Recent from talks
Contribute something
Nothing was collected or created yet.
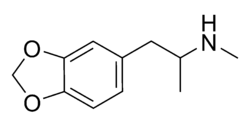
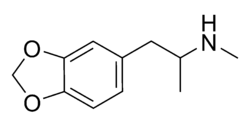 Skeletal structures of (R)-MDMA (top) and (S)-MDMA (bottom) | |
 Ball-and-stick models of (R)-MDMA (top) and (S)-MDMA (bottom) | |
| Clinical data | |
|---|---|
| Pronunciation | methylenedioxymethamphetamine: /ˌmɛθɪliːndaɪˈɒksi/ /ˌmɛθæmˈfɛtəmiːn/ |
| Other names | 3,4-MDMA; Ecstasy (E, X, XTC); Midomafetamine; Molly; Mandy;[2][3] Pingers/Pingas[4] |
| AHFS/Drugs.com | MDMA |
| Dependence liability | Physical: Not typical[5] Psychological: Moderate[6] |
| Addiction liability | Low–moderate[7][8][9] |
| Routes of administration | Common: By mouth[10] Uncommon: Insufflation,[10] inhalation,[10] injection,[10][11] rectal |
| Drug class | Entactogen; Stimulant; Psychedelic; Serotonin–norepinephrine–dopamine releasing agent; Serotonin 5-HT2 receptor agonist |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Oral: Unknown[13] |
| Protein binding | Unknown[14] |
| Metabolism | Liver, CYP450 extensively involved, including CYP2D6 |
| Metabolites | MDA, HMMA, HMA, HHMA, HHA, THMA, THA, MDP2P, MDOH[15] |
| Onset of action | Oral: 30–45 min[13] |
| Elimination half-life | |
| Duration of action | 3–6 hours[18][8][13] |
| Excretion | Kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
| Formula | C11H15NO2 |
| Molar mass | 193.246 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| Density | 1.1 g/cm3 |
| Boiling point | 105 °C (221 °F) at 0.4 mmHg (experimental) |
| |
| |
| (verify) | |
3,4-Methylenedioxymethamphetamine (MDMA), commonly known as ecstasy (tablet form), and molly (crystal form),[19][20] is an entactogen with stimulant and minor psychedelic properties.[17][21][22]
MDMA was first synthesized in 1912 by Merck chemist Anton Köllisch.[23] It was used to enhance psychotherapy beginning in the 1970s and became popular as a street drug in the 1980s.[24][25] MDMA is commonly associated with dance parties, raves, and electronic dance music.[26] Tablets sold as ecstasy may be mixed with other substances such as ephedrine, amphetamine, and methamphetamine.[24] In 2016, about 21 million people between the ages of 15 and 64 used ecstasy (0.3% of the world population).[27] In the United States, as of 2017, about 7% of people have used MDMA at some point in their lives and 0.9% have used it in the last year.[28] The lethal risk from one dose of MDMA is estimated to be from 1 death in 20,000 instances to 1 death in 50,000 instances.[29]
The purported pharmacological effects that may be prosocial include altered sensations, increased energy, empathy, and pleasure.[22][24] When taken by mouth, effects begin in 30 to 45 minutes and last three to six hours.[13][25] Short-term adverse effects include grinding of the teeth, blurred vision, sweating, and a rapid heartbeat,[24] and extended use can also lead to addiction, memory problems, paranoia, and difficulty sleeping. Deaths have been reported due to increased body temperature and dehydration. MDMA acts primarily by increasing the release of the neurotransmitters serotonin, dopamine, and norepinephrine in parts of the brain.[24][25] It belongs to the substituted amphetamine classes of drugs.[10][30] MDMA is structurally similar to mescaline (a psychedelic), methamphetamine (a stimulant), as well as endogenous monoamine neurotransmitters such as serotonin, norepinephrine, and dopamine.[31]
MDMA has limited approved medical uses in a small number of countries,[32] but is illegal in most jurisdictions.[33] MDMA-assisted psychotherapy is a promising and generally safe treatment for post-traumatic stress disorder when administered in controlled therapeutic settings.[34][35] In the United States, the Food and Drug Administration (FDA) has given MDMA breakthrough therapy status (though there no current clinical indications in the US).[36] Canada has allowed limited distribution of MDMA upon application to and approval by Health Canada.[37] In Australia, it may be prescribed in the treatment of PTSD by specifically authorised psychiatrists.[38]
Uses
[edit]Recreational
[edit]MDMA is often considered the drug of choice within the rave culture and is also used at clubs, festivals, and house parties.[15] In the rave environment, the sensory effects of music and lighting are often highly synergistic with the drug. The psychedelic amphetamine quality of MDMA offers multiple appealing aspects to users in the rave setting. Some users enjoy the feeling of mass communion from the inhibition-reducing effects of the drug, while others use it as party fuel because of the drug's stimulatory effects.[39] MDMA is used less often than other stimulants, typically less than once per week.[40]
MDMA is sometimes taken in conjunction with other psychoactive drugs such as LSD,[41] psilocybin mushrooms, 2C-B, and ketamine. The combination with LSD is called "candy-flipping".[41] The combination with 2C-B is called "nexus flipping". For this combination, most people take the MDMA first, wait until the peak is over, and then take the 2C-B.[42]
MDMA is often co-administered with alcohol, methamphetamine, and prescription drugs such as SSRIs with which MDMA has several drug-drug interactions.[43][44][45] Three life-threatening reports of MDMA co-administration with ritonavir have been reported;[46] with ritonavir having severe and dangerous drug-drug interactions with a wide range of both psychoactive, anti-psychotic, and non-psychoactive drugs.[47]
Medical
[edit]As of 2023, MDMA therapies have only been approved for research purposes, with no widely accepted medical indications,[10][48][49] although this varies by jurisdiction. Before it was widely banned, it saw limited use in psychotherapy.[8][10][50] In 2017 the United States Food and Drug Administration (FDA) granted breakthrough therapy designation for MDMA-assisted psychotherapy for post-traumatic stress disorder (PTSD).[51][52]
Some researchers have proposed that psychedelics in general may act as active "super placebos" used for therapeutic purposes.[53][54]
Others
[edit]Small doses of MDMA are used by some religious practitioners as an entheogen to enhance prayer or meditation.[55] MDMA has been used as an adjunct to New Age spiritual practices.[56]
Forms
[edit]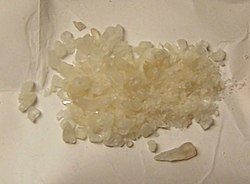
MDMA has become widely known as ecstasy (shortened "E", "X", or "XTC"), usually referring to its tablet form, although this term may also include the presence of possible adulterants or diluents. The UK term "mandy" and the US term "molly" colloquially refer to MDMA in a crystalline powder form that is thought to be free of adulterants.[2][3][57] MDMA is also sold in the form of the hydrochloride salt, either as loose crystals or in gelcaps.[58][59] MDMA tablets can sometimes be found in a shaped form that may depict characters from popular culture. These are sometimes collectively referred to as "fun tablets".[60][61]
Partly due to the global supply shortage of sassafras oil—a problem largely assuaged by use of improved or alternative modern methods of synthesis—the purity of substances sold as molly have been found to vary widely. Some of these substances contain methylone, ethylone, MDPV, mephedrone, or any other of the group of compounds commonly known as bath salts, in addition to, or in place of, MDMA.[3][57][58][59] Powdered MDMA ranges from pure MDMA to crushed tablets with 30–40% purity.[10] MDMA tablets typically have low purity due to bulking agents that are added to dilute the drug and increase profits (notably lactose) and binding agents.[10] Tablets sold as ecstasy sometimes contain 3,4-methylenedioxyamphetamine (MDA), 3,4-methylenedioxyethylamphetamine (MDEA), other amphetamine derivatives, caffeine, opiates, or painkillers.[8] Some tablets contain little or no MDMA.[8][10][62] The proportion of seized ecstasy tablets with MDMA-like impurities has varied annually and by country.[10] The average content of MDMA in a preparation is 70 to 120 mg with the purity having increased since the 1990s.[8]
MDMA is usually consumed by mouth. It is also sometimes snorted.[24]
Effects
[edit]In general, MDMA users report feeling the onset of subjective effects within 30 to 60 minutes of oral consumption and reaching peak effect at 75 to 120 minutes, which then plateaus for about 3.5 hours.[63] The desired short-term psychoactive effects of MDMA have been reported to include:
- Euphoria – a sense of general well-being and happiness[22][64]
- Increased self-confidence, sociability, and perception of facilitated communication[8][22][64]
- Entactogenic effects—increased empathy or feelings of closeness with others[22][64] and oneself[8]
- Dilated pupils[8]
- Relaxation and reduced anxiety[8]
- Increased emotionality[8]
- A sense of inner peace[64]
- Mild hallucination[64]
- Enhanced sensation, perception, or sexuality[8][22][64]
- Altered sense of time[25]
The experience elicited by MDMA depends on the dose, setting, and user.[8] The variability of the induced altered state is lower compared to other psychedelics. For example, MDMA used at parties is associated with high motor activity, reduced sense of identity, and poor awareness of surroundings. Use of MDMA individually or in small groups in a quiet environment and when concentrating, is associated with increased lucidity, concentration, sensitivity to aesthetic aspects of the environment, enhanced awareness of emotions, and improved capability of communication.[15][65] In psychotherapeutic settings, MDMA effects have been characterized by infantile ideas, mood lability, and memories and moods connected with childhood experiences.[65][66]
MDMA has been described as an "empathogenic" drug because of its empathy-producing effects.[67][68] Results of several studies show the effects of increased empathy with others.[67] When testing MDMA for medium and high doses, it showed increased hedonic and arousal continuum.[69][70] The effect of MDMA increasing sociability is consistent, while its effects on empathy have been more mixed.[71]
Side effects
[edit]Short-term
[edit]Acute adverse effects are usually the result of high or multiple doses, although single dose toxicity can occur in susceptible individuals.[22] The most serious short-term physical health risks of MDMA are hyperthermia and dehydration.[64][72] Cases of life-threatening or fatal hyponatremia (excessively low sodium concentration in the blood) have developed in MDMA users attempting to prevent dehydration by consuming excessive amounts of water without replenishing electrolytes.[64][72][29]
The immediate adverse effects of MDMA use can include:
- Bruxism (grinding and clenching of the teeth)[8][15][22]
- Dehydration[15][64][72]
- Diarrhea[64]
- Erectile dysfunction[8][73]
- Hyperthermia[8][15][72]
- Increased wakefulness or insomnia[8][64]
- Increased perspiration and sweating[64][72]
- Increased heart rate and blood pressure[8][15][72]
- Increased psychomotor activity[8]
- Loss of appetite[8][62]
- Nausea and vomiting[22]
- Visual and auditory hallucinations (rarely)[8]
Other adverse effects that may occur or persist for up to a week following cessation of moderate MDMA use include:[62][22]
- Physiological
- Psychological
Long-term
[edit]As of 2015[update], the long-term effects of MDMA on human brain structure and function have not been fully determined.[76] However, there is consistent evidence of structural and functional deficits in MDMA users with high lifetime exposure.[76] These structural or functional changes appear to be dose dependent and may be less prominent in MDMA users with only a moderate (typically <50 doses used and <100 tablets consumed) lifetime exposure. Nonetheless, moderate MDMA use may still be neurotoxic and what constitutes moderate use is not clearly established.[77]
Furthermore, it is not clear yet whether "typical" recreational users of MDMA (1 to 2 pills of 75 to 125 mg MDMA or analogue every 1 to 4 weeks) will develop neurotoxic brain lesions.[78] Long-term exposure to MDMA in humans has been shown to produce marked neurodegeneration in striatal, hippocampal, prefrontal, and occipital serotonergic axon terminals.[76][79] Neurotoxic damage to serotonergic axon terminals has been shown to persist for more than two years.[79] Elevations in brain temperature from MDMA use are positively correlated with MDMA-induced neurotoxicity.[15][76][77] However, most studies on MDMA and serotonergic neurotoxicity in humans focus more on heavy users who consume as much as seven times or more the amount that most users report taking. The evidence for the presence of serotonergic neurotoxicity in casual users who take lower doses less frequently is not conclusive.[80]
However, adverse neuroplastic changes to brain microvasculature and white matter have been observed to occur in humans using low doses of MDMA.[15][76] Reduced gray matter density in certain brain structures has also been noted in human MDMA users.[15][76] Global reductions in gray matter volume, thinning of the parietal and orbitofrontal cortices, and decreased hippocampal activity have been observed in long term users.[8] The effects established so far for recreational use of ecstasy lie in the range of moderate to severe effects for serotonin transporter reduction.[81]
Impairments in multiple aspects of cognition, including attention, learning, memory, visual processing, and sleep, have been found in regular MDMA users.[8][22][82][76] The magnitude of these impairments is correlated with lifetime MDMA usage[22][82][76] and are partially reversible with abstinence.[8] Several forms of memory are impaired by chronic ecstasy use;[22][82] however, the effects for memory impairments in ecstasy users are generally small overall.[83][84] MDMA use is also associated with increased impulsivity and depression.[8]
Serotonin depletion following MDMA use can cause depression in subsequent days. In some cases, depressive symptoms persist for longer periods.[8] Some studies indicate repeated recreational use of ecstasy is associated with depression and anxiety, even after quitting the drug.[85] Depression is one of the main reasons for cessation of use.[8]
At high doses, MDMA induces a neuroimmune response that, through several mechanisms, increases the permeability of the blood–brain barrier, thereby making the brain more susceptible to environmental toxins and pathogens.[86][87][page needed] In addition, MDMA has immunosuppressive effects in the peripheral nervous system and pro-inflammatory effects in the central nervous system.[88]
MDMA may increase the risk of cardiac valvulopathy in heavy or long-term users due to activation of serotonin 5-HT2B receptors.[89][90] MDMA induces cardiac epigenetic changes in DNA methylation, particularly hypermethylation changes.[91]
Reinforcement disorders
[edit]Approximately 60% of MDMA users experience withdrawal symptoms when they stop taking MDMA.[62] Some of these symptoms include fatigue, loss of appetite, depression, and trouble concentrating.[62] Tolerance to some of the desired and adverse effects of MDMA is expected to occur with consistent MDMA use.[62] A 2007 delphic analysis of a panel of experts in pharmacology, psychiatry, law, policing and others estimated MDMA to have a psychological dependence and physical dependence potential roughly three-fourths to four-fifths that of cannabis.[92]
MDMA has been shown to induce ΔFosB in the nucleus accumbens.[93] Because MDMA releases dopamine in the striatum, the mechanisms by which it induces ΔFosB in the nucleus accumbens are analogous to other dopaminergic psychostimulants.[93][94] Therefore, chronic use of MDMA at high doses can result in altered brain structure and drug addiction that occur as a consequence of ΔFosB overexpression in the nucleus accumbens.[94] MDMA is less addictive than other stimulants such as methamphetamine and cocaine.[95][96] Compared with amphetamine, MDMA and its metabolite MDA are less reinforcing.[97]
One study found approximately 15% of chronic MDMA users met the DSM-IV diagnostic criteria for substance dependence.[98] However, there is little evidence for a specific diagnosable MDMA dependence syndrome because MDMA is typically used relatively infrequently.[40]
There are currently no medications to treat MDMA addiction.[99]
During pregnancy
[edit]MDMA is a moderately teratogenic drug (i.e., it is toxic to the fetus).[100][101] In utero exposure to MDMA is associated with a neuro- and cardiotoxicity[101] and impaired motor functioning. Motor delays may be temporary during infancy or long-term. The severity of these developmental delays increases with heavier MDMA use.[82][102] MDMA has been shown to promote the survival of fetal dopaminergic neurons in culture.[103]
Overdose
[edit]MDMA overdose symptoms vary widely due to the involvement of multiple organ systems. Some of the more overt overdose symptoms are listed in the table below. The number of instances of fatal MDMA intoxication is low relative to its usage rates. In most fatalities, MDMA was not the only drug involved. Acute toxicity is mainly caused by serotonin syndrome and sympathomimetic effects.[98] Sympathomimetic side effects can be managed with carvedilol.[104][105] MDMA's toxicity in overdose may be exacerbated by caffeine, with which it is frequently cut in order to increase volume.[106] A scheme for management of acute MDMA toxicity has been published focusing on treatment of hyperthermia, hyponatraemia, serotonin syndrome, and multiple organ failure.[107]
| System | Minor or moderate overdose[108] | Severe overdose[108] |
|---|---|---|
| Cardiovascular |
| |
| Central nervous system |
||
| Musculoskeletal |
| |
| Respiratory | ||
| Urinary | ||
| Other |
|
Interactions
[edit]A number of drug interactions can occur between MDMA and other drugs, including serotonergic drugs.[62][112] MDMA also interacts with drugs which inhibit CYP450 enzymes, like ritonavir (Norvir), particularly CYP2D6 inhibitors.[62] Life-threatening reactions and death have occurred in people who took MDMA while on ritonavir.[113] Bupropion, a strong CYP2D6 inhibitor, has been found to increase MDMA exposure with administration of MDMA.[114][115] Concurrent use of MDMA with certain other serotonergic drugs can result in a life-threatening condition called serotonin syndrome.[8][62] Severe overdose resulting in death has also been reported in people who took MDMA in combination with certain monoamine oxidase inhibitors (MAOIs),[8][62] such as phenelzine (Nardil), tranylcypromine (Parnate), or moclobemide (Aurorix, Manerix).[116] Serotonin reuptake inhibitors (SRIs) such as citalopram (Celexa), duloxetine (Cymbalta), fluoxetine (Prozac), and paroxetine (Paxil) have been shown to block most of the subjective effects of MDMA.[117] Norepinephrine reuptake inhibitors (NRIs) such as reboxetine (Edronax) have been found to reduce emotional excitation and feelings of stimulation with MDMA but do not appear to influence its entactogenic or mood-elevating effects.[117]
MDMA induces the release of monoamine neurotransmitters and thereby acts as an indirectly acting sympathomimetic and produces a variety of cardiostimulant effects.[114] It dose-dependently increases heart rate, blood pressure, and cardiac output.[114][118] SRIs like citalopram and paroxetine, as well as the serotonin 5-HT2A receptor antagonist ketanserin, have been found to partially block the increases in heart rate and blood pressure with MDMA.[114][119] It is notable in this regard that serotonergic psychedelics such as psilocybin, which act as serotonin 5-HT2A receptor agonists, likewise have sympathomimetic effects.[120][121][122] The NRI reboxetine and the serotonin–norepinephrine reuptake inhibitor (SNRI) duloxetine block MDMA-induced increases in heart rate and blood pressure.[114] Conversely, bupropion, a norepinephrine–dopamine reuptake inhibitor (NDRI) with only weak dopaminergic activity,[123][124] reduced MDMA-induced heart rate and circulating norepinephrine increases but did not affect MDMA-induced blood pressure increases.[114][115] On the other hand, the robust NDRI methylphenidate, which has sympathomimetic effects of its own, has been found to augment the cardiovascular effects and increases in circulating norepinephrine and epinephrine levels induced by MDMA.[114][125]
The non-selective beta blocker pindolol blocked MDMA-induced increases in heart rate but not blood pressure.[114][104][126] The α2-adrenergic receptor agonist clonidine did not affect the cardiovascular effects of MDMA, though it reduced blood pressure.[114][104][127] The α1-adrenergic receptor antagonists doxazosin and prazosin blocked or reduced MDMA-induced blood pressure increases but augmented MDMA-induced heart rate and cardiac output increases.[114][104][128][118] The dual α1- and β-adrenergic receptor blocker carvedilol reduced MDMA-induced heart rate and blood pressure increases.[114][104][105] In contrast to the cases of serotonergic and noradrenergic agents, the dopamine D2 receptor antagonist haloperidol did not affect the cardiovascular responses to MDMA.[114][129] Due to the theoretical risk of "unopposed α-stimulation" and possible consequences like coronary vasospasm, it has been suggested that dual α1- and β-adrenergic receptor antagonists like carvedilol and labetalol, rather than selective beta blockers, should be used in the management of stimulant-induced sympathomimetic toxicity, for instance in the context of overdose.[104][130]
Pharmacology
[edit]Pharmacodynamics
[edit]| Target | Affinity (Ki, nM) |
|---|---|
| SERT | 0.73–13,300 (Ki) 380–2,500 (IC50) 50–72 (EC50) (rat) |
| NET | 27,000–30,500 (Ki) 360–405 (IC50) 54–110 (EC50) (rat) |
| DAT | 6,500–>10,000 (Ki) 1,440–21,000 (IC50) 51–278 (EC50) (rat) |
| 5-HT1A | 6,300–12,200 (Ki) 36,000 nM (EC50) 64% (Emax) |
| 5-HT1B | >10,000 |
| 5-HT1D | >10,000 |
| 5-HT1E | >10,000 |
| 5-HT1F | ND |
| 5-HT2A | 4,600–>10,000 (Ki) 6,100–12,484 (EC50) 40–55% (Emax) |
| 5-HT2B | 500–2,000 (Ki) 2,000–>20,000 (EC50) 32% (Emax) |
| 5-HT2C | 4,400–>13,000 (Ki) 831–9,100 (EC50) 92% (Emax) |
| 5-HT3 | >10,000 |
| 5-HT4 | ND |
| 5-HT5A | >10,000 |
| 5-HT6 | >10,000 |
| 5-HT7 | >10,000 |
| α1A | 6,900–>10,000 |
| α1B | >10,000 |
| α1D | ND |
| α2A | 2,532–15,000 |
| α2B | 1,785 |
| α2C | 1,123–1,346 |
| β1, β2 | >10,000 |
| D1 | >13,600 |
| D2 | 25,200 |
| D3 | >17,700 |
| D4 | >10,000 |
| D5 | >10,000 |
| H1 | 2,138–>14,400 |
| H2 | >10,000 |
| H3, H4 | ND |
| M1 | >10,000 |
| M2 | >10,000 |
| M3 | 1,850–>10,000 |
| M4 | 8,250–>10,000 |
| M5 | 6,340–>10,000 |
| nACh | >10,000 |
| TAAR1 | 250–370 (Ki) (rat) 1,000–1,700 (EC50) (rat) 56% (Emax) (rat) 2,400–3,100 (Ki) (mouse) 4,000 (EC50) (mouse) 71% (Emax) (mouse) 35,000 (EC50) (human) 26% (Emax) (human) |
| I1 | 220 |
| σ1, σ2 | ND |
| Notes: The smaller the value, the more avidly the drug binds to the site. Proteins are human unless otherwise specified. Refs:[131][132][17][133][134][135] [136][137][138][139][140][141] | |
MDMA is an entactogen or empathogen, as well as a stimulant, euphoriant, and weak psychedelic.[17][142] It is a substrate of the monoamine transporters (MATs) and acts as a monoamine releasing agent (MRA).[17][143][144][145] The drug is specifically a well-balanced serotonin–norepinephrine–dopamine releasing agent (SNDRA).[17][143][144][145] To a lesser extent, MDMA also acts as a serotonin–norepinephrine–dopamine reuptake inhibitor (SNDRI).[17][143][144] MDMA enters monoaminergic neurons via the MATs and then, via poorly understood mechanisms, reverses the direction of these transporters to produce efflux of the monoamine neurotransmitters rather than the usual reuptake.[17][146][147][148] Induction of monoamine efflux by amphetamines in general may involve intracellular Na+ and Ca2+ elevation and PKC and CaMKIIα activation.[146][147][148] MDMA also acts on the vesicular monoamine transporter 2 (VMAT2) on synaptic vesicles to increase the cytosolic concentrations of the monoamine neurotransmitters available for efflux.[17][143] By inducing release and reuptake inhibition of serotonin, norepinephrine, and dopamine, MDMA increases levels of these neurotransmitters in the brain and periphery.[17][143]
In addition to its actions as an SNDRA, MDMA directly but more modestly interacts with a number of monoamine and other receptors.[17][131][132][133][149] It is a low-potency partial agonist of the serotonin 5-HT2 receptors, including of the serotonin 5-HT2A, 5-HT2B, and 5-HT2C receptors.[17][150][151][152][149] The drug also interacts with α2-adrenergic receptors, with the sigma σ1 and σ2 receptors, and with the imidazoline I1 receptor.[17][131][132][133] Along with the preceding receptor interactions, MDMA is a potent partial agonist of the rodent trace amine-associated receptor 1 (TAAR1).[139][140] Conversely however, due to species differences, it is far weaker in terms of potency as an agonist of the human TAAR1.[17][139][140][153] Moreover, MDMA appears to act as a weak partial agonist of the human TAAR1 rather than as an efficacious agonist.[139][140] In relation to the preceding findings, MDMA has been said to be essentially inactive as a human TAAR1 agonist.[17] TAAR1 activation is thought to auto-inhibit and constrain the effects of amphetamines that possess TAAR1 agonism, for instance MDMA in rodents.[143][154][155][134][156]
Elevation of serotonin, norepinephrine, and dopamine levels by MDMA is believed to mediate most of the drug's effects, including its entactogenic, stimulant, euphoriant, hyperthermic, and sympathomimetic effects.[17][143][157][71] The entactogenic effects of MDMA, including increased sociability, empathy, feelings of closeness, and reduced aggression, are thought to be mainly due to induction of serotonin release.[71][117][18] The exact serotonin receptors responsible for MDMA's entactogenic effects are unclear, but may include the serotonin 5-HT1A receptor,[158] 5-HT1B receptor,[159] and 5-HT2A receptor,[160] as well as 5-HT1A receptor-mediated oxytocin release and consequent activation of the oxytocin receptor.[17][71][161][162][142] Induction of dopamine release is thought to be importantly involved in the stimulant and euphoriant effects of MDMA,[17][150][163] while induction of norepinephrine release and serotonin 5-HT2A receptor stimulation are believed to mediate its sympathomimetic effects.[114][143] Activation of serotonin 5-HT1B and 5-HT2A receptors is also thought to be involved in the stimulant and euphoriant effects of MDMA, while serotonin 5-HT2C receptor activation is thought to constrain these effects and limit MDMA's reinforcing potential.[164][165][166][167][168][169] Serotonin 5-HT2B receptor signaling appears to be required for MDMA-induced serotonin release and effects.[170][171][172][173][174] MDMA has been associated with a unique subjective "magic" or euphoria that few or no other known entactogens are said to fully reproduce.[175][176] The mechanisms underlying this property of MDMA are unknown, but it has been theorized to be due to a specific mixture and balance of pharmacological activities, including combined serotonin, norepinephrine, and dopamine release and direct serotonin receptor agonism.[177][175][176][178]
MDMA is often said to have mild or weak psychedelic effects.[179][117][18][180] These effects are said to be dose-dependent, such that greater hallucinogenic effects are produced at higher doses.[179][181] The mild hallucinogenic effects of MDMA include perceptual changes like intensification of visual, auditory, and tactile perception (e.g., brightened colors), a state of dissociation with feelings of depersonalization and derealization (e.g., "oceanic boundlessness"), and thinking disturbances.[179][182][117][180][119][183][181] Conversely, overt hallucinations do not occur, MDMA's hallucinogenic effects are described as "non-problematic" for users, and are said to be less than those of 3,4-methylenedioxyamphetamine (MDA) or especially those of serotonergic psychedelics like psilocybin.[182][119][18] The hallucinogenic effects of MDMA have been theorized to be mediated by serotonin 5-HT2A receptor activation analogously to the case of classical psychedelics.[179][119][181][184][182][16] Accordingly, the serotonin 5-HT2A receptor antagonist ketanserin has been reported to reduce MDMA-induced perceptual changes in humans.[179][117][119][181] Conversely however, it failed to affect MDMA-induced feelings of dissociation and oceanic boundlessness.[179][117][181] In contrast, the serotonin reuptake inhibitor citalopram, which blocks MDMA-induced serotonin release, diminished all of the psychoactive and hallucinogenic effects of MDMA.[179][117][183][119] It has been noted that N-methylation of psychedelic phenethylamines, as in the structural difference between MDA and MDMA, has invariably greatly reduced or abolished their psychedelic activity.[185][186] Whereas MDA and psychedelics like psilocybin induce the head-twitch response in rodents, a behavioral proxy of psychedelic effects, findings on MDMA and the head-twitch response are mixed and conflicting.[187][188][117] In addition, whereas MDA fully substitutes for psychedelics like LSD and DOM in rodent drug discrimination tests, MDMA does not do so, nor do psychedelics generally fully substitute for MDMA.[189][117][190][191]
Long-term repeated activation of serotonin 5-HT2B receptors by MDMA is thought to result in increased risk of organ complications such as valvular heart disease (VHD) and primary pulmonary hypertension (PPH).[192][193][120][194][177][195] MDMA has been associated with serotonergic neurotoxicity.[196][18][197] This may be due to formation of toxic MDMA metabolites and/or induction of simultaneous serotonin and dopamine release, with consequent uptake of dopamine into serotonergic neurons and breakdown into toxic species.[196][18][197] Serotonin 5-HT2 receptor agonists or serotonergic psychedelics may potentiate the neurotoxicity of MDMA.[198][199][200][201]
MDMA is a racemic mixture of two enantiomers, (S)-MDMA and (R)-MDMA.[150][16] (S)-MDMA is much more potent as an SNDRA in vitro and in producing MDMA-like subjective effects in humans than (R)-MDMA.[150][145][16][202] By contrast, (R)-MDMA acts as a lower-potency serotonin–norepinephrine releasing agent (SNRA) with weak or negligible effects on dopamine.[150][145][203] Relatedly, (R)-MDMA shows weak or negligible stimulant-like and rewarding effects in animals.[150][204] Both (S)-MDMA and (R)-MDMA produce entactogen-type effects in animals and humans.[150][16] In addition, both (S)-MDMA and (R)-MDMA are weak agonists of the serotonin 5-HT2 receptors.[150][163][16][151][152] (R)-MDMA is more potent and efficacious as a serotonin 5-HT2A and 5-HT2B receptor agonist than (S)-MDMA, whereas (S)-MDMA is somewhat more potent as an agonist of the serotonin 5-HT2C receptor.[150][163][16] Due to it being a more potent serotonin 5-HT2A receptor agonist than (S)-MDMA, (R)-MDMA has been hypothesized to have greater psychedelic effects than (S)-MDMA or racemic MDMA.[205][16] However, this proved not to be the case in a direct clinical comparison of (R)-MDMA, (S)-MDMA, and racemic MDMA, with equivalent hallucinogen-like effects instead found between the three interventions.[205][16]
MDMA produces MDA as a minor active metabolite.[108] Peak levels of MDA are about 5 to 10% of those of MDMA and total exposure to MDA is almost 10% of that of MDMA with oral MDMA administration.[108][193] As a result, MDA may contribute to some extent to the effects of MDMA.[108][184] MDA is an entactogen, stimulant, and weak psychedelic similarly to MDMA.[18] Like MDMA, it acts as a potent and well-balanced SNDRA and as a weak serotonin 5-HT2 receptor agonist.[145][151][152] However, MDA shows much more potent and efficacious serotonin 5-HT2A, 5-HT2B, and 5-HT2C receptor agonism than MDMA.[163][184][152][151] Accordingly, MDA produces greater psychedelic effects than MDMA in humans[18] and might particularly contribute to the mild psychedelic-like effects of MDMA.[184] On the other hand, MDA may also be importantly involved in toxicity of MDMA, such as cardiac valvulopathy.[206][193][151]
