Recent from talks
Contribute something
Nothing was collected or created yet.
Addiction
View on Wikipedia
| Addiction | |
|---|---|
 | |
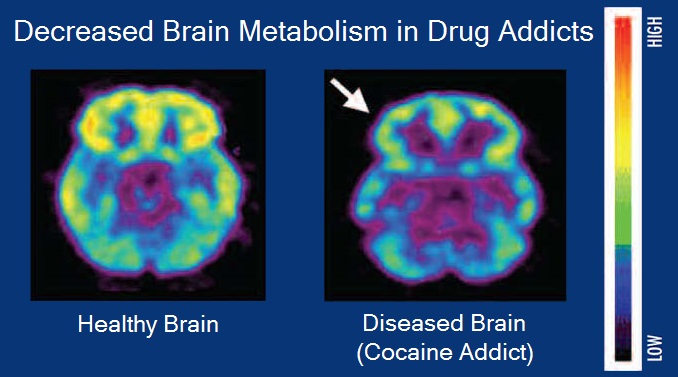
| Brain positron emission tomography images that compare brain metabolism in a healthy individual and an individual with a cocaine addiction | |
| Specialty | Psychiatry, clinical psychology, toxicology, addiction medicine |
| Symptoms | Recurring compulsion to engage in rewarding activity despite negative consequences |
| Risk factors | Family history, adverse childhood experiences, attention deficit hyperactivity disorder |
| Treatment | Cognitive behavioral therapy, behavior modification, medication |
Addiction is a neuropsychological disorder characterized by a persistent and intense urge to use a drug or engage in a behavior that produces natural reward, despite substantial harm and other negative consequences. Repetitive drug use can alter brain function in synapses similar to natural rewards like food or falling in love[1] in ways that perpetuate craving and weakens self-control for people with pre-existing vulnerabilities.[2] This phenomenon – drugs reshaping brain function – has led to an understanding of addiction as a brain disorder with a complex variety of psychosocial as well as neurobiological factors that are implicated in the development of addiction.[3][4][5] While mice given cocaine showed the compulsive and involuntary nature of addiction,[a] for humans this is more complex, related to behavior[6] or personality traits.[7]
Classic signs of addiction include compulsive engagement in rewarding stimuli, preoccupation with substances or behavior, and continued use despite negative consequences. Habits and patterns associated with addiction are typically characterized by immediate gratification (short-term reward),[8][9] coupled with delayed deleterious effects (long-term costs).[4][10]
Examples of substance addiction include alcoholism, cannabis addiction, amphetamine addiction, cocaine addiction, nicotine addiction, opioid addiction, and eating or food addiction. Behavioral addictions may include gambling addiction, shopping addiction, stalking, pornography addiction, internet addiction, social media addiction, video game addiction, and sexual addiction. The DSM-5 and ICD-10 only recognize gambling addictions as behavioral addictions, but the ICD-11 also recognizes gaming addictions.[11]
Signs and symptoms
[edit]Signs and symptoms of drug addiction can vary depending on the type of addiction. Symptoms may include:
- Continuation of drug use despite the knowledge of consequences[12]
- Disregarding financial status when it comes to drug purchases
- Ensuring a stable supply of the drug
- Needing more of the drug over time to achieve similar effects[12]
- Social and work life impacted due to drug use[12]
- Unsuccessful attempts to stop drug use[12]
- Urge to use drug regularly
Other signs and symptoms can be categorized across relevant dimensions:
| Behavioral Changes | Physical Changes | Social Changes |
|---|---|---|
|
|
|
Substance use disorder
[edit]| Addiction and dependence glossary[3][14][15] | |
|---|---|
| |
The DSM-5 discourages using the term "drug addiction" because of its "uncertain definition and its potentially negative connotation" and prefers the term "substance use disorder" to describe the wide range of the disorder, from a mild form to a severe state of chronically relapsing, compulsive pattern of drug taking.[16]
SUD, belongs to the class of substance-related disorders, is a chronic and relapsing brain disorder that features drug seeking and drug abuse, despite their harmful effects.[17] This form of addiction changes brain circuitry such that the brain's reward system is compromised,[18] causing functional consequences for stress management and self-control.[17] Damage to the functions of the organs involved can persist throughout a lifetime and cause death if untreated.[17] Substances involved with drug addiction include alcohol, nicotine, marijuana, opioids, cocaine, amphetamines, and even foods with high fat and sugar content.[19] Addictions can begin experimentally in social contexts[20] and can arise from the use of prescribed medications or a variety of other measures.[21]
It has been shown to work in phenomenological, conditioning (operant and classical), cognitive models, and the cue reactivity model. However, no one model completely illustrates substance abuse.[22]
Risk factors for addiction include:
- Aggressive behavior (particularly in childhood)
- Availability of substance[20]
- Community economic status[citation needed]
- Experimentation[20]
- Epigenetics
- Impulsivity (attentional, motor, or non-planning)[23]
- Lack of parental supervision[20]
- Lack of peer refusal skills[20]
- Mental disorders[20]
- Method substance is taken[17]
- Usage of substance in youth[20]
Food addiction
[edit]The diagnostic criteria for food or eating addiction has not been categorized or defined in references such as the Diagnostic and Statistical Manual of Mental Disorders (DSM or DSM-5) and is based on subjective experiences similar to substance use disorders.[12][23] Food addiction may be found in those with eating disorders, though not all people with eating disorders have food addiction and not all of those with food addiction have a diagnosed eating disorder.[12] Long-term frequent and excessive consumption of foods high in fat, salt, or sugar, such as chocolate, can produce an addiction[24][25] similar to drugs since they trigger the brain's reward system, such that the individual may desire the same foods to an increasing degree over time.[26][12][23] The signals sent when consuming highly palatable foods have the ability to counteract the body's signals for fullness and persistent cravings will result.[26] Those who show signs of food addiction may develop food tolerances, in which they eat more, despite the food becoming less satisfactory.[26]
Chocolate's sweet flavor and pharmacological ingredients are known to create a strong craving or feel 'addictive' by the consumer.[27] A person who has a strong liking for chocolate may refer to themselves as a chocoholic.
Risk factors for developing food addiction include excessive overeating and impulsivity.[23]
The Yale Food Addiction Scale (YFAS), version 2.0, is the current standard measure for assessing whether an individual exhibits signs and symptoms of food addiction.[28][12][23] It was developed in 2009 at Yale University on the hypothesis that foods high in fat, sugar, and salt have addictive-like effects which contribute to problematic eating habits.[29][26] The YFAS is designed to address 11 substance-related and addictive disorders (SRADs) using a 25-item self-report questionnaire, based on the diagnostic criteria for SRADs as per DSM-5.[30][12] A potential food addiction diagnosis is predicted by the presence of at least two out of 11 SRADs and a significant impairment to daily activities.[31]
The Barratt Impulsiveness Scale, specifically the BIS-11 scale, and the UPPS-P Impulsive Behavior subscales of Negative Urgency and Lack of Perseverance have been shown to have relation to food addiction.[23]
Behavioral addiction
[edit]The term behavioral addiction refers to a compulsion to engage in a natural reward – which is a behavior that is inherently rewarding (i.e., desirable or appealing) – despite adverse consequences.[9][24][25] Preclinical evidence has demonstrated that marked increases in the expression of ΔFosB through repetitive and excessive exposure to a natural reward induces the same behavioral effects and neuroplasticity as occurs in a drug addiction.[24][32][33][34]
Addiction can exist without psychotropic drugs, an idea that was popularized by psychologist Stanton Peele.[35] These are termed behavioral addictions. Such addictions may be passive or active, but they commonly contain reinforcing features, which are found in most addictions.[35] Sexual behavior, eating, gambling, playing video games, and shopping are all associated with compulsive behaviors in humans and have been shown to activate the mesolimbic pathway and other parts of the reward system.[24] Based on this evidence, sexual addiction, gambling addiction, video game addiction, and shopping addiction are classified accordingly.[24]
Causes
[edit]Personality theories
[edit]Personality theories of addiction are psychological models that associate personality traits or modes of thinking (i.e., affective states) with an individual's proclivity for developing an addiction. Data analysis demonstrates that psychological profiles of drug users and non-users have significant differences and the psychological predisposition to using different drugs may be different.[36] Models of addiction risk that have been proposed in psychology literature include: an affect dysregulation model of positive and negative psychological affects, the reinforcement sensitivity theory of impulsiveness and behavioral inhibition, and an impulsivity model of reward sensitization and impulsiveness.[37][38][39][40][41]
Neuropsychology
[edit]The transtheoretical model of change (TTM) can point to how someone may be conceptualizing their addiction and the thoughts around it, including not being aware of their addiction.[42]
Cognitive control and stimulus control, which is associated with operant and classical conditioning, represent opposite processes (i.e., internal vs external or environmental, respectively) that compete over the control of an individual's elicited behaviors.[43] Cognitive control, and particularly inhibitory control over behavior, is impaired in both addiction and attention deficit hyperactivity disorder.[44][45] Stimulus-driven behavioral responses (i.e., stimulus control) that are associated with a particular rewarding stimulus tend to dominate one's behavior in an addiction.[45]
| Operant conditioning | Extinction | ||||||||||||||||||||||||||||||
| Reinforcement Increase behavior | Punishment Decrease behavior | ||||||||||||||||||||||||||||||
| Positive reinforcement Add appetitive stimulus following correct behavior | Negative reinforcement | Positive punishment Add noxious stimulus following behavior | Negative punishment Remove appetitive stimulus following behavior | ||||||||||||||||||||||||||||
| Escape Remove noxious stimulus following correct behavior | Active avoidance Behavior avoids noxious stimulus | ||||||||||||||||||||||||||||||
Stimulus control of behavior
[edit]In operant conditioning, behavior is influenced by outside stimulus, such as a drug. The operant conditioning theory of learning is useful in understanding why the mood-altering or stimulating consequences of drug use can reinforce continued use (an example of positive reinforcement) and why the addicted person seeks to avoid withdrawal through continued use (an example of negative reinforcement). Stimulus control is using the absence of the stimulus or presence of a reward to influence the resulting behavior.[42]
Cognitive control of behavior
[edit]Cognitive control is the intentional selection of thoughts, behaviors, and emotions, based on our environment. It has been shown that drugs alter the way our brains function, and its structure.[46][18] Cognitive functions such as learning, memory, and impulse control, are affected by drugs.[46] These effects promote drug use, as well as hinder the ability to abstain from it.[46] The increase in dopamine release is prominent in drug use, specifically in the ventral striatum and the nucleus accumbens.[46] Dopamine is responsible for producing pleasurable feelings, as well driving us to perform important life activities. Addictive drugs cause a significant increase in this reward system, causing a large increase in dopamine signaling as well as increase in reward-seeking behavior, in turn motivating drug use.[46][18] This promotes the development of a maladaptive drug to stimulus relationship.[47] Early drug use leads to these maladaptive associations, later affecting cognitive processes used for coping, which are needed to successfully abstain from them.[46][42]
Evolutionary perspectives
[edit]Some scholars have proposed evolutionary explanations for addiction, suggesting that vulnerabilities to substance or behavioural dependence reflect by-products or dysregulated expressions of reward and learning systems that were adaptive in ancestral environments. Classic accounts argue that purified drugs and rapid delivery methods exploit ancient motivational circuitry by providing "false fitness signals" that mimic cues once linked to survival or reproduction.[48] Other reviews emphasise how psychoactive substances and behavioural reinforcers act on conserved mechanisms for reward, reinforcement, and emotion, which in modern settings can be overstimulated or maladapted.[49][50] These perspectives do not replace proximate neurobiological models, but aim instead to situate contemporary patterns of vulnerability within a broader evolutionary framework.[51][52]
Risk factors
[edit]A number of genetic and environmental risk factors exist for developing an addiction.[3][53] Genetic and environmental risk factors each account for roughly half of an individual's risk for developing an addiction;[3] the contribution from epigenetic risk factors to the total risk is unknown.[53] Even in individuals with a relatively low genetic risk, exposure to sufficiently high doses of an addictive drug for a long period of time (e.g., weeks–months) can result in an addiction.[3] Adverse childhood events are associated with negative health outcomes, such as substance use disorder. Childhood abuse or exposure to violent crime is related to developing a mood or anxiety disorder, as well as a substance dependence risk.[54]
Genetic factors
[edit]Genetic factors, along with socio-environmental (e.g., psychosocial) factors, have been established as significant contributors to addiction vulnerability.[3][53][55][12] Studies done on 350 hospitalized drug-dependent patients showed that over half met the criteria for alcohol abuse, with a role of familial factors being prevalent.[56] Genetic factors account for 40–60% of the risk factors for alcoholism.[57] Similar rates of heritability for other types of drug addiction have been indicated, specifically in genes that encode the Alpha5 Nicotinic Acetylcholine Receptor.[58] Knestler hypothesized in 1964 that a gene or group of genes might contribute to predisposition to addiction in several ways. For example, altered levels of a normal protein due to environmental factors may change the structure or functioning of specific brain neurons during development. These altered brain neurons could affect the susceptibility of an individual to an initial drug use experience. In support of this hypothesis, animal studies have shown that environmental factors such as stress can affect an animal's genetic expression.[58]
In humans, twin studies into addiction have provided some of the highest-quality evidence of this link, with results finding that if one twin is affected by addiction, the other twin is likely to be as well, and to the same substance.[59] Further evidence of a genetic component is research findings from family studies which suggest that if one family member has a history of addiction, the chances of a relative or close family developing those same habits are much higher than one who has not been introduced to addiction at a young age.[60]
