Recent from talks
Nothing was collected or created yet.
Hormone replacement therapy
View on Wikipedia

Hormone replacement therapy (HRT), also known as menopausal hormone therapy or postmenopausal hormone therapy, is a form of hormone therapy used to treat symptoms associated with female menopause.[1][2] Effects of menopause can include symptoms such as hot flashes, accelerated skin aging, vaginal dryness, decreased muscle mass, and complications such as osteoporosis (bone loss), sexual dysfunction, and vaginal atrophy. They are mostly caused by low levels of female sex hormones (e.g. estrogens) that occur during menopause.[1][2]
Estrogens and progestogens are the main hormone drugs used in HRT. Progesterone is the main female sex hormone that occurs naturally and is also manufactured into a drug that is used in menopausal hormone therapy.[1] Although both classes of hormones can have symptomatic benefit, progestogen is specifically added to estrogen regimens, unless the uterus has been removed, to avoid the increased risk of endometrial cancer. Unopposed estrogen therapy promotes endometrial hyperplasia and increases the risk of cancer, while progestogen reduces this risk.[3][4] Androgens like testosterone are sometimes used as well.[5] HRT is available through a variety of different routes.[1][2]
The long-term effects of HRT on most organ systems vary by age and time since the last physiological exposure to hormones, and there can be large differences in individual regimens, factors which have made analyzing effects difficult.[6] The Women's Health Initiative (WHI) is an ongoing study of over 27,000 women that began in 1991, with the most recent analyses suggesting that, when initiated within 10 years of menopause, HRT reduces all-cause mortality and risks of coronary disease, osteoporosis, and dementia; after 10 years the beneficial effects on mortality and coronary heart disease are no longer apparent, though there are decreased risks of hip and vertebral fractures and an increased risk of venous thromboembolism when taken orally.[7][8]
"Bioidentical" hormone replacement is a development in the 21st century and uses manufactured compounds with "exactly the same chemical and molecular structure as hormones that are produced in the human body."[9] These are mainly manufactured from plant steroids[10] and can be a component of either registered pharmaceutical or custom-made compounded preparations, with the latter generally not recommended by regulatory bodies due to their lack of standardization and formal oversight.[11] Bioidentical hormone replacement has inadequate clinical research to determine its safety and efficacy as of 2017.[12]
The current indications for use from the United States Food and Drug Administration (FDA) include short-term treatment of menopausal symptoms, such as vasomotor hot flashes or vaginal atrophy, and prevention of osteoporosis.[13]
Medical uses
[edit]Approved uses of HRT in the United States include short-term treatment of menopausal symptoms such as hot flashes and vaginal atrophy, and prevention of osteoporosis.[13] The American College of Obstetrics and Gynecology (ACOG) approves of HRT for symptomatic relief of menopausal symptoms,[14] and advocates its use beyond the age of 65 in appropriate scenarios.[15] The 2016 annual meeting of The Menopause Society (formerly the North American Menopause Society) mentioned that HRT may have more benefits than risks in women before the age of 60.[16]
A consensus expert opinion published by The Endocrine Society stated that when taken during perimenopause or the initial years of menopause, HRT carries fewer risks than previously published, and reduces all cause mortality in most scenarios.[2] The American Association of Clinical Endocrinologists (AACE) has also released position statements approving of HRT when appropriate.[12]
Women receiving this treatment are usually post-, peri-, or surgically induced menopausal. Menopause is the permanent cessation of menstruation resulting from loss of ovarian follicular activity, defined as beginning twelve months after the final natural menstrual cycle. This twelve month time point divides menopause into early and late transition periods known as 'perimenopause' and 'postmenopause'.[4] Premature menopause can occur if the ovaries are surgically removed, as can be done to treat ovarian or uterine cancer.
Demographically, the vast majority of data available is in postmenopausal American women with concurrent pre-existing conditions and an average age of over 60 years.[17]
Menopausal symptoms
[edit]
HRT is often given as a short-term relief from menopausal symptoms during perimenopause.[18] Potential menopausal symptoms include:[1][2]
- Hot flashes – vasomotor symptoms
- Vulvovaginal atrophy – atrophic vaginitis and dryness
- Dyspareunia – painful sexual intercourse due to vaginal atrophy and lack of lubrication
- Bone loss – decreased bone mineral density, which can eventually lead to osteopenia, osteoporosis, and associated fractures
- Decreased sexual desire
- Defeminization – diminished feminine fat distribution and accelerated skin aging[19][20]
- Sleep disturbances and joint pain
The most common of these are loss of sexual drive and vaginal dryness.[4][21]
The use of hormone therapy for heart health among menopausal women has declined significantly over the past few decades.[22] In 1999, nearly 27% of menopausal women in the U.S. used estrogen, but by 2020, that figure had dropped to less than 5%.[23][24] Recent evidence in 2024 suggests evidence supporting the cardiovascular benefits of hormone therapy, including improvements in insulin resistance and other heart-related markers.[25] This adds to a growing body of research highlighting hormone therapy's effectiveness, not only for heart health but also for managing menopausal symptoms like hot flashes, disrupted sleep, vaginal dryness, and painful intercourse.[26] Despite its proven benefits, many menopausal women avoid hormone therapy, often due to lingering misconceptions about its risks and societal discomfort with openly discussing menopause.[22]
Sexual function
[edit]
HRT can help with the lack of sexual desire and sexual dysfunction that can occur with menopause. Epidemiological surveys of women between 40 and 69 years suggest that 75% of women remain sexually active after menopause.[4] With increasing life spans, women today are living one third or more of their lives in a postmenopausal state, a period during which healthy sexuality can be integral to their quality of life.[27]
Decreased libido and sexual dysfunction are common issues in postmenopausal women, an entity referred to hypoactive sexual desire disorder (HSDD); its signs and symptoms can both be improved by HRT.[5][28] Several hormonal changes take place during this period, including a decrease in estrogen and an increase in follicle-stimulating hormone. For most women, the majority of change occurs during the late perimenopausal and postmenopausal stages.[4] Decreases in sex hormone-binding globulin (SHBG) and inhibin (A and B) also occur. Testosterone is present in women at a lower level than men, peaking at age 30 and declining gradually with age; there is less variation during the menopausal transition relative to estrogen and progesterone.[4]
A global consensus position statement has advised that postmenopausal testosterone replacement to premenopausal levels can be effective for HSDD. Safety information for testosterone treatment is not available beyond two years of continuous therapy however and dosing above physiologic levels is not advised.[29] Testosterone patches have been found to restore sexual desire in post menopausal women.[30] There is insufficient data to evaluate the impact of testosterone replacement on heart disease, breast cancer, with most trials having included women taking concomitant estrogen and progesterone and with testosterone therapy itself being relatively short in duration. In the setting of this limited data, testosterone therapy has not been associated with adverse events.[29]
Not all women are responsive, especially those with preexisting sexual difficulties.[21] Estrogen replacement can restore vaginal cells, pH levels, and blood flow to the vagina, all of which tend to deteriorate at the onset of menopause. Pain or discomfort with sex appears to be the most responsive component to estrogen.[21] It also has been shown to have positive effects on the urinary tract.[21] Estrogen can also reduce vaginal atrophy and increase sexual arousal, frequency and orgasm.[21]
The effectiveness of hormone replacement can decline in some women after long-term use.[21] A number of studies have also found that the combined effects of estrogen/androgen replacement therapy can increase libido and arousal over estrogen alone.[21] Tibolone, a synthetic steroid with estrogenic, androgenic, and progestogenic properties that is available in Europe, has the ability to improve mood, libido, and physical symptomatology. In various placebo-controlled studies, improvements in vasomotor symptoms, emotional response, sleep disturbances, physical symptoms, and sexual desire have been seen, though it also carries a similar risk profile to conventional HRT.[5]
Muscle and bone
[edit]There is a significant decrease in hip fracture risk during treatment that to a lesser degree persists after HRT is stopped.[31][32] It also helps collagen formation, which in turn improves intervertebral disc and bone strength.[33]
Hormone replacement therapy in the form of estrogen and androgen can be effective at reversing the effects of aging on muscle.[34] Lower testosterone is associated with lower bone density and higher free testosterone is associated with lower hip fracture rates in older women.[35] Testosterone therapy, which can be used for decreased sexual function, can also increase bone mineral density and muscle mass.[29]
Side effects
[edit]Side effects in HRT occur with varying frequency and include:[36]
Common
[edit]- Headache
- Upset stomach, stomach cramps or bloating
- Diarrhea
- Appetite and weight changes
- Changes in sex drive or performance
- Nervousness
- Brown or black patches on the skin
- Acne
- Swelling of hands, feet, or lower legs due to fluid retention
- Changes in menstrual flow
- Breast tenderness, enlargement, or discharge
- Sudden difficulty wearing contact lenses
Uncommon
[edit]- Double vision
- Severe abdominal pain
- Yellowing of skin or eyes
- Severe depression
- Unusual bleeding
- Loss of appetite
- Skin rash
- Lassitude
- Fever
- Dark-colored urine
- Light colored stool
- Chorea[37]
Health effects
[edit]Heart disease
[edit]
The effect of HRT in menopause appears to be divergent, with lower risk of heart disease when started within five years, but no impact after ten.[38][39][40] For women who are in early menopause and have no issues with their cardiovascular health, HRT comes with a low risk of adverse cardiovascular events.[41] There may be an increase in heart disease if HRT is given twenty years post-menopause.[31] This variability has led some reviews to suggest an absence of significant effect on morbidity.[42] Importantly, there is no difference in long-term mortality from HRT, regardless of age.[6]
A Cochrane review suggested that women starting HRT less than 10 years after menopause had lower mortality and coronary heart disease, without any strong effect on the risk of stroke and pulmonary embolism.[38] Those starting therapy more than 10 years after menopause showed little effect on mortality and coronary heart disease, but an increased risk of stroke. Both therapies had an association with venous clots and pulmonary embolism.[38]
HRT with estrogen and progesterone also improves cholesterol levels. With menopause, HDL decreases, while LDL, triglycerides and lipoprotein a increase, patterns that reverse with estrogen. Beyond this, HRT improves heart contraction, coronary blood flow, sugar metabolism, and decreases platelet aggregation and plaque formation. HRT may promote reverse cholesterol transport through induction of cholesterol ABC transporters.[43] Atherosclerosis imaging trials show that HRT decreases the formation of new vascular lesions, but does not reverse the progression of existing lesions.[44] HRT also results in a large reduction in the pro-thrombotic lipoprotein a.[45]
Studies on cardiovascular disease with testosterone therapy have been mixed, with some suggesting no effect or a mild negative effect, though others have shown an improvement in surrogate markers such as cholesterol, triglycerides and weight.[29][46] Testosterone has a positive effect on vascular endothelial function and tone with observational studies suggesting that women with lower testosterone may be at greater risk for heart disease. Available studies are limited by small sample size and study design. Low sex hormone-binding globulin, which occurs with menopause, is associated with increased body mass index and risk for type 2 diabetes.[35]
Blood clots
[edit]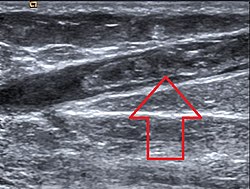
Effects of hormone replacement therapy on venous blood clot formation and potential for pulmonary embolism may vary with different estrogen and progestogen therapies, and with different doses or method of use.[17] Comparisons between routes of administration suggest that when estrogens are applied to the skin or vagina, there is a lower risk of blood clots,[17][47] whereas when used orally, the risk of blood clots and pulmonary embolism is increased.[38] Skin and vaginal routes of hormone therapy are not subject to first pass metabolism, and so lack the anabolic effects that oral therapy has on liver synthesis of vitamin K-dependent clotting factors, possibly explaining why oral therapy may increase blood clot formation.[48]
While a 2018 review found that taking progesterone and estrogen together can decrease this risk,[47] other reviews reported an increased risk of blood clots and pulmonary embolism when estrogen and progestogen were combined, particularly when treatment was started 10 years or more after menopause and when the women were older than 60 years.[17][38]
The risk of venous thromboembolism may be reduced with bioidentical preparations, though research on this is only preliminary.[49]
Stroke
[edit]Multiple studies suggest that the possibility of HRT related stroke is absent if therapy is started within five years of menopause,[50] and that the association is absent or even preventive when given by non-oral routes.[8] Ischemic stroke risk was increased during the time of intervention in the WHI, with no significant effect after the cessation of therapy[31] and no difference in mortality at long term follow up.[6] When oral synthetic estrogen or combined estrogen-progestogen treatment is delayed until five years from menopause, cohort studies in Swedish women have suggested an association with hemorrhagic and ischemic stroke.[50] Another large cohort of Danish women suggested that the specific route of administration was important, finding that although oral estrogen increased risk of stroke, absorption through the skin had no impact, and vaginal estrogen actually had a decreased risk.[8]
Endometrial cancer
[edit]
In postmenopausal women, continuous combined estrogen plus progestin decreases endometrial cancer incidence.[51] The duration of progestogen therapy should be at least 14 days per cycle to prevent endometrial disease.[52]
Endometrial cancer has been grouped into two forms in the context of hormone replacement. Type 1 is the most common, can be associated with estrogen therapy, and is usually low grade. Type 2 is not related to estrogen stimulation and usually higher grade and poorer in prognosis.[53] The endometrial hyperplasia that leads to endometrial cancer with estrogen therapy can be prevented by concomitant administration of progestogen.[53] The extensive use of high-dose estrogens for birth control in the 1970s is thought to have resulted in a significant increase in the incidence of type 1 endometrial cancer.[54]
Paradoxically, progestogens do promote the growth of uterine fibroids, and a pelvic ultrasound can be performed before beginning HRT to make sure there are no underlying uterine or endometrial lesions.[53]
Androgens do not stimulate endometrial proliferation in post menopausal women, and appear to inhibit the proliferation induced by estrogen to a certain extent.[55]
There is insufficient high‐quality evidence to inform women considering hormone replacement therapy after treatment for endometrial cancer.[56]
Breast cancer
[edit]In general, hormone replacement therapy to treat menopause is associated with only a small increased risk of breast cancer.[57][58][59] The level of risk also depends on the type of HRT, the duration of the treatment and the age of the person.[58][60] Oestrogen-only HRT, taken by people who had a hysterectomy, comes with an extremely low level of breast cancer risk. The most commonly taken combined HRT (oestrogen and progestogen) is linked to a small risk of breast cancer. This risk is lower for women in their 50s and higher for older women. The risk increases with the duration of HRT. When HRT is taken for a year or less, there is no increased risk of breast cancer. HRT taken for more than 5 years comes with an increased risk but the risk reduces after the therapy is stopped.[58][59]
There is a non-statistically significant increased rate of breast cancer for hormone replacement therapy with synthetic progestogens.[6] The risk may be reduced with bioidentical progesterone,[61] though the only prospective study that suggested this was underpowered due to the rarity of breast cancer in the control population. There have been no randomized controlled trials as of 2018.[62] The relative risk of breast cancer also varies depending on the interval between menopause and HRT and route of synthetic progestin administration.[63][64]
The most recent follow up of the Women's Health Initiative participants demonstrated a lower incidence of breast cancer in post-hysterectomy participants taking equine estrogen alone, though the relative risk was increased if estrogen was taken with medroxyprogesterone.[24] Estrogen is usually only given alone in the setting of a hysterectomy due to the increased risk of vaginal bleeding and uterine cancer with unopposed estrogen.[65][66]
HRT has been more strongly associated with risk of breast cancer in women with lower body mass indices (BMIs). No breast cancer association has been found with BMIs of over 25.[67] It has been suggested by some that the absence of significant effect in some of these studies could be due to selective prescription to overweight women who have higher baseline estrone, or to the very low progesterone serum levels after oral administration leading to a high tumor inactivation rate.[68]
Evaluating the response of breast tissue density to HRT using mammography appears to help assessing the degree of breast cancer risk associated with therapy; women with dense or mixed-dense breast tissue have a higher risk of developing breast cancer than those with low density tissue.[69]
Micronized progesterone does not appear to be associated with breast cancer risk when used for less than five years with limited data suggesting an increased risk when used for longer duration.[70]
For women who previously have had breast cancer, it is recommended to first consider other options for menopausal effects, such as bisphosphonates or selective estrogen receptor modulators (SERMs) for osteoporosis, cholesterol-lowering agents and aspirin for cardiovascular disease, and vaginal estrogen for local symptoms. Observational studies of systemic HRT after breast cancer are generally reassuring. If HRT is necessary after breast cancer, estrogen-only therapy or estrogen therapy with a progestogen may be safer options than combined systemic therapy.[71] In women who are BRCA1 or BRCA2 mutation carriers, HRT does not appear to impact breast cancer risk.[72] The relative number of women using HRT who also obtain regular screening mammograms is higher than that in women who do not use HRT, a factor which has been suggested as contributing to different breast cancer detection rates in the two groups.[73]
With androgen therapy, pre-clinical studies have suggested an inhibitory effect on breast tissue though the majority of epidemiological studies suggest a positive association.[74]
Ovarian cancer
[edit]HRT is associated with an increased risk of ovarian cancer, with women using HRT having about one additional case of ovarian cancer per 1,000 users.[75] This risk is decreased when progestogen therapy is given concomitantly, as opposed to estrogen alone, and also decreases with increasing time since stopping HRT.[76] Regarding the specific subtype, there may be a higher risk of serous cancer, but no association with clear cell, endometrioid, or mucinous ovarian cancer.[76] Hormonal therapy in ovarian cancer survivors after surgical removal of the ovaries is generally thought to improval survival rates.[77]
Other cancers
[edit]Colorectal cancer
[edit]In the WHI, women who took combined estrogen-progesterone therapy had a lower risk of getting colorectal cancer. However, the cancers they did have were more likely to have spread to lymph nodes or distant sites than colorectal cancer in women not taking hormones.[78] In colorectal cancer survivors, usage of HRT is thought to lead to lower recurrence risk and overall mortality.[79]
Cervical cancer
[edit]There appears to be a significantly decreased risk of cervical squamous cell cancer in post menopausal women treated with HRT and a weak increase in adenocarcinoma. No studies have reported an increased risk of recurrence when HRT is used with cervical cancer survivors.[80]
Neurodegenerative disorders
[edit]As of 2024 there has been conflicting evidence from clinical studies regarding the beneficial effects of estrogens at reducing the risk of Alzheimer's Disease.[81] For prevention, the WHI suggested in 2013, that HRT may increase risk of dementia if initiated after 65 years of age, but have a neutral outcome or be neuroprotective for those between 50 and 55 years.[31] However, the prospective ELITE trial showed negligible effects on verbal memory and other mental skills regardless of how soon after menopause a woman began HRT.[82]
A 2012 review of clinical and epidemiological studies of HRT and AD, PD, FTD and HIV related dementia concluded results were inconclusive at this time.[83]
The majority of clinical and epidemiological studies show either no association with the risk of developing Parkinson's disease[84][85] or inconclusive results.[83][86] One Danish study suggested an increased risk of Parkinson's with HRT in cyclical dosing schedules.[87]
Other randomized trials have shown HRT to improve executive and attention processes outside of the context of dementia in postmenopausal women, both in asymptomatic and those with mild cognitive impairment.[88][89][90]
As of 2011, estrogen replacement in post menopausal women with Parkinson's disease appeared to improve motor symptoms and activities of daily living , with significant improvement of UPDRS scores.[91] Testosterone replacement has also shown to be associated with small statistically significant improvements in verbal learning and memory in postmenopausal women[92] but DHEA has not been found to improve cognitive performance after menopause.[35]
Pre-clinical studies have indicated that endogenous estrogen and testosterone are neuroprotective and can prevent brain amyloid deposition.[93][94]
Contraindications
[edit]The following are absolute and relative contraindications to HRT:[95]
Absolute contraindications
[edit]- Undiagnosed vaginal bleeding
- Severe liver disease
- Pregnancy
- Severe coronary artery disease
- Aggressive breast, uterine or ovarian cancer
Relative contraindications
[edit]- Migraine headaches
- History of breast cancer
- History of ovarian cancer
- Venous thrombosis
- History of uterine fibroids
- Atypical ductal hyperplasia of the breast
- Active gallbladder disease (cholangitis, cholecystitis)
- Well-differentiated and early endometrial cancer – once treatment for the malignancy is complete, is no longer an absolute contraindication.