The duration of action of MDMA (3–6 hours) is much shorter than its elimination half-life (8–9 hours) would imply.[207] In relation to this, MDMA's duration and the offset of its effects appear to be determined more by rapid acute tolerance rather than by circulating drug concentrations.[43] Similar findings have been made for amphetamine and methamphetamine.[208][209][210][211] One mechanism by which tolerance to MDMA may occur is internalization of the serotonin transporter (SERT).[212][213][214][215][216] Although MDMA and serotonin are not significant TAAR1 agonists in humans, TAAR1 activation by MDMA may result in SERT internalization, for instance in rodents in whom MDMA is a potent TAAR1 agonist.[215][216][217][139] It is thought that brain serotonin levels are depleted after MDMA administration but that levels typically return to normal within 24 to 48 hours.[8]
| Compound | Serotonin | Norepinephrine | Dopamine |
|---|---|---|---|
| Amphetamine | ND | ND | ND |
| (S)-Amphetamine (d) | 698–1,765 | 6.6–7.2 | 5.8–24.8 |
| (R)-Amphetamine (l) | ND | 9.5 | 27.7 |
| Methamphetamine | ND | ND | ND |
| (S)-Methamphetamine (d) | 736–1,292 | 12.3–13.8 | 8.5–24.5 |
| (R)-Methamphetamine (l) | 4,640 | 28.5 | 416 |
| MDA | 160 | 108 | 190 |
| MDMA | 49.6–72 | 54.1–110 | 51.2–278 |
| (S)-MDMA (d) | 74 | 136 | 142 |
| (R)-MDMA (l) | 340 | 560 | 3,700 |
| MDEA | 47 | 2,608 | 622 |
| MBDB | 540 | 3,300 | >100,000 |
| MDAI | 114 | 117 | 1,334 |
| Notes: The smaller the value, the more strongly the drug releases the neurotransmitter. The assays were done in rat brain synaptosomes and human potencies may be different. See also Monoamine releasing agent § Activity profiles for a larger table with more compounds. Refs:[145][151][218][219][220][221][222][223][17] | |||
| Compound | 5-HT2A | 5-HT2B | 5-HT2C | |||
|---|---|---|---|---|---|---|
| EC50 (nM) | Emax | EC50 (nM) | Emax | EC50 (nM) | Emax | |
| Serotonin | 53 | 92% | 1.0 | 100% | 22 | 91% |
| MDA | 1,700 | 57% | 190 | 80% | ND | ND |
| (S)-MDA (d) | 18,200 | 89% | 100 | 81% | 7,400 | 73% |
| (R)-MDA (l) | 5,600 | 95% | 150 | 76% | 7,400 | 76% |
| MDMA | 6,100 | 55% | 2,000–>20,000 | 32% | ND | ND |
| (S)-MDMA (d) | 10,300 | 9% | 6,000 | 38% | 2,600 | 53% |
| (R)-MDMA (l) | 3,100 | 21% | 900 | 27% | 5,400 | 27% |
| Notes: The smaller the Kact or EC50 value, the more strongly the compound produces the effect. Refs:[152][151][224] | ||||||
Pharmacokinetics
[edit]Absorption
[edit]The MDMA concentration in the bloodstream starts to rise after about 30 minutes,[225] and reaches its maximal concentration between 1.5 and 3 hours after oral administration.[226] It is then slowly metabolized and excreted, with levels of MDMA and its metabolites decreasing to half their peak concentration over the next several hours.[227] The duration of action of MDMA is about 3 to 6 hours.[18]
Distribution
[edit]The plasma protein binding of MDMA is unknown.[14]
Metabolism
[edit]
Metabolites of MDMA that have been identified in humans include 3,4-methylenedioxyamphetamine (MDA), 4-hydroxy-3-methoxymethamphetamine (HMMA), 4-hydroxy-3-methoxyamphetamine (HMA), 3,4-dihydroxyamphetamine (DHA) (also called alpha-methyldopamine (α-Me-DA)), 3,4-methylenedioxyphenylacetone (MDP2P), and 3,4-methylenedioxy-N-hydroxyamphetamine (MDOH). The contributions of these metabolites to the psychoactive and toxic effects of MDMA are an area of active research. 80% of MDMA is metabolised in the liver, and about 20% is excreted unchanged in the urine.[15]
MDMA is known to be metabolized by two main metabolic pathways: (1) O-demethylenation followed by catechol-O-methyltransferase (COMT)-catalyzed methylation or glucuronide/sulfate conjugation; and (2) N-dealkylation, deamination, and oxidation to the corresponding benzoic acid derivatives conjugated with glycine.[108] The metabolism may be primarily by cytochrome P450 (CYP450) enzymes CYP2D6 and CYP3A4 and COMT. Complex, nonlinear pharmacokinetics arise via autoinhibition of CYP2D6 and CYP2D8, resulting in zeroth order kinetics at higher doses. It is thought that this can result in sustained and higher concentrations of MDMA if the user takes consecutive doses of the drug.[228][non-primary source needed]
Elimination
[edit]MDMA and metabolites are primarily excreted as conjugates, such as sulfates and glucuronides.[229] MDMA is a chiral compound and has been almost exclusively administered as a racemate. However, the two enantiomers have been shown to exhibit different kinetics. The disposition of MDMA may also be stereoselective, with the S-enantiomer having a shorter elimination half-life and greater excretion than the R-enantiomer. Evidence suggests[230] that the area under the blood plasma concentration versus time curve (AUC) was two to four times higher for the (R)-enantiomer than the (S)-enantiomer after a 40 mg oral dose in human volunteers. Likewise, the plasma half-life of (R)-MDMA was significantly longer than that of the (S)-enantiomer (5.8 ± 2.2 hours vs 3.6 ± 0.9 hours).[62] However, because MDMA excretion and metabolism have nonlinear kinetics,[231] the half-lives would be higher at more typical doses (100 mg is sometimes considered a typical dose).[226]
Chemistry
[edit]Reactors used to synthesize MDMA on an industrial scale in a clandestine chemical factory in Cikande, Indonesia |
MDMA is in the substituted methylenedioxyphenethylamine and substituted amphetamine classes of chemicals. As a free base, MDMA is a colorless oil insoluble in water.[10] The most common salt of MDMA is the hydrochloride salt;[10] pure MDMA hydrochloride is water-soluble and appears as a white or off-white powder or crystal.[10]
Synthesis
[edit]There are numerous methods available to synthesize MDMA via different intermediates.[232][233][234][235] The original MDMA synthesis described in Merck's patent involves brominating safrole to 1-(3,4-methylenedioxyphenyl)-2-bromopropane and then reacting this adduct with methylamine.[236][237] Most illicit MDMA is synthesized using MDP2P (3,4-methylenedioxyphenyl-2-propanone) as a precursor. MDP2P in turn is generally synthesized from piperonal, safrole or isosafrole.[238] One method is to isomerize safrole to isosafrole in the presence of a strong base, and then oxidize isosafrole to MDP2P. Another method uses the Wacker process to oxidize safrole directly to the MDP2P intermediate with a palladium catalyst. Once the MDP2P intermediate has been prepared, a reductive amination leads to racemic MDMA (an equal parts mixture of (R)-MDMA and (S)-MDMA).[citation needed] Relatively small quantities of essential oil are required to make large amounts of MDMA. The essential oil of Ocotea cymbarum, for example, typically contains between 80 and 94% safrole. This allows 500 mL of the oil to produce between 150 and 340 grams of MDMA.[239]
Detection in body fluids
[edit]MDMA and MDA may be quantitated in blood, plasma or urine to monitor for use, confirm a diagnosis of poisoning or assist in the forensic investigation of a traffic or other criminal violation or a sudden death. Some drug abuse screening programs rely on hair, saliva, or sweat as specimens. Most commercial amphetamine immunoassay screening tests cross-react significantly with MDMA or its major metabolites, but chromatographic techniques can easily distinguish and separately measure each of these substances. The concentrations of MDA in the blood or urine of a person who has taken only MDMA are, in general, less than 10% those of the parent drug.[228][240][241]
History
[edit]Early research and use
[edit]MDMA was first synthesized and patented in 1912 by Merck chemist Anton Köllisch.[242][243] At the time, Merck was interested in developing substances that stopped abnormal bleeding. Merck wanted to avoid an existing patent held by Bayer for one such compound: hydrastinine. Köllisch developed a preparation of a hydrastinine analogue, methylhydrastinine, at the request of fellow lab members, Walther Beckh and Otto Wolfes. MDMA (called methylsafrylamin, safrylmethylamin or N-Methyl-a-Methylhomopiperonylamin in Merck laboratory reports) was an intermediate compound in the synthesis of methylhydrastinine. Merck was not interested in MDMA itself at the time.[243] On 24 December 1912, Merck filed two patent applications that described the synthesis and some chemical properties of MDMA[244] and its subsequent conversion to methylhydrastinine.[245] Merck records indicate its researchers returned to the compound sporadically. A 1920 Merck patent describes a chemical modification to MDMA.[242][246]
MDMA's analogue 3,4-methylenedioxyamphetamine (MDA) was first synthesized in 1910 as a derivative of adrenaline.[242] Gordon A. Alles, the discoverer of the psychoactive effects of amphetamine, also discovered the psychoactive effects of MDA in 1930 in a self-experiment in which he administered a high dose (126 mg) to himself.[242][247][248] However, he did not subsequently describe these effects until 1959.[249][247][248] MDA was later tested as an appetite suppressant by Smith, Kline & French and for other uses by other groups in the 1950s.[242] In relation to the preceding, the psychoactive effects of MDA were discovered well before those of MDMA.[242][249]
In 1927, Max Oberlin studied the pharmacology of MDMA while searching for substances with effects similar to adrenaline or ephedrine, the latter being structurally similar to MDMA. Compared to ephedrine, Oberlin observed that it had similar effects on vascular smooth muscle tissue, stronger effects at the uterus, and no "local effect at the eye". MDMA was also found to have effects on blood sugar levels comparable to high doses of ephedrine. Oberlin concluded that the effects of MDMA were not limited to the sympathetic nervous system. Research was stopped "particularly due to a strong price increase of safrylmethylamine", which was still used as an intermediate in methylhydrastinine synthesis. Albert van Schoor performed simple toxicological tests with the drug in 1952, most likely while researching new stimulants or circulatory medications. After pharmacological studies, research on MDMA was not continued. In 1959, Wolfgang Fruhstorfer synthesized MDMA for pharmacological testing while researching stimulants. It is unclear if Fruhstorfer investigated the effects of MDMA in humans.[243]
Outside of Merck, other researchers began to investigate MDMA. In 1953 and 1954, the United States Army commissioned a study of toxicity and behavioral effects in animals injected with mescaline and several analogues, including MDMA. Conducted at the University of Michigan in Ann Arbor, these investigations were declassified in October 1969 and published in 1973.[250][249] A 1960 Polish paper by Biniecki and Krajewski describing the synthesis of MDMA as an intermediate was the first published scientific paper on the substance.[243][249][251]
MDA appeared as a recreational drug in the mid-1960s.[242] MDMA may have been in non-medical use in the western United States in 1968.[242][252] An August 1970 report at a meeting of crime laboratory chemists indicates MDMA was being used recreationally in the Chicago area by 1970.[249][253] MDMA likely emerged as a substitute for MDA,[254] a drug at the time popular among users of psychedelics[255] which was made a Schedule 1 controlled substance in the United States in 1970.[256][257]
Shulgin's research
[edit]
American chemist and psychopharmacologist Alexander Shulgin reported he synthesized MDMA in 1965 while researching methylenedioxy compounds at Dow Chemical Company, but did not test the psychoactivity of the compound at this time. Around 1970, Shulgin sent instructions for N-methylated MDA (MDMA) synthesis to the founder of a Los Angeles chemical company who had requested them. This individual later provided these instructions to a client in the Midwest. Shulgin may have suspected he played a role in the emergence of MDMA in Chicago.[249]
Shulgin first heard of the psychoactive effects of N-methylated MDA around 1975 from a young student who reported "amphetamine-like content".[249] Around 30 May 1976, Shulgin again heard about the effects of N-methylated MDA,[249] this time from a graduate student in a medicinal chemistry group he advised at San Francisco State University[255][258] who directed him to the University of Michigan study.[259] She and two close friends had consumed 100 mg of MDMA and reported positive emotional experiences.[249] Following the self-trials of a colleague at the University of San Francisco, Shulgin synthesized MDMA and tried it himself in September and October 1976.[249][255] Shulgin first reported on MDMA in a presentation at a conference in Bethesda, Maryland in December 1976.[249] In 1978, he and David E. Nichols published a report on the drug's psychoactive effect in humans.[242] They described MDMA as inducing "an easily controlled altered state of consciousness with emotional and sensual overtones" comparable "to marijuana, to psilocybin devoid of the hallucinatory component, or to low levels of MDA".[260]
While not finding his own experiences with MDMA particularly powerful,[259][261] Shulgin was impressed with the drug's disinhibiting effects and thought it could be useful in therapy.[261] Believing MDMA allowed users to strip away habits and perceive the world clearly, Shulgin called the drug window.[259][262] Shulgin occasionally used MDMA for relaxation, referring to it as "my low-calorie martini", and gave the drug to friends, researchers, and others who he thought could benefit from it.[259] One such person was Leo Zeff, a psychotherapist who had been known to use psychedelic substances in his practice. When he tried the drug in 1977, Zeff was impressed with the effects of MDMA and came out of his semi-retirement to promote its use in therapy. Over the following years, Zeff traveled around the United States and occasionally to Europe, eventually training an estimated four thousand psychotherapists in the therapeutic use of MDMA.[261][263] Zeff named the drug Adam, believing it put users in a state of primordial innocence.[255]
Psychotherapists who used MDMA believed the drug eliminated the typical fear response and increased communication. Sessions were usually held in the home of the patient or the therapist. The role of the therapist was minimized in favor of patient self-discovery accompanied by MDMA induced feelings of empathy. Depression, substance use disorders, relationship problems, premenstrual syndrome, and autism were among several psychiatric disorders MDMA assisted therapy was reported to treat.[257] According to psychiatrist George Greer, therapists who used MDMA in their practice were impressed by the results. Anecdotally, MDMA was said to greatly accelerate therapy.[261] According to David Nutt, MDMA was widely used in the western US in couples counseling, and was called empathy. Only later was the term ecstasy used for it, coinciding with rising opposition to its use.[264][265]
Rising recreational use
[edit]In the late 1970s and early 1980s, "Adam" spread through personal networks of psychotherapists, psychiatrists, users of psychedelics, and yuppies. Hoping MDMA could avoid criminalization like LSD and mescaline, psychotherapists and experimenters attempted to limit the spread of MDMA and information about it while conducting informal research.[257][266] Early MDMA distributors were deterred from large scale operations by the threat of possible legislation.[267] Between the 1970s and the mid-1980s, this network of MDMA users consumed an estimated 500,000 doses.[22][268]
A small recreational market for MDMA developed by the late 1970s,[269] consuming perhaps 10,000 doses in 1976.[256] By the early 1980s MDMA was being used in Boston and New York City nightclubs such as Studio 54 and Paradise Garage.[270][271] Into the early 1980s, as the recreational market slowly expanded, production of MDMA was dominated by a small group of therapeutically minded Boston chemists. Having commenced production in 1976, this "Boston Group" did not keep up with growing demand and shortages frequently occurred.[267]
Perceiving a business opportunity, Michael Clegg, the Southwest distributor for the Boston Group, started his own "Texas Group" backed financially by Texas friends.[267][272] In 1981,[267] Clegg had coined "Ecstasy" as a slang term for MDMA to increase its marketability.[262][266] Starting in 1983,[267] the Texas Group mass-produced MDMA in a Texas lab[266] or imported it from California[262] and marketed tablets using pyramid sales structures and toll-free numbers.[268] MDMA could be purchased via credit card and taxes were paid on sales.[267] Under the brand name "Sassyfras", MDMA tablets were sold in brown bottles.[266] The Texas Group advertised "Ecstasy parties" at bars and discos, describing MDMA as a "fun drug" and "good to dance to".[267] MDMA was openly distributed in Austin and Dallas–Fort Worth area bars and nightclubs, becoming popular with yuppies, college students, and gays.[254][267][268]
Recreational use also increased after several cocaine dealers switched to distributing MDMA following experiences with the drug.[268] A California laboratory that analyzed confidentially submitted drug samples first detected MDMA in 1975. Over the following years the number of MDMA samples increased, eventually exceeding the number of MDA samples in the early 1980s.[273][274] By the mid-1980s, MDMA use had spread to colleges around the United States.[267]: 33
Media attention and scheduling
[edit]United States
[edit]
In an early media report on MDMA published in 1982, a Drug Enforcement Administration (DEA) spokesman stated the agency would ban the drug if enough evidence for abuse could be found.[267] By mid-1984, MDMA use was becoming more noticed. Bill Mandel reported on "Adam" in a 10 June San Francisco Chronicle article, but misidentified the drug as methyloxymethylenedioxyamphetamine (MMDA). In the next month, the World Health Organization identified MDMA as the only substance out of twenty phenethylamines to be seized a significant number of times.[266]
After a year of planning and data collection, MDMA was proposed for scheduling by the DEA on 27 July 1984, with a request for comments and objections.[266][275] The DEA was surprised when a number of psychiatrists, psychotherapists, and researchers objected to the proposed scheduling and requested a hearing.[257] In a Newsweek article published the next year, a DEA pharmacologist stated that the agency had been unaware of its use among psychiatrists.[276] An initial hearing was held on 1 February 1985 at the DEA offices in Washington, D.C., with administrative law judge Francis L. Young presiding.[266] It was decided there to hold three more hearings that year: Los Angeles on 10 June, Kansas City, Missouri on 10–11 July, and Washington, D.C., on 8–11 October.[257][266]
Sensational media attention was given to the proposed criminalization and the reaction of MDMA proponents, effectively advertising the drug.[257] In response to the proposed scheduling, the Texas Group increased production from 1985 estimates of 30,000 tablets a month to as many as 8,000 per day, potentially making two million ecstasy tablets in the months before MDMA was made illegal.[277] By some estimates the Texas Group distributed 500,000 tablets per month in Dallas alone.[262] According to one participant in an ethnographic study, the Texas Group produced more MDMA in eighteen months than all other distribution networks combined across their entire histories.[267] By May 1985, MDMA use was widespread in California, Texas, southern Florida, and the northeastern United States.[252][278] According to the DEA there was evidence of use in twenty-eight states[279] and Canada.[252] Urged by Senator Lloyd Bentsen, the DEA announced an emergency Schedule I classification of MDMA on 31 May 1985. The agency cited increased distribution in Texas, escalating street use, and new evidence of MDA (an analog of MDMA) neurotoxicity as reasons for the emergency measure.[278][280][281] The ban took effect one month later on 1 July 1985[277] in the midst of Nancy Reagan's "Just Say No" campaign.[282][283]
As a result of several expert witnesses testifying that MDMA had an accepted medical usage, the administrative law judge presiding over the hearings recommended that MDMA be classified as a Schedule III substance. Despite this, DEA administrator John C. Lawn overruled and classified the drug as Schedule I.[257][284] Harvard psychiatrist Lester Grinspoon then sued the DEA, claiming that the DEA had ignored the medical uses of MDMA, and the federal court sided with Grinspoon, calling Lawn's argument "strained" and "unpersuasive", and vacated MDMA's Schedule I status.[285] Despite this, less than a month later Lawn reviewed the evidence and reclassified MDMA as Schedule I again, claiming that the expert testimony of several psychiatrists claiming over 200 cases where MDMA had been used in a therapeutic context with positive results could be dismissed because they were not published in medical journals.[257] In 2017, the FDA granted breakthrough therapy designation for its use with psychotherapy for PTSD. However, this designation has been questioned and problematized.[286]
United Nations
[edit]While engaged in scheduling debates in the United States, the DEA also pushed for international scheduling.[277] In 1985, the World Health Organization's Expert Committee on Drug Dependence recommended that MDMA be placed in Schedule I of the 1971 United Nations Convention on Psychotropic Substances. The committee made this recommendation on the basis of the pharmacological similarity of MDMA to previously scheduled drugs, reports of illicit trafficking in Canada, drug seizures in the United States, and lack of well-defined therapeutic use. While intrigued by reports of psychotherapeutic uses for the drug, the committee viewed the studies as lacking appropriate methodological design and encouraged further research. Committee chairman Paul Grof dissented, believing international control was not warranted at the time and a recommendation should await further therapeutic data.[287] The Commission on Narcotic Drugs added MDMA to Schedule I of the convention on 11 February 1986.[288]
Post-scheduling
[edit]
The use of MDMA in Texas clubs declined rapidly after criminalization, but by 1991, the drug became popular among young middle-class whites and in nightclubs.[267] In 1985, MDMA use became associated with acid house on the Spanish island of Ibiza.[267]: 50 [289] Thereafter, in the late 1980s, the drug spread alongside rave culture to the United Kingdom and then to other European and American cities.[267]: 50 Illicit MDMA use became increasingly widespread among young adults in universities and later, in high schools. Since the mid-1990s, MDMA has become the most widely used amphetamine-type drug by college students and teenagers.[290]: 1080 MDMA became one of the four most widely used illicit drugs in the US, along with cocaine, heroin, and cannabis.[262] According to some estimates as of 2004, only marijuana attracts more first time users in the United States.[262]
After MDMA was criminalized, most medical use stopped, although some therapists continued to prescribe the drug illegally. Later,[when?] Charles Grob initiated an ascending-dose safety study in healthy volunteers. Subsequent FDA-approved MDMA studies in humans have taken place in the United States in Detroit (Wayne State University), Chicago (University of Chicago), San Francisco (UCSF and California Pacific Medical Center), Baltimore (NIDA–NIH Intramural Program), and South Carolina. Studies have also been conducted in Switzerland (University Hospital of Psychiatry, Zürich), the Netherlands (Maastricht University), and Spain (Universitat Autònoma de Barcelona).[291]
"Molly", short for 'molecule', was recognized as a slang term for crystalline or powder MDMA in the 2000s.[292][293]
In 2010, the BBC reported that use of MDMA had decreased in the UK in previous years. This may be due to increased seizures during use and decreased production of the precursor chemicals used to manufacture MDMA. Unwitting substitution with other drugs, such as mephedrone and methamphetamine,[294] as well as legal alternatives to MDMA, such as BZP, MDPV, and methylone, are also thought to have contributed to its decrease in popularity.[295]
In 2017, it was found that some pills being sold as MDMA contained pentylone, which can cause very unpleasant agitation and paranoia.[296]
According to David Nutt, when safrole was restricted by the United Nations in order to reduce the supply of MDMA, producers in China began using anethole instead, but this gives para-methoxyamphetamine (PMA, also known as "Dr Death"), which is much more toxic than MDMA and can cause overheating, muscle spasms, seizures, unconsciousness, and death. People wanting MDMA are sometimes sold PMA instead.[264]
In 2025, the BBC reported on a study of 650 survivors from the Nova music festival massacre. Two-thirds were under the influence of recreational drugs (MDMA, LSD, marijuana or psilocybin) when Hamas attacked the festival on October 7, 2023. MDMA appeared to have a protective effect against later problems with sleeping and emotional distress.[297][298]
Society and culture
[edit]| Substance | Best estimate |
Low estimate |
High estimate |
|---|---|---|---|
| Amphetamine- type stimulants |
34.16 | 13.42 | 55.24 |
| Cannabis | 192.15 | 165.76 | 234.06 |
| Cocaine | 18.20 | 13.87 | 22.85 |
| Ecstasy | 20.57 | 8.99 | 32.34 |
| Opiates | 19.38 | 13.80 | 26.15 |
| Opioids | 34.26 | 27.01 | 44.54 |
Legal status
[edit]MDMA is legally controlled in most of the world under the UN Convention on Psychotropic Substances and other international agreements, although exceptions exist for research and limited medical use. In general, the unlicensed use, sale or manufacture of MDMA are all criminal offences.
Australia
[edit]In Australia, MDMA was rescheduled on 1 July 2023 as a schedule 8 substance (available on prescription) when used in the treatment of PTSD, while remaining a schedule 9 substance (prohibited) for all other uses. For the treatment of PTSD, MDMA can only be prescribed by psychiatrists with specific training and authorisation.[300] In 1986, MDMA was declared an illegal substance because of its allegedly harmful effects and potential for misuse.[301] Any non-authorised sale, use or manufacture is strictly prohibited by law. Permits for research uses on humans must be approved by a recognized ethics committee on human research.
In Western Australia under the Misuse of Drugs Act 1981 4.0g of MDMA is the amount required determining a court of trial, 2.0g is considered a presumption with intent to sell or supply and 28.0g is considered trafficking under Australian law.[302]
The Australian Capital Territory passed legislation to decriminalise the possession of small amounts of MDMA, which took effect in October 2023.[303][304]
Canada
[edit]In Canada, MDMA is listed as a Schedule 1[305] as it is an analogue of amphetamine.[306] The Controlled Drugs and Substances Act was updated as a result of the Safe Streets and Communities Act changing amphetamines from Schedule III to Schedule I in March 2012. In 2022, the federal government granted British Columbia a 3-year exemption, legalizing the possession of up to 2.5 grams (0.088 oz) of MDMA in the province from February 2023 until February 2026.[307][308]
Finland
[edit]Scheduled in the "government decree on substances, preparations and plants considered to be narcotic drugs".[309] Ecstasy is considered a very dangerous illegal drug.[310]
Netherlands
[edit]In 2024, a Dutch state commission issued a report advocating for MDMA to be made available to patients with PTSD.[311]
In June 2011, the Expert Committee on the List (Expertcommissie Lijstensystematiek Opiumwet) issued a report which discussed the evidence for harm and the legal status of MDMA, arguing in favor of maintaining it on List I.[312][313][314]
United Kingdom
[edit]In the United Kingdom, MDMA was made illegal in 1977 by a modification order to the existing Misuse of Drugs Act 1971. Although MDMA was not named explicitly in this legislation, the order extended the definition of Class A drugs to include various ring-substituted phenethylamines.[315][316] The drug is therefore illegal to sell, buy, or possess without a licence in the UK. Penalties include a maximum of seven years and/or unlimited fine for possession; life and/or unlimited fine for production or trafficking.
Some researchers such as David Nutt have criticized the scheduling of MDMA, which he determined to be a relatively harmless drug.[317][318] An editorial he wrote in the Journal of Psychopharmacology, where he compared the risk of harm for horse riding (1 adverse event in 350) to that of ecstasy (1 in 10,000) resulted in his dismissal, leading to the resignation of several of his colleagues from the ACMD.[319]
United States
[edit]In the United States, MDMA is listed in Schedule I of the Controlled Substances Act.[320] In a 2011 federal court hearing, the American Civil Liberties Union successfully argued that the sentencing guideline for MDMA/ecstasy is based on outdated science, leading to excessive prison sentences.[321] Other courts have upheld the sentencing guidelines. The United States District Court for the Eastern District of Tennessee explained its ruling by noting that "an individual federal district court judge simply cannot marshal resources akin to those available to the Commission for tackling the manifold issues involved with determining a proper drug equivalency."[312]
Demographics
[edit]
In 2014, 3.5% of 18-to-25-year-olds had used MDMA in the United States.[8] In the European Union as of 2018, 4.1% of adults (15–64 years old) have used MDMA at least once in their life, and 0.8% had used it in the last year.[322] Among young adults, 1.8% had used MDMA in the last year.[322]
In Europe, an estimated 37% of regular club-goers aged 14 to 35 used MDMA in the past year according to the 2015 European Drug report.[8] The highest one-year prevalence of MDMA use in Germany in 2012 was 1.7% among people aged 25 to 29 compared with a population average of 0.4%.[8] Among adolescent users in the United States between 1999 and 2008, girls were more likely to use MDMA than boys.[323]
Economics
[edit]Europe
[edit]In 2008 the European Monitoring Centre for Drugs and Drug Addiction noted that although there were some reports of tablets being sold for as little as €1, most countries in Europe then reported typical retail prices in the range of €3 to €9 per tablet, typically containing 25–65 mg of MDMA.[324] By 2014 the EMCDDA reported that the range was more usually between €5 and €10 per tablet, typically containing 57–102 mg of MDMA, although MDMA in powder form was becoming more common.[325]
North America
[edit]The United Nations Office on Drugs and Crime stated in its 2014 World Drug Report that US ecstasy retail prices range from US$1 to $70 per pill, or from $15,000 to $32,000 per kilogram.[326] A new research area named Drug Intelligence aims to automatically monitor distribution networks based on image processing and machine learning techniques, in which an Ecstasy pill picture is analyzed to detect correlations among different production batches.[327] These novel techniques allow police scientists to facilitate the monitoring of illicit distribution networks.