The data implicating specific genes in the development of drug addiction is mixed for most genes. Many addiction studies that aim to identify specific genes focus on common variants with an allele frequency of greater than 5% in the general population. When associated with disease, these only confer a small amount of additional risk with an odds ratio of 1.1–1.3 percent; this has led to the development the rare variant hypothesis, which states that genes with low frequencies in the population (<1%) confer much greater additional risk in the development of the disease.[61]
Genome-wide association studies (GWAS) are used to examine genetic associations with dependence, addiction, and drug use.[55] These studies rarely identify genes from proteins previously described via animal knockout models and candidate gene analysis. Instead, large percentages of genes involved in processes such as cell adhesion are commonly identified. The important effects of endophenotypes are typically not capable of being captured by these methods. Genes identified in GWAS for drug addiction may be involved either in adjusting brain behavior before drug experiences, subsequent to them, or both.[62]
Environmental factors
[edit]Environmental risk factors for addiction are the experiences of an individual during their lifetime that interact with the individual's genetic composition to increase or decrease his or her vulnerability to addiction.[3] For example, after the nationwide[where?] outbreak of COVID-19, more people quit (vs. started) smoking; and smokers, on average, reduced the quantity of cigarettes they consumed.[63] More generally, a number of different environmental factors have been implicated as risk factors for addiction, including various psychosocial stressors. The National Institute on Drug Abuse (NIDA) and studies cite lack of parental supervision, the prevalence of peer substance use, substance availability, and poverty as risk factors for substance use among children and adolescents.[64][20] The brain disease model of addiction posits that an individual's exposure to an addictive drug is the most significant environmental risk factor for addiction.[65] Many researchers, including neuroscientists, indicate that the brain disease model presents a misleading, incomplete, and potentially detrimental explanation of addiction.[66]
The psychoanalytic theory model defines addiction as a form of defense against feelings of hopelessness and helplessness as well as a symptom of failure to regulate powerful emotions related to adverse childhood experiences (ACEs), various forms of maltreatment and dysfunction experienced in childhood. In this case, the addictive substance provides brief but total relief and positive feelings of control.[42] The Adverse Childhood Experiences Study by the Centers for Disease Control and Prevention has shown a strong dose–response relationship between ACEs and numerous health, social, and behavioral problems throughout a person's lifespan, including substance use disorder.[67] Children's neurological development can be permanently disrupted when they are chronically exposed to stressful events such as physical, emotional, or sexual abuse, physical or emotional neglect, witnessing violence in the household, or a parent being incarcerated or having a mental illness. As a result, the child's cognitive functioning or ability to cope with negative or disruptive emotions may be impaired. Over time, the child may adopt substance use as a coping mechanism or as a result of reduced impulse control, particularly during adolescence.[67][20][42] Vast amounts of children who experienced abuse have gone on to have some form of addiction in their adolescence or adult life.[68] This pathway towards addiction that is opened through stressful experiences during childhood can be avoided by a change in environmental factors throughout an individual's life and opportunities of professional help.[68] If one has friends or peers who engage in drug use favorably, the chances of them developing an addiction increases. Family conflict and home management is a cause for one to become engaged in drug use.[69]
Social control theory
[edit]According to Travis Hirschi's social control theory, adolescents with stronger attachments to family, religious, academic, and other social institutions are less likely to engage in delinquent and maladaptive behavior such as drug use leading to addiction.[70]
Age
[edit]Adolescence represents a period of increased vulnerability for developing an addiction.[71] In adolescence, the incentive-rewards systems in the brain mature well before the cognitive control center. This consequentially grants the incentive-rewards systems a disproportionate amount of power in the behavioral decision-making process. Therefore, adolescents are increasingly likely to act on their impulses and engage in risky, potentially addictive behavior before considering the consequences.[72] Not only are adolescents more likely to initiate and maintain drug use, but once addicted they are more resistant to treatment and more liable to relapse.[73][74]
Most individuals are exposed to and use addictive drugs for the first time during their teenage years.[75] In the United States, there were just over 2.8 million new users of illicit drugs in 2013 (7,800 new users per day);[75] among them, 54.1% were under 18 years of age.[75] In 2011, there were approximately 20.6 million people in the United States over the age of 12 with an addiction.[76] Over 90% of those with an addiction began drinking, smoking or using illicit drugs before the age of 18.[76]
Comorbid disorders
[edit]Individuals with comorbid (i.e., co-occurring) mental health disorders such as depression, anxiety, attention-deficit/hyperactivity disorder (ADHD) or post-traumatic stress disorder are more likely to develop substance use disorders.[77][78][79][20] The NIDA cites early aggressive behavior as a risk factor for substance use.[64] The National Bureau of Economic Research found that there is a "definite connection between mental illness and the use of addictive substances" and a majority of mental health patients participate in the use of these substances: 38% alcohol, 44% cocaine, and 40% cigarettes.[80]
Epigenetic
[edit]Epigenetics is the study of stable phenotypic changes that do not involve alterations in the DNA sequence.[81] Illicit drug use has been found to cause epigenetic changes in DNA methylation, as well as chromatin remodeling.[82] The epigenetic state of chromatin may pose as a risk for the development of substance addictions.[82] It has been found that emotional stressors, as well as social adversities may lead to an initial epigenetic response, which causes an alteration to the reward-signalling pathways.[82] This change may predispose one to experience a positive response to drug use.[82]
Transgenerational epigenetic inheritance
[edit]Epigenetic genes and their products (e.g., proteins) are the key components through which environmental influences can affect the genes of an individual:[53] they serve as the mechanism responsible for transgenerational epigenetic inheritance, a phenomenon in which environmental influences on the genes of a parent can affect the associated traits and behavioral phenotypes of their offspring (e.g., behavioral responses to environmental stimuli).[53] In addiction, epigenetic mechanisms play a central role in the pathophysiology of the disease;[3] it has been noted that some of the alterations to the epigenome which arise through chronic exposure to addictive stimuli during an addiction can be transmitted across generations, in turn affecting the behavior of one's children (e.g., the child's behavioral responses to addictive drugs and natural rewards).[53][83]
The general classes of epigenetic alterations that have been implicated in transgenerational epigenetic inheritance include DNA methylation, histone modifications, and downregulation or upregulation of microRNAs.[53] With respect to addiction, more research is needed to determine the specific heritable epigenetic alterations that arise from various forms of addiction in humans and the corresponding behavioral phenotypes from these epigenetic alterations that occur in human offspring.[53][83] Based on preclinical evidence from animal research, certain addiction-induced epigenetic alterations in rats can be transmitted from parent to offspring and produce behavioral phenotypes that decrease the offspring's risk of developing an addiction.[note 1][53] More generally, the heritable behavioral phenotypes that are derived from addiction-induced epigenetic alterations and transmitted from parent to offspring may serve to either increase or decrease the offspring's risk of developing an addiction.[53][83]
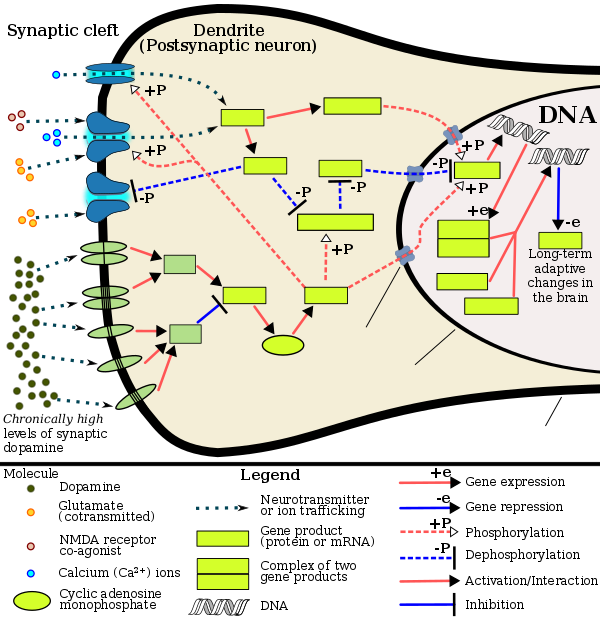
Mechanisms
[edit]Addiction is a disorder of the brain's reward system developing through transcriptional and epigenetic mechanisms as a result of chronically high levels of exposure to an addictive stimulus (e.g., eating food, the use of cocaine, engagement in sexual activity, participation in high-thrill cultural activities such as gambling, etc.) over extended time.[3][84][24] DeltaFosB (ΔFosB), a gene transcription factor, is a critical component and common factor in the development of virtually all forms of behavioral and drug addictions.[84][24][85][25] Two decades of research into ΔFosB's role in addiction have demonstrated that addiction arises, and the associated compulsive behavior intensifies or attenuates, along with the overexpression of ΔFosB in the D1-type medium spiny neurons of the nucleus accumbens.[3][84][24][85] Due to the causal relationship between ΔFosB expression and addictions, it is used preclinically as an addiction biomarker.[3][84][85] ΔFosB expression in these neurons directly and positively regulates drug self-administration and reward sensitization through positive reinforcement, while decreasing sensitivity to aversion.[note 2][3][84]
| Transcription factor glossary | |
|---|---|
| |
Chronic addictive drug use causes alterations in gene expression in the mesocorticolimbic projection.[25][93][94] The most important transcription factors that produce these alterations are ΔFosB, cAMP response element binding protein (CREB), and nuclear factor kappa B (NF-κB).[25] ΔFosB is the most significant biomolecular mechanism in addiction because the overexpression of ΔFosB in the D1-type medium spiny neurons in the nucleus accumbens is necessary and sufficient for many of the neural adaptations and behavioral effects (e.g., expression-dependent increases in drug self-administration and reward sensitization) seen in drug addiction.[25] ΔFosB expression in nucleus accumbens D1-type medium spiny neurons directly and positively regulates drug self-administration and reward sensitization through positive reinforcement while decreasing sensitivity to aversion.[note 2][3][84] ΔFosB has been implicated in mediating addictions to many different drugs and drug classes, including alcohol, amphetamine and other substituted amphetamines, cannabinoids, cocaine, methylphenidate, nicotine, opiates, phenylcyclidine, and propofol, among others.[84][25][93][95][96] ΔJunD, a transcription factor, and G9a, a histone methyltransferase, both oppose the function of ΔFosB and inhibit increases in its expression.[3][25][97] Increases in nucleus accumbens ΔJunD expression (via viral vector-mediated gene transfer) or G9a expression (via pharmacological means) reduces, or with a large increase can even block, many of the neural and behavioral alterations that result from chronic high-dose use of addictive drugs (i.e., the alterations mediated by ΔFosB).[85][25]
ΔFosB plays an important role in regulating behavioral responses to natural rewards, such as palatable food, sex, and exercise.[25][98] Natural rewards, like drugs of abuse, induce gene expression of ΔFosB in the nucleus accumbens, and chronic acquisition of these rewards can result in a similar pathological addictive state through ΔFosB overexpression.[24][25][98] Consequently, ΔFosB is the key transcription factor involved in addictions to natural rewards (i.e., behavioral addictions) as well;[25][24][98] in particular, ΔFosB in the nucleus accumbens is critical for the reinforcing effects of sexual reward.[98] Research on the interaction between natural and drug rewards suggests that dopaminergic psychostimulants (e.g., amphetamine) and sexual behavior act on similar biomolecular mechanisms to induce ΔFosB in the nucleus accumbens and possess bidirectional cross-sensitization effects that are mediated through ΔFosB.[24][33][34] This phenomenon is notable since, in humans, a dopamine dysregulation syndrome, characterized by drug-induced compulsive engagement in natural rewards (specifically, sexual activity, shopping, and gambling), has been observed in some individuals taking dopaminergic medications.[24]
ΔFosB inhibitors (drugs or treatments that oppose its action) may be an effective treatment for addiction and addictive disorders.[99]
The release of dopamine in the nucleus accumbens plays a role in the reinforcing qualities of many forms of stimuli, including naturally reinforcing stimuli like palatable food and sex.[100][101][12] Altered dopamine neurotransmission is frequently observed following the development of an addictive state.[24][18] In humans and lab animals that have developed an addiction, alterations in dopamine or opioid neurotransmission in the nucleus accumbens and other parts of the striatum are evident.[24] Use of certain drugs (e.g., cocaine) affect cholinergic neurons that innervate the reward system, in turn affecting dopamine signaling in this region.[102]
A recent study in Addiction reports that GLP-1 agonist medications, such as semaglutide, which are commonly used for diabetes and weight management, may also reduce the risk of overdose and alcohol intoxication in people with substance use disorders.[103] The study analyzed nearly nine years of health records from 1.3 million individuals across 136 U.S. hospitals, including 500,000 with opioid use disorder and over 800,000 with alcohol use disorder.[104] Researchers found that those who used Ozempic or similar medications had a 40% lower risk of opioid overdose and a 50% lower risk of alcohol intoxication compared to those not using these drugs.
Reward system
[edit]Mesocorticolimbic pathway
[edit]ΔFosB accumulation from excessive drug use
Top: this depicts the initial effects of high dose exposure to an addictive drug on gene expression in the nucleus accumbens for various Fos family proteins (i.e., c-Fos, FosB, ΔFosB, Fra1, and Fra2).
Bottom: this illustrates the progressive increase in ΔFosB expression in the nucleus accumbens following repeated twice daily drug binges, where these phosphorylated (35–37 kilodalton) ΔFosB isoforms persist in the D1-type medium spiny neurons of the nucleus accumbens for up to 2 months.[91][105] |
Understanding the pathways in which drugs act and how drugs can alter those pathways is key when examining the biological basis of drug addiction. The reward pathway, known as the mesolimbic pathway,[18] or its extension, the mesocorticolimbic pathway, is characterized by the interaction of several areas of the brain.
