Recent from talks
Nothing was collected or created yet.
Common cold
View on Wikipedia
| Common cold | |
|---|---|
| Other names | Cold, acute viral nasopharyngitis, nasopharyngitis, viral rhinitis, rhinopharyngitis, acute coryza, head cold,[1] upper respiratory tract infection (URTI)[2] |
 | |
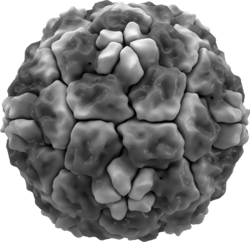
| A representation of the molecular surface of one variant of human rhinovirus | |
| Specialty | Infectious disease |
| Symptoms | Cough, sore throat, runny nose, fever, muscle aches, fatigue, headache, anorexia[3][4] |
| Complications | Usually none, but occasionally otitis media, sinusitis, pneumonia and sepsis can occur[5] |
| Usual onset | ~2 days from exposure[6] |
| Duration | 1–3 weeks[3][7] |
| Causes | Viral (usually rhinovirus)[8] |
| Diagnostic method | Based on symptoms |
| Differential diagnosis | Allergic rhinitis, bronchitis, bronchiolitis,[9] pertussis, sinusitis[5] |
| Prevention | Hand washing, cough etiquette, vitamin C[3][10] |
| Treatment | Symptomatic therapy,[3] zinc[11] |
| Medication | NSAIDs[12] |
| Frequency | 2–3 per year (adults) 6–8 per year (children)[13] |
The common cold, or the cold, is a viral infectious disease of the upper respiratory tract that primarily affects the respiratory mucosa of the nose, throat, sinuses, and larynx.[6][8] Signs and symptoms may appear in as little as two days after exposure to the virus.[6] These may include coughing, sore throat, runny nose, sneezing, headache, fatigue, and fever.[3][4] People usually recover in seven to ten days,[3] but some symptoms may last up to three weeks.[7] Occasionally, those with other health problems may develop pneumonia.[3]
Well over 200 virus strains are implicated in causing the common cold, with rhinoviruses, coronaviruses, adenoviruses and enteroviruses being the most common.[14] They spread through the air or indirectly through contact with objects in the environment, followed by transfer to the mouth or nose.[3] Risk factors include going to child care facilities, not sleeping well, and psychological stress.[6] The symptoms are mostly due to the body's immune response to the infection rather than to tissue destruction by the viruses themselves.[15] The symptoms of influenza are similar to those of a cold, although usually more severe and less likely to include a runny nose.[6][16]
There is no vaccine for the common cold.[3] This is due to the rapid mutation and wide variation of viruses that cause the common cold.[17] The primary methods of prevention are hand washing; not touching the eyes, nose or mouth with unwashed hands; and staying away from sick people.[3] People are considered contagious as long as the symptoms are still present.[18] Some evidence supports the use of face masks.[10] There is also no cure, but the symptoms can be treated.[3] Zinc may reduce the duration and severity of symptoms if started shortly after the onset of symptoms.[11] Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen may help with pain.[12] Antibiotics, however, should not be used, as all colds are caused by viruses rather than bacteria.[19] There is no good evidence that cough medicines are effective.[6][20]
The common cold is the most frequent infectious disease in humans.[21] Under normal circumstances, the average adult gets two to three colds a year, while the average child may get six to eight colds a year.[8][13] Infections occur more commonly during the winter.[3] These infections have existed throughout human history.[22]
Signs and symptoms
[edit]The typical symptoms of a cold include cough, runny nose, sneezing, nasal congestion, and a sore throat, sometimes accompanied by muscle ache, fatigue, headache, and loss of appetite.[23] A sore throat is present in about 40% of cases, a cough in about 50%,[8] and muscle aches in about 50%.[4] In adults, a fever is generally not present but it is common in infants and young children.[4] The cough is usually mild compared to that accompanying influenza.[4] While a cough and a fever indicate a higher likelihood of influenza in adults, a great deal of similarity exists between these two conditions.[24] A number of the viruses that cause the common cold may also result in asymptomatic infections.[25][26]
The color of the mucus or nasal secretion may vary from clear to yellow to green and does not indicate the class of agent causing the infection.[27]
Progression
[edit]
A cold usually begins with fatigue, a feeling of being chilled, sneezing, and a headache, followed in a couple of days by a runny nose and cough.[23] Symptoms may begin within sixteen hours of exposure[28] and typically peak two to four days after onset.[4][29] They usually resolve in seven to ten days, but some can last for up to three weeks.[7] The average duration of cough is eighteen days[30] and in some cases people develop a post-viral cough which can linger after the infection is gone.[31] In children, the cough lasts for more than ten days in 35–40% of cases and continues for more than 25 days in 10%.[32]
Causes
[edit]Viruses
[edit]
The common cold is an infection of the upper respiratory tract which can be caused by many different viruses. The most commonly implicated is a rhinovirus (30–80%), a type of picornavirus with 99 known serotypes.[33] Other commonly implicated viruses include coronaviruses, adenoviruses, enteroviruses, parainfluenza and RSV.[34] Frequently more than one virus is present.[35] In total, more than 200 viral types are associated with colds.[4] The viral cause of some common colds (20–30%) is unknown.[34]
Transmission
[edit]The common cold virus is typically transmitted via airborne droplets, direct contact with infected nasal secretions, or fomites (contaminated objects).[8][36] Which of these routes is of primary importance has not been determined.[37] As with all respiratory pathogens once presumed to transmit via respiratory droplets, it is highly likely to be carried by the aerosols generated during routine breathing, talking, and singing.[38] The viruses may survive for prolonged periods in the environment (over 18 hours for rhinoviruses) and can be picked up by people's hands and subsequently carried to their eyes or noses where infection occurs.[36] Transmission from animals is considered highly unlikely; an outbreak documented at a British scientific base on Adelaide Island after seventeen weeks of isolation was thought to have been caused by transmission from a contaminated object or an asymptomatic human carrier, rather than from the husky dogs which were also present at the base.[39]