As of October 2015[update], most of the MDMA in the United States is produced in British Columbia, Canada and imported by Canada-based Asian transnational criminal organizations.[57] The market for MDMA in the United States is relatively small compared to methamphetamine, cocaine, and heroin.[57] In the United States, about 0.9 million people used ecstasy in 2010.[24]
Australia
[edit]MDMA is particularly expensive in Australia, costing A$15–A$30 per tablet. In terms of purity data for Australian MDMA, the average is around 34%, ranging from less than 1% to about 85%. The majority of tablets contain 70–85 mg of MDMA. Most MDMA enters Australia from the Netherlands, the UK, Asia, and the US.[328]
Corporate logos on pills
[edit]A number of ecstasy manufacturers brand their pills with a logo, often that of an unrelated corporation.[329] Some pills depict logos of products or media popular with children, such as Shaun the Sheep.[330]
Research
[edit]MDMA-assisted psychotherapy shows promising efficacy and a generally tolerable safety profile for treating PTSD, with meta-analyses indicating symptom reduction, though careful dosing and controlled therapeutic settings are essential to minimize risks.[34][35]
MDMA is being investigated as a potential treatment for social impairments in autism.[331]
The British critical psychiatrist Joanna Moncrieff has critiqued the use and study of MDMA and related drugs like psychedelics for treatment of psychiatric disorders, highlighting concerns including excessive hype around these drugs, blurred lines between medical and recreational use, flawed clinical trial findings, financial conflicts of interest, strong expectancy effects and large placebo responses, short-term benefits over placebo, and their potential for adverse effects, among others.[332]
See also
[edit]References
[edit]- ^ "FDA Substance Registration System". United States National Library of Medicine. Archived from the original on 31 August 2017. Retrieved 31 August 2017.
- ^ a b Luciano RL, Perazella MA (June 2014). "Nephrotoxic effects of designer drugs: synthetic is not better!". Nature Reviews. Nephrology. 10 (6): 314–324. doi:10.1038/nrneph.2014.44. ISSN 1759-5061. PMID 24662435. S2CID 9817771.
- ^ a b c "DrugFacts: MDMA (Ecstasy or Molly)". National Institute on Drug Abuse. Archived from the original on 3 December 2014. Retrieved 2 December 2014.
- ^ "Pingers, pingas, pingaz: how drug slang affects the way we use and understand drugs". The Conversation. 8 January 2020. Archived from the original on 15 January 2021.
- ^ Palmer RB (2012). Medical toxicology of drug abuse: synthesized chemicals and psychoactive plants. Hoboken, N.J.: John Wiley & Sons. p. 139. ISBN 978-0-471-72760-6. Archived from the original on 13 January 2023. Retrieved 4 September 2017.
- ^ Upfal J (2022). Australian Drug Guide: The Plain Language Guide to Drugs and Medicines of All Kinds (9th ed.). Melbourne: Black Inc. p. 319. ISBN 978-1-76064-319-5.
Habit-forming potential moderate. Ecstasy may induce psychological dependence and tolerance to its effect when used frequently.
- ^ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and Addictive Disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 375. ISBN 978-0-07-148127-4.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai Betzler F, Viohl L, Romanczuk-Seiferth N (January 2017). "Decision-making in chronic ecstasy users: a systematic review". The European Journal of Neuroscience. 45 (1): 34–44. doi:10.1111/ejn.13480. PMID 27859780. S2CID 31694072.
...the addictive potential of MDMA itself is relatively small.
- ^ Jerome L, Schuster S, Yazar-Klosinski BB (March 2013). "Can MDMA play a role in the treatment of substance abuse?" (PDF). Current Drug Abuse Reviews. 6 (1): 54–62. doi:10.2174/18744737112059990005. PMID 23627786. S2CID 9327169. Archived from the original (PDF) on 3 August 2020.
Animal and human studies demonstrate moderate abuse liability for MDMA, and this effect may be of most concern to those treating substance abuse disorders.
- ^ a b c d e f g h i j k l m n "Methylenedioxymethamphetamine (MDMA or 'Ecstasy')". EMCDDA. European Monitoring Centre for Drugs and Drug Addiction. Archived from the original on 1 January 2016. Retrieved 17 October 2014.
- ^ "Methylenedioxymethamphetamine (MDMA, ecstasy)". Drugs and Human Performance Fact Sheets. National Highway Traffic Safety Administration. Archived from the original on 3 May 2012.
- ^ Anvisa (24 July 2023). "RDC Nº 804 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 804 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 25 July 2023). Archived from the original on 27 August 2023. Retrieved 27 August 2023.
- ^ a b c d Freye E (28 July 2009). "Pharmacological Effects of MDMA in Man". Pharmacology and Abuse of Cocaine, Amphetamines, Ecstasy and Related Designer Drugs. Springer Netherlands. pp. 151–160. doi:10.1007/978-90-481-2448-0_24. ISBN 978-90-481-2448-0.
- ^ a b "Midomafetamine: Uses, Interactions, Mechanism of Action". DrugBank Online. 31 July 2007. Retrieved 11 December 2024.
- ^ a b c d e f g h i j k l m n o p Carvalho M, Carmo H, Costa VM, Capela JP, Pontes H, Remião F, et al. (August 2012). "Toxicity of amphetamines: an update". Archives of Toxicology. 86 (8): 1167–1231. Bibcode:2012ArTox..86.1167C. doi:10.1007/s00204-012-0815-5. PMID 22392347. S2CID 2873101.
- ^ a b c d e f g h i j k Straumann I, Avedisian I, Klaiber A, Varghese N, Eckert A, Rudin D, et al. (August 2024). "Acute effects of R-MDMA, S-MDMA, and racemic MDMA in a randomized double-blind cross-over trial in healthy participants". Neuropsychopharmacology. 50 (2): 362–371. doi:10.1038/s41386-024-01972-6. PMC 11631982. PMID 39179638.
- ^ a b c d e f g h i j k l m n o p q r s t Dunlap LE, Andrews AM, Olson DE (October 2018). "Dark Classics in Chemical Neuroscience: 3,4-Methylenedioxymethamphetamine" (PDF). ACS Chemical Neuroscience. 9 (10): 2408–2427. doi:10.1021/acschemneuro.8b00155. PMC 6197894. PMID 30001118.
- ^ a b c d e f g h i Oeri HE (May 2021). "Beyond ecstasy: Alternative entactogens to 3,4-methylenedioxymethamphetamine with potential applications in psychotherapy". Journal of Psychopharmacology. 35 (5). Oxford, England: 512–536. doi:10.1177/0269881120920420. PMC 8155739. PMID 32909493.
- ^ Palamar JJ (7 December 2016). "There's something about Molly: The underresearched yet popular powder form of ecstasy in the United States". Substance Abuse. 38 (1): 15–17. doi:10.1080/08897077.2016.1267070. PMC 5578728. PMID 27925866.
- ^ Skaug HA, ed. (14 December 2020). "Hva er tryggest av molly og ecstasy?" [What is safer: molly or ecstasy?]. Ung.no (in Norwegian). Norwegian Directorate for Children, Youth and Family Affairs. Archived from the original on 11 August 2022. Retrieved 20 June 2022.
MDMA er virkestoffet i både Molly-krystaller og Ecstasy-tabletter. (MDMA is the active substance in both Molly crystals and Ecstasy tablets)
- ^ Green AR, Mechan AO, Elliott JM, O'Shea E, Colado MI (September 2003). "The pharmacology and clinical pharmacology of 3,4-methylenedioxymethamphetamine (MDMA, "ecstasy")". Pharmacological Reviews. 55 (3): 463–508. doi:10.1124/pr.55.3.3. PMID 12869661.
- ^ a b c d e f g h i j k l m n o p q Meyer JS (2013). "3,4-methylenedioxymethamphetamine (MDMA): current perspectives". Substance Abuse and Rehabilitation. 4: 83–99. doi:10.2147/SAR.S37258. PMC 3931692. PMID 24648791.
- ^ Freudenmann RW, Öxler F, Bernschneider-Reif S (August 2006). "The origin of MDMA (ecstasy) revisited: the true story reconstructed from the original documents" (PDF). Addiction. 101 (9). Abingdon, England: 1241–1245. doi:10.1111/j.1360-0443.2006.01511.x. PMID 16911722. Archived (PDF) from the original on 22 September 2020. Retrieved 23 May 2019.
Although MDMA was, in fact, first synthesized at Merck in 1912, it was not tested pharmacologically because it was only an unimportant precursor in a new synthesis for haemostatic substances.
- ^ a b c d e f g Anderson L, ed. (18 May 2014). "MDMA". Drugs.com. Drugsite Trust. Archived from the original on 23 March 2016. Retrieved 30 March 2016.
- ^ a b c d "DrugFacts: MDMA (Ecstasy/Molly)". National Institute on Drug Abuse. February 2016. Archived from the original on 23 March 2016. Retrieved 30 March 2016.
- ^ World Health Organization (2004). Neuroscience of Psychoactive Substance Use and Dependence. World Health Organization. pp. 97–. ISBN 978-92-4-156235-5. Archived from the original on 28 April 2016.
- ^ World Drug Report 2018 (PDF). United Nations. June 2018. p. 7. ISBN 978-92-1-148304-8. Archived (PDF) from the original on 27 July 2018. Retrieved 14 July 2018.
- ^ "MDMA (Ecstasy/Molly)". National Institute on Drug Abuse. Archived from the original on 15 July 2018. Retrieved 14 July 2018.
- ^ a b c d e f g White CM (March 2014). "How MDMA's pharmacology and pharmacokinetics drive desired effects and harms". Journal of Clinical Pharmacology. 54 (3): 245–252. doi:10.1002/jcph.266. PMID 24431106. S2CID 6223741.
- ^ Freye E (2009). Pharmacology and Abuse of Cocaine, Amphetamines, Ecstasy and Related Designer Drugs: A comprehensive review on their mode of action, treatment of abuse and intoxication. Springer Science & Business Media. p. 147. ISBN 978-90-481-2448-0. Archived from the original on 13 January 2023. Retrieved 12 May 2020.
- ^ Lyles J, Cadet JL (May 2003). "Methylenedioxymethamphetamine (MDMA, Ecstasy) neurotoxicity: cellular and molecular mechanisms". Brain Research. Brain Research Reviews. 42 (2): 155–168. doi:10.1016/S0165-0173(03)00173-5. PMID 12738056. S2CID 45330713.
- ^ Philipps D (1 May 2018). "Ecstasy as a Remedy for PTSD? You Probably Have Some Questions". The New York Times. Archived from the original on 1 January 2022. Retrieved 14 July 2018.
- ^ Patel V (2010). Mental and neurological public health a global perspective (1st ed.). San Diego, CA: Academic Press/Elsevier. p. 57. ISBN 978-0-12-381527-9. Archived from the original on 10 September 2017.
- ^ a b Tedesco S, Gajaram G, Chida S, Ahmad A, Pentak M, Kelada M, et al. (May 2021). "The Efficacy of MDMA (3,4-Methylenedioxymethamphetamine) for Post-traumatic Stress Disorder in Humans: A Systematic Review and Meta-Analysis". Cureus. 13 (5) e15070. doi:10.7759/cureus.15070. PMC 8207489. PMID 34150406.
- ^ a b Smith KW, Sicignano DJ, Hernandez AV, White CM (April 2022). "MDMA-Assisted Psychotherapy for Treatment of Posttraumatic Stress Disorder: A Systematic Review With Meta-Analysis". Journal of Clinical Pharmacology. 62 (4): 463–471. doi:10.1002/jcph.1995. PMID 34708874.
- ^ Nuwer R (3 May 2021). "A Psychedelic Drug Passes a Big Test for PTSD Treatment". The New York Times. Archived from the original on 5 June 2021. Retrieved 5 June 2021.
- ^ "Subsection 56(1) class exemption for practitioners, agents, pharmacists, persons in charge of a hospital, hospital employees, and licensed dealers to conduct activities with psilocybin and MDMA in relation to a special access program authorization". Health Canada. 5 January 2022. Archived from the original on 11 February 2022. Retrieved 20 February 2022.
- ^ "Change to classification of psilocybin and MDMA to enable prescribing by authorised psychiatrists". 3 February 2023. Archived from the original on 4 February 2024. Retrieved 4 February 2024.
- ^ Reynolds S (1999). Generation Ecstasy: Into the World of Techno and Rave Culture. Routledge. p. 81. ISBN 978-0-415-92373-6. Archived from the original on 8 November 2023. Retrieved 13 October 2020.
- ^ a b McCrady BS, Epstein EE, eds. (2013). Addictions: a comprehensive guidebook (Second ed.). Oxford: Oxford University Press. p. 299. ISBN 978-0-19-975366-6. Archived from the original on 13 January 2023. Retrieved 11 January 2017.
- ^ a b Zeifman RJ, Kettner H, Pagni BA, Mallard A, Roberts DE, Erritzoe D, et al. (August 2023). "Co-use of MDMA with psilocybin/LSD may buffer against challenging experiences and enhance positive experiences". Scientific Reports. 13 (1) 13645. Bibcode:2023NatSR..1313645Z. doi:10.1038/s41598-023-40856-5. PMC 10444769. PMID 37608057.
- ^ Weiss S (16 February 2024). "Nexus Flipping: What Happens When You Combine MDMA and 2C-B". DoubleBlind Mag. Retrieved 10 July 2024.
- ^ a b Hysek CM, Simmler LD, Nicola VG, Vischer N, Donzelli M, Krähenbühl S, et al. (4 May 2012). Laks J (ed.). "Duloxetine inhibits effects of MDMA ("ecstasy") in vitro and in humans in a randomized placebo-controlled laboratory study". PLOS ONE. 7 (5) e36476. Bibcode:2012PLoSO...736476H. doi:10.1371/journal.pone.0036476. PMC 3344887. PMID 22574166.
Fig. 7 shows the mean PD effects of MDMA plotted against simultaneous plasma concentrations at the different time points (hysteresis loops). The increases in "any drug effect" (Fig. 7a) and MAP (Fig. 7b) returned to baseline within 6 h when MDMA concentrations were still high. This clockwise hysteresis indicates that a smaller MDMA effect was seen at a given plasma concentration later in time, indicating rapid acute pharmacodynamic tolerance, which was similarly described for cocaine [33]. [...] Figure 7. Pharmacokinetic-pharmacodynamic (PK-PD) relationship. MDMA effects are plotted against simultaneous MDMA plasma concentrations (a, b). The time of sampling is noted next to each point in minutes or hours after MDMA administration. The clockwise hysteresis indicates acute tolerance to the effects of MDMA.
- ^ Yuki F, Rie I, Miki K, Mitsuhiro W, Naotaka K, Kenichiro N (April 2013). "Warning against co-administration of 3,4-methylenedioxymethamphetamine (MDMA) with methamphetamine from the perspective of pharmacokinetic and pharmacodynamic evaluations in rat brain". European Journal of Pharmaceutical Sciences. 49 (1): 57–64. doi:10.1016/j.ejps.2013.01.014. PMID 23395913.
- ^ Hamida SB, Tracqui A, de Vasconcelos AP, Szwarc E, Lazarus C, Kelche C, et al. (July 2009). "Ethanol increases the distribution of MDMA to the rat brain: possible implications in the ethanol-induced potentiation of the psychostimulant effects of MDMA". The International Journal of Neuropsychopharmacology. 12 (6): 749–759. doi:10.1017/s1461145708009693. PMID 19046482. S2CID 24230367.
- ^ Oesterheld JR, Armstrong SC, Cozza KL (1 March 2004). "Ecstasy: pharmacodynamic and pharmacokinetic interactions". Psychosomatics. 45 (1): 84–87. doi:10.1176/appi.psy.45.1.84. PMID 14709765.
- ^ Carpenter M, Berry H, Pelletier AL (May 2019). "Clinically Relevant Drug-Drug Interactions in Primary Care". American Family Physician. 99 (9): 558–564. PMID 31038898.
- ^ Sessa B, Nutt D (January 2015). "Making a medicine out of MDMA". The British Journal of Psychiatry. 206 (1): 4–6. doi:10.1192/bjp.bp.114.152751. PMID 25561485.
- ^ Ebrahimian Z, Karimi Z, Khoshnoud MJ, Namavar MR, Daraei B, Haidari MR (1 February 2017). "Behavioral and Stereological Analysis of the Effects of Intermittent Feeding Diet on the Orally Administrated MDMA ("ecstasy") in Mice". Innovations in Clinical Neuroscience. 14 (1–2): 40–52. PMC 5373794. PMID 28386520.
MDMA is listed as a Schedule 1 drug by the United States Drug Enforcement Agency, meaning that currently there are no accepted medical uses for MDMA in the United States, there is a lack of accepted safety for use under medical supervision, and there is a high potential for abuse.
- ^ Climko RP, Roehrich H, Sweeney DR, Al-Razi J (1986). "Ecstacy: a review of MDMA and MDA". International Journal of Psychiatry in Medicine. 16 (4): 359–372. doi:10.2190/dcrp-u22m-aumd-d84h. PMID 2881902. S2CID 31902958.
- ^ Wan W (6 August 2017). "Ecstasy could be 'breakthrough' therapy for soldiers, others suffering from PTSD". The Washington Post. Archived from the original on 28 August 2017. Retrieved 3 April 2021.
- ^ Kupferschmidt K (26 August 2017). "All clear for the decisive trial of ecstasy in PTSD patients". Science (magazine). Archived from the original on 28 December 2021. Retrieved 3 April 2021.
- ^ Dupuis D, Veissière S (October 2022). "Culture, context, and ethics in the therapeutic use of hallucinogens: Psychedelics as active super-placebos?". Transcultural Psychiatry. 59 (5): 571–578. doi:10.1177/13634615221131465. PMID 36263513.
- ^ van Elk M, Yaden DB (September 2022). "Pharmacological, neural, and psychological mechanisms underlying psychedelics: A critical review". Neuroscience and Biobehavioral Reviews. 140 104793. doi:10.1016/j.neubiorev.2022.104793. hdl:1887/3515020. PMID 35878791.
In addition, the strong prior expectations that many people have about psychedelics directly contribute to the psychedelic experience and as a consequence it has been suggested that psychedelics may act as a 'super-placebo' (Hartogsohn, 2016). Specifically, strong prior expectations (e.g., that a specific intervention will likely trigger a mystical experience) will increase the likelihood of having e.g., a mystical-type experience (Maij et al., 2019), and this placebo-effect is further boosted by the psychedelic-induced suggestibility.
- ^ Saunders N (29 July 1995). "The Agony and Ecstasy of God's path". Council on Spiritual Practices (CSP). Archived from the original on 24 April 2013. Retrieved 11 June 2011.
- ^ Watson L, Beck J (1991). "New age seekers: MDMA use as an adjunct to spiritual pursuit" (PDF). Journal of Psychoactive Drugs. 23 (3): 261–270. doi:10.1080/02791072.1991.10471587. PMID 1685513. Archived from the original on 22 November 2004. Retrieved 28 April 2024.
{{cite journal}}: CS1 maint: bot: original URL status unknown (link) - ^ a b c d "MDMA (3,4-Methylenedioxymethamphetamine)" (PDF). 2015 National Drug Threat Assessment Summary. United States Department of Justice, Drug Enforcement Administration. October 2015. pp. 85–88. Archived from the original (PDF) on 10 April 2016. Retrieved 10 April 2016.
- ^ a b Molly Madness. Drugs, Inc. (TV documentary). National Geographic Channel. 13 August 2014. ASIN B00LIC368M.
- ^ a b Manic Molly. Drugs, Inc. (TV documentary). National Geographic Channel. 10 December 2014. ASIN B00LIC368M.
- ^ Kelly M (20 June 2019). "Man arrested for possession of ecstasy tablets shaped like Wario". Nintendo Enthusiast. Archived from the original on 24 June 2021. Retrieved 17 June 2021.
- ^ "Groesbeck: Students caught with deceptively shaped Ecstasy pills". KWTX. 31 October 2019. Archived from the original on 24 June 2021. Retrieved 17 June 2021.
- ^ a b c d e f g h i j k l m n o p q r s "3,4-Methylenedioxymethamphetamine". Hazardous Substances Data Bank. National Library of Medicine. 28 August 2008. Archived from the original on 4 April 2019. Retrieved 22 August 2014.
- ^ Liechti ME, Gamma A, Vollenweider FX (March 2001). "Gender differences in the subjective effects of MDMA". Psychopharmacology. 154 (2): 161–168. doi:10.1007/s002130000648. PMID 11314678. S2CID 20251888.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad Greene SL, Kerr F, Braitberg G (October 2008). "Review article: amphetamines and related drugs of abuse". Emergency Medicine Australasia. 20 (5): 391–402. doi:10.1111/j.1742-6723.2008.01114.x. PMID 18973636. S2CID 20755466.
- ^ a b Landriscina F (1995). "MDMA and the states of Consciousness". Eleusis. 2: 3–9.
- ^ Baggott MJ, Kirkpatrick MG, Bedi G, de Wit H (June 2015). "Intimate insight: MDMA changes how people talk about significant others". Journal of Psychopharmacology. 29 (6). Oxford, England: 669–677. doi:10.1177/0269881115581962. PMC 4698152. PMID 25922420.
- ^ a b Schmid Y, Hysek CM, Simmler LD, Crockett MJ, Quednow BB, Liechti ME (September 2014). "Differential effects of MDMA and methylphenidate on social cognition" (PDF). Journal of Psychopharmacology. 28 (9). Oxford, England: 847–856. doi:10.1177/0269881114542454. PMID 25052243. S2CID 25713943. Archived (PDF) from the original on 17 September 2020. Retrieved 29 June 2019.
- ^ Wardle MC, de Wit H (October 2014). "MDMA alters emotional processing and facilitates positive social interaction". Psychopharmacology. 231 (21): 4219–4229. doi:10.1007/s00213-014-3570-x. PMC 4194242. PMID 24728603.
- ^ Bravo GL (2001). "What does MDMA feel like?". In Holland J (ed.). Ecstasy: The complete guide. A comprehensive look at the risks and benefits of MDMA. Rochester: Park Street Press.
- ^ Metzner R (2005). "Psychedelic, Psychoactive, and Addictive Drugs and States of Consciousness". In Earleywine M (ed.). Mind-Altering Drugs: The Science of Subjective Experience. New York: Oxford University. Archived from the original on 9 October 2017. Retrieved 8 October 2017.
- ^ a b c d Kamilar-Britt P, Bedi G (October 2015). "The prosocial effects of 3,4-methylenedioxymethamphetamine (MDMA): Controlled studies in humans and laboratory animals". Neuroscience and Biobehavioral Reviews. 57: 433–446. doi:10.1016/j.neubiorev.2015.08.016. PMC 4678620. PMID 26408071.
- ^ a b c d e f g Keane M (February 2014). "Recognising and managing acute hyponatraemia". Emergency Nurse. 21 (9): 32–6, quiz 37. doi:10.7748/en2014.02.21.9.32.e1128. PMID 24494770.
- ^ Spauwen LW, Niekamp AM, Hoebe CJ, Dukers-Muijrers NH (February 2015). "Drug use, sexual risk behaviour and sexually transmitted infections among swingers: a cross-sectional study in The Netherlands". Sexually Transmitted Infections. 91 (1): 31–36. doi:10.1136/sextrans-2014-051626. PMID 25342812.
It is known that some recreational drugs (eg, MDMA or GHB) may hamper the potential to ejaculate or maintain an erection.
- ^ Hahn IH (25 March 2015). "MDMA Toxicity: Background, Pathophysiology, Epidemiology". Medscape. Archived from the original on 11 May 2016. Retrieved 14 May 2016.
- ^ Parrott AC (2012). "13. MDMA and LSD". In Verster J, Brady K, Galanter M, Conrod P (eds.). Drug Abuse and Addiction in Medical Illness: Causes, Consequences and Treatment. Springer Science & Business Media. p. 179. ISBN 978-1-4614-3375-0.
- ^ a b c d e f g h Garg A, Kapoor S, Goel M, Chopra S, Chopra M, Kapoor A, et al. (2015). "Functional Magnetic Resonance Imaging in Abstinent MDMA Users: A Review". Current Drug Abuse Reviews. 8 (1): 15–25. doi:10.2174/1874473708666150303115833. PMID 25731754.
- ^ a b Mueller F, Lenz C, Steiner M, Dolder PC, Walter M, Lang UE, et al. (March 2016). "Neuroimaging in moderate MDMA use: A systematic review". Neuroscience and Biobehavioral Reviews. 62: 21–34. doi:10.1016/j.neubiorev.2015.12.010. PMID 26746590.
- ^ Gouzoulis-Mayfrank E, Daumann J (2009). "Neurotoxicity of drugs of abuse--the case of methylenedioxyamphetamines (MDMA, ecstasy), and amphetamines". Dialogues in Clinical Neuroscience. 11 (3): 305–317. doi:10.31887/DCNS.2009.11.3/egmayfrank. PMC 3181923. PMID 19877498.
- ^ a b Halpin LE, Collins SA, Yamamoto BK (February 2014). "Neurotoxicity of methamphetamine and 3,4-methylenedioxymethamphetamine". Life Sciences. 97 (1): 37–44. doi:10.1016/j.lfs.2013.07.014. PMC 3870191. PMID 23892199.
In contrast, MDMA produces damage to serotonergic, but not dopaminergic axon terminals in the striatum, hippocampus, and prefrontal cortex (Battaglia et al., 1987, O'Hearn et al., 1988). The damage associated with Meth and MDMA has been shown to persist for at least 2 years in rodents, non-human primates and humans (Seiden et al., 1988, Woolverton et al., 1989, McCann et al., 1998, Volkow et al., 2001a, McCann et al., 2005)
- ^ Szigeti B, Winstock AR, Erritzoe D, Maier LJ (July 2018). "Are ecstasy induced serotonergic alterations overestimated for the majority of users?". Journal of Psychopharmacology. 32 (7). Oxford, England: 741–748. doi:10.1177/0269881118767646. PMID 29733742. S2CID 13660975.
Given the dose-response relationship between MDMA exposure and SERT reductions and the statistically non-significant SERT binding differences for users with use levels similar to the majority of real-life users, it can be speculated that SERT levels may not be significantly affected for most recreational ecstasy users.
- ^ Roberts CA, Jones A, Montgomery C (April 2016). "Meta-analysis of molecular imaging of serotonin transporters in ecstasy/polydrug users". Neuroscience and Biobehavioral Reviews. 63: 158–167. doi:10.1016/j.neubiorev.2016.02.003. PMID 26855234.
- ^ a b c d Parrott AC (2014). "The potential dangers of using MDMA for psychotherapy". Journal of Psychoactive Drugs. 46 (1): 37–43. doi:10.1080/02791072.2014.873690. PMID 24830184. S2CID 23485480.
- ^ Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al. (January 2009). "The harmful health effects of recreational ecstasy: a systematic review of observational evidence". Health Technology Assessment. 13 (6). Winchester, England: iii–iv, ix–xii, 1–315. doi:10.3310/hta13050. hdl:10871/11534. PMID 19195429.
- ^ Kuypers KP, Theunissen EL, van Wel JH, de Sousa Fernandes Perna EB, Linssen A, Sambeth A, et al. (2016). "Verbal Memory Impairment in Polydrug Ecstasy Users: A Clinical Perspective". PLOS ONE. 11 (2) e0149438. Bibcode:2016PLoSO..1149438K. doi:10.1371/journal.pone.0149438. PMC 4764468. PMID 26907605.
- ^ Laws KR, Kokkalis J (August 2007). "Ecstasy (MDMA) and memory function: a meta-analytic update". Human Psychopharmacology. 22 (6): 381–388. doi:10.1002/hup.857. PMID 17621368. S2CID 25353240.
- ^ Kousik SM, Napier TC, Carvey PM (2012). "The effects of psychostimulant drugs on blood brain barrier function and neuroinflammation". Frontiers in Pharmacology. 3: 121. doi:10.3389/fphar.2012.00121. PMC 3386512. PMID 22754527.
- ^ McMillan B, Starr C (2014). Human biology (10th ed.). Belmont, CA: Brooks/Cole Cengage Learning. ISBN 978-1-133-59916-6.
- ^ Boyle NT, Connor TJ (September 2010). "Methylenedioxymethamphetamine ('Ecstasy')-induced immunosuppression: a cause for concern?". British Journal of Pharmacology. 161 (1): 17–32. doi:10.1111/J.1476-5381.2010.00899.X. PMC 2962814. PMID 20718737.
- ^ Cavero I, Guillon JM (2014). "Safety Pharmacology assessment of drugs with biased 5-HT(2B) receptor agonism mediating cardiac valvulopathy". Journal of Pharmacological and Toxicological Methods. 69 (2): 150–161. doi:10.1016/j.vascn.2013.12.004. PMID 24361689.
- ^ Padhariya K, Bhandare R, Canney D, Velingkar V (2017). "Cardiovascular Concern of 5-HT2B Receptor and Recent Vistas in the Development of Its Antagonists". Cardiovascular & Hematological Disorders Drug Targets. 17 (2): 86–104. doi:10.2174/1871529X17666170703115111. PMID 28676029.
- ^ Koczor CA, Ludlow I, Hight RS, Jiao Z, Fields E, Ludaway T, et al. (November 2015). "Ecstasy (MDMA) Alters Cardiac Gene Expression and DNA Methylation: Implications for Circadian Rhythm Dysfunction in the Heart". Toxicological Sciences. 148 (1): 183–191. doi:10.1093/toxsci/kfv170. PMC 4731408. PMID 26251327.
- ^ Nutt D, King LA, Saulsbury W, Blakemore C (March 2007). "Development of a rational scale to assess the harm of drugs of potential misuse". Lancet. 369 (9566). London, England: 1047–1053. doi:10.1016/S0140-6736(07)60464-4. PMID 17382831. S2CID 5903121.