- The projections from the ventral tegmental area (VTA) are a network of dopaminergic neurons with co-localized postsynaptic glutamate receptors (AMPAR and NMDAR). These cells respond when stimuli indicative of a reward are present.[12] The VTA supports learning and sensitization development and releases dopamine (DA) into the forebrain.[106] These neurons project and release DA into the nucleus accumbens,[107] through the mesolimbic pathway. Virtually all drugs causing drug addiction increase the DA release in the mesolimbic pathway.[108][18]
- The nucleus accumbens (NAcc) is one output of the VTA projections. The nucleus accumbens itself consists mainly of GABAergic medium spiny neurons (MSNs).[109] The NAcc is associated with acquiring and eliciting conditioned behaviors, and is involved in the increased sensitivity to drugs as addiction progresses.[106][23] Overexpression of ΔFosB in the nucleus accumbens is a necessary common factor in essentially all known forms of addiction;[3] ΔFosB is a strong positive modulator of positively reinforced behaviors.[3]
- The prefrontal cortex, including the anterior cingulate and orbitofrontal cortices,[110][23] is another VTA output in the mesocorticolimbic pathway; it is important for the integration of information which helps determine whether a behavior will be elicited.[111] It is critical for forming associations between the rewarding experience of drug use and cues in the environment. Importantly, these cues are strong mediators of drug-seeking behavior and can trigger relapse even after months or years of abstinence.[112][18]
Other brain structures that are involved in addiction include:
- The basolateral amygdala projects into the NAcc and is thought to be important for motivation.[111]
- The hippocampus is involved in drug addiction, because of its role in learning and memory. Much of this evidence stems from investigations showing that manipulating cells in the hippocampus alters DA levels in NAcc and firing rates of VTA dopaminergic cells.[107]
Role of dopamine and glutamate
[edit]Dopamine is the primary neurotransmitter of the reward system in the brain. It plays a role in regulating movement, emotion, cognition, motivation, and feelings of pleasure.[113] Natural rewards, like eating, as well as recreational drug use cause a release of dopamine, and are associated with the reinforcing nature of these stimuli.[113][114][12] Nearly all addictive drugs, directly or indirectly, act on the brain's reward system by heightening dopaminergic activity.[115][18]
Excessive intake of many types of addictive drugs results in repeated release of high amounts of dopamine, which in turn affects the reward pathway directly through heightened dopamine receptor activation. Prolonged and abnormally high levels of dopamine in the synaptic cleft can induce receptor downregulation in the neural pathway. Downregulation of mesolimbic dopamine receptors can result in a decrease in the sensitivity to natural reinforcers.[113]
Drug seeking behavior is induced by glutamatergic projections from the prefrontal cortex to the nucleus accumbens. This idea is supported with data from experiments showing that drug seeking behavior can be prevented following the inhibition of AMPA glutamate receptors and glutamate release in the nucleus accumbens.[110]
Reward sensitization
[edit]| Target gene |
Target expression |
Neural effects | Behavioral effects |
|---|---|---|---|
| c-Fos | ↓ | Molecular switch enabling the chronic induction of ΔFosB[note 3] |
– |
| dynorphin | ↓ [note 4] |
• Downregulation of κ-opioid feedback loop | • Increased drug reward |
| NF-κB | ↑ | • Expansion of NAcc dendritic processes • NF-κB inflammatory response in the NAcc • NF-κB inflammatory response in the CP |
• Increased drug reward • Locomotor sensitization |
| GluR2 | ↑ | • Decreased sensitivity to glutamate | • Increased drug reward |
| Cdk5 | ↑ | • GluR1 synaptic protein phosphorylation • Expansion of NAcc dendritic processes |
Decreased drug reward (net effect) |
Reward sensitization is a process that causes an increase in the amount of reward (specifically, incentive salience[note 5]) that is assigned by the brain to a rewarding stimulus (e.g., a drug). In simple terms, when reward sensitization to a specific stimulus (e.g., a drug) occurs, an individual's "wanting" or desire for the stimulus itself and its associated cues increases.[118][117][119] Reward sensitization normally occurs following chronically high levels of exposure to the stimulus.[18] ΔFosB expression in D1-type medium spiny neurons in the nucleus accumbens has been shown to directly and positively regulate reward sensitization involving drugs and natural rewards.[3][84][85]
"Cue-induced wanting" or "cue-triggered wanting", a form of craving that occurs in addiction, is responsible for most of the compulsive behavior that people with addictions exhibit.[117][119] During the development of an addiction, the repeated association of otherwise neutral and even non-rewarding stimuli with drug consumption triggers an associative learning process that causes these previously neutral stimuli to act as conditioned positive reinforcers of addictive drug use (i.e., these stimuli start to function as drug cues).[117][120][119] As conditioned positive reinforcers of drug use, these previously neutral stimuli are assigned incentive salience (which manifests as a craving) – sometimes at pathologically high levels due to reward sensitization – which can transfer to the primary reinforcer (e.g., the use of an addictive drug) with which it was originally paired.[117][120][119]
Research on the interaction between natural and drug rewards suggests that dopaminergic psychostimulants (e.g., amphetamine) and sexual behavior act on similar biomolecular mechanisms to induce ΔFosB in the nucleus accumbens and possess a bidirectional reward cross-sensitization effect[note 6] that is mediated through ΔFosB.[24][33][34] In contrast to ΔFosB's reward-sensitizing effect, CREB transcriptional activity decreases user's sensitivity to the rewarding effects of the substance. CREB transcription in the nucleus accumbens is implicated in psychological dependence and symptoms involving a lack of pleasure or motivation during drug withdrawal.[3][105][116]
| Form of neuroplasticity or behavioral plasticity |
Type of reinforcer | Ref. | |||||
|---|---|---|---|---|---|---|---|
| Opiates | Psychostimulants | High fat or sugar food | Sexual intercourse | Physical exercise (aerobic) |
Environmental enrichment | ||
| ΔFosB expression in nucleus accumbens D1-type MSNs |
↑ | ↑ | ↑ | ↑ | ↑ | ↑ | [24] |
| Behavioral plasticity | |||||||
| Escalation of intake | Yes | Yes | Yes | [24] | |||
| Psychostimulant cross-sensitization |
Yes | Not applicable | Yes | Yes | Attenuated | Attenuated | [24] |
| Psychostimulant self-administration |
↑ | ↑ | ↓ | ↓ | ↓ | [24] | |
| Psychostimulant conditioned place preference |
↑ | ↑ | ↓ | ↑ | ↓ | ↑ | [24] |
| Reinstatement of drug-seeking behavior | ↑ | ↑ | ↓ | ↓ | [24] | ||
| Neurochemical plasticity | |||||||
| CREB phosphorylation in the nucleus accumbens |
↓ | ↓ | ↓ | ↓ | ↓ | [24] | |
| Sensitized dopamine response in the nucleus accumbens |
No | Yes | No | Yes | [24] | ||
| Altered striatal dopamine signaling | ↓DRD2, ↑DRD3 | ↑DRD1, ↓DRD2, ↑DRD3 | ↑DRD1, ↓DRD2, ↑DRD3 | ↑DRD2 | ↑DRD2 | [24] | |
| Altered striatal opioid signaling | No change or ↑μ-opioid receptors |
↑μ-opioid receptors ↑κ-opioid receptors |
↑μ-opioid receptors | ↑μ-opioid receptors | No change | No change | [24] |
| Changes in striatal opioid peptides | ↑dynorphin No change: enkephalin |
↑dynorphin | ↓enkephalin | ↑dynorphin | ↑dynorphin | [24] | |
| Mesocorticolimbic synaptic plasticity | |||||||
| Number of dendrites in the nucleus accumbens | ↓ | ↑ | ↑ | [24] | |||
| Dendritic spine density in the nucleus accumbens |
↓ | ↑ | ↑ | [24] | |||
Neuroepigenetic mechanisms
[edit]Altered epigenetic regulation of gene expression within the brain's reward system plays a significant and complex role in the development of drug addiction.[97][121] Addictive drugs are associated with three types of epigenetic modifications within neurons.[97] These are (1) histone modifications, (2) epigenetic methylation of DNA at CpG sites at (or adjacent to) particular genes, and (3) epigenetic downregulation or upregulation of microRNAs which have particular target genes.[97][25][121] As an example, while hundreds of genes in the cells of the nucleus accumbens (NAc) exhibit histone modifications following drug exposure – particularly, altered acetylation and methylation states of histone residues[121] – most other genes in the NAc cells do not show such changes.[97]
Diagnosis
[edit]Classification
[edit]DSM-5
[edit]The fifth edition of the DSM uses the term substance use disorder to refer to a spectrum of drug use-related disorders. The DSM-5 eliminates the terms abuse and dependence from diagnostic categories, instead using the specifiers of mild, moderate and severe to indicate the extent of disordered use. These specifiers are determined by the number of diagnostic criteria present in a given case. In the DSM-5, the term drug addiction is synonymous with severe substance use disorder.[122][15]
The DSM-5 introduced a new diagnostic category for behavioral addictions. Problem gambling is the only condition included in this category in the fifth edition.[123] Internet gaming disorder is listed as a "condition requiring further study" in the DSM-5.[124]
Past editions have used physical dependence and the associated withdrawal syndrome to identify an addictive state. Physical dependence occurs when the body has adjusted by incorporating the substance into its "normal" functioning – i.e., attains homeostasis – and therefore physical withdrawal symptoms occur on cessation of use.[125] Tolerance is the process by which the body continually adapts to the substance and requires increasingly larger amounts to achieve the original effects. Withdrawal refers to physical and psychological symptoms experienced when reducing or discontinuing a substance that the body has become dependent on. Symptoms of withdrawal generally include but are not limited to body aches, anxiety, irritability, intense cravings for the substance, dysphoria, nausea, hallucinations, headaches, cold sweats, tremors, and seizures. During acute physical opioid withdrawal, symptoms of restless legs syndrome are common and may be profound. This phenomenon originated the idiom "kicking the habit".
Medical researchers who actively study addiction have criticized the DSM classification of addiction for being flawed and involving arbitrary diagnostic criteria.[126]
ICD-11
[edit]The eleventh revision of the International Classification of Diseases, commonly referred to as ICD-11, conceptualizes diagnosis somewhat differently. ICD-11 first distinguishes between problems with psychoactive substance use ("Disorders due to substance use") and behavioral addictions ("Disorders due to addictive behaviours").[127] With regard to psychoactive substances, ICD-11 explains that the included substances initially produce "pleasant or appealing psychoactive effects that are rewarding and reinforcing with repeated use, [but] with continued use, many of the included substances have the capacity to produce dependence. They have the potential to cause numerous forms of harm, both to mental and physical health."[128] Instead of the DSM-5 approach of one diagnosis ("Substance Use Disorder") covering all types of problematic substance use, ICD-11 offers three diagnostic possibilities: 1) Episode of Harmful Psychoactive Substance Use, 2) Harmful Pattern of Psychoactive Substance Use, and 3) Substance Dependence.[128]
Screening and assessment
[edit]Addictions Neuroclinical Assessment
[edit]The Addictions Neuroclinical Assessment is used to diagnose addiction disorders. This tool measures three different domains: executive function, incentive salience, and negative emotionality.[129][130] Executive functioning consists of processes that would be disrupted in addiction.[130] In the context of addiction, incentive salience determines how one perceives the addictive substance.[130] Increased negative emotional responses have been found with individuals with addictions.[130]
Tobacco, Alcohol, Prescription Medication, and Other Substance Use (TAPS)
[edit]This is a screening and assessment tool in one, assessing commonly used substances. This tool allows for a simple diagnosis, eliminating the need for several screening and assessment tools, as it includes both TAPS-1 and TAPS-2, screening and assessment tools respectively. The screening component asks about the frequency of use of the specific substance (tobacco, alcohol, prescription medication, and other).[131] If an individual screens positive, the second component will begin. This dictates the risk level of the substance.[131]
CRAFFT
[edit]The CRAFFT (Car-Relax-Alone-Forget-Family and Friends-Trouble) is a screening tool that is used in medical centers. The CRAFFT is in version 2.1 and has a version for nicotine and tobacco use called the CRAFFT 2.1+N.[132] This tool is used to identify substance use, substance related driving risk, and addictions among adolescents. This tool uses a set of questions for different scenarios.[133] In the case of a specific combination of answers, different question sets can be used to yield a more accurate answer. After the questions, the DSM-5 criteria are used to identify the likelihood of the person having substance use disorder.[133] After these tests are done, the clinician is to give the "5 RS" of brief counseling.
The five Rs of brief counseling includes:[133]
- REVIEW screening results
- RECOMMEND to not use
- RIDING/DRIVING risk counseling
- RESPONSE: elicit self-motivational statements
- REINFORCE self-efficacy
Drug Abuse Screening Test (DAST-10)
[edit]The Drug Abuse Screening Test (DAST) is a self-reporting tool that measures problematic substance use.[134] Responses to this test are recorded as yes or no answers, and scored as a number between zero and 28. Drug abuse or dependence, are indicated by a cut off score of 6.[134] Three versions of this screening tool are in use: DAST-28, DAST-20, and DAST-10. Each of these instruments are copyrighted by Dr. Harvey A. Skinner.[134]
Alcohol, Smoking, and Substance Involvement Test (ASSIST)
[edit]The Alcohol, Smoking, and Substance Involvement Test (ASSIST) is an interview-based questionnaire consisting of eight questions developed by the WHO.[135] The questions ask about lifetime use; frequency of use; urge to use; frequency of health, financial, social, or legal problems related to use; failure to perform duties; if anyone has raised concerns over use; attempts to limit or moderate use; and use by injection.[136]
Prevention
[edit]Abuse liability
[edit]Abuse or addiction liability is the tendency to use drugs in a non-medical situation. This is typically for euphoria, mood changing, or sedation.[137] Abuse liability is used when the person using the drugs wants something that they otherwise can not obtain. The only way to obtain this is through the use of drugs. When looking at abuse liability there are a number of determining factors in whether the drug is abused. These factors are: the chemical makeup of the drug, the effects on the brain, and the age, vulnerability, and the health (mental and physical) of the population being studied.[137] There are a few drugs with a specific chemical makeup that leads to a high abuse liability. These are: cocaine, heroin, inhalants, marijuana, MDMA (ecstasy), methamphetamine, PCP, synthetic cannabinoids, synthetic cathinones (bath salts), nicotine (e.g. tobacco), and alcohol.[138]
Potential vaccines for addiction to substances
[edit]Vaccines for addiction have been investigated as a possibility since the early 2000s.[139] The general theory of a vaccine intended to "immunize" against drug addiction or other substance abuse is that it would condition the immune system to attack and consume or otherwise disable the molecules of such substances that cause a reaction in the brain, thus preventing the addict from being able to realize the effect of the drug. Addictions that have been floated as targets for such treatment include nicotine, opioids, and fentanyl.[140][141][142][143] Vaccines have been identified as potentially being more effective than other anti-addiction treatments, due to "the long duration of action, the certainty of administration and a potential reduction of toxicity to important organs".[144]
Specific addiction vaccines in development include:
- NicVAX, a conjugate vaccine intended to reduce or eliminate physical dependence on nicotine.[145] This proprietary vaccine is being developed by Nabi Biopharmaceuticals[146] of Rockville, MD. with the support from the U.S. National Institute on Drug Abuse. NicVAX consists of the hapten 3'-aminomethylnicotine which has been conjugated (attached) to Pseudomonas aeruginosa exotoxin A.[147]
- TA-CD, an active vaccine[148] developed by the Xenova Group which is used to negate the effects of cocaine. It is created by combining norcocaine with inactivated cholera toxin. It works in much the same way as a regular vaccine. A large protein molecule attaches to cocaine, which stimulates response from antibodies, which destroy the molecule. This also prevents the cocaine from crossing the blood–brain barrier, negating the euphoric high and rewarding effect of cocaine caused from stimulation of dopamine release in the mesolimbic reward pathway. The vaccine does not affect the user's "desire" for cocaine—only the physical effects of the drug.[149]
- TA-NIC, used to create human antibodies to destroy nicotine in the human body so that it is no longer effective.[150]
As of September 2023, it was further reported that a vaccine "has been tested against heroin and fentanyl and is on its way to being tested against OxyContin".[151]
Treatment
[edit]To be effective, treatment for addiction that is pharmacological or biologically based need to be accompanied by other interventions such as cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT); individual and group psychotherapy, behavior modification strategies, twelve-step programs, and residential treatment facilities.[152][20] The transtheoretical model (TTM) can be used to determine when treatment can begin and which method will be most effective. If treatment begins too early, it can cause a person to become defensive and resistant to change.[42][153]
Epidemiology
[edit]Due to cultural variations, the proportion of individuals who develop a drug or behavioral addiction within a specified time period (i.e., the prevalence) varies over time, by country, and across national population demographics (e.g., by age group, socioeconomic status, etc.).[53] Where addiction is viewed as unacceptable, there will be fewer people addicted.