History and research
[edit]The extraction of CEEs from the urine of pregnant mares led to the marketing in 1942 of Premarin, one of the earlier forms of estrogen to be introduced.[96][97] From that time until the mid-1970s, estrogen was administered without a supplemental progestogen. Beginning in 1975, studies began to show that without a progestogen, unopposed estrogen therapy with Premarin resulted in an eight-fold increased risk of endometrial cancer, eventually causing sales of Premarin to plummet.[96] It was recognized in the early 1980s that the addition of a progestogen to estrogen reduced this risk to the endometrium.[96] This led to the development of combined estrogen–progestogen therapy, most commonly with a combination of conjugated equine estrogen (Premarin) and medroxyprogesterone (Provera).[96]
Trials
[edit]The Women's Health Initiative trials were conducted between 1991 and 2006 and were the first large, double-blind, placebo-controlled clinical trials of HRT in healthy women.[96] Their results were both positive and negative, suggesting that during the time of hormone therapy itself, there are increases in invasive breast cancer, stroke and lung clots. Other risks include increased endometrial cancer, gallbladder disease, and urinary incontinence, while benefits include decreased hip fractures, decreased incidence of diabetes, and improvement of vasomotor symptoms. There is also an increased risk of dementia with HRT in women over 65, though at younger ages it appears to be neuroprotective. After the cessation of HRT, the WHI continued to observe its participants, and found that most of these risks and benefits dissipated, though some elevation in breast cancer risk did persist.[31] Other studies have also suggested an increased risk of ovarian cancer.[76]
The arm of the WHI receiving combined estrogen and progestin therapy was closed prematurely in 2002 by its Data Monitoring Committee (DMC) due to perceived health risks, though this occurred a full year after the data suggesting increased risk became manifest. In 2004, the arm of the WHI in which post-hysterectomy patients were being treated with estrogen alone was also closed by the DMC. Clinical medical practice changed based upon two parallel Women's Health Initiative (WHI) studies of HRT. Prior studies were smaller, and many were of women who electively took hormonal therapy. One portion of the parallel studies followed over 16,000 women for an average of 5.2 years, half of whom took placebo, while the other half took a combination of CEEs and MPA (Prempro). This WHI estrogen-plus-progestin trial was stopped prematurely in 2002 because preliminary results suggested risks of combined CEEs and progestins exceeded their benefits. The first report on the halted WHI estrogen-plus-progestin study came out in July 2002.[98]
Initial data from the WHI in 2002 suggested mortality to be lower when HRT was begun earlier, between age 50 to 59, but higher when begun after age 60. In older patients, there was an apparent increased incidence of breast cancer, heart attacks, venous thrombosis, and stroke, although a reduced incidence of colorectal cancer and bone fracture. At the time, The WHI recommended that women with non-surgical menopause take the lowest feasible dose of HRT for the shortest possible time to minimize associated risks.[98] Some of the WHI findings were again found in a larger national study done in the United Kingdom, known as the Million Women Study (MWS). As a result of these findings, the number of women taking HRT dropped precipitously.[99] In 2012, the United States Preventive Task Force (USPSTF) concluded that the harmful effects of combined estrogen and progestin therapy likely exceeded their chronic disease prevention benefits.[100][101]
In 2002 when the first WHI follow up study was published, with HRT in post menopausal women, both older and younger age groups had a slightly higher incidence of breast cancer, and both heart attack and stroke were increased in older patients, although not in younger participants. Breast cancer was increased in women treated with estrogen and a progestin, but not with estrogen and progesterone or estrogen alone. Treatment with unopposed estrogen (i.e., an estrogen alone without a progestogen) is contraindicated if the uterus is still present, due to its proliferative effect on the endometrium. The WHI also found a reduced incidence of colorectal cancer when estrogen and a progestogen were used together, and most importantly, a reduced incidence of bone fractures. Ultimately, the study found disparate results for all cause mortality with HRT, finding it to be lower when HRT was begun during ages 50–59, but higher when begun after age 60. The authors of the study recommended that women with non-surgical menopause take the lowest feasible dose of hormones for the shortest time to minimize risk.[98]
The data published by the WHI suggested supplemental estrogen increased risk of venous thromboembolism and breast cancer but was protective against osteoporosis and colorectal cancer, while the impact on cardiovascular disease was mixed.[102] These results were later supported in trials from the United Kingdom, but not in more recent studies from France and China. Genetic polymorphism appears to be associated with inter-individual variability in metabolic response to HRT in postmenopausal women.[103][104]
The WHI reported statistically significant increases in rates of breast cancer, coronary heart disease, strokes and pulmonary emboli. The study also found statistically significant decreases in rates of hip fracture and colorectal cancer. "A year after the study was stopped in 2002, an article was published indicating that estrogen plus progestin also increases the risks of dementia."[105] The conclusion of the study was that the HRT combination presented risks that outweighed its measured benefits. The results were almost universally reported as risks and problems associated with HRT in general, rather than with Prempro, the specific proprietary combination of CEEs and MPA studied.[citation needed]
After the increased clotting found in the first WHI results was reported in 2002, the number of Prempro prescriptions filled reduced by almost half. Following the WHI results, a large percentage of HRT users opted out of them, which was quickly followed by a sharp drop in breast cancer rates. The decrease in breast cancer rates has continued in subsequent years.[106] An unknown number of women started taking alternatives to Prempro, such as compounded bioidentical hormones, though researchers have asserted that compounded hormones are not significantly different from conventional hormone therapy.[107]
The other portion of the parallel studies featured women who were post hysterectomy and so received either placebo progestogen or CEEs alone. This group did not show the risks demonstrated in the combination hormone study, and the estrogen-only study was not halted in 2002. However, in February 2004 it, too, was halted. While there was a 23% decreased incidence of breast cancer in the estrogen-only study participants, risks of stroke and pulmonary embolism were increased slightly, predominantly in patients who began HRT over the age of 60.[108]
Several other large studies and meta-analyses have reported reduced mortality for HRT in women younger than age 60 or within 10 years of menopause, and a debatable or absent effect on mortality in women over 60.[2][109][110][111][112][113]
Though research thus far has been substantial, further investigation is needed to fully understand differences in effect for different types of HRT and lengths of time since menopause.[114][115][33] As of 2023[update], for example, no trial has studied women who begin taking HRT around age 50 and continue taking it for longer than 10 years.[116]
Available forms
[edit]
There are five major human steroid hormones: estrogens, progestogens, androgens, mineralocorticoids, and glucocorticoids. Estrogens and progestogens are the two most often used in menopause. They are available in a wide variety of FDA approved and non–FDA-approved formulations.[9]
In women with intact uteruses, estrogens are almost always given in combination with progestogens, as long-term unopposed estrogen therapy is associated with a markedly increased risk of endometrial hyperplasia and endometrial cancer.[1][2] Conversely, in women who have undergone a hysterectomy or do not have a uterus, a progestogen is not required, and estrogen can be used alone. There are many combined formulations which include both estrogen and progestogen.[citation needed]
Specific types of hormone replacement include:[1][2]
- Estrogens – bioidentical estrogens like estradiol and estriol, animal-derived estrogens like conjugated estrogens (CEEs), and synthetic estrogens like ethinylestradiol
- Progestogens – bioidentical progesterone, and progestins (synthetic progestogens) like medroxyprogesterone acetate (MPA), norethisterone, and dydrogesterone
- Androgens – bioidentical testosterone and dehydroepiandrosterone (DHEA), and synthetic anabolic steroids like methyltestosterone and nandrolone decanoate[117][118]
Tibolone – a synthetic medication available in Europe but not the United States– is more effective than placebo but less effective than combination hormone therapy in postmenopausal women. It may have a decreased risk of breast and colorectal cancer, though conversely it can be associated with vaginal bleeding, endometrial cancer, and increase the risk of stroke in women over age 60 years.[119][120]
Vaginal estrogen can improve local atrophy and dryness, with fewer systemic effects than estrogens delivered by other routes.[121] Sometimes an androgen, generally testosterone, can be added to treat diminished libido.[122][123]
Continuous versus cyclic
[edit]Dosage is often varied cyclically to more closely mimic the ovarian hormone cycle, with estrogens taken daily and progestogens taken for about two weeks every month or every other month, a schedule referred to as 'cyclic' or 'sequentially combined'. Alternatively, 'continuous combined' HRT can be given with a constant daily hormonal dosage.[124] Continuous combined HRT is associated with less complex endometrial hyerplasia than cyclic.[125] Impact on breast density appears to be similar in both regimen timings.[126]
Route of administration
[edit]
The medications used in menopausal HRT are available in numerous different formulations for use by a variety of different routes of administration:[1][2]
- Oral administration – tablets, capsules
- Transdermal administration – patches, gels, creams
- Vaginal administration – tablets, creams, suppositories, rings
- Intramuscular or subcutaneous injection – solutions in vials or ampoules
- Subcutaneous implant – surgically-inserted pellets placed into fat tissue
- Less commonly sublingual, buccal, intranasal, and rectal administration, as well as intrauterine devices
More recently developed forms of drug delivery are alleged to have increased local effect lower dosing, fewer side effects, and constant rather than cyclical serum hormone levels.[1][2] Transdermal and vaginal estrogen, in particular, avoid first pass metabolism through the liver. This in turn prevents an increase in clotting factors and accumulation of anti-estrogenic metabolites, resulting in fewer adverse side effects, particularly with regard to cardiovascular disease and stroke.[127]
Injectable forms of estradiol exist and have been used occasionally in the past.[128][129] However, they are rarely used in menopausal hormone therapy in modern times and are no longer recommended.[128][130] Instead, other non-oral forms of estradiol such as transdermal estradiol are recommended and may be used.[128] Estradiol injectables are generally well-tolerated and convenient, requiring infrequent administration.[128][129] However, this form of estradiol does not release estradiol at a constant rate and there are very high circulating estradiol levels soon after injection followed by a rapid decline in levels.[128] Injections may also be painful.[128] Examples of estradiol injectables that may be used in menopausal hormone therapy include estradiol valerate and estradiol cypionate.[128][129] In terms of injectable progestogens, injectable progesterone is associated with pain and injection site reactions as well as a short duration of action requiring very frequent injections, and is similarly not recommended in menopausal hormone therapy.[131][129]
Bioidentical hormone therapy
[edit]Bioidentical hormone therapy (BHT) is the usage of hormones that are chemically identical to those produced in the body. Although proponents of BHT claim advantages over non-bioidentical or conventional hormone therapy, the FDA does not recognize the term 'bioidentical hormone', stating there is no scientific evidence that these hormones are identical to their naturally occurring counterparts.[11][132] There are, however, FDA approved products containing hormones classified as 'bioidentical'.[12][9]
Bioidentical hormones can be used in either pharmaceutical or compounded preparations, with the latter generally not recommended by regulatory bodies due to their lack of standardization and regulatory oversight.[11] Most classifications of bioidentical hormones do not take into account manufacturing, source, or delivery method of the products, and so describe both non-FDA approved compounded products and FDA approved pharmaceuticals as 'bioidentical'.[9] The British Menopause Society has issued a consensus statement endorsing the distinction between "compounded" forms (cBHRT), described as unregulated, custom made by specialty pharmacies and subject to heavy marketing and "regulated" pharmaceutical grade forms (rBHRT), which undergo formal oversight by entities such as the FDA and form the basis of most clinical trials.[133] Some practitioners recommending compounded bioidentical HRT also use salivary or serum hormonal testing to monitor response to therapy, a practice not endorsed by current clinical guidelines in the United States and Europe.[134]
Bioidentical hormones in pharmaceuticals may have very limited clinical data, with no randomized controlled prospective trials to date comparing them to their animal derived counterparts. Some pre-clinical data has suggested a decreased risk of venous thromboembolism, cardiovascular disease, and breast cancer.[11] As of 2012, guidelines from the North American Menopause Society, the Endocrine Society, the International Menopause Society, and the European Menopause and Andropause Society endorsed the reduced risk of bioidentical pharmaceuticals for those with increased clotting risk.[11][135]
