Recent from talks
Nothing was collected or created yet.
Intracranial hemorrhage
View on Wikipedia
| Intracranial hemorrhage | |
|---|---|
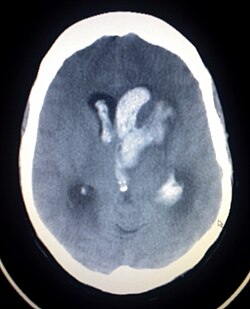 | |
| Axiali CT scan of a spontaneous intracranial hemorrhage | |
| Specialty | Emergency medicine |
| Symptoms | Same symptoms as ischemic stroke, but unconsciousness, headache, nausea, stiff neck, and seizures are more often in brain hemorrhages than ischemic strokes |
| Complications | Coma, persistent vegetative state, cardiac arrest (when bleeding is in the brain stem or is severe), death |
| Types | Intracerebral hemorrhage, subarachnoid hemorrhage, epidural bleed, subdural bleed |
| Causes | Stroke, head injury, ruptured aneurysm |
Intracranial hemorrhage (ICH) refers to any form of bleeding within the skull.[1] It can result from trauma, vascular abnormalities, hypertension, or other medical conditions. ICH is broadly categorized into several subtypes based on the location of the bleed: intracerebral hemorrhage (including intraparenchymal and intraventricular hemorrhages), subarachnoid hemorrhage, epidural hemorrhage, and subdural hematoma. Each subtype has distinct causes, clinical features, and treatment approaches.[2]
Epidemiology
[edit]Acute, spontaneous intracranial hemorrhage (ICH) is the second most common form of stroke, affecting approximately 2 million people worldwide each year.[3] In the United States, intracranial hemorrhage accounts for about 20% of all cerebrovascular accidents, with an incidence of approximately 20 cases per 100,000 people annually. [4] Intracranial hemorrhages is diagnosed more frequently in men and individuals over the age of 55, with incidence increasing with age.[4] In low-income countries, the risk is higher, potentially due to reduced access to healthcare and limited education about primary prevention.[4]
Risk factors and causes
[edit]Intracranial hemorrhage (ICH) may be classified as either traumatic or non-traumatic (spontaneous). Traumatic causes include head trauma resulting from falls, vehicular accidents, or physical assault. Non-traumatic causes are more varied and often related to underlying conditions. Chronic hypertension is the most common non-traumatic cause, particularly in deep brain structures such as the basal ganglia, thalamus, pons, and posterior fossa.[3] Other spontaneous causes include cerebral amyloid angiopathy, especially among the elderly, as well as bleeding disorders such as hemophilia and thrombocytopenia, vascular malformations like arteriovenous malformation (AVMs), and brain tumors.
The use of anticoagulant or antiplatelet medications, such as warfarin and aspirin, has been associated with increased hematoma volume and expansion.[3] Illicit drug use, particularly cocaine and methamphetamine, can cause abrupt spikes in blood pressure leading to vessel rupture and subsequent hemorrhage.[3]
Additional risk factors that increase the likelihood of intracranial hemorrhage include smoking, heavy alcohol consumption, advanced age, a family history of stroke, diabetes, hyperlipidemia, obesity, and sedentary lifestyle. Hypertension remains the most prevalent and well-established risk factor, contributing to over 60% of primary bleeds.[3]
Signs and symptoms
[edit]Intracranial hemorrhage is a dynamic and potentially life-threatening process that begins with blood extravasation into the brain parenchyma.[5] This can be followed by bleeding extension, cerebral edema formation, and increased intracranial pressure (ICP), all of which can lead to neural tissue compression.[5]
Common signs and symptoms include a sudden onset of focal neurological deficits, which vary depending on the location of the hemorrhage. Decreased levels of consciousness are frequently observed and are assessed using the Glasgow Coma Scale (GCS). Other manifestations include headache, nausea, vomiting, and seizures. Patients may also present with speech disturbances, unilateral weakness or paralysis, sensory deficits, visual impairments, and problems with coordination or balance. Raised diastolic blood pressure is a common clinical finding.
Seizures occur in up to 70% of causes, usually within the first 24 to 72 hours following hemorrhage onset.[5] If bleeding extends into the ventricles, hydrocephalus may develop. Brainstem hemorrhages are especially dangerous and can result in cardiorespiratory instability, decreased consciousness, and even cardiac arrest.[4] Long-term complications of intracranial hemorrhages may include post-stroke epilepsy and vascular cognitive impairment.[3]
Diagnosis
[edit]
A non-contrast CT scan (computed tomography) of the brain is commonly used as the initial imaging modality in suspected cases of intracranial hemorrhage. CT is preferred in emergency settings due to its speed, availability, and high sensitivity for detecting acute brain injuries, enabling rapid triage and surgical decision-making. Examples of brain diseases that require urgent intervention are: large-volume hemorrhage, brain herniation, and cerebral infarction. Additional advantages of CT imaging include its effectiveness in detecting bony fractures, vascular injuries, and cerebrospinal fluid (CSF) leaks.
Despite its advantages, MRI (magnetic resonance imaging) has higher sensitivity than CT scan for the detection of epidural hemorrhage, subdural hemorrhage, subarachnoid hemorrhage, non hemorrhagic contusions in the cortex, hemorrhagic parenchymal contusions, brainstem injuries, and white matter axonal injuries. MRI is typically used when a patient continues to display neurological symptoms despite a normal CT scan.[5] However, the use of MRI is limited by safety concerns regarding metallic foreign bodies, longer imaging times, and higher sensitivity to motion, reducing availability, and increased cost. [6]
A swirl sign on CT imaging— representing areas of low density with surrounding areas of high density— suggest active intracranial bleeding. The presence of this sign is associated with an increase in risk of death within one month and a poor functional prognosis at three months among survivors.[6]
Traumatic
[edit]Intracranial hemorrhages are broadly classified into intra-axial and extra-axial types, based on the location of the bleeding relative to the brain tissue.[7]
Intra-axial hemorrhage refers to bleeding that occurs within the brain parenchyma or ventricular system.[7] This category includes intraparenchymal hemorrhage, which involves bleeding directly into the brain tissue, and intraventricular hemorrhage, which involves bleeding into the brain’s ventricular system—commonly observed in premature infants. Intra-axial hemorrhages are generally associated with a poorer prognosis and are more challenging to manage than extra-axial hemorrhages.[1] Traumatic forms of intra-axial hemorrhage include hemorrhagic parenchymal contusions and cerebral microhemorrhages.[2]
Extra-axial hemorrhage occurs within the cranial vault but outside the brain tissue.[7] It encompasses three main subtypes: epidural hematoma, subdural hematoma, and subarachnoid hemorrhage, each defined by the specific meningeal compartment in which the bleeding occurs.[2]
Hemorrhagic parenchymal contusion
[edit]Hemorrhagic parenchymal contusions most commonly occur following significant head trauma, particularly in cases involving rapid head movement or direct impact.[8] These injuries result from the disruption of small arterial or venous vessels, leading to hemorrhage within the brain parenchyma.[8] On computed tomography (CT), they appear as hyperdense lesions. Magnetic resonance imaging (MRI), particularly with gradient echo sequences, is more sensitive than CT in detecting small hemorrhagic contusions.[1]
Contusions are frequently observed in areas of the brain adjacent to the base of the skull, such as the inferior frontal lobess and temporal lobes, commonly resulting from coup-contrecoup injuries.[7] Those with parenchymal contusion require frequent follow-up imaging because such contusions may grow large enough to become hemorrhage and exert a significant mass effect on the brain.[1]
Cerebral microhemorrhage
[edit]Cerebral microhemorrhages are small-scale hemorrhagic lesions that can be considered a minor form of hemorrhagic parenchymal contusion.[2] They are typically located within the cerebral white matter and are challenging to detect using CT imaging. However, they are more readily identified on MRI, particularly with gradient echo or susceptibility-weighted imaging (SWI), where they appear as hypointense foci due to susceptibility blooming artifacts.[9] Such microhemorrhages are frequently associated with diffuse axonal injury and located near the grey–white matter junction.[1]
Epidural hemorrhage
[edit]Epidural hemorrhage (also known as extradural hemorrhage, EDH) refers to bleeding between the dura mater and the inner surface of the skull, typically resulting from traumatic head injury. This condition is characterized by its inability to cross cranial suture lines due to the tight adhesion of the dura to the skull at these points. However, in rare cases—especially in children where skull sutures are not fully fused—epidural hemorrhages may extend across sutures if a fracture involves them.[1]
On computed tomography (CT), epidural hemorrhages typically appear as biconvex (lentiform) hyperdense lesions confined by sutural boundaries.[2] The source of bleeding may be arterial or venous. Arterial injuries, such as to the middle meninges artery, commonly at the pterion, lead to rapidly expanding hematomas.[1] Venous sources are usually slower-growing and may involve dural venous sinuses, including the falx cerebri, tentorium cerebelli, or the superior sagittal sinus.[1]
Anterior temporal EDH is usually caused by sphenoparietal sinus. Such EDH is limited and does not require surgery because its extension is confined within the sphenosquamosal suture and the superior or inferior orbital fissures.[6] In 20% to 50% of epidural hemorrhage cases, there is a lucid interval during which the patient regains temporary consciousness after an initial loss; this is then followed by deterioration of conscious state.[10]
When the epidural hematoma is large enough, it will cause mass effect on contralateral brain which lead to midline, subfalcine (below the falx cerebri), and trans-tentorial (crossing tentorium cerebelli) herniations. This phenomenon can cause the subject to lose consciousness and eventually death.[1] Large EDH often requires emergent surgical clot evacuation.[1] Embolisation of middle meningeal artery is performed if the hemorrhage is medium or small.[6]
Subdural hemorrhage
[edit]Subdural hemorrhage (SDH) results from tearing of the bridging veins in the subdural space between the dura and arachnoid mater. It can cross the suture lines, but not across dural reflections such as falx cerebri or tentorium cerebelli.[6] Therefore, subdural hematoma are typically confined to one side of the cerebral hemisphere.[1]
Density of SDH reduces as it progresses from acute to chronic forms. However, areas with low density may not represent chronic SDH entirely as unclotted blood products that are due to active bleed can also give low density appearance on CT scans especially those with coagulopathy. Those with SDH that have same density with brain parenchyma may represent acute bleed such as those with anemia, arachnoid tear, and the mixing of hemorrhage and CSF. SDH usually have high or mixed densities during first two days of trauma, followed by isodensity at 11 days after trauma, and hypodensity after 14 days of trauma. Membranes with granulation tissue can rupture within SDH, and give high density appearance on CT scan. Over a prolonged period of time, calcifications can form. SDH can be treated with burr hole drainage, craniotomy or port system placement for blood clot evacuation, or middle meningeal artery embolisation.[6]
Subdural hematoma maybe less acute than epidural hematoma due to slower blood accumulation, but it still has the potential to cause brain herniation that may require surgical evacuation.[1] Clinical features depend on the location and severity of the injury. Patients may have a history of loss of consciousness but they recover and do not relapse. Symptoms vary but may include loss of consciousness, seizures, or focal neurologic deficits, with an onset that can be delayed by hours to days after injury.[7]
Subarachnoid hemorrhage
[edit]A subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. Trauma can also cause SAH when the arteries and veins coursing through the subarachnoid space are ruptured.[11]
On CT imaging, traumatic SAH is usually localized to the cerebral sulci near the vertex of the head and typically spares the basal cisterns.[11] Severe trauma can cause SAH in all regions of the brain. When the SAH volume is large, rarely it can cause cerebral infarction a few days after trauma due to arterial vasospasm.
Although CT scans are more frequently used for initial evaluation, MRI is more sensitive than CT in detecting SAH. Findings may include hyperintense signal of fluid-attenuated inversion recovery (FLAIR) sequence and blooming artifact on susceptibility weighted imaging (SWI).[1]
Further vascular imaging, such as CT angiography (CTA) or MR angiography (MRA), is recommended in certain situations—particularly when a skull fracture involves the carotid canal, due to the risk of post-traumatic vasospasm impairing cerebral perfusion. These imaging techniques are also used when the hemorrhage pattern is atypical for trauma, as in isolated SAH located in the basal cisterns, Sylvian fissure, or anterior interhemispheric fissure. Such patterns may suggest ruptured intracranial aneurysms, and warrant further investigation.[6]
Non-traumatic
[edit]Hypertensive bleed
[edit]Hypertensive intracerebral hemorrhage (ICH) typically occurs in individuals between 50 and 60 years of age and is associated with high mortality, with case fatality rates ranging from 30% to 50%.[5] Such hemorrhages are typically located in the basal ganglia, cerebellum, or occipital lobes. Less common locations, such as lobar bleeds within the cerebral cortex or intracranial bleeds in people younger than 50 years of age, should prompt further investigation for alternative etiologies, such as brain tumors or cerebral arteriovenous malformation.
The size of the hemorrhage can vary, ranging from small, asymptomatic lesions to large hematomas causing mass effect and increased intracranial pressure. Follow-up CT imaging is recommended to monitor hematoma expansion, ventricular extension, or progressive cerebral edema, all of which are associated with poorer outcomes.
CT angiography (CTA) may be used to assess active bleeding. The presence of a "spot sign"—contrast pooling within the hematoma on delayed-phase imaging—suggests ongoing hemorrhage and is considered a predictor of hematoma and worse clinical prognosis.[1]
Cerebral amyloid angiopathy
[edit]Cerebral amyloid angiopathy (CAA) is a cerebrovascular accident disorder characterized by the deposition of amyloid beta (AB) peptide within the brain. Accumulation of such peptide proteins within the walls of the arteries can cause weakening of the walls and can increase the risk of microhemorrhages.
SAH due to CAA typically occurs in individuals over the age of 60 and can present with transient motor or sensor symptoms. Hemorrhages associated with CAA are usually localized to the lobar white matter adjacent to the cortex, sparing deeper brain structure such as the basal ganglia, brainstem, and posterior fossa. This pattern helps differentiate CAA-related hemorrhage from other causes, such as vasculitis.