Asia
[edit]The prevalence of alcohol dependence is not as high as is seen in other regions. In Asia, not only socioeconomic factors but biological factors influence drinking behavior.[154]
Internet addiction disorder is highest in the Philippines, according to both the IAT (Internet Addiction Test) – 5% and the CIAS-R (Revised Chen Internet Addiction Scale) – 21%.[155]
Australia
[edit]The prevalence of substance use disorder among Australians was reported at 5.1% in 2009.[156] In 2019 the Australian Institute of Health and Welfare conducted a national drug survey that quantified drug use for various types of drugs and demographics.[157] The survey found that in 2019, 11% of people over 14 years old smoke daily; that 9.9% of those who drink alcohol, which equates to 7.5% of the total population age 14 or older, may qualify as alcohol dependent; that 17.5% of the 2.4 million people who used cannabis in the last year may have hazardous use or a dependence problem; and that 63.5% of about 300000 recent users of meth and amphetamines were at risk for developing problem use.[157]
Europe
[edit]In 2015, the estimated prevalence among the adult population was 18.4% for heavy episodic alcohol use (in the past 30 days); 15.2% for daily tobacco smoking; and 3.8% for cannabis use, 0.77% for amphetamine use, 0.37% for opioid use, and 0.35% for cocaine use in 2017. The mortality rates for alcohol and illicit drugs were highest in Eastern Europe.[158] Data shows a downward trend of alcohol use among children 15 years old in most European countries between 2002 and 2014. First-time alcohol use before the age of 13 was recorded for 28% of European children in 2014.[20]
United States
[edit]Based on representative samples of the US youth population in 2011[update], the lifetime prevalence[note 7] of addictions to alcohol and illicit drugs has been estimated to be approximately 8% and 2–3% respectively.[159] Based on representative samples of the US adult population in 2011[update], the 12-month prevalence of alcohol and illicit drug addictions were estimated at 12% and 2–3% respectively.[159] The lifetime prevalence of prescription drug addictions is around 4.7%.[160]
As of 2021,[update] 43.7 million people aged 12 or older surveyed by the National Survey on Drug Use and Health in the United States needed treatment for an addiction to alcohol, nicotine, or other drugs. The groups with the highest number of people were 18–25 years (25.1%) and "American Indian or Alaska Native" (28.7%).[161] Only about 10%, or a little over 2 million, receive any form of treatments, and those that do generally do not receive evidence-based care.[162][163] One-third of inpatient hospital costs and 20% of all deaths in the US every year are the result of untreated addictions and risky substance use.[162][163] In spite of the massive overall economic cost to society, which is greater than the cost of diabetes and all forms of cancer combined, most doctors in the US lack the training to effectively address a drug addiction.[162][163]
Estimates of lifetime prevalence rates in the US are 1–2% for compulsive gambling, 5% for sexual addiction, 2.8% for food addiction, and 5–6% for compulsive shopping.[24] The time-invariant prevalence rate for sexual addiction and related compulsive sexual behavior (e.g., compulsive masturbation with or without pornography, compulsive cybersex, etc.) within the US ranges from 3–6% of the population.[32]
According to a 2017 poll conducted by the Pew Research Center, almost half of US adults know a family member or close friend who has struggled with a drug addiction at some point in their life.[164]
In 2019, opioid addiction was acknowledged as a national crisis in the United States.[165] An article in The Washington Post stated that "America's largest drug companies flooded the country with pain pills from 2006 through 2012, even when it became apparent that they were fueling addiction and overdoses."
The National Epidemiologic Survey on Alcohol and Related Conditions found that from 2012 to 2013 the prevalence of Cannabis use disorder in U.S. adults was 2.9%.[166]
Canada
[edit]A Statistics Canada Survey in 2012 found the lifetime prevalence and 12-month prevalence of substance use disorders were 21.6%, and 4.4% in those 15 and older.[167] Alcohol abuse or dependence reported a lifetime prevalence of 18.1% and a 12-month prevalence of 3.2%.[167] Cannabis abuse or dependence reported a lifetime prevalence of 6.8% and a 12-month prevalence of 3.2%.[167] Other drug abuse or dependence has a lifetime prevalence of 4.0% and a 12-month prevalence of 0.7%.[167] Substance use disorder is a term used interchangeably with a drug addiction.[168]
In Ontario, Canada between 2009 and 2017, outpatient visits for mental health and addiction increased from 52.6 to 57.2 per 100 people, emergency department visits increased from 13.5 to 19.7 per 1000 people and the number of hospitalizations increased from 4.5 to 5.5 per 1000 people.[169] Prevalence of care needed increased the most among the 14–17 age group overall.[169]
South America
[edit]The realities of opioid use and opioid use disorder in Latin America may be deceptive if observations are limited to epidemiological findings. In the United Nations Office on Drugs and Crime report,[170] although South America produced 3% of the world's morphine and heroin and 0.01% of its opium, prevalence of use is uneven. According to the Inter-American Commission on Drug Abuse Control, consumption of heroin is low in most Latin American countries, although Colombia is the area's largest opium producer. Mexico, because of its border with the United States, has the highest incidence of use.[171]
Etymology
[edit]The word addiction derives from the Latin "addico", meaning "giving over" with both positive connotations (devotion, dedication) and negative ones (being enslaved to a creditor in Roman law). This dual meaning persisted in traditional English dictionaries, encompassing both legal surrender and personal devotion to habits. Later, 19th century temperance movements narrowed the definition of addiction to just drug-related disease, ignoring behavioral addictions and the possibility of positive or neutral addictions. This restrictive view opposes the current understanding of addiction.[172]
Addiction and addictive behavior are polysemes denoting a category of mental disorders, of neuropsychological symptoms, or of merely maladaptive/harmful habits and lifestyles.[173] A common use of the term addiction in medicine is for neuropsychological symptoms denoting pervasive/excessive and intense urges to engage in a category of behavioral compulsions or impulses towards sensory rewards (e.g., alcohol, betel quid, drugs, sex, gambling, video gaming).[174][175][176][177][127] Addictive disorders or addiction disorders are mental disorders involving high intensities of addictions (as neuropsychological symptoms) that induce functional disabilities (i.e., limit subjects' social/family and occupational activities); the two categories of such disorders are substance-use addictions and behavioral addictions.[178][173][177][127]
The etymology of the term addiction throughout history has been misunderstood and has taken on various meanings associated with the word.[179] An example is the usage of the word in the religious landscape of early modern Europe.[180] "Addiction" at the time meant "to attach" to something, giving it both positive and negative connotations. The object of this attachment could be characterized as "good or bad".[181] The meaning of addiction during the early modern period was mostly associated with positivity and goodness;[180] during this early modern and highly religious era of Christian revivalism and Pietistic tendencies,[180] it was seen as a way of "devoting oneself to another".[181]
The suffixes "-holic" and "-holism"
[edit]In contemporary modern English "-holic" is a suffix that can be added to a subject to denote an addiction to it. It was extracted from the word alcoholism (one of the first addictions to be widely identified both medically and socially) (correctly the root "alcohol" plus the suffix "-ism") by misdividing or rebracketing it into "alco" and "-holism". There are correct medico-legal terms for such addictions: dipsomania is the medico-legal term for alcoholism;[182] other examples are in this table:[citation needed]
| Colloquial term | Addiction to | Medico-legal term |
|---|---|---|
| chocoholic | chocolate | |
| danceaholic | dance | choreomania |
| rageaholic | rage | |
| sexaholic | sex | hypersexuality, satyriasis, nymphomania |
| sugarholic | sugar | saccharomania |
| workaholic | work | ergomania |
History
[edit]Modern research on addiction has led to a better understanding of the disease with research on the topic dating back to 1875, specifically on morphine addiction.[183] This furthered the understanding of addiction being a medical condition. It was not until the 19th century that addiction was seen and acknowledged in the Western world as a disease, being both a physical condition and mental illness.[184] Today, addiction is understood both as a biopsychosocial and neurological disorder that negatively impacts those who are affected by it, most commonly associated with the use of drugs and excessive use of alcohol.[4] The understanding of addiction has changed throughout history, which has impacted and continues to impact the ways it is medically treated and diagnosed.[citation needed]
Addiction and art
[edit]The arts can be used in a variety of ways to address issues related to addiction. Art can be used as a form of therapy in the treatment of substance use disorders. Creative activities like painting, sculpting, music, and writing can help people express their feelings and experiences in safe and healthy ways. The arts can be used as an assessment tool to identify underlying issues that may be contributing to a person's substance use disorder. Through art, individuals can gain insights into their own motivations and behaviors that can be helpful in determining a course of treatment. Finally, the arts can be used to advocate for those suffering from a substance use disorder by raising awareness of the issue and promoting understanding and compassion. Through art, individuals can share their stories, increase awareness, and offer support and hope to those struggling with substance use disorders.
As therapy
[edit]Addiction treatment is complex and not always effective due to engagement and service availability concerns, so researchers prioritize efforts to improve treatment retention and decrease relapse rates.[185][186] Characteristics of substance abuse may include feelings of isolation, a lack of confidence, communication difficulties, and a perceived lack of control.[187] In a similar vein, people suffering from substance use disorders tend to be highly sensitive, creative, and as such, are likely able to express themselves meaningfully in creative arts such as dancing, painting, writing, music, and acting.[188] Further evidenced by Waller and Mahony (2002)[189] and Kaufman (1981),[190] the creative arts therapies can be a suitable treatment option for this population especially when verbal communication is ineffective.
Primary advantages of art therapy in the treatment of addiction have been identified as:[191][192]
- Assess and characterize a client's substance use issues
- Bypassing a client's resistances, defenses, and denial
- Containing shame or anger
- Facilitating the expression of suppressed and/or complicated emotions
- Highlighting a client's strengths
- Providing an alternative to verbal communication (via use of symbols) and conventional forms of therapy
- Providing clients with a sense of control
- Tackling feelings of isolation
Art therapy is an effective method of dealing with substance abuse in comprehensive treatment models. When included in psychoeducational programs, art therapy in a group setting can help clients internalize taught concepts in a more personalized manner.[193] During the course of treatment, by examining and comparing artwork created at different times, art therapists can be helpful in identifying and diagnosing issues, as well as charting the extent or direction of improvement as a person detoxifies.[193] Where increasing adherence to treatment regimes and maintaining abstinence is the target; art therapists can aid by customizing treatment directives (encourage the client to create collages that compare pros and cons, pictures that compare past and present and future, and drawings that depict what happened when a client went off medication).[193]
Art therapy can function as a complementary therapy used in conjunction with more conventional therapies and can integrate with harm reduction protocols to minimize the negative effects of drug use.[194][192] An evaluation of art therapy incorporation within a pre-existing Addiction Treatment Programme based on the 12 step Minnesota Model endorsed by the Alcoholics Anonymous found that 66% of participants expressed the usefulness of art therapy as a part of treatment.[195][192] Within the weekly art therapy session, clients were able to reflect and process the intense emotions and cognitions evoked by the programme. In turn, the art therapy component of the programme fostered stronger self-awareness, exploration, and externalization of repressed and unconscious emotions of clients, promoting the development of a more integrated 'authentic self'.[196][192]
Despite the large number of randomized control trials, clinical control trials, and anecdotal evidence supporting the effectiveness of art therapies for use in addiction treatment, a systematic review conducted in 2018 could not find enough evidence on visual art, drama, dance and movement therapy, or 'arts in health' methodologies to confirm their effectiveness as interventions for reducing substance misuse.[197] Music therapy was identified to have potentially strong beneficial effects in aiding contemplation and preparing those diagnosed with substance use for treatment.[197]
As an assessment tool
[edit]The Formal Elements Art Therapy Scale (FEATS) is an assessment tool used to evaluate drawings created by people suffering from substance use disorders by comparing them to drawings of a control group (consisting of individuals without SUDs).[198][192] FEATS consists of twelve elements, three of which were found to be particularly effective at distinguishing the drawings of those with SUDs from those without: Person, Realism, and Developmental. The Person element assesses the degree to which a human features are depicted realistically, the Realism element assesses the overall complexity of the artwork, and the Developmental element assesses "developmental age" of the artwork in relation to standardized drawings from children and adolescents.[198] By using the FEATS assessment tool, clinicians can gain valuable insight into the drawings of individuals with SUDs, and can compare them to those of the control group. Formal assessments such as FEATS provide healthcare providers with a means to quantify, standardize, and communicate abstract and visceral characteristics of SUDs to provide more accurate diagnoses and informed treatment decisions.[198]
Other artistic assessment methods include the Bird's Nest Drawing: a useful tool for visualizing a client's attachment security.[199][192] This assessment method looks at the amount of color used in the drawing, with a lack of color indicating an 'insecure attachment', a factor that the client's therapist or recovery framework must take into account.[200]
Art therapists working with children of parents suffering from alcoholism can use the Kinetic Family Drawings assessment tool to shed light on family dynamics and help children express and understand their family experiences.[201][192] The KFD can be used in family sessions to allow children to share their experiences and needs with parents who may be in recovery from alcohol use disorder. Depiction of isolation of self and isolation of other family members may be an indicator of parental alcoholism.[201]
Advocacy
[edit]Stigma can lead to feelings of shame that can prevent people with substance use disorders from seeking help and interfere with provision of harm reduction services.[202][203][204] It can influence healthcare policy, making it difficult for these individuals to access treatment.[205] For designing and implementing effective and evidence-based stigma prevention and intervention, it is important do both, identify persons who are more likely to be stigmatized (e.g., male or those addicted to drugs believed to be "stronger") and target those more likely to stigmatize (e.g., those with lacking or limited familiarity with addiction or more conservative individuals).[206][207][208][209]
Artists attempt to change the societal perception of addiction from a punishable moral offense to instead a chronic illness necessitating treatment. This form of advocacy can help to relocate the fight of addiction from a judicial perspective to the public health system.[210]
Artists who have personally lived with addiction or undergone recovery may use art to depict their experiences in a manner that uncovers the "human face of addiction". By bringing experiences of addiction and recovery to a personal level and breaking down the "us and them", the viewer may be more inclined to show compassion, forego stereotypes and stigma of addiction, and label addiction as a social rather than individual problem.[210]
According to Santora[210] the main purposes in using art as a form of advocacy in the education and prevention of substance use disorders include:
- Addiction art exhibitions can come from a variety of sources, but the underlying message of these works is the same: to communicate through emotions without relying on intellectually demanding/gatekept facts and figures. These exhibitions can either stand alone, reinforce, or challenge facts.