Transmission is common in daycare and schools due to the proximity of many children with little immunity and poor hygiene.[40] These infections are then brought home to other members of the family.[40] There is no evidence that recirculated air during commercial flight is a method of transmission.[36] People sitting close to each other appear to be at greater risk of infection.[37]
Other
[edit]Herd immunity, generated from previous exposure to cold viruses, plays an important role in limiting viral spread, as seen with younger populations that have greater rates of respiratory infections.[41] Poor immune function is a risk factor for disease.[41][42] Insufficient sleep and malnutrition have been associated with a greater risk of developing infection following rhinovirus exposure; this is believed to be due to their effects on immune function.[43][44] Breast feeding decreases the risk of acute otitis media and lower respiratory tract infections among other diseases,[45] and it is recommended that breast feeding be continued when an infant has a cold.[46] In the developed world breast feeding may not be protective against the common cold in and of itself.[47]
Pathophysiology
[edit]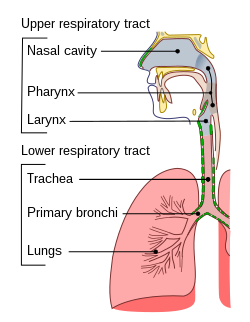
The symptoms of the common cold are believed to be primarily related to the immune response to the virus.[15] The mechanism of this immune response is virus-specific. For example, the rhinovirus is typically acquired by direct contact; it binds to humans via ICAM-1 receptors and the CDHR3 receptor through unknown mechanisms to trigger the release of inflammatory mediators.[15] These inflammatory mediators then produce the symptoms.[15] It does not generally cause damage to the nasal epithelium.[4] The respiratory syncytial virus (RSV), on the other hand, is contracted by direct contact and airborne droplets. It then replicates in the nose and throat before spreading to the lower respiratory tract.[48] RSV does cause epithelium damage.[48] Human parainfluenza virus typically results in inflammation of the nose, throat, and bronchi.[49] In young children, when it affects the trachea, it may produce the symptoms of croup, due to the small size of their airways.[49]
Diagnosis
[edit]The distinction between viral upper respiratory tract infections is loosely based on the location of symptoms, with the common cold affecting primarily the nose (rhinitis), throat (pharyngitis), and lungs (bronchitis).[8] There can be significant overlap, and more than one area can be affected.[8] Self-diagnosis is frequent.[4] Isolation of the viral agent involved is rarely performed,[50] and it is generally not possible to identify the virus type through symptoms.[4]
Prevention
[edit]The only useful ways to reduce the spread of cold viruses are physical and engineering measures[10] such as using correct hand washing technique, respirators, and improvement of indoor air. In the healthcare environment, gowns and disposable gloves are also used.[10] Droplet precautions cannot reliably protect against inhalation of common-cold-laden aerosols. Instead, airborne precautions such as respirators, ventilation, and HEPA/high MERV filters, are the only reliable protection against cold-laden aerosols.[38] Isolation or quarantine is not used as the disease is so widespread and symptoms are non-specific. There is no vaccine to protect against the common cold.[51] Vaccination has proven difficult as there are so many viruses involved and because they mutate rapidly.[10][52] Creation of a broadly effective vaccine is, therefore, highly improbable.[53]
Regular hand washing appears to be effective in reducing the transmission of cold viruses, especially among children.[54] Whether the addition of antivirals or antibacterials to normal hand washing provides greater benefit is unknown.[54] Wearing face masks when around people who are infected may be beneficial; however, there is insufficient evidence for maintaining a greater social distance.[54]
It is unclear whether zinc supplements affect the likelihood of contracting a cold.[55]
Management
[edit]
Treatments of the common cold primarily involve medications and other therapies for symptomatic relief.[13] Getting plenty of rest, drinking fluids to maintain hydration, and gargling with warm salt water are reasonable conservative measures.[56] Much of the benefit from symptomatic treatment is, however, attributed to the placebo effect.[57] As of 2010,[update] no medications or herbal remedies had been conclusively demonstrated to shorten the duration of infection.[58]
Symptomatic
[edit]
Treatments that may help with symptoms include pain medication and medications for fevers such as ibuprofen[12] and acetaminophen (paracetamol).[59] However, it is not clear whether acetaminophen helps with symptoms.[60] It is not known if over-the-counter cough medications are effective for treating an acute cough.[61] Cough medicines are not recommended for use in children due to a lack of evidence supporting effectiveness and the potential for harm.[62][63] In 2009, Canada restricted the use of over-the-counter cough and cold medication in children six years and under due to concerns regarding risks and unproven benefits.[62] The misuse of dextromethorphan (an over-the-counter cough medicine) has led to its ban in a number of countries.[64] Intranasal corticosteroids have not been found to be useful.[65]
In adults, short term use of nasal decongestants may have a small benefit.[66] Antihistamines may improve symptoms in the first day or two; however, there is no longer-term benefit and they have adverse effects such as drowsiness.[67] Other decongestants such as pseudoephedrine appear effective in adults.[68][66] Combined oral analgesics, antihistaminics, and decongestants are generally effective for older children and adults.[69] Ipratropium nasal spray may reduce the symptoms of a runny nose but has little effect on stuffiness.[70] Ipratropium may also help with coughs in adults.[71] The safety and effectiveness of nasal decongestant use in children is unclear.[66]
Due to lack of studies, it is not known whether increased fluid intake improves symptoms or shortens respiratory illness.[72] As of 2017, heated and humidified air, such as via RhinoTherm, is of unclear benefit.[73] One study has found chest vapor rub to provide some relief of nocturnal cough, congestion, and sleep difficulty.[74]
Some experts advise against physical exercise if there are symptoms such as fever, widespread muscle aches or fatigue.[75][76] It is regarded as safe to perform moderate exercise if the symptoms are confined to the head, including runny nose, nasal congestion, sneezing, or a minor sore throat.[75][76] There is a popular belief that having a hot drink can help with cold symptoms, but evidence to support this is very limited.[77]