Compounding
[edit]Compounding for HRT is generally discouraged by the FDA and medical industry in the United States due to a lack of regulation and standardized dosing.[11][132] The U.S. Congress did grant the FDA explicit but limited oversight of compounded drugs in a 1997 amendment to the Federal Food, Drug, and Cosmetic Act (FDCA), but they have encountered obstacles in this role since that time. After 64 patient deaths and 750 harmed patients from a 2012 meningitis outbreak due to contaminated steroid injections, Congress passed the 2013 Drug Quality and Security Act, authorizing creation by the FDA of a voluntary registration for facilities that manufactured compounded drugs, and reinforcing FDCA regulations for traditional compounding.[136] The DQSA and its reinforcement of provision §503A of the FDCA solidifies FDA authority to enforce FDCA regulation of against compounders of bioidentical hormone therapy.[136]
In the United Kingdom, on the other hand, compounding is a regulated activity. The Medicines and Healthcare products Regulatory Agency regulates compounding performed under a Manufacturing Specials license and the General Pharmaceutical Council regulates compounding performed within a pharmacy. All testosterone prescribed in the United Kingdom is bioidentical, with its use supported by the National Health Service. There is also marketing authorisation for male testosterone products. National Institute for Health and Care Excellence guideline 1.4.8 states: "consider testosterone supplementation for menopausal women with low sexual desire if HRT alone is not effective". The footnote adds: "at the time of publication (November 2015), testosterone did not have a United Kingdom marketing authorisation for this indication in women. Bioidentical progesterone is used in IVF treatment and for pregnant women who are at risk of premature labour."[citation needed]
Society and culture
[edit]Wyeth controversy
[edit]Wyeth, now a subsidiary of Pfizer, was a pharmaceutical company that marketed the HRT products Premarin (CEEs) and Prempro (CEEs + MPA).[137][138] In 2009, litigation involving Wyeth resulted in the release of 1,500 documents that revealed practices concerning its promotion of these medications.[137][138][139] The documents showed that Wyeth commissioned dozens of ghostwritten reviews and commentaries that were published in medical journals to promote unproven benefits of its HRT products, downplay their harms and risks, and cast competing therapies in a negative light.[137][138][139] Starting in the mid-1990s and continuing for over a decade, Wyeth pursued an aggressive "publication plan" strategy to promote its HRT products through the use of ghostwritten publications.[139] It worked mainly with DesignWrite, a medical writing firm.[139] Between 1998 and 2005, Wyeth had 26 papers promoting its HRT products published in scientific journals.[137]
These favorable publications emphasized the benefits and downplayed the risks of its HRT products, especially the "misconception" of the association of its products with breast cancer.[139] The publications defended unsupported cardiovascular "benefits" of its products, downplayed risks such as breast cancer, and promoted off-label and unproven uses like prevention of dementia, Parkinson's disease, vision problems, and wrinkles.[138] In addition, Wyeth emphasized negative messages against the SERM raloxifene for osteoporosis, instructed writers to stress the fact that "alternative therapies have increased in usage since the WHI even though there is little evidence that they are effective or safe...", called into question the quality and therapeutic equivalence of approved generic CEE products, and made efforts to spread the notion that the unique risks of CEEs and MPA were a class effect of all forms of menopausal HRT: "Overall, these data indicate that the benefit/risk analysis that was reported in the Women's Health Initiative can be generalized to all postmenopausal hormone replacement therapy products."[138]
Following the publication of the WHI data in 2002, the stock prices for the pharmaceutical industry plummeted, and huge numbers of women stopped using HRT.[140] The stocks of Wyeth, which supplied the Premarin and Prempro that were used in the WHI trials, decreased by more than 50%, and never fully recovered.[140] Some of their articles in response promoted themes such as the following: "the WHI was flawed; the WHI was a controversial trial; the population studied in the WHI was inappropriate or was not representative of the general population of menopausal women; results of clinical trials should not guide treatment for individuals; observational studies are as good as or better than randomized clinical trials; animal studies can guide clinical decision-making; the risks associated with hormone therapy have been exaggerated; the benefits of hormone therapy have been or will be proven, and the recent studies are an aberration."[96] Similar findings were observed in a 2010 analysis of 114 editorials, reviews, guidelines, and letters by five industry-paid authors.[96] These publications promoted positive themes and challenged and criticized unfavorable trials such as the WHI and MWS.[96] In 2009, Wyeth was acquired by Pfizer in a deal valued at US$68 billion.[141][142] Pfizer, a company that produces Provera and Depo-Provera (MPA) and has also engaged in medical ghostwriting, continues to market Premarin and Prempro, which remain best-selling medications.[96][139]
According to Fugh-Berman (2010), "Today, despite definitive scientific data to the contrary, many gynecologists still believe that the benefits of [HRT] outweigh the risks in asymptomatic women. This non-evidence–based perception may be the result of decades of carefully orchestrated corporate influence on medical literature."[138] As many as 50% of physicians have expressed skepticism about large trials like the WHI and HERS in a 2011 survey.[143] The positive perceptions of many physicians of HRT in spite of large trials showing risks that potentially outweigh any benefits may be due to the efforts of pharmaceutical companies like Wyeth, according to May and May (2012) and Fugh-Berman (2015).[139][96]
Popularity
[edit]The 1990s showed a dramatic decline in prescription rates, though more recently they have begun to rise again.[127][82] Transdermal therapy, in part due to its lack of increase in venous thromboembolism, is now often the first choice for HRT in the United Kingdom. Conjugate equine estrogen, in distinction, has a potentially higher thrombosis risk and is now not commonly used in the UK, replaced by estradiol based compounds with lower thrombosis risk. Oral progestogen combinations such as medroxyprogesterone acetate have changed to dyhydrogesterone, due to a lack of association of the latter with venous clot.[144]
See also
[edit]References
[edit]- ^ a b c d e f g h i Stuenkel CA, Davis SR, Gompel A, Lumsden MA, Murad MH, Pinkerton JV, Santen RJ (November 2015). "Treatment of Symptoms of the Menopause: An Endocrine Society Clinical Practice Guideline" (PDF). J. Clin. Endocrinol. Metab. 100 (11): 3975–4011. doi:10.1210/jc.2015-2236. PMID 26444994.
- ^ a b c d e f g h i j Santen RJ, Allred DC, Ardoin SP, Archer DF, Boyd N, Braunstein GD, Burger HG, Colditz GA, Davis SR, Gambacciani M, Gower BA, Henderson VW, Jarjour WN, Karas RH, Kleerekoper M, Lobo RA, Manson JE, Marsden J, Martin KA, Martin L, Pinkerton JV, Rubinow DR, Teede H, Thiboutot DM, Utian WH (July 2010). "Postmenopausal hormone therapy: an Endocrine Society scientific statement". J. Clin. Endocrinol. Metab. 95 (7 Suppl 1): s1 – s66. doi:10.1210/jc.2009-2509. PMC 6287288. PMID 20566620.
- ^ Shuster, Lynne T.; Rhodes, Deborah J.; Gostout, Bobbie S.; Grossardt, Brandon R.; Rocca, Walter A. (2010). "Premature menopause or early menopause: Long-term health consequences". Maturitas. 65 (2): 161–166. doi:10.1016/j.maturitas.2009.08.003. ISSN 0378-5122. PMC 2815011. PMID 19733988.
- ^ a b c d e f Eden KJ, Wylie KR (1 July 2009). "Quality of sexual life and menopause". Women's Health. 6 (4): 385–396. doi:10.2217/WHE.09.24. PMID 19586430.
- ^ a b c Ziaei S., Moghasemi M., Faghihzadeh S. (2010). "Comparative effects of conventional hormone replacement therapy and tibolone on climacteric symptoms and sexual dysfunction in postmenopausal women". Climacteric. 13 (3): 147–156. doi:10.1016/j.maturitas.2006.04.014. PMID 16730929.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d Manson, JE; Aragaki, AK; Rossouw, JE; Anderson, GL; Prentice, RL; LaCroix, AZ; Chlebowski, RT; Howard, BV; Thomson, CA; Margolis, KL; Lewis, CE; Stefanick, ML; Jackson, RD; Johnson, KC; Martin, LW; Shumaker, SA; Espeland, MA; Wactawski-Wende, J; WHI, Investigators. (12 September 2017). "Menopausal Hormone Therapy and Long-term All-Cause and Cause-Specific Mortality: The Women's Health Initiative Randomized Trials". JAMA. 318 (10): 927–938. doi:10.1001/jama.2017.11217. PMC 5728370. PMID 28898378.
- ^ Langer, RD; Hodis, HN; Lobo, RA; Allison, MA (February 2021). "Hormone replacement therapy – where are we now?". Climacteric. 24 (1): 3–10. doi:10.1080/13697137.2020.1851183. PMID 33403881. S2CID 230783545.
- ^ a b c Løkkegaard, E; Nielsen, LH; Keiding, N (August 2017). "Risk of Stroke With Various Types of Menopausal Hormone Therapies: A National Cohort Study". Stroke. 48 (8): 2266–2269. doi:10.1161/STROKEAHA.117.017132. PMID 28626058. S2CID 207579406.
- ^ a b c d Files, JA; Ko, MG; Pruthi, S (July 2011). "Bioidentical hormone therapy". Mayo Clinic Proceedings. 86 (7): 673–80, quiz 680. doi:10.4065/mcp.2010.0714. PMC 3127562. PMID 21531972.
- ^ "Bioidentical hormones". Cleveland Clinic. 12 December 2012.
- ^ a b c d e f Conaway E (March 2011). "Bioidentical hormones: an evidence-based review for primary care providers". J Am Osteopath Assoc. 111 (3): 153–64. PMID 21464264.
- ^ a b c Cobin, RH; Goodman, NF; AACE Reproductive Endocrinology Scientific, Committee. (1 July 2017). "Position Statement on Menopause – 2017 Update" (PDF). Endocrine Practice. 23 (7): 869–880. doi:10.4158/EP171828.PS. PMID 28703650. Archived from the original (PDF) on 1 March 2019. Retrieved 1 March 2019.
- ^ a b "USPTF Consensus Statement". 2012. Archived from the original on 30 May 2013. Retrieved 14 May 2013.
- ^ Lewis, Ricki. "ACOG Revises Guidelines on Treating Menopause Symptoms". login.medscape.com. Medscape. Retrieved 4 March 2019.
- ^ "Hormone Therapy and Heart Disease – ACOG". www.acog.org. Committee on Gynecologic Practice. Retrieved 4 March 2019.
- ^ "Medscape". www.medscape.com.
- ^ a b c d Marjoribanks, Jane; Farquhar, Cindy; Roberts, Helen; Lethaby, Anne; Lee, Jasmine (17 January 2017). "Long-term hormone therapy for perimenopausal and postmenopausal women". The Cochrane Database of Systematic Reviews. 1 (1) CD004143. doi:10.1002/14651858.CD004143.pub5. ISSN 1469-493X. PMC 6465148. PMID 28093732.
- ^ "Menopause treatments". National Health Service, United Kingdom. 2019. Retrieved 23 February 2018.
- ^ Raine-Fenning NJ, Brincat MP, Muscat-Baron Y (2003). "Skin aging and menopause: implications for treatment". Am J Clin Dermatol. 4 (6): 371–8. doi:10.2165/00128071-200304060-00001. PMID 12762829. S2CID 20392538.
- ^ Zouboulis CC, Makrantonaki E (June 2012). "Hormonal therapy of intrinsic aging". Rejuvenation Res. 15 (3): 302–12. doi:10.1089/rej.2011.1249. PMID 22533363.
- ^ a b c d e f g Sarrel, P.M. (2000). Effects of hormone replacement therapy on sexual psychophysiology and behavior in postmenopause. Journal of Women's Health and Gender-Based Medicine, 9, 25–32
- ^ a b Gaffney, Theresa (3 December 2024). "There's an effective treatment for menopause symptoms. Why do so few women use it?". STAT. Retrieved 8 December 2024.
- ^ Writing Group for the Women's Health Initiative Investigators (17 July 2002). "Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women: Principal Results From the Women's Health Initiative Randomized Controlled Trial". JAMA: The Journal of the American Medical Association. 288 (3): 321–333. doi:10.1001/jama.288.3.321. PMID 12117397.
- ^ a b Chlebowski, Rowan T.; Anderson, Garnet L.; Aragaki, Aaron K.; Manson, JoAnn E.; Stefanick, Marcia L.; Pan, Kathy; Barrington, Wendy; Kuller, Lewis H.; Simon, Michael S.; Lane, Dorothy; Johnson, Karen C.; Rohan, Thomas E.; Gass, Margery L. S.; Cauley, Jane A.; Paskett, Electra D. (28 July 2020). "Association of Menopausal Hormone Therapy With Breast Cancer Incidence and Mortality During Long-term Follow-up of the Women's Health Initiative Randomized Clinical Trials". JAMA. 324 (4): 369–380. doi:10.1001/jama.2020.9482. ISSN 0098-7484. PMC 7388026. PMID 32721007.
- ^ Members, Menopause (4 September 2024). "Ongoing Individualized Hormone Therapy Appears to Have No Age Limit". The Menopause Society. Retrieved 8 December 2024.
- ^ Manson, JoAnn E.; Crandall, Carolyn J.; Rossouw, Jacques E.; Chlebowski, Rowan T.; Anderson, Garnet L.; Stefanick, Marcia L.; Aragaki, Aaron K.; Cauley, Jane A.; Wells, Gretchen L.; LaCroix, Andrea Z.; Thomson, Cynthia A.; Neuhouser, Marian L.; Van Horn, Linda; Kooperberg, Charles; Howard, Barbara V. (28 May 2024). "The Women's Health Initiative Randomized Trials and Clinical Practice: A Review". JAMA. 331 (20): 1748–1760. doi:10.1001/jama.2024.6542. ISSN 0098-7484. PMID 38691368.
- ^ Miller M.M.; Franklin K.B.J. (1999). "Theoretical basis for the benefit of postmenopausal estrogen substitution". Experimental Gerontology. 34 (5): 587–604. doi:10.1016/S0531-5565(99)00032-7. PMID 10530785. S2CID 43031351.
- ^ Gonzalez, M.; Viagara, G.; Caba, F.; Molina, E. (2004). "Sexual function, menopause and hormone replacement therapy (HRT)". The European Menopause Journal. 48 (4): 411–420. doi:10.1016/j.maturitas.2003.10.005. PMID 15283933.
- ^ a b c d Davis, SR; Baber, R; Panay, N; Bitzer, J; Perez, SC; Islam, RM; Kaunitz, AM; Kingsberg, SA; Lambrinoudaki, I; Liu, J; Parish, SJ; Pinkerton, J; Rymer, J; Simon, JA; Vignozzi, L; Wierman, ME (September 2019). "Global Consensus Position Statement on the Use of Testosterone Therapy for Women". The Journal of Sexual Medicine. 16 (9): 1331–1337. doi:10.1016/j.jsxm.2019.07.012. hdl:2158/1176450. PMID 31488288. S2CID 201845588. Archived from the original on 2 July 2022 – via INFN Open Access Repository.
- ^ Johansen, N; Lindén Hirschberg, A; Moen, MH (August 2020). "The role of testosterone in menopausal hormone treatment. What is the evidence?". Acta Obstetricia et Gynecologica Scandinavica. 99 (8): 966–969. doi:10.1111/aogs.13819. PMID 32027015. S2CID 211050248.