- A powerful educational tool for increasing awareness and understanding of addiction as a medical illness. Exhibitions featuring personal stories and images can help to create lasting impressions on diverse audiences (including addiction scientists/researchers, family/friends of those affected by addiction etc.), highlighting the humanity of the problem and in turn encouraging compassion and understanding.
- A way to destigmatize substance use disorders and shift public perception from viewing them as a moral failing to understanding them as a chronic medical condition which requires treatment.
- Provide those who are struggling with addiction assurance and encouragement of healing, and let them know that they are not alone in their struggle.
- The use of visual arts can help bring attention to the lack of adequate substance use treatment, prevention, and education programs and services in a healthcare system. Messages can encourage policymakers to allocate more resources to addiction treatment and prevention from federal, state, and local levels.
The Temple University College of Public Health department conducted a project to promote awareness around opioid use and reduce associated stigma by asking students to create art pieces that were displayed on a website they created and promoted via social media.[211] Quantitative and qualitative data was recorded to measure engagement, and the student artists were interviewed, which revealed a change in perspective and understanding, as well as greater appreciation of diverse experiences. Ultimately, the project found that art was an effective medium for empowering both the artist creating the work and the person interacting with it.[211]
Another author critically examined works by contemporary Canadian artists that deal with addiction via the metaphor of a cultural landscape to "unmap" and "remap" ideologies related to Indigenous communities and addiction to demonstrate how colonial violence in Canada has drastically impacted the relationship between Indigenous peoples, their land, and substance abuse.[212]
A project known as "Voice" was a collection of art, poetry and narratives created by women living with a history of addiction to explore women's understanding of harm reduction, challenge the effects of stigma and give voice to those who have historically been silenced or devalued.[213] In the project, nurses with knowledge of mainstream systems, aesthetic knowing, feminism and substance use organized weekly gatherings, wherein women with histories of substance use and addiction worked alongside a nurse to create artistic expressions. Creations were presented at several venues, including an International Conference on Drug Related Harm, a Nursing Conference and a local gallery to positive community response.[213]
Social scientific models
[edit]
Biopsychosocial–cultural–spiritual
[edit]While regarded biomedically as a neuropsychological disorder, addiction is multi-layered, with biological, psychological, social, cultural, and spiritual (biopsychosocial–cultural–spiritual) elements.[214][215] A biopsychosocial–cultural–spiritual approach fosters the crossing of disciplinary boundaries, and promotes holistic considerations of addiction.[216][217][218] A biopsychosocial–cultural–spiritual approach considers, for example, how physical environments influence experiences, habits, and patterns of addiction.
Ethnographic engagements and developments in fields of knowledge have contributed to biopsychosocial–cultural–spiritual understandings of addiction, including the work of Philippe Bourgois, whose fieldwork with street-level drug dealers in East Harlem highlights correlations between drug use and structural oppression in the United States.[219] Prior models that have informed the prevailing biopsychosocial–cultural–spiritual consideration of addiction include:
Cultural model
[edit]The cultural model, an anthropological understanding of the emergence of drug use and abuse, was developed by Dwight Heath.[220] Heath undertook ethnographic research and fieldwork with the Camba people of Bolivia from June 1956 to August 1957.[221] Heath observed that adult members of society drank 'large quantities of rum and became intoxicated for several contiguous days at least twice a month'.[220] This frequent, heavy drinking from which intoxication followed was typically undertaken socially, during festivals.[221] Having returned in 1989, Heath observed that while much had changed, 'drinking parties' remained, as per his initial observations, and 'there appear to be no harmful consequences to anyone'.[222] Heath's observations and interactions reflected that this form of social behavior, the habitual heavy consumption of alcohol, was encouraged and valued, enforcing social bonds in the Camba community.[221] Despite frequent intoxication, "even to the point of unconsciousness", the Camba held no concept of alcoholism (a form of addiction), and no visible social problems associated with drunkenness, or addiction, were apparent.[220]
As noted by Merrill Singer, Heath's findings, when considered alongside subsequent cross-cultural experiences, challenged the perception that intoxication is socially 'inherently disruptive'.[220] Following this fieldwork, Heath proposed the 'cultural model', suggesting that 'problems' associated with heavy drinking, such as alcoholism – a recognised form addiction – were cultural: that is, that alcoholism is determined by cultural beliefs, and therefore varies among cultures. Heath's findings challenged the notion that 'continued use [of alcohol] is inexorably addictive and damaging to the consumer's health'.[221][220]
The cultural model did face criticism by Sociologist Robin Room and others, who felt anthropologists could "downgrade the severity of the problem".[220] Merrill Singer found it notable that the ethnographers working within the prominence of the cultural model were part of the 'wet generation': while not blind to the 'disruptive, dysfunctional and debilitating effects of alcohol consumption', they were products 'socialized to view alcohol consumption as normal'.[220]
Subcultural model
[edit]Historically, addiction has been viewed from the etic perspective, defining users through the pathology of their condition.[223] As reports of drug use rapidly increased, the cultural model found application in anthropological research exploring western drug subculture practices.[220]
The approach evolved from the ethnographic exploration into the lived experiences and subjectivities of 1960s and 70s drug subcultures.[220] The seminal publication "Taking care of business", by Edward Preble and John J. Casey, documented the daily lives of New York street-based intravenous heroin users in detail, providing insight into the dynamic social worlds and activities that surrounded their drug use.[224] These findings challenge popular narratives of immorality and deviance, conceptualizing substance abuse as a social phenomenon. The prevailing culture can have an influence on drug taking behaviors, along with the physical and psychological effects of the drug.[225] To marginalized individuals, drug subcultures can provide social connection, symbolic meaning, and socially constructed purpose that they may feel is unattainable through conventional means.[225] The subcultural model demonstrates the complexities of addiction, highlighting the need for an integrated approach. It contends that a biosocial approach is required to achieve a holistic understanding of addiction.[220]
Critical medical anthropology model
[edit]Emerging in the early 1980s, the critical medical anthropology model was introduced, and as Merrill Singer offers 'was applied quickly to the analysis of drug use'.[220] Where the cultural model of the 1950s looked at the social body, the critical medical anthropology model revealed the body politic, considering drug use and addiction within the context of macro level structures including larger political systems, economic inequalities, and the institutional power held over social processes.[220]
Highly relevant to addiction, the three issues emphasized in the model are:
- Self-medication
- The social production of suffering
- The political economy (Licit and Illicit Drugs)[220]
These three key points highlight how drugs may come to be used to self-medicate the psychological trauma of socio-political disparity and injustice, intertwining with licit and illicit drug market politics.[220] Social suffering, "the misery among those on the weaker end of power relations in terms of physical health, mental health and lived experience", is used by anthropologists to analyze how individuals may have personal problems caused by political and economic power.[220] From the perspective of critical medical anthropology heavy drug use and addiction is a consequence of such larger scale unequal distributions of power.[220]
The three models developed here – the cultural model, the subcultural model, and the Critical Medical Anthropology Model – display how addiction is not an experience to be considered only biomedically. Through consideration of addiction alongside the biological, psychological, social, cultural and spiritual (biopsychosocial–spiritual) elements which influence its experience, a holistic and comprehensive understanding can be built.
Social learning models
[edit]Social learning theory
[edit]Albert Bandura's 1977 social learning theory posits that individuals acquire addictive behaviors by observing and imitating models in their social environment.[226][227] The likelihood of engaging in and sustaining similar addictive behaviors is influenced by the reinforcement and punishment observed in others. The principle of reciprocal determinism suggests that the functional relationships between personal, environmental, and behavioral factors act as determinants of addictive behavior.[228] Thus, effective treatment targets each dynamic facet of the biopsychosocial disorder.
Transtheoretical model (stages of change model)
[edit]The transtheoretical model of change suggests that overcoming an addiction is a stepwise process that occurs through several stages.[229]
Precontemplation: This initial stage precedes individuals considering a change in their behavior. They might be oblivious to or in denial of their addiction, failing to recognize the need for change.
Contemplation is the stage in which individuals become aware of the problems caused by their addiction and are considering change. Although they may not fully commit, they weigh the costs and benefits of making a shift.
Preparation: Individuals in this stage are getting ready to change. They might have taken preliminary steps, like gathering information or making small commitments, in preparation for behavioral change.
Action involves actively modifying behavior by making specific, observable changes to address the addictive behavior. The action stage requires significant effort and commitment.
Maintenance: After successfully implementing a change, individuals enter the maintenance stage, where they work to sustain the new behavior and prevent relapse. This stage is characterized by ongoing effort and consolidation of gains.
Termination/relapse prevention: Recognizing that relapse is a common part of the change process, this stage focuses on identifying and addressing factors that may lead to a return to old behaviors. Relapse is viewed as an opportunity for learning and strategy adjustment, with the ultimate goal of eliminating or terminating the targeted behavior.
The transtheoretical model can be helpful in guiding development of tailored behavioral interventions that can promote lasting change. Progression through these stages may not always follow a linear path, as individuals may move back and forth between stages. Resistance to change is recognized as an expected part of the process.
Addiction causes an "astoundingly high financial and human toll" on individuals and society as a whole.[230][159][162] In the United States, the total economic cost to society is greater than that of all types of diabetes and all cancers combined.[162] These costs arise from the direct adverse effects of drugs and associated healthcare costs (e.g., emergency medical services and outpatient and inpatient care), long-term complications (e.g., lung cancer from smoking tobacco products, liver cirrhosis and dementia from chronic alcohol consumption, and meth mouth from methamphetamine use), the loss of productivity and associated welfare costs, fatal and non-fatal accidents (e.g., traffic collisions), suicides, homicides, and incarceration, among others.[230][159][162][231] The US National Institute on Drug Abuse has found that overdose deaths in the US have almost tripled among males and females from 2002 to 2017, with 72,306 overdose deaths reported in 2017 in the US.[232] 2020 marked the year with the highest number of overdose deaths over a 12-month period, with 81,000 overdose deaths, exceeding the records set in 2017.[233]
See also
[edit]Endnotes
[edit]- ^ In other words, a person cannot control the neurobiological processes that occur in the body in response to using an addictive drug. A person can make a voluntary choice to, for example, start using a drug (or not), or to seek help after becoming addicted, although resisting the urge to use drug(s) becomes increasingly difficult as addiction worsens. See [2] for detailed discussion.
Notes
[edit]- ^ According to a review of experimental animal models that examined the transgenerational epigenetic inheritance of epigenetic marks that occur in addiction, alterations in histone acetylation – specifically, di-acetylation of lysine residues 9 and 14 on histone 3 (i.e., H3K9ac2 and H3K14ac2) in association with BDNF gene promoters – have been shown to occur within the medial prefrontal cortex (mPFC), testes, and sperm of cocaine-addicted male rats.[53] These epigenetic alterations in the rat mPFC result in increased BDNF gene expression within the mPFC, which in turn blunts the rewarding properties of cocaine and reduces cocaine self-administration.[53] The male but not female offspring of these cocaine-exposed rats inherited both epigenetic marks (i.e., di-acetylation of lysine residues 9 and 14 on histone 3) within mPFC neurons, the corresponding increase in BDNF expression within mPFC neurons, and the behavioral phenotype associated with these effects (i.e., a reduction in cocaine reward, resulting in reduced cocaine-seeking by these male offspring).[53] Consequently, the transmission of these two cocaine-induced epigenetic alterations (i.e., H3K9ac2 and H3K14ac2) in rats from male fathers to male offspring served to reduce the offspring's risk of developing an addiction to cocaine.[53] As of 2018,[update] neither the heritability of these epigenetic marks in humans nor the behavioral effects of the marks within human mPFC neurons has been established.[53]
- ^ a b A decrease in aversion sensitivity, in simpler terms, means that an individual's behavior is less likely to be influenced by undesirable outcomes.
- ^ In other words, c-Fos repression allows ΔFosB to more rapidly accumulate within the D1-type medium spiny neurons of the nucleus accumbens because it is selectively induced in this state.[3] Before c-Fos repression, all Fos family proteins (e.g., c-Fos, Fra1, Fra2, FosB, and ΔFosB) are induced together, with ΔFosB expression increasing to a lesser extent.[3]
- ^ According to two medical reviews, ΔFosB has been implicated in causing both increases and decreases in dynorphin expression in different studies;[84][116] this table entry reflects only a decrease.
- ^ Incentive salience, the "motivational salience" for a reward, is a "desire" or "want" attribute, which includes a motivational component, that the brain assigns to a rewarding stimulus.[117][118] As a consequence, incentive salience acts as a motivational "magnet" for a rewarding stimulus that commands attention, induces approach, and causes the rewarding stimulus to be sought out.[117]
- ^ In simplest terms, this means that when either amphetamine or sex is perceived as more alluring or desirable through reward sensitization, this effect occurs with the other as well.
- ^ The lifetime prevalence of an addiction is the percentage of individuals in a population that developed an addiction at some point in their life.
- Image legend
- ^ (Text color) Transcription factors
References
[edit]- ^ Heather N, Best D, Kawalek A, Field M, Lewis M, Rotgers F, et al. (4 July 2018). "Challenging the brain disease model of addiction: European launch of the addiction theory network". Addiction Research & Theory. 26 (4): 249–255. doi:10.1080/16066359.2017.1399659. ISSN 1606-6359.
- ^ a b Heilig M, MacKillop J, Martinez D, Rehm J, Leggio L, Vanderschuren LJ (September 2021). "Addiction as a brain disease revised: why it still matters, and the need for consilience". Neuropsychopharmacology. 46 (10): 1715–1723. doi:10.1038/s41386-020-00950-y. ISSN 0893-133X. PMC 8357831. PMID 33619327.
pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them.
- ^ a b c d e f g h i j k l m n o p q r s t Nestler EJ (December 2013). "Cellular basis of memory for addiction". Dialogues in Clinical Neuroscience. 15 (4): 431–443. PMC 3898681. PMID 24459410.
Despite the importance of numerous psychosocial factors, at its core, drug addiction involves a biological process: the ability of repeated exposure to a drug of abuse to induce changes in a vulnerable brain that drive the compulsive seeking and taking of drugs, and loss of control over drug use, that define a state of addiction. ... A large body of literature has demonstrated that such ΔFosB induction in D1-type [nucleus accumbens] neurons increases an animal's sensitivity to drug as well as natural rewards and promotes drug self-administration, presumably through a process of positive reinforcement ... Another ΔFosB target is cFos: as ΔFosB accumulates with repeated drug exposure it represses c-Fos and contributes to the molecular switch whereby ΔFosB is selectively induced in the chronic drug-treated state.41 ... Moreover, there is increasing evidence that, despite a range of genetic risks for addiction across the population, exposure to sufficiently high doses of a drug for long periods of time can transform someone who has relatively lower genetic loading into an addict.
