Recent from talks
Nothing was collected or created yet.
Naturopathy
View on Wikipedia
| Alternative medicine | |
|---|---|
 A homeopathic preparation of Hepar sulph – homeopathy can be offered as part of naturopathic treatment.[1] | |
| Claims | Diseases are cured through the body's "natural healing" ability which is primarily aided by practices labelled as "natural" (and not primarily by pharmaceutical drugs, surgery, and other treatments within evidence-based medicine, not seen as "natural"), comprising widely ranging "nature cures" and any form of alternative medicine that may be labelled as "natural" |
| Related fields | Alternative medicine |
| Original proponents | Benedict Lust; Sebastian Kneipp |
| MeSH | D009324 |
| See also | Humorism, heroic medicine, vitalism |
| Part of a series on |
| Alternative medicine |
|---|
 |
Naturopathy, or naturopathic medicine, is a form of alternative medicine.[1] A wide array of practices branded as "natural", "non-invasive", or promoting "self-healing" are employed by its practitioners, who are known as naturopaths. These treatments range from the pseudoscientific and thoroughly discredited, such as homeopathy, to the widely accepted, such as certain forms of psychotherapy.[2][3][4] The ideology and methods of naturopathy are based on vitalism and folk medicine rather than evidence-based medicine, although practitioners may use techniques supported by evidence.[5][6][7] The ethics of naturopathy have been called into question by medical professionals and its practice has been characterized as quackery.[8][9][10][11][12]
Naturopathic practitioners commonly encourage alternative treatments that are rejected by conventional medicine, including resistance to surgery or vaccines for some patients.[13][14][15][16] The diagnoses made by naturopaths often have no basis in science and are often not accepted by mainstream medicine.[8][17]
Naturopaths frequently campaign for legal recognition in the United States. Naturopathy is prohibited in three U.S. states (Florida, South Carolina, and Tennessee) and tightly regulated in many others. Some states, however, allow naturopaths to perform minor surgery or even prescribe drugs. While some schools exist for naturopaths, and some jurisdictions allow such practitioners to call themselves doctors, the lack of accreditation, scientific medical training, and quantifiable positive results means they lack the competency of true medical doctors.
History
[edit]The term "naturopathy" originates from "natura" (Latin root for birth) and "pathos" (the Greek root for suffering) to suggest "natural healing".[18] Naturopaths claim the ancient Greek "Father of Medicine", Hippocrates, as the first advocate of naturopathic medicine, before the term existed.[18][19] Naturopathy has its roots in the 19th-century Natural Cure movement of Europe.[20][21] After graduating as a licenciate of the Royal College of Physicians of Edinburgh in 1879, Thomas Allinson began promoting his hygienic medicine in London, advocating a natural diet, exercise, and avoidance of tobacco and overwork.[22][23]
The term naturopathy was coined in 1895 by John Scheel,[24] and bought by Benedict Lust, whom naturopaths consider to be the "Father of U.S. Naturopathy".[25] Lust had been schooled in hydrotherapy and other natural health practices in Germany by Father Sebastian Kneipp; Kneipp sent Lust to the United States to spread his drugless methods.[26] Lust defined naturopathy as a broad discipline rather than a particular method, and included such techniques as hydrotherapy, herbal medicine, and homeopathy, as well as eliminating overeating, tea, coffee, and alcohol.[1] He described the body in spiritual and vitalistic terms with "absolute reliance upon the cosmic forces of man's nature".[27] According to the Merriam-Webster Dictionary, the first known use of "naturopathy" in print is from 1901.[28]
From 1901, Lust founded the American School of Naturopathy in New York. In 1902, the original North American Kneipp Societies were discontinued and renamed "Naturopathic Societies". In September 1919, the Naturopathic Society of America was dissolved and Benedict Lust founded the American Naturopathic Association to supplant it.[25][29] Naturopaths became licensed under naturopathic or drugless practitioner laws in 25 states in the first three decades of the twentieth century.[25] Naturopathy was adopted by many chiropractors, and several schools offered both Doctor of Naturopathy (ND) and Doctor of Chiropractic (DC) degrees.[25] Estimates of the number of naturopathic schools active in the United States during this period vary from about one to two dozen.[11][24][25]
After a period of rapid growth, naturopathy went into decline for several decades after the 1930s. In 1910, the Carnegie Foundation for the Advancement of Teaching published the Flexner Report, which criticized many aspects of medical education, especially quality and lack of scientific rigour. The advent of penicillin and other "miracle drugs" and the consequent popularity of modern medicine also contributed to naturopathy's decline. In the 1940s and 1950s, a broadening in scope of practice laws led many chiropractic schools to drop their ND degrees, though many chiropractors continued to practice naturopathy. From 1940 to 1963, the American Medical Association campaigned against heterodox medical systems. By 1958, practice of naturopathy was licensed in only five states.[25] In 1968, the United States Department of Health, Education, and Welfare issued a report on naturopathy concluding that naturopathy was not grounded in medical science and that naturopathic education was inadequate to prepare graduates to make appropriate diagnosis and provide treatment; the report recommends against expanding Medicare coverage to include naturopathic treatments.[11][30] In 1977 an Australian committee of inquiry reached similar conclusions; it did not recommend licensure for naturopaths.[31]
Beginning in the 1970s, there was a revival of interest in the United States and Canada, in conjunction with the "holistic health" movement.[25][1] As of 2009[update], fifteen U.S. states, Puerto Rico, the US Virgin Islands and the District of Columbia licensed naturopathic doctors,[32] and the State of Washington requires insurance companies to offer reimbursement for services provided by naturopathic physicians.[33][34] On the other hand, some states such as South Carolina and Tennessee prohibit the practice of naturopathy.[35][36][37]
In the United States, the Indian Health Service began accepting naturopathic doctors in their clinics and practice in 2013, also making loan repayment available to ND's.[38]
In 2015, a former naturopathic doctor, Britt Marie Hermes, began writing critically about her experience being trained in and practicing naturopathic medicine.[39][40] Her blog garnered a large following among skeptics while enraging some proponents of alternative medicine.[41]
-
Sebastian Kneipp c. 1898, a Bavarian priest and forefather of naturopathy[26]
-
Benedict Lust c. 1902, the founder of naturopathy in the U.S.[25]
-
Britt Marie Hermes c. 2016, a former naturopathic doctor and major critic of naturopathic medicine[40]
Practice
[edit]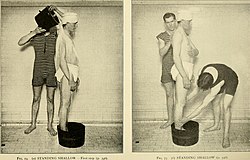


In 2003, a report[45] was presented by Kimball C. Atwood, an American medical doctor and researcher from Newton, Massachusetts, best known as a critic of naturopathic medicine, stating among other criticisms that "The practice of naturopathy is based on a belief in the body's ability to heal itself through a special vital energy or force guiding bodily processes internally".[8]
Diagnosis and treatment concern primarily alternative therapies and "natural" methods that naturopaths claim promote the body's natural ability to heal.[1][46] Many naturopaths in India now use modern diagnostic techniques in their practice.[47] Naturopaths focus on a holistic approach, avoiding the use of surgery and conventional medicines.[11] Naturopaths aim to prevent illness through stress reduction and changes to diet and lifestyle, often rejecting the methods of evidence-based medicine.[5][48]
A consultation typically begins with a comprehensive patient interview assessing lifestyle, medical history, emotional tone, and physical features, as well as physical examination.[1] Many naturopaths present themselves as primary care providers, and some naturopathic physicians may prescribe drugs, perform minor surgery, and integrate other conventional medical approaches such as diet and lifestyle counselling with their naturopathic practice.[1][49] Traditional naturopaths deal exclusively with lifestyle changes, not diagnosing or treating disease. Naturopaths do not generally recommend vaccines and antibiotics, based in part on the early views that shaped the profession, and they may provide alternative remedies even in cases where evidence-based medicine has been shown effective.[10]
Methods
[edit]Naturopaths are often opposed to mainstream medicine and take an antivaccinationist stance.[10]
The particular modalities used by a naturopath vary with training and scope of practice. These may include herbalism, homeopathy,[42] acupuncture, nature cures, physical medicine, applied kinesiology,[50] colonic enemas,[26][43] chelation therapy,[12] color therapy,[50] cranial osteopathy, hair analysis, iridology,[50] live blood analysis, ozone therapy,[11] psychotherapy, public health measures and hygiene,[48] reflexology,[50] rolfing,[29] massage therapy, and traditional Chinese medicine. Nature cures include a range of therapies based on exposure to natural elements such as sunshine, fresh air, or heat or cold, as well as nutrition advice such as following a vegetarian and whole food diet, fasting, or abstention from alcohol and sugar.[51] Physical medicine includes naturopathic, osseous, or soft tissue manipulative therapy, sports medicine, exercise, and hydrotherapy. Psychological counseling includes meditation, relaxation, and other methods of stress management.[51]
A 2004 survey determined the most commonly prescribed naturopathic therapeutics in Washington state and Connecticut were botanical medicines, vitamins, minerals, homeopathy, and allergy treatments.[42] An examination published in 2011 of naturopathic clinic websites in Alberta and British Columbia found that the most commonly advertised therapies were homeopathy, botanical medicine, nutrition, acupuncture, lifestyle counseling, and detoxification.[43]