Antibiotics and antivirals
[edit]Antibiotics have no effect against viral infections, including the common cold.[78] Due to their side effects, antibiotics cause overall harm but nevertheless are still frequently prescribed.[78][79] Some of the reasons that antibiotics are so commonly prescribed include people's expectations for them, physicians' desire to help, and the difficulty in excluding complications that may be amenable to antibiotics.[80] There are no effective antiviral drugs for the common cold even though some preliminary research has shown benefits.[13][81]
Zinc
[edit]Zinc supplements may shorten the duration of colds by up to 33% and reduce the severity of symptoms if supplementation begins within 24 hours of the onset of symptoms.[11][55][82][83][84] Some zinc remedies directly applied to the inside of the nose have led to the loss of the sense of smell.[11][85] A 2017 review did not recommend the use of zinc for the common cold for various reasons;[20] whereas a 2017 and 2018 review both recommended the use of zinc, but also advocated further research on the topic.[82][83]
Alternative medicine
[edit]While there are many alternative medicines and Chinese herbal medicines supposed to treat the common cold, there is insufficient scientific evidence to support their use.[13][86] As of 2015, there is weak evidence to support nasal irrigation with saline.[87] There is no firm evidence that Echinacea products or garlic provide any meaningful benefit in treating or preventing colds.[88][89]
Vitamins C and D
[edit]Vitamin C supplementation does not affect the incidence of the common cold, but may reduce its duration if taken on a regular basis.[90] There is no conclusive evidence that vitamin D supplementation is efficacious in the prevention or treatment of respiratory tract infections.[91]
Prognosis
[edit]The common cold is generally mild and self-limiting with most symptoms generally improving in a week.[8] In children, half of cases resolve in 10 days and 90% in 15 days.[92] Severe complications, if they occur, are usually in the very old, the very young, or those who are immunosuppressed.[21] Secondary bacterial infections may occur resulting in sinusitis, pharyngitis, or an ear infection.[93] It is estimated that sinusitis occurs in 8% and ear infection in 30% of cases.[94]
Epidemiology
[edit]The common cold is the most common human disease[21] and affects people all over the globe.[40] Adults typically have two to three infections annually,[8] and children may have six to ten colds a year (and up to twelve colds a year for school children).[13] Rates of symptomatic infections increase in the elderly due to declining immunity.[41]
Weather
[edit]A common misconception is that one can "catch a cold" merely through prolonged exposure to cold weather.[95] Although it is now known that colds are viral infections, the prevalence of many such viruses are indeed seasonal, occurring more frequently during cold weather.[96] The reason for the seasonality has not been conclusively determined.[97] Possible explanations may include cold temperature-induced changes in the respiratory system,[98] decreased immune response,[99] and low humidity causing an increase in viral transmission rates, perhaps due to dry air allowing small viral droplets to disperse farther and stay in the air longer.[100]
The apparent seasonality may also be due to social factors, such as people spending more time indoors near infected people,[98] and especially children at school.[40][97] Although normal exposure to cold does not increase one's risk of infection, severe exposure leading to significant reduction of body temperature (hypothermia) may put one at a greater risk for the common cold: although controversial, the majority of evidence suggests that it may increase susceptibility to infection.[99]
History
[edit]
While the cause of the common cold was identified in the 1950s, the disease appears to have been with humanity since its early history.[22] Its symptoms and treatment are described in the Egyptian Ebers papyrus, the oldest existing medical text, written before the 16th century BCE.[102] The name "cold" came into use in the 16th century, due to the similarity between its symptoms and those of exposure to cold weather.[103]
In the United Kingdom, the Common Cold Unit (CCU) was set up by the Medical Research Council in 1946 and it was where the rhinovirus was discovered in 1956.[104] In the 1970s, the CCU demonstrated that treatment with interferon during the incubation phase of rhinovirus infection protects somewhat against the disease,[105] but no practical treatment could be developed. The unit was closed in 1989, two years after it completed research of zinc gluconate lozenges in the prevention and treatment of rhinovirus colds, the only successful treatment in the history of the unit.[106]
Research directions
[edit]Antivirals have been tested for effectiveness in the common cold; as of 2009, none had been both found effective and licensed for use.[81] There are trials of the anti-viral drug pleconaril which shows promise against picornaviruses as well as trials of BTA-798.[107] The oral form of pleconaril had safety issues and an aerosol form is being studied.[107] The genomes of all known human rhinovirus strains have been sequenced.[108]
Societal impact
[edit]The economic impact of the common cold is not well understood in much of the world.[94] In the United States, the common cold leads to 75–100 million physician visits annually at a conservative cost estimate of $7.7 billion per year. Americans spend $2.9 billion on over-the-counter drugs and another $400 million on prescription medicines for symptom relief.[109] More than one-third of people who saw a doctor received an antibiotic prescription, which has implications for antibiotic resistance.[109] An estimated 22–189 million school days are missed annually due to a cold. As a result, parents missed 126 million workdays to stay home to care for their children. When added to the 150 million workdays missed by employees who have a cold, the total economic impact of cold-related work loss exceeds $20 billion per year.[56][109] This accounts for 40% of time lost from work in the United States.[110]
References
[edit]Notes
- ^ Pramod JR (2008). Textbook of Oral Medicine. Jaypee Brothers Publishers. p. 336. ISBN 978-81-8061-562-7. Archived from the original on 29 May 2016.