Lay summary: "Scientists want new drug rankings". BBC News. 23 March 2007. Archived from the original on 2 December 2007. Retrieved 4 April 2008. - ^ a b Olausson P, Jentsch JD, Tronson N, Neve RL, Nestler EJ, Taylor JR (September 2006). "DeltaFosB in the nucleus accumbens regulates food-reinforced instrumental behavior and motivation". The Journal of Neuroscience. 26 (36): 9196–9204. doi:10.1523/JNEUROSCI.1124-06.2006. PMC 6674495. PMID 16957076.
- ^ a b Robison AJ, Nestler EJ (October 2011). "Transcriptional and epigenetic mechanisms of addiction". Nature Reviews. Neuroscience. 12 (11): 623–637. doi:10.1038/nrn3111. PMC 3272277. PMID 21989194.
- ^ Mack AH, Brady KT, Miller SI, Frances RJ (12 May 2016). Clinical Textbook of Addictive Disorders. Guilford Publications. p. 169. ISBN 978-1-4625-2169-2.
MDMA's addictive liability appears to be lower than that of other drugs of abuse....
- ^ Favrod-Coune T, Broers B (July 2010). "The Health Effect of Psychostimulants: A Literature Review". Pharmaceuticals. 3 (7). Basel, Switzerland: 2333–2361. doi:10.3390/ph3072333. PMC 4036656. PMID 27713356.
It seems to present a smaller addiction potential than cocaine or methamphetamine.
- ^ Ries R, Miller SC, Fiellin DA (2009). Principles of addiction medicine (4th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. p. 226. ISBN 978-0-7817-7477-2. Archived from the original on 13 January 2023. Retrieved 11 January 2017.
MDA and MDMA are less reinforcing than amphetamine...
- ^ a b Steinkellner T, Freissmuth M, Sitte HH, Montgomery T (January 2011). "The ugly side of amphetamines: short- and long-term toxicity of 3,4-methylenedioxymethamphetamine (MDMA, 'Ecstasy'), methamphetamine and D-amphetamine". Biological Chemistry. 392 (1–2): 103–115. doi:10.1515/BC.2011.016. PMC 4497800. PMID 21194370.
...approximately 15% of routine MDMA users recently fit the diagnostic criteria for MDMA dependence according to the Diagnostic and Statistical Manual, fourth edition/DSMIV.
- ^ Mack AH, Brady KT, Miller SI, Frances RJ (12 May 2016). Clinical Textbook of Addictive Disorders. Guilford Publications. p. 171. ISBN 978-1-4625-2169-2. Archived from the original on 19 January 2023. Retrieved 13 October 2020.
There are no known pharmacological treatments for MDMA addiction.
- ^ Vorhees CV (November 1997). "Methods for detecting long-term CNS dysfunction after prenatal exposure to neurotoxins". Drug and Chemical Toxicology. 20 (4): 387–399. doi:10.3109/01480549709003895. PMID 9433666.
- ^ a b Meamar R, Karamali F, Sadeghi HM, Etebari M, Nasr-Esfahani MH, Baharvand H (June 2010). "Toxicity of ecstasy (MDMA) towards embryonic stem cell-derived cardiac and neural cells". Toxicology in Vitro. 24 (4): 1133–1138. Bibcode:2010ToxVi..24.1133M. doi:10.1016/j.tiv.2010.03.005. PMID 20230888.
In summary, MDMA is a moderate teratogen that could influence cardiac and neuronal differentiation in the ESC model and these results are in concordance with previous in vivo and in vitro models.
- ^ Singer LT, Moore DG, Fulton S, Goodwin J, Turner JJ, Min MO, et al. (2012). "Neurobehavioral outcomes of infants exposed to MDMA (Ecstasy) and other recreational drugs during pregnancy". Neurotoxicology and Teratology. 34 (3): 303–310. Bibcode:2012NTxT...34..303S. doi:10.1016/j.ntt.2012.02.001. PMC 3367027. PMID 22387807.
- ^ Lipton JW, Tolod EG, Thompson VB, Pei L, Paumier KL, Terpstra BT, et al. (October 2008). "3,4-Methylenedioxy-N-methamphetamine (ecstasy) promotes the survival of fetal dopamine neurons in culture". Neuropharmacology. 55 (5): 851–859. doi:10.1016/j.neuropharm.2008.06.062. PMC 2572681. PMID 18655796.
- ^ a b c d e f Richards JR, Albertson TE, Derlet RW, Lange RA, Olson KR, Horowitz BZ (May 2015). "Treatment of toxicity from amphetamines, related derivatives, and analogues: a systematic clinical review". Drug and Alcohol Dependence. 150: 1–13. doi:10.1016/j.drugalcdep.2015.01.040. PMID 25724076.
- ^ a b Hysek C, Schmid Y, Rickli A, Simmler LD, Donzelli M, Grouzmann E, et al. (August 2012). "Carvedilol inhibits the cardiostimulant and thermogenic effects of MDMA in humans". British Journal of Pharmacology. 166 (8): 2277–2288. doi:10.1111/j.1476-5381.2012.01936.x. PMC 3448893. PMID 22404145.
- ^ Vanattou-Saïfoudine N, McNamara R, Harkin A (November 2012). "Caffeine provokes adverse interactions with 3,4-methylenedioxymethamphetamine (MDMA, 'ecstasy') and related psychostimulants: mechanisms and mediators". British Journal of Pharmacology. 167 (5): 946–959. doi:10.1111/j.1476-5381.2012.02065.x. PMC 3492978. PMID 22671762.
- ^ Hall AP, Henry JA (June 2006). "Acute toxic effects of 'Ecstasy' (MDMA) and related compounds: overview of pathophysiology and clinical management". British Journal of Anaesthesia. 96 (6): 678–685. doi:10.1093/bja/ael078. PMID 16595612.
- ^ a b c d e f g de la Torre R, Farré M, Roset PN, Pizarro N, Abanades S, Segura M, et al. (April 2004). "Human pharmacology of MDMA: pharmacokinetics, metabolism, and disposition" (PDF). Therapeutic Drug Monitoring. 26 (2): 137–144. doi:10.1097/00007691-200404000-00009. PMID 15228154. Archived from the original (PDF) on 5 March 2014. Retrieved 25 October 2009.
- ^ a b c d e f Kellum JA, Gunn SR, Singer M (2008). Oxford American Handbook of Critical Care. Oxford University Press. p. 464. ISBN 978-0-19-530528-9. OCLC 1003197730.
- ^ Chummun H, Tilley V, Ibe J (2010). "3,4-methylenedioxyamfetamine (ecstasy) use reduces cognition". British Journal of Nursing. 19 (2). Mark Allen Publishing: 94–100. PMID 20235382.
- ^ Pendergraft WF, Herlitz LC, Thornley-Brown D, Rosner M, Niles JL (November 2014). "Nephrotoxic effects of common and emerging drugs of abuse". Clinical Journal of the American Society of Nephrology. 9 (11): 1996–2005. doi:10.2215/CJN.00360114. PMC 4220747. PMID 25035273.
- ^ Silins E, Copeland J, Dillon P (August 2007). "Qualitative review of serotonin syndrome, ecstasy (MDMA) and the use of other serotonergic substances: hierarchy of risk". The Australian and New Zealand Journal of Psychiatry. 41 (8): 649–655. doi:10.1080/00048670701449237. PMID 17620161. S2CID 25832516.
- ^ Papaseit E, Pérez-Mañá C, Torrens M, Farré A, Poyatos L, Hladun O, et al. (May 2020). "MDMA interactions with pharmaceuticals and drugs of abuse". Expert Opinion on Drug Metabolism & Toxicology. 16 (5): 357–369. doi:10.1080/17425255.2020.1749262. PMID 32228243. S2CID 214750903.
- ^ a b c d e f g h i j k l m Fonseca DA, Ribeiro DM, Tapadas M, Cotrim MD (July 2021). "Ecstasy (3,4-methylenedioxymethamphetamine): Cardiovascular effects and mechanisms". European Journal of Pharmacology. 903 174156. doi:10.1016/j.ejphar.2021.174156. PMID 33971177.
- ^ a b Schmid Y, Rickli A, Schaffner A, Duthaler U, Grouzmann E, Hysek CM, et al. (April 2015). "Interactions between bupropion and 3,4-methylenedioxymethamphetamine in healthy subjects". The Journal of Pharmacology and Experimental Therapeutics. 353 (1): 102–111. doi:10.1124/jpet.114.222356. PMID 25655950.
- ^ Vuori E, Henry JA, Ojanperä I, Nieminen R, Savolainen T, Wahlsten P, et al. (March 2003). "Death following ingestion of MDMA (ecstasy) and moclobemide". Addiction. 98 (3). Abingdon, England: 365–368. doi:10.1046/j.1360-0443.2003.00292.x. PMID 12603236.
- ^ a b c d e f g h i j Halberstadt AL, Nichols DE (2020). "Serotonin and serotonin receptors in hallucinogen action". Handbook of the Behavioral Neurobiology of Serotonin. Handbook of Behavioral Neuroscience. Vol. 31. pp. 843–863. doi:10.1016/B978-0-444-64125-0.00043-8. ISBN 978-0-444-64125-0. ISSN 1569-7339. S2CID 241134396.
- ^ a b Mendelson J, Baggott MJ, Li L, Coyle J, Galloway GP (2012). "Poster Session II (PII 1-111): PII-41. MDMA-Induced Increases in Blood Pressure Are Not Mediated by α-Adrenergic Mechanisms and Are Not Due To Elevated Peripheral Vascular Resistance". Clinical Pharmacology & Therapeutics. 91 (S1 [American Society for Clinical Pharmacology and Therapeutics Abstract of papers, 2012 Annual Meeting Gaylord National Hotel and Convention Center National Harbor, Maryland March 14–17, 2012]): S51–S93 (S66–S66). doi:10.1038/clpt.2011.361. ISSN 0009-9236.
MDMA increased heart rate (HR) by 25 bpm (p<.001), [cardiac output (CO)] by 1.75 L/min (p<0.01) but did not alter [stroke volume (SV)] or [systemic vascular resistance (SVR)]. Compared to MDMA alone the combination of MDMA + prazosin further increased HR by 24 bpm (p<0.001) and CO by 3.3L/min (p<0.02). MDMA increased systolic and diastolic blood pressure (SBP, DBP) by 26 mmHg (p<0.001 each); prazosin attenuated MDMA effects on DBP by 9.3 mmHg (p<001) but did not alter SBP. [...] MDMA increases HR, producing elevations in CO. The hypertensive effects of MDMA are not due to elevated peripheral vascular resistance and the blood pressure effects of MDMA are not attenuated by α-adrenergic blockade, suggesting that MDMA may produce CV effects through non-α-adrenergic mechanisms.
- ^ a b c d e f Liechti ME, Saur MR, Gamma A, Hell D, Vollenweider FX (October 2000). "Psychological and physiological effects of MDMA ("Ecstasy") after pretreatment with the 5-HT(2) antagonist ketanserin in healthy humans". Neuropsychopharmacology. 23 (4): 396–404. doi:10.1016/S0893-133X(00)00126-3. PMID 10989266.
- ^ a b Wsół A (December 2023). "Cardiovascular safety of psychedelic medicine: current status and future directions". Pharmacological Reports. 75 (6): 1362–1380. doi:10.1007/s43440-023-00539-4. PMC 10661823. PMID 37874530.
- ^ Neumann J, Dhein S, Kirchhefer U, Hofmann B, Gergs U (2024). "Effects of hallucinogenic drugs on the human heart". Frontiers in Pharmacology. 15 1334218. doi:10.3389/fphar.2024.1334218. PMC 10869618. PMID 38370480.
- ^ Ley L, Holze F, Arikci D, Becker AM, Straumann I, Klaiber A, et al. (October 2023). "Comparative acute effects of mescaline, lysergic acid diethylamide, and psilocybin in a randomized, double-blind, placebo-controlled cross-over study in healthy participants". Neuropsychopharmacology. 48 (11): 1659–1667. doi:10.1038/s41386-023-01607-2. PMC 10517157. PMID 37231080.
- ^ Hart XM, Spangemacher M, Defert J, Uchida H, Gründer G (April 2024). "Update Lessons from PET Imaging Part II: A Systematic Critical Review on Therapeutic Plasma Concentrations of Antidepressants". Therapeutic Drug Monitoring. 46 (2): 155–169. doi:10.1097/FTD.0000000000001142. PMID 38287888.
- ^ Eap CB, Gründer G, Baumann P, Ansermot N, Conca A, Corruble E, et al. (October 2021). "Tools for optimising pharmacotherapy in psychiatry (therapeutic drug monitoring, molecular brain imaging and pharmacogenetic tests): focus on antidepressants" (PDF). The World Journal of Biological Psychiatry. 22 (8): 561–628. doi:10.1080/15622975.2021.1878427. PMID 33977870. S2CID 234472488. Archived (PDF) from the original on 5 May 2022. Retrieved 10 April 2022.
- ^ Hysek CM, Simmler LD, Schillinger N, Meyer N, Schmid Y, Donzelli M, et al. (March 2014). "Pharmacokinetic and pharmacodynamic effects of methylphenidate and MDMA administered alone or in combination" (PDF). The International Journal of Neuropsychopharmacology. 17 (3): 371–381. doi:10.1017/S1461145713001132. PMID 24103254.
- ^ Hysek CM, Vollenweider FX, Liechti ME (August 2010). "Effects of a beta-blocker on the cardiovascular response to MDMA (Ecstasy)" (PDF). Emergency Medicine Journal. 27 (8): 586–589. doi:10.1136/emj.2009.079905. PMID 20378736.
- ^ Hysek CM, Brugger R, Simmler LD, Bruggisser M, Donzelli M, Grouzmann E, et al. (February 2012). "Effects of the α₂-adrenergic agonist clonidine on the pharmacodynamics and pharmacokinetics of 3,4-methylenedioxymethamphetamine in healthy volunteers". The Journal of Pharmacology and Experimental Therapeutics. 340 (2): 286–294. doi:10.1124/jpet.111.188425. PMID 22034656.
- ^ Hysek CM, Fink AE, Simmler LD, Donzelli M, Grouzmann E, Liechti ME (October 2013). "α₁-Adrenergic receptors contribute to the acute effects of 3,4-methylenedioxymethamphetamine in humans". Journal of Clinical Psychopharmacology. 33 (5): 658–666. doi:10.1097/JCP.0b013e3182979d32. PMID 23857311.
- ^ Liechti ME, Vollenweider FX (July 2000). "Acute psychological and physiological effects of MDMA ("Ecstasy") after haloperidol pretreatment in healthy humans". European Neuropsychopharmacology. 10 (4): 289–295. doi:10.1016/s0924-977x(00)00086-9. PMID 10871712.
- ^ Richards JR, Hollander JE, Ramoska EA, Fareed FN, Sand IC, Izquierdo Gómez MM, et al. (May 2017). "β-Blockers, Cocaine, and the Unopposed α-Stimulation Phenomenon". Journal of Cardiovascular Pharmacology and Therapeutics. 22 (3): 239–249. doi:10.1177/1074248416681644. PMID 28399647.
- ^ a b c "PDSP Database". UNC (in Zulu). Retrieved 11 December 2024.
- ^ a b c Liu T. "BindingDB BDBM50010588 (RS)-3,4-(methylenedioxy)methamphetamine::1-(1,3-Benzodioxol-5-yl)-N-methyl-2-propanamine::1-(1,3-benzodioxol-5-yl)-N-methylpropan-2-amine::3,4-methylenedioxymethamphetamine::CHEMBL43048::DL-(3,4-Methylenedioxy)methamphetamine::MDMA::N,alpha-dimethyl-1,3-benzodioxole-5-ethanamine::N-Methyl-3,4-methylenedioxyamphetamine::US11767305, Compound MDMA". BindingDB. Retrieved 11 December 2024.
- ^ a b c Ray TS (February 2010). "Psychedelics and the human receptorome". PLOS ONE. 5 (2) e9019. Bibcode:2010PLoSO...5.9019R. doi:10.1371/journal.pone.0009019. PMC 2814854. PMID 20126400.
- ^ a b Simmler LD, Buser TA, Donzelli M, Schramm Y, Dieu LH, Huwyler J, et al. (January 2013). "Pharmacological characterization of designer cathinones in vitro". British Journal of Pharmacology. 168 (2): 458–470. doi:10.1111/j.1476-5381.2012.02145.x. PMC 3572571. PMID 22897747.
β-Keto-analogue cathinones also exhibited approximately 10-fold lower affinity for the TA1 receptor compared with their respective non-β-keto amphetamines. [...] Activation of TA1 receptors negatively modulates dopaminergic neurotransmission. Importantly, methamphetamine decreased DAT surface expression via a TA1 receptor-mediated mechanism and thereby reduced the presence of its own pharmacological target (Xie and Miller, 2009). MDMA and amphetamine have been shown to produce enhanced DA and 5-HT release and locomotor activity in TA1 receptor knockout mice compared with wild-type mice (Lindemann et al., 2008; Di Cara et al., 2011). Because methamphetamine and MDMA auto-inhibit their neurochemical and functional effects via TA1 receptors, low affinity for these receptors may result in stronger effects on monoamine systems by cathinones compared with the classic amphetamines.
- ^ Simmler LD, Rickli A, Hoener MC, Liechti ME (April 2014). "Monoamine transporter and receptor interaction profiles of a new series of designer cathinones". Neuropharmacology. 79: 152–160. doi:10.1016/j.neuropharm.2013.11.008. PMID 24275046.
- ^ Rickli A, Kopf S, Hoener MC, Liechti ME (July 2015). "Pharmacological profile of novel psychoactive benzofurans". British Journal of Pharmacology. 172 (13): 3412–3425. doi:10.1111/bph.13128. PMC 4500375. PMID 25765500.
- ^ Luethi D, Kolaczynska KE, Walter M, Suzuki M, Rice KC, Blough BE, et al. (July 2019). "Metabolites of the ring-substituted stimulants MDMA, methylone and MDPV differentially affect human monoaminergic systems". Journal of Psychopharmacology. 33 (7). Oxford, England: 831–841. doi:10.1177/0269881119844185. PMC 8269116. PMID 31038382.
- ^ Eshleman AJ, Forster MJ, Wolfrum KM, Johnson RA, Janowsky A, Gatch MB (March 2014). "Behavioral and neurochemical pharmacology of six psychoactive substituted phenethylamines: mouse locomotion, rat drug discrimination and in vitro receptor and transporter binding and function". Psychopharmacology. 231 (5): 875–888. doi:10.1007/s00213-013-3303-6. PMC 3945162. PMID 24142203.
- ^ a b c d e Gainetdinov RR, Hoener MC, Berry MD (July 2018). "Trace Amines and Their Receptors". Pharmacological Reviews. 70 (3): 549–620. doi:10.1124/pr.117.015305. PMID 29941461.
- ^ a b c d Simmler LD, Buchy D, Chaboz S, Hoener MC, Liechti ME (April 2016). "In Vitro Characterization of Psychoactive Substances at Rat, Mouse, and Human Trace Amine-Associated Receptor 1" (PDF). The Journal of Pharmacology and Experimental Therapeutics. 357 (1): 134–144. doi:10.1124/jpet.115.229765. PMID 26791601. Archived from the original (PDF) on 9 May 2025.
- ^ Sotnikova TD, Caron MG, Gainetdinov RR (August 2009). "Trace amine-associated receptors as emerging therapeutic targets". Molecular Pharmacology. 76 (2): 229–235. doi:10.1124/mol.109.055970. PMC 2713119. PMID 19389919.
- ^ a b Nichols DE (2022). "Entactogens: How the Name for a Novel Class of Psychoactive Agents Originated". Frontiers in Psychiatry. 13 863088. doi:10.3389/fpsyt.2022.863088. PMC 8990025. PMID 35401275.
- ^ a b c d e f g h Docherty JR, Alsufyani HA (August 2021). "Pharmacology of Drugs Used as Stimulants". Journal of Clinical Pharmacology. 61 (Suppl 2): S53 – S69. doi:10.1002/jcph.1918. PMID 34396557.
Receptor-mediated actions of amphetamine and other amphetamine derivatives [...] may involve trace amine-associated receptors (TAARs) at which amphetamine and MDMA also have significant potency.85–87 Many stimulants have potency at the rat TAAR1 in the micromolar range but tend to be about 5 to 10 times less potent at the human TAAR1, [...] Activation of the TAAR1 receptor causes inhibition of dopaminergic transmission in the mesocorticolimbic system, and TAAR1 agonists attenuated psychostimulant abuse-related behaviors.89 It is likely that TAARs contribute to the actions of specific stimulants to modulate dopaminergic, serotonergic, and glutamate signaling,90 and drugs acting on the TAAR1 may have therapeutic potential.91 In the periphery, stimulants such as MDMA and cathinone produce vasoconstriction, part of which may involve TAARs, although only relatively high concentrations produced vascular contractions resistant to a cocktail of monoamine antagonist drugs.86
- ^ a b c Rothman RB, Baumann MH (October 2003). "Monoamine transporters and psychostimulant drugs". European Journal of Pharmacology. 479 (1–3): 23–40. doi:10.1016/j.ejphar.2003.08.054. PMID 14612135.
- ^ a b c d e f Rothman RB, Baumann MH (2006). "Therapeutic potential of monoamine transporter substrates". Current Topics in Medicinal Chemistry. 6 (17): 1845–1859. doi:10.2174/156802606778249766. PMID 17017961.
- ^ a b Sulzer D, Sonders MS, Poulsen NW, Galli A (April 2005). "Mechanisms of neurotransmitter release by amphetamines: a review". Progress in Neurobiology. 75 (6): 406–433. doi:10.1016/j.pneurobio.2005.04.003. PMID 15955613.
- ^ a b Reith ME, Gnegy ME (2020). "Molecular Mechanisms of Amphetamines". Substance Use Disorders. Handbook of Experimental Pharmacology. Vol. 258. pp. 265–297. doi:10.1007/164_2019_251. ISBN 978-3-030-33678-3. PMID 31286212.
- ^ a b Vaughan RA, Henry LK, Foster JD, Brown CR (2024). "Post-translational mechanisms in psychostimulant-induced neurotransmitter efflux". Pharmacological Advances in Central Nervous System Stimulants. Advances in Pharmacology. Vol. 99. pp. 1–33. doi:10.1016/bs.apha.2023.10.003. ISBN 978-0-443-21933-7. PMID 38467478.
- ^ a b Jain MK, Gumpper RH, Slocum ST, Schmitz GP, Madsen JS, Tummino TA, et al. (July 2025). "The polypharmacology of psychedelics reveals multiple targets for potential therapeutics" (PDF). Neuron. 113 (19): 3129–3142.e9. doi:10.1016/j.neuron.2025.06.012. PMID 40683247.
- ^ a b c d e f g h i Pitts EG, Curry DW, Hampshire KN, Young MB, Howell LL (February 2018). "(±)-MDMA and its enantiomers: potential therapeutic advantages of R(-)-MDMA". Psychopharmacology. 235 (2): 377–392. doi:10.1007/s00213-017-4812-5. PMID 29248945.
- ^ a b c d e f g Setola V, Hufeisen SJ, Grande-Allen KJ, Vesely I, Glennon RA, Blough B, et al. (June 2003). "3,4-methylenedioxymethamphetamine (MDMA, "Ecstasy") induces fenfluramine-like proliferative actions on human cardiac valvular interstitial cells in vitro". Molecular Pharmacology. 63 (6): 1223–1229. doi:10.1124/mol.63.6.1223. PMID 12761331. S2CID 839426.
- ^ a b c d e Nash JF, Roth BL, Brodkin JD, Nichols DE, Gudelsky GA (August 1994). "Effect of the R(-) and S(+) isomers of MDA and MDMA on phosphatidyl inositol turnover in cultured cells expressing 5-HT2A or 5-HT2C receptors". Neuroscience Letters. 177 (1–2): 111–115. doi:10.1016/0304-3940(94)90057-4. PMID 7824160.
- ^ Lewin AH, Miller GM, Gilmour B (December 2011). "Trace amine-associated receptor 1 is a stereoselective binding site for compounds in the amphetamine class". Bioorganic & Medicinal Chemistry. 19 (23): 7044–7048. doi:10.1016/j.bmc.2011.10.007. PMC 3236098. PMID 22037049.
- ^ Espinoza S, Gainetdinov RR (2014). "Neuronal Functions and Emerging Pharmacology of TAAR1". Taste and Smell. Topics in Medicinal Chemistry. Vol. 23. Cham: Springer International Publishing. pp. 175–194. doi:10.1007/7355_2014_78. ISBN 978-3-319-48925-4.
Interestingly, the concentrations of amphetamine found to be necessary to activate TAAR1 are in line with what was found in drug abusers [3, 51, 52]. Thus, it is likely that some of the effects produced by amphetamines could be mediated by TAAR1. Indeed, in a study in mice, MDMA effects were found to be mediated in part by TAAR1, in a sense that MDMA auto-inhibits its neurochemical and functional actions [46]. Based on this and other studies (see other section), it has been suggested that TAAR1 could play a role in reward mechanisms and that amphetamine activity on TAAR1 counteracts their known behavioral and neurochemical effects mediated via dopamine neurotransmission.
- ^ Kuropka P, Zawadzki M, Szpot P (May 2023). "A narrative review of the neuropharmacology of synthetic cathinones-Popular alternatives to classical drugs of abuse". Human Psychopharmacology. 38 (3) e2866. doi:10.1002/hup.2866. PMID 36866677.
Another feature that distinguishes [synthetic cathinones (SCs)] from amphetamines is their negligible interaction with the trace amine associated receptor 1 (TAAR1). Activation of this receptor reduces the activity of dopaminergic neurones, thereby reducing psychostimulatory effects and addictive potential (Miller, 2011; Simmler et al., 2016). Amphetamines are potent agonists of this receptor, making them likely to self‐inhibit their stimulating effects. In contrast, SCs show negligible activity towards TAAR1 (Kolaczynska et al., 2021; Rickli et al., 2015; Simmler et al., 2014, 2016). [...] It is worth noting, however, that for TAAR1 there is considerable species variability in its interaction with ligands, and it is possible that the in vitro activity of [rodent TAAR1 agonists] may not translate into activity in the human body (Simmler et al., 2016). The lack of self‐regulation by TAAR1 may partly explain the higher addictive potential of SCs compared to amphetamines (Miller, 2011; Simmler et al., 2013).
- ^ Di Cara B, Maggio R, Aloisi G, Rivet JM, Lundius EG, Yoshitake T, et al. (November 2011). "Genetic deletion of trace amine 1 receptors reveals their role in auto-inhibiting the actions of ecstasy (MDMA)". The Journal of Neuroscience. 31 (47): 16928–16940. doi:10.1523/JNEUROSCI.2502-11.2011. PMC 6623861. PMID 22114263.
- ^ Rein B, Raymond K, Boustani C, Tuy S, Zhang J, St Laurent R, et al. (April 2024). "MDMA enhances empathy-like behaviors in mice via 5-HT release in the nucleus accumbens". Science Advances. 10 (17) eadl6554. Bibcode:2024SciA...10L6554R. doi:10.1126/sciadv.adl6554. PMC 11042730. PMID 38657057.
- ^ Esaki H, Sasaki Y, Nishitani N, Kamada H, Mukai S, Ohshima Y, et al. (May 2023). "Role of 5-HT1A receptors in the basolateral amygdala on 3,4-methylenedioxymethamphetamine-induced prosocial effects in mice". European Journal of Pharmacology. 946 175653. doi:10.1016/j.ejphar.2023.175653. PMID 36907260.
- ^ Heifets BD, Salgado JS, Taylor MD, Hoerbelt P, Cardozo Pinto DF, Steinberg EE, et al. (December 2019). "Distinct neural mechanisms for the prosocial and rewarding properties of MDMA". Science Translational Medicine. 11 (522) eaaw6435. doi:10.1126/scitranslmed.aaw6435. PMC 7123941. PMID 31826983.
- ^ Pitts EG, Minerva AR, Chandler EB, Kohn JN, Logun MT, Sulima A, et al. (September 2017). "3,4-Methylenedioxymethamphetamine Increases Affiliative Behaviors in Squirrel Monkeys in a Serotonin 2A Receptor-Dependent Manner". Neuropsychopharmacology. 42 (10): 1962–1971. doi:10.1038/npp.2017.80. PMC 5561347. PMID 28425496.
- ^ Blanco-Gandía MC, Mateos-García A, García-Pardo MP, Montagud-Romero S, Rodríguez-Arias M, Miñarro J, et al. (September 2015). "Effect of drugs of abuse on social behaviour: a review of animal models". Behavioural Pharmacology. 26 (6): 541–570. doi:10.1097/FBP.0000000000000162. PMID 26221831.
- ^ Heifets BD, Olson DE (January 2024). "Therapeutic mechanisms of psychedelics and entactogens". Neuropsychopharmacology. 49 (1): 104–118. doi:10.1038/s41386-023-01666-5. PMC 10700553. PMID 37488282.
- ^ a b c d Kaur H, Karabulut S, Gauld JW, Fagot SA, Holloway KN, Shaw HE, et al. (2023). "Balancing Therapeutic Efficacy and Safety of MDMA and Novel MDXX Analogues as Novel Treatments for Autism Spectrum Disorder". Psychedelic Medicine. 1 (3). New Rochelle, N.Y.: 166–185. doi:10.1089/psymed.2023.0023. PMC 11661495. PMID 40046567.
It is postulated that MDMA-induced neuronal apoptosis arises from directly stimulating the 5HT2A receptor. However, it is unclear whether MDMA binds here directly or whether one of its active metabolites (for example, MDA exhibits a 5-HT2A affinity almost 10-fold better than MDMA) is responsible.70,80,81 In addition, R-MDMA more potently activates 5-HT2A second messenger signaling, with S-MDMA having a minimal effect and racemic MDMA acting as a weak partial agonist.
- ^ Bankson MG, Cunningham KA (June 2001). "3,4-Methylenedioxymethamphetamine (MDMA) as a unique model of serotonin receptor function and serotonin-dopamine interactions". The Journal of Pharmacology and Experimental Therapeutics. 297 (3): 846–852. doi:10.1016/S0022-3565(24)29607-5. PMID 11356903. Archived from the original on 9 December 2024.