- ^ a b c d e Manson, JE; Chlebowski, RT; Stefanick, ML; Aragaki, AK; Rossouw, JE; Prentice, RL; Anderson, G; Howard, BV; Thomson, CA; LaCroix, AZ; Wactawski-Wende, J; Jackson, RD; Limacher, M; Margolis, KL; Wassertheil-Smoller, S; Beresford, SA; Cauley, JA; Eaton, CB; Gass, M; Hsia, J; Johnson, KC; Kooperberg, C; Kuller, LH; Lewis, CE; Liu, S; Martin, LW; Ockene, JK; O'Sullivan, MJ; Powell, LH; Simon, MS; Van Horn, L; Vitolins, MZ; Wallace, RB (2 October 2013). "Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women's Health Initiative randomized trials". JAMA. 310 (13): 1353–68. doi:10.1001/jama.2013.278040. PMC 3963523. PMID 24084921.
- ^ Zhu, L; Jiang, X; Sun, Y; Shu, W (April 2016). "Effect of hormone therapy on the risk of bone fractures: a systematic review and meta-analysis of randomized controlled trials". Menopause. 23 (4): 461–70. doi:10.1097/GME.0000000000000519. PMID 26529613. S2CID 26110755.
- ^ a b Studd J (March 2010). "Ten reasons to be happy about hormone replacement therapy: a guide for patients". Menopause Int. 16 (1): 44–6. doi:10.1258/mi.2010.010001. PMID 20424287. S2CID 33414205.
- ^ Tiidus, PM (August 2011). "Benefits of estrogen replacement for skeletal muscle mass and function in post-menopausal females: evidence from human and animal studies". The Eurasian Journal of Medicine. 43 (2): 109–14. doi:10.5152/eajm.2011.24. PMC 4261347. PMID 25610174.
- ^ a b c Shifren, JL; Davis, SR (August 2017). "Androgens in postmenopausal women: a review". Menopause. 24 (8): 970–979. doi:10.1097/GME.0000000000000903. PMID 28609390. S2CID 39876534.
- ^ Deleruyelle, LJ (2017). "Menopausal Symptom Relief and Side Effects Experienced by Women Using Compounded Bioidentical Hormone Replacement Therapy and Synthetic Conjugated Equine Estrogen and/or Progestin Hormone Replacement Therapy, Part 3". International Journal of Pharmaceutical Compounding. 21 (1): 6–16. PMID 28346192.
- ^ Suchowersky O, Muthipeedika J (December 2005). "A case of late-onset chorea". Nat Clin Pract Neurol. 1 (2): 113–6. doi:10.1038/ncpneuro0052. PMID 16932507. S2CID 11410333.
- ^ a b c d e Boardman, HM; Hartley, L; Eisinga, A; Main, C; Roqué i Figuls, M; Bonfill Cosp, X; Gabriel Sanchez, R; Knight, B (10 March 2015). "Hormone therapy for preventing cardiovascular disease in post-menopausal women". The Cochrane Database of Systematic Reviews. 2015 (3) CD002229. doi:10.1002/14651858.CD002229.pub4. hdl:20.500.12105/9999. ISSN 1469-493X. PMC 10183715. PMID 25754617. S2CID 22188456.
- ^ Hodis, HN; Mack, WJ; Henderson, VW; Shoupe, D; Budoff, MJ; Hwang-Levine, J; Li, Y; Feng, M; Dustin, L; Kono, N; Stanczyk, FZ; Selzer, RH; Azen, SP; ELITE Research, Group. (31 March 2016). "Vascular Effects of Early versus Late Postmenopausal Treatment with Estradiol". The New England Journal of Medicine. 374 (13): 1221–31. doi:10.1056/NEJMoa1505241. PMC 4921205. PMID 27028912.
- ^ Writing Group on Behalf of Workshop Consensus (October 2009). "Aging, menopause, cardiovascular disease and HRT. International Menopause Society Consensus Statement". Climacteric. 12 (5): 368–77. doi:10.1080/13697130903195606. PMID 19811229. S2CID 218865937.
- ^ "Committee Opinion No. 565: Hormone Therapy and Heart Disease". Obstetrics & Gynecology. 121 (6): 1407–1410. June 2013. doi:10.1097/01.AOG.0000431053.33593.2d. ISSN 0029-7844. PMID 23812486. S2CID 30775537.
- ^ Saeaib, N; Peeyananjarassri, K; Liabsuetrakul, T; Buhachat, R; Myriokefalitaki, E (28 January 2020). "Hormone replacement therapy after surgery for epithelial ovarian cancer". The Cochrane Database of Systematic Reviews. 1 (1) CD012559. doi:10.1002/14651858.CD012559.pub2. PMC 7027384. PMID 31989588.
- ^ Darabi, M.; Rabbani, M.; Ani, M.; Zarean, E.; Panjehpour, M.; Movahedian, A. (2011). "Increased leukocyte ABCA1 gene expression in post-menopausal women on hormone replacement therapy". Gynecological Endocrinology. 27 (9): 701–705. doi:10.3109/09513590.2010.507826. PMID 20807164. S2CID 203464.
- ^ Hodis, HN; Mack, WJ (1 May 2022). "Menopausal Hormone Replacement Therapy and Reduction of All-Cause Mortality and Cardiovascular Disease: It Is About Time and Timing". Cancer Journal (Sudbury, Mass.). 28 (3): 208–223. doi:10.1097/PPO.0000000000000591. PMC 9178928. PMID 35594469.
- ^ Gregersen, I; Høibraaten, E; Holven, KB; Løvdahl, L; Ueland, T; Mowinckel, MC; Dahl, TB; Aukrust, P; Halvorsen, B; Sandset, PM (December 2019). "Effect of hormone replacement therapy on atherogenic lipid profile in postmenopausal women". Thrombosis Research. 184: 1–7. doi:10.1016/j.thromres.2019.10.005. hdl:10852/75276. PMID 31677448.
- ^ Spoletini, I; Vitale, C; Pelliccia, F; Fossati, C; Rosano, GM (December 2014). "Androgens and cardiovascular disease in postmenopausal women: a systematic review". Climacteric. 17 (6): 625–34. doi:10.3109/13697137.2014.887669. PMID 24559253. S2CID 33413274.
- ^ a b Scarabin, P.-Y. (August 2018). "Progestogens and venous thromboembolism in menopausal women: an updated oral versus transdermal estrogen meta-analysis". Climacteric. 21 (4): 341–345. doi:10.1080/13697137.2018.1446931. ISSN 1473-0804. PMID 29570359. S2CID 4229701.
- ^ Olié, V. R.; Canonico, M.; Scarabin, P. Y. (2010). "Risk of venous thrombosis with oral versus transdermal estrogen therapy among postmenopausal women". Current Opinion in Hematology. 17 (5): 457–463. doi:10.1097/MOH.0b013e32833c07bc. PMID 20601871. S2CID 205827003.
- ^ Rott, H (2014). "Prevention and treatment of venous thromboembolism during HRT: current perspectives". International Journal of General Medicine. 7: 433–40. doi:10.2147/IJGM.S46310. PMC 4155999. PMID 25210472.
- ^ a b Carrasquilla GD, Frumento P, Berglund A, Borgfeldt C, Bottai M, Chiavenna C, Eliasson M, Engström G, Hallmans G, Jansson JH, Magnusson PK, Nilsson PM, Pedersen NL, Wolk A, Leander K (November 2017). "Postmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies". PLOS Med. 14 (11) e1002445. doi:10.1371/journal.pmed.1002445. PMC 5693286. PMID 29149179.
- ^ Chlebowski, RT; Anderson, GL; Sarto, GE; Haque, R; Runowicz, CD; Aragaki, AK; Thomson, CA; Howard, BV; Wactawski-Wende, J; Chen, C; Rohan, TE; Simon, MS; Reed, SD; Manson, JE (March 2016). "Continuous Combined Estrogen Plus Progestin and Endometrial Cancer: The Women's Health Initiative Randomized Trial". Journal of the National Cancer Institute. 108 (3) djv350. doi:10.1093/jnci/djv350. PMC 5072373. PMID 26668177.
- ^ Archer, DF (2001). "The effect of the duration of progestin use on the occurrence of endometrial cancer in postmenopausal women". Menopause. 8 (4): 245–51. doi:10.1097/00042192-200107000-00005. PMID 11449081. S2CID 38526018.
- ^ a b c Kim, JJ; Kurita, T; Bulun, SE (February 2013). "Progesterone action in endometrial cancer, endometriosis, uterine fibroids, and breast cancer". Endocrine Reviews. 34 (1): 130–62. doi:10.1210/er.2012-1043. PMC 3565104. PMID 23303565.
- ^ Young, Robert; Arlan F., Jr Fuller; Fuller, Arlan F.; Michael V. Seiden (2004). Uterine cancer. Hamilton, Ont: B.C. Decker. ISBN 978-1-55009-163-2.
- ^ Zang, H; Sahlin, L; Masironi, B; Eriksson, E; Lindén Hirschberg, A (June 2007). "Effects of testosterone treatment on endometrial proliferation in postmenopausal women". The Journal of Clinical Endocrinology and Metabolism. 92 (6): 2169–75. doi:10.1210/jc.2006-2171. PMID 17341565.
- ^ "Endometrial cancer risk was lower in women who used continuous combined HRT than in non-users". Evidence-based Obstetrics & Gynecology. 8 (1–2): 68–69. March 2006. doi:10.1016/j.ebobgyn.2006.01.011. ISSN 1361-259X.
- ^ Collaborative Group on Hormonal Factors in Breast Cancer (September 2019). "Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence". Lancet. 394 (10204): 1159–1168. doi:10.1016/S0140-6736(19)31709-X. PMC 6891893. PMID 31474332.
- ^ a b c "Risk of breast cancer with HRT depends on therapy type and duration". NIHR Evidence. National Institute for Health and Care Research. 20 December 2021. doi:10.3310/alert_48575.
- ^ a b Vinogradova Y, Coupland C, Hippisley-Cox J (October 2020). "Use of hormone replacement therapy and risk of breast cancer: nested case-control studies using the QResearch and CPRD databases". BMJ. 371 m3873. doi:10.1136/bmj.m3873. PMC 7592147. PMID 33115755.
- ^ Vinogradova, Yana; Coupland, Carol; Hippisley-Cox, Julia (28 October 2020). "Use of hormone replacement therapy and risk of breast cancer: nested case-control studies using the QResearch and CPRD databases". BMJ. 371 m3873. doi:10.1136/bmj.m3873. ISSN 1756-1833. PMC 7592147. PMID 33115755.
- ^ Fournier, A. S.; Berrino, F.; Clavel-Chapelon, F. O. (2007). "Unequal risks for breast cancer associated with different hormone replacement therapies: Results from the E3N cohort study". Breast Cancer Research and Treatment. 107 (1): 103–111. doi:10.1007/s10549-007-9523-x. PMC 2211383. PMID 17333341.
- ^ Zeng, Z; Jiang, X; Li, X; Wells, A; Luo, Y; Neapolitan, R (2018). "Conjugated equine estrogen and medroxyprogesterone acetate are associated with decreased risk of breast cancer relative to bioidentical hormone therapy and controls". PLOS ONE. 13 (5) e0197064. Bibcode:2018PLoSO..1397064Z. doi:10.1371/journal.pone.0197064. PMC 5955567. PMID 29768475.
- ^ Beral, V; Reeves, G; Bull, D; Green, J (16 February 2011). "Breast cancer risk in relation to the interval between menopause and starting hormone therapy". Journal of the National Cancer Institute. 103 (4): 296–305. doi:10.1093/jnci/djq527. PMC 3039726. PMID 21278356.
- ^ Letendre, I.; Lopes, P. (2012). "Ménopause et risques carcinologiques". Journal de Gynécologie Obstétrique et Biologie de la Reproduction. 41 (7): F33 – F37. doi:10.1016/j.jgyn.2012.09.006. PMID 23062839.
- ^ Anderson, G. L.; Limacher, M.; Assaf, A. R.; Bassford, T.; Beresford, S. A.; Black, H.; Bonds, D.; Brunner, R.; Brzyski, R.; Caan, B.; Chlebowski, R.; Curb, D.; Gass, M.; Hays, J.; Heiss, G.; Hendrix, S.; Howard, B. V.; Hsia, J.; Hubbell, A.; Jackson, R.; Johnson, K. C.; Judd, H.; Kotchen, J. M.; Kuller, L.; Lacroix, A. Z.; Lane, D.; Langer, R. D.; Lasser, N.; Lewis, C. E.; Manson, J. (2004). "Effects of Conjugated Equine Estrogen in Postmenopausal Women with Hysterectomy: The Women's Health Initiative Randomized Controlled Trial". JAMA: The Journal of the American Medical Association. 291 (14): 1701–1712. doi:10.1001/jama.291.14.1701. PMID 15082697.
- ^ Stefanick ML; Anderson GL; Margolis KL; et al. (2006). "Effects of conjugated equine estrogens on breast cancer and mammography screening in postmenopausal women with hysterectomy". JAMA. 295 (14): 1647–57. doi:10.1001/jama.295.14.1647. PMID 16609086.
- ^ "Association between hormone replacement therapy use and breast cancer risk varies by race/ethnicity, body mass index, and breast density". JNCI Journal of the National Cancer Institute. 105 (18). 2013. doi:10.1093/jnci/djt264. ISSN 0027-8874.
- In turn citing: Hou, N.; Hong, S.; Wang, W.; Olopade, O. I.; Dignam, J. J.; Huo, D. (2013). "Hormone Replacement Therapy and Breast Cancer: Heterogeneous Risks by Race, Weight, and Breast Density". JNCI Journal of the National Cancer Institute. 105 (18): 1365–1372. doi:10.1093/jnci/djt207. ISSN 0027-8874. PMC 3776262. PMID 24003037.
- ^ Kuhl, H.; Schneider, H. P. G. (2013). "Progesterone – promoter or inhibitor of breast cancer". Climacteric. 16 (Suppl 1): 54–68. doi:10.3109/13697137.2013.768806. PMID 23336704. S2CID 20808536.
- ^ Azam, S; Lange, T; Huynh, S; Aro, AR; von Euler-Chelpin, M; Vejborg, I; Tjønneland, A; Lynge, E; Andersen, ZJ (June 2018). "Hormone replacement therapy, mammographic density, and breast cancer risk: a cohort study". Cancer Causes & Control. 29 (6): 495–505. doi:10.1007/s10552-018-1033-0. PMC 5938298. PMID 29671181.
- ^ Stute, P; Wildt, L; Neulen, J (April 2018). "The impact of micronized progesterone on breast cancer risk: a systematic review". Climacteric. 21 (2): 111–122. doi:10.1080/13697137.2017.1421925. PMID 29384406. S2CID 3642971.
- ^ Management of the menopause after breast cancer Archived 7 April 2016 at archive.today, from The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. College Statement C-Gyn 15. 1st Endorsed: February 2003. Current: November 2011. Review: November 2014
- ^ Gordhandas, S; Norquist, BM; Pennington, KP; Yung, RL; Laya, MB; Swisher, EM (April 2019). "Hormone replacement therapy after risk reducing salpingo-oophorectomy in patients with BRCA1 or BRCA2 mutations; a systematic review of risks and benefits". Gynecologic Oncology. 153 (1): 192–200. doi:10.1016/j.ygyno.2018.12.014. PMID 30661763. S2CID 58593390.
- ^ Heinig, M; Schwarz, S; Haug, U (16 February 2021). "Self-selection for mammography screening according to use of hormone replacement therapy: A systematic literature review". Cancer Epidemiology. 71 (Pt A) 101812. doi:10.1016/j.canep.2020.101812. PMID 33608235. S2CID 231970420.
- ^ Kotsopoulos, J; Narod, SA (January 2012). "Androgens and breast cancer". Steroids. 77 (1–2): 1–9. doi:10.1016/j.steroids.2011.10.002. PMID 22015396. S2CID 32022318.
- ^ Collaborative Group on Epidemiological Studies of Ovarian Cancer (12 February 2015). "Menopausal hormone use and ovarian cancer risk: individual participant meta-analysis of 52 epidemiological studies". The Lancet. 385 (9980): 1835–1842. doi:10.1016/S0140-6736(14)61687-1. PMC 4427760. PMID 25684585.