In 2020, a survey of methods used by naturopaths in fourteen countries reported that 27% of clients received acupuncture, 22% homeopathy, 16% "other energetic medicines", and 13.5% were given hydrotherapy. A mean of 4.0 "treatments" were provided to each customer. One-third (33%) of patients consulted with only the naturopath to manage their primary health concern.[52]
Evidence basis
[edit]

Naturopathy as a whole lacks an adequate scientific basis,[5] and it is rejected by the medical community.[5] Although it includes valid lifestyle advice from mainstream medicine (healthy sleep, balanced diet, regular exercise),[10] it typically adds a range of pseudoscientific beliefs.[18] Some methods rely on immaterial "vital energy fields", the existence of which has not been proven, and there is concern that naturopathy as a field tends towards isolation from general scientific discourse.[18][55][56] Naturopathy is criticized for its reliance on and its association with unproven, disproven, and other controversial alternative medical treatments, and for its vitalistic underpinnings.[10][11] Natural substances known as nutraceuticals show little promise in treating diseases, especially cancer, as laboratory experiments have shown limited therapeutic effect on biochemical pathways, while clinical trials demonstrate poor bioavailability.[57] According to the American Cancer Society, "scientific evidence does not support claims that naturopathic medicine can cure cancer or any other disease".[11] According to Britt Hermes, naturopath student programs are problematic because "As a naturopath [student], you are making justifications to make the rules and to fudge the standards of how to interpret research all along the way. Because if you don't, you're not left with anything, basically".[58]
In 2015, the Australian Government's Department of Health published the results of a review of alternative therapies that sought to determine if any were suitable for being covered by health insurance; Naturopathy was one of 17 therapies evaluated for which no clear evidence of effectiveness was found.[59]
Kimball C. Atwood IV writes, in the journal Medscape General Medicine,[8]
Naturopathic physicians now claim to be primary care physicians proficient in the practice of both "conventional" and "natural" medicine. Their training, however, amounts to a small fraction of that of medical doctors who practice primary care. An examination of their literature, moreover, reveals that it is replete with pseudoscientific, ineffective, unethical, and potentially dangerous practices.
In another article, Atwood writes that "Physicians who consider naturopaths to be their colleagues thus find themselves in opposition to one of the fundamental ethical precepts of modern medicine. If naturopaths are not to be judged "nonscientific practitioners", the term has no useful meaning".[12]
A former licensed naturopathic doctor, Britt Marie Hermes, states that "any product that is sold by a naturopath almost guarantees that there is no reliable scientific data to support whatever health claims are made,[60] and that while some naturopaths claim to only practice evidence based medicine, "the problem is, all naturopaths in an accredited naturopathic program are required to extensively study homeopathy, herbal medicine, energy healing, chiropractic techniques, water therapy" and other pseudoscientific practices.[58] Hermes further notes that, while some naturopaths claim that their method can be effective treatments for psychological disorders, "no naturopathic treatment has been clinically proven to be safe and effective for bipolar disorder or any other condition."[61]
According to Arnold S. Relman, the Textbook of Natural Medicine is inadequate as a teaching tool, as it omits to mention or treat in detail many common ailments, improperly emphasizes treatments "not likely to be effective" over those that are, and promotes unproven herbal remedies at the expense of pharmaceuticals. He concludes that "the risks to many sick patients seeking care from the average naturopathic practitioner would far outweigh any possible benefits".[62]
The Massachusetts Medical Society states, "Naturopathic practices are unchanged by research and remain a large assortment of erroneous and potentially dangerous claims mixed with a sprinkling of non-controversial dietary and lifestyle advice."[63]
Safety of natural treatments
[edit]Naturopaths often recommend exposure to naturally occurring substances, such as sunshine, herbs and certain foods, as well as activities they describe as natural, such as exercise, meditation and relaxation. Naturopaths claim that these natural treatments help restore the body's innate ability to heal itself without the adverse effects of conventional medicine. However, "natural" methods and chemicals are not necessarily safer or more effective than "artificial" or "synthetic" ones, and any treatment capable of eliciting an effect may also have deleterious side effects.[11][26][64][65]
Certain naturopathic treatments offered by naturopaths, such as homeopathy, rolfing, and iridology, are widely considered pseudoscience or quackery.[66][67][68] Stephen Barrett of QuackWatch and the National Council Against Health Fraud has stated that naturopathy is "simplistic and that its practices are riddled with quackery".[26][69] "Non-scientific health care practitioners, including naturopaths, use unscientific methods and deception on a public who, lacking in-depth health care knowledge, must rely upon the assurance of providers. Quackery not only harms people, it undermines the ability to conduct scientific research and should be opposed by scientists", says William T. Jarvis.[70] In the 2018 Australian case against Marlyin Bodnar, who advised a mother to treat her infant son's eczema with a raw food diet which nearly led to the child's starvation death, Judge Peter Berman said, "Well intentioned but seriously misguided advice is, as the facts of this case demonstrate, capable of causing great harm and even death to vulnerable children."[71] Furthermore, Britt Hermes criticizes the "pervasive culture of patient blaming" among naturopathic practitioners, where "when something doesn't work for the patient and the patient is not experiencing all of the positive effects and zero side-effects that are promised with the therapy, it's never because the therapy doesn't work, it's because the patient didn't do something right."[58]
Vaccination
[edit]
Many naturopathy practitioners voice their opposition to vaccination. The reasons for this opposition are based, in part, on the early views which shaped the foundation of this occupation.[72] A naturopathy textbook, co-authored by Joseph Pizzorno, recalls anti-vaccine beliefs associated with the founding of naturopathy in the United States: "a return to nature in regulating the diet, breathing, exercising, bathing and the employment of various forces" in lieu of the smallpox vaccine.[73]
In general, evidence about associations between naturopathy and pediatric vaccination is sparse, but "published reports suggest that only a minority of naturopathic physicians actively support full vaccination".[74][75] In Washington state from 2000 to 2003, children were significantly less likely to receive immunizations if they had seen a naturopath.[74] A survey of naturopathic students published in 2004 found that students at the Canadian College of Naturopathic Medicine became less likely to recommend vaccinations to their patients and became more distrustful of public health and conventional medicine as they advanced in the program.[15]
The British Columbia Naturopathic Association lists several major concerns regarding the pediatric vaccine schedule and vaccines in general,[76] and the group's policy is to not advocate for or against vaccines.[77] The Oregon Association of Naturopathic Physicians reports that many naturopaths "customize" the pediatric vaccine schedule.[78]
As of April 25, 2022, a British Columbia government report found that 69.2% of naturopaths reported having received at least two COVID vaccines or receiving a medical exemption. This was much lower than all the other regulated medical professions in the report. The number for two professions – dieticians and physicians/surgeons – was 98%.[79][80]
As of 2016[update], the American Association of Naturopathic Physicians, which is the largest professional organization for licensed naturopaths in the U.S., is "still discussing its stance on vaccinations".[81]
Practitioners
[edit]Naturopath practitioners can generally be categorized into three groups: 1) those with a government issued license; 2) those who practice outside of an official status ("traditional naturopaths"); 3) those who are primarily another kind of health professional who also practices naturopathy.[11][82][83][84][85]
In Switzerland, these divisions fall between those with a federal diploma, those recognized by health insurances, and those with neither federal diploma nor recognition by health insurances. Naturopaths with federal diploma can be divided into four categories: European traditional medicine, Chinese traditional medicine, ayurvedic medicine and homeopathy.[86][87] The number of listed naturopaths (including traditional healers) in Switzerland rose from 223 in 1970 to 1835 in 2000.[88]
Licensed naturopaths
[edit]Licensed naturopaths may be referred to as "naturopathic doctors" or "naturopathic physicians" in 26 US states or territories and 5 Canadian provinces.[89] Licensed naturopaths present themselves as primary care providers.[1][49] Licensed naturopaths do not receive comparable training to medical doctors in terms of the quality of education or quantity of hours.[8][17]
In British Columbia, legislation permits licensed naturopaths to use the title "doctor" or "physician".[90] However, section 102 of the bylaw of the College of Naturopathic Physicians of British Columbia (CNPBC), the terms "naturopathic" or "naturopathic medicine" must be included anytime the term doctor or physician is used by a member of the CNPBC.[91][92][93][94]
Education
[edit]

Licensed naturopaths must pass the Naturopathic Physicians Licensing Examinations (NPLEX) administered by the North American Board of Naturopathic Examiners (NABNE)[95] after graduating from a program accredited by the Council on Naturopathic Medical Education (CNME).[49][96] Training in CNME-accredited programs includes basic medical diagnostics and procedures such as rudimentary physical exams and common blood tests, in addition to pseudoscientific modalities, such as homeopathy, acupuncture, and energy modalities.[8][12][26][1] These accredited programs have been criticized for misrepresenting their medical rigor and teaching subjects that are antithetical to the best understandings of science and medicine.[26][97][98] The CNME as an accrediting authority has been characterized as unreliable and suffering from conflicts of interest.[99][100][101] The naturopathic licensing exam has been called a mystery by those outside the naturopathic profession[12][63] and criticized for testing on homeopathic remedies,[97] including for the use to treat pediatric emergencies.[39]