- ^ Baumann MH, Clark RD, Rothman RB (August 2008). "Locomotor stimulation produced by 3,4-methylenedioxymethamphetamine (MDMA) is correlated with dialysate levels of serotonin and dopamine in rat brain". Pharmacology, Biochemistry, and Behavior. 90 (2): 208–217. doi:10.1016/j.pbb.2008.02.018. PMC 2491560. PMID 18403002.
Determining the role of specific 5-HT receptors in MDMA's effects in vivo is complicated by the presence of 14 different 5-HT receptor subtypes (Barnes and Sharp, 1999; Hoyer et al., 2002), many of which affect DA function (Alex and Pehek, 2007; Bubar and Cunningham, 2006). Nonetheless, there is general agreement that 5-HT1B, 5-HT2A and 5-HT2C receptor subtypes influence locomotor effects of MDMA. Hyperactivity produced by MDMA is mimicked by administration of the 5-HT1B agonist RU-24969 (Rempel et al., 1993), and 5-HT1B antagonists inhibit MDMA-induced ambulation (Callaway and Geyer, 1992b; Fletcher et al., 2002; McCreary et al., 1999). 5-HT2A antagonists reduce ambulation produced by MDMA (Fletcher et al., 2002; Kehne et al., 1996), whereas 5-HT2C antagonists markedly enhance it (Bankson and Cunningham, 2002; Fletcher et al., 2006). Taken together, these data reveal that 5-HT1B and 5-HT2A receptors facilitate, while 5-HT2C receptors suppress, forward locomotion evoked by MDMA administration. Importantly, the neural circuits underlying serotonergic modulation of MDMA-induced activity are largely unexplored.
- ^ Bankson MG, Cunningham KA (January 2002). "Pharmacological studies of the acute effects of (+)-3,4-methylenedioxymethamphetamine on locomotor activity: role of 5-HT(1B/1D) and 5-HT(2) receptors". Neuropsychopharmacology. 26 (1): 40–52. doi:10.1016/S0893-133X(01)00345-1. PMID 11751031.
- ^ Cole JC, Sumnall HR (May 2003). "The pre-clinical behavioural pharmacology of 3,4-methylenedioxymethamphetamine (MDMA)". Neuroscience and Biobehavioral Reviews. 27 (3): 199–217. doi:10.1016/s0149-7634(03)00031-9. PMID 12788333.
[...] 5-HT1B receptor agonists elicit locomotor hyperactivity similar to MDMA [247] and transgenic mice lacking the SERT or 5-HT1B receptor show no or reduced MDMA-induced locomotion and a behavioural pattern qualitatively reminiscent of other amphetamines [262,27]. Prior 5-HT depletion or pre-treatment of animals with SSRIs or 5-HT1B receptor antagonists block low dose MDMA hyperkinesis [42,44]. Activation of this receptor subtype may be fundamental in defining MDMAspecific locomotor activity. The 5-HT2A antagonist MDL 100,907 blocked high dose (20 mg/kg) but not low dose (3 mg/kg) MDMA-induced locomotion [157].5-HT2C receptor antagonists potentiated locomotor activation after low dose MDMA [20,115]. It has been proposed that unmasking of 5-HT1B receptor-mediated hyperactivity via 5-HT2C antagonism is only possible in the presence of the elevated DA and 5-HT concentrations seen after MDMA [19].
- ^ Pomrenze MB, Vaillancourt S, Salgado JS, Raymond KB, Llorach P, Sacai H, et al. (July 2025). "5-HT2C receptors in the nucleus accumbens constrain the rewarding effects of MDMA". Molecular Psychiatry. 30 (11): 5405–5416. doi:10.1038/s41380-025-03128-4. PMC 12532699. PMID 40707786.
- ^ Canal CE, Murnane KS (January 2017). "The serotonin 5-HT2C receptor and the non-addictive nature of classic hallucinogens". Journal of Psychopharmacology. 31 (1). Oxford, England: 127–143. doi:10.1177/0269881116677104. PMC 5445387. PMID 27903793.
- ^ Martinez-Price D, Krebs-Thomson K, Geyer M (1 January 2002). "Behavioral Psychopharmacology of MDMA and MDMA-Like Drugs: A Review of Human and Animal Studies". Addiction Research & Theory. 10 (1). Informa UK Limited: 43–67. doi:10.1080/16066350290001704. ISSN 1606-6359.
- ^ Stove CP, De Letter EA, Piette MH, Lambert WE (August 2010). "Mice in ecstasy: advanced animal models in the study of MDMA". Current Pharmaceutical Biotechnology. 11 (5): 421–433. doi:10.2174/138920110791591508. PMID 20420576.
- ^ Doly S, Valjent E, Setola V, Callebert J, Hervé D, Launay JM, et al. (March 2008). "Serotonin 5-HT2B receptors are required for 3,4-methylenedioxymethamphetamine-induced hyperlocomotion and 5-HT release in vivo and in vitro". The Journal of Neuroscience. 28 (11): 2933–2940. doi:10.1523/JNEUROSCI.5723-07.2008. PMC 6670669. PMID 18337424.
Here we show that acute pharmacological inhibition or genetic ablation of the 5-HT2B receptor in mice completely abolishes MDMA-induced hyperlocomotion and 5-HT release in nucleus accumbens and ventral tegmental area. Furthermore, the 5-HT2B receptor dependence of MDMA-stimulated release of endogenous 5-HT from superfused midbrain synaptosomes suggests that 5-HT2B receptors act, unlike any other 5-HT receptor, presynaptically to affect MDMA-stimulated 5-HT release.
- ^ Doly S, Bertran-Gonzalez J, Callebert J, Bruneau A, Banas SM, Belmer A, et al. (23 November 2009). "Role of Serotonin via 5-HT2B Receptors in the Reinforcing Effects of MDMA in Mice". PLOS ONE. 4 (11) e7952. Bibcode:2009PLoSO...4.7952D. doi:10.1371/journal.pone.0007952. ISSN 1932-6203. PMC 2775951. PMID 19956756.
- ^ Belmer A, Quentin E, Diaz SL, Guiard BP, Fernandez SP, Doly S, et al. (2018). "Positive regulation of raphe serotonin neurons by serotonin 2B receptors". Neuropsychopharmacology. 43 (7): 1623–1632. doi:10.1038/s41386-018-0013-0. ISSN 0893-133X. PMC 5983540. PMID 29453444.
- ^ a b Baggott M (23 June 2023). Beyond Ecstasy: Progress in Developing and Understanding a Novel Class of Therapeutic Medicine. PS2023 [Psychedelic Science 2023, June 19–23, 2023, Denver, Colorado]. Denver, CO: Multidisciplinary Association for Psychedelic Studies.
- ^ a b "Better Than Ecstasy: Progress in Developing a Novel Class of Therapeutic with Matthew Baggott, PhD". YouTube. 6 March 2024. Retrieved 20 November 2024.
- ^ a b Rothman RB, Baumann MH (July 2002). "Therapeutic and adverse actions of serotonin transporter substrates". Pharmacology & Therapeutics. 95 (1): 73–88. doi:10.1016/s0163-7258(02)00234-6. PMID 12163129.
- ^ Luethi D, Liechti ME (April 2020). "Designer drugs: mechanism of action and adverse effects" (PDF). Archives of Toxicology. 94 (4): 1085–1133. Bibcode:2020ArTox..94.1085L. doi:10.1007/s00204-020-02693-7. PMC 7225206. PMID 32249347.
- ^ a b c d e f g Liechti ME, Vollenweider FX (December 2001). "Which neuroreceptors mediate the subjective effects of MDMA in humans? A summary of mechanistic studies". Human Psychopharmacology. 16 (8): 589–598. doi:10.1002/hup.348. PMID 12404538.
- ^ a b Schenk S, Newcombe D (December 2018). "Methylenedioxymethamphetamine (MDMA) in Psychiatry: Pros, Cons, and Suggestions". Journal of Clinical Psychopharmacology. 38 (6): 632–638. doi:10.1097/JCP.0000000000000962. PMID 30303861.
- ^ a b c d e Puxty DJ, Ramaekers JG, de la Torre R, Farré M, Pizarro N, Pujadas M, et al. (2017). "MDMA-Induced Dissociative State not Mediated by the 5-HT2A Receptor". Frontiers in Pharmacology. 8 455. doi:10.3389/fphar.2017.00455. PMC 5504523. PMID 28744219.
- ^ a b c Meyer JS (2013). "3,4-methylenedioxymethamphetamine (MDMA): current perspectives". Substance Abuse and Rehabilitation. 4: 83–99. doi:10.2147/SAR.S37258. PMC 3931692. PMID 24648791.
- ^ a b Liechti ME, Baumann C, Gamma A, Vollenweider FX (May 2000). "Acute psychological effects of 3,4-methylenedioxymethamphetamine (MDMA, "Ecstasy") are attenuated by the serotonin uptake inhibitor citalopram". Neuropsychopharmacology. 22 (5): 513–521. doi:10.1016/S0893-133X(99)00148-7. PMID 10731626.
- ^ a b c d Simmler LD, Liechti ME (2018). "Pharmacology of MDMA- and Amphetamine-Like New Psychoactive Substances". New Psychoactive Substances. Handbook of Experimental Pharmacology. Vol. 252. pp. 143–164. doi:10.1007/164_2018_113. ISBN 978-3-030-10560-0. PMID 29633178.
MDMA is also a low-potency partial agonist of the 5-HT2A receptor. Although not frequent, mild hallucinogen-like effects of MDMA have been reported, which may be attributable to 5-HT2A agonism (Nichols 2004; Liechti et al. 2000). MDA, the active metabolite of MDMA (Hysek et al. 2011), shows a tenfold higher potency for 5-HT2A agonism than MDMA (Rickli et al. 2015c). MDA likely contributes to the mode of action of MDMA and might contribute to the mild hallucinogenic effects of MDMA.
- ^ Nichols DE (2018). Chemistry and Structure-Activity Relationships of Psychedelics. Current Topics in Behavioral Neurosciences. Vol. 36. pp. 1–43. doi:10.1007/7854_2017_475. ISBN 978-3-662-55878-2. PMID 28401524.
Although the most active tryptamine hallucinogens are N,N-dialkylated, the phenethylamines generally cannot tolerate even a single N-substitution. Even small groups such as methyl or ethyl (see Table 2) abolish their hallucinogenic activity.
- ^ Jacob P, Shulgin AT (1994). "Structure-Activity Relationships of the Classic Hallucinogens and Their Analogs". In Lin GC, Glennon RA (eds.). Hallucinogens: An Update (PDF). National Institute on Drug Abuse Research Monograph Series. Vol. 146. National Institute on Drug Abuse. pp. 74–91. PMID 8742795. Archived from the original on 13 July 2025.
[MDA] is also remarkable because the N-methyl homolog 3,4 (MDMA) has biological activity, although the nature of its action places it outside of this review. No other phenethylamine hallucinogen retains central activity on N-methylation.
- ^ Halberstadt AL, Geyer MA (2018). "Effect of Hallucinogens on Unconditioned Behavior". Behavioral Neurobiology of Psychedelic Drugs. Current Topics in Behavioral Neurosciences. Vol. 36. pp. 159–199. doi:10.1007/7854_2016_466. ISBN 978-3-662-55878-2. PMC 5787039. PMID 28224459.
[MDxx] have been assessed in head twitch studies. Racemic [MDA] and S-(+)-MDA reportedly induce WDS in monkeys and rats, respectively (Schlemmer and Davis 1986; Hiramatsu et al. 1989). Although [MDMA] does not induce the HTR in mice, both of the stereoisomers of MDMA have been shown to elicit the response (Fantegrossi et al. 2004, 2005b). 5-HT depletion inhibits the response to S-(+)-MDMA but does not alter the response to R-(−)-MDMA, suggesting the isomers act through different mechanisms (Fantegrossi et al. 2005b). This suggestion is consistent with the fact that S-(+)- and R-(−)-MDMA exhibit qualitatively distinct pharmacological profiles, with the S-(+)isomer working primarily as a monoamine releaser (Johnson et al. 1986; Baumann et al. 2008; Murnane et al. 2010) and the R-(−)-enantiomer acting directly through 5-HT2A receptors (Lyon et al. 1986; Nash et al. 1994). In contrast to their effects in mice, Hiramatsu reported that S-(+)- and R-(−)-MDMA fail to produce WDS in rats (Hiramatsu et al. 1989). The discrepant findings with MDMA in mice and rats may reflect species differences in sensitivity to the HTR (see below for further discussion).
- ^ Dunlap LE (2022). Development of Non-Hallucinogenic Psychoplastogens (Thesis). University of California, Davis. Retrieved 18 November 2024.
Finally, since R-MDMA is known to partially substitute for LSD in animal models we decided to test both compounds in the head twitch response assay (HTR) (FIG 3.3C).3 The HTR is a well-validated mouse model for predicting the hallucinogenic potential of test drugs. Serotonergic psychedelics will cause a rapid back and forth head movement in mice. The potency measured in the HTR assay has been shown to correlate very well with the human potencies of psychedelics.18 Neither R-MDMA or [...] produced any head twitches at all doses tested, suggesting that neither has high hallucinogenic potential.
- ^ Nichols DE (2016). "Psychedelics". Pharmacological Reviews. 68 (2): 264–355. doi:10.1124/pr.115.011478. ISSN 0031-6997. PMC 4813425. PMID 26841800.
- ^ Nichols DE, Oberlender R (1989). "Structure-activity relationships of MDMA-like substances". NIDA Research Monograph. 94: 1–29. PMID 2575223.
- ^ Nichols DE, Oberlender R (1990). "Structure-activity relationships of MDMA and related compounds: a new class of psychoactive drugs?". Annals of the New York Academy of Sciences. 600: 613–23, discussion 623–5. doi:10.1007/978-1-4613-1485-1_7. PMID 1979214.
- ^ McIntyre RS (2023). "Serotonin 5-HT2B receptor agonism and valvular heart disease: implications for the development of psilocybin and related agents". Expert Opinion on Drug Safety. 22 (10): 881–883. doi:10.1080/14740338.2023.2248883. PMID 37581427.
- ^ a b c Tagen M, Mantuani D, van Heerden L, Holstein A, Klumpers LE, Knowles R (September 2023). "The risk of chronic psychedelic and MDMA microdosing for valvular heart disease" (PDF). Journal of Psychopharmacology. 37 (9). Oxford, England: 876–890. doi:10.1177/02698811231190865. PMID 37572027.
[...] Both [MDMA and MDA] bind to the human 5-HT2B receptor, although with a 5-fold lower Ki value for MDA compared to MDMA (Ray, 2010; Setola et al., 2003). Both compounds were agonists in an assay of PI hydrolysis, with MDA (EC50=190nM) 10-fold more potent than MDMA (EC50=2000 nM) in addition to greater intrinsic efficacy (90% vs 32%) (Setola et al., 2003). [...] A 50mg dose of MDMA resulted in a mean plasma Cmax 266nM for MDMA and 28.5nM for MDA (de la Torre et al., 2000).
- ^ Rothman RB, Baumann MH (May 2009). "Serotonergic drugs and valvular heart disease". Expert Opinion on Drug Safety. 8 (3): 317–329. doi:10.1517/14740330902931524. PMC 2695569. PMID 19505264.
- ^ Rothman RB, Baumann MH (April 2002). "Serotonin releasing agents. Neurochemical, therapeutic and adverse effects". Pharmacology, Biochemistry, and Behavior. 71 (4): 825–836. doi:10.1016/s0091-3057(01)00669-4. PMID 11888573.
- ^ a b Costa G, Gołembiowska K (January 2022). "Neurotoxicity of MDMA: Main effects and mechanisms" (PDF). Experimental Neurology. 347 113894. doi:10.1016/j.expneurol.2021.113894. hdl:11584/325355. PMID 34655576.
- ^ a b Sprague JE, Everman SL, Nichols DE (June 1998). "An integrated hypothesis for the serotonergic axonal loss induced by 3,4-methylenedioxymethamphetamine". Neurotoxicology. 19 (3): 427–441. PMID 9621349.
- ^ Green AR, Mechan AO, Elliott JM, O'Shea E, Colado MI (September 2003). "The pharmacology and clinical pharmacology of 3,4-methylenedioxymethamphetamine (MDMA, "ecstasy")". Pharmacol Rev. 55 (3): 463–508. doi:10.1124/pr.55.3.3. PMID 12869661.
- ^ Gudelsky GA, Yamamoto BK, Nash JF (November 1994). "Potentiation of 3,4-methylenedioxymethamphetamine-induced dopamine release and serotonin neurotoxicity by 5-HT2 receptor agonists". Eur J Pharmacol. 264 (3): 325–330. doi:10.1016/0014-2999(94)90669-6. PMID 7698172.
- ^ Schmidt CJ, Black CK, Abbate GM, Taylor VL (October 1990). "Methylenedioxymethamphetamine-induced hyperthermia and neurotoxicity are independently mediated by 5-HT2 receptors". Brain Res. 529 (1–2): 85–90. doi:10.1016/0006-8993(90)90813-q. PMID 1980848.
- ^ Armstrong BD, Paik E, Chhith S, Lelievre V, Waschek JA, Howard SG (2004). "Potentiation of (DL)-3,4-methylenedioxymethamphetamine (MDMA)-induced toxicity by the serotonin 2A receptior partial agonist d-lysergic acid diethylamide (LSD), and the protection of same by the serotonin 2A/2C receptor antagonist MDL 11,939". Neuroscience Research Communications. 35 (2): 83–95. doi:10.1002/nrc.20023.
- ^ Anderson GM, Braun G, Braun U, Nichols DE, Shulgin AT (1978). "Absolute configuration and psychotomimetic activity". NIDA Research Monograph (22): 8–15. PMID 101890.
- ^ Acquas E, Pisanu A, Spiga S, Plumitallo A, Zernig G, Di Chiara G (July 2007). "Differential effects of intravenous R,S-(+/-)-3,4-methylenedioxymethamphetamine (MDMA, Ecstasy) and its S(+)- and R(-)-enantiomers on dopamine transmission and extracellular signal regulated kinase phosphorylation (pERK) in the rat nucleus accumbens shell and core". Journal of Neurochemistry. 102 (1): 121–132. doi:10.1111/j.1471-4159.2007.04451.x. PMID 17564678.
- ^ Curry DW, Young MB, Tran AN, Daoud GE, Howell LL (January 2018). "Separating the agony from ecstasy: R(-)-3,4-methylenedioxymethamphetamine has prosocial and therapeutic-like effects without signs of neurotoxicity in mice". Neuropharmacology. 128: 196–206. doi:10.1016/j.neuropharm.2017.10.003. PMC 5714650. PMID 28993129.
- ^ a b Bedi G (October 2024). "Is the stereoisomer R-MDMA a safer version of MDMA?". Neuropsychopharmacology. 50 (2): 360–361. doi:10.1038/s41386-024-02009-8. PMC 11631934. PMID 39448866.
- ^ Luethi D, Liechti ME (2021). "Drugs of Abuse Affecting 5-HT2B Receptors". 5-HT2B Receptors. The Receptors. Vol. 35. Cham: Springer International Publishing. pp. 277–289. doi:10.1007/978-3-030-55920-5_16. ISBN 978-3-030-55919-9.
Notably, in a study by Rickli and colleagues, MDMA did not activate the 5-HT2B receptor in the functional assay at investigated concentrations (EC50 > 20 μM); however, [MDA], the main psychoactive N-demethylated phase I metabolite of MDMA, potently activated the receptor at submicromolar concentrations [14]. This suggests that the metabolite MDA rather than MDMA itself may lead to valvulopathy and that there could be a significant metabolic contribution to MDMA-induced effects and adverse effect.
- ^ Mead J, Parrott A (May 2020). "Mephedrone and MDMA: A comparative review". Brain Research. 1735 146740. doi:10.1016/j.brainres.2020.146740. PMID 32087112.
A controlled study on eight experienced MDMA users reported that 1.5 mg/kg (comparable to what was deemed a typical dosage amount) consumed orally resulted in the subjective effects peaking within 2 h of ingestion (Harris et al., 2002). Other research indicates effects to emerge between 20 and 60 min, with them peaking between 60 and 90 min and lasting up to 5 h (Green et al., 2003). A dose of 100 mg has a half-life of 8–9h(De la Torre et al., 2004), although as mentioned above, users are unaware of the dose they ingest.
- ^ Ermer JC, Pennick M, Frick G (May 2016). "Lisdexamfetamine Dimesylate: Prodrug Delivery, Amphetamine Exposure and Duration of Efficacy". Clinical Drug Investigation. 36 (5): 341–356. doi:10.1007/s40261-015-0354-y. PMC 4823324. PMID 27021968.
- ^ Cruickshank CC, Dyer KR (July 2009). "A review of the clinical pharmacology of methamphetamine". Addiction. 104 (7). Abingdon, England: 1085–1099. doi:10.1111/j.1360-0443.2009.02564.x. PMID 19426289.
Metabolism does not appear to be altered by chronic exposure, thus dose escalation appears to arise from pharmacodynamic rather than pharmacokinetic tolerance [24]. [...] The terminal plasma half-life of methamphetamine of approximately 10 hours is similar across administration routes, but with substantial inter-individual variability. Acute effects persist for up to 8 hours following a single moderate dose of 30 mg [30]. [...] peak plasma methamphetamine concentration occurs after 4 hours [35]. Nevertheless, peak cardiovascular and subjective effects occur rapidly (within 5–15 minutes). The dissociation between peak plasma concentration and clinical effects indicates acute tolerance, which may reflect rapid molecular processes such as redistribution of vesicular monoamines and internalization of monoamine receptors and transporters [6,36]. Acute subjective effects diminish over 4 hours, while cardiovascular effects tend to remain elevated. This is important, as the marked acute tachyphylaxis to subjective effects may drive repeated use within intervals of 4 hours, while cardiovascular risks may increase [11,35].
- ^ Abbas K, Barnhardt EW, Nash PL, Streng M, Coury DL (April 2024). "A review of amphetamine extended release once-daily options for the management of attention-deficit hyperactivity disorder". Expert Review of Neurotherapeutics. 24 (4): 421–432. doi:10.1080/14737175.2024.2321921. PMID 38391788.
For several decades, clinical benefits of amphetamines have been limited by the pharmacologic half-life of around 4 hours. Although higher doses can produce higher maximum concentrations, they do not affect the half-life of the dose. Therefore, to achieve longer durations of effect, stimulants had to be dosed at least twice daily. Further, these immediate-release doses were found to have their greatest effect shortly after administration, with a rapid decline in effect after reaching peak blood concentrations. The clinical correlation of this was found in comparing math problems attempted and solved between a mixed amphetamine salts preparation (MAS) 10 mg once at 8 am vs 8 am followed by 12 pm [14]. The study also demonstrated the phenomenon of acute tolerance, where even if blood concentrations were maintained over the course of the day, clinical efficacy in the form of math problems attempted and solved would diminish over the course of the day. These findings eventually led to the development of a once daily preparation (MAS XR) [15], which is a composition of 50% immediate-release beads and 50% delayed release beads intended to mimic this twice-daily dosing with only a single administration.
- ^ van Gaalen MM, Schlumbohm C, Folgering JH, Adhikari S, Bhattacharya C, Steinbach D, et al. (April 2019). "Development of a Semimechanistic Pharmacokinetic-Pharmacodynamic Model Describing Dextroamphetamine Exposure and Striatal Dopamine Response in Rats and Nonhuman Primates following a Single Dose of Dextroamphetamine". The Journal of Pharmacology and Experimental Therapeutics. 369 (1): 107–120. doi:10.1124/jpet.118.254508. PMID 30733244.
Acute tolerance has been demonstrated for methamphetamine in rats (Segal and Kuczenski, 2006), and for D-amphetamine in rats (Lewander, 1971), [non-human primates (NHPs)] (Jedema et al., 2014) and humans (Angrist et al., 1987; Brauer et al., 1996; Dolder et al., 2017). In vivo measurement of dopamine by microdialysis was used in rats and NHPs to evaluate these time-dependent effects. In humans, various subjective measures of mood related to the drug's euphoric effects were observed to decline more rapidly than plasma concentrations following D-amphetamine oral doses ranging from 20 to 40 mg (Angrist et al., 1987; Brauer et al., 1996; Dolder et al., 2017). Whereas peak plasma concentrations and subjective effects occurred between 2 and 4 hours following administration, drug effect measures had largely returned to baseline values by 8 hours despite continued exposure to the drug (mean half-life = 8 hours following a 40 mg dose (Dolder et al., 2017)).
- ^ Bisagno V, Cadet JL (2021). "Methamphetamine and MDMA Neurotoxicity: Biochemical and Molecular Mechanisms". Handbook of Neurotoxicity. Cham: Springer International Publishing. pp. 1–24. doi:10.1007/978-3-030-71519-9_80-1. ISBN 978-3-030-71519-9.
Injections of large doses of MDMA cause massive release of 5-HT from presynaptic vesicles, followed by a rapid decrease in 5-HT and 5-hydroxyindoleacetic acid (5-HIAA) levels and decreased TPH activity (Górska et al., 2018; Lyles & Cadet, 2003). There do not appear to be losses of 5-HT uptake sites at early time points after MDMA administration (Lyles & Cadet, 2003). [...] MDMA also perturbs the function of SERT (Green et al., 2003), a marker of the integrity of serotonin neurons (Blakely et al., 1994). By virtue of its moderating synaptic 5-HT levels, SERT is crucial for the process of 5-HT neurotransmission (Green et al., 2003). MDMA downregulates SERT function without altering SERT mRNA or protein expression, and this rapid downregulation is sustained for at least 90 min and is dose-dependent (Kivell et al., 2010).
- ^ Kivell B, Day D, Bosch P, Schenk S, Miller J (June 2010). "MDMA causes a redistribution of serotonin transporter from the cell surface to the intracellular compartment by a mechanism independent of phospho-p38-mitogen activated protein kinase activation". Neuroscience. 168 (1): 82–95. doi:10.1016/j.neuroscience.2010.03.018. PMID 20298763.
- ^ Holley A, Simonson B, Kivell BM (April 2013). "MDMA regulates serotonin transporter function via a Protein kinase C dependent mechanism". Journal of Addiction & Prevention. 1 (1): 5. ISSN 2330-2178.
- ^ a b Underhill S, Amara S (2020). "MDMA and TAAR1-mediated RhoA Activation in Serotonin Neurons". The FASEB Journal. 34 (S1): 1. doi:10.1096/fasebj.2020.34.s1.05856. ISSN 0892-6638.
- ^ a b Underhill S, Amara S (2022). "3,4-methylenedioxymethamphetamine (MDMA) stimulates activation of TAAR1 and subsequent neurotransmitter transporter internalization in serotonin neurons". The FASEB Journal. 36 (S1) fasebj.2022.36.S1.R5394. doi:10.1096/fasebj.2022.36.S1.R5394. ISSN 0892-6638.
- ^ Kittler K, Lau T, Schloss P (March 2010). "Antagonists and substrates differentially regulate serotonin transporter cell surface expression in serotonergic neurons". European Journal of Pharmacology. 629 (1–3): 63–67. doi:10.1016/j.ejphar.2009.12.010. PMID 20006597.
Our results show that exposure to the SSRIs citalopram, fluoxetine, sertraline and paroxetine all induced SERT internalization, but with different efficacies. The substrates 5-HT and MDMA also induced SERT internalization, while cocaine elevated SERT cell surface expression.
- ^ Rothman RB, Baumann MH, Dersch CM, Romero DV, Rice KC, Carroll FI, et al. (January 2001). "Amphetamine-type central nervous system stimulants release norepinephrine more potently than they release dopamine and serotonin". Synapse. 39 (1). New York, N.Y.: 32–41. doi:10.1002/1098-2396(20010101)39:1<32::AID-SYN5>3.0.CO;2-3. PMID 11071707. S2CID 15573624.
- ^ Rothman RB, Partilla JS, Baumann MH, Lightfoot-Siordia C, Blough BE (April 2012). "Studies of the biogenic amine transporters. 14. Identification of low-efficacy "partial" substrates for the biogenic amine transporters". The Journal of Pharmacology and Experimental Therapeutics. 341 (1): 251–262. doi:10.1124/jpet.111.188946. PMC 3364510. PMID 22271821.
- ^ Marusich JA, Antonazzo KR, Blough BE, Brandt SD, Kavanagh PV, Partilla JS, et al. (February 2016). "The new psychoactive substances 5-(2-aminopropyl)indole (5-IT) and 6-(2-aminopropyl)indole (6-IT) interact with monoamine transporters in brain tissue". Neuropharmacology. 101: 68–75. doi:10.1016/j.neuropharm.2015.09.004. PMC 4681602. PMID 26362361.
- ^ Nagai F, Nonaka R, Satoh Hisashi Kamimura K (March 2007). "The effects of non-medically used psychoactive drugs on monoamine neurotransmission in rat brain". European Journal of Pharmacology. 559 (2–3): 132–137. doi:10.1016/j.ejphar.2006.11.075. PMID 17223101.
- ^ Halberstadt AL, Brandt SD, Walther D, Baumann MH (March 2019). "2-Aminoindan and its ring-substituted derivatives interact with plasma membrane monoamine transporters and α2-adrenergic receptors". Psychopharmacology. 236 (3): 989–999. doi:10.1007/s00213-019-05207-1. PMC 6848746. PMID 30904940.
- ^ Blough B (July 2008). "Dopamine-releasing agents" (PDF). In Trudell ML, Izenwasser S (eds.). Dopamine Transporters: Chemistry, Biology and Pharmacology. Hoboken [NJ]: Wiley. pp. 305–320. ISBN 978-0-470-11790-3. OCLC 181862653. OL 18589888W.
- ^ Kolaczynska KE, Ducret P, Trachsel D, Hoener MC, Liechti ME, Luethi D (June 2022). "Pharmacological characterization of 3,4-methylenedioxyamphetamine (MDA) analogs and two amphetamine-based compounds: N,α-DEPEA and DPIA". European Neuropsychopharmacology. 59: 9–22. doi:10.1016/j.euroneuro.2022.03.006. PMID 35378384.