- ^ a b c Shi, LF; Wu, Y; Li, CY (April 2016). "Hormone therapy and risk of ovarian cancer in postmenopausal women: a systematic review and meta-analysis". Menopause. 23 (4): 417–24. doi:10.1097/GME.0000000000000550. PMID 26506499. S2CID 32195397.
- ^ Guidozzi, F (December 2013). "Estrogen therapy in gynecological cancer survivors". Climacteric. 16 (6): 611–7. doi:10.3109/13697137.2013.806471. PMID 23952524. S2CID 38122562.
- ^ "Menopausal Hormone Therapy and Cancer Risk". www.cancer.org. Retrieved 4 March 2019.
- ^ Jang, YC; Huang, HL; Leung, CY (9 December 2019). "Association of hormone replacement therapy with mortality in colorectal cancer survivor: a systematic review and meta-analysis". BMC Cancer. 19 (1): 1199. doi:10.1186/s12885-019-6428-0. PMC 6902524. PMID 31818262.
- ^ Vargiu, V; Amar, ID; Rosati, A; Dinoi, G; Turco, LC; Capozzi, VA; Scambia, G; Villa, P (25 November 2020). "Hormone replacement therapy and cervical cancer: a systematic review of the literature". Climacteric. 24 (2): 120–127. doi:10.1080/13697137.2020.1826426. PMID 33236658. S2CID 227166430.
- ^ Appleman, Maria-Luisa; Thomas, Jeremy L.; Weiss, Alison R.; Nilaver, Benjamin I.; Cervera-Juanes, Rita; Kohama, Steven G.; Urbanski, Henryk F. (2023). "Effect of hormone replacement therapy on amyloid beta (Aβ) plaque density in the rhesus macaque amygdala". Frontiers in Aging Neuroscience. 15 1326747. doi:10.3389/fnagi.2023.1326747. ISSN 1663-4365. PMC 10808750. PMID 38274989.
- ^ a b "Hormone therapy for brain performance: No effect, whether started early or late". www.sciencedaily.com. 20 July 2016. Retrieved 23 April 2025.
- ^ a b Dye, RV; Miller, KJ; Singer, EJ; Levine, AJ (2012). "Hormone replacement therapy and risk for neurodegenerative diseases". International Journal of Alzheimer's Disease. 2012 258454. doi:10.1155/2012/258454. PMC 3324889. PMID 22548198.
- ^ Nicoletti, A; Nicoletti, G; Arabia, G; Annesi, G; De Mari, M; Lamberti, P; Grasso, L; Marconi, R; Epifanio, A; Morgante, L; Cozzolino, A; Barone, P; Quattrone, A; Zappia, M (December 2011). "Reproductive factors and Parkinson's disease: a multicenter case-control study". Movement Disorders. 26 (14): 2563–6. doi:10.1002/mds.23951. PMID 21956541. S2CID 40143658.
- ^ Noyce, AJ; Bestwick, JP; Silveira-Moriyama, L; Hawkes, CH; Giovannoni, G; Lees, AJ; Schrag, A (December 2012). "Meta-analysis of early nonmotor features and risk factors for Parkinson disease". Annals of Neurology. 72 (6): 893–901. doi:10.1002/ana.23687. PMC 3556649. PMID 23071076.
- ^ Wang, P; Li, J; Qiu, S; Wen, H; Du, J (2015). "Hormone replacement therapy and Parkinson's disease risk in women: a meta-analysis of 14 observational studies". Neuropsychiatric Disease and Treatment. 11: 59–66. doi:10.2147/NDT.S69918. PMC 4317144. PMID 25657580.
- ^ Rugbjerg, K; Christensen, J; Tjønneland, A; Olsen, JH (April 2013). "Exposure to estrogen and women's risk for Parkinson's disease: a prospective cohort study in Denmark". Parkinsonism & Related Disorders. 19 (4): 457–60. doi:10.1016/j.parkreldis.2013.01.008. PMID 23402992.
- ^ Yoon, BK; Chin, J; Kim, JW; Shin, MH; Ahn, S; Lee, DY; Seo, SW; Na, DL (August 2018). "Menopausal hormone therapy and mild cognitive impairment: a randomized, placebo-controlled trial". Menopause. 25 (8): 870–876. doi:10.1097/GME.0000000000001140. PMID 29846283. S2CID 44174553.
- ^ Rasgon, NL; Geist, CL; Kenna, HA; Wroolie, TE; Williams, KE; Silverman, DH (2014). "Prospective randomized trial to assess effects of continuing hormone therapy on cerebral function in postmenopausal women at risk for dementia". PLOS ONE. 9 (3) e89095. Bibcode:2014PLoSO...989095R. doi:10.1371/journal.pone.0089095. PMC 3951184. PMID 24622517.
- ^ Schmidt R, Fazekas F, Reinhart B, Kapeller P, Fazekas G, Offenbacher H, Eber B, Schumacher M, Freidl W (November 1996). "Estrogen replacement therapy in older women: a neuropsychological and brain MRI study". Journal of the American Geriatrics Society. 44 (11): 1307–13. doi:10.1111/j.1532-5415.1996.tb01400.x. PMID 8909345. S2CID 22921797.
- ^ Parkinson Study Group POETRY, Investigators. (December 2011). "A randomized pilot trial of estrogen replacement therapy in post-menopausal women with Parkinson's disease". Parkinsonism & Related Disorders. 17 (10): 757–60. doi:10.1016/j.parkreldis.2011.07.007. PMID 21824799.
- ^ Diamanti-Kandarakis, E; Dattilo, M; Macut, D; Duntas, L; Gonos, ES; Goulis, DG; Gantenbein, CK; Kapetanou, M; Koukkou, E; Lambrinoudaki, I; Michalaki, M; Eftekhari-Nader, S; Pasquali, R; Peppa, M; Tzanela, M; Vassilatou, E; Vryonidou, A (June 2017). "Mechanisms in Endocrinology: Aging and anti-aging: a Combo-Endocrinology overview". European Journal of Endocrinology. 176 (6): R283 – R308. doi:10.1530/EJE-16-1061. PMID 28264815.
- ^ Vest, RS; Pike, CJ (February 2013). "Gender, sex steroid hormones, and Alzheimer's disease". Hormones and Behavior. 63 (2): 301–7. doi:10.1016/j.yhbeh.2012.04.006. PMC 3413783. PMID 22554955.
- ^ Pike, CJ; Carroll, JC; Rosario, ER; Barron, AM (July 2009). "Protective actions of sex steroid hormones in Alzheimer's disease". Frontiers in Neuroendocrinology. 30 (2): 239–58. doi:10.1016/j.yfrne.2009.04.015. PMC 2728624. PMID 19427328.
- ^ MacLennan, AH (August 2011). "HRT in difficult circumstances: are there any absolute contraindications?". Climacteric. 14 (4): 409–17. doi:10.3109/13697137.2010.543496. PMID 21355685. S2CID 25426141.
- ^ a b c d e f g h i j Fugh-Berman, Adriane (2015). "The Science of Marketing: How Pharmaceutical Companies Manipulated Medical Discourse on Menopause". Women's Reproductive Health. 2 (1): 18–23. doi:10.1080/23293691.2015.1039448. ISSN 2329-3691.
- ^ IARC Working Group on the Evaluation of Carcinogenic Risks to Humans; World Health Organization; International Agency for Research on Cancer (2007). Combined Estrogen-progestogen Contraceptives and Combined Estrogen-progestogen Menopausal Therapy. World Health Organization. pp. 205–. ISBN 978-92-832-1291-1.
- ^ a b c Writing Group for the Women's Health Initiative Investigators (2002). "Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women: Principal Results From the Women's Health Initiative Randomized Controlled Trial". JAMA. 288 (3): 321–333. doi:10.1001/jama.288.3.321. PMID 12117397.
- ^ Chlebowski RT, Kuller LH, Prentice RL, Stefanick ML, Manson JE, Gass M, et al. (February 2009). "Breast cancer after use of estrogen plus progestin in postmenopausal women". The New England Journal of Medicine. 360 (6): 573–87. doi:10.1056/NEJMoa0807684. PMC 3963492. PMID 19196674.
- ^ Kreatsoulas, C.; Anand, S. S. (2013). "Menopausal hormone therapy for the primary prevention of chronic conditions. U.S. Preventive Services Task Force Recommendation Statement" (PDF). Polskie Archiwum Medycyny Wewnetrznej. 123 (3): 112–117. PMID 23396275.
- ^ Nelson, H. D.; Walker, M.; Zakher, B.; Mitchell, J. (2012). "Menopausal hormone therapy for the primary prevention of chronic conditions: A systematic review to update the U.S. Preventive Services Task Force recommendations". Annals of Internal Medicine. 157 (2): 104–113. doi:10.7326/0003-4819-157-2-201207170-00466. PMID 22786830.
- ^ George, James L.; Colman, Robert W.; Goldhaber, Samuel Z.; Victor J. Marder (2006). Hemostasis and thrombosis: basic principles and clinical practice. Hagerstown, MD: Lippincott Williams & Wilkins. pp. 1239. ISBN 978-0-7817-4996-1.
- ^ Darabi M, Ani M, Panjehpour M, Rabbani M, Movahedian A, Zarean E (2011). "Effect of estrogen receptor β A1730G polymorphism on ABCA1 gene expression response to postmenopausal hormone replacement therapy". Genetic Testing and Molecular Biomarkers. 15 (1–2): 11–5. doi:10.1089/gtmb.2010.0106. PMID 21117950.
- ^ Chlebowski, R. T.; Anderson, G. L. (2015). "Menopausal hormone therapy and breast cancer mortality: clinical implications". Therapeutic Advances in Drug Safety. 6 (2): 45–56. doi:10.1177/2042098614568300. ISSN 2042-0986. PMC 4406918. PMID 25922653.
- ^ Mazzucco AE, Santoro E, DeSoto M, Lee JH (December 2010). "Hormone Therapy and Menopause". National Research Center for Women and Families.
- ^ Gina Kolata (19 April 2007). "Sharp Drop in Rates of Breast Cancer Holds". New York Times.
- ^ Roni Caryn Rabin (28 August 2007). "For a Low-Dose Hormone, Take Your Pick". New York Times.
Many women seeking natural remedies have turned to compounding pharmacies, which use bioidentical hormones that are chemically synthesized but with the same molecular structure as hormones produced by a woman's body.
- ^ John Gever (5 April 2011). "New WHI Estrogen Analysis Shows Lower Breast Ca Risk". MedPageToday.
- ^ Salpeter, S. R.; Cheng, J.; Thabane, L.; Buckley, N. S.; Salpeter, E. E. (2009). "Bayesian Meta-analysis of Hormone Therapy and Mortality in Younger Postmenopausal Women". The American Journal of Medicine. 122 (11): 1016–1022.e1. doi:10.1016/j.amjmed.2009.05.021. PMID 19854329.
- ^ Anderson, G. L.; Chlebowski, R. T.; Rossouw, J. E.; Rodabough, R. J.; McTiernan, A.; Margolis, K. L.; Aggerwal, A.; David Curb, J. D.; Hendrix, S. L.; Allan Hubbell, F. A.; Khandekar, J.; Lane, D. S.; Lasser, N.; Lopez, A. M.; Potter, J.; Ritenbaugh, C. (2006). "Prior hormone therapy and breast cancer risk in the Women's Health Initiative randomized trial of estrogen plus progestin". Maturitas. 55 (2): 103–115. doi:10.1016/j.maturitas.2006.05.004. PMID 16815651.
- ^ Hulley, S.; Grady, D.; Bush, T.; Furberg, C.; Herrington, D.; Riggs, B.; Vittinghoff, E. (1998). "Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group". JAMA: The Journal of the American Medical Association. 280 (7): 605–613. doi:10.1001/jama.280.7.605. PMID 9718051.
- ^ Salpeter, S. R.; Walsh, J. M. E.; Greyber, E.; Ormiston, T. M.; Salpeter, E. E. (2004). "Mortality associated with hormone replacement therapy in younger and older women". Journal of General Internal Medicine. 19 (7): 791–804. doi:10.1111/j.1525-1497.2004.30281.x. PMC 1492478. PMID 15209595.
- ^ Grodstein, F.; Stampfer, M. J.; Colditz, G. A.; Willett, W. C.; Manson, J. E.; Joffe, M.; Rosner, B.; Fuchs, C.; Hankinson, S. E.; Hunter, D. J.; Hennekens, C. H.; Speizer, F. E. (1997). "Postmenopausal Hormone Therapy and Mortality". New England Journal of Medicine. 336 (25): 1769–1775. doi:10.1056/NEJM199706193362501. PMID 9187066.
- ^ Bethea CL (February 2011). "MPA: Medroxy-Progesterone Acetate Contributes to Much Poor Advice for Women". Endocrinology. 152 (2): 343–345. doi:10.1210/en.2010-1376. PMC 3037166. PMID 21252179.
- ^ Harman SM, Brinton EA, Cedars M, Lobo R, Manson JE, Merriam GR, Miller VM, Naftolin F, Santoro N (March 2005). "KEEPS: The Kronos Early Estrogen Prevention Study". Climacteric. 8 (1): 3–12. doi:10.1080/13697130500042417. PMID 15804727. S2CID 37219662.
- ^ Dominus, Susan (1 February 2023). "Women Have Been Misled About Menopause". The New York Times. ISSN 0362-4331. Retrieved 7 February 2023.
No research has yet followed women who start in their 50s and stay on continuously into their 60s.
- ^ Morley JE, Perry HM (May 2003). "Androgens and women at the menopause and beyond". J. Gerontol. A Biol. Sci. Med. Sci. 58 (5): M409–16. doi:10.1093/gerona/58.5.M409. PMID 12730248.
- ^ Garefalakis M, Hickey M (2008). "Role of androgens, progestins and tibolone in the treatment of menopausal symptoms: a review of the clinical evidence". Clin Interv Aging. 3 (1): 1–8. doi:10.2147/CIA.S1043. PMC 2544356. PMID 18488873.
- ^ Formoso, G; Perrone, E; Maltoni, S; Balduzzi, S; Wilkinson, J; Basevi, V; Marata, AM; Magrini, N; D'Amico, R; Bassi, C; Maestri, E (12 October 2016). "Short-term and long-term effects of tibolone in postmenopausal women". The Cochrane Database of Systematic Reviews. 10 (10) CD008536. doi:10.1002/14651858.CD008536.pub3. ISSN 1469-493X. PMC 6458045. PMID 27733017.
- ^ Cummings, SR; Ettinger, B; Delmas, PD; Kenemans, P; Stathopoulos, V; Verweij, P; Mol-Arts, M; Kloosterboer, L; Mosca, L; Christiansen, C; Bilezikian, J; Kerzberg, EM; Johnson, S; Zanchetta, J; Grobbee, DE; Seifert, W; Eastell, R; LIFT Trial, Investigators. (14 August 2008). "The effects of tibolone in older postmenopausal women". The New England Journal of Medicine. 359 (7): 697–708. doi:10.1056/NEJMoa0800743. PMC 3684062. PMID 18703472.
- ^ Estrogen (Vaginal Route) from Mayo Clinic / Thomson Healthcare Inc. Portions of this document last updated: 1 November 2011
- ^ Somboonporn, W; Davis, S; Seif, MW; Bell, R (19 October 2005). "Testosterone for peri- and postmenopausal women". The Cochrane Database of Systematic Reviews (4) CD004509. doi:10.1002/14651858.CD004509.pub2. PMID 16235365. S2CID 21619940.
- ^ North American Menopause, Society. (2005). "The role of testosterone therapy in postmenopausal women: position statement of The North American Menopause Society". Menopause. 12 (5): 496–511, quiz 649. doi:10.1097/01.gme.0000177709.65944.b0. PMID 16145303. S2CID 5122078.
- ^ Drapier-Faure, E; Azoulay, C; Abramovici, Y (July 2005). "[Acceptability of continuous combined versus cyclical HRT: a French multicentric randomized clinical study]". Gynécologie, obstétrique & fertilité. 33 (7–8): 498–504. doi:10.1016/j.gyobfe.2005.04.024. PMID 16005674.
