ADHD symptoms in adults and children, with moderate effect sizes on attention and impulsivity, though larger randomized controlled trials are needed to confirm long-term safety.[177] In post-traumatic stress disorder (PTSD), SNRIs such as venlafaxine continue to show promise in addressing hyperarousal and re-experiencing symptoms, with recent evidence supporting their role in combination with psychotherapy. A 2025 review of pharmacotherapy for PTSD indicated that venlafaxine, at doses of 150-300 mg/day, achieved response rates comparable to SSRIs, with particular benefits for mood stabilization in veterans and trauma survivors, based on network meta-analyses of over 20 trials. Emerging data also suggest SNRIs may enhance extinction learning in exposure-based therapies, potentially improving outcomes in treatment-resistant cases.[178] Preliminary research points to neuroprotective potential of SNRIs in neurodegenerative diseases, including Alzheimer's disease (AD) and related dementias. Additionally, SNRIs like duloxetine have shown anti-microglial activation effects in preclinical models of neurodegeneration, reducing oxidative stress and tau pathology, though human trials remain limited and emphasize comorbid depression management over direct disease modification.[179] In chronic fatigue syndrome (CFS/ME), SNRIs provide symptomatic relief for pain and sleep disturbances but lack robust evidence for core fatigue reduction, with systematic reviews indicating limited clinically meaningful benefits over placebo for quality of life.[180]References
- https://wikem.org/wiki/SNRI_Toxicity