- ^ Mas M, Farré M, de la Torre R, Roset PN, Ortuño J, Segura J, et al. (July 1999). "Cardiovascular and neuroendocrine effects and pharmacokinetics of 3, 4-methylenedioxymethamphetamine in humans". The Journal of Pharmacology and Experimental Therapeutics. 290 (1): 136–145. doi:10.1016/S0022-3565(24)34877-3. PMID 10381769.
- ^ a b de la Torre R, Farré M, Ortuño J, Mas M, Brenneisen R, Roset PN, et al. (February 2000). "Non-linear pharmacokinetics of MDMA ('ecstasy') in humans". British Journal of Clinical Pharmacology. 49 (2): 104–109. doi:10.1046/j.1365-2125.2000.00121.x. PMC 2014905. PMID 10671903.
- ^ Farré M, Roset PN, Lopez CH, Mas M, Ortuño J, Menoyo E, et al. (September 2000). "Pharmacology of MDMA in humans". Annals of the New York Academy of Sciences. 914 (1): 225–237. Bibcode:2000NYASA.914..225D. doi:10.1111/j.1749-6632.2000.tb05199.x. PMID 11085324. S2CID 29247621.
- ^ a b Kolbrich EA, Goodwin RS, Gorelick DA, Hayes RJ, Stein EA, Huestis MA (June 2008). "Plasma pharmacokinetics of 3,4-methylenedioxymethamphetamine after controlled oral administration to young adults". Therapeutic Drug Monitoring. 30 (3): 320–332. doi:10.1097/FTD.0b013e3181684fa0. PMC 2663855. PMID 18520604.
- ^ Shima N, Kamata H, Katagi M, Tsuchihashi H, Sakuma T, Nemoto N (September 2007). "Direct determination of glucuronide and sulfate of 4-hydroxy-3-methoxymethamphetamine, the main metabolite of MDMA, in human urine". Journal of Chromatography. B, Analytical Technologies in the Biomedical and Life Sciences. 857 (1): 123–129. doi:10.1016/j.jchromb.2007.07.003. PMID 17643356.
- ^ Fallon JK, Kicman AT, Henry JA, Milligan PJ, Cowan DA, Hutt AJ (July 1999). "Stereospecific analysis and enantiomeric disposition of 3, 4-methylenedioxymethamphetamine (Ecstasy) in humans". Clinical Chemistry. 45 (7): 1058–1069. doi:10.1093/clinchem/45.7.1058. PMID 10388483.
- ^ Mueller M, Peters FT, Maurer HH, McCann UD, Ricaurte GA (October 2008). "Nonlinear pharmacokinetics of (+/-)3,4-methylenedioxymethamphetamine (MDMA, "Ecstasy") and its major metabolites in squirrel monkeys at plasma concentrations of MDMA that develop after typical psychoactive doses". The Journal of Pharmacology and Experimental Therapeutics. 327 (1): 38–44. doi:10.1124/jpet.108.141366. PMID 18591215. S2CID 38043715.
- ^ Milhazes N, Martins P, Uriarte E, Garrido J, Calheiros R, Marques MP, et al. (July 2007). "Electrochemical and spectroscopic characterisation of amphetamine-like drugs: application to the screening of 3,4-methylenedioxymethamphetamine (MDMA) and its synthetic precursors". Analytica Chimica Acta. 596 (2): 231–241. Bibcode:2007AcAC..596..231M. doi:10.1016/j.aca.2007.06.027. hdl:10316/45124. PMID 17631101.
- ^ Milhazes N, Cunha-Oliveira T, Martins P, Garrido J, Oliveira C, Rego AC, et al. (October 2006). "Synthesis and cytotoxic profile of 3,4-methylenedioxymethamphetamine ("ecstasy") and its metabolites on undifferentiated PC12 cells: A putative structure-toxicity relationship" (PDF). Chemical Research in Toxicology. 19 (10): 1294–1304. doi:10.1021/tx060123i. hdl:10316/12872. PMID 17040098. Archived (PDF) from the original on 28 June 2021. Retrieved 24 September 2019.
- ^ Baxter EW, Reitz AB (April 2004). "Reductive aminations of carbonyl compounds with borohydride and borane reducing agents". Organic Reactions. 59. Hoboken, New Jersey, United States: 59. doi:10.1002/0471264180.or059.01. ISBN 978-0-471-26418-7.
- ^ Gimeno P, Besacier F, Bottex M, Dujourdy L, Chaudron-Thozet H (December 2005). "A study of impurities in intermediates and 3,4-methylenedioxymethamphetamine (MDMA) samples produced via reductive amination routes". Forensic Science International. 155 (2–3): 141–157. doi:10.1016/j.forsciint.2004.11.013. PMID 16226151.
- ^ Palhol F, Boyer S, Naulet N, Chabrillat M (September 2002). "Impurity profiling of seized MDMA tablets by capillary gas chromatography". Analytical and Bioanalytical Chemistry. 374 (2): 274–281. doi:10.1007/s00216-002-1477-6. PMID 12324849. S2CID 42666306.
- ^ Renton RJ, Cowie JS, Oon MC (August 1993). "A study of the precursors, intermediates and reaction by-products in the synthesis of 3,4-methylenedioxymethylamphetamine and its application to forensic drug analysis". Forensic Science International. 60 (3): 189–202. doi:10.1016/0379-0738(93)90238-6. PMID 7901132.
- ^ Mohan J, ed. (June 2014). World Drug Report 2014 (PDF). Vienna, Austria: United Nations Office on Drugs and Crime. pp. 2, 3, 123–152. ISBN 978-92-1-056752-7. Archived (PDF) from the original on 13 November 2014. Retrieved 1 December 2014.
- ^ "Early Warning - MDMA and MDA Producers Using Ocotea Cymbarum as a Precursor" (PDF). DEA Microgram Newsletter. 38 (11). Drug Enforcement Agency, U.S. Department of Justice: 166. 11 November 2005. Archived from the original (PDF) on 18 October 2012.
- ^ Barnes AJ, De Martinis BS, Gorelick DA, Goodwin RS, Kolbrich EA, Huestis MA (March 2009). "Disposition of MDMA and metabolites in human sweat following controlled MDMA administration". Clinical Chemistry. 55 (3): 454–462. doi:10.1373/clinchem.2008.117093. PMC 2669283. PMID 19168553.
- ^ Baselt RC (2011). Disposition of toxic drugs and chemicals in man (9th ed.). Seal Beach, Ca.: Biomedical Publications. pp. 1078–1080. ISBN 978-0-9626523-8-7.
- ^ a b c d e f g h i Passie T (29 June 2023). The History of MDMA. Oxford University Press. pp. 6–16, 18, 27, 29, 32, 40. doi:10.1093/oso/9780198867364.001.0001. ISBN 978-0-19-886736-4.
- ^ a b c d Bernschneider-Reif S, Oxler F, Freudenmann RW (November 2006). "The origin of MDMA ("ecstasy")--separating the facts from the myth". Die Pharmazie. 61 (11): 966–972. PMID 17152992.
- ^ Darmstadt FE (16 May 1914). "German Patent 274350: Verfahren zur Darstellung von Alkyloxyaryl-, Dialkyloxyaryl- und Alkylendioxyarylaminopropanen bzw. deren am Stickstoff monoalkylierten Derivaten". Kaiserliches Patentamt. Archived from the original on 28 August 2021. Retrieved 12 April 2009.
- ^ Darmstadt FE (15 October 1914). "German Patent 279194: Verfahren zur Darstellung von Hydrastinin Derivaten". Kaiserliches Patentamt. Archived from the original on 28 August 2021. Retrieved 20 July 2009.
- ^ Shulgin AT (1990). "History of MDMA". In Peroutka SJ (ed.). Ecstasy: The Clinical, Pharmacological and Neurotoxicological Effects of the Drug MDMA. Topics in the Neurosciences. Vol. 9. Boston, MA: Springer US. pp. 1–20 (2, 14). doi:10.1007/978-1-4613-1485-1_1. ISBN 978-1-4612-8799-5. Retrieved 15 May 2025.
- ^ a b Alles GA (1959). "Some Relations Between Chemical Structure and Physiological Action of Mescaline and Related Compounds / Structure and Action of Phenethylamines". In Abramson HA (ed.). Neuropharmacology: Transactions of the Fourth Conference, September 25, 26, and 27, 1957, Princeton, N. J. New York: Josiah Macy Foundation. pp. 181–268. OCLC 9802642. Archived from the original on 21 March 2025.
- ^ a b Alles GA (1959). "Subjective Reactions to Phenethylamine Hallucinogens". A Pharmacologic Approach to the Study of the Mind. Springfield: CC Thomas. pp. 238–250 (241–246). ISBN 978-0-398-04254-7.
{{cite book}}: ISBN / Date incompatibility (help) - ^ a b c d e f g h i j k Benzenhöfer U, Passie T (August 2010). "Rediscovering MDMA (ecstasy): the role of the American chemist Alexander T. Shulgin". Addiction. 105 (8). Abingdon, England: 1355–1361. doi:10.1111/j.1360-0443.2010.02948.x. PMID 20653618.
- ^ Hardman HF, Haavik CO, Seevers MH (June 1973). "Relationship of the structure of mescaline and seven analogs to toxicity and behavior in five species of laboratory animals". Toxicology and Applied Pharmacology. 25 (2): 299–309. Bibcode:1973ToxAP..25..299H. doi:10.1016/S0041-008X(73)80016-X. hdl:2027.42/33868. PMID 4197635. Archived from the original on 21 October 2008. Retrieved 19 April 2009.
- ^ Biniecki S, Krajewski E (1960). "Production of d,1-N-methyl-beta-(3,4-methylenedioxyphenyl)-isopropylamine and d,1-N-methyl-beta-(3,4-dimthoxyphenyl)-isopropylamine". Acta Polon Pharm (in Polish). 17: 421–425.
- ^ a b c Siegel RK (October 1986). "MDMA. Nonmedical use and intoxication" (PDF). Journal of Psychoactive Drugs. 18 (4): 349–354. doi:10.1080/02791072.1986.10472368. PMID 2880950. Archived (PDF) from the original on 4 March 2016. Retrieved 11 August 2015.
- ^ The first confirmed sample was seized and identified by Chicago Police in 1970, see Sreenivasan VR (1972). "Problems in Identification of Methylenedioxy and Methoxy Amphetamines". Journal of Criminal Law, Criminology, and Police Science. 63 (2): 304–312. doi:10.2307/1142315. JSTOR 1142315. Archived from the original on 21 October 2008. Retrieved 19 April 2009.
- ^ a b Foderaro LW (11 December 1988). "Psychedelic Drug Called Ecstasy Gains Popularity in Manhattan Nightclubs". The New York Times. Archived from the original on 17 November 2015. Retrieved 27 August 2015.
- ^ a b c d Brown E (September 2002). "Professor X". Wired. Archived from the original on 25 June 2015. Retrieved 4 January 2015.
- ^ a b Beck JE (April 1987). "Drug Abuse Series: MDMA". Erowid. Drug Abuse Information and Monitoring Project. Archived from the original on 4 August 2015. Retrieved 6 August 2015.
- ^ a b c d e f g h Pentney AR (2001). "An exploration of the history and controversies surrounding MDMA and MDA". Journal of Psychoactive Drugs. 33 (3): 213–221. doi:10.1080/02791072.2001.10400568. PMID 11718314. S2CID 31142434.
- ^ "Alexander 'Sasha' Shulgin". Alexander Shulgin Research Institute. Archived from the original on 20 December 2014. Retrieved 8 January 2015.
- ^ a b c d Shulgin AT, Shulgin A (1991). "Chapters 12, 22". PiHKAL: A Chemical Love Story (7th printing, 1st ed.). Berkeley, CA: Transform Press. ISBN 978-0-9630096-0-9.
- ^ Shulgin AT, Nichols DE (1978). "Characterization of Three New Psychotomimetics". In Willette RE, Stillman RJ (eds.). The Psychopharmacology of Hallucinogens. New York: Pergamon Press. pp. 74–83. ISBN 978-0-08-021938-7. Archived from the original on 15 May 2013. Retrieved 4 January 2015.
- ^ a b c d Bennett D (30 January 2005). "Dr. Ecstasy". The New York Times Magazine. Archived from the original on 17 November 2011. Retrieved 10 February 2017.
- ^ a b c d e f Jennings P (1 April 2004). "Ecstasy Rising". Primetime Thursday. No. Special edition. ABC News. Archived from the original on 27 May 2015.
- ^ Shulgin A (2004). "Tribute to Jacob" (PDF). In Doblin R (ed.). The Secret Chief Revealed (2nd ed.). Sarasota, Fl: Multidisciplinary Association for Psychedelic Studies. pp. 17–18. ISBN 978-0-9660019-6-9. Archived from the original (PDF) on 16 September 2018. Retrieved 7 January 2015.
- ^ a b "Ecstasy on Prescription". BBC Business Daily. 29 May 2018. Archived from the original on 10 July 2021. Retrieved 10 July 2021.
- ^ Milroy CM (February 1999). "Ten years of 'ecstasy'". Journal of the Royal Society of Medicine. 92 (2): 68–72. doi:10.1177/014107689909200206. PMC 1297063. PMID 10450215.
- ^ a b c d e f g h Eisner B (1994). Ecstasy: The MDMA Story (Expanded 2nd ed.). Berkeley, CA: Ronin Publishing. ISBN 978-0-914171-68-3. Archived from the original on 13 January 2023. Retrieved 1 February 2016.
- ^ a b c d e f g h i j k l m n Beck J, Rosenbaum M (1994). "The Distribution of Ecstasy". Pursuit of Ecstasy: The MDMA Experience. Albany: State Univ. of New York Press. ISBN 978-0-7914-1817-8.
- ^ a b c d Doblin R, Rosenbaum M (1991). "Chapter 6: Why MDMA Should Not Have Been Made Illegal" (PDF). In Inciardi JA (ed.). The Drug Legalization Debate (2nd ed.). London: SAGE Publications, Inc. ISBN 978-0-8039-3678-2. Retrieved 10 August 2015.
- ^ Collin M, Godfrey J (2010). "The Technologies of Pleasure". Altered State: The Story of Ecstasy Culture and Acid House (Updated new ed.). London: Profile Books. ISBN 978-1-84765-641-4.
- ^ Savlov M (12 June 2000). "Countdown to Ecstasy: A New Drug for a New Millennium". The Austin Chronicle. Weekly Wire. Archived from the original on 21 January 2016. Retrieved 6 August 2015.
- ^ Owen F, Gavin L (20 October 2013). "Molly Isn't Who You Think She Is: A Deeper Look at MDMA". Playboy. Archived from the original on 27 July 2015. Retrieved 6 August 2015.
- ^ Sylvan R (2005). "A Brief History of the Rave Scene". Trance Formation: The Spiritual and Religious Dimensions of Global Rave Culture. New York, NY: Routledge. pp. 21–22. ISBN 978-0-415-97090-7.
- ^ Parrott AC (May 2004). "Is ecstasy MDMA? A review of the proportion of ecstasy tablets containing MDMA, their dosage levels, and the changing perceptions of purity" (PDF). Psychopharmacology. 173 (3–4): 234–241. doi:10.1007/s00213-003-1712-7. PMID 15007594. S2CID 3347303. Archived (PDF) from the original on 18 September 2015. Retrieved 7 August 2015.
- ^ Renfroe CL (October 1986). "MDMA on the street: Analysis Anonymous". Journal of Psychoactive Drugs. 18 (4): 363–369. doi:10.1080/02791072.1986.10472371. PMID 2880953.
- ^ "Schedules of Controlled Substances Proposed Placement of 3,4-Methylenedioxymethamphetamine in Schedule I" (PDF). Federal Register. 49 (146) 30210. 27 July 1984. Archived (PDF) from the original on 4 March 2016. Retrieved 15 January 2015.
- ^ Adler J, Abramson P, Katz S, Hager M (15 April 1985). "Getting High on 'Ecstasy'" (PDF). Newsweek Magazine. Life/Style. p. 96. Archived (PDF) from the original on 20 April 2016. Retrieved 1 February 2015.
- ^ a b c Holland J (2001). "The History of MDMA". In Holland J (ed.). Ecstasy: the complete guide; a comprehensive look at the risks and benefits of MDMA. Rochester, VT: Park Street Press. ISBN 978-0-89281-857-0.
- ^ a b "U.S. will ban 'ecstasy,' a hallucinogenic drug". The New York Times. The Associated Press. 1 June 1985. Archived from the original on 24 May 2015. Retrieved 29 April 2015.
- ^ "MDMA – FDA REPORT, 1985". Erowid. Food and Drug Administration. 1985. Archived from the original on 11 August 2015. Retrieved 11 August 2015.
- ^ Baker K (30 May 1985). "DEA To Ban "Ecstasy" – The Drug MDMA". The Associated Press. Archived from the original on 31 August 2018. Retrieved 7 August 2015.
- ^ Corwin M (31 May 1985). "U.S. to Ban Use of Drug MDMA: Street Abuse Cited; Used by Psychiatrists". Los Angeles Times. Archived from the original on 17 November 2015. Retrieved 11 August 2015.
- ^ Weber B (7 June 2014). "Alexander Shulgin, Psychedelia Researcher, Dies at 88". The New York Times. Archived from the original on 5 September 2015. Retrieved 28 August 2015.
- ^ Vastag B (3 June 2014). "Chemist Alexander Shulgin, popularizer of the drug Ecstasy, dies at 88". The Washington Post. WP Company LLC. Archived from the original on 5 August 2015. Retrieved 28 August 2015.
- ^ "Ecstasy has its pros and cons". Kokomo Tribune. Kokomo, Indiana. Harper's Bazaar. 23 November 1985. p. 6. Archived from the original on 28 August 2021. Retrieved 9 September 2017 – via newspaperarchive.com.

- ^ "Lester Grinspoon, M.d., Petitioner, v. Drug Enforcement Administration, Respondent, 828 F.2d 881 (1st Cir. 1987)". Justia Law. US Court of Appeals for the First Circuit. Archived from the original on 9 October 2021. Retrieved 9 October 2021.
- ^ Halvorsen JØ, Naudet F, Cristea IA (October 2021). "Challenges with benchmarking of MDMA-assisted psychotherapy" (PDF). Nature Medicine. 27 (10): 1689–1690. doi:10.1038/s41591-021-01525-0. PMID 34635857. S2CID 238636360. Archived (PDF) from the original on 22 May 2022. Retrieved 9 May 2022.
- ^ WHO Expert Committee on Drug Dependence: Twenty-second Report (PDF). Geneva: World Health Organization. 1985. pp. 24–25. Archived from the original (PDF) on 19 October 2014. Retrieved 29 August 2012.
- ^ "Decision to place MDMA into Schedule I" (PDF). UNODC. Commission on Narcotic Drugs. 11 February 1986. Archived (PDF) from the original on 22 September 2015. Retrieved 9 May 2015.
- ^ McKinley JC (12 September 2013). "Overdoses of 'Molly' Led to Electric Zoo Deaths". The New York Times. Archived from the original on 4 December 2013. Retrieved 9 December 2013.
- ^ Nelson LS, Lewin NA, Howland MA, Hoffman RS, Goldfrank LR, Flomenbaum NE (2011). Goldfrank's toxicologic emergencies (9th ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-160593-9.
- ^ "Bibliography of Psychedelic Research Studies". Multidisciplinary Association for Psychedelic Studies (MAPS). Santa Cruz, CA. Archived from the original on 3 December 2013.
- ^ James SD (23 February 2015). "What Is Molly and Why Is It Dangerous?". NBCNews.com. Archived from the original on 24 February 2015. Retrieved 23 February 2015.
Why is it called Molly? That's short for "molecule." "You can put a ribbon and bow on it and call it a cute name like 'Molly' and people are all in," said Paul Doering, professor emeritus of pharmacology at the University of Florida.
- ^ Aleksander I (21 June 2013). "Molly: Pure, but Not So Simple". The New York Times. Archived from the original on 1 January 2022. Retrieved 24 February 2015.
- ^ "Mephedrone (4-Methylmethcathinone) appearing in "Ecstasy" in the Netherlands". 19 September 2010. Archived from the original on 5 November 2012. Retrieved 31 December 2012.
- ^ "Why ecstasy is 'vanishing' from UK nightclubs". BBC News. 19 January 2010. Archived from the original on 7 September 2017. Retrieved 14 February 2010.
- ^ Bish J (4 August 2017). "Watch Out for Pentylone, the Horrible New MDMA Additive". Vice. Archived from the original on 1 September 2020. Retrieved 31 May 2018.
- ^ Williamson L (7 March 2025). "MDMA may have protected Nova attack survivors from trauma, study suggests". BBC Home. Retrieved 16 March 2025.
- ^ Burns B (8 March 2025). "MDMA and LSD may have helped October 7 survivors". news.com.au. Retrieved 16 March 2025.
- ^ "Annual prevalence of use of drugs, by region and globally, 2016". World Drug Report 2018. United Nations Office on Drugs and Crime. 2018. Retrieved 7 July 2018.
- ^ "MDMA and psilocybin: What GPs need to know". Newsgp. Archived from the original on 13 June 2023. Retrieved 13 June 2023.
- ^ Bedi G (29 March 2018). "Is psychiatry ready for medical MDMA?". The Conversation. Archived from the original on 4 January 2023. Retrieved 12 April 2024.
- ^ "Misuse of Drugs Act 1981". The Government of Western Australia. Department of the Premier and Cabinet. 23 October 1981. Archived from the original on 18 August 2016. Retrieved 22 July 2016.
- ^ "ACT government decriminalises small amounts of illicit drugs including speed, heroin and cocaine". ABC News. Australian Broadcasting Corporation. 20 October 2022. Archived from the original on 13 June 2023. Retrieved 13 June 2023.
- ^ Roy T (27 October 2023). "The ACT has today decriminalised small amounts of some illicit drugs. But what does that mean?". ABC News. Retrieved 7 June 2024.
- ^ "Schedule I". Controlled Drugs and Substances Act. Isomer Design. Archived from the original on 10 November 2013. Retrieved 9 December 2013.
- ^ "Definitions and interpretations". Controlled Drugs and Substances Act. Isomer Design. Archived from the original on 10 November 2013. Retrieved 9 December 2013.
- ^ "Decriminalizing people who use drugs in B.C." Government of BC. Government Communications and Public Engagement. Archived from the original on 9 March 2023. Retrieved 8 March 2023.
- ^ "B.C. recorded 211 toxic drug deaths — almost 7 a day — in January, coroner reports". CBC.ca. 7 March 2023. Archived from the original on 8 March 2023. Retrieved 8 March 2023.
- ^ "Valtioneuvoston asetus huumausaineina pidettävistä aineista, valmisteista ja kasveista | 543/2008 | Lainsäädäntö | Finlex".
- ^ "KKO:2005:56 | 11.5.2005 | Ennakkopäätökset | Korkein oikeus | Finlex".
- ^ Zaken MV (31 May 2024). "MDMA /// Beyond Ecstasy - Report - Government.nl". www.government.nl. Retrieved 6 April 2025.
- ^ a b Hennig AC (2014). "An Examination of Federal Sentencing Guidelines' Treatment of MDMA ('Ecstasy')". Belmont Law Review. 1: 267. SSRN 2481227.
- ^ "Rapport Drugs in Lijsten". Rijksoverheid.nl. 27 June 2011. Archived from the original on 6 March 2012. Retrieved 29 August 2012.
- ^ "Committee: the current system of the Opium Act does not have to be changed". government.nl. 24 June 2011. Archived from the original on 29 April 2012. Retrieved 29 August 2012.
- ^ Power M (2013). Drugs 2.0: the web revolution that's changing how the world gets high (epub file). London: Portobello. ISBN 978-1-84627-459-6.
- ^ "Misuse of Drugs Act 1971". Statutelaw.gov.uk. 5 January 1998. Archived from the original on 28 August 2021. Retrieved 11 June 2011.
- ^ Hope C (7 February 2009). "Ecstasy 'no more dangerous than horse riding'". Telegraph.co.uk. Archived from the original on 10 December 2015. Retrieved 4 December 2015.
- ^ Nutt DJ (January 2009). "Equasy-- an overlooked addiction with implications for the current debate on drug harms". Journal of Psychopharmacology. 23 (1). Oxford, England: 3–5. doi:10.1177/0269881108099672. PMID 19158127. S2CID 32034780.
- ^ Johnson A (2 November 2009). "Why Professor David Nutt was shown the door". The Guardian. London. Archived from the original on 18 January 2014. Retrieved 3 November 2009.
- ^ Schedules of Controlled Substances; Scheduling of 3,4-Methylenedioxymethamphetamine (MDMA) Into Schedule I of the Controlled Substances Act; Remand, 53 Fed. Reg. 5,156 (DEA 22 February 1988).
- ^ "Court Rejects Harsh Federal Drug Sentencing Guideline as Scientifically Unjustified". American Civil Liberties Union. 15 July 2011. Archived from the original on 14 March 2014. Retrieved 29 August 2012.
- ^ a b "Statistical Bulletin 2018 — prevalence of drug use". European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). Archived from the original on 31 December 2018. Retrieved 5 February 2019.
- ^ Wu P, Liu X, Pham TH, Jin J, Fan B, Jin Z (November 2010). "Ecstasy use among US adolescents from 1999 to 2008". Drug and Alcohol Dependence. 112 (1–2): 33–38. doi:10.1016/j.drugalcdep.2010.05.006. PMC 2967577. PMID 20570447.
- ^ European Monitoring Centre for Drugs and Drug Addiction (2008). Annual report: the state of the drugs problem in Europe (PDF). Luxembourg: Office for Official Publications of the European Communities. p. 49. ISBN 978-92-9168-324-6. Archived from the original (PDF) on 25 April 2013. Retrieved 1 December 2008.
- ^ European Monitoring Centre for Drugs Drug Addiction (2014). "Ecstasy: high purity powder available". European Drug Report (PDF). European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). p. 26. doi:10.2810/32306. ISBN 978-92-9168-694-0. Archived from the original (PDF) on 7 September 2014. Retrieved 4 June 2014.
- ^ "Ecstasy-type substances Retail and wholesale prices* and purity levels, by drug, region and country or territory". United Nations Office on Drugs and Crime. Archived from the original on 8 December 2015. Retrieved 2 January 2015.
- ^ Camargo J, Esseiva P, González F, Wist J, Patiny L (November 2012). "Monitoring of illicit pill distribution networks using an image collection exploration framework". Forensic Science International. 223 (1–3): 298–305. doi:10.1016/j.forsciint.2012.10.004. PMID 23107059. Archived from the original on 28 August 2021. Retrieved 9 December 2013.
- ^ Dillon P. "10 years of ecstasy and other party drug use in Australia: What have we done and what is there left to do?". Drugtext.org. Archived from the original on 9 February 2012.
- ^ "Erowid MDMA Vault: Images". Archived from the original on 6 March 2016. Retrieved 3 March 2016.
- ^ Cork T (31 July 2015). "Now sick dealers peddle Shaun the Sheep Ecstasy tablets". Western Daily Press. Archived from the original on 12 August 2015. Retrieved 3 March 2016.
- ^ Chaliha D, Mamo JC, Albrecht M, Lam V, Takechi R, Vaccarezza M (1 July 2021). "A Systematic Review of the MDMA Model to Address Social Impairment in Autism". Current Neuropharmacology. 19 (7): 1101–1154. doi:10.2174/1570159X19666210101130258. PMC 8686313. PMID 33388021.
- ^ Moncrieff J (16 January 2025). "Alternative Approaches: The Good, the Bad and the Worrying: Psychedelics for Depression". Chemically Imbalanced: The Making and Unmaking of the Serotonin Myth. Flint. ISBN 978-1-80399-680-6. Retrieved 16 October 2025.
External links
[edit]- A Multi-Site Phase 3 Study of MDMA-Assisted Therapy for PTSD (MAPP2)
- "MDMA Facts and Statistics". National Institute on Drug Abuse. 15 June 2020.