- ^ Lee H, Kang B, Hong M, Lee HL, Choi JY, Lee JA (July 2020). "Eunkyosan for the common cold: A PRISMA-compliment systematic review of randomised, controlled trials". Medicine. 99 (31) e21415. doi:10.1097/MD.0000000000021415. PMC 7402720. PMID 32756141.
- ^ a b c d e f g h i j k l "Common Colds: Protect Yourself and Others". CDC. 6 October 2015. Archived from the original on 5 February 2016. Retrieved 4 February 2016.
- ^ a b c d e f g h i j Eccles R (November 2005). "Understanding the symptoms of the common cold and influenza". The Lancet. Infectious Diseases. 5 (11): 718–25. doi:10.1016/S1473-3099(05)70270-X. PMC 7185637. PMID 16253889.
- ^ a b Bennett JE, Dolin R, Blaser MJ (2014). Principles and Practice of Infectious Diseases. Elsevier Health Sciences. p. 750. ISBN 978-1-4557-4801-3. Archived from the original on 8 September 2017.
- ^ a b c d e f Allan GM, Arroll B (February 2014). "Prevention and treatment of the common cold: making sense of the evidence". CMAJ. 186 (3): 190–9. doi:10.1503/cmaj.121442. PMC 3928210. PMID 24468694.
- ^ a b c Heikkinen T, Järvinen A (January 2003). "The common cold". Lancet. 361 (9351): 51–9. doi:10.1016/S0140-6736(03)12162-9. PMC 7112468. PMID 12517470.
- ^ a b c d e f g h i Arroll B (March 2011). "Common cold". BMJ Clinical Evidence. 2011 (3): 1510. PMC 3275147. PMID 21406124.
Common colds are defined as upper respiratory tract infections that affect the predominantly nasal part of the respiratory mucosa
- ^ "Bronchiolitis: Symptoms and Causes". Mayo Clinic. Archived from the original on 3 May 2022. Retrieved 3 May 2022.
- ^ a b c d e Eccles p. 209
- ^ a b c d "Zinc – Fact Sheet for Health Professionals". Office of Dietary Supplements, US National Institutes of Health. 10 July 2019. Archived from the original on 25 March 2021. Retrieved 27 December 2019.
Although studies examining the effect of zinc treatment on cold symptoms have had somewhat conflicting results, overall zinc appears to be beneficial under certain circumstances.... In September of 2007, Caruso and colleagues published a structured review of the effects of zinc lozenges, nasal sprays, and nasal gels on the common cold [69]. Of the 14 randomized, placebo-controlled studies included, 7 (5 using zinc lozenges, 2 using a nasal gel) showed that the zinc treatment had a beneficial effect and 7 (5 using zinc lozenges, 1 using a nasal spray, and 1 using lozenges and a nasal spray) showed no effect. More recently, a Cochrane review concluded that "zinc (lozenges or syrup) is beneficial in reducing the duration and severity of the common cold in healthy people, when taken within 24 hours of onset of symptoms" [73]. The author of another review completed in 2004 also concluded that zinc can reduce the duration and severity of cold symptoms [68]. However, more research is needed to determine the optimal dosage, zinc formulation and duration of treatment before a general recommendation for zinc in the treatment of the common cold can be made [73]. As previously noted, the safety of intranasal zinc has been called into question because of numerous reports of anosmia (loss of smell), in some cases long-lasting or permanent, from the use of zinc-containing nasal gels or sprays [17–19].
- ^ a b c Kim SY, Chang YJ, Cho HM, Hwang YW, Moon YS (September 2015). "Non-steroidal anti-inflammatory drugs for the common cold". The Cochrane Database of Systematic Reviews. 2015 (9) CD006362. doi:10.1002/14651858.CD006362.pub4. PMC 10040208. PMID 26387658.