Diagnosis of CAA is often based on the Boston criteria, which incorporate clinical, radiological, and histopathological findings to estimate the likelihood of CAA as the cause of hemorrhage. A definitive diagnosis requires histopathological confirmation via brain biopsy or post-mortem examination.[1]
On CT imaging, CAA-related hemorrhages appear as hyperdense lobar intra-axial bleeds, typically in subcortical regions. Diffuse with white matter hypodensities may also be observed, suggesting chronic microangiopathic changes. MRI, especially using gradient echo (GRE) and susceptibility-weighted imaging (SWI) sequences, can detect microbleeds and cortical superficial siderosis, which appear as blooming artifacts—a key imaging feature of CAA.[1]
Hemorrhagic conversion of ischemic infarction
[edit]43% of those with infarcted brain tissue will develop hemorrhagic conversion. Risk of hemorrhagic is further increased with recanalisation of veins or arteries. Several types of hemorrhages can occur such as petechial hemorrhages around the infarcted margin (HI1), confluent petechial hemorrhages within the infarcted tissue (HI2), hematoma occupying less than 30% of the infarcted tissue (PH1), hematoma involving greater than 30% of infarcted tissue with small mass effect (PH2), and hematoma involving greater than 30% of the infarcted tissue with significant mass effect. However, only PH2 is clinically significant.[1] Those who has infarction should be monitored frequently with CT brains to access hemorrhagic conversions or worsening vasogenic oedema that may require neurosurgical decompression.[1] Dual energy CT scan maybe useful to differentiate the high densities caused by reperfusion hemorrhage (bleeding after endovascular stroke treatment) and high density due to iodinated contrast administered during cerebral angiography.[1]
Cerebral aneurysm
[edit]Besides from head injury, it may occur spontaneously, usually from a ruptured cerebral aneurysm (focal outpouchings with weakened walls on the arteries on the brain surface that are prone to rupture).[1] Symptoms of SAH include a severe headache with a rapid onset (thunderclap headache), vomiting, confusion or a lowered level of consciousness, and sometimes seizures.[12] CT scan has 100% sensitivity of detecting SAH at 6 to 24 hours after symptoms onset.[1] The diagnosis is generally confirmed with a CT scan of the head. If CT scan is normal but SAH is still strongly suspected, lumbar puncture can be done at six to twelfth hours after the onset of headache. This is to determine the presence of blood within the cerebrospinal fluid (CSF). Those with SAH will have blood and bilirubin within their CSF because of the degradation of their red blood cells. Meanwhile, those who has blood within CSF due to traumatic lumbar puncture will not have bilirubin within CSF.[12] SAH is generally located within basal cisterns, extends diffusely to all subarachnoid spaces (cerebral sulci) or into the ventricular system, or brain parenchyma. Modified Fisher scale is used to describe the volume and distribution of SAH, just predicting the probability of cerebral artery vasospasm after SAH.[1]
Treatment is by prompt neurosurgery or radiologically-guided interventions with medications and other treatments to help prevent recurrence of the bleeding and complications. Since the 1990s, many aneurysms are treated by a minimal invasive procedure known as endovascular coiling, which is carried out by instrumentation through large blood vessels. However, this procedure has higher recurrence rates than the more invasive craniotomy with clipping.[12]
Cerebral ateriovenous malformation
[edit]Cerebral ateriovenous malformation (Cerebral AVM) is characterised by abnormal shunting between cerebral arteries and veins without going through capillaries. Instead the blood goes through a collection of small vessels from arteries to veins. These collection of abnormal small vessels is termed as "nidus". This condition happens in 0.1% of the population has a risk of 2 to 4% per year for intracranial bleeding. Once ruptured, it results in intraparenchymal hemorrhage, intraventricular hemorrhage and SAH. Rupture of cerebral AVM often occurs in young people and children. Cerebral AVM can be diagnosed by computed tomography angiography (CTA) brain, magnetic resonance angiography (MRA) brain, or digital subtraction angiography (DSA). DSA is important to determine whether there is nidal or perinidal aneurysm.[1]
Dural arteriovenous fistulae
[edit]Dural arteriovenous fistulae (DAVF) is the direct connection between dural or cerebral arteries with dural venous sinuses or cortical veins. It accounts for 10 to 15% of intracranial arteriovenous shunts. DAVF lacks a nidus. Signs and symptoms of DAVF are: headache, tinnitus, neurological deficits involving cranial nerves, and increased intracranial pressure. DAVF once ruptured, will produce intraparenchymal hemorrhage or SAH. Increase in number of vessels near dural venous sinuses as seen on CTA is suggestive of DVAF. 4DCT may increase the sensitivity of detecting DAVF.[1] In MRI scans, susceptibility weighted imaging (SWI) and arterial spin labelling sequences (labelling protons in blood without the use of contrast media to determine blood flow) are useful in evaluating DAVF. The patterns of draining veins from the fistula determines the risk of DAVF rupture. Increased pressure within the dural venous sinuses causes backpressure into the cortical veins, thus making cortical veins more prone to rupture. The risk of hemorrhage is graded by Cognard and Borden grading systems. These grading systems are based upon the DSA.[1]
Cortical venous and cerebral venous sinus thrombosis
[edit]Dural venous sinus thrombosis (DVST) and cortical venous thrombosis (CVT) commonly presents with headache, increased intracranial pressure, or seizures. DVST is more common than CVT. DVST are frequently caused by infections in the skull base, dehydration, thrombophilia, meningioma, and other dural tumours.[1] On CT scans, brain parenchymal hemorrhage that does not confined to specific arterial territory along with hyperdense appearance on dural venous sinuses raises the suspicion of DVST. Further evaluation with CT venography, MR venography, and post gadolinium MRI provides accurate diagnosis of venous thrombosis and follow-up after treatment. These studies demonstrate thrombus as filling defect or lack of signal.[1]
Vasculitis and vasculopathy
[edit]Those with vasculitis may be presented with headache, behavioural changes, neurological deficits, or intracranial bleeding. Sulcal SAH is the most common form of intracranial bleed caused by vasculitis. On CT scans, sulcal SAH is seen as hyperdensity within the cerebral sulcus, while on MRI, it is seen as hyperintensity on FLAIR sequence, and hypointensity on GRE/SWI sequence. DSA is important in making the diagnosis of vasculitis or vasculopathy.[1]
Mycotic aneurysm
[edit]It is arterial outpouchings arise from distal cerebral arteries. These are pseudoaneurysm, caused by thrombus clogging the distal arteries, which results in inflammation and small tears at the site of occlusion. These inflammation and thrombis can caused by infective endocarditis, artificial heart valve or other heart problems. Similar to vasculitis, rupture of mycotic aneurysm also causes SAH in cerebral sulci, mostly located in the vertex. If mycotic aneurysm is located more proximally, it will produce diffuse SAH pattern. CTA or MRA would produce focal outpouching or increase in diameter of the vessel. Meanwhile, GRE/SWI MRI sequence would produce focal hypointensity. Small mycotic aneurysms are difficult to be seen on CT or MRI. Thus, DSA is useful in identifying these lesions.[1]
Management
[edit]For those who is already on blood thinners such as aspirin or clopidogrel for prevention of myocardial infarction or stroke, traumatic intracranial hemorrhage should prompt the use of platelet function assays (PFA-100) to assess the effect of these antiplalelet agents. After that, plateletpheresis can be started to increase the aggregation of platelets, thus stopping the intracranial bleed. In those with impaired kidney functions, desmopressin or cryoprecipitate can be used instead.[13]
From limited observational data, it may be relatively safe to restart blood thinners after an ICH as it is associated with reduced thromboembolic complications with similar risk of recurrent hemorrhage when compared to those did not start blood thinners after an ICH.[14]
Comparison
[edit]| Compared quality | Epidural | Subdural |
|---|---|---|
| Location | Between the skull and the inner meningeal layer of the dura mater or between outer endosteal and inner meningeal layer of dura mater | Between the meningeal layers of dura mater and the Arachnoid mater |
| Involved vessel | Temperoparietal locus (most likely) – Middle meningeal artery Frontal locus – anterior ethmoidal artery Occipital locus – transverse or sigmoid sinuses Vertex locus – superior sagittal sinus |
Bridging veins |
| Symptoms (depending on the severity)[15] | Lucid interval followed by unconsciousness | Gradually increasing headache and confusion |
| CT scan appearance | Biconvex lens | Crescent-shaped |
References
[edit]- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac Caceres, J. Alfredo; Goldstein, Joshua N. (2013-08-01). "Intracranial hemorrhage". Emergency Medicine Clinics of North America. 30 (3): 771–794. doi:10.1016/j.emc.2012.06.003. ISSN 1558-0539. PMC 3443867. PMID 22974648.
- ^ a b c d e Naidich, Thomas P., ed. (2013). Imaging of the brain. Expert radiology series. Philadelphia: Saunders/Elsevier. ISBN 978-1-4160-5009-4. OCLC 820170496.
- ^ a b c d e f Fernando, Shannon M.; Qureshi, Danial; Talarico, Robert; Tanuseputro, Peter; Dowlatshahi, Dar; Sood, Manish M.; Smith, Eric E.; Hill, Michael D.; McCredie, Victoria A.; Scales, Damon C.; English, Shane W.; Rochwerg, Bram; Kyeremanteng, Kwadwo (2021-05-09). "Intracerebral Hemorrhage Incidence, Mortality, and Association With Oral Anticoagulation Use: A Population Study". Stroke. 52 (5): 1673–1681. doi:10.1161/STROKEAHA.120.032550. ISSN 0039-2499. PMID 33685222.
- ^ a b c d Imoisili, Omoye E.; Chung, Alina; Tong, Xin; Hayes, Donald K.; Loustalot, Fleetwood (2024-05-23). "Prevalence of Stroke — Behavioral Risk Factor Surveillance System, United States, 2011–2022". MMWR. Morbidity and Mortality Weekly Report. 73 (20): 449–455. doi:10.15585/mmwr.mm7320a1. ISSN 0149-2195. PMC 11115433. PMID 38781110.
- ^ a b c d e Rajashekar, Devika; Liang, John W. (2025), "Intracerebral Hemorrhage", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31971743, retrieved 2025-05-08
- ^ a b c d e f g Schweitzer AD, Niogi SN, Whitlow CT, Tsiouris AJ (October 2019). "Traumatic Brain Injury: Imaging Patterns and Complications". Radiographics. 39 (6): 1571–1595. doi:10.1148/rg.2019190076. PMID 31589576. S2CID 203926019.
- ^ a b c d e Tenny, Steven; Das, Joe M.; Thorell, William (2025), "Intracranial Hemorrhage", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29262016, retrieved 2025-05-09
- ^ a b Heit, Jeremy J.; Iv, Michael; Wintermark, Max (2016-12-12). "Imaging of Intracranial Hemorrhage". Journal of Stroke. 19 (1): 11–27. doi:10.5853/jos.2016.00563. ISSN 2287-6391. PMC 5307932. PMID 28030895.
- ^ Halefoglu, Ahmet Mesrur; Yousem, David Mark (2018-04-28). "Susceptibility weighted imaging: Clinical applications and future directions". World Journal of Radiology. 10 (4): 30–45. doi:10.4329/wjr.v10.i4.30. ISSN 1949-8470. PMC 5971274. PMID 29849962.
- ^ Kushner D (1998). "Mild traumatic brain injury: toward understanding manifestations and treatment". Archives of Internal Medicine. 158 (15): 1617–1624. doi:10.1001/archinte.158.15.1617. PMID 9701095.
- ^ a b Ziu, Endrit; Khan Suheb, Mahammed Z.; Mesfin, Fassil B. (2025), "Subarachnoid Hemorrhage", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 28722987, retrieved 2025-05-09
- ^ a b c van Gijn J, Kerr RS, Rinkel GJ (January 2007). "Subarachnoid haemorrhage". Lancet. 369 (9558): 306–318. doi:10.1016/S0140-6736(07)60153-6. PMID 17258671. S2CID 29126514.
- ^ "Antiplatelet agent reversal in adults with traumatic intracranial haemorrahge" (PDF). Department of Surgical Education at Orlando Regional Medical Center. Archived from the original (PDF) on 18 June 2022. Retrieved 26 June 2022.
- ^ Murthy SB, Gupta A, Merkler AE, Navi BB, Mandava P, Iadecola C, et al. (June 2017). "Restarting Anticoagulant Therapy After Intracranial Hemorrhage: A Systematic Review and Meta-Analysis". Stroke. 48 (6): 1594–1600. doi:10.1161/STROKEAHA.116.016327. PMC 5699447. PMID 28416626.
- ^ McDonough VT, King B. "What's the Difference Between a Subdural and Epidural Hematoma?" (PDF). BrainLine. WETA-TV. Archived from the original (PDF) on 21 August 2010.
Further reading
[edit]- Shepherd S. 2004. "Head Trauma." Emedicine.com.
- Vinas FC and Pilitsis J. 2004. "Penetrating Head Trauma." Emedicine.com.
- Julian A. Mattiello, M.D., Ph.D. Michael Munz, M.D. 2001. "Four Types of Acute Post-Traumatic Intracranial Hemorrhage" The New England Journal of Medicine
External links
[edit]- ^ Capodanno D (July 2018). "To unsubscribe, please click here". EuroIntervention. 14 (4): e367 – e369. doi:10.4244/eijv14i4a63. PMID 30028297.