Chemical and Pharmacological Foundations
Molecular Structure and Synthesis
3,4-Methylenedioxymethamphetamine (MDMA) possesses the molecular formula C₁₁H₁₅NO₂ and a molar mass of 193.24 g/mol.[14] Its systematic IUPAC name is 1-(1,3-benzodioxol-5-yl)-N-methylpropan-2-amine.[15] The molecule consists of a benzene ring substituted with a methylenedioxy group at positions 3 and 4, attached to a propan-2-amine chain with an N-methyl substituent, classifying it as a substituted phenethylamine.[14] MDMA contains a chiral center at the carbon bearing the amino group, existing as a racemic mixture of (R)- and (S)-enantiomers in typical preparations, with the (S)-enantiomer exhibiting greater serotonergic activity.[16] The structure can be visualized as a fusion of the methylenedioxyphenyl ring to the beta position of N-methylamphetamine.[17] MDMA was first synthesized on December 24, 1912, by Merck chemist Anton Köllisch as an intermediate in an alternative route to produce the hemostatic agent methylhydrastinin, bypassing a Bayer patent on hydrastinin synthesis.[5] [18] The Merck process involved condensing piperonyl methyl ketone (an intermediate derived from piperonal or safrole derivatives) with methylamine, followed by reduction, though pharmacological testing of MDMA itself was not conducted at the time.[12] Contemporary laboratory synthesis of MDMA typically proceeds from controlled precursors such as safrole, isosafrole, or piperonal.[19] A common route isomerizes safrole to isosafrole, oxidizes it to 3,4-methylenedioxyphenyl-2-propanone (MDP2P or PMK), and then performs reductive amination with methylamine using agents like aluminum amalgam or sodium cyanoborohydride to yield the amine product.[20] [12] Alternative paths employ piperonal via nitropropene reduction or Henry reaction followed by methylation and reduction.[21] These methods produce racemic MDMA, with purification via acidification to the hydrochloride salt and recrystallization.[21] Due to MDMA's Schedule I status under the UN 1971 Convention, precursor chemicals like safrole, PMK, and piperonal are internationally regulated, complicating both legitimate and illicit production.[22]Pharmacodynamics
MDMA exerts its primary pharmacological effects through the reversal of monoamine transporters on presynaptic neurons, leading to efflux of serotonin (5-HT), dopamine (DA), and norepinephrine (NE) into the synaptic cleft.[3] It acts as a substrate for the serotonin transporter (SERT), dopamine transporter (DAT), and norepinephrine transporter (NET), entering the neuron and promoting carrier-mediated exchange that expels intracellular monoamines.[23] Additionally, MDMA inhibits the vesicular monoamine transporter 2 (VMAT2), displacing monoamines from synaptic vesicles into the cytoplasm, thereby increasing their availability for release.[24] This mechanism results in elevated extracellular levels of these neurotransmitters, with the greatest potency observed for 5-HT release, followed by NE and DA.[2] The stereochemistry of MDMA influences its pharmacodynamic profile, as it exists as a racemic mixture of S-(+)- and R-(-)-enantiomers. The S-(+)-enantiomer demonstrates higher potency in releasing DA and NE, contributing more to stimulant-like effects, while both enantiomers release 5-HT, though R-(-)-MDMA shows relative selectivity for serotonergic effects without substantial DA elevation at behaviorally relevant doses.[25] [26] R-(-)-MDMA has been noted for prosocial properties potentially linked to 5-HT2A receptor interactions, whereas S-(+)-MDMA inhibits both SERT and DAT more effectively.[27] At higher concentrations, MDMA exhibits affinity for various receptors, including 5-HT2A, histamine H1, and muscarinic M1/M2 subtypes, though these interactions are secondary to its transporter-mediated actions and may contribute to peripheral effects like hyperthermia or cardiovascular stimulation.[28] The net increase in monoamine signaling underlies MDMA's empathogenic, entactogenic, and stimulant properties, with 5-HT release particularly implicated in mood elevation and prosocial behavior.[3]Pharmacokinetics and Metabolism
MDMA is rapidly absorbed following oral administration, the primary route of recreational and therapeutic use, with time to peak plasma concentrations generally ranging from 1 to 2 hours post-ingestion.[2] Plasma concentrations do not increase linearly with dose due to saturable metabolism, resulting in non-linear pharmacokinetics where higher doses produce disproportionately elevated exposure.[29] The elimination half-life averages 7 to 9 hours in extensive metabolizers, though this varies with dose, individual genetics, and enantiomeric composition, with ranges reported from 4.6 to 16 hours.[30] [31] MDMA undergoes extensive hepatic metabolism primarily via cytochrome P450 2D6 (CYP2D6), accounting for the major O-demethylenation pathway that converts the parent compound to 3,4-methylenedioxy-3-hydroxy-methamphetamine (HHMA), which is subsequently methylated by catechol-O-methyltransferase (COMT) to 4-hydroxy-3-methoxy-methamphetamine (HMA).[2] [24] A secondary pathway involves N-demethylation to 3,4-methylenedioxyamphetamine (MDA), which possesses its own psychoactive properties and contributes to overall effects.[29] CYP2D6 polymorphisms significantly influence this process; poor metabolizers, comprising about 5-10% of Caucasians, exhibit reduced enzyme activity, leading to slower clearance, higher parent compound levels, and increased risk of adverse effects, while ultra-rapid metabolizers show accelerated metabolism.[31] [32] MDMA itself can inhibit CYP2D6, further contributing to non-linearity during acute exposure.[33] The enantiomers of racemic MDMA display differential handling: (S)-MDMA, the more pharmacodynamically active isomer, undergoes faster metabolism and has a shorter half-life (approximately 5 hours) compared to (R)-MDMA (11-14 hours), affecting overall disposition in therapeutic contexts where stereochemistry may be considered.[34] Distribution is widespread, with rapid penetration into the brain due to lipophilicity, though protein binding is low at around 34%.[24] Excretion occurs mainly renally, with less than 10% of the dose eliminated unchanged; the majority (over 70%) appears in urine as conjugated metabolites (glucuronides and sulfates) of HHMA, HMA, and MDA within 24-72 hours, influenced by urine pH and flow rates.[32] [3] Biliary and fecal elimination is minor.[2]Therapeutic Research and Applications
MDMA-Assisted Therapy for PTSD
MDMA-assisted therapy for post-traumatic stress disorder (PTSD) combines administration of MDMA with psychotherapy sessions, typically involving two or three doses of 75-125 mg MDMA per session, spaced several weeks apart, under the guidance of trained therapists to facilitate emotional processing of trauma.[35] This approach, pioneered by the Multidisciplinary Association for Psychedelic Studies (MAPS), aims to reduce fear responses and enhance therapeutic alliance by leveraging MDMA's effects on serotonin, dopamine, and oxytocin release, which may promote empathy and decrease amygdala hyperactivity associated with PTSD symptoms.[36] Initial phase 2 trials, conducted from 2004 to 2017, reported remission rates of up to 68% in participants with chronic, treatment-resistant PTSD, prompting FDA breakthrough therapy designation in 2017.[35] However, as an advocacy organization funding the research, MAPS has faced scrutiny for potential conflicts of interest influencing trial design and interpretation.[37] Phase 3 trials, MAPP1 (NCT03537014, completed 2019) and MAPP2 (NCT04077437, completed 2021), randomized 194 participants with moderate to severe PTSD to MDMA-assisted therapy or psychotherapy plus placebo.[38] In MAPP1, published in 2023, the MDMA group showed a mean change in Clinician-Administered PTSD Scale (CAPS-5) score of -23.7 points versus -14.8 for placebo at 18 weeks (p=0.01), with 67% of MDMA participants no longer meeting PTSD diagnostic criteria compared to 32% in placebo.[39] MAPP2 yielded similar results, with 71.2% remission in the MDMA arm versus 47.6% in placebo, alongside improvements in functional impairment measured by the Sheehan Disability Scale. Pooled analyses indicated sustained benefits at 12-month follow-up, with 86.5% of treatment-resistant cases achieving clinically significant symptom reduction.[40] Adverse events were generally mild, including transient increases in blood pressure and anxiety, though cardiovascular risks remain a concern for patients with comorbidities.[39] Despite these outcomes, methodological limitations undermine confidence in the placebo-controlled efficacy. Blinding failed in over 90% of MAPP2 participants, who correctly identified MDMA due to its distinct euphoric and physiological effects, potentially inflating perceived benefits through expectancy bias.[41] Therapists, often MAPS-affiliated and unblinded, may have introduced performance bias, compounded by allegations of ethical lapses such as a therapist's sexual misconduct with participants, prompting FDA concerns over study integrity.[37] Critics argue the trials lack active comparators and long-term safety data, with incomplete evidence on neurotoxicity risks in vulnerable populations.[42] Lykos Therapeutics (formerly MAPS) submitted a New Drug Application in 2023, but the FDA rejected it in August 2024, citing insufficient evidence of effectiveness and safety, including unaddressed hepatotoxicity signals.[43] A complete response letter in September 2025 reiterated these issues, requiring a new phase 3 trial without current approval as of October 2025.[44] Proponents contend the rejection overlooks real-world remission rates, while skeptics emphasize the need for rigorous, unbiased replication to distinguish pharmacological effects from nonspecific therapy enhancements.[45]Other Potential Medical Uses
MDMA-assisted psychotherapy has been investigated in small-scale studies for treating social anxiety symptoms in adults with autism spectrum disorder. A phase 2 pilot trial involving 18 autistic adults administered MDMA (up to 125 mg per session) in conjunction with psychotherapy sessions, resulting in statistically significant reductions in social anxiety symptoms as measured by the Liebowitz Social Anxiety Scale (LSAS), with improvements sustained for at least six months post-treatment in most participants.[46] Participants reported enhanced empathy, openness, and interpersonal closeness during sessions, with no serious adverse events attributed to MDMA.[47] These findings suggest MDMA may facilitate prosocial behaviors and reduce avoidance in social contexts, though the study's open-label design and small sample limit generalizability, and larger randomized controlled trials are required to confirm efficacy.[48] Preliminary research also explores MDMA-assisted therapy for anxiety associated with life-threatening illnesses, such as advanced cancer. An open-label feasibility study with 12 participants facing terminal diagnoses delivered two or three MDMA sessions (75-125 mg doses) alongside psychotherapy, yielding reductions in anxiety scores on the Beck Anxiety Inventory and improvements in quality of life metrics, with effects persisting up to 12 months in some cases.[49] Qualitative analyses indicated increased acceptance of mortality and enhanced emotional processing, potentially linked to MDMA's effects on serotonin release and fear extinction.[50] Adverse effects were mild and transient, primarily including fatigue and jaw clenching.[51] However, the absence of a control group and small cohort size necessitate further validation through rigorous trials to establish causal benefits over placebo or standard care.[52] Other applications, such as adjunctive treatment for alcohol use disorder, have shown mixed results; one review of MDMA-assisted interventions noted greater reductions in alcohol consumption severity compared to drug use, but lacked consistent evidence of broad abstinence or superiority over existing therapies.[53] Investigations into conditions like borderline personality disorder or general treatment-resistant depression remain in early stages, with anecdotal or preclinical support but insufficient clinical data to support routine use.[54] Overall, while these exploratory efforts highlight MDMA's potential to augment psychotherapy by promoting emotional openness and reducing defensiveness, the evidence base consists primarily of pilot studies, and regulatory approval beyond PTSD contexts is pending larger-scale confirmation of safety and efficacy.[55]Clinical Trials, Evidence, and Regulatory Hurdles
MDMA-assisted psychotherapy has primarily been investigated for treating post-traumatic stress disorder (PTSD) through clinical trials sponsored by the Multidisciplinary Association for Psychedelic Studies (MAPS), now affiliated with Lykos Therapeutics. Phase 2 trials, completed between 2001 and 2016, involved small cohorts (n=20–107) and reported remission rates of 68–83% in MDMA groups versus 23–29% in therapy-only controls, with MDMA doses of 75–125 mg per session combined with non-directive psychotherapy.[56] These early studies prompted the U.S. Food and Drug Administration (FDA) to grant breakthrough therapy designation in 2017, recognizing preliminary evidence of substantial improvement over existing therapies. Two pivotal phase 3 trials (MAPP1 and MAPP2), randomized, double-blind, placebo-controlled studies enrolling 194 participants with moderate to severe PTSD, were conducted from 2018 to 2021. In MAPP1, published in 2023, the MDMA group (n=52) showed a mean change in Clinician-Administered PTSD Scale (CAPS-5) score of -23.7 points versus -14.8 for placebo (n=51; p=0.005), with 71.2% of MDMA participants no longer meeting PTSD diagnostic criteria at 18 weeks compared to 47.6% in placebo.[39] MAPP2 yielded similar results, with 67.2% remission in MDMA versus 32.3% in placebo arms.[57] Safety data indicated transient elevations in blood pressure and heart rate, with no serious drug-related adverse events; however, elevated liver enzymes occurred in 6.7% of MDMA participants.[58] Despite these outcomes, the evidence base faces scrutiny for methodological limitations inherent to psychedelic trials. MDMA's distinctive subjective effects—euphoria, empathy enhancement, and sensory alterations—compromise blinding, as participants and therapists could readily distinguish active drug from placebo, potentially inflating efficacy via expectancy and allegiance biases.[59] Independent analyses have highlighted unverified functional unblinding rates exceeding 90% in similar studies, questioning the placebo control's validity.[42] MAPS-sponsored trials, while peer-reviewed, originate from an advocacy organization with a pro-psychedelic stance, raising concerns of selective reporting; broader meta-analyses of MDMA-assisted therapy affirm symptom reductions (effect size d=1.2–1.5) but emphasize small sample sizes, lack of long-term follow-up beyond 12 months, and underrepresentation of diverse populations (e.g., <10% non-white participants).[60] Safety evidence remains provisional, with trials using controlled doses (≤180 mg/session) showing low incidence of severe events, though extrapolation to real-world use is cautioned due to recreational neurotoxicity data.[61] Regulatory progress stalled following Lykos's New Drug Application submission in November 2023. An FDA Psychopharmacologic Drugs Advisory Committee in June 2024 voted 9–2 against efficacy and 10–1 against a favorable risk-benefit profile, citing blinding failures, ethical lapses (including a therapist-patient boundary violation allegation), insufficient abuse liability assessment, and gaps in cardiovascular safety for comorbid patients.[43] The FDA issued a complete response letter on August 9, 2024, rejecting approval and mandating an additional phase 3 trial with enhanced controls, such as active placebos to mitigate unblinding.[62] As of October 2025, MDMA retains Schedule I status under the Controlled Substances Act, denoting high abuse potential and no accepted medical use, which imposes DEA oversight on research, manufacturing quotas, and scheduling rescheduling barriers even if FDA approves.[63] These hurdles, compounded by psychotherapy's non-FDA-regulated component and stigma from MDMA's recreational history, have delayed therapeutic access, though expanded access programs persist for compassionate use in treatment-resistant cases.[64] Legislative efforts, like the 2023 Breakthrough Therapies Act, aim to ease Schedule I research but have not altered MDMA's classification.[65]Recreational and Non-Medical Use
Patterns of Use and Demographics
Recreational MDMA use predominantly occurs in social nightlife settings such as electronic dance music events, raves, clubs, and festivals, where it is employed to enhance euphoria, sensory perception, and interpersonal connections during prolonged dancing and socializing.[66] [67] Users typically consume it in these environments to sustain energy and amplify positive emotions amid crowds and music, with patterns often involving group consumption with friends rather than solitary use.[68] While historically tied to rave culture, use has expanded beyond dedicated rave scenes to broader party contexts, including house parties and live music events, particularly among young adults seeking controlled, occasional enhancement of recreational experiences.[69] [70] Prevalence of past-year MDMA use in the United States stands at approximately 0.9% among adults aged 12 and older, with elevated rates among younger cohorts: 2.6% for ages 19–30 and up to 7.1% for those aged 18–25.[71] [72] [73] In Europe, an estimated 2.2% of young adults aged 15–34 reported past-year use between 2015 and 2023, equating to about 2.2 million individuals across EU countries.[74] Among high school seniors in the US, past-year use hovers around 4.4%, though rates vary by subgroup.[75] Globally, use remains episodic rather than habitual, with most users reporting infrequent dosing—often 1–4 times per year—aligned with specific social events rather than daily or weekly patterns.[76] Demographically, MDMA use skews toward urban young adults, with higher odds among males in many contexts, such as 9.7% past-month prevalence for males aged 25–34 in Ireland compared to lower female rates.[77] However, patterns differ by population; for instance, among Asian American and Pacific Islander adults, females exhibit 1.45 times higher lifetime use odds than males.[78] Religious affiliation correlates with lower use odds among youth, while polysubstance patterns are common, with MDMA frequently combined with alcohol, cannabis, or stimulants at events to modulate effects.[75] Use declines sharply after age 35, with those over 50 showing minimal engagement, reflecting its association with youth-oriented nightlife.[71]| Region/Group | Past-Year Prevalence | Key Demographic Notes |
|---|---|---|
| US Adults (12+) | 0.9% | Highest in 18–25 (7.1%); younger ages elevated odds[73] [71] |
| US 19–30 | 2.6% | Tied to social events[72] |
| EU Young Adults (15–34) | 2.2% | ~2.2 million users; event-driven[74] |
| US High School Seniors | 4.4% | Lower among females, religious students[75] |
Forms, Administration, and Adulteration
MDMA is most commonly distributed in tablet form, known as ecstasy, which are often pressed into colorful shapes imprinted with logos to create brand identities for users.[79] These tablets typically contain varying amounts of MDMA, with street doses ranging from 50 to 150 mg per tablet, though content can fluctuate significantly across batches.[3] Harm reduction guidelines recommend initial recreational doses of 80–120 mg, considering 150 mg a strong to heavy dose that elevates risks. In powder or crystal form, referred to as molly, MDMA is marketed as a purer alternative, appearing as white to off-white crystals or fine powder, often sold in capsules or small bags.[80] Less frequently, it is encountered as a liquid solution.[80] The primary method of administration is oral ingestion, achieved by swallowing tablets, gel capsules, or "bombs"—small wraps of powder folded into paper or gelatine for consumption.[81] Snorting crushed powder or tablets is a secondary route, though less common due to discomfort and nasal irritation, while injection or smoking occurs rarely.[82] [80] Oral administration leads to effects onset within 30-60 minutes, with duration of 3-6 hours depending on dose and individual factors. Redosing after an initial 150 mg dose is strongly discouraged for harm reduction, as it significantly increases risks of neurotoxicity, overheating, dehydration, serotonin depletion, and other adverse effects. If redosing despite this, wait 1.5–2 hours and limit the booster to half the initial dose or less (e.g., 50–75 mg max), ensuring the total session amount stays under 225–250 mg; however, the safest practice is to avoid redosing, start with lower initial doses (80–120 mg), and space uses 1–3 months apart. Adulteration is prevalent in street MDMA, particularly in ecstasy tablets, which frequently contain little to no MDMA and instead include substitutes or fillers such as methamphetamine, amphetamine, caffeine, paracetamol, or novel psychoactive substances like PMMA.[83] [84] Analyses of seized samples show that misrepresentation is common, with users expecting MDMA but receiving other compounds that may amplify toxicity or alter effects.[85] Molly crystals generally exhibit higher purity than tablets, but testing reveals variability, with impurities including synthesis byproducts or cutting agents like MDA.[86] [87] Such adulterants contribute to unpredictable dosing and heightened health risks, as evidenced by forensic drug analyses.[88]Subjective and Acute Effects
Users report that MDMA's subjective effects typically begin 30 to 60 minutes after oral ingestion of doses ranging from 75 to 125 mg, with peak intensity occurring around 90 minutes and principal effects persisting for 3 to 5 hours.[89][90] These timelines can vary based on dose, individual metabolism, and environmental factors such as setting and co-ingested substances.[91] Prominent positive subjective effects include euphoria, heightened mood, and prosocial emotions such as increased empathy, trust, and emotional closeness to others. MDMA is sometimes referred to as the "love drug" (or similar terms like "hug drug" or "empathy drug") because it induces strong feelings of empathy, affection, emotional openness, and a desire for intimacy and connection with others, often leading users to feel loving and compassionate.[25][92] In controlled studies, MDMA administration leads to self-reported enhancements in sociability and reductions in interpersonal defensiveness, often attributed to elevated oxytocin levels facilitating bonding-like responses.[93][94] Users frequently describe a sense of emotional openness and decreased anxiety or fear, contributing to its appeal in social and recreational contexts.[90] Anecdotal reports, particularly from online forums such as Reddit's r/SEXONDRUGS, suggest that MDMA, often combined with cannabis, can increase women's emotional openness, arousal, and directness about sexual desires or discussions of sex. This effect is linked to MDMA's enhancement of empathy and emotional honesty, promoting more open expression of desires, while cannabis may contribute to relaxation and intensified physical sensations. Experiences vary, with some women reporting heightened sexual interest and expressiveness, though MDMA can sometimes impair physical sexual performance despite elevated desire.[95] Sensory and perceptual alterations are also common, with enhanced appreciation of tactile sensations, music, and visual stimuli, often described as intensified or synesthetic.[92] Acute effects may include increased energy and alertness, alongside mild distortions in time perception.[92] Dose-dependent factors influence intensity; lower doses emphasize empathogenic qualities, while higher recreational amounts (e.g., over 150 mg) can produce initial effects of intense euphoria, enhanced empathy, and pronounced sensory enhancement but risk introducing negative subjective states like confusion or transient anxiety.[91][96] Gender differences appear in some reports, with females potentially experiencing stronger peak effects or prolonged duration due to pharmacokinetic variations.[91] Overall, these subjective experiences drive non-medical use, though empirical data from clinical settings underscore their context-dependence, with supportive environments enhancing positives and mitigating potential distress.[97]Health Effects and Risks
Short-Term Physiological Effects
MDMA administration acutely elevates heart rate and blood pressure in humans, with studies reporting dose-dependent increases; for instance, a 1.7 mg/kg intravenous dose produced systolic blood pressure rises of up to 40 mmHg and heart rate elevations of approximately 30 beats per minute above baseline.[98] [99] These cardiovascular effects stem from MDMA's release of catecholamines like norepinephrine, mimicking sympathomimetic stimulants.[100] Body temperature also rises significantly, often leading to hyperthermia, particularly under conditions of physical exertion or environmental heat, as MDMA impairs thermoregulation via serotonin-mediated mechanisms in the hypothalamus.[92] [101] Clinical observations note core temperature increases of 1-2°C, which can escalate to life-threatening levels exceeding 41°C in recreational settings, exacerbated by dehydration from sweating and reduced thirst perception.[102] [103] At high doses, initial physiological effects prominently include tachycardia, hypertension, mydriasis, diaphoresis, and bruxism. Other short-term physiological responses include jaw clenching due to heightened muscle tension and serotonin release, alongside dilated pupils (mydriasis), dry mouth (xerostomia), and occasional nausea or blurred vision from autonomic activation.[92] [104] These effects typically onset within 30-60 minutes of oral ingestion, peak at 1-2 hours, and subside over 4-6 hours, though residual elevations in heart rate and blood pressure may persist.[98]Long-Term Neurotoxicity and Cognitive Impacts
Preclinical studies in rodents and nonhuman primates have demonstrated that MDMA induces selective and dose-dependent neurotoxicity to serotonin (5-HT) neurons, characterized by axonal degeneration, reduced 5-HT transporter density, and persistent deficits in serotonergic markers lasting months to years post-exposure.[105] In squirrel monkeys, plasma MDMA concentrations comparable to human recreational doses produced lasting serotonergic deficits overlapping with those observed in users.[106] Primate models further reveal abnormal 5-HT innervation patterns in forebrain regions, including the hippocampus and neocortex, persisting up to seven years after treatment, with partial but incomplete recovery in some areas.[107] Human evidence for MDMA-related neurotoxicity is primarily correlational, derived from neuroimaging and postmortem analyses, but confounded by factors such as polydrug use, frequency of exposure, and premorbid differences. Positron emission tomography (PET) studies using ligands like [11C]McN5652 have shown global and regional decreases in 5-HT transporter binding in ecstasy users, with reductions correlating to lifetime MDMA exposure and persisting for weeks to months after abstinence.[108] A 1998 study reported 20-50% lower 5-HT transporter density in cortical and subcortical regions among moderate users compared to controls, suggesting structural damage to serotonergic axons.[109] However, longitudinal data indicate potential partial recovery with prolonged abstinence, though deficits in 5-HT innervation may endure in heavy users.[110] Cognitive impairments linked to chronic MDMA use predominantly affect memory domains, with meta-analyses identifying moderate deficits in verbal and visual memory, alongside subtler effects on executive function and attention, independent of acute intoxication.[111] Prospective cohort studies of novice users report decreased verbal memory performance following low-dose exposure (e.g., 1-2 tablets), persisting at 3-month follow-up despite minimal confounding drug use.[112] These effects align with serotonergic disruption in hippocampus-dependent processes, as evidenced by correlations between reduced 5-HT transporter density and impaired verbal recall in abstinent users.[113] Neuroimaging meta-analyses confirm structural and functional alterations in MDMA users' brains, including reduced gray matter volume and altered activation in memory-related regions, though causality remains debated due to self-selection biases in recreational cohorts.[114] Despite consistent preclinical toxicity and associative human data, some reviews highlight inconsistencies in cognitive outcomes, attributing variability to dosage, purity, co-use of substances like alcohol or stimulants, and methodological limitations in user-control matching.[115] Heavy users (>100 occasions) exhibit more pronounced deficits than light users, but population-level studies often fail to isolate MDMA's isolated contribution, underscoring the need for controlled, prospective designs to disentangle neurotoxic causality from lifestyle confounders.[116] Overall, while animal models establish a mechanistic basis for serotonergic damage, human cognitive impacts appear dose-related and potentially reversible with abstinence, though long-term risks for high-exposure individuals warrant caution.[117]Psychiatric, Cardiovascular, and Other Adverse Outcomes
MDMA use, particularly in recreational contexts, can precipitate acute psychiatric symptoms such as heightened anxiety, paranoia, and, infrequently, psychosis. Case reports have documented persistent psychotic episodes, including delusions and hallucinations, following single or repeated doses, with symptoms enduring for months despite cessation and requiring antipsychotic treatment.[118][119] Post-acute phases often involve a "comedown" characterized by depression, irritability, fatigue, sleep disturbances, and severe anxiety, attributed to serotonin depletion and lasting days to a week.[94][120] Long-term psychiatric risks from chronic use include elevated self-reported depression and anxiety symptoms, with observational studies showing small but consistent associations compared to non-users or polydrug controls.[121][122] These effects may stem from sustained serotonergic disruption, though confounding by lifestyle factors, polydrug exposure, and self-medication for underlying mental health issues complicates causality attribution.[123] In controlled clinical trials for MDMA-assisted psychotherapy, psychiatric adverse events remain mild and transient, with no evidence of lasting mood disorders.[61] Cardiovascular effects of MDMA are primarily acute and sympathomimetic, manifesting as dose-dependent tachycardia, hypertension, and elevated myocardial oxygen demand, akin to infusions of 20-40 μg/kg/min dobutamine.[124] These changes, exacerbated by hyperthermia and dehydration, increase risks of arrhythmias, myocardial infarction, stroke, and vascular dysfunction, particularly in users with preexisting cardiac conditions or during prolonged physical exertion like dancing.[100][125] Animal studies reveal underlying mechanisms including serotonin-mediated cardiac myocyte activation via 5-HT2B receptors, reduced myocardial serotonin levels, and shifts toward fatty acid metabolism, potentially contributing to long-term cardiotoxicity.[126] Other adverse outcomes encompass hyperthermia, a leading cause of MDMA-related fatalities with 41 documented cases linked to multi-organ failure, and hyponatremia, responsible for 10 deaths—all in females—due to excessive water intake and antidiuretic hormone release.[122] Acute kidney and liver injury often arise secondary to rhabdomyolysis, disseminated intravascular coagulation, or hemodynamic instability in overdose settings.[122] Observational data indicate low overall mortality, with ecstasy as the sole agent in approximately 10-17 annual UK deaths from 1996-2006, though polydrug interactions amplify risks.[122] In therapeutic administration, these severe systemic effects are absent, with events confined to transient issues like bruxism, nausea, and appetite suppression.[127]Dependence, Addiction, and Reinforcement
MDMA exhibits low potential for physical dependence and addiction compared to classical stimulants like cocaine or amphetamines, with most users not developing compulsive patterns of use despite repeated exposure.[128] Preclinical studies in rodents and primates consistently show limited self-administration of MDMA, with animals maintaining only low intake levels on daily schedules and acquisition rates lower than for cocaine (e.g., fewer than 50% of rats acquire stable self-administration at doses of 0.5–1.0 mg/kg/infusion).[129] [128] This contrasts with high-reinforcing drugs, where robust dose-response curves and progressive ratio breakpoints indicate strong motivational drive; MDMA's reinforcing effects are weaker and often context-dependent, failing to sustain high responding under progressive ratio schedules.[130] In humans, epidemiological data indicate that dependence is rare among MDMA users, with lifetime prevalence of ecstasy dependence estimated at under 15% among regular users in surveys, far below rates for substances like opioids or cocaine.[131] Psychological craving and compulsive redosing can occur during acute intoxication due to dopaminergic reinforcement mechanisms, but rapid tolerance to MDMA's euphoric and empathogenic effects—mediated primarily by massive serotonin release followed by depletion—typically limits binge patterns and long-term escalation.[132] No severe physical withdrawal syndrome akin to that of alcohol or benzodiazepines has been documented; post-use symptoms are limited to fatigue, depression, and irritability lasting 1–3 days, attributable to neurotransmitter recovery rather than dependence.[120] Reinforcement of MDMA use arises from its dual action on serotonin (5-HT) and dopamine systems, with prosocial effects linked to 5-HT1B receptor activation promoting social bonding, while acute reward requires intact dopaminergic signaling in mesolimbic pathways.[133] However, repeated administration leads to diminished reinforcing efficacy due to serotonin transporter downregulation and tolerance, reducing the incentive for frequent dosing; animal models confirm that MDMA-primed reinstatement of seeking behavior is weaker than for amphetamines.[134] Case reports of dependence exist, meeting DSM criteria via tolerance, withdrawal, and inability to cut down, but these are exceptional and often involve polydrug use or high-dose chronic patterns, underscoring MDMA's overall low abuse liability.[135] [136]Toxicity and Interactions
Overdose Symptoms and Management