- ^ a b c "Drugs, Brains, and Behavior: The Science of Addiction – Drug Misuse and Addiction". www.drugabuse.gov. North Bethesda, Maryland: National Institute on Drug Abuse. 13 July 2020. Retrieved 23 December 2021.
- ^ Henden E (2017). "Addiction, Compulsion, and Weakness of the Will: A Dual-Process Perspective.". In Heather N, Gabriel S (eds.). Addiction and Choice: Rethinking the Relationship. Oxford, UK: Oxford University Press. pp. 116–132.
- ^ Heinz A, Beck A, Halil MG, Pilhatsch M, Smolka MN, Liu S (24 July 2019). "Addiction as Learned Behavior Patterns". Journal of Clinical Medicine. 8 (8): 1086. doi:10.3390/jcm8081086. ISSN 2077-0383. PMC 6723628. PMID 31344831.
- ^ Wingo T, Nesil T, Choi JS, Li MD (September 2016). "Novelty Seeking and Drug Addiction in Humans and Animals: From Behavior to Molecules". Journal of Neuroimmune Pharmacology. 11 (3): 456–470. doi:10.1007/s11481-015-9636-7. ISSN 1557-1890. PMC 4837094. PMID 26481371.
- ^ Angres DH, Bettinardi-Angres K (October 2008). "The disease of addiction: origins, treatment, and recovery". Disease-a-Month. 54 (10): 696–721. doi:10.1016/j.disamonth.2008.07.002. PMID 18790142.
- ^ a b Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and Addictive Disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (second ed.). New York: McGraw-Hill Medical. pp. 364–65, 375. ISBN 978-0-07-148127-4.
The defining feature of addiction is compulsive, out-of-control drug use, despite negative consequences. ...
compulsive eating, shopping, gambling, and sex – so-called "natural addictions" – Indeed, addiction to both drugs and behavioral rewards may arise from similar dysregulation of the mesolimbic dopamine system. - ^ Marlatt GA, Baer JS, Donovan DM, Kivlahan DR (1988). "Addictive behaviors: etiology and treatment". Annu Rev Psychol. 39: 223–52. doi:10.1146/annurev.ps.39.020188.001255. PMID 3278676.
- ^ ME (12 September 2019). "Gaming Addiction in ICD-11: Issues and Implications". Psychiatric Times. Psychiatric Times Vol 36, Issue 9. 36 (9). Archived from the original on 3 March 2020. Retrieved 3 March 2020.
- ^ a b c d e f g h i j k l m n di Giacomo E, Aliberti F, Pescatore F, Santorelli M, Pessina R, Placenti V, et al. (August 2022). "Disentangling binge eating disorder and food addiction: a systematic review and meta-analysis". Eating and Weight Disorders. 27 (6): 1963–1970. doi:10.1007/s40519-021-01354-7. PMC 9287203. PMID 35041154.
- ^ a b c "Mental Health and Substance Use Co-Occurring Disorders". MentalHealth.gov. Retrieved 29 November 2022.
- ^ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and Addictive Disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 364–375. ISBN 978-0-07-148127-4.
- ^ a b Volkow ND, Koob GF, McLellan AT (January 2016). "Neurobiologic Advances from the Brain Disease Model of Addiction". New England Journal of Medicine. 374 (4): 363–371. doi:10.1056/NEJMra1511480. PMC 6135257. PMID 26816013.
Substance-use disorder: A diagnostic term in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) referring to recurrent use of alcohol or other drugs that causes clinically and functionally significant impairment, such as health problems, disability, and failure to meet major responsibilities at work, school, or home. Depending on the level of severity, this disorder is classified as mild, moderate, or severe.
Addiction: A term used to indicate the most severe, chronic stage of substance-use disorder, in which there is a substantial loss of self-control, as indicated by compulsive drug taking despite the desire to stop taking the drug. In the DSM-5, the term addiction is synonymous with the classification of severe substance-use disorder. - ^ Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (5th ed.). American Psychiatric Association. 2013. ISBN 978-0-89042-554-1.
- ^ a b c d NIDA (13 July 2020). "Drug Misuse and Addiction". National Institute of Drug Abuse. U.S. Department of Health and Human Services. Archived from the original on 27 January 2022. Retrieved 15 November 2022.
- ^ a b c d e f g h i Levy N (2019). "Chapter 5 Addiction: The belief oscillation hypothesis". In Pickard H, Ahmed SH (eds.). The Routledge handbook of philosophy and science of addiction. Wellcome Trust–Funded Monographs and Book Chapters. Oxon (UK): Routledge. doi:10.4324/9781315689197-6. ISBN 978-1-138-90928-1. OCLC 1042341025. PMID 31017751. S2CID 242067468.
- ^ "Food addiction: Symptoms and management". www.medicalnewstoday.com. 17 February 2020. Retrieved 15 November 2022.
- ^ a b c d e f g h i j k l Skylstad V, Babirye JN, Kiguli J, Solheim Skar AM, et al. (March 2022). "Are we overlooking alcohol use by younger children?". BMJ Paediatrics Open. 6 (1) e001242. doi:10.1136/bmjpo-2021-001242. PMC 8905875. PMID 36053657.
- ^ "Drug addiction (substance use disorder) – Symptoms and causes". Mayo Clinic. Retrieved 15 November 2022.
- ^ Drummond DC (3 May 2002). "Theories of drug craving, ancient and modern". Addiction. 96 (1): 33–46. doi:10.1046/j.1360-0443.2001.961333.x. PMID 11177518.
- ^ a b c d e f g h Maxwell AL, Gardiner E, Loxton NJ (9 February 2020). "Investigating the relationship between reward sensitivity, impulsivity, and food addiction: A systematic review". European Eating Disorders Review. 28 (4): 368–384. doi:10.1002/erv.2732. ISSN 1099-0968. PMID 32142199. S2CID 212565361.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac Olsen CM (December 2011). "Natural rewards, neuroplasticity, and non-drug addictions". Neuropharmacology. 61 (7): 1109–22. doi:10.1016/j.neuropharm.2011.03.010. PMC 3139704. PMID 21459101.
Functional neuroimaging studies in humans have shown that gambling (Breiter et al, 2001), shopping (Knutson et al, 2007), orgasm (Komisaruk et al, 2004), playing video games (Koepp et al, 1998; Hoeft et al, 2008) and the sight of appetizing food (Wang et al, 2004a) activate many of the same brain regions (i.e., the mesocorticolimbic system and extended amygdala) as drugs of abuse (Volkow et al, 2004). ... Cross-sensitization is also bidirectional, as a history of amphetamine administration facilitates sexual behavior and enhances the associated increase in NAc DA ... As described for food reward, sexual experience can also lead to activation of plasticity-related signaling cascades. The transcription factor delta FosB is increased in the NAc, PFC, dorsal striatum, and VTA following repeated sexual behavior (Wallace et al., 2008; Pitchers et al., 2010b). This natural increase in delta FosB or viral overexpression of delta FosB within the NAc modulates sexual performance, and NAc blockade of delta FosB attenuates this behavior (Hedges et al, 2009; Pitchers et al., 2010b). Further, viral overexpression of delta FosB enhances the conditioned place preference for an environment paired with sexual experience (Hedges et al., 2009). ... In some people, there is a transition from "normal" to compulsive engagement in natural rewards (such as food or sex), a condition that some have termed behavioral or non-drug addictions (Holden, 2001; Grant et al., 2006a). ... In humans, the role of dopamine signaling in incentive-sensitization processes has recently been highlighted by the observation of a dopamine dysregulation syndrome in some people taking dopaminergic drugs. This syndrome is characterized by a medication-induced increase in (or compulsive) engagement in non-drug rewards such as gambling, shopping, or sex (Evans et al, 2006; Aiken, 2007; Lader, 2008)."
Table 1: Summary of plasticity observed following exposure to drug or natural reinforcers" - ^ a b c d e f g h i j k l m Robison AJ, Nestler EJ (November 2011). "Transcriptional and epigenetic mechanisms of addiction". Nat. Rev. Neurosci. 12 (11): 623–37. doi:10.1038/nrn3111. PMC 3272277. PMID 21989194.
ΔFosB has been linked directly to several addiction-related behaviors ... Importantly, genetic or viral overexpression of ΔJunD, a dominant negative mutant of JunD which antagonizes ΔFosB- and other AP-1-mediated transcriptional activity, in the NAc or OFC blocks these key effects of drug exposure14,22–24. This indicates that ΔFosB is both necessary and sufficient for many of the changes wrought in the brain by chronic drug exposure. ΔFosB is induced in D1-type NAc MSNs by chronic consumption of several natural rewards, including sucrose, high fat food, sex, wheel running, where it promotes that consumption14,26–30. This implicates ΔFosB in the regulation of natural rewards under normal conditions and perhaps during pathological addictive-like states.
- ^ a b c d Goodman B (3 September 2022). Casarella J (ed.). "Food Addiction Signs and Treatments". WebMD. Retrieved 9 March 2023.
- ^ Nehlig A (2004). Coffee, tea, chocolate, and the brain. Boca Raton: CRC Press. pp. 203–218. ISBN 978-0-429-21192-8.
- ^ "Yale Food Addiction Scale". Food and Addiction Science & Treatment Lab. Department of Psychology, University of Michigan. Retrieved 1 November 2022.
- ^ Gearhardt AN, Corbin WR, Brownell KD (February 2016). "Development of the Yale Food Addiction Scale Version 2.0". Psychology of Addictive Behaviors. 30 (1): 113–121. doi:10.1037/adb0000136. PMID 26866783.
- ^ Brunault P, Berthoz S, Gearhardt AN, Gierski F, Kaladjian A, Bertin E, et al. (8 September 2020). "The Modified Yale Food Addiction Scale 2.0: Validation Among Non-Clinical and Clinical French-Speaking Samples and Comparison With the Full Yale Food Addiction Scale 2.0". Frontiers in Psychiatry. 11 480671. doi:10.3389/fpsyt.2020.480671. PMC 7509420. PMID 33033480.
- ^ Hauck C, Cook B, Ellrott T (February 2020). "Food addiction, eating addiction and eating disorders". The Proceedings of the Nutrition Society. 79 (1): 103–112. doi:10.1017/S0029665119001162. PMID 31744566. S2CID 208186539.
- ^ a b Karila L, Wéry A, Weinstein A, Cottencin O, Petit A, Reynaud M, et al. (2014). "Sexual addiction or hypersexual disorder: different terms for the same problem? A review of the literature". Curr. Pharm. Des. 20 (25): 4012–20. doi:10.2174/13816128113199990619. PMID 24001295. S2CID 19042860.
Sexual addiction, which is also known as hypersexual disorder, has largely been ignored by psychiatrists, even though the condition causes serious psychosocial problems for many people. A lack of empirical evidence on sexual addiction is the result of the disease's complete absence from versions of the Diagnostic and Statistical Manual of Mental Disorders. ... Existing prevalence rates of sexual addiction-related disorders range from 3% to 6%. Sexual addiction/hypersexual disorder is used as an umbrella construct to encompass various types of problematic behaviors, including excessive masturbation, cybersex, pornography use, sexual behavior with consenting adults, telephone sex, strip club visitation, and other behaviors. The adverse consequences of sexual addiction are similar to the consequences of other addictive disorders. Addictive, somatic and psychiatric disorders coexist with sexual addiction. In recent years, research on sexual addiction has proliferated, and screening instruments have increasingly been developed to diagnose or quantify sexual addiction disorders. In our systematic review of the existing measures, 22 questionnaires were identified. As with other behavioral addictions, the appropriate treatment of sexual addiction should combine pharmacological and psychological approaches.
- ^ a b c Pitchers KK, Vialou V, Nestler EJ, Laviolette SR, Lehman MN, Coolen LM (February 2013). "Natural and drug rewards act on common neural plasticity mechanisms with ΔFosB as a key mediator". The Journal of Neuroscience. 33 (8): 3434–42. doi:10.1523/JNEUROSCI.4881-12.2013. PMC 3865508. PMID 23426671.
Drugs of abuse induce neuroplasticity in the natural reward pathway, specifically the nucleus accumbens (NAc), thereby causing development and expression of addictive behavior. ... Together, these findings demonstrate that drugs of abuse and natural reward behaviors act on common molecular and cellular mechanisms of plasticity that control vulnerability to drug addiction, and that this increased vulnerability is mediated by ΔFosB and its downstream transcriptional targets. ... Sexual behavior is highly rewarding (Tenk et al., 2009), and sexual experience causes sensitized drug-related behaviors, including cross-sensitization to amphetamine (Amph)-induced locomotor activity (Bradley and Meisel, 2001; Pitchers et al., 2010a) and enhanced Amph reward (Pitchers et al., 2010a). Moreover, sexual experience induces neural plasticity in the NAc similar to that induced by psychostimulant exposure, including increased dendritic spine density (Meisel and Mullins, 2006; Pitchers et al., 2010a), altered glutamate receptor trafficking, and decreased synaptic strength in prefrontal cortex-responding NAc shell neurons (Pitchers et al., 2012). Finally, periods of abstinence from sexual experience were found to be critical for enhanced Amph reward, NAc spinogenesis (Pitchers et al., 2010a), and glutamate receptor trafficking (Pitchers et al., 2012). These findings suggest that natural and drug reward experiences share common mechanisms of neural plasticity
- ^ a b c Beloate LN, Weems PW, Casey GR, Webb IC, Coolen LM (February 2016). "Nucleus accumbens NMDA receptor activation regulates amphetamine cross-sensitization and deltaFosB expression following sexual experience in male rats". Neuropharmacology. 101: 154–64. doi:10.1016/j.neuropharm.2015.09.023. PMID 26391065. S2CID 25317397.
- ^ a b Alavi SS, Ferdosi M, Jannatifard F, Eslami M, Alaghemandan H, Setare M (April 2012). "Behavioral Addiction versus Substance Addiction: Correspondence of Psychiatric and Psychological Views". International Journal of Preventive Medicine. 3 (4): 290–294. PMC 3354400. PMID 22624087.
- ^ Fehrman E, Egan V, Gorban AN, Levesley J, Mirkes EM, Muhammad AK (2019). Personality Traits and Drug Consumption. A Story Told by Data. Springer, Cham. arXiv:2001.06520. doi:10.1007/978-3-030-10442-9. ISBN 978-3-030-10441-2. S2CID 151160405.
- ^ Cheetham A, Allen NB, Yücel M, Lubman DI (August 2010). "The role of affective dysregulation in drug addiction". Clin Psychol Rev. 30 (6): 621–34. doi:10.1016/j.cpr.2010.04.005. PMID 20546986.