Intracranial hemorrhage
View on GrokipediaEpidemiology
Incidence and prevalence
Intracranial hemorrhage (ICH), encompassing subtypes such as intracerebral and subarachnoid hemorrhage, has an estimated annual global age-standardized incidence of approximately 45-50 per 100,000 individuals for non-traumatic cases (intracerebral ~40, subarachnoid ~5-10), with traumatic subtypes adding to the overall burden but less commonly aggregated in global stroke data.[4][5] Updated analyses from global stroke registries between 2023 and 2025 indicate higher incidence in low- and middle-income countries, where age-standardized rates for intracerebral hemorrhage can exceed 60 per 100,000, compared to 10-20 per 100,000 in high-income settings, driven by disparities in healthcare access and risk factor management.[6] Incidence also escalates with age, particularly beyond 55 years, reflecting the cumulative impact of vascular pathologies. Incidence figures primarily reflect non-traumatic cases; traumatic ICH, such as epidural (1-5 per 100,000) and subdural, contributes additionally, often linked to head injury rates of 300-500 per 100,000 annually.[1] Among stroke subtypes, intracerebral hemorrhage constitutes approximately 25-30% of all cases worldwide (28.8% per 2021 Global Burden of Disease study, higher in low-income regions at up to 40%, versus 10-15% in high-income settings), while subarachnoid hemorrhage accounts for about 5-6%, highlighting their roles as the primary forms of hemorrhagic stroke.[5][7] These proportions are derived from large-scale epidemiological studies, with intracerebral hemorrhage showing greater variability across regions due to its strong association with hypertension. Prevalence estimates further underscore the burden, with over 16 million people living with sequelae from intracerebral hemorrhage alone in 2021.[7][8][9] Demographic trends reveal a higher incidence among males, who experience rates approximately 1.5 times those of females across most age groups, attributed to differences in risk exposure and vascular health. For non-traumatic intracranial hemorrhage, incidence peaks between ages 55 and 75, aligning with the onset of chronic conditions like hypertension. In contrast, traumatic cases exhibit a bimodal pattern, with elevated rates in young adults (typically 18-30 years) from high-impact injuries such as motor vehicle accidents and in the elderly (over 75 years) due to falls, contributing to a substantial portion of overall cases in emergency settings.[9][10][11] Recent epidemiological data indicate a decline in age-standardized incidence rates in high-income countries, largely due to enhanced hypertension screening and control programs, as evidenced by reductions of up to 30-40% since 1990. However, global absolute numbers are rising amid aging populations, with projections from 2024 analyses suggesting continued increases in low- and middle-income regions unless preventive measures expand. These trends are informed by comprehensive registries, emphasizing the need for targeted interventions in vulnerable demographics.[12][4]Mortality and morbidity
Intracranial hemorrhage (ICH) is associated with substantial mortality, with 30-day case fatality rates for spontaneous intracerebral hemorrhage typically ranging from 30% to 40%.[13] Mortality varies significantly by hematoma volume, where lesions exceeding 30 mL are linked to over 50% 30-day mortality, as established in the original intracerebral hemorrhage (ICH) score prognostic model. Among survivors of intracerebral hemorrhage, morbidity remains high, with 50% to 70% experiencing significant long-term disability, defined as a modified Rankin Scale (mRS) score of 3 to 6 at 6 months post-event.[14] Approximately 20% to 30% of these survivors require institutional long-term care due to persistent neurological deficits.[15] Mortality rates differ by subtype; traumatic epidural hematomas carry a lower risk of 5% to 10% if surgically evacuated promptly, reflecting their more favorable prognosis with rapid intervention.[16] In contrast, non-traumatic hypertensive intracerebral hemorrhages exhibit 40% to 50% 30-day mortality, driven by underlying vascular fragility and expansion risks.[17] Recent 2024 American Heart Association (AHA) performance measures for spontaneous ICH underscore persistent high morbidity from secondary brain injuries, though 1-year survival has improved to approximately 60% in cohorts benefiting from enhanced acute care protocols.[13] Early intervention, such as blood pressure control, plays a key role in mitigating these outcomes.[13]Risk factors
Modifiable risk factors
Hypertension is the most prominent modifiable risk factor for intracranial hemorrhage (ICH), with chronic elevation of systolic blood pressure (SBP) strongly linked to vascular fragility and rupture, particularly in deep brain regions. Each 10 mm Hg increase in SBP is associated with at least a 60% higher risk of ICH, and levels exceeding 160 mm Hg are associated with approximately a 3- to 4-fold higher relative risk compared to normotensive individuals. Effective blood pressure management through antihypertensive medications and lifestyle interventions can reduce the risk of recurrent ICH by approximately 50% per 10 mm Hg reduction in SBP, underscoring its role in primary prevention.[18][19] Use of anticoagulants and antiplatelet agents substantially elevates ICH risk, primarily by impairing hemostasis and exacerbating bleeding propensity in the event of vascular injury. Warfarin and direct oral anticoagulants (DOACs) increase the odds of ICH by 2- to 5-fold compared to non-users, with higher anticoagulation intensity correlating to greater hazard; dual antiplatelet therapy further doubles this risk relative to monotherapy. Risk mitigation is achievable through regular monitoring of international normalized ratio (INR) for vitamin K antagonists, adherence to reversal protocols like prothrombin complex concentrates for acute bleeds, and careful patient selection for therapy in high-risk profiles.[20] Excessive alcohol consumption and tobacco smoking are behavioral factors that heighten ICH susceptibility by promoting hypertension, endothelial dysfunction, and coagulopathy. Heavy alcohol intake, defined as more than 50 g per day (approximately 3-4 standard drinks), elevates ICH risk by 1.5- to 2-fold, with acute binge episodes (>120 g) conferring up to an 11-fold immediate hazard through induced hypertension and platelet inhibition. Smoking, particularly current use, raises ICH odds by promoting arterial stiffness and microaneurysm formation, though cessation can lower this risk progressively, approaching baseline levels within 5 years.[21][22][23] Other modifiable contributors include obesity, uncontrolled diabetes, and illicit drug use, which compound vascular stress and hemorrhagic potential. Elevated body mass index (BMI >30 kg/m²) and central adiposity increase ICH odds via associated hypertension and diabetes, with genetic studies indicating mediation through type 2 diabetes in over 50% of cases. Uncontrolled diabetes promotes microangiopathy and cerebral microbleeds, further amplifying risk. Cocaine and amphetamines, through acute sympathomimetic effects, heighten ICH incidence by 10- to 20-fold in users, especially young adults, by inducing severe hypertension and vasospasm. Recent guidelines, including the 2022 American Heart Association update, advocate routine screening for these factors and targeted interventions like weight management, glycemic control, and substance abuse treatment to mitigate ICH burden.[19][20][24]Non-modifiable risk factors
Advanced age is a significant non-modifiable risk factor for intracranial hemorrhage (ICH), with the incidence rising exponentially after age 55 and increasing 5- to 10-fold in individuals over 65 years compared to younger adults, primarily due to age-related vessel fragility and cerebral amyloid angiopathy.[25][26] In population-based studies, the annual ICH incidence escalates from approximately 2.3 per 100,000 person-years in those aged 18 to 44 years to over 147 per 100,000 in those 85 years and older, underscoring the profound impact of aging on cerebrovascular integrity.[25] Male sex confers a 1.3- to 1.5-fold higher risk of ICH compared to females, potentially influenced by hormonal differences such as lower estrogen levels in men that may offer less vascular protection.[27] Epidemiological data indicate male incidence rates of about 22.8 per 100,000 versus 18.4 per 100,000 in females, with this disparity persisting across age groups and contributing to higher overall male burden of spontaneous ICH.[28] Ethnicity also plays a key role, with higher ICH rates observed in Asian and Black populations; for instance, non-Hispanic Black individuals experience approximately twice the incidence compared to White populations, while Asians show elevated rates of 18 to 24 per 100,000 in regions like Japan and Korea versus 8 to 15 per 100,000 in Western countries.[29][7] These disparities are attributed to genetic and environmental interactions but remain evident even after adjusting for other factors.[29] A history of prior stroke or family history of vascular disease further elevates ICH risk, with prior ischemic or hemorrhagic stroke increasing the odds by 2- to 3-fold due to underlying shared vascular pathologies.[30] Family history of stroke, particularly in first-degree relatives, is associated with a 1.5- to 2-fold heightened risk, reflecting heritable components of cerebrovascular disease.[31] Genetic predispositions, such as specific apolipoprotein E (APOE) alleles, contribute to amyloid angiopathy-related ICH; the APOE ε2 allele increases hemorrhage risk in cerebral amyloid angiopathy by promoting amyloid deposition in vessel walls, while ε4 is linked to recurrent lobar hemorrhages.[32][33] These non-modifiable factors can be amplified by modifiable risks like hypertension, further compounding overall susceptibility.[25]Pathophysiology
Mechanisms of hemorrhage
Intracranial hemorrhage arises primarily from the rupture of cerebral blood vessels, leading to blood extravasation into the brain parenchyma, ventricles, or subarachnoid space. In traumatic cases, the mechanism involves mechanical forces that cause shearing or stretching of vessels as the brain moves relative to the skull during impact.[1] This motion disrupts the integrity of arteries, veins, and bridging vessels, resulting in immediate vessel wall tears and bleeding.[34] In non-traumatic, spontaneous hemorrhage, vessel rupture often stems from structural weaknesses; chronic hypertension promotes the formation of microaneurysms known as Charcot-Bouchard aneurysms in small penetrating arteries, which weaken under sustained high pressure and eventually burst.[35] Similarly, cerebral amyloid angiopathy involves amyloid-beta deposition in vessel walls, particularly in cortical and leptomeningeal arteries, eroding the structural support and predisposing to rupture.[36] Disruption of the coagulation cascade further contributes to hemorrhage initiation and propagation by impairing hemostasis. In spontaneous intracerebral hemorrhage, underlying coagulopathies—such as those from anticoagulant use, liver disease, or inherited deficiencies—create an imbalance that hinders clot formation, allowing unchecked extravasation.[37] Platelets play a critical role in primary hemostasis by adhering to the damaged endothelium and aggregating to form a plug, but deficiencies or dysfunction prevent this initial seal.[38] Secondary hemostasis relies on the coagulation cascade, where activated factors culminate in fibrin polymerization to stabilize the clot; failures here, often due to factor shortages or inhibitors, lead to inadequate fibrin mesh formation and persistent bleeding.[37] Following the initial rupture, hematoma expansion exacerbates the injury through dynamic growth in the first few hours. Studies indicate that hematoma volume can increase by 20-40% within the initial 6 hours post-hemorrhage, driven by ongoing active bleeding from unstable vessels and the development of perihematomal edema.[39] This expansion reflects continued extravasation and fluid accumulation around the hematoma, amplifying mass effect and tissue damage.[40] Biomechanical factors, particularly shear stress, influence vessel vulnerability across both traumatic and spontaneous hemorrhages. In trauma, rapid acceleration-deceleration forces generate high shear stresses on vessel walls, promoting rupture in susceptible areas like perforating arteries.[41] For aneurysmal hemorrhages, localized low wall shear stress at bifurcation sites fosters endothelial dysfunction and wall thinning, increasing rupture risk.[42] Recent 2024 research underscores perihematomal inflammation as a key driver in this process, where inflammatory mediators exacerbate vessel permeability and contribute to secondary edema around the hematoma.[43]Secondary brain injury
Secondary brain injury in intracranial hemorrhage refers to the progressive damage occurring after the initial bleed, driven by a cascade of pathophysiological processes that amplify neuronal loss and tissue destruction beyond the primary hematoma. This phase involves mechanical, biochemical, and inflammatory mechanisms that can significantly worsen outcomes if not addressed.[36] Elevated intracranial pressure (ICP) is a key contributor to secondary injury, arising from the mass effect of the expanding hematoma, which compresses surrounding brain tissue and can lead to herniation syndromes. Sustained ICP above 20 mm Hg impairs cerebral perfusion and exacerbates ischemia, with studies showing its presence in up to 70% of monitored intracerebral hemorrhage (ICH) patients. Clinical manifestation often includes Cushing's triad—hypertension, bradycardia, and irregular respirations—signaling brainstem compression and impending herniation.[24][44][45] Perihematomal edema (PHE) further aggravates mass effect, forming around the hematoma due to both cytotoxic and vasogenic mechanisms. Cytotoxic edema predominates early, resulting from cellular energy failure and ion pump dysfunction in the first hours post-bleed, while vasogenic edema emerges later from blood-brain barrier (BBB) permeability, peaking between days 3 and 5 and contributing substantially to the overall lesion volume—often approaching or exceeding the hematoma size itself. This edema expansion can double the effective mass effect, promoting midline shift and secondary ischemia.[46][47][48] Compression of adjacent tissue by the hematoma and edema creates an ischemic penumbra-like zone, where hypoperfusion leads to secondary infarction despite preserved viability in some areas. This region experiences reduced blood flow from mechanical compression, compounded by excitotoxicity from glutamate release—derived from neuronal stress and cell death—which overactivates NMDA receptors and triggers calcium influx, mitochondrial dysfunction, and apoptotic pathways. Additionally, erythrocyte lysis releases hemoglobin, leading to iron-mediated oxidative stress, and thrombin from the coagulation cascade induces neuroinflammation and BBB disruption. Elevated extracellular glutamate levels have been documented in perihematomal tissue, correlating with expanded infarct zones.[24][49][50] Systemic inflammatory responses amplify these local effects, with cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) driving neuroinflammation and further BBB breakdown. These pro-inflammatory mediators, released by activated microglia and infiltrating leukocytes, promote vasogenic edema and neuronal apoptosis, with peripheral blood levels elevated in ICH patients. Recent 2025 studies highlight neuroinflammation as a therapeutic target, showing that modulating microglial polarization reduces cytokine-driven injury and improves outcomes in preclinical models. BBB disruption facilitates leukocyte influx and toxin entry, perpetuating a vicious cycle of edema and ischemia.[51][52]Signs and symptoms