MDMA overdose primarily manifests through sympathomimetic toxicity, serotonin excess, and environmental factors exacerbated by the drug's effects, leading to potentially life-threatening complications. Common symptoms include severe hyperthermia, often exceeding 40°C (104°F), resulting from increased metabolic rate, impaired heat dissipation, and dehydration in hot, crowded settings like raves.[31] [89] Patients may exhibit tachycardia, hypertension, and arrhythmias due to catecholamine surge, alongside agitation, hallucinations, and seizures from serotonergic overstimulation.[31] [137] Hyponatremia, stemming from excessive water intake combined with MDMA-induced antidiuretic hormone release and thirst, can cause nausea, headache, confusion, and cerebral edema in severe cases.[31] [89] Other presentations include rhabdomyolysis, disseminated intravascular coagulation (DIC), acute kidney injury, and multi-organ failure, particularly when hyperthermia is uncontrolled.[138] [31] Serotonin syndrome, characterized by autonomic instability, neuromuscular abnormalities (e.g., clonus, hyperreflexia), and altered mental status, overlaps with MDMA toxicity and arises from excessive serotonin release, potentially worsened by co-ingestants like SSRIs.[89] [31] Fatal outcomes, reported in case series, often involve temperatures above 42°C (107.6°F), with autopsy findings of cerebral edema, hepatic necrosis, and coagulopathy. A dose of 600 mg (approximately 8.6 mg/kg for a 70 kg individual) carries a high mortality risk, primarily from refractory hyperthermia, cardiovascular collapse, and multi-organ failure, with survival unlikely without rapid intervention; however, no fixed lethal dose exists due to variability in metabolism, environment, and purity.[139] [89] Management focuses on supportive care, rapid cooling, and seizure control, as no specific antidote exists. Initial assessment prioritizes airway protection, oxygenation, and intravenous access; benzodiazepines such as lorazepam or midazolam are first-line for agitation, seizures, and sympathomimetic effects to mitigate acidosis and hyperthermia.[138] [137] Aggressive hyperthermia treatment involves removing clothing, evaporative cooling with misting and fans, ice packs to groin/axillae/neck, and immersion in cold water if feasible; dantrolene may be considered for refractory cases mimicking malignant hyperthermia, though evidence is limited to case reports.[138] [140] Fluid resuscitation corrects dehydration but requires caution in hyponatremic patients—free water restriction or hypertonic saline (3%) for symptomatic hyponatremia with sodium below 120 mEq/L, guided by serum osmolality and neurology consultation.[31] [138] Cardiovascular support avoids pure beta-blockers (risking unopposed alpha stimulation); labetalol or esmolol with vasodilators like nitroprusside can be used if needed.[138] For suspected serotonin syndrome, cyproheptadine (a serotonin antagonist) at 12 mg orally followed by 2 mg every two hours may aid, alongside discontinuation of serotonergic agents.[138] Monitoring in an intensive care setting is essential for complications like rhabdomyolysis (treated with aggressive hydration and alkalinization if indicated) or DIC (supportive transfusions).[31] Prognosis improves with early intervention, but delays in cooling correlate with mortality rates up to 50% in severe hyperthermia cases.[89]Drug Interactions and Contraindications
MDMA, a serotonin, dopamine, and norepinephrine releaser, exhibits significant pharmacodynamic and pharmacokinetic interactions with various substances, primarily due to its effects on monoamine transporters and metabolism via cytochrome P450 enzymes like CYP2D6.[3] Concomitant use with monoamine oxidase inhibitors (MAOIs) poses a high risk of serotonin syndrome, characterized by hyperthermia, autonomic instability, and potentially fatal outcomes, as MDMA's serotonin release combines with MAOI-mediated inhibition of breakdown.[141][142] Case reports document severe hyperthermia and altered mental status following MDMA ingestion with serotonergic agents, underscoring the additive serotonergic load.[143] Selective serotonin reuptake inhibitors (SSRIs) such as citalopram, sertraline, and fluoxetine typically attenuate MDMA's subjective and physiological effects by occupying the serotonin transporter (SERT), blocking MDMA's entry into neurons and subsequent release of intracellular serotonin stores; this interaction reduces euphoria and cardiovascular stimulation without consistently precipitating serotonin syndrome in controlled settings.[144][145] However, certain antidepressants like bupropion, venlafaxine, citalopram, and sertraline correlate with elevated mortality odds in postmortem analyses of MDMA users, potentially via CYP2D6 inhibition prolonging MDMA exposure or enhanced cardiovascular toxicity.[146] Serotonin-norepinephrine reuptake inhibitors (SNRIs) may similarly blunt effects while increasing serotonin syndrome risk through combined transporter blockade and release.[147] Co-administration with stimulants such as cocaine, methamphetamine, or amphetamines exacerbates cardiovascular strain, including hypertension and tachycardia, due to synergistic sympathomimetic activity, and may accelerate dopamine depletion leading to prolonged neurotoxicity or acute anxiety.[148][149] Alcohol potentiates dehydration and impairs thermoregulation, as MDMA's hyperthermic effects compound ethanol-induced diuresis, though it may subjectively mitigate some anxiety; combined use also heightens risks of impaired judgment and hyponatremia from overhydration.[148][150] Pharmacokinetic interactions with CYP2D6 substrates or inhibitors, including some opioids or antipsychotics, can elevate MDMA plasma levels, intensifying toxicity.[144] Contraindications include pre-existing cardiovascular conditions, as even a 125 mg dose elevates resting heart rate by approximately 30 beats per minute and systolic blood pressure, risking arrhythmias or myocardial ischemia in those with hypertension or coronary disease.[141] Hepatic or renal impairment warrants avoidance, given MDMA's metabolism to active metabolites like MDA and reliance on renal excretion.[3] Individuals with schizophrenia, bipolar disorder, or other psychotic vulnerabilities face heightened exacerbation risks from MDMA's dopaminergic effects, potentially precipitating mania or hallucinations.[92] Pregnancy and breastfeeding are contraindicated due to teratogenic potential and transfer via milk, though data remain limited to animal models and case reports.[82]Historical Development
Early Synthesis and Pre-Recreational Research (1912–1970s)
MDMA, or 3,4-methylenedioxymethamphetamine, was first synthesized on December 24, 1912, by German chemist Anton Köllisch at the Merck pharmaceutical company in Darmstadt.[12] Köllisch produced the compound as an intermediate in a research program aimed at developing hemostatic agents to control bleeding, specifically as a precursor to methylhydrastinine, a derivative intended to mimic the styptic effects of hydrastine.[151] The synthesis involved reacting safrole with hydrobromic acid to form bromosafrole, followed by amination with methylamine, though the exact route prioritized efficiency for the target hemostatic.[152] Merck patented this process in 1914 under German Patent 274,350, but the compound itself, initially termed "methylsafrylamin," received no dedicated pharmacological evaluation at the time due to its role as a mere synthetic stepping stone.[151] Early assessments of MDMA's properties were limited and incidental. In 1927, Merck pharmacologists tested the compound in rabbits for potential effects on blood coagulation, finding mild activity but no further pursuit, as psychoactive or empathogenic qualities were neither observed nor investigated.[4] Claims of MDMA being developed as an appetite suppressant or for other direct therapeutic uses during this era stem from unsubstantiated narratives and lack primary evidence from Merck records.[153] By 1959, Merck revisited MDMA in additional animal studies, again focusing on peripheral physiological responses without noting central nervous system stimulation or toxicity profiles that would later define its profile.[4] These evaluations remained confined to non-human models, with no documented human administration or clinical trials prior to the 1970s.[151] Throughout the mid-20th century, MDMA saw sporadic rediscovery in academic and industrial chemistry contexts but no systematic research into its biological activity. References to the compound appeared in chemical literature as a derivative of amphetamine analogs, yet it elicited minimal interest beyond structural novelty, overshadowed by wartime priorities and the dominance of other sympathomimetics.[154] Absent recreational or therapeutic application, MDMA languished as an obscure synthetic footnote until independent chemists in the late 1960s and early 1970s began exploring phenethylamine variations, setting the stage for later evaluations.[155] No credible records indicate clandestine or military human testing in the 1940s or 1950s, despite occasional unverified assertions in secondary accounts.[156]Shulgin's Work and Initial Therapeutic Exploration (1970s–1980s)
In the mid-1970s, American chemist Alexander "Sasha" Shulgin, who had synthesized numerous psychoactive phenethylamines after leaving Dow Chemical in 1967, learned of MDMA's unique effects from a graduate student and resynthesized the compound, originally patented by Merck in 1914. Shulgin self-administered a 120 mg dose in September 1976, describing outcomes that included heightened sensory awareness, emotional openness, and reduced defensiveness without significant hallucinations or disorientation, distinguishing it from traditional stimulants or psychedelics.[154][157] Shulgin's 1978 publication with David Nichols marked the first peer-reviewed human study of MDMA, detailing its pharmacokinetics and subjective effects such as empathy enhancement and anxiety reduction, which suggested potential for psychotherapeutic applications. In 1977, he introduced MDMA to retired psychotherapist Leo Zeff, who, after experiencing its facilitative effects on introspection and interpersonal trust, resumed practice and trained over 140 therapists in its use by 1985, often dubbing it "Adam" for its purported return to a primordial emotional state. Zeff's sessions emphasized MDMA's role in bypassing ego defenses to access repressed material, with clients reporting profound relational insights absent the perceptual distortions of LSD.[158][159] Ann Shulgin, Alexander's wife and a family therapist, began incorporating MDMA into informal sessions around 1980 to aid friends in resolving relational conflicts, noting its capacity to foster compassion and dissolve interpersonal barriers. This underground therapeutic network expanded through the early 1980s, with practitioners valuing MDMA's short duration (3-5 hours) and low toxicity profile for outpatient use, though lacking formal clinical trials due to regulatory constraints. By 1984, an estimated 4,000-5,000 individuals had received MDMA-assisted therapy, primarily for trauma, depression, and couples counseling, before federal emergency scheduling in 1985 curtailed open exploration.[160][155]Recreational Popularization and Legal Scheduling (1980s–1990s)
MDMA's recreational use emerged in the early 1980s, primarily in Dallas, Texas, where underground chemists scaled up synthesis for distribution in nightclubs like the Starck Club, attracting a diverse crowd including professionals and partygoers seeking its empathogenic effects.[161][162] By 1984, MDMA—often sold as "Ecstasy" tablets, a name coined in the early 1980s by a Los Angeles-based distributor to make the drug more marketable for recreational use, replacing the earlier therapeutic name "Adam" and reflecting the intense feelings of euphoria, emotional closeness, and bliss it produces—was openly available in Texas venues, with reports of widespread use mingling social groups across sexual orientations and backgrounds, prompting initial law enforcement attention.[163] This shift from therapeutic to party settings fueled rapid popularization, with an estimated thousands of doses consumed weekly in Dallas alone by mid-decade.[161] The escalating recreational demand, particularly in Texas, led the Drug Enforcement Administration (DEA) to initiate scheduling proceedings. On July 27, 1984, the DEA published a notice proposing MDMA's placement in Schedule I of the Controlled Substances Act, classifying it as having high abuse potential and no accepted medical use.[164] Urged by Senator Lloyd Bentsen amid reports of increasing distribution, the DEA announced an emergency Schedule I ban on May 31, 1985, effective July 1, 1985—the agency's first use of emergency scheduling authority for a new substance.[165][166] Administrative hearings from 1985 to 1986 featured testimony from psychotherapists and researchers advocating for MDMA's therapeutic potential, culminating in an administrative law judge's May 1986 recommendation for Schedule III placement, citing evidence of accepted safety under medical supervision.[167][168] DEA Administrator John C. Lawn overruled this in 1987, prioritizing documented recreational abuse patterns and neurotoxicity concerns over therapeutic claims, with the permanent Schedule I classification published in the Federal Register on February 22, 1988.[169][170] Into the late 1980s and 1990s, MDMA solidified its association with rave culture, spreading from U.S. clubs to European scenes, particularly the UK acid house movement influenced by Ibiza DJs, where it enhanced prolonged dancing and social bonding at all-night events.[171] This era's underground production often yielded impure tablets, contributing to variable dosing and early reports of adverse events, though its appeal persisted due to perceived low risk compared to other stimulants.[161]Post-Scheduling Research and Policy Debates (2000s–Present)
Following the placement of MDMA in Schedule I under the U.S. Controlled Substances Act in 1985, research faced significant barriers due to federal restrictions on Schedule I substances, which classify them as lacking accepted medical use and high abuse potential. However, nonprofit organizations like the Multidisciplinary Association for Psychedelic Studies (MAPS) initiated efforts to resume clinical investigations, securing the first U.S. Food and Drug Administration (FDA)-approved human trial of MDMA-assisted psychotherapy for post-traumatic stress disorder (PTSD) in 2001. This phase 1 study, completed in 2004, involved 12 participants and reported reductions in PTSD symptoms without serious adverse events, prompting further trials despite ongoing DEA oversight limiting production and distribution.[172] Subsequent phase 2 trials, conducted from 2004 to 2010 under MAPS sponsorship, demonstrated that MDMA-assisted therapy—typically involving 2–3 sessions of 75–125 mg MDMA doses combined with psychotherapy—yielded response rates of 68–83% in PTSD patients, with sustained symptom reductions observed in long-term follow-ups up to 4.4 years post-treatment, where approximately 75% of participants no longer met PTSD diagnostic criteria. These findings led to FDA granting breakthrough therapy designation in 2017, expediting development based on preliminary evidence of substantial improvement over existing treatments. Phase 3 trials (MAPP1 and MAPP2), randomized and double-blind, enrolled 194 participants and reported clinically meaningful reductions in PTSD severity (Clinician-Administered PTSD Scale scores dropping by 23–24 points on MDMA versus 14–15 on placebo), with 67% achieving remission in the MDMA arm compared to 32% in placebo. However, these results have been critiqued for methodological flaws, including functional unblinding—over 90% of MDMA participants and 75% of placebo participants correctly guessed their assignment due to MDMA's distinct psychoactive effects, potentially inflating efficacy via expectancy bias.[173][39][41] Policy debates intensified as phase 3 data were submitted for FDA approval in 2023, highlighting tensions between therapeutic potential and Schedule I constraints. Proponents, including MAPS (later Lykos Therapeutics), argued for rescheduling to Schedule III, citing administrative law judge Francis Young's 1987 recommendation against Schedule I placement due to evidence of safety under medical supervision and low abuse potential in therapeutic contexts—a ruling overruled by DEA Administrator John Lawn amid concerns over recreational use patterns. Critics, including some researchers and regulators, emphasized insufficient long-term safety data, ethical lapses in trials (such as allegations of therapist-patient boundary violations and undisclosed MAPS founder involvement in studies), and biases from advocacy-funded research, which may prioritize positive outcomes over rigorous controls. The FDA's Psychopharmacologic Drugs Advisory Committee voted 9–2 against approval in June 2024, citing unblinding, inadequate cardiovascular risk assessments, and gaps in diverse population data; the agency issued a Complete Response Letter in August 2024, requiring additional phase 3 trials without guaranteeing future approval. As of 2025, MDMA remains Schedule I federally, with no accepted medical use, though limited expanded access programs allow compassionate use for severe PTSD cases.[174][37][175] Internationally, policy shifts have fueled U.S. debates; Australia's Therapeutic Goods Administration rescheduled MDMA (and psilocybin) to allow psychiatrist-prescribed use for PTSD and depression in 2023, based on similar trial data, prompting calls for comparable reforms amid critiques that Schedule I status hinders empirical validation of MDMA's risk-benefit profile. Ongoing discussions question the DEA's scheduling criteria, arguing they conflate recreational harms (e.g., acute serotonin syndrome, hyperthermia) with controlled therapeutic administration, where abuse potential appears minimal due to infrequent dosing and supervision. Yet, skepticism persists regarding generalizability, given trials' small sample sizes (n<100 per arm), exclusion of comorbid conditions common in PTSD populations, and reliance on subjective outcomes vulnerable to placebo effects—issues compounded by MAPS' dual role as funder and advocate, raising conflict-of-interest concerns. These debates underscore broader tensions in psychedelic policy: balancing preliminary efficacy signals against evidentiary gaps and historical precedents of overstated therapeutic claims for scheduled substances.[45][176]Legal and Regulatory Framework
International Treaties and Scheduling
MDMA is controlled internationally primarily under the 1971 United Nations Convention on Psychotropic Substances, which establishes schedules for psychotropic substances based on their potential for abuse, therapeutic utility, and safety profile.[177] This treaty, ratified by over 180 countries, requires signatories to implement domestic controls prohibiting non-medical production, trade, and possession of scheduled substances, with limited exceptions for scientific research under license. MDMA, or 3,4-methylenedioxymethamphetamine, was added to Schedule I—the most restrictive category—indicating a high potential for abuse, no accepted medical use in treatment, and lack of safety for use under medical supervision. Schedule I placement mandates criminalization of recreational and unauthorized uses, with allowances only for minimal quantities in authorized scientific studies.[178] The scheduling process for MDMA began in the mid-1980s amid rising recreational use reports in the United States and Europe. In 1984, the U.S. Drug Enforcement Administration requested a World Health Organization (WHO) review, leading to an Expert Committee on Drug Dependence assessment in 1985 that recommended Schedule I status, citing abuse liability evidenced by animal studies on serotonin neurotoxicity and human self-reports of dependence, despite limited human clinical data at the time.[179] The UN Commission on Narcotic Drugs (CND) formally adopted this recommendation on February 20, 1986, during its 32nd session in Vienna, binding parties to implement controls by August 1986.[155] This decision followed emergency scheduling in the U.S. in 1985 and aligned with broader efforts to curb emerging synthetic drug markets, though critics noted the WHO's reliance on preclinical data from analogs like MDA rather than comprehensive MDMA-specific epidemiology.[179] No provisions for rescheduling exist without a formal WHO review and CND vote, which has not occurred despite subsequent research suggesting potential therapeutic benefits for post-traumatic stress disorder; Schedule I status thus precludes routine medical authorization globally, though some nations grant research waivers.[180] Precursors like safrole and piperonal, used in MDMA synthesis, fall under Table I of the 1988 United Nations Convention against Illicit Traffic in Narcotic Drugs and Psychotropic Substances, requiring export/import licensing to prevent diversion, but this addresses supply chains rather than the substance itself.[181] The 1961 Single Convention on Narcotic Drugs does not cover MDMA, as it targets traditional narcotics rather than synthetic amphetamine derivatives.[178] These treaties collectively enforce a prohibitionist framework, with non-compliance risking international sanctions, though enforcement varies by state capacity and policy priorities.United States Regulations
MDMA is classified as a Schedule I controlled substance under the Controlled Substances Act, signifying high potential for abuse, no currently accepted medical use in treatment in the United States, and lack of accepted safety for use under medical supervision.[182][6] The Drug Enforcement Administration (DEA) imposed emergency scheduling on MDMA effective July 1, 1985, following a Federal Register notice on May 31, 1985, amid concerns over increasing recreational distribution and emerging evidence of neurotoxicity in animal studies. This action invoked the emergency provisions of 21 U.S.C. § 811(h), allowing temporary placement in Schedule I for up to one year pending further review.[183] Administrative hearings ensued, with testimony from researchers advocating for Schedule III placement based on preliminary therapeutic observations, contrasted by DEA arguments emphasizing abuse liability akin to other amphetamines.[169] The emergency classification was upheld through judicial review, and MDMA was permanently scheduled in Schedule I on March 23, 1988, after the DEA finalized rulemaking.[184] This status prohibits manufacture, distribution, possession, and importation outside of DEA-authorized research protocols, with federal penalties including up to 20 years imprisonment for trafficking offenses.[182] Notwithstanding Schedule I constraints, the Food and Drug Administration (FDA) designated MDMA-assisted psychotherapy as a breakthrough therapy for severe post-traumatic stress disorder (PTSD) on August 25, 2017, enabling accelerated clinical development and FDA guidance.[64] Phase 3 trials sponsored by the Multidisciplinary Association for Psychedelic Studies (MAPS), now Lykos Therapeutics, reported significant symptom reductions in PTSD patients, yet the FDA rejected their New Drug Application in August 2024, citing deficiencies in trial design, bias risks, and need for confirmatory data via an additional Phase 3 study.[185][186] As of October 2025, MDMA retains Schedule I status, blocking therapeutic approval without rescheduling, though expanded access and investigator-initiated research continue under DEA Schedule I registrations.[6] State-level decriminalization efforts, such as Oregon's Measure 110, do not alter federal prohibitions on MDMA.[187]Variations in Other Jurisdictions
In Australia, MDMA was rescheduled on July 1, 2023, to permit authorised psychiatrists to prescribe it as a Schedule 8 controlled substance for treating post-traumatic stress disorder (PTSD) in patients unresponsive to standard therapies, marking the first national approval for MDMA-assisted psychotherapy worldwide.[188][189] This pathway requires special access via the Therapeutic Goods Administration (TGA), as no MDMA products are fully approved on the Australian Register of Therapeutic Goods, and prescriptions are limited to specific psychiatric conditions with rigorous oversight.[190] Possession, production, or supply outside this medical framework remains prohibited under the Poisons Standard.[188] In Canada, MDMA is classified as a Schedule I substance under the Controlled Drugs and Substances Act, prohibiting its possession, production, trafficking, or importation except under strict exemptions for research or medical purposes.[191] However, British Columbia implemented a three-year decriminalization pilot on January 31, 2023, exempting adults from criminal charges for possessing up to 2.5 grams of MDMA combined with other opioids, cocaine, or methamphetamine for personal use in private settings, aiming to redirect resources toward harm reduction rather than enforcement.[192][193] This provincial policy, extended until January 31, 2026, does not legalize MDMA or permit sales, and federal law still imposes penalties up to seven years imprisonment for possession offenses outside the pilot.[191] The United Kingdom designates MDMA as a Class A drug under the Misuse of Drugs Act 1971, subjecting possession to up to seven years imprisonment, an unlimited fine, or both, with harsher penalties for supply or production.[194] It is also listed in Schedule 1 of the Misuse of Drugs Regulations 2001, restricting it to research-only use due to the government's assessment of no recognized therapeutic value, despite ongoing clinical trials for PTSD.[195] Across Europe, MDMA is uniformly prohibited under national implementations of the 1971 UN Convention on Psychotropic Substances, with possession and supply criminalized in all member states.[196] Portugal stands out for decriminalizing personal possession of up to 1 gram of MDMA since 2001, treating it as an administrative offense subject to dissuasion commissions rather than criminal prosecution, though production and trafficking remain felonies.[197] Other countries, such as the Netherlands, enforce strict bans despite tolerant policies toward cannabis coffeeshops, with MDMA seizures and purity monitoring indicating robust underground markets.[196] Israel permits compassionate use of MDMA for PTSD treatment since 2019 under medical exemptions, but recreational possession is illegal.[198] In most Asian, African, and Latin American jurisdictions, MDMA holds equivalent Schedule I status with severe penalties, reflecting adherence to international treaties without notable therapeutic exceptions as of 2025.[193]Societal Implications and Controversies
Cultural and Economic Dimensions
MDMA, commonly known as ecstasy, became intrinsically linked to the emergence of rave culture in the late 1980s, particularly in the United Kingdom, where it fueled extended dancing sessions amid the rise of house and acid house music scenes imported from Ibiza.[199] This association transformed nightlife, with MDMA's empathogenic effects—promoting feelings of emotional openness, intimacy, and euphoria—aligning with the communal, hedonistic ethos of electronic dance music (EDM) events.[200][155] Early perceptions positioned MDMA as a relatively benign "positive" substance within these subcultures, contrasting with harder drugs like cocaine or heroin, though this view overlooked emerging evidence of neurotoxicity and overdose risks.[201] The drug's cultural footprint expanded globally through music festivals and club scenes, where it enhanced sensory experiences of rhythm and light, fostering a sense of unity and escapism from societal norms.[202] In contemporary contexts, such as the 2023 Nova music festival in Israel, anecdotal and preliminary neuroscientific reports suggest MDMA use may have mitigated post-traumatic stress symptoms among survivors of the Hamas attack, highlighting its perceived role in emotional processing beyond recreation.[203] However, rave culture's stigma persists, often tied to concerns over polydrug use, dehydration, and serotonin depletion, with epidemiological data indicating higher prevalence of MDMA consumption at EDM events compared to general populations.[204][205] Economically, the European MDMA market sustains a robust illicit economy, primarily supplied by clandestine laboratories in the Netherlands and Belgium, which dominate production and export to other regions.[206] This trade yields substantial profits for organized crime networks, with a minimum estimated annual retail value in Europe exceeding billions of euros, driven by high demand at festivals and clubs.[207] Production efficiency has increased, with one kilogram of ecstasy tablets generating 21 to 58 kilograms of waste, underscoring environmental costs alongside low raw material expenses from precursor chemicals like safrole derivatives.[22] Black market pricing reflects supply chain dynamics, with U.S. retail doses (typically 70-100 mg MDMA per pill) averaging $15-25, while wholesale variations across cities indicate regional flows from production hubs.[208][209] Disruptions, such as precursor restrictions, have prompted adaptations in synthesis methods, maintaining market resilience despite enforcement efforts.[210] The illicit trade's profitability stems from negligible production costs relative to retail markups, paralleling patterns in other synthetic drugs, though exact global figures remain elusive due to underreporting and clandestine operations.[211]Public Health and Policy Critiques
Recreational MDMA use is associated with acute risks including hyperthermia, dehydration, hyponatremia, and cardiovascular complications, which can lead to organ failure or death, particularly in settings like crowded raves where environmental factors exacerbate physiological stress.[122] [89] Overdose deaths linked to MDMA are relatively rare compared to opioids, with UK estimates from the late 1990s placing the annual death rate per 10,000 users aged 15-24 at 0.2 to 5.3, though adulterants like PMA increase lethality by delaying onset and prompting redosing.[212] In the US, MDMA-related fatalities often involve polysubstance use, contributing to broader stimulant overdose trends, but pure MDMA toxicity remains a concern due to serotonin syndrome and hyperthermic crises.[80] Chronic effects raise concerns of serotonergic neurotoxicity, with human studies showing reduced serotonin transporter density and CSF 5-HIAA levels in users, correlating with verbal memory impairments and mood dysregulation even after abstinence.[113] [213] While moderate use shows inconsistent neuroimaging changes, heavy or frequent exposure links to persistent axonal damage in animal models translated to humans, potentially underlying long-term anxiety, depression, and cognitive deficits, though causation is confounded by polydrug use and pre-existing vulnerabilities.[214] [215] Critics note that pro-therapeutic advocacy may underemphasize these risks, as institutional biases in academia favor novel treatments over conservative harm assessments.[216] Addiction potential is lower than for classical stimulants, with past-year US use at 1.0% among those aged 12+, but 92% of initiates progressing to other substances like cocaine or heroin, amplifying public health burdens via polysubstance escalation.[217] [218] Dependence manifests psychologically through craving and tolerance, though physical withdrawal is mild, yet repeated use sustains demand in illicit markets prone to contamination.[219] Policy critiques center on MDMA's Schedule I classification under the US Controlled Substances Act since 1985, which equates its abuse liability and medical void to heroin despite empirical data showing lower lethality and emerging therapeutic signals, arguably stifling research while failing to curb recreational prevalence.[220] Enforcement has driven black-market impurities, heightening acute risks, as prohibition precludes purity regulation akin to alcohol or tobacco.[122] Recent FDA advisory rejection of MDMA-assisted therapy for PTSD in June 2024 cited study flaws like functional unblinding, inadequate safety data, and ethical lapses in blinding, underscoring policy tensions between innovation and evidentiary rigor amid psychedelics' resurgence.[221] [222] This scheduling rigidity, rooted in 1980s moral panic rather than updated risk-benefit analysis, exemplifies causal disconnects in drug policy, where blanket bans ignore dose-dependent harms and controlled-use potentials.[223]Debates on Therapeutic Value vs. Risks
Proponents of MDMA-assisted psychotherapy (MDMA-AP) for post-traumatic stress disorder (PTSD) cite phase 3 clinical trials demonstrating significant symptom reduction. In the MAPP2 trial, a multi-site, randomized, double-blind, placebo-controlled study involving 104 participants with moderate to severe PTSD, MDMA-AP led to a 71.2% rate of participants no longer meeting PTSD diagnostic criteria at 18 weeks, compared to 47.6% in the placebo group receiving therapy alone; the change in Clinician-Administered PTSD Scale (CAPS-5) scores was -23.7 points for MDMA versus -14.8 for placebo.[39] A meta-analysis of earlier studies similarly found MDMA-AP associated with greater reductions in PTSD symptoms, with response rates up to 83% in some cohorts.[224] Advocates, including the Multidisciplinary Association for Psychedelic Studies (MAPS), argue these outcomes represent a breakthrough for treatment-resistant PTSD, attributing efficacy to MDMA's facilitation of emotional processing and reduced fear response in therapy sessions, with effects persisting beyond acute dosing.[57] Critics, however, highlight methodological flaws undermining these claims, particularly unblinding where over 90% of MDMA recipients and 75% of placebo participants correctly guessed their assignment due to MDMA's distinct psychoactive effects, potentially inflating perceived benefits through expectancy bias.[41] The U.S. Food and Drug Administration (FDA) rejected Lykos Therapeutics' (formerly MAPS) new drug application in August 2024, citing inadequate study design, insufficient diversity in trial populations, and limited long-term safety data; an advisory committee voted 9-2 against efficacy and 10-1 against balancing risks with benefits.[43] Additional scrutiny includes ethical concerns, such as therapist involvement in advocacy and data integrity issues leading to retractions of three MDMA-AP papers in 2024, raising questions of bias in MAPS-funded research where sponsors influenced protocol and analysis.[225] Independent reviews note that while short-term symptom relief occurs, sustained effects remain unproven against standard therapies like prolonged exposure, and trials lacked active comparators to isolate MDMA's contribution from psychotherapy.[37] Risks of MDMA-AP include acute cardiovascular effects such as elevated blood pressure and heart rate, observed in trials and linked to sympathomimetic action, with potential for dysrhythmias or hypertensive crises in vulnerable patients.[100] Neurotoxicity concerns stem from preclinical data showing serotonin neuron depletion and axonal damage after high or repeated doses, though human therapeutic protocols (80-180 mg, 2-3 sessions) report no confirmed long-term deficits; critics argue insufficient monitoring for subtle, cumulative effects like impaired memory or mood dysregulation.[226] Trial data revealed increased odds of side effects (e.g., transient anxiety, jaw clenching) versus placebo, alongside rare serious adverse events including suicidal ideation in 3-6% of participants across phases, potentially exacerbated by MDMA's serotonergic modulation.[227] Broader debates emphasize abuse liability, as MDMA's Schedule I status reflects recreational risks of dependence and overdose, with therapeutic diversion posing public health threats if approved without strict controls.[90]| Aspect | Therapeutic Evidence | Risk Concerns |
|---|---|---|
| Efficacy | Phase 3 trials show CAPS-5 reductions of 20+ points; remission rates 67-71% at 18 weeks.[39] | Blinding failures and bias in sponsor-led studies question attribution to MDMA over therapy/expectancy.[41] |
| Safety | Generally well-tolerated in controlled doses; no confirmed cardiac valvulopathy in pharma-grade use.[90] | Acute CV strain, potential neurotoxicity, elevated suicidal events (RR ~1.0 but low certainty).[228][226] |
| Long-term | Some follow-up suggests durability up to 1 year. | Lacks Phase 4 data; recreational parallels suggest addiction/serotonergic depletion risks.[229] |