- ^ Feeley, KM; Wells, M (June 2001). "Hormone replacement therapy and the endometrium". Journal of Clinical Pathology. 54 (6): 435–40. doi:10.1136/jcp.54.6.435. PMC 1731456. PMID 11376015.
- ^ Junkermann, H; von Holst, T; Lang, E; Rakov, V (14 February 2005). "Influence of different HRT regimens on mammographic density". Maturitas. 50 (2): 105–10. doi:10.1016/j.maturitas.2004.04.008. PMID 15653007.
- ^ a b Beck, KL; Anderson, MC; Kirk, JK (August 2017). "Transdermal estrogens in the changing landscape of hormone replacement therapy". Postgraduate Medicine. 129 (6): 632–636. doi:10.1080/00325481.2017.1334507. PMID 28540770. S2CID 205452835.
- ^ a b c d e f g Yoo JW, Lee CH (May 2006). "Drug delivery systems for hormone therapy". J Control Release. 112 (1): 1–14. doi:10.1016/j.jconrel.2006.01.021. PMID 16530874.
- ^ a b c d Kuhl H (August 2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric. 8 (Suppl 1): 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- ^ Martin, K. A.; Barbieri, R. L.; Crowley, W. F. Jr. (24 September 2021). "Preparations for menopausal hormone therapy". UpToDate. Retrieved 2 February 2022.
Not recommended. Depot estrogen—Estrogen is also available in some, but not all, countries as long-acting (three to four weeks) injections of either estradiol cypionate or estradiol valerate. Given the other effective estrogen options, we do not use this approach (table 1).
- ^ Unfer V, Casini ML, Marelli G, Costabile L, Gerli S, Di Renzo GC (August 2005). "Different routes of progesterone administration and polycystic ovary syndrome: a review of the literature". Gynecol Endocrinol. 21 (2): 119–27. doi:10.1080/09513590500170049. PMID 16109599. S2CID 24890723.
- ^ a b "FDA Takes Action Against Compounded Menopause Hormone Therapy Drugs". FDA. 9 January 2008. Archived from the original on 14 June 2009. Retrieved 17 February 2009.
- ^ Panay, N; Medical Advisory Council of the British Menopause, Society. (June 2019). "BMS – Consensus statement: Bioidentical HRT". Post Reproductive Health. 25 (2): 61–63. doi:10.1177/2053369119841844. PMID 31192760. S2CID 189816648.
- ^ Cirigliano, M (June 2007). "Bioidentical hormone therapy: a review of the evidence". Journal of Women's Health. 16 (5): 600–31. doi:10.1089/jwh.2006.0311. PMID 17627398.
- ^ Simon JA (July 2014). "What if the Women's Health Initiative had used transdermal estradiol and oral progesterone instead?". Menopause. 21 (7): 769–83. doi:10.1097/GME.0000000000000169. PMID 24398406. S2CID 30292136.
- ^ a b Pinkerton, JV; Pickar, JH (February 2016). "Update on medical and regulatory issues pertaining to compounded and FDA-approved drugs, including hormone therapy". Menopause. 23 (2): 215–23. doi:10.1097/GME.0000000000000523. PMC 4927324. PMID 26418479.
- ^ a b c d Singer, Natasha (4 August 2009). "Medical Papers by Ghostwriters Pushed Therapy". The New York Times. Retrieved 13 July 2018.
- ^ a b c d e f Fugh-Berman AJ (September 2010). "The haunting of medical journals: how ghostwriting sold "HRT"". PLOS Med. 7 (9) e1000335. doi:10.1371/journal.pmed.1000335. PMC 2935455. PMID 20838656.
- ^ a b c d e f g Steve Kent May; Steve May (20 January 2012). Case Studies in Organizational Communication: Ethical Perspectives and Practices: Ethical Perspectives and Practices. SAGE. pp. 197–. ISBN 978-1-4129-8309-9.
- ^ a b Miller VM, Harman SM (November 2017). "An update on hormone therapy in postmenopausal women: mini-review for the basic scientist". Am. J. Physiol. Heart Circ. Physiol. 313 (5): H1013 – H1021. doi:10.1152/ajpheart.00383.2017. PMC 5792205. PMID 28801526.
- ^ Sorkin, Andrew Ross; Wilson, Duff (25 January 2009). "Pfizer Agrees to Pay $68 Billion for Rival Drug Maker Wyeth". The New York Times.
- ^ "Pfizer Sizes Up: Closes $68B Wyeth Deal". CNBC. 19 October 2009.
- ^ Tao M, Teng Y, Shao H, Wu P, Mills EJ (2011). "Knowledge, perceptions and information about hormone therapy (HT) among menopausal women: a systematic review and meta-synthesis". PLOS ONE. 6 (9) e24661. Bibcode:2011PLoSO...624661T. doi:10.1371/journal.pone.0024661. PMC 3174976. PMID 21949743.
- ^ Davies, M; Hamoda, H; British Menopause Society Medical Advisory, Council. (11 February 2019). "Hormone replacement therapy: changes in prescribing practice". BMJ (Clinical Research Ed.). 364: l633. doi:10.1136/bmj.l633. PMID 30745316. S2CID 73435897.
External links
[edit]- Menopause treatment, Hormone Health Network, The Endocrine Society
- Sexual Health and Menopause Online, The North American Menopause Society
- Menopause, US Food and Drug Administration
- British Menopause Society
Hormone replacement therapy
View on GrokipediaOverview
Definition and Primary Contexts
Hormone replacement therapy (HRT) consists of the exogenous administration of one or more hormones to restore or supplement levels diminished by physiological processes such as aging, surgical removal of hormone-producing organs, or pathological conditions like hypogonadism.[1] This approach aims to mitigate symptoms arising from hormonal deficiencies, including vasomotor instability, genitourinary changes, mood alterations, and metabolic alterations, by mimicking the endocrine milieu of reproductive years. In clinical practice, HRT formulations typically include estrogens, progestogens, or androgens, selected based on the deficient hormone and patient-specific factors such as reproductive status and contraindications.[12] The primary context for HRT application is the menopausal transition in women, where ovarian follicle depletion leads to a precipitous decline in estrogen and progesterone production, occurring on average around age 51.[2] Systemic HRT in this setting typically involves estrogen, with progestogen added if the uterus is intact to prevent endometrial hyperplasia, and predominantly targets symptoms such as hot flashes (experienced by 75-85% of women), mood swings, sleep disturbances, reduced libido, and accelerated bone loss due to hypoestrogenism.[13][14][15] This phase, encompassing perimenopause and postmenopause, affects approximately 1.1 billion women globally by 2025. HRT does not delay menopause in perimenopausal women who are still ovulating; it relieves symptoms such as hot flashes, irregular periods, and vaginal dryness by supplementing declining hormones, but it does not slow ovarian aging, prevent follicle depletion, or postpone the natural cessation of ovulation and menstruation that defines menopause. Menopause occurs when ovaries stop functioning regardless of HRT use; HRT may mask symptoms or induce withdrawal bleeding but does not alter the underlying biological timeline.[2] HRT with estrogen alone is used for hysterectomized women, while combined estrogen-progestogen regimens are employed otherwise to counteract endometrial proliferation risks.[1] A secondary but established context involves hypogonadism, defined as inadequate gonadal steroidogenesis resulting in subphysiological sex hormone levels, which can be primary (gonadal failure) or secondary (pituitary/hypothalamic dysfunction).[16] In women with premature ovarian insufficiency—diagnosed when amenorrhea precedes age 40—HRT with estrogen and progestogen is recommended until at least the typical menopausal age to prevent long-term sequelae like cardiovascular disease and osteoporosis.[17] For men, testosterone replacement—often encompassed under broader HRT terminology—addresses late-onset hypogonadism, characterized by serum testosterone below 300 ng/dL and symptoms including reduced muscle mass, erectile dysfunction, and mood disorders, with prevalence rising to 30-50% in men over 70.[1] These contexts underscore HRT's role in endocrine restoration, though applications remain tailored to verified deficiencies confirmed via laboratory assays and clinical evaluation.[18]Hormonal Mechanisms Involved
Hormone replacement therapy (HRT) supplies exogenous sex steroids to mimic endogenous hormone production disrupted by ovarian failure in menopause or testicular insufficiency in hypogonadism. Estrogens, the primary component in menopausal HRT, diffuse across cell membranes and bind intracellular estrogen receptors α (ERα) and β (ERβ), which are ligand-activated transcription factors. Upon binding, estrogen-receptor complexes dimerize, translocate to the nucleus, and recruit coactivators to estrogen response elements on DNA, thereby upregulating or downregulating target genes involved in cell proliferation, vascular endothelial function, bone remodeling, and neuroprotection.[19] Non-genomic rapid signaling via membrane-associated ERs also contributes, modulating ion channels and kinase pathways for effects like vasodilation.[19] Progestogens, often combined with estrogens in women with intact uteri, bind progesterone receptors (PR-A and PR-B isoforms) to oppose unopposed estrogen's mitogenic effects on the endometrium. Progesterone-receptor binding induces conformational changes, facilitating co-regulator recruitment and transcriptional repression of proliferative genes while promoting secretory differentiation and apoptosis in endometrial cells, thus reducing hyperplasia risk.[1] Progestogens further influence hypothalamic-pituitary-ovarian feedback and may exert neuroprotective effects via allopregnanolone metabolites interacting with GABA_A receptors.[20] In male hypogonadism, testosterone replacement acts predominantly through the androgen receptor (AR), a nuclear receptor that, upon testosterone or dihydrotestosterone binding, dimerizes and binds androgen response elements to enhance transcription of genes promoting spermatogenesis, erythropoiesis, muscle hypertrophy via IGF-1 signaling, and bone formation by osteoblasts.[21] Conversion to estradiol via aromatase provides additional estrogenic benefits, while 5α-reduction to dihydrotestosterone amplifies androgenic actions in prostate and skin.[22] These mechanisms collectively restore physiological homeostasis, though tissue-specific responses vary due to receptor density and cofactor availability.[19]Medical Uses
Menopausal Symptom Relief
Hormone replacement therapy (HRT), primarily involving estrogen with or without progestogen, serves as the most effective pharmacological intervention for alleviating vasomotor symptoms (VMS) of menopause, including hot flashes and night sweats, which affect over 80% of menopausal women.[23] Randomized controlled trials and meta-analyses demonstrate that systemic estrogen therapy reduces VMS frequency by approximately 75% with standard doses and 65% with low doses, outperforming non-hormonal alternatives like SSRIs or SNRIs.[24] Beyond VMS, systemic HRT improves mood symptoms such as swings and depressive symptoms in menopausal women, with prospective studies linking vasomotor symptom relief to mood enhancements.[14] It may also enhance libido in a significant proportion of women by addressing hypoestrogenism's effects on sexual desire and overall well-being.[25] Conjugated estrogens exhibit particular efficacy in decreasing VMS frequency, while estradiol and drospirenone show strong reductions in severity.[26] For genitourinary syndrome of menopause (GSM), encompassing vaginal dryness, dyspareunia, and urinary symptoms, low-dose vaginal estrogen provides targeted relief by restoring epithelial integrity and moisture, with meta-analyses confirming significant improvements in symptoms and sexual function compared to placebo.[27] Systemic HRT also mitigates GSM but is typically reserved for women with concurrent VMS due to broader effects.[28] Evidence from 2020-2025 guidelines, including those from the British Menopause Society, endorses HRT initiation under age 60 or within 10 years of menopause onset for optimal symptom control, emphasizing individualized assessment to balance benefits against risks.[29] Placebo-controlled trials highlight HRT's superiority, with estrogen achieving up to 80% reduction in hot flash episodes versus 30-50% for non-hormonal options, though placebo responses can account for 30-40% of perceived improvement in some studies.[30][31] Network meta-analyses comparing HRT to newer agents like fezolinetant affirm estrogen's edge in moderate-to-severe VMS relief, though non-hormonal therapies serve as alternatives for contraindications.[32] Overall, HRT's efficacy stems from counteracting hypoestrogenism's direct physiological impacts on thermoregulation and urogenital tissues, supported by causal mechanisms observed in clinical pathophysiology.[8]Osteoporosis Prevention
Hormone replacement therapy (HRT), particularly estrogen-containing regimens, prevents postmenopausal bone loss by mimicking premenopausal estrogen levels, which inhibit osteoclast activity and promote osteoblast function to maintain bone mineral density (BMD).[33] In randomized controlled trials and meta-analyses, HRT has consistently increased BMD at the lumbar spine, hip, and forearm by 2-5% annually during the first few years of treatment in early postmenopausal women.[34] This effect persists with continued use but diminishes upon discontinuation, with BMD declining faster than in non-users, leading to accelerated bone resorption.[35] Meta-analyses of randomized trials demonstrate that HRT reduces the risk of vertebral fractures by approximately 30-35% and non-vertebral fractures by 20-27%, with relative risks ranging from 0.66 to 0.73 across studies involving thousands of postmenopausal women.[36] For hip fractures specifically, observational data and subset analyses from trials like the Women's Health Initiative indicate a 30-50% risk reduction in younger postmenopausal women (aged 50-59 at initiation), though benefits are less pronounced in older cohorts starting therapy more than 10 years post-menopause.[37] These fracture reductions correlate directly with BMD gains and are independent of baseline fracture risk in some analyses, underscoring HRT's causal role in preserving bone architecture.[38] Combining HRT with weight-bearing exercise further augments BMD gains, with systematic reviews showing additive effects of up to 1-2% additional increase at key sites compared to HRT alone, though exercise alone yields smaller benefits.[39] Transdermal estrogen routes may offer comparable BMD preservation to oral forms while potentially minimizing some cardiovascular risks associated with first-pass liver metabolism, as evidenced in head-to-head trials.[40] Guidelines from bodies like the International Osteoporosis Foundation endorse HRT for osteoporosis prevention in symptomatic early postmenopausal women at high fracture risk, provided contraindications such as breast cancer history are absent, emphasizing its cost-effectiveness over bisphosphonates in this group.[41][33] Long-term adherence is critical, as post-HRT fracture risk rises by up to 55% within years of cessation compared to continuous users.[42]Hypogonadism in Men
Male hypogonadism refers to a clinical syndrome resulting from failure of the testes to produce adequate testosterone, manifesting in symptoms including diminished libido, erectile dysfunction, reduced muscle mass and strength, increased body fat, fatigue, depressed mood, and decreased bone mineral density.[43] Diagnosis requires the presence of these signs or symptoms alongside consistently low serum total testosterone concentrations, typically below 300 ng/dL confirmed by at least two early morning measurements (7-10 AM) to account for diurnal variation, with additional evaluation of luteinizing hormone and follicle-stimulating hormone levels to distinguish primary (testicular) from secondary (pituitary/hypothalamic) causes.[44][45][43] Testosterone replacement therapy (TRT) is indicated for men with confirmed symptomatic hypogonadism to restore testosterone levels to the mid-normal range (typically 400-700 ng/dL), aiming to alleviate symptoms and prevent complications such as osteoporosis.[21] The Endocrine Society recommends initiating TRT only after excluding contraindications like untreated prostate or breast cancer, severe untreated sleep apnea, or uncontrolled heart failure, with baseline assessments including prostate-specific antigen, hematocrit, and cardiovascular risk evaluation.[21] Therapy should be lifelong unless the underlying cause is reversible, with discontinuation typically resulting in the return of hypogonadal symptoms such as fatigue and low energy; regular monitoring of testosterone levels, hematocrit (to detect erythrocytosis, which occurs in up to 40% of patients), and prostate health every 3-12 months initially.[46][22][47] Randomized controlled trials and meta-analyses demonstrate that TRT improves sexual function, including libido and erectile performance (measured by International Index of Erectile Function scores), lean body mass, bone mineral density, and hemoglobin levels in hypogonadal men, with effect sizes varying by age and baseline testosterone but generally modest for mood and energy.[48][49][50] Benefits are more pronounced in younger men (<40 years) with pathological hypogonadism compared to age-related decline, where improvements in sexual symptoms persist but are smaller.[51][21] Adverse effects include elevated hematocrit leading to potential thromboembolism (requiring dose adjustment or phlebotomy if >54%), acne, gynecomastia, and suppression of spermatogenesis rendering TRT contraindicated in men desiring fertility.[22][21] Regarding cardiovascular risk, early observational concerns of increased events have not been substantiated in recent placebo-controlled trials and meta-analyses of hypogonadal men, showing no elevation in major adverse cardiovascular events, all-cause mortality, or prostate cancer incidence with up to 3 years of therapy.[52][53][50] Long-term prostate safety remains under study, but current evidence supports monitoring rather than routine discontinuation for elevated PSA unless biopsy confirms cancer.[21]Other Indications