General presentation
Intracranial hemorrhage typically presents with a sudden onset of severe headache, often described as the worst headache of one's life, accompanied by nausea and vomiting due to elevated intracranial pressure (ICP).[2] This headache is reported in approximately 33-44% of cases and can manifest as a thunderclap headache—reaching maximum intensity within seconds to minutes—particularly in subarachnoid hemorrhage (occurring in about 50% of such cases), though it is less common in other hemorrhage types.[53][54] Nausea and vomiting occur in 30-50% of patients, reflecting meningeal irritation or ICP elevation, and are more pronounced in acute presentations.[53] Altered mental status is a hallmark feature, ranging from mild confusion or lethargy to deep coma, with approximately 50% of patients exhibiting some impairment in level of consciousness at presentation.[53] The Glasgow Coma Scale (GCS) score is less than 13 in about 60% of cases, indicating moderate to severe neurological compromise and correlating with poorer prognosis.[55] These changes often develop abruptly as blood accumulates, compressing vital brain structures. Focal neurological deficits, such as hemiparesis or aphasia, affect 10-40% of patients and may appear progressively, while seizures occur in 6-15% at or near onset, potentially exacerbating brain injury.[53][56] Vital sign abnormalities, including hypertension (systolic blood pressure >180 mmHg in many cases), are common and reflect autonomic dysregulation from ICP rise or underlying vascular pathology.[2] The condition frequently progresses with rapid neurological deterioration over minutes to hours due to hematoma expansion and secondary edema, though analyses indicate that about 30% of patients initially present with mild symptoms (e.g., NIHSS ≤5) before worsening.[57] While core features are shared, symptom intensity can vary by hemorrhage location, such as deeper deficits in lobar versus basal ganglia bleeds.[58]Location-specific features
The symptoms of intracranial hemorrhage vary significantly based on its anatomical location, influencing the pattern of neurological dysfunction. Extra-axial hemorrhages, such as epidural and subdural types, classically feature a lucid interval after initial injury, during which the patient regains consciousness briefly before experiencing rapid deterioration due to mass effect from the accumulating blood.[1] This progression often manifests as focal neurological deficits, including hemiparesis or pupillary abnormalities, as the hematoma compresses adjacent brain tissue.[59] In contrast, intra-axial parenchymal hemorrhages typically exhibit a more gradual onset over minutes to hours, evolving into deep coma and global impairments like quadriparesis, especially when involving the brainstem.[60][61] Such deficits arise from direct disruption of deep neural pathways and secondary edema, leading to widespread motor and sensory loss.[2] Subarachnoid hemorrhage provokes meningeal irritation from blood in the subarachnoid space, commonly causing neck stiffness, photophobia, and severe headache.[62] Additionally, blood within the cerebrospinal fluid can obstruct pathways, resulting in hydrocephalus with symptoms of elevated intracranial pressure.[1] Intraventricular hemorrhage frequently induces acute obstructive hydrocephalus by blocking cerebrospinal fluid flow, presenting with signs of increased intracranial pressure such as bradycardia and the Cushing response (hypertension accompanied by bradycardia and irregular respirations).[1][63] These location-specific manifestations may overlap with nonspecific symptoms like headache and vomiting seen across hemorrhage types.[2]Diagnosis
Clinical evaluation
The clinical evaluation of suspected intracranial hemorrhage (ICH) begins with a detailed history to identify key risk factors and onset characteristics. Patients often report a sudden onset of severe headache, vomiting, or altered mental status, distinguishing ICH from more gradual ischemic events. Inquiry into recent trauma, anticoagulant or antiplatelet use, and underlying conditions such as hypertension is essential, as these influence management and prognosis. The National Institutes of Health Stroke Scale (NIHSS) is routinely applied to quantify neurological deficits, providing a standardized score from 0 to 42 that correlates with ICH severity, hematoma volume, and outcomes like 30-day mortality and functional recovery.[64][65] Physical examination focuses on rapid assessment of neurological function and vital signs to detect herniation or increased intracranial pressure (ICP). Key findings include pupillary asymmetry or dilatation, which may indicate brainstem compression; motor testing for hemiparesis, posturing, or flaccidity; and inspection for external signs of trauma such as scalp lacerations or Battle's sign. Glasgow Coma Scale (GCS) evaluation, ranging from 3 to 15, gauges level of consciousness and is integral to prognostic tools. Vital sign monitoring reveals signs of elevated ICP, including Cushing's triad of hypertension, bradycardia, and irregular respirations, alongside reduced consciousness or cranial nerve palsies.[1][63][66] Prognostication employs the ICH Score, a validated tool predicting 30-day mortality (0% for score 0 to 100% for score 6) based on five components: GCS (3-4 points: 2; 5-12: 1; 13-15: 0), age ≥80 years (1 point), infratentorial location (1 point), ICH volume ≥30 mL (1 point), and intraventricular hemorrhage extension (1 point). These latter elements require initial imaging confirmation but are incorporated post-acquisition for bedside risk stratification. The NIHSS complements this by forecasting functional outcomes with accuracy comparable to the ICH Score.[55][67] Differential diagnosis prioritizes distinguishing ICH from ischemic stroke, which may present with similar focal deficits but lacks thunderclap headache, and seizures, which occur in up to 10.6% of ICH cases versus 8.6% in ischemic stroke and can mimic motor symptoms. Clinical clues include agitation or vomiting more common in hemorrhage, though urgent neuroimaging is needed for definitive separation.[68][69] Prehospital protocols, per the 2022 American Heart Association/American Stroke Association guidelines, emphasize rapid transport to comprehensive stroke centers capable of neurosurgical intervention, with avoidance of hypotension (systolic blood pressure <90 mm Hg) or extreme hypertension to prevent secondary injury. Regional systems should facilitate early ICH identification and stabilization en route.[24]Imaging techniques
Non-contrast computed tomography (CT) serves as the gold standard for initial diagnosis of acute intracranial hemorrhage due to its widespread availability, rapid acquisition, and high sensitivity in the hyperacute phase.[70] Non-contrast CT has nearly 100% sensitivity for detecting acute hemorrhage in the hyperacute phase, particularly for intraparenchymal bleeds, with sensitivity for subarachnoid hemorrhage approximately 98% when performed within 6 hours and exceeding 90% within 24 hours.[71] Acute blood appears hyperdense on non-contrast CT scans, typically with Hounsfield unit (HU) values ranging from 40 to 90, allowing reliable detection of parenchymal, subarachnoid, subdural, and epidural hemorrhages.[72] Follow-up non-contrast CT is essential for monitoring hematoma expansion, which occurs in up to 40% of cases within the first 24 hours, guiding decisions on interventions like reversal of anticoagulation.[70] If non-contrast CT is negative but suspicion for subarachnoid hemorrhage remains high (e.g., thunderclap headache within 6 hours of onset), lumbar puncture is recommended to detect xanthochromia or blood in the cerebrospinal fluid (CSF).[24] Magnetic resonance imaging (MRI) complements CT by providing superior characterization of hemorrhage chronicity, etiology, and subtle features not visible on CT. Gradient-echo (GRE) T2*-weighted sequences are particularly sensitive for detecting cerebral microbleeds, appearing as small hypointense foci due to magnetic susceptibility effects from hemosiderin deposition, with detection rates improved by susceptibility-weighted imaging (SWI) variants.[73] Fluid-attenuated inversion recovery (FLAIR) sequences excel at identifying subarachnoid hemorrhage as hyperintense signal in the cerebrospinal fluid spaces, offering higher sensitivity than CT in subacute stages.[74] MRI is especially valuable for chronic hemorrhages, where blood evolves to isointense or hypointense signals on T1- and T2-weighted images, and for detecting underlying cerebral amyloid angiopathy through patterns of lobar microbleeds.[75] CT angiography (CTA) and MR angiography (MRA) are critical for identifying vascular causes of non-traumatic intracranial hemorrhage, such as aneurysms and arteriovenous malformations (AVMs). CTA demonstrates high sensitivity (up to 92%) for detecting aneurysms greater than 3 mm and associated AVM nidi as tangled vascular structures with early venous drainage.[76] MRA provides comparable accuracy for AVMs and aneurysms without ionizing radiation, though CTA is preferred in acute settings for its speed.[77] MR venography (MRV) or CT venography (CTV) is indicated when cerebral venous thrombosis is suspected, revealing filling defects in dural sinuses or veins, with MRV considered the noninvasive reference standard.[78] Advanced imaging techniques enhance prognostic assessment and guide therapy in select cases. Perfusion imaging via CT or MR assesses the ischemic penumbra surrounding the hematoma, identifying hypoperfused but viable tissue at risk of secondary injury, with mismatch between perfusion deficit and diffusion restriction indicating potential salvageable regions.[79] Recent advancements in dual-energy CT (DECT), as of 2024, enable material decomposition to differentiate hematoma age and composition, distinguishing acute hyperdense blood (iodine map negative) from subacute or contrast staining (positive iodine overlay), with diagnostic accuracy exceeding 95% for post-thrombectomy hemorrhage prediction.[80] These techniques integrate with clinical evaluation to refine management, such as selecting patients for minimally invasive evacuation.[81]Traumatic
Hemorrhagic parenchymal contusion
Hemorrhagic parenchymal contusion refers to focal bruising of the brain tissue accompanied by bleeding, resulting from direct traumatic damage to small vessels within the parenchyma.[82] This injury typically arises from coup-contrecoup mechanisms, where acceleration-deceleration forces cause the brain to impact against the skull, producing contusions at the site of impact (coup) and the opposite side (contrecoup).[83] Such forces are common in high-velocity trauma, like motor vehicle accidents or falls, and contusions frequently occur in the frontal and temporal lobes due to the brain's anatomy and the irregular surfaces of the skull base.[84] On imaging, these contusions appear as irregular, patchy areas of hemorrhage, often measuring less than 3 cm in diameter and occurring as multiple lesions in a single patient.[85] They primarily involve the cortical grey matter and adjacent subcortical white matter, with hyperdense blood on initial CT scans.[82] Over the first few days, contusions evolve through hemorrhagic expansion, followed by surrounding edema and eventual tissue liquefaction, leading to necrosis and resorption of the hematoma.[86] This progression can occur in up to 75% of cases, contributing to clinical deterioration.[87] Associated complications include perilesional edema, which exacerbates mass effect, and secondary ischemia from vascular compression or blood toxicity to neurons.[82] Hemorrhagic parenchymal contusions occur in 20-30% of patients with severe traumatic brain injury, representing a significant contributor to morbidity.[88] Unlike diffuse axonal injury, which involves widespread microscopic shearing without prominent focal bleeding, contusions are macroscopically visible focal lesions with hemorrhagic components.[89] Management is primarily supportive, focusing on intracranial pressure control, seizure prophylaxis, and reversal of coagulopathy to prevent expansion.[82] Surgical intervention, such as craniotomy for hematoma evacuation, is reserved for cases with significant mass effect causing herniation or refractory hypertension.[90]Cerebral microhemorrhage
Cerebral microhemorrhages, also known as traumatic microbleeds, are defined as small, punctate hypointense foci less than 5 mm in diameter, visible on T2*-weighted gradient-recalled echo or susceptibility-weighted MRI sequences, representing hemosiderin deposits from acute or chronic leakage of blood from small vessels.[73] These lesions arise primarily in the context of traumatic brain injury (TBI), where mechanical shear forces during acceleration-deceleration events stretch and rupture the walls of small perforating arteries and veins, leading to extravasation of red blood cells into the surrounding brain tissue.[91] In moderate TBI, such microhemorrhages are identified in approximately 47% of cases, often co-occurring with diffuse axonal injury and serving as an indicator of widespread microvascular disruption.[92] As markers of diffuse vascular injury, cerebral microhemorrhages reflect underlying endothelial damage and blood-brain barrier compromise, which can exacerbate secondary brain injury through inflammation and edema.[91] Their presence, particularly in greater numbers, is associated with poorer functional outcomes following TBI, including increased disability and cognitive impairment, independent of lesion location or overall injury severity.[93] In patients with acute ischemic stroke who have a history of trauma-related microhemorrhages, a burden exceeding 5 lesions significantly elevates the risk of symptomatic intracerebral hemorrhage after intravenous thrombolysis, with odds ratios indicating up to a twofold increase in hemorrhagic complications.[94] Detection of these microhemorrhages relies on advanced MRI techniques, such as susceptibility-weighted imaging, which enhances sensitivity compared to conventional sequences.[73] Recent research from 2025 has further linked cerebral microhemorrhages to the early neuropathological changes underlying chronic traumatic encephalopathy (CTE) in athletes exposed to repetitive head impacts, such as in football, where microhemorrhages correlate with neuronal loss and tau pathology in sulcal depths even before overt CTE symptoms emerge.[95] These findings underscore the role of cumulative microvascular trauma in long-term neurodegeneration among contact-sport participants.[96]Epidural hemorrhage