- ^ a b c d e f Simasek M, Blandino DA (February 2007). "Treatment of the common cold". American Family Physician. 75 (4): 515–20. PMID 17323712. Archived from the original on 26 September 2007.
- ^ "Common Cold". Centers for Disease Control and Prevention. Archived from the original on 1 February 2016. Retrieved 27 January 2021.
- ^ a b c d Eccles p. 112
- ^ "Cold Versus Flu". 11 August 2016. Archived from the original on 6 January 2017. Retrieved 5 January 2017.
- ^ "Colds: How to Prevent Them". Yale Medicine. Retrieved 21 November 2024.
- ^ "Common cold". nhs.uk. 18 October 2017. Retrieved 21 November 2024.
- ^ Harris AM, Hicks LA, Qaseem A (March 2016). "Appropriate Antibiotic Use for Acute Respiratory Tract Infection in Adults: Advice for High-Value Care From the American College of Physicians and the Centers for Disease Control and Prevention". Annals of Internal Medicine. 164 (6): 425–34. doi:10.7326/M15-1840. PMID 26785402. S2CID 746771.
- ^ a b Malesker MA, Callahan-Lyon P, Ireland B, Irwin RS (November 2017). "Pharmacologic and Nonpharmacologic Treatment for Acute Cough Associated With the Common Cold: CHEST Expert Panel Report". Chest. 152 (5): 1021–1037. doi:10.1016/j.chest.2017.08.009. PMC 6026258. PMID 28837801.
A suggestion for the use of zinc lozenges in healthy adults with cough due to common cold was considered by the expert panel. However, due to weak evidence, the potential side effects of zinc, and the relatively benign and common nature of the condition being treated, the panel did not approve inclusion of this suggestion.
- ^ a b c Eccles p. 1
- ^ a b Eccles R, Weber O (2009). Common cold. Basel: Birkhäuser. p. 3. ISBN 978-3-7643-9894-1. Archived from the original on 8 May 2016.
- ^ a b Eccles p. 24
- ^ Eccles p. 26
- ^ Eccles p. 129
- ^ Eccles p. 50
- ^ Eccles p. 30
- ^ Helms RA, ed. (2006). Textbook of therapeutics: drug and disease management (8. ed.). Philadelphia, Pa. [u.a.]: Lippincott Williams & Wilkins. p. 1882. ISBN 978-0-7817-5734-8. Archived from the original on 30 April 2016.
- ^ Turner RB, Hayden FG (2003). "Rhinovirus". In Rübsamen-Waigmann H, et al. (eds.). Viral Infections and Treatment. New York: CRC Press. p. 111. ISBN 978-0-8247-4247-8. Archived from the original on 4 May 2016.
- ^ Ebell MH, Lundgren J, Youngpairoj S (2013). "How long does a cough last? Comparing patients' expectations with data from a systematic review of the literature". Annals of Family Medicine. 11 (1): 5–13. doi:10.1370/afm.1430. PMC 3596033. PMID 23319500.
- ^ Dicpinigaitis PV (May 2011). "Cough: an unmet clinical need". British Journal of Pharmacology. 163 (1): 116–24. doi:10.1111/j.1476-5381.2010.01198.x. PMC 3085873. PMID 21198555.
- ^ Goldsobel AB, Chipps BE (March 2010). "Cough in the pediatric population". The Journal of Pediatrics. 156 (3): 352–8. doi:10.1016/j.jpeds.2009.12.004. PMID 20176183.
- ^ Palmenberg AC, Spiro D, Kuzmickas R, Wang S, Djikeng A, Rathe JA, et al. (April 2009). "Sequencing and analyses of all known human rhinovirus genomes reveal structure and evolution". Science. 324 (5923): 55–9. Bibcode:2009Sci...324...55P. doi:10.1126/science.1165557. PMC 3923423. PMID 19213880.
- ^ a b Janicki-Deverts D, Crittenden CN (2020). "Common Cold: Cause". In Gellman MD (ed.). Encyclopedia of Behavioral Medicine (2nd ed.). Springer. p. 504. doi:10.1007/978-3-030-39903-0_795. ISBN 978-3-030-39901-6. S2CID 242944824.
- ^ Eccles p. 107
- ^ a b c Eccles R, Weber O (2009). Common cold (Online-Ausg. ed.). Basel: Birkhäuser. p. 197. ISBN 978-3-7643-9894-1. Archived from the original on 2 May 2016.
- ^ a b Eccles pp. 211, 215
- ^ a b Wang CC, Prather KA, Sznitman J, Jimenez JL, Lakdawala SS, Tufekci Z, Marr LC (27 August 2021). "Airborne transmission of respiratory viruses". Science. 373 (6558) eabd9149. doi:10.1126/science.abd9149. PMC 8721651. PMID 34446582.
- ^ Allen TR, Bradburne AF, Stott EJ, Goodwin CS, Tyrrell DA (December 1973). "An outbreak of common colds at an Antarctic base after seventeen weeks of complete isolation". The Journal of Hygiene. 71 (4): 657–67. doi:10.1017/s0022172400022920. PMC 2130424. PMID 4520509.
- ^ a b c d Papadopoulos NG, Xatzipsaltis M, Johnston SL (2009). "Rhinoviruses". In Zuckerman AJ, et al. (eds.). Principles and Practice of Clinical Virology (6th ed.). John Wiley & Sons. p. 496. ISBN 978-0-470-74139-9. Archived from the original on 3 June 2016.