- ^ Franken IH, Muris P (2006). "BIS/BAS personality characteristics and college students' substance use". Personality and Individual Differences. 40 (7): 1497–503. doi:10.1016/j.paid.2005.12.005.
- ^ Genovese JE, Wallace D (December 2007). "Reward sensitivity and substance abuse in middle school and high school students". J Genet Psychol. 168 (4): 465–69. doi:10.3200/GNTP.168.4.465-469. PMID 18232522. S2CID 207640075.
- ^ Kimbrel NA, Nelson-Gray RO, Mitchell JT (April 2007). "Reinforcement sensitivity and maternal style as predictors of psychopathology". Personality and Individual Differences. 42 (6): 1139–49. doi:10.1016/j.paid.2006.06.028.
- ^ Dawe S, Loxton NJ (May 2004). "The role of impulsivity in the development of substance use and eating disorders". Neurosci Biobehav Rev. 28 (3): 343–51. doi:10.1016/j.neubiorev.2004.03.007. PMID 15225976. S2CID 24435589.
- ^ a b c d e f Hill R, Harris J (2 November 2021). "Psychological Approaches to Addiction". In Day E (ed.). Seminars in addiction psychiatry (2nd ed.). Cambridge: Cambridge University Press. pp. 147–169. doi:10.1017/9781911623199.009. ISBN 978-1-911623-19-9. S2CID 242036830.
- ^ Washburn DA (2016). "The Stroop effect at 80: The competition between stimulus control and cognitive control". J Exp Anal Behav. 105 (1): 3–13. doi:10.1002/jeab.194. PMID 26781048.
Today, arguably more than at any time in history, the constructs of attention, executive functioning, and cognitive control seem to be pervasive and preeminent in research and theory. Even within the cognitive framework, however, there has long been an understanding that behavior is multiply determined, and that many responses are relatively automatic, unattended, contention-scheduled, and habitual. Indeed, the cognitive flexibility, response inhibition, and self-regulation that appear to be hallmarks of cognitive control are noteworthy only in contrast to responses that are relatively rigid, associative, and involuntary.
- ^ Diamond A (2013). "Executive functions". Annu Rev Psychol. 64: 135–68. doi:10.1146/annurev-psych-113011-143750. PMC 4084861. PMID 23020641.
Core EFs are inhibition [response inhibition (self-control – resisting temptations and resisting acting impulsively) and interference control (selective attention and cognitive inhibition)], working memory, and cognitive flexibility (including creatively thinking "outside the box," seeing anything from different perspectives, and quickly and flexibly adapting to changed circumstances). ... EFs and prefrontal cortex are the first to suffer, and suffer disproportionately, if something is not right in your life. They suffer first, and most, if you are stressed (Arnsten 1998, Liston et al. 2009, Oaten & Cheng 2005), sad (Hirt et al. 2008, von Hecker & Meiser 2005), lonely (Baumeister et al. 2002, Cacioppo & Patrick 2008, Campbell et al. 2006, Tun et al. 2012), sleep deprived (Barnes et al. 2012, Huang et al. 2007), or not physically fit (Best 2010, Chaddock et al. 2011, Hillman et al. 2008). Any of these can cause you to appear to have a disorder of EFs, such as ADHD, when you do not. You can see the deleterious effects of stress, sadness, loneliness, and lack of physical health or fitness at the physiological and neuroanatomical level in prefrontal cortex and at the behavioral level in worse EFs (poorer reasoning and problem solving, forgetting things, and impaired ability to exercise discipline and self-control). ...
EFs can be improved (Diamond & Lee 2011, Klingberg 2010). ... At any age across the life cycle EFs can be improved, including in the elderly and in infants. There has been much work with excellent results on improving EFs in the elderly by improving physical fitness (Erickson & Kramer 2009, Voss et al. 2011) ... Inhibitory control (one of the core EFs) involves being able to control one's attention, behavior, thoughts, and/or emotions to override a strong internal predisposition or external lure, and instead do what's more appropriate or needed. Without inhibitory control we would be at the mercy of impulses, old habits of thought or action (conditioned responses), and/or stimuli in the environment that pull us this way or that. Thus, inhibitory control makes it possible for us to change and for us to choose how we react and how we behave rather than being unthinking creatures of habit. It doesn't make it easy. Indeed, we usually are creatures of habit and our behavior is under the control of environmental stimuli far more than we usually realize, but having the ability to exercise inhibitory control creates the possibility of change and choice. ... The subthalamic nucleus appears to play a critical role in preventing such impulsive or premature responding (Frank 2006). - ^ a b Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 13: Higher Cognitive Function and Behavioral Control". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 313–21. ISBN 978-0-07-148127-4.
• Executive function, the cognitive control of behavior, depends on the prefrontal cortex, which is highly developed in higher primates and especially humans.
• Working memory is a short-term, capacity-limited cognitive buffer that stores information and permits its manipulation to guide decision-making and behavior. ...
These diverse inputs and back projections to both cortical and subcortical structures put the prefrontal cortex in a position to exert what is called "top-down" control or cognitive control of behavior. ... The prefrontal cortex receives inputs not only from other cortical regions, including association cortex, but also, via the thalamus, inputs from subcortical structures subserving emotion and motivation, such as the amygdala (Chapter 14) and ventral striatum (or nucleus accumbens; Chapter 15). ...
In conditions in which prepotent responses tend to dominate behavior, such as in drug addiction, where drug cues can elicit drug seeking (Chapter 15), or in attention deficit hyperactivity disorder (ADHD; described below), significant negative consequences can result. ... ADHD can be conceptualized as a disorder of executive function; specifically, ADHD is characterized by reduced ability to exert and maintain cognitive control of behavior. Compared with healthy individuals, those with ADHD have diminished ability to suppress inappropriate prepotent responses to stimuli (impaired response inhibition) and diminished ability to inhibit responses to irrelevant stimuli (impaired interference suppression). ... Functional neuroimaging in humans demonstrates activation of the prefrontal cortex and caudate nucleus (part of the striatum) in tasks that demand inhibitory control of behavior. Subjects with ADHD exhibit less activation of the medial prefrontal cortex than healthy controls even when they succeed in such tasks and utilize different circuits. ... Early results with structural MRI show thinning of the cerebral cortex in ADHD subjects compared with age-matched controls in prefrontal cortex and posterior parietal cortex, areas involved in working memory and attention. - ^ a b c d e f Gould TJ (December 2010). "Addiction and cognition". Addiction Science & Clinical Practice. 5 (2): 4–14. PMC 3120118. PMID 22002448.
- ^ Feltenstein MW, See RE (May 2008). "The neurocircuitry of addiction: an overview". British Journal of Pharmacology. 154 (2): 261–274. doi:10.1038/bjp.2008.51. PMC 2442446. PMID 18311189.
- ^ Nesse R (1998). "Emotional disorders in evolutionary perspective". British Journal of Medical Psychology. 71 (4): 397–415. doi:10.1111/j.2044-8341.1998.tb01000.x. ISSN 2044-8341. PMID 9875953.
- ^ Durrant R, Adamson S, Todd F, Sellman D (13 November 2009). "Drug use and addiction: evolutionary perspective". Australian and New Zealand Journal of Psychiatry. 43 (11): 1049–1056. doi:10.3109/00048670903270449. ISSN 0004-8674. PMID 20001400.
- ^ Saah T (29 June 2005). "The evolutionary origins and significance of drug addiction". Harm Reduction Journal. 2 (1) 8. doi:10.1186/1477-7517-2-8. ISSN 1477-7517. PMC 1174878. PMID 15987511.
- ^ Sullivan RJ, Hagen EH, Hammerstein P (19 March 2008). "Revealing the paradox of drug reward in human evolution". Proceedings of the Royal Society B: Biological Sciences. 275 (1640): 1231–1241. doi:10.1098/rspb.2007.1673. ISSN 0962-8452. PMC 2367444. PMID 18353749.
- ^ Sullivan RJ, Hagen EH, Hammerstein P (19 March 2008). "Revealing the paradox of drug reward in human evolution". Proceedings of the Royal Society B: Biological Sciences. 275 (1640): 1231–1241. doi:10.1098/rspb.2007.1673. PMC 2367444. PMID 18353749.
- ^ a b c d e f g h i j k l m n o p Vassoler FM, Sadri-Vakili G (2014). "Mechanisms of transgenerational inheritance of addictive-like behaviors". Neuroscience. 264: 198–206. doi:10.1016/j.neuroscience.2013.07.064. PMC 3872494. PMID 23920159.
However, the components that are responsible for the heritability of characteristics that make an individual more susceptible to drug addiction in humans remain largely unknown given that patterns of inheritance cannot be explained by simple genetic mechanisms (Cloninger et al., 1981; Schuckit et al., 1972). The environment plays a large role in the development of addiction as evidenced by great societal variability in drug use patterns between countries and across time (UNODC, 2012). Therefore, both genetics and the environment contribute to an individual's vulnerability to become addicted following an initial exposure to drugs of abuse. ...
The evidence presented here demonstrates that rapid environmental adaptation occurs following exposure to a number of stimuli. Epigenetic mechanisms represent the key components by which the environment can influence genetics, and they provide the missing link between genetic heritability and environmental influences on the behavioral and physiological phenotypes of the offspring. - ^ Douglas KR, Chan G, Gelernter J, Arias AJ, Anton RF, Weiss RD, et al. (January 2010). "Adverse childhood events as risk factors for substance dependence: partial mediation by mood and anxiety disorders". Addictive Behaviors. 35 (1): 7–13. doi:10.1016/j.addbeh.2009.07.004. PMC 2763992. PMID 19720467.
- ^ a b Saunders GR, Wang X, Chen F, Jang SK, Liu M, Wang C, et al. (December 2022). "Genetic diversity fuels gene discovery for tobacco and alcohol use". Nature. 612 (7941). Nature Research: 720–724. Bibcode:2022Natur.612..720S. doi:10.1038/s41586-022-05477-4. PMC 9771818. PMID 36477530. S2CID 254434507.
- ^ Mirin SM, Weiss RD, Griffin ML, Michael JL (1 January 1991). "Psychopathology in drug abusers and their families". Comprehensive Psychiatry. 32 (1): 36–51. doi:10.1016/0010-440X(91)90068-N. PMID 2001619.
- ^ Mayfield RD, Harris RA, Schuckit MA (May 2008). "Genetic factors influencing alcohol dependence". British Journal of Pharmacology. 154 (2): 275–287. doi:10.1038/bjp.2008.88. PMC 2442454. PMID 18362899.
- ^ a b Kendler KS, Neale MC, Heath AC, Kessler RC, Eaves LJ (May 1994). "A twin-family study of alcoholism in women". The American Journal of Psychiatry. 151 (5): 707–715. doi:10.1176/ajp.151.5.707. PMID 8166312.
- ^ Crowe JR (1991). "Genetics of alcoholism". Alcohol Health and Research World: 1–11. Retrieved 13 December 2017.
- ^ Melemis SM. "The Genetics of Addiction – Is Addiction a Disease?". I Want to Change My Life. Retrieved 17 September 2018.
- ^ Clarke TK, Crist RC, Kampman KM, Dackis CA, Pettinati HM, O'Brien CP, et al. (2013). "Low frequency genetic variants in the μ-opioid receptor (OPRM1) affect risk for addiction to heroin and cocaine". Neuroscience Letters. 542: 71–75. doi:10.1016/j.neulet.2013.02.018. PMC 3640707. PMID 23454283.
- ^ Hall FS, Drgonova J, Jain S, Uhl GR (December 2013). "Implications of genome wide association studies for addiction: are our a priori assumptions all wrong?". Pharmacology & Therapeutics. 140 (3): 267–79. doi:10.1016/j.pharmthera.2013.07.006. PMC 3797854. PMID 23872493.
- ^ Yang H, Ma J (August 2021). "How the COVID-19 pandemic impacts tobacco addiction: Changes in smoking behavior and associations with well-being". Addictive Behaviors. 119 106917. doi:10.1016/j.addbeh.2021.106917. PMC 9186053. PMID 33862579. S2CID 233278782.
- ^ a b "What are risk factors and protective factors?". National Institute on Drug Abuse. Archived from the original on 30 April 2020. Retrieved 13 December 2017.
- ^ "Understanding Drug Use and Addiction". www.drugabuse.gov. National Institute on Drug Abuse. 6 June 2018. Retrieved 29 May 2020.
- ^ Lewis M (October 2018). Longo DL (ed.). "Brain Change in Addiction as Learning, Not Disease". The New England Journal of Medicine. 379 (16): 1551–1560. doi:10.1056/NEJMra1602872. PMID 30332573. S2CID 205117578.
Addictive activities are determined neither solely by brain changes nor solely by social conditions ... the narrowing seen in addiction takes place within the behavioral repertoire, the social surround, and the brain — all at the same time.
- ^ a b "Adverse Childhood Experiences". samhsa.gov. Rockville, Maryland, United States: Substance Abuse and Mental Health Services Administration. Archived from the original on 9 October 2016. Retrieved 26 September 2016.
- ^ a b Enoch MA (March 2011). "The role of early life stress as a predictor for alcohol and drug dependence". Psychopharmacology. 214 (1): 17–31. doi:10.1007/s00213-010-1916-6. PMC 3005022. PMID 20596857.
- ^ "Environmental Risk Factors". learn.genetics.utah.edu. Archived from the original on 17 September 2018. Retrieved 17 September 2018.
- ^ Marcos AC, Bahr SJ (June 1988). "Control Theory and Adolescent Drug Use". Youth & Society. 19 (4): 395–425. doi:10.1177/0044118X88019004003. ISSN 0044-118X. S2CID 143860602.
- ^ Spear LP (June 2000). "The adolescent brain and age-related behavioral manifestations". Neuroscience and Biobehavioral Reviews. 24 (4): 417–63. CiteSeerX 10.1.1.461.3295. doi:10.1016/s0149-7634(00)00014-2. PMID 10817843. S2CID 14686245.
- ^ Hammond CJ, Mayes LC, Potenza MN (April 2014). "Neurobiology of adolescent substance use and addictive behaviors: treatment implications". Adolescent Medicine. 25 (1): 15–32. PMC 4446977. PMID 25022184.
- ^ Catalano RF, Hawkins JD, Wells EA, Miller J, Brewer D (1990). "Evaluation of the effectiveness of adolescent drug abuse treatment, assessment of risks for relapse, and promising approaches for relapse prevention". The International Journal of the Addictions. 25 (9A – 10A): 1085–140. doi:10.3109/10826089109081039. PMID 2131328.
- ^ Perepletchikova F, Krystal JH, Kaufman J (November 2008). "Practitioner review: adolescent alcohol use disorders: assessment and treatment issues". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 49 (11): 1131–54. doi:10.1111/j.1469-7610.2008.01934.x. PMC 4113213. PMID 19017028.