Several schools in North America exist for the study of naturopathic medicine, some accredited by the CNME.[102] The CNME and the Association of Accredited Naturopathic Medical Colleges (AANMC) claim entrance requirements and curricula at accredited colleges are often similar or comparable to those required and offered at conventional medical schools.[103] However, the lack of accreditation by the Liaison Committee on Medical Education may indicate insufficiency of scientific medical training and/or quantifiable positive results, and accordingly it remains disputed whether graduates of medical colleges accredited by the CNME have the competency of Medical Doctors and Doctors of Osteopathy.[17][104]
Naturopathic doctors are not eligible for medical residencies, which are available exclusively for medical doctors and doctors of osteopathic medicine. There are limited post-graduate "residency" positions available to naturopathic doctors offered through naturopathic schools and naturopathic clinics approved by the CNME.[105] Most naturopathic doctors do not complete such a residency,[42] and naturopathic doctors are not mandated to complete one for licensure,[11] except in the states of Utah and Connecticut.[106] Continuing education in naturopathic modalities for health care professionals varies greatly.[50]
Political activity in the United States
[edit]Naturopathic practitioners affiliated with the CNME-accredited schools lobby state, provincial, and federal governments for medical licensure and participation in social health programs.[81][107] The American Association of Naturopathic Physicians represents licensed naturopaths in the United States;[81] the Canadian Association of Naturopathic Doctors represents licensed naturopaths in Canada.[107] Naturopathic lobbying efforts are funded by vitamin and supplement makers[81] and focus on portraying naturopathic education as comparable to medical education received by physicians and on having high professional standards.[107][108] Medical societies and advocacy groups dispute these claims by citing evidence of licensed naturopathic practitioners using pseudoscientific methods without a sound evidence basis and lacking adequate clinical training to diagnose and treat disease competently according to the standard of care.[81][108][109][110] Jann Bellamy has characterized the process by which naturopathic practitioners and other practitioners of pseudoscience convince lawmakers to provide them with medical licenses as "legislative alchemy".[111]
Since 2005, the Massachusetts Medical Society has opposed licensure based on concerns that NDs are not required to participate in residency and concerns that the practices of naturopaths included many "erroneous and potentially dangerous claims".[112] The Massachusetts Special Commission on Complementary and Alternative Medical Practitioners rejected their concerns and recommended licensure.[113] The Massachusetts Medical Society states:[63]
Naturopathic medical school is not a medical school in anything but the appropriation of the word medical. Naturopathy is not a branch of medicine. It is a hodge podge of nutritional advice, home remedies and discredited treatments ... Naturopathic colleges claim accreditation but follow a true "alternative" accreditation method that is virtually meaningless. They are not accredited by the same bodies that accredit real medical schools and while some courses have similar titles to the curricula of legitimate medical schools the content is completely different.
In 2015, a former naturopathic doctor, Britt Marie Hermes, who graduated from Bastyr University and practiced as a licensed ND in Washington and Arizona, began advocating against naturopathic medicine.[114][39][115] In addition to opposing further licensure, she believes that NDs should not be allowed to use the titles "doctor" or "physician",[39] and be barred from treating children.[116][117] She states:[118]
Naturopaths aggressively lobby for laws to issue them medical licenses. I would characterize this political effort as a perverted redefinition of the words "physician", "doctor", "medical school", and "residency" in order to mask the inadequacy of the training provided in naturopathic programs. ND students do not realize that they are taking educational shortcuts and therefore do not possess any demonstrable competencies found in modern medicine.
Traditional naturopaths
[edit]
Traditional naturopaths are represented in the United States by the American Naturopathic Association (ANA), representing about 1,800 practitioners[119] and the American Naturopathic Medical Association (ANMA).[25]
The level of naturopathic training varies among traditional naturopaths in the United States. Traditional naturopaths may complete non-degree certificate programs or undergraduate degree programs and generally refer to themselves as naturopathic consultants. These programs often offer online unaccredited degrees, but do not offer comprehensive biomedical education or clinical training.
Traditional naturopathic practitioners surveyed in Australia perceive evidence-based medicine to be an ideological assault on their beliefs in vitalistic and holistic principles.[5] They advocate for the integrity of natural medicine practice.[5]
Naturopaths graduating from accredited programs argued in 2002 that their training used evidence-based scientific principles unlike traditional naturopathic programs,[120] but this claim remains inaccurate.[8][26]
Regulation
[edit]Naturopathy is practiced in many countries and is subject to different standards of regulation and levels of acceptance. The scope of practice varies widely between jurisdictions, with some covering naturopathy under medical regulation and allowing practitioners to prescribe drugs and perform minor surgery, while other jurisdictions outlaw naturopathy entirely.[citation needed]
Australia
[edit]In 1977, a Commonwealth Government inquiry reviewed all colleges of naturopathy in Australia and found that despite having syllabuses appearing to cover the basic biomedical sciences, actual lectures had little connection to those syllabuses and no significant practical work was available. In addition, there did not appear to be significant or systematic coverage of techniques favoured by naturopaths, such as homeopathy, Bach's floral remedies, or mineral salts.[31]
The position of the Australian Medical Association is that "evidence-based aspects of complementary medicine can be part of patient care by a medical practitioner", but it has concerns that there is "limited efficacy evidence regarding most complementary medicine. Unproven complementary medicines and therapies can pose a risk to patient health either directly through misuse or indirectly if a patient defers seeking medical advice." The AMA's position on regulation is that "there should be appropriate regulation of complementary medicine practitioners and their activities".[121]
In 2015, the Australian government found no clear evidence of effectiveness for naturopathy.[59] Accordingly, In 2017 the Australian government named naturopathy as a practice that would not qualify for insurance subsidies, saying this step would "ensure taxpayer funds are expended appropriately and not directed to therapies lacking evidence".[122]
India
[edit]In India, naturopathy is overseen by the Department of Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy (AYUSH); there is a 5½-year degree in "Bachelor of Naturopathy and Yogic Sciences" (BNYS) degree that was offered by twelve colleges in India as of August 2010[update].[123] The National Institute of Naturopathy in Pune that operates under AYUSH, which was established on December 22, 1986, and encourages facilities for standardization and propagation of the existing knowledge and its application through research in naturopathy throughout India.[124][125]
North America
[edit]In five Canadian provinces, seventeen U.S. states, and the District of Columbia, naturopathic doctors who are trained at an accredited school of naturopathic medicine in North America are entitled to use the designation ND or NMD. Elsewhere, the designations "naturopath", "naturopathic doctor", and "doctor of natural medicine" are generally unprotected or prohibited.[37][83]
In North America, each jurisdiction that regulates naturopathy defines a local scope of practice for naturopathic doctors that can vary considerably. Some regions permit minor surgery, access to prescription drugs, spinal manipulations, midwifery (natural childbirth), and gynecology; other regions exclude these from the naturopathic scope of practice or prohibit the practice of naturopathy entirely.[37][126]
Canada
[edit]Five Canadian provinces license naturopathic doctors: Ontario, British Columbia, Manitoba, Saskatchewan, and Alberta.[127][128] British Columbia has the largest scope of practice in Canada, allowing certified NDs to prescribe pharmaceuticals and perform minor surgeries.[129] Ontario also permits prescription from a modified formulary list, following separate examination.[130]
United States
[edit]- U.S. jurisdictions that currently regulate or license naturopathy include Alaska, Arizona, California, Connecticut, Colorado, Delaware, District of Columbia, Hawaii, Idaho, Kansas, Maine, Maryland, Massachusetts, Minnesota, Montana, New Hampshire, New Mexico, North Dakota, Oregon, Pennsylvania, Rhode Island, Wisconsin, Puerto Rico,[131] US Virgin Islands, Utah, Vermont, and Washington.[130][32] Additionally, Virginia licenses the practice of naturopathy under a grandfather clause. (This was previously also the case in Florida, though currently no practitioners remain active under the grandfather provisions).[37][132]
- U.S. jurisdictions that permit access to prescription drugs: Arizona, California, District of Columbia, Hawaii, Idaho, Kansas, Maine, Montana, New Hampshire, New Mexico, Oregon, Utah, Vermont, and Washington.[130]
- U.S. jurisdictions that permit minor surgery: Arizona, District of Columbia, Kansas, Maine, Montana, Oregon, Utah, Vermont, and Washington.