- ^ a b c Eccles p. 78
- ^ Eccles p. 166
- ^ Cohen S, Doyle WJ, Alper CM, Janicki-Deverts D, Turner RB (January 2009). "Sleep habits and susceptibility to the common cold". Archives of Internal Medicine. 169 (1): 62–7. doi:10.1001/archinternmed.2008.505. PMC 2629403. PMID 19139325.
- ^ Eccles pp. 160–65
- ^ McNiel ME, Labbok MH, Abrahams SW (July 2010). "What are the risks associated with formula feeding? A re-analysis and review". Breastfeeding Review. 18 (2): 25–32. PMID 20879657.
- ^ Lawrence RA, Lawrence RM (2010). Breastfeeding: A guide for the medical profession (7th ed.). Maryland Heights, Mo.: Mosby/Elsevier. p. 478. ISBN 978-1-4377-3590-1. Archived from the original on 17 June 2016.
- ^ Nelson KE, Williams CM (2007), Infectious Disease Epidemiology: Theory and Practice (2nd ed.), Jones & Bartlett Learning, pp. 724–, ISBN 978-0-7637-2879-3, archived from the original on 20 May 2016
- ^ a b Eccles p. 116
- ^ a b Eccles p. 122
- ^ Eccles pp. 51–52
- ^ CDC (11 February 2019). "Common Colds". Centers for Disease Control and Prevention. Archived from the original on 27 September 2020. Retrieved 18 September 2020.
- ^ Montesinos-Guevara C, Buitrago-Garcia D, Felix ML, Guerra CV, Hidalgo R, Martinez-Zapata MJ, Simancas-Racines D (14 December 2022). "Vaccines for the common cold". The Cochrane Database of Systematic Reviews. 2022 (12) CD002190. doi:10.1002/14651858.CD002190.pub6. ISSN 1469-493X. PMC 9749450. PMID 36515550.
- ^ Lawrence DM (2009). "Gene studies shed light on rhinovirus diversity". Lancet Infect Dis. 9 (5): 278. doi:10.1016/S1473-3099(09)70123-9.
- ^ a b c Jefferson T, Dooley L, Ferroni E, Al-Ansary LA, van Driel ML, Bawazeer GA, Jones MA, Hoffmann TC, Clark J, Beller EM, Glasziou PP, Conly JM (30 January 2023). "Physical interventions to interrupt or reduce the spread of respiratory viruses". The Cochrane Database of Systematic Reviews. 1 (1) CD006207. doi:10.1002/14651858.CD006207.pub6. ISSN 1469-493X. PMC 9885521. PMID 36715243.
- ^ a b Singh M, Das RR (June 2013). Singh M (ed.). "Zinc for the common cold". The Cochrane Database of Systematic Reviews (6) CD001364. doi:10.1002/14651858.CD001364.pub4. PMID 23775705. (Retracted, see doi:10.1002/14651858.CD001364.pub5, PMID 25924708, Retraction Watch)
- ^ a b "Common Cold". National Institute of Allergy and Infectious Diseases. 27 November 2006. Archived from the original on 6 September 2008. Retrieved 11 June 2007.
- ^ Eccles p. 261
- ^ "Common Cold: Treatments and Drugs". Mayo Clinic. Archived from the original on 12 February 2010. Retrieved 9 January 2010.
- ^ Eccles R (August 2006). "Efficacy and safety of over-the-counter analgesics in the treatment of common cold and flu". Journal of Clinical Pharmacy and Therapeutics. 31 (4): 309–19. doi:10.1111/j.1365-2710.2006.00754.x. PMID 16882099. S2CID 22793984.
- ^ Li S, Yue J, Dong BR, Yang M, Lin X, Wu T (July 2013). "Acetaminophen (paracetamol) for the common cold in adults". The Cochrane Database of Systematic Reviews. 2013 (7) CD008800. doi:10.1002/14651858.CD008800.pub2. PMC 7389565. PMID 23818046.
- ^ Smith SM, Schroeder K, Fahey T (November 2014). "Over-the-counter (OTC) medications for acute cough in children and adults in community settings". The Cochrane Database of Systematic Reviews. 2014 (11) CD001831. doi:10.1002/14651858.CD001831.pub5. PMC 7061814. PMID 25420096.
- ^ a b Shefrin AE, Goldman RD (November 2009). "Use of over-the-counter cough and cold medications in children" (PDF). Canadian Family Physician. 55 (11): 1081–3. PMC 2776795. PMID 19910592. Archived (PDF) from the original on 23 September 2015.
- ^ Vassilev ZP, Kabadi S, Villa R (March 2010). "Safety and efficacy of over-the-counter cough and cold medicines for use in children". Expert Opinion on Drug Safety. 9 (2): 233–42. doi:10.1517/14740330903496410. PMID 20001764. S2CID 12952868.
- ^ Eccles p. 246
- ^ Hayward G, Thompson MJ, Perera R, Del Mar CB, Glasziou PP, Heneghan CJ (October 2015). "Corticosteroids for the common cold" (PDF). The Cochrane Database of Systematic Reviews. 2016 (10) CD008116. doi:10.1002/14651858.cd008116.pub3. PMC 8734596. PMID 26461493. Archived (PDF) from the original on 9 November 2020. Retrieved 12 December 2019.