Hormone replacement therapy (HRT) is recommended for women with primary ovarian insufficiency (POI), defined as cessation of ovarian function before age 40, to manage hypoestrogenic symptoms such as vasomotor instability, urogenital atrophy, and reduced bone density, while mitigating long-term risks including osteoporosis, cardiovascular disease, and impaired quality of life.[17] [54] The American Society for Reproductive Medicine's 2025 guideline endorses estrogen-progestogen regimens approximating physiological levels until the typical age of natural menopause (around 51 years), as this approach better preserves bone health and cardiovascular function compared to combined oral contraceptives, which provide supraphysiological hormone doses and may elevate thrombosis risk.[55] In POI cases with intermittent ovarian activity, HRT does not preclude attempts at natural conception but requires monitoring for potential resumption of endogenous function.[55] In Turner syndrome, a genetic condition involving monosomy X or structural X chromosome abnormalities leading to ovarian dysgenesis and primary hypogonadism, HRT with low-dose estrogen is initiated around ages 11-12 to induce puberty, followed by cyclic progestogen addition after 2-3 years to prevent endometrial hyperplasia and support uterine development if fertility preservation is pursued via oocyte donation.[56] Long-term continuation until age 50 is advised to maintain secondary sexual characteristics, cardiovascular health, and bone mineral density, with evidence showing that untreated hypogonadism in these patients correlates with aortic dilation and increased fracture rates.[56] Dosing typically escalates gradually (e.g., from 0.25-0.5 μg/day transdermal estradiol) to mimic pubertal progression, as abrupt higher doses risk epiphyseal closure and suboptimal height outcomes.[56] HRT is utilized in adults with gender dysphoria to induce secondary sex characteristics congruent with identified gender, administering estrogen plus anti-androgens (e.g., spironolactone or cyproterone acetate) to transgender women and testosterone to transgender men.[57] Short-term data indicate phenotypic changes such as breast development or voice deepening, but randomized controlled trials are scarce, and observational studies report elevated risks including a 3-fold increase in cardiovascular mortality for transgender women on ethinyl estradiol, higher stroke and myocardial infarction incidence overall, and potential breast cancer elevation in transgender women comparable to cisgender females after 5+ years.[58] [59] [60] Thrombotic events are noted particularly with oral estrogens, while testosterone in transgender men raises polycythemia risk but shows lower overall clotting incidence; long-term mortality remains higher than age-matched controls regardless of regimen, underscoring the need for individualized risk assessment and monitoring amid limited high-quality evidence.[61] [62]Forms and Administration
Estrogen and Progestogen Types
Estrogens employed in hormone replacement therapy (HRT) are categorized by their chemical structure and origin, with estradiol (17β-estradiol, E2) serving as the principal bioidentical form due to its potency and structural identity to the endogenous hormone produced by ovaries.[1] Micronized oral estradiol, available in doses of 0.5–2 mg daily, undergoes first-pass hepatic metabolism, while transdermal estradiol (patches delivering 0.025–0.1 mg/day) and gels (0.5–1.5 mg/day) bypass this, yielding more physiologic serum levels with reduced clotting factor elevation.[63] [1] Conjugated equine estrogens (CEE), derived from pregnant mare urine and comprising sulfate esters of estrone (E1), equilin, and other equine estrogens, were historically prevalent in formulations like 0.625 mg oral Premarin but exhibit variable bioavailability and higher thrombotic risk compared to estradiol due to non-human estrogens and hepatic effects.[1] [63] Synthetic conjugated estrogens (e.g., menest) and esterified estrogens (e.g., Estratab, combining E1 and E2 esters) offer alternatives but lack the bioidentical purity of estradiol and have been less favored in recent guidelines for their heterogeneous composition.[1] Ethinyl estradiol, a highly potent synthetic variant with ethinyl substitution enhancing oral absorption, is rarely used in menopausal HRT due to increased potency and venous thromboembolism risk, reserved more for contraceptive contexts.[1] Progestogens, required in HRT for women with an intact uterus to counteract estrogen-induced endometrial hyperplasia, encompass micronized progesterone—the bioidentical form derived from plant sources and administered orally (100–200 mg for 12–14 days cyclically or continuously) or vaginally—and various synthetic progestins classified by structure: pregnane derivatives (e.g., medroxyprogesterone acetate, MPA, 2.5–10 mg oral daily, as in the Women's Health Initiative trial), 19-nortestosterone derivatives (e.g., norethindrone 0.35–1 mg or levonorgestrel 0.15 mg), and retroprogesterone derivatives (e.g., dydrogesterone 10 mg).[64] [65] Micronized progesterone demonstrates endometrial protection with a more neutral metabolic profile, including lower breast cancer associations in observational data compared to certain progestins like MPA, which exhibits androgenic and glucocorticoid activity influencing lipid profiles and inflammation.[64] [65] Synthetic progestins vary in potency and side effects; for instance, MPA activates glucocorticoid receptors, potentially elevating cardiovascular risks, whereas dydrogesterone, a stereoisomer of progesterone, more closely mimics natural effects without 19-nortestosterone's virilizing potential.[64] Guidelines from bodies like the Endocrine Society prioritize micronized progesterone or dydrogesterone over nortestosterone-derived progestins for combined HRT to minimize adverse metabolic impacts.[66] [64]| Type | Examples | Key Characteristics | Common Doses in HRT |
|---|---|---|---|
| Estrogens | |||
| Bioidentical Estradiol | Oral micronized, transdermal patch/gel | Physiologic mimic; lower VTE risk transdermally | Oral: 1 mg; Transdermal: 0.05 mg/day |
| Conjugated Equine | Premarin (oral) | Mixture including non-human estrogens; hepatic first-pass | 0.625 mg oral |
| Esterified/Synthetic Conjugated | Estratab, synthetic CEE | Equine-derived alternatives; variable composition | 0.625–1.25 mg oral |
| Progestogens | |||
| Micronized Progesterone | Utrogestan (oral/vaginal) | Bioidentical; minimal androgenicity | 100–200 mg cyclic/continuous |
| Pregnane Progestins | Medroxyprogesterone acetate (MPA) | Synthetic; glucocorticoid activity | 2.5–5 mg continuous |
| 19-Nortestosterone Progestins | Norethindrone, Levonorgestrel | Androgenic; potent endometrial effect | 0.5–1 mg continuous |
| Retroprogesterone | Dydrogesterone | Progesterone stereoisomer; low side effects | 10 mg continuous |
Bioidentical Hormones
Bioidentical hormones refer to steroid hormones that possess the identical molecular structure and chemical composition as those endogenously produced by the human body, such as 17β-estradiol, progesterone, and testosterone.[67] These are typically synthesized from plant-derived sterols, like those in soy or yams, through chemical processes to replicate human hormones precisely.[68] In contrast to non-bioidentical alternatives, such as conjugated equine estrogens (e.g., Premarin) or synthetic progestins (e.g., medroxyprogesterone acetate), bioidentical forms are promoted by some clinicians for their purported alignment with physiological hormones, potentially leading to fewer side effects.[69] Several bioidentical hormones are available in FDA-approved formulations for hormone replacement therapy (HRT), including oral micronized progesterone (e.g., Prometrium, approved in 1999 for menopausal symptoms), transdermal or oral 17β-estradiol (e.g., Estrace, approved since 1971), and topical testosterone gels for hypogonadism in men (e.g., AndroGel, approved 2000).[70] These approved products undergo rigorous testing for efficacy, safety, and manufacturing consistency, demonstrating benefits comparable to other HRT forms in alleviating menopausal vasomotor symptoms and preventing bone loss when initiated near menopause onset.[71] However, "compounded bioidentical hormone therapy" (cBHT) involves custom preparations from compounding pharmacies, often including combinations like estradiol, progesterone, and estriol (not FDA-approved for systemic use), tailored via saliva or blood testing—a practice lacking standardization and FDA oversight.[72][73] Administration routes for bioidentical hormones mirror those of conventional HRT: oral capsules, transdermal patches or gels, vaginal creams or rings, and subcutaneous pellets for compounded forms.[69] Proponents argue that bioidentical hormones, due to their structural identity, may yield more predictable pharmacokinetics and reduced risks like thromboembolism compared to synthetics, citing differences in hepatic first-pass metabolism for transdermal estradiol.[74] Yet, systematic reviews of randomized trials find no robust evidence that bioidentical hormones—approved or compounded—confer superior safety or efficacy over FDA-approved non-bioidentical HRT; outcomes for symptom relief, cardiovascular events, and cancer risks align closely, with cBHT introducing variability from inconsistent dosing and purity.[71][75] The FDA explicitly states that compounded bioidenticals have not been demonstrated as safer or more effective, and their use is not recommended when approved alternatives exist, due to risks of under- or overdosing and contamination.[72][76] Professional societies, including the North American Menopause Society and American College of Obstetricians and Gynecologists, caution against routine cBHT prescription, emphasizing the absence of large-scale, long-term data supporting superiority claims and highlighting regulatory gaps that undermine quality control.[77] For instance, a 2020 National Academies report reviewed available studies and concluded that cBHT should be restricted to cases of allergy to FDA-approved product ingredients or unique dosing needs unmet by commercial options, as empirical evidence from trials shows equivalent therapeutic profiles without added benefits.[78] While bioidentical estradiol and progesterone exhibit bioequivalent effects to endogenous hormones in short-term studies, the inclusion of unapproved components like estriol in compounded regimens lacks validation for systemic HRT, potentially elevating unquantified risks.[79] Overall, selection of bioidentical forms should prioritize FDA-approved products over compounded ones for verifiable safety and efficacy in clinical practice.[80]Routes and Regimens
Hormone replacement therapy (HRT) employs multiple routes of administration to deliver estrogen, progestogen, or testosterone, tailored to achieve systemic or local effects while minimizing risks such as hepatic first-pass metabolism associated with oral routes. Systemic estrogen is primarily administered orally (e.g., conjugated equine estrogens 0.3–0.625 mg daily or estradiol 1–2 mg daily) or transdermally (e.g., patches delivering 0.025–0.1 mg estradiol daily or gels 0.5–1.5 mg daily), with transdermal methods preferred in some guidelines for reducing venous thromboembolism risk due to avoidance of prothrombotic liver effects.[81][82][83] The route of administration also impacts pharmacokinetic profiles and clinical outcomes beyond thrombosis risk. Oral estrogen leads to fluctuating estradiol levels due to daily peaks and troughs from dosing as well as first-pass hepatic metabolism, which are associated with worse mood outcomes including increased depressive symptoms, anxiety, and emotional sensitivity to stress, similar to effects in the menopausal transition.[84] In contrast, transdermal administration achieves more stable estradiol levels, linked to improved mood, reduced anxiety, and better sleep quality. For lipid profiles, transdermal HRT has neutral or beneficial effects, such as no increase or decrease in triglycerides with a favorable overall profile, while oral HRT may increase triglycerides despite potential improvements in HDL/LDL ratios.[85] Oral HRT can be suitable for women in overall good health with no history of clots or heart disease, particularly those with severe symptoms who prefer the convenience of daily dosing; it may be safe at low doses but requires individualized physician evaluation considering age, medical history, and necessary tests.[1][8] Vaginal routes, using creams, rings, or tablets (e.g., estradiol 10 mcg twice weekly), provide localized relief for urogenital symptoms with minimal systemic absorption.[86] Intramuscular injections of estrogen esters, though less common today, offer longer-duration effects but require medical administration.[87] Progestogens in combined HRT are delivered orally (e.g., micronized progesterone 100–200 mg daily or norethisterone 1 mg daily), transdermally, vaginally, or via intrauterine devices (e.g., levonorgestrel-releasing IUD releasing 20 mcg daily initially).[1][88] The intrauterine route minimizes systemic exposure, reducing side effects like mood changes while protecting the endometrium.[88] For men with hypogonadism, testosterone regimens include intramuscular injections (e.g., testosterone enanthate or cypionate 50–400 mg every 2–4 weeks), daily transdermal gels (50–100 mg applied to skin), patches (2–5 mg daily), or subcutaneous pellets implanted every 3–6 months.[81] Oral testosterone undecanoate (40–80 mg two to three times daily with meals) is an option but shows variable efficacy due to absorption issues.[89] Regimens for combined estrogen-progestogen HRT in women with intact uteri distinguish sequential (cyclical) from continuous combined approaches to balance symptom relief and endometrial protection. Sequential regimens involve daily estrogen with progestogen added for 10–14 days monthly (e.g., micronized progesterone 200 mg for 12 days), inducing withdrawal bleeding and suiting perimenopausal women with irregular cycles.[1][87] Continuous combined regimens administer both hormones daily (e.g., estradiol 1 mg plus norethisterone 0.5 mg), often eliminating bleeding after initial months and preferred for postmenopausal women to enhance adherence and bone density gains.[90][87] Estrogen-only regimens (e.g., 0.5–1 mg daily) apply post-hysterectomy, while testosterone dosing adjusts to maintain mid-normal serum levels (300–1000 ng/dL), monitored every 3–6 months.[21] Individualization accounts for age, BMI, and comorbidities, with lowest effective doses recommended.[91]Efficacy and Benefits
Evidence from Randomized Trials
Randomized controlled trials (RCTs) consistently demonstrate that menopausal hormone therapy (MHT), a form of hormone replacement therapy, effectively alleviates vasomotor symptoms such as hot flashes and night sweats. A systematic review of RCTs indicates that MHT reduces hot flash frequency by approximately 75% and severity by 87% in a dose-dependent manner, compared to about 50% reduction with placebo.[66] Shorter-term RCTs, often lasting 6-12 months, confirm these benefits, with conjugated equine estrogens (CEE) plus medroxyprogesterone acetate (MPA) or estradiol-based regimens showing superior efficacy over non-hormonal alternatives for moderate-to-severe symptoms.[92] These trials typically enroll symptomatic perimenopausal or early postmenopausal women, aged 45-55, highlighting MHT's role in symptom management rather than universal prevention.[8] For bone health, RCTs including the Women's Health Initiative (WHI) provide evidence of MHT's efficacy in preventing osteoporosis-related fractures. The WHI estrogen-plus-progestin trial, involving 16,608 postmenopausal women followed for a mean of 5.6 years, reported a 33% reduction in hip fractures and a 24% reduction in total fractures with CEE 0.625 mg plus MPA 2.5 mg daily versus placebo.[4] Meta-analyses of RCTs further substantiate these findings, showing MHT increases bone mineral density (BMD) at the spine, hip, and forearm by 2-7% over 2-3 years, with a nonsignificant trend toward reduced vertebral and nonvertebral fracture incidence (relative risk 0.77 for nonvertebral fractures).[34] These benefits are most pronounced in early postmenopausal women and diminish upon discontinuation, as evidenced by post-trial follow-up data.[93] Additional RCTs support improvements in quality of life and genitourinary symptoms. A 20-week RCT of estradiol replacement in early postmenopausal women found enhancements in mood, cognitive function, and overall well-being compared to placebo.[94] For vaginal atrophy, RCTs demonstrate MHT restores mucosal integrity and reduces symptoms like dryness and dyspareunia, with local estrogen therapies showing comparable efficacy to systemic options in smaller trials.[95] However, the WHI trials, conducted in older women (mean age 63), underscore that benefits for chronic disease prevention are limited, with primary efficacy observed in symptom relief among younger subgroups.[96] Overall, RCT evidence prioritizes MHT for short-term use in symptomatic women, with benefits outweighing placebo in targeted outcomes.[97]Age and Timing Considerations