- Three U.S. states specifically prohibit the practice of naturopathy: Florida,[133][134] South Carolina[35][37] and Tennessee.[36][37]
Switzerland
[edit]The Swiss Federal Constitution defines the Swiss Confederation and the Cantons of Switzerland within the scope of their powers to oversee complementary medicine.[135] In particular, the Federal authorities must set up diplomas for the practice of non-scientific medicine. The first of such diplomas has been validated in April 2015 for the practice of naturopathy.[86] There is a long tradition of naturopathy and traditional medicine in Switzerland.[136] The Cantons of Switzerland make their own public health regulations. Although the law in certain cantons is typically monopolistic, the authorities are relatively tolerant with regard to alternative practitioners.[87]
United Kingdom
[edit]Naturopathy is not regulated in the United Kingdom. In 2012, publicly funded universities in the United Kingdom dropped their alternative medicine programs, including naturopathy.[137]
See also
[edit]- Appeal to nature
- Arnold Ehret
- Essential nutrient
- Friedrich Eduard Bilz
- Barbara O'Neill
- Health freedom movement
- Heilpraktiker
- Kneipp facility
- List of ineffective cancer treatments
- List of topics characterized as pseudoscience
- Megavitamin therapy
- Orthomolecular medicine
- Osteopathy and osteopathic medicine
- Phytonutrient
- Therapeutic nihilism
References
[edit]- ^ a b c d e f g h i Boughton RJ, Frey B (2005). "Naturopathic Medicine". Gale Encyclopedia of Alternative Medicine (2nd ed.). Gale. Archived from the original on June 24, 2013. Retrieved March 21, 2015.
- ^ Baran GR, Kiani MF, Samuel SP (2014). "Science, Pseudoscience, and Not Science: How do They Differ?". Healthcare and Biomedical Technology in the 21st Century. pp. 19–57. doi:10.1007/978-1-4614-8541-4_2. ISBN 978-1-4614-8540-7.
within the traditional medical community it is considered to be quackery
- ^ Paul S. Boyer (2001). The Oxford companion to United States history. Oxford University Press. p. 630. ISBN 978-0-19-508209-8. Retrieved January 15, 2013.
After 1847, when regular doctors organized the American Medical Association (AMA), that body led the war on "quackery", especially targeting dissenting medical groups such as homeopaths, who prescribed infinitesimally small doses of medicine. Ironically, even as the AMA attacked all homeopathy as quackery, educated homeopathic physicians were expelling untrained quacks from their ranks.
- ^ Psychotherapy can be evidence based, or pseudoscientific however, see:
- Lilienfeld SO (December 2015). "Introduction to special section on pseudoscience in psychiatry". The Canadian Journal of Psychiatry. 60 (12): 531–533. doi:10.1177/070674371506001202. PMC 4679160. PMID 26720820.
Although the boundaries separating pseudoscience from science are fuzzy, pseudosciences are characterized by several warning signs – fallible but useful indicators that distinguish them from most scientific disciplines. ... In contrast to most accepted medical interventions, which are prescribed for a circumscribed number of conditions, many pseudoscientific techniques lack boundary conditions of application. For example, some proponents of Thought Field Therapy, an intervention that purports to correct imbalances in unobservable energy fields, using specified bodily tapping algorithms, maintain that it can be used to treat virtually any psychological condition, and that it is helpful not only for adults but also for children, dogs, and horses.
- Lee CM, Hunsley J (December 2015). "Evidence-based practice: separating science from pseudoscience". The Canadian Journal of Psychiatry. 60 (12): 534–540. doi:10.1177/070674371506001203. PMC 4679161. PMID 26720821.
TFT, a treatment applied to mood, anxiety, and trauma-related disorders, is a prime example of practice founded on pseudoscience. TFT is based on the premise that bodily energy imbalances cause negative emotions. Treatment is purported to rectify imbalances by tapping on acupuncture meridians. Virtually no peer-reviewed research supports this treatment rationale. With only methodologically weak reports available in the literature, the so-called science cited to support TFT is primarily anecdotal and does not rule out placebo effects. Despite these criticisms, the TFT website continues to advance unsupported claims about TFT's ability to cure almost any emotional problem.
- Lilienfeld SO (December 2015). "Introduction to special section on pseudoscience in psychiatry". The Canadian Journal of Psychiatry. 60 (12): 531–533. doi:10.1177/070674371506001202. PMC 4679160. PMID 26720820.
- ^ a b c d e f Jagtenberg T, Evans S, Grant A, Howden I, Lewis M, Singer J (April 2006). "Evidence-based medicine and naturopathy". Journal of Alternative and Complementary Medicine. 12 (3): 323–328. doi:10.1089/acm.2006.12.323. PMID 16646733.
- ^ Tabish SA (2008). "Complementary and Alternative Healthcare: Is it Evidence-based?". International Journal of Health Sciences. 2 (1): v–ix. PMC 3068720. PMID 21475465.
- ^ Goldenberg JZ, Burlingham BS, Guiltinan J, Oberg EB (August 2017). "Shifting attitudes towards research and evidence-based medicine within the naturopathic medical community". Advances in Integrative Medicine. 4 (2): 49–55. doi:10.1016/j.aimed.2017.08.003.
- ^ a b c d e f g Atwood KC (December 2003). "Naturopathy: a critical appraisal". MedGenMed. 5 (4): 39. PMID 14745386. Archived from the original on March 2, 2013. Retrieved September 4, 2013.(registration required)
- ^ Gorski DH (October 2014). "Integrative oncology: really the best of both worlds?". Nature Reviews. Cancer. 14 (10): 692–700. doi:10.1038/nrc3822. PMID 25230880. S2CID 33539406.
- ^ a b c d e Singh S, Ernst E (2009). Naturopathy. Transworld. pp. 197–. ISBN 978-1-4090-8180-7. Archived from the original on February 6, 2016. Retrieved January 27, 2016.
many naturopaths are against mainstream medicine and advise their patients accordingly – for instance many are not in favour of vaccination.
{{cite book}}:|work=ignored (help) - ^ a b c d e f g h i j Russell J, ed. (2009). American Cancer Society complete guide to complementary & alternative cancer therapies. American Cancer Society. pp. 116–119. ISBN 978-1-60443-054-7. OCLC 671655748.