- ^ a b c Deckx L, De Sutter AI, Guo L, Mir NA, van Driel ML (October 2016). "Nasal decongestants in monotherapy for the common cold". The Cochrane Database of Systematic Reviews. 2016 (10) CD009612. doi:10.1002/14651858.CD009612.pub2. PMC 6461189. PMID 27748955.
- ^ De Sutter AI, Saraswat A, van Driel ML (November 2015). "Antihistamines for the common cold". The Cochrane Database of Systematic Reviews. 2015 (11) CD009345. doi:10.1002/14651858.CD009345.pub2. hdl:1854/LU-7237869. PMC 9468790. PMID 26615034. Archived from the original on 5 May 2020. Retrieved 12 December 2019.
- ^ Taverner D, Latte J (January 2007). Latte GJ (ed.). "Nasal decongestants for the common cold". The Cochrane Database of Systematic Reviews (1) CD001953. doi:10.1002/14651858.CD001953.pub3. PMID 17253470.
- ^ De Sutter AI, Eriksson L, van Driel ML (21 January 2022). "Oral antihistamine-decongestant-analgesic combinations for the common cold". The Cochrane Database of Systematic Reviews. 1 (1) CD004976. doi:10.1002/14651858.CD004976.pub4. ISSN 1469-493X. PMC 8780136. PMID 35060618.
- ^ AlBalawi ZH, Othman SS, Alfaleh K (June 2013). "Intranasal ipratropium bromide for the common cold". The Cochrane Database of Systematic Reviews. 2013 (6) CD008231. doi:10.1002/14651858.CD008231.pub3. PMC 6492479. PMID 23784858.
- ^ DeGeorge KC, Ring DJ, Dalrymple SN (September 2019). "Treatment of the Common Cold". American Family Physician. 100 (5): 281–289. PMID 31478634.
- ^ Guppy MP, Mickan SM, Del Mar CB, Thorning S, Rack A (February 2011). Guppy MP (ed.). "Advising patients to increase fluid intake for treating acute respiratory infections". The Cochrane Database of Systematic Reviews. 2011 (2) CD004419. doi:10.1002/14651858.CD004419.pub3. PMC 7197045. PMID 21328268.
- ^ Singh M, Singh M, Jaiswal N, Chauhan A (August 2017). "Heated, humidified air for the common cold". The Cochrane Database of Systematic Reviews. 2017 (8) CD001728. doi:10.1002/14651858.CD001728.pub6. PMC 6483632. PMID 28849871.
- ^ Paul IM, Beiler JS, King TS, Clapp ER, Vallati J, Berlin CM (December 2010). "Vapor rub, petrolatum, and no treatment for children with nocturnal cough and cold symptoms". Pediatrics. 126 (6): 1092–9. doi:10.1542/peds.2010-1601. PMC 3600823. PMID 21059712.
- ^ a b Laskowski ER (9 February 2017). "Is it OK to exercise if I have a cold?". Mayo Clinic. Archived from the original on 19 July 2017. Retrieved 4 July 2017.
- ^ a b "Clearing the Air on Exercise and the Common Cold". American College of Sports Medicine. Archived from the original on 22 July 2017. Retrieved 4 July 2017.
- ^ "Hot drinks ease cold and flu". National Health Service. 10 December 2008. Archived from the original on 25 November 2020. Retrieved 27 January 2021.
- ^ a b Kenealy T, Arroll B (June 2013). "Antibiotics for the common cold and acute purulent rhinitis". The Cochrane Database of Systematic Reviews. 2013 (6) CD000247. doi:10.1002/14651858.CD000247.pub3. PMC 7044720. PMID 23733381.
- ^ Eccles p. 238
- ^ Eccles p. 234
- ^ a b Eccles p. 218
- ^ a b Rondanelli M, Miccono A, Lamburghini S, Avanzato I, Riva A, Allegrini P, et al. (2018). "Self-Care for Common Colds: The Pivotal Role of Vitamin D, Vitamin C, Zinc, and Echinacea in Three Main Immune Interactive Clusters (Physical Barriers, Innate and Adaptive Immunity) Involved during an Episode of Common Colds-Practical Advice on Dosages and on the Time to Take These Nutrients/Botanicals in order to Prevent or Treat Common Colds". Evidence-Based Complementary and Alternative Medicine. 2018 5813095. doi:10.1155/2018/5813095. PMC 5949172. PMID 29853961.
Considering zinc, the supplementation may shorten the duration of colds by approximately 33%. CC patients may be instructed to try zinc within 24 hours of onset of symptoms.
- ^ a b Hemilä H, Fitzgerald JT, Petrus EJ, Prasad A (2017). "Zinc Acetate Lozenges May Improve the Recovery Rate of Common Cold Patients: An Individual Patient Data Meta-Analysis". Open Forum Infectious Diseases. 4 (2) ofx059. doi:10.1093/ofid/ofx059. PMC 5410113. PMID 28480298.
The 3-fold increase in the rate of recovery from the common cold is a clinically important effect. The optimal formulation of zinc lozenges and an ideal frequency of their administration should be examined. Given the evidence of efficacy, common cold patients may be instructed to try zinc acetate lozenges within 24 hours of onset of symptoms.