An epidural hemorrhage, also known as an epidural hematoma, is a type of traumatic intracranial hemorrhage characterized by bleeding into the potential space between the dura mater and the inner table of the skull, typically forming a lens-shaped collection of blood.[16] It most commonly results from arterial rupture, leading to rapid accumulation of blood under arterial pressure, which can cause significant mass effect on the brain.[3] This condition accounts for approximately 8% to 19% of cases in patients with traumatic brain injury requiring evaluation.[97] The primary cause is trauma, with about 90% of cases involving laceration of the middle meningeal artery due to an overlying temporal or temporoparietal skull fracture from high-impact head injury, such as falls, motor vehicle accidents, or assaults.[16] Less frequently, venous sources like dural sinuses may contribute, but arterial etiology predominates, resulting in swift hematoma expansion.[3] Risk factors include activities that increase head trauma likelihood, such as contact sports or motorcycling without helmets, as well as anticoagulant use that exacerbates bleeding.[3] Clinically, patients often experience a classic progression: brief loss of consciousness at the time of injury, followed by a lucid interval lasting minutes to hours (observed in 14% to 21% of cases), during which the individual appears neurologically intact before rapid deterioration due to expanding hematoma and rising intracranial pressure.[16] Symptoms during decompensation include severe headache, vomiting, confusion, hemiparesis, and pupillary dilation, signaling impending herniation; these reflect general signs of elevated intracranial pressure such as Cushing's triad (hypertension, bradycardia, irregular respirations).[16] Diagnosis relies on urgent neuroimaging, with noncontrast computed tomography (CT) as the gold standard, revealing a hyperdense, biconvex (lentiform) extra-axial collection that does not cross cranial suture lines due to dural attachments.[16] The "swirl sign" on CT indicates active bleeding and active extravasation, correlating with poorer outcomes if present.[16] Midline shift is often absent in early stages but develops with larger volumes; hematoma size is quantified using the ABC/2 method on CT slices.[16] Magnetic resonance imaging (MRI) may be adjunctive but is less practical in acute trauma settings.[98] Treatment is primarily surgical, with urgent craniotomy and hematoma evacuation recommended for significant lesions to prevent irreversible brain damage from compression.[16] Indications for surgery include hematoma volume exceeding 30 mL, thickness greater than 15 mm, midline shift over 5 mm, or clinical signs of herniation such as Glasgow Coma Scale score below 9 with anisocoria.[16] Conservative management with close neurological monitoring and serial imaging is appropriate for smaller, asymptomatic hematomas (volume under 30 mL, no deficits, GCS above 8), though immediate neurosurgical consultation is essential.[98] In patients on anticoagulants, reversal agents like vitamin K or fresh frozen plasma are administered concurrently.[98]Subdural hemorrhage
Subdural hemorrhage, also known as subdural hematoma, refers to a crescent-shaped collection of blood in the subdural space between the dura mater and the arachnoid membrane, typically resulting from traumatic tearing of bridging veins that span the subdural space.[99] These veins are particularly vulnerable in the context of head trauma, where acceleration-deceleration forces cause them to rupture, leading to bleeding that accumulates over the brain's convexities.[100] In the elderly, even minor trauma can precipitate this due to age-related brain atrophy, which stretches and weakens the bridging veins, increasing their susceptibility to shear injury.[101] Subdural hemorrhages are classified based on the time from injury to symptom onset and their appearance on computed tomography (CT) imaging. Acute subdural hemorrhages develop within 3 days of trauma and appear hyperdense on CT due to fresh blood.[102] Subacute forms occur between 3 and 21 days post-injury, showing mixed density as the blood begins to liquefy.[103] Chronic subdural hemorrhages form beyond 3 weeks, presenting as hypodense collections from organized, liquefied blood products.[102] In traumatic brain injury (TBI), subdural hemorrhage accounts for 20-30% of cases, particularly in severe injuries, with mortality rates reaching 50-90% in acute severe instances due to associated brain herniation and secondary insults.[104] The elderly population is disproportionately affected, as cerebral atrophy enlarges the subdural space, allowing greater blood accumulation before symptoms manifest, often delaying diagnosis.[105] Radiographic and clinical features include mass effect from the hematoma, leading to midline shift as the expanding collection compresses the underlying brain tissue.[106] In chronic cases, neomembrane formation around the hematoma can entrap and compress cortical veins, potentially causing ischemia, while hygromas—collections of cerebrospinal fluid-like effusion—may develop adjacent to or within the resolving hematoma, contributing to persistent symptoms.[107] These hemorrhages often occur in mixed injuries with contusions, complicating the clinical picture.[104] Management of subdural hemorrhage is guided by acuity and clinical stability, with surgical intervention prioritized for significant mass effect or neurological deterioration. Acute cases typically require urgent craniotomy to evacuate the hematoma, control active bleeding, and decompress the brain, especially when midline shift exceeds 5 mm.[102] For chronic subdural hemorrhages, burr hole evacuation under local or general anesthesia, often with irrigation and subdural drain placement, remains the standard, reducing recurrence rates compared to conservative approaches.[99] Recent 2024 consensus data emphasize that early surgical drainage in decompensating patients improves neurological outcomes and lowers treatment failure rates, with adjunctive techniques like middle meningeal artery embolization showing promise in reducing recurrences to as low as 4-15% when combined with surgery.[108]Traumatic subarachnoid hemorrhage
Traumatic subarachnoid hemorrhage (tSAH) results from the disruption of blood vessels within the subarachnoid space due to mechanical trauma, typically involving laceration of superficial cortical arteries or veins, or extension of bleeding from adjacent parenchymal contusions.[109] This injury pattern is a common component of traumatic brain injury (TBI), occurring in 33-60% of patients with moderate to severe TBI.[109] On non-contrast computed tomography (CT), tSAH appears as linear or sulcal hyperdensities confined to the cortical fissures or basal cisterns, distinguishing it from more diffuse patterns seen in other hemorrhages.[110] It is associated with a risk of cerebral vasospasm in 19-39% of cases, potentially leading to delayed cerebral ischemia, as well as hydrocephalus due to impaired cerebrospinal fluid absorption.[109][111] Additionally, tSAH elevates the risk of seizures compared to non-traumatic subarachnoid hemorrhage, with electrographic seizures reported in up to 12% of monitored patients.[109] Clinical presentation often includes headache and meningismus from meningeal irritation, alongside nonspecific TBI symptoms such as nausea, vomiting, or altered consciousness.[110] In the context of trauma, these features may overlap with those of basilar skull fractures.[110] Outcomes are influenced by tSAH's contribution to overall TBI severity, accounting for approximately 15% of TBI-related mortality through secondary complications like ischemia and raised intracranial pressure.[109] The Brain Trauma Foundation guidelines recommend intracranial pressure monitoring in severe TBI cases with abnormal CT findings, including tSAH, to guide management and mitigate delayed ischemia.[110] Differentiation from aneurysmal subarachnoid hemorrhage relies primarily on a clear history of trauma.[109]Non-traumatic
Hypertensive intracerebral hemorrhage
Hypertensive intracerebral hemorrhage (HICH) arises from the rupture of small penetrating arteries damaged by chronic hypertension, leading to spontaneous bleeding within the brain parenchyma. The underlying pathology involves hypertensive vasculopathy, characterized by lipohyalinosis, fibrinoid necrosis, and the formation of Charcot-Bouchard microaneurysms—microscopic saccular dilatations less than 300 μm in diameter—primarily in the lenticulostriate branches of the middle cerebral artery.[35] These microaneurysms develop due to repeated hypertensive stress causing vessel wall thinning and weakening, resulting in hemorrhage upon rupture.[112] HICH accounts for the majority of non-traumatic intracerebral hemorrhages, comprising approximately 70-90% of spontaneous cases.[113] The most frequent locations for HICH are deep brain structures, with 40-50% occurring in the basal ganglia (particularly the putamen) and 10-15% in the thalamus, reflecting the vulnerability of perforating arteries supplying these regions; combined, these sites account for 50-60% of cases.[114] Lobar hemorrhages are less common in pure hypertensive etiology, comprising about 20-50% but often involving other factors.[114] Clinical features include rapid progression with sudden onset of focal neurological deficits, headache, and altered consciousness due to mass effect and increased intracranial pressure; hematoma expansion occurs in up to 40% of cases within the first 24 hours.[2] Intraventricular extension is seen in approximately 40% of HICH, exacerbating outcomes through hydrocephalus and further neurological deterioration.[115] Key risk factors include chronic uncontrolled hypertension, particularly systolic blood pressure exceeding 180 mmHg, which promotes arteriolar damage and rupture.[24] A 2025 pooled analysis of the INTERACT trials, including the 2023 INTERACT3 study—a large randomized trial—demonstrated that early intensive blood pressure lowering (target systolic <140 mmHg within 6 hours) reduces hematoma expansion risk and improves functional outcomes, with odds ratios of 0.85 for better modified Rankin Scale scores and 0.83 for reduced mortality, especially when initiated within 3 hours of onset.[116] Demographically, HICH predominantly affects older adults over 60 years, with higher incidence in Asian populations (up to 22 per 100,000 person-years) compared to global averages of 15-20 per 100,000 annually, attributed to greater prevalence of hypertension and genetic predispositions.[117][25]Cerebral amyloid angiopathy
Cerebral amyloid angiopathy (CAA) is a cerebrovascular disorder characterized by the progressive deposition of amyloid beta (Aβ) protein in the media and adventitia of small- to medium-sized arteries in the cerebral cortex and leptomeninges, leading to vessel wall fragility and increased risk of hemorrhage.[118] This amyloid accumulation, primarily Aβ40, disrupts vascular integrity through mechanisms such as smooth muscle cell loss, basement membrane thickening, and perivascular inflammation, ultimately weakening the blood vessels and predisposing them to rupture.[119] Pathologically, CAA is graded from mild (limited Aβ in vessel walls) to severe (widespread deposition with fibrinoid necrosis and microaneurysms), and it predominantly affects cortical and leptomeningeal vessels while sparing deep perforating arteries.[120] Diagnosis of CAA relies on the Boston criteria version 2.0, which integrate clinical presentation, MRI findings, and exclusion of alternative causes to classify cases as probable or possible without requiring histopathological confirmation.[121] Key MRI features include lobar cerebral microbleeds (typically multiple and cortical), cortical superficial siderosis, and white matter perivascular spaces, which support a probable diagnosis in patients aged 50 years or older presenting with spontaneous intracerebral hemorrhage (ICH), transient focal neurological episodes, or cognitive impairment.[122] These criteria emphasize the role of susceptibility-weighted imaging to detect microbleeds, with high specificity when combined with the absence of atypical features like deep hemorrhages.[123] Clinically, CAA manifests as recurrent lobar ICH, with an estimated 30% risk of recurrence following an initial event, often involving nonhypertensive mechanisms that distinguish it from deeper vascular pathologies.[124] It is also associated with convexity subarachnoid hemorrhage (cSAH), which appears as superficial blood along the cortical surface on imaging and signals underlying vascular amyloidosis, as well as cognitive decline in approximately 50% of cases, contributing to dementia through chronic microhemorrhages and white matter injury.[125] The prevalence of CAA increases with age, affecting 5-8% of individuals over 70 years, based on autopsy and imaging studies in cognitively normal elderly populations.[126] Recent 2025 research has linked CAA severity to apolipoprotein E (APOE) ε2 and ε4 alleles, with ε4 conferring a dose-dependent risk for vascular Aβ deposition and hemorrhage, while ε2 may exacerbate lobar involvement despite some protective effects against parenchymal amyloid.[127][128] Management of CAA focuses on hemorrhage prevention and supportive care, as no disease-modifying therapies are currently approved. Anticoagulants and antiplatelet agents should be avoided or used cautiously due to their association with heightened ICH recurrence risk in affected patients.[129] Anti-amyloid monoclonal antibodies, such as lecanemab and donanemab, are FDA-approved for early Alzheimer's disease but carry substantial risks of amyloid-related imaging abnormalities (ARIA), including edema and hemorrhage, particularly in those with preexisting CAA and are generally contraindicated; clinical guidelines emphasize careful patient selection, APOE genotyping, and monitoring.[130] Overall, treatment prioritizes blood pressure control below 140/90 mmHg and multidisciplinary monitoring for cognitive and neurological symptoms.[131]Hemorrhagic transformation of ischemic stroke
Hemorrhagic transformation (HT) refers to bleeding into the infarcted brain tissue following an acute ischemic stroke, often precipitated by reperfusion therapies such as intravenous thrombolysis.[132] This secondary complication arises due to the fragility of the blood-brain barrier in ischemic areas, leading to extravasation of blood.[133] While it can occur spontaneously, the risk increases significantly with treatments like tissue plasminogen activator (tPA).[134] HT is classified into two main types based on the European Cooperative Acute Stroke Study (ECASS) criteria: hemorrhagic infarction (HI), characterized by petechial or multifocal bleeding without significant mass effect, and parenchymal hematoma (PH), which involves a space-occupying hematoma that can cause clinical deterioration due to mass effect.[135] HI is further subdivided into HI1 (small petechiae) and HI2 (confluent petechiae), while PH includes PH1 (hematoma <30% of infarcted area) and PH2 (hematoma >30% with substantial space occupation).[136] Parenchymal hematomas occur in approximately 5-10% of patients receiving tPA, compared to lower rates in untreated ischemic strokes.[134] Key risk factors for HT include large infarct size, cardioembolic stroke etiology, advanced age, and administration of thrombolytic therapy.[137] Other contributors encompass hypertension, hyperglycemia, and low levels of alpha-2-antiplasmin.[138] Predictive scores such as the HAT (Hemorrhage After Thrombolysis) score incorporate factors like age, baseline glucose, atrial fibrillation, and thrombolysis to stratify risk, aiding in clinical decision-making.[139] HT typically manifests between 24 and 72 hours after the onset of ischemia, though it can appear as early as 6 hours in reperfused cases and peak within the first 4 days.[132] Symptomatic HT, particularly PH, worsens neurological outcomes in 20-30% of affected patients, increasing mortality and disability rates due to secondary injury from mass effect and edema.[140] Prevention strategies emphasize risk stratification per American Heart Association (AHA)/American Stroke Association guidelines, which contraindicate tPA in patients with extensive infarcts (>1/3 of middle cerebral artery territory) or high-risk features to minimize HT incidence. Blood pressure management during thrombolysis (target <180/105 mmHg) and serial imaging with non-contrast CT or MRI are recommended to monitor for early signs of transformation.[141] In high-risk cases, extended thrombolysis windows are approached cautiously, with 2021 AHA updates reinforcing these limits, unchanged in subsequent reviews through 2024.[142]Aneurysmal subarachnoid hemorrhage