- ^ a b c d e Atwood KC (March 2004). "Naturopathy, pseudoscience, and medicine: myths and fallacies vs truth". MedGenMed. 6 (1): 33. PMC 1140750. PMID 15208545.
- ^ Wilson K, Busse JW, Gilchrist A, Vohra S, Boon H, Mills E (March 2005). "Characteristics of pediatric and adolescent patients attending a naturopathic college clinic in Canada". Pediatrics. 115 (3): e338-43. doi:10.1542/peds.2004-1901. PMID 15741360.
- ^ Busse JW, Wilson K, Campbell JB (November 2008). "Attitudes towards vaccination among chiropractic and naturopathic students". Vaccine. 26 (49): 6237–6243. doi:10.1016/j.vaccine.2008.07.020. PMID 18674581.
- ^ a b Wilson K, Mills E, Boon H, Tomlinson G, Ritvo P (January 2004). "A survey of attitudes towards paediatric vaccinations amongst Canadian naturopathic students". Vaccine. 22 (3–4): 329–334. doi:10.1016/j.vaccine.2003.08.014. PMID 14670313.
- ^ Engler BD, Mielczarek EV (2014). "Selling Pseudoscience: A Rent in the Fabric of American Medicine". Skeptical Inquirer. 38 (3).
- ^ a b c "Family Physicians versus Naturopaths" (PDF). aafp.org. American Academy of Family Physicians. Archived (PDF) from the original on June 16, 2015. Retrieved July 20, 2015.
- ^ a b c d Jarvis WT (January 30, 2001) [copyright 1997]. "NCAHF Fact Sheet on Naturopathy". National Council Against Health Fraud. Archived from the original on September 27, 2011. Retrieved April 17, 2009.
- ^ "What is Naturopathy?". College of Naturopathic Medicine website. East Grinstead, England. Archived from the original on September 18, 2010. Retrieved September 16, 2015.
- ^ Brown PS (April 1988). "Nineteenth-century American health reformers and the early nature cure movement in Britain". Medical History. 32 (2): 174–194. doi:10.1017/S0025727300047980. PMC 1139856. PMID 3287059.
- ^ Langley S. "History of Naturopathy". College of Naturopathic Medicine website. UK. Archived from the original on August 29, 2012.
- ^ "How it all began". Allinson Flour website. Silver Spoon, British Sugar, Associated British Foods. Archived from the original on August 13, 2010. Retrieved September 3, 2008.
- ^ Beard JA (May 3, 2008). "A system of hygienic medicine (1886) and The advantages of wholemeal bread (1889)". BMJ. Views & Reviews: Medical Classics. 336 (7651): 1023. doi:10.1136/bmj.39562.446528.59. PMC 2364871.
- ^ a b "Report 12 of the Council on Scientific Affairs (A-97)" (PDF). American Medical Association. 1997. Archived from the original (PDF) on November 5, 2013. Retrieved September 3, 2013.
- Lay summary in: "1997 Annual Meeting of the American Medical Association: Summaries and Recommendations of the Council on Scientific Affairs" (PDF). American Medical Association. 1997. Archived from the original (PDF) on January 2, 2014.
- ^ a b c d e f g h i Baer HA (September 2001). "The sociopolitical status of U.S. naturopathy at the dawn of the 21st century". Medical Anthropology Quarterly. 15 (3): 329–346. doi:10.1525/maq.2001.15.3.329. PMID 11693035.
- ^ a b c d e f g h Barrett S (November 26, 2013). "A close look at naturopathy". QuackWatch. Archived from the original on April 6, 2011. Retrieved March 21, 2015.
- ^ Lust, Benedict cited in: Whorton JC (2002). Nature Cures : The History of Alternative Medicine in America: The History of Alternative Medicine in America. Oxford: Oxford University Press. p. 224. ISBN 978-0-19-534978-8. Retrieved September 3, 2013.
- ^ "Naturopathy - Definition of Naturopathy by Merriam-Webster". Archived from the original on November 19, 2015. Retrieved October 27, 2015.
- ^ a b Beyerstein BL, Downie S (May 12, 2004). "Naturopathy: A Critical Analysis". NaturoWatch. QuackWatch. Archived from the original on March 7, 2009. Retrieved March 21, 2009.
- ^ "HEW Report on Naturopathy (1968)". QuackWatch. August 30, 1999. Archived from the original on August 14, 2010. Retrieved September 3, 2013. Citing: Cohen WJ (1969). Independent Practitioners Under Medicare: A Report to the Congress. United States Department of Health, Education, and Welfare. OCLC 3000280.
- ^ a b "Naturopathy: Report of the Australian Committee of Inquiry (1977)". NaturoWatch. QuackWatch. December 25, 2003. Archived from the original on September 6, 2010. Retrieved September 3, 2013. Citing: Webb EC, et al. (1977). Report of the Committee of Inquiry into Chiropractic, Osteopathy, Homoeopathy and Naturopathy. Canberra: Australian Government Publishing Service. ISBN 978-0-642-92287-8.
- ^ a b "Licensed States & Licensing Authorities". American Association of Naturopathic Physicians website. 2009. Archived from the original on November 30, 2009.
- ^ "Washington Administrative Code: Title 284, Chapter 43, Section 205: Every category of health providers". Washington State Legislature. August 28, 1999. Archived from the original on October 11, 2011. Retrieved November 19, 2010. (effective)
- ^ Minott R (July 3, 1996). "Insuring Alternatives". NewsHour with Jim Lehrer. PBS. Online NewsHour transcript.
- ^ a b "Title 40, Chapter 31, Sections 10 & 20". South Carolina Code of Laws (Unannotated), Current through the end of the 2007 Regular Session. South Carolina Legislative Council. Archived from the original on January 12, 2009.
- ^ a b State of Tennessee (2013). "Title 63 Professions of the Healing Arts, Chapter 6 Medicine and Surgery, Part 2 General Provisions". Tennessee Code Annotated. Justia. 63.6.205 Practice of naturopathy. Archived from the original on October 7, 2013. Retrieved September 7, 2013.
- ^ a b c d e f AMA Scope of Practice Data Series: Naturopaths. American Medical Association (Report). 2009. Archived from the original on June 29, 2016. Retrieved July 30, 2016 – via The Alaska State Legislature.
- ^ "https://newsmaven.io/indiancountrytoday/archive/introducing-naturopathic-doctors-to-indian-health-service-clinics-Rn_RipOYh0Kgd9KR-5Ou_A/ Archived October 5, 2019, at the Wayback Machine"
- ^ a b c d Senapathy K (May 31, 2016). "Why Is Big Naturopathy Afraid Of This Lone Whistleblower?". Forbes. US. Archived from the original on March 22, 2020. Retrieved September 5, 2017.
- ^ a b Thielking M (October 20, 2016). "'Essentially witchcraft:' A former naturopath takes on the field". STAT. Archived from the original on October 25, 2016. Retrieved October 30, 2016.
- ^ Devlin H (March 27, 2018). "The naturopath whistleblower: 'It is surprisingly easy to sell snake oil'". Guardian. Retrieved August 23, 2021.
- ^ a b c d Boon HS, Cherkin DC, Erro J, Sherman KJ, Milliman B, Booker J, et al. (October 2004). "Practice patterns of naturopathic physicians: results from a random survey of licensed practitioners in two US States". BMC Complementary and Alternative Medicine. 4 14. doi:10.1186/1472-6882-4-14. PMC 529271. PMID 15496231.
- ^ a b c d Caulfield T, Rachul C (September 2011). "Supported by science?: what canadian naturopaths advertise to the public". Allergy, Asthma, and Clinical Immunology. 7 (1) 14. doi:10.1186/1710-1492-7-14. PMC 3182944. PMID 21920039.
- ^ Smith K (2012). "Homeopathy is Unscientific and Unethical". Bioethics. 26 (9): 508–512. doi:10.1111/j.1467-8519.2011.01956.x. S2CID 143067523. Archived from the original on October 29, 2017. Retrieved October 28, 2017.
- ^ Atwood KC (December 30, 2003). "Naturopathy: a critical appraisal". MedGenMed: Medscape General Medicine. 5 (4): 39. ISSN 1531-0132. PMID 14745386.