![Coronary artery plaque formation][float-right] The timing hypothesis posits that the initiation of menopausal hormone replacement therapy (HRT) closer to the onset of menopause—typically within 10 years or before age 60—yields more favorable cardiovascular outcomes compared to later initiation, due to the influence on early-stage atherosclerosis progression rather than advanced plaque disruption.[98] This hypothesis emerged from subgroup analyses of the Women's Health Initiative (WHI) trials, where younger women (aged 50-59) experienced lower absolute risks of adverse events and potential benefits in coronary heart disease reduction, contrasting with null or harmful effects in older cohorts with mean age around 63 at enrollment.[8] Meta-analyses of randomized trials support reduced all-cause mortality by up to 39% and coronary artery disease incidence by 32% when HRT is started before age 60 or within 10 years of menopause, particularly with estrogen-progestogen combinations in women with an intact uterus.[99] These benefits extend to menopausal symptom alleviation and osteoporosis prevention, which are more pronounced and sustained with early intervention, as delayed therapy may diminish efficacy against vasomotor symptoms and bone loss.[24] However, even early initiation carries persistent risks such as stroke, with meta-regression indicating no significant age-modifying effect for thromboembolic events.[100] Average age at natural menopause is 51 years, with 95% of women experiencing it between 45 and 55, informing the "critical window" for optimal HRT timing to maximize neuroprotective and cardiometabolic advantages while minimizing harms.[101] Guidelines from bodies like the North American Menopause Society endorse HRT for symptom management in women under 60 or within a decade of menopause onset, provided risks are individualized, reflecting evidence that later starts (e.g., beyond 10 years post-menopause) correlate with heightened cardiovascular and mortality risks without commensurate benefits.[102] Long-term follow-up data reinforce that cumulative exposure duration, rather than isolated age, modulates breast cancer associations, though early starters may face modestly elevated short-term risks offset by overall mortality reductions.[103]Long-Term Outcomes
![Coronary artery plaque formation][float-right] Long-term use of menopausal hormone replacement therapy (HRT) has been associated with reduced all-cause mortality in women initiating treatment near menopause onset, with meta-analyses of randomized trials reporting up to a 39% relative risk reduction compared to placebo, particularly when started before age 60 or within 10 years of menopause.[5] This benefit aligns with the timing hypothesis, where early intervention mitigates accelerated postmenopausal atherosclerosis, as evidenced by lower composite cardiovascular outcomes including death, myocardial infarction, and heart failure hospitalization in observational cohorts of younger users.[8] However, overall randomized trial data, such as from the Women's Health Initiative, show neutral effects on mortality across broader age groups, highlighting the importance of initiation timing.[11] Skeletal outcomes demonstrate consistent long-term benefits, with HRT reducing the incidence of osteoporotic fractures by preventing bone loss; randomized trials indicate a 30-50% lower risk of hip, vertebral, and other fractures during treatment, persisting to some degree post-discontinuation depending on duration of prior use.[104] For instance, 2-3 years of therapy in healthy women yields sustained preventive effects on bone mass and fracture risk over decades, as shown in the PERF study.[105] Discontinuation leads to accelerated bone loss and elevated fracture risk, more pronounced after longer prior exposure, underscoring HRT's role in osteoporosis prevention when continued as needed.00048-0/fulltext) Cardiovascular effects favor early HRT, with reduced coronary heart disease events in recently postmenopausal women; a 2012 randomized trial follow-up reported lower long-term CVD outcomes with opposed estrogen-progestogen therapy started within years of menopause.[106] Transdermal routes may further minimize risks compared to oral, showing no increased cardiovascular disease incidence in contemporary analyses.[9] Biological aging markers also improve with HRT, correlating with lower all-cause mortality and incident coronary events in meta-analyses.[99] Cognitive long-term outcomes indicate no adverse effects and potential preservation of verbal memory when HRT is initiated in midlife; systematic reviews of trials near menopause show standardized mean differences of 0.394 in verbal memory improvement with estrogen therapy.[107] In low-cardiovascular-risk women, short-term exposure yields no long-term cognitive decline, as confirmed by 10-year follow-ups in studies like KEEPS-Cog.[108] Overall, these outcomes support targeted HRT for symptom relief and prevention in appropriate candidates, with benefits accruing over years to decades.Risks and Adverse Effects
The risks of hormone replacement therapy (HRT) are generally low for healthy women under age 60 or within 10 years of menopause onset, but can include blood clots (higher with oral forms), stroke, and a small increase in breast cancer after several years of combined estrogen-progestogen therapy. HRT is not suitable for everyone, such as those with certain cancer histories or high clot risk.Cardiovascular and Thromboembolic Risks
Hormone replacement therapy (HRT), particularly oral formulations containing estrogen and progestogen, has been linked to elevated risks of coronary heart disease and stroke in postmenopausal women, with effects modulated by age at initiation and proximity to menopause onset. In randomized trials like the Women's Health Initiative, combined estrogen-progestin therapy increased coronary events (hazard ratio 1.24, 95% CI 1.00-1.54) and stroke (HR 1.37, 95% CI 1.07-1.76) among women averaging 63 years old.[8] However, subgroup analyses support a "timing hypothesis," where initiation within 10 years of menopause or before age 60 may yield neutral or reduced coronary risk (RR 0.70 for mortality in early starters), contrasting with harm in older women.[8] [109] A 2024 meta-analysis confirmed that menopausal hormone therapy fails to lower overall cardiovascular events and increases stroke risk across studies, though arterial dilation improves.[10] Recent observational data reinforce formulation-specific risks: oral estrogen-progestin therapy associates with higher heart disease incidence compared to non-users, while transdermal or tibolone options show lesser or no elevation.[9] Age-stratified findings indicate increased coronary risk even in the 50-59 group for certain regimens, though absolute event rates remain low (e.g., 3-4 additional events per 1000 women-years).[9] Stroke risk similarly rises with oral HRT (RR ~1.3-1.5 in trials), persisting across ages but potentially mitigated if started early post-menopause (decreased risk 0-5 years after onset vs. never-use).[110] [10] Thromboembolic risks, including deep vein thrombosis and pulmonary embolism, are markedly higher with oral estrogen due to first-pass hepatic effects promoting coagulation factor changes and protein C resistance, unlike transdermal routes. Meta-analyses report a 48-66% relative increase in venous thromboembolism (VTE) for oral estrogen-only (RR 1.48, 95% CI 1.05-2.07) or combined therapy, with no significant elevation for transdermal (RR 0.95, 95% CI 0.57-1.61).[111] [112] Oral regimens confer ~2-fold VTE risk (RR 1.92, 95% CI 1.24-2.99), amplified by progestins, obesity, or higher doses, while transdermal estrogen avoids this prothrombotic profile.[8] [82] Absolute risks are modest (2-4 additional cases per 1000 user-years), but contraindications apply in thrombophilia or prior events.[83] Commercial insurance data affirm transdermal HRT neutrality and lower oral estradiol risks versus other estrogens.[113]Cancer Associations
Hormone replacement therapy (HRT), particularly combined estrogen-progestin therapy (EPT), has been associated with an increased risk of breast cancer in postmenopausal women. In the Women's Health Initiative (WHI) randomized trial, women assigned to EPT experienced a hazard ratio of 1.24 (95% CI 1.01-1.53) for invasive breast cancer after a mean follow-up of 5.6 years, translating to approximately 8 additional cases per 10,000 women per year compared to placebo.[3] This risk increased with duration of use, with meta-analyses confirming relative risks of around 2.0 for 5-9 years of EPT.[114] Estrogen-only therapy (ET), evaluated in hysterectomized women in the WHI, showed no significant increase in breast cancer risk and possibly a slight reduction in long-term follow-up (HR 0.79, 95% CI 0.65-0.97 after 18 years).[115] Recent studies indicate that risks are higher for progesterone-containing regimens than bioidentical micronized progesterone, with the latter showing lower breast cancer incidence in observational data (RR 0.67).[116] Unopposed estrogen therapy substantially elevates the risk of endometrial cancer due to endometrial proliferation without progestogenic opposition. Systematic reviews report odds ratios exceeding 2.0 for ever-use of unopposed estrogen, with risk rising proportionally to duration and dose; for example, use beyond 5 years can increase risk up to 10-fold.[117] Adding progestin mitigates this: continuous combined HRT appears neutral or protective, while sequential regimens may confer a modest increase (OR 1.5-2.0).[117] The National Cancer Institute summarizes that this excess risk from unopposed estrogen is eliminated by concurrent progestin administration.[118] Evidence on ovarian cancer is less consistent but suggests a small increased risk with prolonged HRT use, particularly ET. A 2015 collaborative reanalysis of 52 studies found a relative risk of 1.41 (95% CI 1.26-1.59) for 5 years of use starting around age 50, equating to about one extra case per 1,000 users over 5 years.[119] Meta-analyses indicate higher risks for serous and endometrioid subtypes, though recent trends show diminishing associations, possibly due to shorter durations and modern formulations.[120] Combined HRT shows neutral or lower risks in some trials compared to ET alone.[121] For colorectal cancer, WHI findings indicate a protective effect from EPT, with a 38% reduction in incidence (HR 0.62, 95% CI 0.42-0.92) during the intervention phase, though mortality was not reduced and tumors were more advanced at diagnosis.[122] ET showed no significant effect on incidence.[123] Observational studies reinforce a lower risk with current or recent HRT use, potentially modulated by genetic factors.[124] Overall cancer risks vary by HRT type, duration, and patient factors, with benefits in some sites offsetting concerns in others; absolute risks remain low for short-term use in symptomatic women.[125]Neurological and Other Effects
Hormone replacement therapy (HRT) has been associated with varied neurological outcomes depending on initiation timing and formulation. Randomized controlled trials, such as those from the Women's Health Initiative Memory Study (WHIMS), demonstrated an increased risk of probable dementia (relative risk [RR] 1.49) and mild cognitive impairment in postmenopausal women aged 65 years or older receiving conjugated equine estrogens plus medroxyprogesterone acetate compared to placebo, with 23 additional dementia cases per 10,000 women per year.[126] This risk was not observed in younger women or with estrogen-only therapy in similar age groups. Meta-analyses of observational studies indicate that HRT initiated within five years of menopause onset may reduce Alzheimer's disease risk by 20% to 32%, potentially due to neuroprotective effects of estradiol on synaptic plasticity and amyloid clearance when brain estrogen receptors remain responsive.[127] Conversely, late initiation correlates with elevated dementia incidence (RR 1.38), highlighting age-dependent vulnerability where prolonged hypoestrogenism alters neuronal resilience.[128] Cognitive function assessments from randomized trials, including the Kronos Early Estrogen Prevention Study Cognitive trial, show no significant long-term benefits or harms from HRT on global cognition, verbal memory, or executive function after 48 months in women starting therapy near menopause.[108] A meta-analysis of 23 randomized controlled trials confirmed neutral effects on overall cognitive performance in healthy postmenopausal women, with inconsistent improvements in verbal memory domains.[129] These findings suggest HRT does not accelerate cognitive decline but offers limited protection against it, influenced by baseline vascular health and apolipoprotein E ε4 carrier status, where early estradiol exposure preserved hippocampal volumes in genetically at-risk individuals.[130] Psychiatric effects include potential mood alterations, with systemic HRT linked to higher depression incidence during perimenopause and early postmenopause (odds ratio up to 1.3 in some cohorts), possibly from fluctuating estrogen impacting serotonin modulation.[131] Transdermal formulations appear to mitigate this, showing lower depression rates (3.3% vs. 5.1% for oral), attributed to reduced hepatic first-pass metabolism and proinflammatory effects.[132] Anxiety and irritability may transiently increase during HRT initiation due to rapid hormonal shifts, though long-term data indicate stabilization without elevated risk in monitored users.[133] Among other adverse effects, HRT elevates gallbladder disease risk, with all formulations—including oral estrogens, tibolone, and topical applications—associated with higher gallstone incidence (RR 1.5–2.0), driven by estrogen-induced cholesterol supersaturation in bile.[134] Estrogen-progestin combinations increase urinary incontinence rates at one year (RR 1.39), likely via pelvic floor relaxation and urethral sphincter weakening, though estrogen-only therapy shows neutral or protective effects on lower urinary tract symptoms in some trials.[135] Increasing the progesterone dose in HRT can cause or exacerbate abdominal cramping, pelvic pain, or uterine cramps in some individuals due to progesterone intolerance; these symptoms vary by individual, dose, and administration method (e.g., oral vs. vaginal), and may be managed by adjusting the dose or route.[136] These risks underscore the need for individualized assessment, as absolute incidences remain low in younger initiators with oral routes conferring higher hepatic burdens.[101]Contraindications and Monitoring
Absolute and Relative Contraindications
Absolute contraindications to systemic menopausal hormone therapy include conditions where the potential risks demonstrably exceed benefits based on elevated incidence of adverse events in clinical trials and observational data. These encompass known or suspected estrogen-sensitive malignancies, such as breast or endometrial cancer, due to documented increased recurrence risks with estrogen exposure.[1][137] Undiagnosed abnormal vaginal bleeding represents another absolute contraindication, as it may signal underlying endometrial pathology requiring investigation prior to therapy initiation.[1] Active or recent (within one year) thromboembolic events, including deep vein thrombosis, pulmonary embolism, stroke, or myocardial infarction, contraindicate use owing to heightened prothrombotic effects of oral estrogens, with hazard ratios for venous thromboembolism reaching 1.5-2.0 in randomized trials.[1][137] Known hereditary or acquired thrombophilias, such as factor V Leiden or protein C/S deficiencies, similarly preclude therapy due to compounded clotting risks.[1] Acute or decompensated liver disease is contraindicated, reflecting impaired estrogen metabolism and potential hepatotoxicity observed in case series.[137] Relative contraindications involve scenarios where therapy may proceed with heightened monitoring, risk mitigation, or alternative routes (e.g., transdermal over oral to minimize thrombotic potential), balancing individual symptom severity against probabilistic harms. Uncontrolled hypertension (systolic ≥180 mmHg or diastolic ≥110 mmHg) qualifies as relative, linked to amplified stroke risk in hypertensive cohorts per meta-analyses of trials like the Women's Health Initiative.[8] Migraine with aura constitutes a relative bar, associated with 2-fold ischemic stroke odds in estrogen users under age 50, though data weaken post-menopause.[6] Hypertriglyceridemia (>400 mg/dL) warrants caution due to rare pancreatitis flares with oral estrogens, resolvable via non-oral formulations.[6] Smoking elevates cardiovascular hazards synergistically, with relative risks for coronary events up to 3.0 in smokers on therapy per cohort studies, advising cessation prior to initiation.[6] Other relatives include controlled hypertension, diabetes mellitus, obesity (BMI ≥30 kg/m²), gallbladder disease, and seizure disorders, where empirical associations with adverse outcomes necessitate individualized assessment rather than blanket exclusion.[1][6] For history of breast cancer, while often deemed absolute for systemic therapy, select low-risk cases (e.g., ductal carcinoma in situ) may permit vaginal low-dose estrogen after oncology consultation, supported by registry data showing no survival detriment.[88]| Category | Examples | Rationale and Evidence |
|---|---|---|
| Absolute | Estrogen-sensitive cancer (breast, endometrial); Undiagnosed vaginal bleeding; Active thromboembolism; Known thrombophilia; Acute liver disease | Direct causal links to recurrence or events; e.g., VTE incidence doubles with oral HRT in trials.[1][137] |
| Relative | Migraine with aura; Uncontrolled hypertension; Smoking; Hypertriglyceridemia; Obesity/Diabetes | Dose/route-dependent risks; e.g., transdermal estrogen halves VTE odds vs. oral in meta-analyses.[8][6] |