Aneurysmal subarachnoid hemorrhage (aSAH) is a subtype of non-traumatic intracranial hemorrhage resulting from the rupture of a saccular, or berry, aneurysm, leading to bleeding into the subarachnoid space. This condition accounts for approximately 85% of spontaneous subarachnoid hemorrhages and has an incidence of 6 to 10 cases per 100,000 population annually worldwide, with higher rates observed in certain regions such as Asia and among women.[143][144][145] Unlike traumatic subarachnoid hemorrhage, which stems from direct head injury, aSAH arises spontaneously from vascular pathology. The mortality rate remains high, at around 40-50%, primarily due to initial hemorrhage severity and secondary complications.[146] Pathologically, berry aneurysms are focal outpouchings of the arterial wall, most commonly (about 85%) located at the bifurcations of the circle of Willis, such as the anterior communicating artery, posterior communicating artery, or middle cerebral artery bifurcation. These aneurysms develop due to hemodynamic stress at branch points, leading to thinning of the media and elastic lamina, which predisposes to rupture under elevated pressure. Key modifiable risk factors include cigarette smoking, which doubles the risk through endothelial damage and promotes aneurysm formation and rupture, and hypertension, which increases wall stress and is associated with a relative risk of up to 2.5. Other contributors include female sex, age over 50, and familial history, though smoking and hypertension account for a significant attributable fraction of cases.[147][148][149][150] Clinical presentation is often dramatic, with approximately 90% of patients experiencing a sudden, severe "thunderclap" headache that reaches maximum intensity within seconds to minutes, described as the worst headache of their life. Associated symptoms may include nausea, vomiting, photophobia, neck stiffness, and loss of consciousness in up to 50% of cases. Up to 40% of patients report a preceding "sentinel" headache—a milder episode days to weeks prior—indicating a warning leak from the aneurysm, though it is often misdiagnosed. Severity is commonly assessed using the Hunt-Hess scale, which grades patients from I (asymptomatic or mild headache) to V (comatose with decerebrate posturing), with grades I-III predicting better outcomes and guiding management decisions.[151][152][153][154] Major complications include rebleeding and cerebral vasospasm. Rebleeding risk is highest immediately after rupture, at about 4% on day 1 and 1.5% per day thereafter in the first month if the aneurysm remains unsecured, contributing to up to 25% of early mortality. Vasospasm, affecting 20-30% of patients, typically occurs between days 4 and 14 post-ictus, peaking around day 7, and can lead to delayed cerebral ischemia through arterial narrowing induced by blood breakdown products in the subarachnoid space. Management prioritizes early aneurysm securing to prevent rebleeding, with endovascular coiling now preferred over surgical clipping in approximately 70-90% of suitable cases as of 2025, based on evidence from trials like ISAT showing reduced procedural morbidity, particularly for anterior circulation aneurysms. Nimodipine is standard for vasospasm prophylaxis, reducing poor outcomes by 30%.[155][156][157][158]Arteriovenous malformation
Arteriovenous malformations (AVMs) are congenital anomalies characterized by a tangled nidus of dilated, abnormal blood vessels that form direct connections between arteries and veins, bypassing the capillary bed. This high-flow shunt creates a fragile vascular structure prone to rupture, resulting in intracranial hemorrhage, which accounts for approximately 2% of all strokes but up to 20% of hemorrhagic strokes in young adults. The nidus typically consists of a compact mass of ectatic vessels, often associated with feeding arteries and draining veins, leading to localized high pressure and potential parenchymal or subarachnoid bleeding. The annual risk of hemorrhage from an untreated AVM is estimated at 2-4%, with higher rates following an initial bleed due to vessel wall weakening.[159][160] Approximately 90% of brain AVMs are located in the supratentorial region, including the cerebral hemispheres, while infratentorial locations are less common but carry a higher rupture risk. These lesions most frequently present between the ages of 20 and 40 years, often with sudden onset of severe headache, seizures, or focal neurological deficits due to hemorrhage. The first episode of bleeding is particularly devastating, with about 10% mortality and permanent disability in 40-50% of survivors, emphasizing the need for early intervention to mitigate long-term morbidity. Surgical risk assessment commonly employs the Spetzler-Martin grading system, which evaluates AVM size, eloquence of adjacent brain tissue, and pattern of venous drainage to predict perioperative complications, with grades I-II indicating low risk and IV-V high risk.[161][162] Diagnosis relies on multimodal imaging, with digital subtraction angiography (DSA) serving as the gold standard for delineating the vascular architecture, including feeder vessels, nidus, and early venous filling. Magnetic resonance imaging (MRI) complements DSA by revealing characteristic flow voids—signal losses on T2-weighted sequences due to rapid blood flow within the nidus—and associated parenchymal changes such as edema or prior hemorrhage. Noninvasive options like MR angiography or CT angiography are often initial screening tools but lack the precision of DSA for treatment planning.[163][164] Treatment strategies for AVM-associated hemorrhage aim to eliminate the nidus and prevent rebleeding, with options including endovascular embolization, stereotactic radiosurgery, and microsurgical resection, selected based on lesion grade, location, and patient factors. Embolization reduces nidal volume by occluding feeders with agents like Onyx, often as a preoperative adjunct; radiosurgery delivers focused radiation to induce gradual obliteration over 2-3 years; and resection provides immediate cure for accessible low-grade lesions. Recent 2024 studies on combined multimodal approaches, such as embolization followed by radiosurgery or surgery, demonstrate high obliteration rates (up to 90%) and substantial reductions in rebleeding risk, with one trial reporting a 70% decrease in annual hemorrhage rates compared to monotherapy. Observation may be appropriate for unruptured, low-risk AVMs, but active intervention is recommended post-hemorrhage to address the elevated 6-18% first-year rebleed risk.[159][165]Dural arteriovenous fistula
A dural arteriovenous fistula (DAVF) is an acquired vascular malformation characterized by abnormal arteriovenous shunts within the dura mater, typically involving meningeal arteries connecting directly to dural veins or sinuses, which can lead to venous hypertension, cortical venous reflux, and intracranial hemorrhage such as subarachnoid or intracerebral types.[166] Unlike parenchymal arteriovenous malformations, DAVFs arise from dural structures and are often associated with venous outflow obstruction.[167] The condition predominantly affects middle-aged adults, with a mean onset around 50-60 years, and shows a slight male predominance in some series.[166] Classification systems stratify DAVFs based on venous drainage patterns to predict hemorrhage risk, with the Borden system dividing them into three types: Type I involves antegrade drainage into a dural sinus without cortical venous reflux and is generally benign; Type II features retrograde sinus drainage with partial cortical reflux; and Type III shows direct cortical venous drainage without sinus involvement, carrying the highest risk.[167] The Cognard classification expands on this with five types, emphasizing direction of flow and reflux: Types I and IIa drain antegrade into sinuses, while Types IIb through V involve cortical venous reflux, with Type V specifically draining into spinal veins or perimedullary veins.[168] Lesions with cortical venous reflux (Borden II-III or Cognard IIb-V) are high-risk, exhibiting an annual hemorrhage rate of approximately 10% in untreated cases, which rises significantly if the fistula has previously bled.[166] The most common location for DAVFs is the transverse-sigmoid sinus junction, accounting for 40-70% of cases, often with a slight left-sided predominance, followed by the cavernous sinus, superior sagittal sinus, and tentorial regions.[169] Clinical presentation varies by location but commonly includes pulsatile tinnitus in 30-50% of patients, particularly with transverse-sigmoid involvement, due to audible arterial flow into the sinus; progressive neurological deficits from venous congestion may also occur.[166] Hemorrhagic manifestations, such as subarachnoid hemorrhage (SAH) or intracerebral hemorrhage (ICH), occur in 15-20% of cases at diagnosis and represent a severe progression driven by cortical venous hypertension.[170] Many DAVFs are idiopathic, but triggers include prior head trauma, which can disrupt dural vessels, or dural sinus thrombosis, leading to venous hypertension and neovascularization; there is notable overlap with cerebral venous thrombosis as a precipitating factor in up to 10-20% of cases.[166] Management prioritizes eliminating the arteriovenous shunt to prevent hemorrhage, with endovascular embolization as the first-line approach, achieving complete angiographic obliteration in 80-90% of cases using transarterial or transvenous routes with liquid embolic agents like Onyx or PHIL.[171] Surgical disconnection is reserved for complex or inaccessible fistulas, offering near-100% cure rates but with higher morbidity.[172] For residual or recurrent DAVFs, particularly after partial embolization, stereotactic radiosurgery (SRS) has emerged as an effective adjunct in 2025 updates, with obliteration rates of 70-85% at 2-3 years follow-up and low complication rates, especially for low-flow residuals without acute hemorrhage.[173] Observation may be considered for asymptomatic Type I lesions without reflux, given their low risk, but intervention is urgent for high-risk types presenting with hemorrhage.[167]Cerebral venous thrombosis
Cerebral venous thrombosis (CVT), also known as cerebral venous sinus thrombosis (CVST), involves the formation of a thrombus within the cerebral veins or dural venous sinuses, which obstructs venous drainage from the brain. This obstruction leads to elevated intracranial pressure, cerebral edema, venous congestion, and potentially venous infarction with associated intracranial hemorrhage. The resulting hemorrhagic complications, such as parenchymal hematomas or subarachnoid hemorrhage, arise from impaired venous outflow and rupture of fragile collaterals, distinguishing CVT from arterial hemorrhagic causes.[174][175] Pathologically, CVT is often precipitated by hypercoagulable states, including dehydration and pregnancy, which promote thrombus formation through mechanisms like endothelial damage, stasis, and increased clotting factors. The superior sagittal sinus is the most frequently involved site, accounting for approximately 60% of cases, often leading to bilateral hemispheric involvement and extensive venous infarction. In pregnancy-related CVT, additional risks such as hyperemesis gravidarum exacerbate hypovolemia and coagulopathy, contributing to sinus occlusion. The overall incidence of CVT is estimated at 1 to 2 per 100,000 individuals annually, with rates up to 3 per 100,000 in women of childbearing age due to hormonal and physiological changes.[174][176][177][178][179][180] Clinically, patients with CVT commonly present with headache in about 90% of cases, often progressive and thunderclap-like, reflecting raised intracranial pressure. Seizures occur in approximately 40% of patients, frequently as a focal or generalized manifestation of cortical irritation from venous infarcts. Hemorrhagic venous infarcts are observed in around 40% of cases on imaging, while subarachnoid hemorrhage may complicate up to 20-30% due to extension of bleeding into the subarachnoid space. Diagnosis relies on neuroimaging, with magnetic resonance venography (MRV) offering high sensitivity (up to 95%) for detecting flow voids and thrombi; the "empty delta sign" on contrast-enhanced CT venography specifically highlights non-filling of the superior sagittal sinus, confirming thrombosis.[174][181][182][183][184] Treatment of CVT prioritizes anticoagulation with unfractionated or low-molecular-weight heparin, even in the presence of intracranial hemorrhage, as it safely halts thrombus propagation and promotes recanalization, improving outcomes and reducing mortality compared to placebo. Meta-analyses indicate that heparin therapy lowers the combined risk of death or dependency by approximately 14-20% in affected patients. For severe or refractory cases, endovascular thrombectomy has emerged as a promising adjunctive therapy by 2025, particularly when anticoagulation fails, with studies showing improved recanalization rates and neurological recovery in selected cohorts.[185][184][186][187]Vasculitis and vasculopathy
Vasculitis and vasculopathy encompass inflammatory and degenerative disorders of cerebral blood vessels that can lead to non-traumatic intracranial hemorrhage through vessel wall damage, stenosis, or rupture. Primary central nervous system (CNS) vasculitis, also known as primary angiitis of the CNS (PACNS), is a rare idiopathic condition confined to the brain and spinal cord vasculature, with an estimated annual incidence of 2.4 cases per 1,000,000 population.[188] Secondary CNS vasculitis arises in the context of systemic autoimmune diseases, such as systemic lupus erythematosus (SLE) or primary Sjögren's syndrome, where immune-mediated inflammation extends to intracranial vessels, occasionally presenting with hemorrhage as an initial manifestation.[189][190] Reversible cerebral vasoconstriction syndrome (RCVS), a non-inflammatory vasculopathy, involves transient multifocal narrowing of cerebral arteries and is associated with up to 30% of cases featuring subarachnoid or intracerebral hemorrhage.[191] Clinical features of these conditions often include severe headache, which is reported in up to 63% of PACNS cases, alongside multifocal neurological deficits such as weakness, cognitive impairment, or encephalopathy due to a combination of ischemic infarcts and hemorrhagic lesions.[192][193] Intracranial hemorrhages in CNS vasculitis are typically multifocal and parenchymal, occurring in approximately 12% of PACNS presentations, though recent analyses suggest a range of 10-15% in broader cohorts including secondary forms.[194] In RCVS, hemorrhagic complications are more frequent, affecting 20-30% of patients and often coexisting with ischemic changes, leading to a severe clinical spectrum with thunderclap headaches and focal deficits.[195] Diagnosis relies on a combination of clinical suspicion and imaging, with cerebral angiography demonstrating segmental narrowing or beading in 60-90% of PACNS cases, while brain biopsy remains the gold standard, confirming vasculitis in about 70% of targeted procedures and identifying alternative diagnoses in up to 37% of cases.[196][197] For secondary vasculitis, serologic markers of underlying autoimmune disease, such as anti-SSA/SSB antibodies in Sjögren's, support the etiology alongside angiographic findings.[190] RCVS is distinguished by reversible vasoconstriction on serial angiography, typically resolving within three months.[191] Risk factors for CNS vasculitis include underlying autoimmune conditions like SLE or Sjögren's syndrome, which predispose to secondary forms through immune complex deposition in vessel walls.[198] Drug-induced triggers, particularly cocaine use, promote endothelial damage and ANCA-associated vasculitis, increasing the likelihood of hemorrhagic events via vasoconstriction and thrombosis.[199] In RCVS, precipitants such as postpartum state, vasoactive drugs, or migraines heighten susceptibility, with female sex and older age as additional modifiers for hemorrhagic subtypes.[195] Management centers on immunosuppression for inflammatory vasculitides, with high-dose glucocorticoids (e.g., prednisone 1 mg/kg/day) achieving remission in 85% of PACNS cases as monotherapy, and combination with cyclophosphamide (e.g., 2 mg/kg/day orally or intravenous pulses) yielding similar 80% response rates in severe or refractory presentations.[200] For secondary forms, treatment targets the underlying autoimmune disease, often incorporating rituximab or maintenance immunosuppressants alongside steroids.[201] RCVS management focuses on blood pressure control and avoidance of triggers, with calcium channel blockers like nimodipine used empirically, though evidence is limited to observational data.[191] Prognosis varies by type and timeliness of intervention; early immunosuppression in PACNS leads to initial remission in 95% of cases and prolonged relapse-free survival in 66%, with functional independence achieved in over 70% at long-term follow-up.[201] Untreated or delayed cases carry higher mortality (8-23%), but prompt therapy improves outcomes to favorable levels in approximately 80% of patients across cohorts.[202] Relapses occur in 25% of cases, necessitating vigilant monitoring.[203]Mycotic aneurysm