- ^ Carroll RT (March 7, 2015). "Naturopathy". The Skeptic's Dictionary. Archived from the original on September 1, 2010. Retrieved March 21, 2015.
- ^ Nair PM, Nanda A (September 2014). "Naturopathic medicine in India: Original Article". Focus on Alternative and Complementary Therapies. 19 (3): 140–147. doi:10.1111/fct.12125.
- ^ a b Pizzorno JE (1999). "Naturopathy: Practice Issues". In Clark CC, Gordon RJ (eds.). Encyclopedia of Complementary Health Practice. Springer Publishing. pp. 57–59. ISBN 978-0-8261-1722-9. Archived from the original on April 13, 2018. Retrieved September 3, 2013.
- ^ a b c "Handbook of Accreditation for Naturopathic Medicine Programs" (PDF). Council on Naturopathic Medical Education. 2007. Archived from the original (PDF) on February 9, 2017. Retrieved November 20, 2010.
- ^ a b c d e Hough HJ, Dower C, O'Neil EH (September 2001). Profile of a Profession: Naturopathic Practice (PDF). Center for the Health Professions, University of California, San Francisco. p. 54. Archived from the original (PDF) on October 2, 2008.
- ^ a b Young J (2007). "Chapters 8 & 13". Complementary Medicine for Dummies. Chichester, England: Wiley. ISBN 978-0-470-02625-0. OCLC 174043853.
- ^ Steel A, Foley H, Bradley R, Van De Venter C, Lloyd I, Schloss J, et al. (February 2020). "Overview of international naturopathic practice and patient characteristics: results from a cross-sectional study in 14 countries". BMC Complementary Medicine and Therapies. 20 (1) 59. doi:10.1186/s12906-020-2851-7. PMC 7076821. PMID 32070338.
- ^ Ernst E (June 1997). "Colonic Irrigation and the Theory of Autointoxication: A Triumph of Ignorance over Science". Journal of Clinical Gastroenterology. 24 (4): 196–198. doi:10.1097/00004836-199706000-00002. PMID 9252839.
- ^ "Code of Federal Regulations Title 21, Sec. 801.415 Maximum acceptable level of ozone". U.S. Food and Drug Administration. April 1, 2015. Archived from the original on March 4, 2016. Retrieved May 18, 2016.
- ^ Herbert V, Barrett S (1994). The Vitamin Pushers: How the "Health Food" Industry is Selling America a Bill of Goods. Buffalo, NY: Prometheus Books. ISBN 978-0-87975-909-4.
- ^ Barrett S, Raso J (1993). Mystical Diets: Paranormal, Spiritual, and Occult Nutrition Practices. Buffalo, New York: Prometheus Books. ISBN 978-0-87975-761-8.
- ^ Ahmad A, Ginnebaugh KR, Li Y, Padhye SB, Sarkar FH (January 2015). "Molecular targets of naturopathy in cancer research: bridge to modern medicine". Nutrients (Review). 7 (1): 321–334. doi:10.3390/nu7010321. PMC 4303842. PMID 25569626.
- ^ a b c "Episode #050, feat. Britt Hermes". The European Skeptics Podcast. November 29, 2016. Archived from the original on September 9, 2018. Retrieved September 15, 2018.
- ^ a b Baggoley C (2015). "Review of the Australian Government Rebate on Natural Therapies for Private Health Insurance" (PDF). Australian Government – Department of Health. Archived from the original (PDF) on June 26, 2016. Retrieved December 12, 2015.
- Lay summary in: Gavura, S. (November 19, 2015). "Australian review finds no benefit to 17 natural therapies". Science-Based Medicine.
- ^ Haglage A, Mak T (May 25, 2016). "Trump Vitamins Were Fortified With B.S." The Daily Beast. Archived from the original on January 14, 2021. Retrieved June 24, 2016.
- ^ Hermes B (April 2020). "Dubious claims in psychotherapy for youth". Skeptical Inquirer. 44 (2): 50.
- ^ Relman AS (April 10, 2002) [January 9, 2001]. "Textbook of Natural Medicine". QuackWatch. Archived from the original on May 11, 2011. Retrieved April 17, 2009.
- ^ a b c "MMS Testimony in Opposition to H. 1992 and S. 1205, An Act to Create a Board of Registration in Naturopathy". Massachusetts Medical Society. Archived from the original on May 22, 2016. Retrieved July 30, 2016.
- ^ Carroll R (November 26, 2012). "Natural". The Skeptic's Dictionary. Archived from the original on May 14, 2011. Retrieved September 8, 2013.
- ^ "NCAHF Position Paper on Over the Counter Herbal Remedies (1995)". National Council Against Health Fraud. 1995. Archived from the original on July 7, 2011. Retrieved April 17, 2009.
- ^ National Science Board (January 15, 2002). "Chapter 7 Science and Technology: Public Attitudes and Public Understanding, Section: Belief in Alternative Medicine". Science and Engineering Indicators - 2002. Arlington, VA: Division of Science Resources Statistics, National Science Foundation. Archived from the original on June 16, 2016. Retrieved April 6, 2018.
- ^ Wahlberg A (December 2007). "A quackery with a difference-new medical pluralism and the problem of 'dangerous practitioners' in the United Kingdom" (PDF). Social Science & Medicine. 65 (11): 2307–2316. doi:10.1016/j.socscimed.2007.07.024. PMID 17719708. Archived (PDF) from the original on January 14, 2021. Retrieved December 10, 2019.
- ^ Barrett S (March 28, 2008). "Iridology is Nonsense". QuackWatch. Archived from the original on April 6, 2011. Retrieved September 8, 2013.
- ^ "Homeopathy". nhs.uk. October 18, 2017. Archived from the original on May 13, 2020. Retrieved May 21, 2020.
- ^ Jarvis WT (August 1992). "Quackery: a national scandal". Clinical Chemistry. 38 (8B Pt 2): 1574–1586. PMID 1643742.
- ^ Sutton C (April 5, 2018). "Naturopath jailed in starving baby case". news.com.au. Archived from the original on April 24, 2018. Retrieved April 24, 2018.
- ^ Ernst E (October 2001). "Rise in popularity of complementary and alternative medicine: reasons and consequences for vaccination". Vaccine. 20 Suppl 1 (Suppl. 1, 5th European Conference on Vaccinology: A Safe Future with Vaccination): S90-3, discussion S89. doi:10.1016/S0264-410X(01)00290-0. PMID 11587822.
- ^ Pizzorno JE, Murray MT (2011). Textbook of Natural Medicine e-edition: Text with Continually Updated Online Reference, 2-Volume Set (third ed.). Elsevier. p. 43. ISBN 978-1-4557-0527-6.
To understand how revolting these products are, let us just refer to the vaccine matter which is supposed to be an efficient preventive of smallpox. [...] The natural system for curing disease is based on a return to nature in regulating the diet, breathing, exercising, bathing and the employment of various forces to eliminate the poisonous products in the system, and so raise the vitality of the patient to a proper standard of health.
- ^ a b Downey L, Tyree PT, Huebner CE, Lafferty WE (November 2010). "Pediatric vaccination and vaccine-preventable disease acquisition: associations with care by complementary and alternative medicine providers". Maternal and Child Health Journal. 14 (6): 922–930. doi:10.1007/s10995-009-0519-5. PMC 2924961. PMID 19760163. Quote is taken from introduction to paper, not from results of research presented in this paper.
- ^ Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á (February 2013). "Are healthcare workers' intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review". BMC Public Health. 13 154. doi:10.1186/1471-2458-13-154. PMC 3602084. PMID 23421987.
- ^ "BCNA Vaccination Position Paper". British Columbia Naturopathic Association. Archived from the original on July 19, 2014. Retrieved July 15, 2014.
- ^ Brown H (December 21, 2007). "Influenza Virus, Vaccination and Naturopathic Practice". Naturopathic Doctor News and Review. Archived from the original on January 14, 2021. Retrieved October 20, 2016.
- ^ "Naturopathic Primary Care" (PDF). Oregon Association of Naturopathic Physicians. Archived (PDF) from the original on June 14, 2013. Retrieved July 15, 2014.
- ^ Larsen K (May 10, 2022). "Naturopaths, chiropractors least vaccinated of all B.C. health professionals, province says". CBC. Retrieved May 11, 2022.