- ^ Hemilä H, Petrus EJ, Fitzgerald JT, Prasad A (November 2016). "Zinc acetate lozenges for treating the common cold: an individual patient data meta-analysis". British Journal of Clinical Pharmacology. 82 (5): 1393–1398. doi:10.1111/bcp.13057. PMC 5061795. PMID 27378206.
- ^ "Loss of Sense of Smell with Intranasal Cold Remedies Containing Zinc". Food and Drug Administration. 2009. Archived from the original on 4 June 2015.
- ^ Wu T, Zhang J, Qiu Y, Xie L, Liu GJ (January 2007). "Chinese medicinal herbs for the common cold". The Cochrane Database of Systematic Reviews (1) CD004782. doi:10.1002/14651858.CD004782.pub2. PMID 17253524.
- ^ King D, Mitchell B, Williams CP, Spurling GK (April 2015). "Saline nasal irrigation for acute upper respiratory tract infections" (PDF). The Cochrane Database of Systematic Reviews. 2015 (4) CD006821. doi:10.1002/14651858.CD006821.pub3. PMC 9475221. PMID 25892369. Archived (PDF) from the original on 5 May 2020. Retrieved 30 December 2018.
- ^ Karsch-Völk M, Barrett B, Kiefer D, Bauer R, Ardjomand-Woelkart K, Linde K (February 2014). "Echinacea for preventing and treating the common cold". The Cochrane Database of Systematic Reviews (Systematic review). 2 (2) CD000530. doi:10.1002/14651858.CD000530.pub3. PMC 4068831. PMID 24554461.
- ^ Lissiman E, Bhasale AL, Cohen M (November 2014). Lissiman E (ed.). "Garlic for the common cold". The Cochrane Database of Systematic Reviews. 11 (11) CD006206. doi:10.1002/14651858.CD006206.pub4. PMC 6465033. PMID 25386977.
- ^ Hemilä H, Chalker E (January 2013). "Vitamin C for preventing and treating the common cold". The Cochrane Database of Systematic Reviews. 1 (1) CD000980. doi:10.1002/14651858.CD000980.pub4. PMC 1160577. PMID 23440782.
- ^ Bradley R, Schloss J, Brown D, Celis D, Finnell J, Hedo R, et al. (December 2020). "The effects of vitamin D on acute viral respiratory infections: A rapid review". Advances in Integrative Medicine. 7 (4): 192–202. doi:10.1016/j.aimed.2020.07.011. PMC 7397989. PMID 32837896.
- ^ Thompson M, Vodicka TA, Blair PS, Buckley DI, Heneghan C, Hay AD (December 2013). "Duration of symptoms of respiratory tract infections in children: systematic review". BMJ. 347 f7027. doi:10.1136/bmj.f7027. PMC 3898587. PMID 24335668.
- ^ Eccles p. 76
- ^ a b Eccles p. 90
- ^ Zuger A (4 March 2003). "'You'll Catch Your Death!' An Old Wives' Tale? Well." The New York Times. Archived from the original on 22 March 2017.
- ^ Eccles p. 79
- ^ a b "Common cold – Background information". National Institute for Health and Clinical Excellence. Archived from the original on 15 November 2012. Retrieved 19 March 2013.
- ^ a b Eccles p. 80
- ^ a b Mourtzoukou EG, Falagas ME (September 2007). "Exposure to cold and respiratory tract infections". The International Journal of Tuberculosis and Lung Disease. 11 (9): 938–43. PMID 17705968.
- ^ Eccles p. 157
- ^ "The Cost of the Common Cold and Influenza". Imperial War Museum: Posters of Conflict. vads. Archived from the original on 27 July 2011.
- ^ Eccles p. 6
- ^ "Cold". Online Etymology Dictionary. Archived from the original on 24 October 2007. Retrieved 12 January 2008.
- ^ Eccles p. 20
- ^ Tyrrell DA (1987). "Interferons and their clinical value". Reviews of Infectious Diseases. 9 (2): 243–9. doi:10.1093/clinids/9.2.243. PMID 2438740.
- ^ Al-Nakib W, Higgins PG, Barrow I, Batstone G, Tyrrell DA (December 1987). "Prophylaxis and treatment of rhinovirus colds with zinc gluconate lozenges". The Journal of Antimicrobial Chemotherapy. 20 (6): 893–901. doi:10.1093/jac/20.6.893. PMC 7110079. PMID 3440773.
- ^ a b Eccles p. 226
- ^ Willingham V (12 February 2009). "Genetic map of cold virus a step toward cure, scientists say". CNN. Archived from the original on 26 April 2009. Retrieved 28 April 2009.
- ^ a b c Fendrick AM, Monto AS, Nightengale B, Sarnes M (February 2003). "The economic burden of non-influenza-related viral respiratory tract infection in the United States". Archives of Internal Medicine. 163 (4): 487–94. doi:10.1001/archinte.163.4.487. PMID 12588210. S2CID 10169748.
- ^ Kirkpatrick GL (December 1996). "The common cold". Primary Care. 23 (4): 657–75. doi:10.1016/S0095-4543(05)70355-9. PMC 7125839. PMID 8890137.
Bibliography
- Eccles R, Weber O, eds. (2009). Common Cold (Illustrated ed.). Springer Science & Business Media. ISBN 978-3-7643-9912-2.