Mycotic aneurysms, also known as infectious aneurysms, represent a rare but critical cause of intracranial hemorrhage, arising from septic embolization that weakens the arterial wall. These pseudoaneurysms typically develop in the context of systemic infections, most commonly infective endocarditis caused by bacterial pathogens such as Staphylococcus aureus or Streptococcus species. Intravenous drug use is a significant risk factor, as it facilitates bacteremia and subsequent embolization to cerebral vessels, with an observed increase in incidence paralleling rising rates of injection drug abuse. They predominantly form in the distal branches of the middle cerebral artery (MCA), reflecting the embolic pathway from cardiac sources. Clinically, mycotic aneurysms often present with subarachnoid hemorrhage (SAH) or intracerebral hemorrhage (ICH) upon rupture, and they may be multiple and small in size, distinguishing them from typical saccular aneurysms. Preceding symptoms frequently include fever and systemic signs of infection, along with embolic ischemic strokes due to septic emboli lodging in cerebral arteries. In patients with infective endocarditis, the presence of these aneurysms contributes to neurological complications, with up to 25% of cases involving multiple lesions. Diagnosis relies on neuroimaging, where computed tomography angiography (CTA) or digital subtraction angiography (DSA) reveals irregular, saccular, or fusiform aneurysmal sacs with surrounding enhancement indicative of infection. Mycotic aneurysms account for 1-5% of all intracranial aneurysms overall, but their incidence rises to 2-5% among patients with infective endocarditis. Early detection is crucial, as these lesions can mimic vasculitis but are differentiated by their septic etiology and embolic history. Treatment centers on prolonged intravenous antibiotics targeted to the causative organism, combined with endovascular or surgical exclusion of the aneurysm to prevent rupture. Endovascular approaches, such as coil embolization, have gained favor for their minimally invasive nature, particularly in unruptured cases, while open surgical clipping or resection is reserved for ruptured or complex lesions. Untreated mycotic aneurysms carry a high rupture risk, with mortality exceeding 80% in some series, underscoring the need for aggressive intervention alongside infection control.Management
Initial stabilization
Initial stabilization of patients presenting with intracranial hemorrhage focuses on rapid assessment and intervention to secure vital functions, prevent secondary brain injury, and mitigate immediate risks of deterioration. Upon arrival, healthcare providers should prioritize the ABCs—airway, breathing, and circulation—while initiating continuous monitoring of vital signs, including blood pressure, to guide subsequent management.[24] Airway protection is critical, particularly in patients with depressed consciousness; endotracheal intubation is recommended for those with a Glasgow Coma Scale (GCS) score of 8 or less or a declining neurological examination to ensure adequate ventilation and prevent aspiration.[24] Oxygenation should be maintained to achieve peripheral oxygen saturation (SpO2) greater than 94% through supplemental oxygen if needed, avoiding hyperoxia which may exacerbate oxidative stress. Blood pressure monitoring begins immediately with frequent assessments, typically every 15 minutes initially, as part of hemodynamic stabilization before targeted interventions.[24] For intracranial pressure (ICP) management, elevating the head of the bed to 30 degrees promotes venous drainage and can help reduce ICP without compromising cerebral perfusion, serving as a first-line nonpharmacologic measure.[204] Temporary hyperventilation to achieve a partial pressure of arterial carbon dioxide (PaCO2) of 35-40 mmHg may be employed briefly in cases of acute herniation or refractory ICP elevation, though prolonged use risks cerebral ischemia and is not recommended routinely.[204] Routine seizure prophylaxis with antiepileptic drugs, such as levetiracetam, is not recommended for all patients with nontraumatic intracranial hemorrhage, as it does not reduce seizure incidence or improve outcomes and may increase adverse effects; however, it may be considered selectively in high-risk cases like lobar hemorrhage, with a loading dose of 1-2 g if initiated.[205] Phenytoin is generally avoided due to potential cardiovascular and cognitive side effects compared to alternatives like levetiracetam.[205] Per 2022 American Heart Association/American Stroke Association (AHA/ASA) protocols, hypoglycemia should be promptly reversed if serum glucose is below 60 mg/dL to prevent worsening neurological injury, while avoiding overly tight glycemic control that risks recurrent hypoglycemia.[24] Temperature control is essential, with pharmacologic treatment of fever (core temperature ≥37.5°C) recommended to potentially improve outcomes, as hyperthermia is associated with expanded hematoma and poorer prognosis.[24] Following these measures, management transitions to specific blood pressure control strategies to limit hematoma expansion.[24]Blood pressure control
In the acute management of intracerebral hemorrhage (ICH), blood pressure control is a cornerstone intervention aimed at reducing hematoma expansion, which occurs in up to 40% of cases and worsens outcomes. Intensive lowering of systolic blood pressure (SBP) to a target of 140 mm Hg, based on evidence from the INTERACT2 trial, has been shown to decrease the probability of significant hematoma growth by approximately 25% relative to standard targets of less than 180 mm Hg, without increasing risks of ischemia. This approach is recommended for patients with mild to moderate ICH (Glasgow Coma Scale score ≥5) and initial SBP between 150 and 220 mm Hg, with treatment initiated as early as possible, ideally within 6 hours of symptom onset. SBP targets below 130 mm Hg should be avoided to prevent cerebral hypoperfusion and ischemia.[24][206] Intravenous antihypertensive agents with rapid onset and short duration are preferred for precise titration and to minimize blood pressure variability, which is independently associated with poor outcomes. Commonly used agents include labetalol, administered as intermittent boluses starting at 10-20 mg every 10-15 minutes (up to a maximum of 300 mg), and nicardipine, given as a continuous infusion starting at 5 mg/hour and titrated by 2.5 mg/hour every 5-15 minutes to achieve the target (maximum 15 mg/hour). These agents allow for smooth, sustained control, with nicardipine favored in many centers for its ease of titration via infusion pumps. Close monitoring is essential, typically via invasive arterial line in an intensive care setting, to ensure real-time adjustments and maintain SBP within the 130-160 mm Hg range post-initial lowering.[24][207] The INTERACT3 trial further supports intensive SBP reduction to less than 140 mm Hg as part of a multifaceted care bundle, demonstrating a 29% reduction in the odds of death or major disability at 6 months compared to standard care. Recent 2025 analyses, including individual patient data meta-analyses from the INTERACT series, reinforce the benefits of early, intensive control in reducing hematoma expansion by up to 30% in select patients, particularly those eligible for advanced interventions. For subarachnoid hemorrhage (SAH), higher SBP targets (e.g., less than 160 mm Hg pre-aneurysm securing) are used to preserve cerebral perfusion, diverging from ICH protocols. This targeted blood pressure strategy integrates with initial stabilization measures to optimize early physiological control.[208]Surgical interventions
Surgical interventions for intracranial hemorrhage aim to evacuate hematomas, secure underlying vascular lesions, or relieve intracranial pressure to prevent herniation and improve outcomes. Indications for surgery include cerebellar hemorrhages exceeding 3 cm in diameter, brainstem compression, hydrocephalus, or clinical deterioration despite optimal medical management.[24] In supratentorial intracerebral hemorrhage (ICH), surgery is considered for superficial lobar clots with neurological decline, as evidenced by the STICH II trial, which demonstrated a modest reduction in unfavorable outcomes (adjusted odds ratio 0.69; 95% CI 0.47-1.01) for early surgery in select patients compared to conservative treatment.[209] Common techniques for supratentorial ICH evacuation include open craniotomy, which involves removing a bone flap to access and aspirate the hematoma but carries risks of brain retraction injury.[210] Minimally invasive approaches, such as endoscopic evacuation or stereotactic thrombolysis, reduce tissue disruption; the MISTIE III trial showed these methods achieved substantial hematoma volume reduction (median 69% at 72 hours) and lowered 30-day mortality from 17.9% in medical management to 15.0% in the surgical arm (non-significant), though overall functional recovery at one year was not significantly improved (45% vs. 41% good outcome).[211] Decompressive craniectomy, often combined with evacuation, enlarges the cranial vault to mitigate mass effect and elevated intracranial pressure, particularly in patients with midline shift greater than 5 mm or deteriorating consciousness.[24] For aneurysmal subarachnoid hemorrhage (SAH), surgical interventions focus on securing the ruptured aneurysm to prevent rebleeding and managing complications like hydrocephalus. Microsurgical clipping involves placing a titanium clip across the aneurysm neck via craniotomy, offering durable occlusion (95-98% complete occlusion rate) especially for wide-necked or posterior circulation aneurysms.[212] Endovascular coiling deploys platinum coils to promote thrombosis within the aneurysm sac, with meta-analyses showing equivalent long-term outcomes to clipping in anterior circulation cases (pooled risk ratio for mortality 0.97; 95% CI 0.82-1.15) but lower procedural morbidity in elderly patients. External ventricular drainage (EVD) is indicated for acute hydrocephalus, reducing intracranial pressure and allowing cerebrospinal fluid diversion, with early placement associated with improved Glasgow Outcome Scale scores in high-grade SAH (odds ratio 1.8; 95% CI 1.2-2.7).[212] Recent advances as of 2025 include the ENRICH trial, which supported early minimally invasive evacuation for lobar ICH using trans-sulcal parafascicular surgery, resulting in improved 180-day functional outcomes (utility-weighted modified Rankin Scale score 0.458 vs. 0.374; difference 0.084, 95% CrI 0.005-0.163) and reduced mortality (9.3% vs. 18%) compared to medical management alone. Patient selection for these interventions relies on imaging to assess hematoma volume, location, and stability.[24]Anticoagulation reversal
Anticoagulation reversal is a critical intervention in the management of intracranial hemorrhage (ICH) among patients on antithrombotic therapy, aimed at minimizing hematoma expansion and improving outcomes by rapidly restoring hemostasis. This process targets the underlying coagulopathy induced by vitamin K antagonists (VKAs), direct oral anticoagulants (DOACs), or antiplatelet agents, which are common modifiable risk factors for ICH progression. Prompt reversal, ideally within 1 hour of presentation, has been associated with reduced mortality and lower rates of hospice transfer, though it carries a risk of subsequent thromboembolic events.[213][24] For patients on warfarin or other VKAs, reversal involves administration of 4-factor prothrombin complex concentrate (PCC) at a dose of 25-50 IU/kg based on body weight and international normalized ratio (INR), combined with intravenous vitamin K (5-10 mg), to achieve an INR ≤1.4 as quickly as possible, preferably within 3 hours. PCC is preferred over fresh frozen plasma (FFP) due to faster INR normalization (median 40 minutes vs. >24 hours with FFP) and reduced hematoma expansion at 3 hours (adjusted difference of 16.9 mL less expansion with PCC). Vitamin K serves as an adjunct to sustain reversal beyond the short half-life of PCC, with repeat INR checks recommended 30 minutes post-PCC and then every 6 hours for 24-48 hours.[24][214][215] In cases of DOAC-associated ICH, specific reversal agents are recommended based on the drug class. For dabigatran (a direct thrombin inhibitor), idarucizumab (5 g IV, administered as two 2.5 g boluses no more than 15 minutes apart) provides rapid and complete reversal of anticoagulant effects, with immediate onset and normalization of activated partial thromboplastin time (aPTT). For factor Xa inhibitors such as apixaban or rivaroxaban, andexanet alfa is the preferred agent (low-dose regimen: 400 mg bolus at 30 mg/min followed by 4 mg/min infusion for up to 120 minutes; high-dose: 800 mg bolus at 30 mg/min followed by 8 mg/min infusion), achieving substantial reduction in anti-factor Xa activity (approximately 90% within 30 minutes in trials) and superior hemostatic efficacy (64% excellent or good hemostasis vs. 53% with usual care, including PCC). If andexanet is unavailable, 4-factor PCC (50 IU/kg) can be used as an alternative, though it is less effective at preventing expansion. These interventions should be initiated as soon as possible, particularly within 18 hours of the last DOAC dose, to limit hematoma growth.[24][215] Reversal of antiplatelet therapy in ICH remains controversial and is generally not recommended outside of perioperative settings. Platelet transfusion (typically 1 unit) is only advised prior to emergency craniotomy in patients on aspirin to reduce postoperative hemorrhage, with no demonstrated benefit for non-surgical cases and potential harm from increased thrombosis risk (Class III recommendation, Level B-R). For patients with aspirin, clopidogrel, or other P2Y12 inhibitors, desmopressin (0.4 mcg/kg IV) may be considered in the context of uremia-associated platelet dysfunction to enhance hemostasis, though evidence is limited. Platelet function typically recovers within 3-10 days after discontinuation, depending on the agent.[24][215] Overall, 2022 American Heart Association/American Stroke Association guidelines and 2024 performance measures emphasize rapid reversal within 1-2 hours to mitigate ICH expansion, which occurs in up to 40% of cases and drives poor outcomes; however, this must be balanced against a 2-3 fold increased thrombosis risk post-reversal, including venous thromboembolism rates up to 10% in-hospital. Monitoring coagulation parameters (e.g., INR, aPTT, anti-Xa levels) guides therapy, with resumption of anticoagulation considered after 4-8 weeks in select patients based on bleeding risk.[24][13][216]Emerging therapies