- ^ "Data published on vaccination status of regulated health professions". news.gov.bc.ca. BC Gov News. May 10, 2022. Retrieved May 11, 2022.
- ^ a b c d e Robins R (May 17, 2016). "Funded by vitamin makers, naturopaths push to expand in US". STAT. Archived from the original on January 14, 2021. Retrieved May 18, 2016.
- ^ "Naturopathy: An Introduction". National Center for Complementary and Integrative Health, National Institutes of Health, United States Department of Health and Human Services. March 2012 [Created April 2007]. Archived from the original on February 23, 2015. Retrieved March 16, 2013.
- ^ a b Iowa Board of Medicine (February 7, 2002). "A Policy Statement on Naturopathy". Iowa Department of Public Health, State of Iowa. Archived from the original on April 12, 2013. Retrieved September 1, 2013.
- ^ The Platform of the American Naturopathic Association as drawn up by the Golden Jubilee Congress. July 27th – August 2nd, 1947
- ^ Naturopathy Work Group. "Traditional Naturopathy Working Session Summary September 23 and October 1, 2008" (PDF). Minnesota Department of Health. Archived from the original (PDF) on July 26, 2011. Retrieved November 20, 2010.
- ^ a b "Naturopathe avec diplôme fédéral". CH: State Secretariat for Education, Research and Innovation. Archived from the original on September 4, 2015.
- ^ a b "Legal Status of Traditional Medicine and Complementary/Alternative Medicine: A Worldwide Review". World Health Organization. Archived from the original on July 5, 2015. Retrieved July 4, 2015.
- ^ "Swiss Federal Statistical Office". Switzerland. Archived from the original on July 8, 2015. Retrieved July 11, 2015.
- ^ "Naturopathic Doctors are Now Licensed in Wisconsin". AANMC. February 17, 2022. Retrieved February 21, 2022.
Wisconsin has just become the 26th U.S. state/territory to regulate naturopathic doctors.
- ^ "Health Professions Act: Naturopathic Physicians Regulation". Victoria, British Columbia: Queen's Printer. October 2008. B.C. Reg. 282/2008 M242/2008. Archived from the original on January 14, 2021. Retrieved August 18, 2016.
- ^ "Bylaws of the College of Naturopathic Physicians of British Columbia" (PDF). Archived from the original (PDF) on February 25, 2021. Retrieved April 14, 2020.
- ^ "Surrey city councillor and naturopath Allison Patton fined and suspended for calling herself a "physician"". February 13, 2020. Archived from the original on January 14, 2021. Retrieved April 14, 2020.
- ^ "Surrey councillor fined, suspended from naturopathy for misusing 'physician' title". February 12, 2020. Archived from the original on January 14, 2021. Retrieved April 14, 2020.
- ^ "Complaint filed against Surrey naturopath-turned-councillor who campaigned as 'physician'". Archived from the original on January 14, 2021. Retrieved April 14, 2020.
- ^ "About Us". North American Board of Naturopathic Examiners. Archived from the original on October 5, 2013. Retrieved September 3, 2013.
- ^ "Naturopathy". NCCIH. Archived from the original on March 31, 2020. Retrieved May 27, 2020.
- ^ a b Gorski D (February 21, 2011). "Naturopathy and Science". ScienceBasedMedicine.org. Archived from the original on January 14, 2021. Retrieved March 3, 2016.
- ^ Hermes B (March 13, 2015). "ND Confession, Part 1: Clinical training inside and out". Science-Based Medicine. Archived from the original on January 14, 2021. Retrieved July 23, 2016.
- ^ Mangan KS (December 2, 1999). "Report Recommends Stripping Naturopathy Council of Its Accrediting Authority". The Chronicle of Higher Education. Archived from the original on January 14, 2021. Retrieved July 23, 2016.
- ^ Hermes B (August 29, 2015). "ND Confession, Part II: The Accreditation of Naturopathic "Medical" Education". Science-Based Medicine. Archived from the original on July 10, 2016. Retrieved July 23, 2016.
- ^ Society for Science-Based Medicine (2014). Report to the Maryland Board of Physicians Naturopathic Advisory Committee: Recommendations for Naturopathic Regulation (Report). Archived from the original on January 14, 2021. Retrieved July 23, 2016.
- ^ "Accredited Naturopathic Medical Schools". Association of Accredited Naturopathic Medical Colleges.
- ^ "ND, MD/DO, NP: WHAT'S THE DIFFERENCE?". Association of Accredited Naturopathic Medical Colleges. Retrieved November 15, 2023.
- ^ "ND Confession, Part II: The Accreditation of Naturopathic "Medical" Education". Science-Based Medicine. August 30, 2015. Retrieved November 15, 2023.
- ^ "Handbook on CNME Postdoctoral Naturopathic Medical Education Sponsor Recognition Process and Standards (2005)" (PDF). Council on Naturopathic Medical Education. Archived from the original (PDF) on June 15, 2006.
- ^ "Application for Licensure: Naturopathic Physician" (PDF). Division of Occupational and Professional Licensing, Utah Department of Commerce. State of Utah. February 17, 2012. p. 1. Archived from the original (PDF) on June 29, 2010. Retrieved September 8, 2013.
- ^ a b c Carly W (April 29, 2016). "Are we being served by the regulation of naturopaths? Not if patients are still being misled". The Globe and Mail. Archived from the original on January 14, 2021. Retrieved July 23, 2016.
- ^ a b "ND vs MD -- Battle Lines Drawn in California". June 3, 2015. Archived from the original on July 25, 2016. Retrieved July 24, 2016.
- ^ Frosch D (February 21, 2011). "Licensing Naturopaths Incites Debate in Colorado". The New York Times. Archived from the original on February 2, 2017. Retrieved July 24, 2016.
- ^ Lambeck L (May 24, 2016). "New law could let Connecticut naturopathic physicians write prescriptions". Connecticut Post. Archived from the original on August 28, 2016. Retrieved July 25, 2016.
- ^ Bellamy J (May 15, 2014). "Legislative Alchemy 2014 (so far)". Science-Based Medicine. Archived from the original on February 20, 2016. Retrieved July 21, 2016.
- ^ "Massachusetts Medical Society Testifies in Opposition to Licensing Naturopaths". Massachusetts Medical Society. May 11, 2005. Archived from the original on July 16, 2011. Retrieved April 17, 2009.
- ^ The Special Commission on Complementary and Alternative Medical Practitioners (January 2002). "Majority Report of the Special Commission on Complementary and Alternative Medical Practitioners: A Report to the Legislature" (PDF). Massachusetts: The Special Commission on Complementary and Alternative Medical Practitioners. Archived (PDF) from the original on January 21, 2012. Retrieved November 10, 2010.
- ^ Hermes B (April 2020). "Beware the Naturopathic Cancer Quack". Skeptical Inquirer. 44 (2): 38–44.
- ^ Belluz J (September 2, 2015). "Why one naturopath quit after watching her peers treat cancer patients". Vox. Archived from the original on October 14, 2017. Retrieved June 13, 2017.
- ^ Jim Brown (April 10, 2016). "Former naturopathic doctor calls for an end to naturopathic pediatrics". The 180. CBC. Archived from the original on June 12, 2016. Retrieved June 8, 2016.
- ^ Kirkey S (April 4, 2016). "Should naturopaths be restricted from treating children after tragic death of Alberta toddler?". National Post. Retrieved June 8, 2016.
- ^ Britt H (June 21, 2016). "How A Former Naturopath Can Help Unravel The Trickery Of Alternative Medicine". Science 2.0. Archived from the original on January 14, 2021. Retrieved July 30, 2016.
- ^ Swartout KA, ed. (2006). Encyclopedia of Associations (44 ed.). Thomson Gale. pp. 1777–1778. ISBN 978-0-7876-8286-6. Archived from the original on December 3, 2016. Retrieved September 4, 2013.
- ^ Smith MJ, Logan AC (January 2002). "Naturopathy". The Medical Clinics of North America. 86 (1): 173–184. doi:10.1016/S0025-7125(03)00079-8. PMID 11795088.
- ^ "AMA Position Statement: Complementary Medicine - 2012". Australian Medical Association. August 28, 2012. Archived from the original on April 2, 2015. Retrieved March 21, 2015.