Recent research into hemostatic agents for intracranial hemorrhage (ICH) has focused on tranexamic acid, an antifibrinolytic drug. The Tranexamic acid for hyperacute primary IntraCerebral Haemorrhage-2 (TICH-2) trial, a large randomized controlled study, demonstrated that tranexamic acid significantly reduces hematoma expansion when administered early, but it did not improve functional outcomes or mortality at 90 days.[217] Ongoing investigations into recombinant activated factor VIIa (rFVIIa), a procoagulant, show promise in limiting hematoma growth in acute ICH, with phase III trials like the FASTEST study evaluating its safety and efficacy in reducing expansion and improving neurological recovery.[218][219] Neuroprotectants represent another frontier, targeting secondary brain injury from inflammation and oxidative stress post-ICH. Minocycline, a tetracycline antibiotic with anti-inflammatory properties, has exhibited neuroprotective effects in preclinical models by inhibiting microglial activation and matrix metalloproteinase-9 expression, thereby preserving the blood-brain barrier and reducing neuronal damage.[220] Clinical trials have confirmed its safety in ICH patients, achieving therapeutic serum levels, though further studies are needed to optimize dosing for functional benefits.[221] Complementing this, stem cell therapies, particularly mesenchymal stem cells, are in phase II trials as of 2025, aiming to promote tissue repair and neurogenesis in subacute ICH by modulating inflammation and supporting endogenous repair mechanisms.[222][223] Biomaterial platforms are emerging to facilitate minimally invasive ICH management, building on surgical advances for hematoma evacuation. Injectable hydrogels, such as gelatin-based formulations loaded with growth factors, enable precise cavity filling post-evacuation, promoting hemostasis and tissue regeneration while minimizing invasiveness.[224] Self-assembling peptide hydrogels like IEIK13 have shown efficacy in intraoperative hemostasis during neurosurgical procedures, forming biocompatible seals to control bleeding.[225] Additionally, gene therapies targeting amyloid-beta in cerebral amyloid angiopathy—a key cause of lobar ICH—are under investigation, with CRISPR-based APOE editing and immunotherapies reducing amyloid deposition and associated vascular fragility in preclinical models.[128][226] The 2024 American Heart Association/American Stroke Association (AHA/ASA) guidelines introduce 15 performance measures for spontaneous ICH care, spanning prehospital to post-discharge phases, to standardize high-quality interventions like timely blood pressure control and rehabilitation access. These metrics aim to enhance adherence to evidence-based practices, thereby improving functional outcomes through reduced variability in care delivery.[13][227]Prognosis
Outcome predictors
The Intracerebral Hemorrhage (ICH) Score is a widely used clinical tool for predicting 30-day mortality in patients with spontaneous ICH, ranging from 0 to 6 points based on five components: Glasgow Coma Scale (GCS) score (2 points for 3-4, 1 point for 5-12, 0 points for 13-15), age greater than 80 years (1 point), infratentorial location (1 point), ICH volume of 30 mL or greater (1 point), and presence of intraventricular hemorrhage extension (1 point).[55] Scores of 3 or higher are associated with 30-day mortality exceeding 50%, with rates reaching 72% for a score of 3, 97% for 4, and 100% for 5 or 6.[55] This score provides a simple, reliable framework for early prognostication and has been validated across multiple cohorts for both mortality and functional outcomes.[228] Hematoma volume and location are key radiological predictors of outcome, with volumes exceeding 60 mL strongly linked to high mortality and poor functional recovery due to greater mass effect and midline shift.[229] Brainstem or infratentorial locations confer worse prognosis compared to supratentorial sites, independent of volume, owing to involvement of critical neural structures.[230] Hematoma expansion, particularly when detected on follow-up CT within 6 hours of symptom onset, approximately doubles the risk of poor functional outcome and mortality by exacerbating secondary brain injury.[39] Serum glial fibrillary acidic protein (GFAP), a biomarker of astrocytic injury, serves as an early indicator of poor prognosis in ICH when levels exceed established thresholds (typically >0.1-0.5 ng/mL at admission, depending on assay), correlating with larger hematoma volumes, neurological deterioration, and increased 30-day mortality.[231] Elevated GFAP reflects the extent of perihematomal tissue damage and has been shown to predict unfavorable outcomes more accurately than imaging alone in acute settings.[232] As of 2025, artificial intelligence models integrating clinical variables, imaging features, and biomarkers like GFAP achieve approximately 80% accuracy (AUC 0.80-0.92) in predicting 90-day functional outcomes and mortality in ICH patients, outperforming traditional scores such as the ICH Score in multimodal validations.[233] These models, often based on machine learning algorithms like random forest or XGBoost, enable personalized risk stratification by analyzing non-contrast CT scans and routine labs.[234] Subtype variations, such as lobar versus deep ICH, can influence model performance but are generally accounted for in feature selection.[235] Pre-existing comorbidities, particularly a premorbid modified Rankin Scale (mRS) score greater than 2 indicating moderate to severe disability, significantly worsen outcomes in ICH by increasing baseline vulnerability to complications like infection and dependency.[236] Patients with premorbid mRS >2 experience higher rates of in-hospital mortality and failure to achieve functional independence at 90 days compared to those with lower scores, emphasizing the need for adjusted prognostic expectations.[237]Long-term effects
Survivors of intracranial hemorrhage frequently experience persistent neurological deficits that impact daily functioning. Hemiparesis, a common motor impairment, affects a substantial proportion of patients, with functional impairments including hemiplegia reported in up to 80% of cases in some studies. Cognitive impairment occurs in 30-50% of survivors, often manifesting as memory dysfunction and executive deficits that hinder rehabilitation and independence. Aphasia is prevalent, particularly following left hemispheric lesions, contributing to communication challenges in up to 20-40% of stroke-related cases, including those due to hemorrhage. Depression affects about 25% of patients in the months following the event, exacerbating disability and reducing adherence to therapy. Long-term effects vary by ICH subtype, with lobar hemorrhages associated with higher recurrence risk due to underlying cerebral amyloid angiopathy. Systemic complications further complicate long-term recovery. Epilepsy develops in 10-20% of patients after intracerebral hemorrhage, with rates reaching 12-25% following subarachnoid hemorrhage due to factors like cortical involvement. The risk of venous thromboembolism remains elevated long-term, with cumulative incidence approaching 5% at 7 years, nearly threefold higher than after ischemic stroke, necessitating ongoing prophylaxis considerations. Quality of life is markedly affected, with only 12-39% of survivors achieving functional independence at 6 months, while approximately 20% require institutionalization due to severe disability. Multidisciplinary rehabilitation, including early intervention, improves functional outcomes such as activities of daily living and modified Rankin Scale scores, enhancing independence and quality of life as demonstrated in recent analyses. These effects are influenced by initial clinical predictors like hematoma volume and location. Recurrence prevention is crucial for mitigating further events. Strict blood pressure control reduces the risk of recurrent ICH by approximately 50%, forming a cornerstone of secondary prevention strategies alongside lifestyle modifications and monitoring for vascular risk factors.[238]Comparison of types
Clinical and diagnostic differences
Intracranial hemorrhages are distinguished clinically by the presence or absence of trauma history, with traumatic cases typically involving a clear mechanism of injury such as blunt head trauma, often leading to immediate or delayed neurological deterioration.[1] In contrast, non-traumatic hemorrhages, which account for the majority of spontaneous cases, frequently present without preceding injury and are commonly associated with underlying vascular pathologies like hypertension or amyloid angiopathy, manifesting as sudden headache, nausea, or focal deficits.[2] For instance, epidural hematomas in traumatic settings may feature a classic lucid interval of temporary consciousness recovery following initial loss, whereas non-traumatic subarachnoid hemorrhages often debut with a severe "thunderclap" headache without trauma.[1][239] Differences also arise based on hemorrhage location, with extra-axial bleeds (epidural and subdural) exerting compressive mass effect that can cause rapid midline shift, herniation, and altered mental status, while intra-axial parenchymal hemorrhages lead to deeper coma and location-specific focal neurological deficits due to direct tissue disruption.[1] Subarachnoid hemorrhages, whether traumatic or non-traumatic, produce irritative symptoms such as nuchal rigidity, photophobia, and meningism from blood in the cerebrospinal fluid, contrasting with the more global or hemispheric deficits seen in intraparenchymal hemorrhages.[74] Intraventricular extension, common in both, exacerbates hydrocephalus and obtundation but is more prognostic in non-traumatic cases linked to hypertension.[2] Diagnostic imaging further delineates types, with traumatic hemorrhages often appearing multifocal and hyperacute on non-contrast CT due to associated contusions or fractures, whereas non-traumatic intraparenchymal hemorrhages show characteristic patterns: hypertensive bleeds as rounded, deep-seated hyperdensities in basal ganglia or thalamus, and amyloid angiopathy as lobar collections with surrounding microbleeds visible on MRI gradient-echo sequences.[74] Epidural hematomas exhibit a biconvex, lens-shaped hyperdensity confined by sutures on CT, while subdural ones form crescentic collections that cross suture lines; subarachnoid blood appears as hyperdensity in cisterns or sulci, best detected acutely on CT but with MRI FLAIR sensitivity for trace amounts.[1]| Type | Typical Signs | Key CT/MRI Features |
|---|---|---|
| Epidural Hematoma (Traumatic) | Headache, lucid interval, rapid deterioration post-trauma | CT: Hyperdense biconvex lens-shaped, suture-limited; often with skull fracture. MRI: Acute T1/T2 hyperintense.[1] |
| Subdural Hematoma (Traumatic/Non-Traumatic) | Altered mental status, confusion (chronic), seizures | CT: Crescentic hyperdense (acute) to hypodense (chronic), crosses sutures. MRI: Variable intensity by age, GRE blooming.[74] |
| Subarachnoid Hemorrhage (Traumatic/Non-Traumatic) | Thunderclap headache, nuchal rigidity, vomiting, LOC | CT: Hyperdense in sulci/cisterns; spares vertex in trauma. MRI: FLAIR hyperintense, SWI hypointense blooming.[1] |
| Intraparenchymal (Traumatic) | Focal deficits, contusion-related symptoms post-injury | CT: Multifocal hyperdense with edema. MRI: GRE detects small foci in temporal/frontal lobes.[74] |
| Intraparenchymal (Hypertensive, Non-Traumatic) | Sudden focal weakness, headache, hypertension history | CT: Rounded hyperdense in basal ganglia/thalamus. MRI: T2* edema, spot sign on CTA for expansion.[2] |
| Intraparenchymal (Amyloid Angiopathy, Non-Traumatic) | Progressive deficits in elderly, no trauma | CT: Lobar hyperdense, spares deep structures. MRI: Multiple cortical microbleeds on SWI.[74] |
Management and outcome variations
Management of intracranial hemorrhage varies significantly between traumatic and non-traumatic types, influencing outcomes such as survival and functional recovery. In traumatic cases, such as epidural or subdural hematomas, surgical intervention is prioritized to evacuate the hematoma and alleviate mass effect, with timing being critical for prognosis. For instance, prompt surgical evacuation of epidural hematomas, ideally within 2-3 hours of neurological deterioration, is associated with excellent outcomes, including up to 90% functional recovery in selected patients with preserved consciousness.[16] Mortality for traumatic intracranial hemorrhages varies widely, from approximately 10% overall to over 40% in severe cases, depending on factors like hematoma location, patient age, and initial Glasgow Coma Scale score, with epidural hematomas generally faring better than subdural ones.[240] Non-traumatic intracranial hemorrhages, including hypertensive intracerebral hemorrhage (ICH) and aneurysmal subarachnoid hemorrhage (SAH), emphasize medical management alongside targeted interventions. For hypertensive ICH, aggressive blood pressure control to a systolic target of 140 mmHg reduces hematoma expansion and improves outcomes without increasing ischemic risk.[24] In aneurysmal SAH, endovascular coiling or clipping of the aneurysm is standard, often combined with nimodipine to prevent vasospasm, yielding 30-day mortality rates of 10-20% in treated patients, though overall 30-50% mortality occurs with complications like rebleeding.[2][239] ICH carries a higher 30-day mortality of 40-50%, with survivors often facing substantial disability.[2] Specific variations in management and outcomes arise in subtypes influenced by underlying pathology. Anticoagulation reversal is crucial in amyloid angiopathy-related or oral anticoagulant-associated ICH, where agents like prothrombin complex concentrate can halt expansion and improve outcomes compared to delayed reversal.[24] Emerging minimally invasive surgery (MIS) techniques show promise for lobar ICH, as demonstrated by the ENRICH trial, where early MIS evacuation within 24 hours led to better functional outcomes at 180 days versus medical management alone, with a utility-weighted modified Rankin scale score difference of 0.084 favoring MIS.[241]| Type | Primary Management | Mortality Range | Key Recovery Factors |
|---|---|---|---|
| Traumatic Epidural | Surgical evacuation (craniotomy <4 hours) | 5-15% | Early intervention, small volume (<30 mL), young age[16] |
| Traumatic Subdural | Surgical evacuation, ICP monitoring | 30-50% | GCS >8, no midline shift, reversal of coagulopathy[240] |
| Hypertensive ICH | BP control (target SBP 140 mmHg), medical | 40-50% | Hematoma volume <30 mL, location (lobar better), rapid BP lowering[24] |
| Aneurysmal SAH | Endovascular coiling/clipping, nimodipine | 10-50% | WFNS grade I-II, no vasospasm, secure aneurysm <72 hours[239] |
| Amyloid Angiopathy ICH | Anticoagulation reversal, conservative | 30-40% | Reversal within 4 hours, avoid antiplatelets, small hematoma[24] |
References
- https://wikem.org/wiki/Subarachnoid_hemorrhage
.jpg/250px-Intracerebral_hemorrage_(CT_scan).jpg)
.jpg)