- ^ Paola S (October 17, 2017). "Homeopathy, naturopathy struck off private insurance list". Australian Journal of Pharmacy. Archived from the original on January 14, 2021. Retrieved January 11, 2018.
- ^ Ministry of AYUSH. Page updated August 21, 2010 AYUSH: Naturopathy Archived 2015-03-06 at the Wayback Machine. Page accessed March 21, 2015
- ^ Ministry of AYUSH. Page updated September 23, 2010 AYUSH: National Institute of Naturopathy, Pune Archived 2015-02-20 at the Wayback Machine. Page accessed March 21, 2015
- ^ "About: National Institute of Naturopathy". Archived from the original on March 6, 2015. Retrieved March 21, 2015.
- ^ "2008 Sunrise Review: Naturopathic Physicians" (PDF). Department of Regulatory Agencies. State of Colorado. January 4, 2008. pp. 18–19. Archived from the original (PDF) on October 2, 2008.
- ^ "Questions: Education and Regulation". Canadian Association of Naturopathic Doctors website. Archived from the original on July 6, 2011. Retrieved September 6, 2013.
- ^ "History of Naturopathic Medicine". www.cand.ca. Archived from the original on January 14, 2021. Retrieved February 17, 2016.
- ^ "B.C. gives naturopaths right to prescribe drugs". CBC News. April 10, 2009. Archived from the original on August 20, 2012. Retrieved September 6, 2013.
- ^ a b c "Naturopathic Regulatory Authority General Information Links". The Federation of Naturopathic Medicine Regulatory Authorities. Retrieved November 15, 2023.
- ^ "Ley para Reglamentar el Ejercicio de la Medicina Naturopática en Puerto Rico [Law to Regulate the Practice of Naturopathic Medicine in Puerto Rico]" (PDF) (in Spanish). December 30, 1997. Archived from the original (PDF) on October 2, 2008.
- ^ "AN ENDANGERED SPECIES NATUROPATHIC DOCTOR IS CLOSE TO EXTINCTION". Orlando Sentinel. September 18, 1986. Retrieved November 17, 2023.
- ^ "Review of State Laws Regulating Naturopathy". American Naturopathic Certification Board. Retrieved November 15, 2023.
- ^ "Title XXXII REGULATION OF PROFESSIONS AND OCCUPATIONS Chapter 462 NATUROPATHY". Online Sunshine. Florida Legislature. Retrieved November 17, 2023.
- ^ "Federal Constitution of the Swiss Confederation". CH. Art. 118a Complementary medicine. Archived from the original on June 21, 2016. Retrieved July 4, 2015. (English translation)
- ^ "Swiss take an holistic approach". The Irish Times. Retrieved November 29, 2021.
- ^ Bevanger L (January 18, 2012). "UK universities drop alternative medicine degree programs". Deutsche Welle. Archived from the original on January 25, 2012. Retrieved February 5, 2012.
External links
[edit]Naturopathy
View on GrokipediaOrigins and Historical Development
Early Foundations in the 19th Century
The foundations of naturopathy emerged in the early 19th century from European hydrotherapy practices and American botanical systems, both rooted in vitalistic philosophies that emphasized the body's innate healing capacity over invasive interventions. Vincenz Priessnitz (1799–1851), an Austrian peasant, pioneered modern hydrotherapy after observing that cold compresses alleviated pain from injuries in the 1820s; he expanded this into comprehensive water cures involving wet sheets, compresses, baths, and exercise, establishing a sanatorium at Gräfenberg that treated thousands by the 1830s and influenced the "water cure" movement across Europe and America.[9][10] These methods rejected the era's dominant heroic medicine—characterized by bloodletting, purging, and mineral drugs—in favor of natural agents like water, air, and diet to support vital forces.[11] In the United States, Samuel Thomson (1769–1843) developed Thomsonianism, a self-reliant botanical system patented on March 2, 1813, as "Thomson's Improved System of Botanic Practice of Medicine," which promoted herbal remedies, steam vapor baths, and laxatives derived from local plants to stimulate the vital heat and expel disease without professional physicians or toxic minerals.[12][13] Thomson's approach, disseminated through "Friendly Botanic Societies" by the 1820s, reflected widespread distrust of allopathic practices amid high mortality from epidemics and reflected vitalistic tenets positing disease as a loss of internal harmony restorable through nature's simples.[14] This movement's emphasis on patient empowerment and rejection of bleeding or calomel purging paralleled European nature cure ideals, fostering a cultural shift toward lifestyle factors like fresh air, exercise, and unadulterated foods.[15] Post-Civil War disillusionment with conventional medicine, exacerbated by the era's high surgical and pharmacological fatality rates—estimated at over 20% for amputations—amplified these influences, spurring adoption of eclectic botanical practices.[13] Wooster Beach (1794–1868), reacting against heroic therapies and Thomson's excesses, founded eclectic medicine in the 1820s, advocating specific plant extracts tailored to symptoms while integrating vitalism and empirical observation; by 1827, he established the United States Infirmary in New York to train practitioners in these non-depletive methods.[16][17] These pre-formal streams converged to prioritize causal restoration via natural means, laying the empirical groundwork for naturopathy's later synthesis without reliance on unproven mechanistic assumptions of the prevailing medical paradigm.[12]Formalization and Key Figures in the Early 20th Century
Benedict Lust formalized naturopathy as a distinct profession by founding the American School of Naturopathy in New York City in 1902, the first institution dedicated to training practitioners in this system.[18] [19] Lust, who had trained in hydrotherapy under Sebastian Kneipp in Germany before immigrating to the United States in 1892, adopted the term "naturopathy"—derived from the Greek natura (nature) and pathos (suffering or disease)—to describe an eclectic approach emphasizing drugless healing through natural means such as diet, exercise, and physical therapies.[20] [19] This school integrated influences from osteopathy, chiropractic, and homeopathy, reflecting Lust's own studies in these fields and his vision of a unified "nature cure" philosophy that viewed the body as self-healing when supported by vital forces.[21] The 1910 Flexner Report, commissioned by the Carnegie Foundation and led by Abraham Flexner, critiqued irregular medical schools, including those offering unorthodox therapies, for lacking scientific foundations and rigorous standards, resulting in the closure of over half of U.S. medical schools by 1935 and marginalizing alternative practices.[22] [23] Despite these pressures, Lust advocated for naturopathy's drugless methods as a counter to allopathic reliance on pharmaceuticals, establishing professional organizations like the American Naturopathic Association in 1902 to standardize practices and lobby for licensure.[24] His efforts included publishing journals such as the Naturopath and Herald of Health to disseminate principles and case studies.[25] Henry Lindlahr emerged as a key theorist, publishing Nature Cure: Philosophy and Practice Based on the Unity of Disease and Cure in 1913, which systematized naturopathic doctrine around the toxemia theory—that chronic disease stems from toxin accumulation in tissues due to dietary errors, inactivity, and suppressed eliminations, with acute illnesses representing the body's corrective crises.[26] [27] Lindlahr, who operated sanatoriums in Chicago, stressed lowering toxemia through fasting, hydrotherapy, and lifestyle reforms to restore vitality, influencing the proliferation of nature cure facilities and correspondence courses before the economic downturn of the 1930s.[28] By the 1920s, naturopathic sanatoriums dotted the U.S., offering holistic regimens that gained popularity amid growing public skepticism toward synthetic drugs, though lacking empirical validation beyond anecdotal reports.[29]


![Sebastian Kneipp c. 1898, a Bavarian priest and forefather of naturopathy[26]](http://upload.wikimedia.org/wikipedia/commons/thumb/f/f8/Portrait_of_Sebastian_Kneipp._Wellcome_L0005598.jpg/250px-Portrait_of_Sebastian_Kneipp._Wellcome_L0005598.jpg)
![Benedict Lust c. 1902, the founder of naturopathy in the U.S.[25]](http://upload.wikimedia.org/wikipedia/commons/thumb/7/7e/BenedictLust.jpg/160px-BenedictLust.jpg)
![Britt Marie Hermes c. 2016, a former naturopathic doctor and major critic of naturopathic medicine[40]](http://upload.wikimedia.org/wikipedia/commons/thumb/a/a6/QED_20161015_129.jpg/250px-QED_20161015_129.jpg)