- ^ a b c "Nationwide Trends". National Institute on Drug Abuse. June 2015. Retrieved 15 December 2017.
- ^ a b "Addiction Statistics – Facts on Drug and Alcohol Addiction". AddictionCenter. Retrieved 17 September 2018.
- ^ SAMHSA. "Risk and Protective Factors". Substance Abuse and Mental Health Administration. Archived from the original on 8 December 2016. Retrieved 19 December 2016.
- ^ "Infographic – Risk Factors of Addiction | Recovery Research Institute". www.recoveryanswers.org. Archived from the original on 17 December 2016. Retrieved 19 December 2016.
- ^ "Drug addiction Risk factors – Mayo Clinic". www.mayoclinic.org. Retrieved 19 December 2016.
- ^ "The Connection Between Mental Illness and Substance Abuse | Dual Diagnosis". Dual Diagnosis. Retrieved 17 September 2018.
- ^ Dupont C, Armant DR, Brenner CA (September 2009). "Epigenetics: definition, mechanisms and clinical perspective". Seminars in Reproductive Medicine. 27 (5): 351–357. doi:10.1055/s-0029-1237423. PMC 2791696. PMID 19711245.
- ^ a b c d Nielsen DA, Utrankar A, Reyes JA, Simons DD, Kosten TR (July 2012). "Epigenetics of drug abuse: predisposition or response". Pharmacogenomics. 13 (10): 1149–1160. doi:10.2217/pgs.12.94. PMC 3463407. PMID 22909205.
- ^ a b c Yuan TF, Li A, Sun X, Ouyang H, Campos C, Rocha NB, et al. (2015). "Transgenerational Inheritance of Paternal Neurobehavioral Phenotypes: Stress, Addiction, Ageing and Metabolism". Mol. Neurobiol. 53 (9): 6367–76. doi:10.1007/s12035-015-9526-2. hdl:10400.22/7331. PMID 26572641. S2CID 25694221.
- ^ a b c d e f g h i j Ruffle JK (November 2014). "Molecular neurobiology of addiction: what's all the (Δ)FosB about?". Am. J. Drug Alcohol Abuse. 40 (6): 428–37. doi:10.3109/00952990.2014.933840. PMID 25083822. S2CID 19157711.
ΔFosB is an essential transcription factor implicated in the molecular and behavioral pathways of addiction following repeated drug exposure. The formation of ΔFosB in multiple brain regions, and the molecular pathway leading to the formation of AP-1 complexes is well understood. The establishment of a functional purpose for ΔFosB has allowed further determination as to some of the key aspects of its molecular cascades[...]As a consequence of our improved understanding of ΔFosB in addiction, it is possible to evaluate the addictive potential of current medications (119), as well as use it as a biomarker for assessing the efficacy of therapeutic interventions (121,122,124). Some of these proposed interventions have limitations (125) or are in their infancy (75). However, it is hoped that some of these preliminary findings may lead to innovative treatments, which are much needed in addiction.
- ^ a b c d e Biliński P, Wojtyła A, Kapka-Skrzypczak L, Chwedorowicz R, Cyranka M, Studziński T (2012). "Epigenetic regulation in drug addiction". Ann. Agric. Environ. Med. 19 (3): 491–96. PMID 23020045.
[...]ΔFosB is considered a primary and causative transcription factor in creating new neural connections in the reward centre, prefrontal cortex, and other regions of the limbic system. This is reflected in the increased, stable and long-lasting level of sensitivity to cocaine and other drugs, and tendency to relapse even after long periods of abstinence.
- ^ a b c Renthal W, Nestler EJ (September 2009). "Chromatin regulation in drug addiction and depression". Dialogues in Clinical Neuroscience. 11 (3): 257–268. doi:10.31887/DCNS.2009.11.3/wrenthal. PMC 2834246. PMID 19877494.
[Psychostimulants] increase cAMP levels in striatum, which activates protein kinase A (PKA) and leads to phosphorylation of its targets. This includes the cAMP response element binding protein (CREB), the phosphorylation of which induces its association with the histone acetyltransferase, CREB binding protein (CBP) to acetylate histones and facilitate gene activation. This is known to occur on many genes including fosB and c-fos in response to psychostimulant exposure. ΔFosB is also upregulated by chronic psychostimulant treatments, and is known to activate certain genes (eg, cdk5) and repress others (eg, c-fos) where it recruits HDAC1 as a corepressor. ... Chronic exposure to psychostimulants increases glutamatergic [signaling] from the prefrontal cortex to the NAc. Glutamatergic signaling elevates Ca2+ levels in NAc postsynaptic elements where it activates CaMK (calcium/calmodulin protein kinases) signaling, which, in addition to phosphorylating CREB, also phosphorylates HDAC5.
Figure 2: Psychostimulant-induced signaling events - ^ Broussard JI (January 2012). "Co-transmission of dopamine and glutamate". The Journal of General Physiology. 139 (1): 93–96. doi:10.1085/jgp.201110659. PMC 3250102. PMID 22200950.
Coincident and convergent input often induces plasticity on a postsynaptic neuron. The NAc integrates processed information about the environment from basolateral amygdala, hippocampus, and prefrontal cortex (PFC), as well as projections from midbrain dopamine neurons. Previous studies have demonstrated how dopamine modulates this integrative process. For example, high frequency stimulation potentiates hippocampal inputs to the NAc while simultaneously depressing PFC synapses (Goto and Grace, 2005). The converse was also shown to be true; stimulation at PFC potentiates PFC–NAc synapses but depresses hippocampal–NAc synapses. In light of the new functional evidence of midbrain dopamine/glutamate co-transmission (references above), new experiments of NAc function will have to test whether midbrain glutamatergic inputs bias or filter either limbic or cortical inputs to guide goal-directed behavior.
- ^ Kanehisa Laboratories (10 October 2014). "Amphetamine – Homo sapiens (human)". KEGG Pathway. Retrieved 31 October 2014.
Most addictive drugs increase extracellular concentrations of dopamine (DA) in nucleus accumbens (NAc) and medial prefrontal cortex (mPFC), projection areas of mesocorticolimbic DA neurons and key components of the "brain reward circuit". Amphetamine achieves this elevation in extracellular levels of DA by promoting efflux from synaptic terminals. ... Chronic exposure to amphetamine induces a unique transcription factor delta FosB, which plays an essential role in long-term adaptive changes in the brain.
- ^ Cadet JL, Brannock C, Jayanthi S, Krasnova IN (2015). "Transcriptional and epigenetic substrates of methamphetamine addiction and withdrawal: evidence from a long-access self-administration model in the rat". Molecular Neurobiology. 51 (2): 696–717 (Figure 1). doi:10.1007/s12035-014-8776-8. PMC 4359351. PMID 24939695.
- ^ a b c Robison AJ, Nestler EJ (November 2011). "Transcriptional and epigenetic mechanisms of addiction". Nature Reviews Neuroscience. 12 (11): 623–637. doi:10.1038/nrn3111. PMC 3272277. PMID 21989194.
ΔFosB serves as one of the master control proteins governing this structural plasticity. ... ΔFosB also represses G9a expression, leading to reduced repressive histone methylation at the cdk5 gene. The net result is gene activation and increased CDK5 expression. ... In contrast, ΔFosB binds to the c-fos gene and recruits several co-repressors, including HDAC1 (histone deacetylase 1) and SIRT 1 (sirtuin 1). ... The net result is c-fos gene repression.
Figure 4: Epigenetic basis of drug regulation of gene expression - ^ a b c d Nestler EJ (December 2012). "Transcriptional mechanisms of drug addiction". Clinical Psychopharmacology and Neuroscience. 10 (3): 136–143. doi:10.9758/cpn.2012.10.3.136. PMC 3569166. PMID 23430970.
The 35-37 kD ΔFosB isoforms accumulate with chronic drug exposure due to their extraordinarily long half-lives. ... As a result of its stability, the ΔFosB protein persists in neurons for at least several weeks after cessation of drug exposure. ... ΔFosB overexpression in nucleus accumbens induces NFκB ... In contrast, the ability of ΔFosB to repress the c-Fos gene occurs in concert with the recruitment of a histone deacetylase and presumably several other repressive proteins such as a repressive histone methyltransferase
- ^ Nestler EJ (October 2008). "Transcriptional mechanisms of addiction: Role of ΔFosB". Philosophical Transactions of the Royal Society B: Biological Sciences. 363 (1507): 3245–3255. doi:10.1098/rstb.2008.0067. PMC 2607320. PMID 18640924.
Recent evidence has shown that ΔFosB also represses the c-fos gene that helps create the molecular switch—from the induction of several short-lived Fos family proteins after acute drug exposure to the predominant accumulation of ΔFosB after chronic drug exposure
- ^ a b Hyman SE, Malenka RC, Nestler EJ (2006). "Neural mechanisms of addiction: the role of reward-related learning and memory". Annu. Rev. Neurosci. 29: 565–98. doi:10.1146/annurev.neuro.29.051605.113009. PMID 16776597.
- ^ Steiner H, Van Waes V (January 2013). "Addiction-related gene regulation: risks of exposure to cognitive enhancers vs. other psychostimulants". Prog. Neurobiol. 100: 60–80. doi:10.1016/j.pneurobio.2012.10.001. PMC 3525776. PMID 23085425.
- ^ Kanehisa Laboratories (2 August 2013). "Alcoholism – Homo sapiens (human)". KEGG Pathway. Retrieved 10 April 2014.
- ^ Kim Y, Teylan MA, Baron M, Sands A, Nairn AC, Greengard P (February 2009). "Methylphenidate-induced dendritic spine formation and DeltaFosB expression in nucleus accumbens". Proc. Natl. Acad. Sci. USA. 106 (8): 2915–20. Bibcode:2009PNAS..106.2915K. doi:10.1073/pnas.0813179106. PMC 2650365. PMID 19202072.
- ^ a b c d e Nestler EJ (January 2014). "Epigenetic mechanisms of drug addiction". Neuropharmacology. 76 (Pt B): 259–68. doi:10.1016/j.neuropharm.2013.04.004. PMC 3766384. PMID 23643695.
Short-term increases in histone acetylation generally promote behavioral responses to the drugs, while sustained increases oppose cocaine's effects, based on the actions of systemic or intra-NAc administration of HDAC inhibitors. ... Genetic or pharmacological blockade of G9a in the NAc potentiates behavioral responses to cocaine and opiates, whereas increasing G9a function exerts the opposite effect (Maze et al., 2010; Sun et al., 2012a). Such drug-induced downregulation of G9a and H3K9me2 also sensitizes animals to the deleterious effects of subsequent chronic stress (Covington et al., 2011). Downregulation of G9a increases the dendritic arborization of NAc neurons, and is associated with increased expression of numerous proteins implicated in synaptic function, which directly connects altered G9a/H3K9me2 in the synaptic plasticity associated with addiction (Maze et al., 2010).
G9a appears to be a critical control point for epigenetic regulation in NAc, as we know it functions in two negative feedback loops. It opposes the induction of ΔFosB, a long-lasting transcription factor important for drug addiction (Robison and Nestler, 2011), while ΔFosB in turn suppresses G9a expression (Maze et al., 2010; Sun et al., 2012a). ... Also, G9a is induced in NAc upon prolonged HDAC inhibition, which explains the paradoxical attenuation of cocaine's behavioral effects seen under these conditions, as noted above (Kennedy et al., 2013). GABAA receptor subunit genes are among those that are controlled by this feedback loop. Thus, chronic cocaine, or prolonged HDAC inhibition, induces several GABAA receptor subunits in NAc, which is associated with increased frequency of inhibitory postsynaptic currents (IPSCs). In striking contrast, combined exposure to cocaine and HDAC inhibition, which triggers the induction of G9a and increased global levels of H3K9me2, leads to blockade of GABAA receptor and IPSC regulation. - ^ a b c d Blum K, Werner T, Carnes S, Carnes P, Bowirrat A, Giordano J, et al. (2012). "Sex, drugs, and rock 'n' roll: hypothesizing common mesolimbic activation as a function of reward gene polymorphisms". Journal of Psychoactive Drugs. 44 (1): 38–55. doi:10.1080/02791072.2012.662112. PMC 4040958. PMID 22641964.
It has been found that deltaFosB gene in the NAc is critical for reinforcing effects of sexual reward. Pitchers and colleagues (2010) reported that sexual experience was shown to cause DeltaFosB accumulation in several limbic brain regions including the NAc, medial pre-frontal cortex, VTA, caudate, and putamen, but not the medial preoptic nucleus. Next, the induction of c-Fos, a downstream (repressed) target of DeltaFosB, was measured in sexually experienced and naive animals. The number of mating-induced c-Fos-IR cells was significantly decreased in sexually experienced animals compared to sexually naive controls. Finally, DeltaFosB levels and its activity in the NAc were manipulated using viral-mediated gene transfer to study its potential role in mediating sexual experience and experience-induced facilitation of sexual performance. Animals with DeltaFosB overexpression displayed enhanced facilitation of sexual performance with sexual experience relative to controls. In contrast, the expression of DeltaJunD, a dominant-negative binding partner of DeltaFosB, attenuated sexual experience-induced facilitation of sexual performance, and stunted long-term maintenance of facilitation compared to DeltaFosB overexpressing group. Together, these findings support a critical role for DeltaFosB expression in the NAc in the reinforcing effects of sexual behavior and sexual experience-induced facilitation of sexual performance. ... both drug addiction and sexual addiction represent pathological forms of neuroplasticity along with the emergence of aberrant behaviors involving a cascade of neurochemical changes mainly in the brain's rewarding circuitry.
- ^ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and addictive disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 384–85. ISBN 978-0-07-148127-4.
- ^ Salamone JD (1992). "Complex motor and sensorimotor functions of striatal and accumbens dopamine: involvement in instrumental behavior processes". Psychopharmacology. 107 (2–3): 160–74. doi:10.1007/bf02245133. PMID 1615120. S2CID 30545845.
- ^ Kauer JA, Malenka RC (November 2007). "Synaptic plasticity and addiction". Nature Reviews. Neuroscience. 8 (11): 844–58. doi:10.1038/nrn2234. PMID 17948030. S2CID 38811195.
- ^ Witten IB, Lin SC, Brodsky M, Prakash R, Diester I, Anikeeva P, et al. (December 2010). "Cholinergic interneurons control local circuit activity and cocaine conditioning". Science. 330 (6011): 1677–81. Bibcode:2010Sci...330.1677W. doi:10.1126/science.1193771. PMC 3142356. PMID 21164015.
- ^ Qeadan F, McCunn A, Tingey B (16 October 2024). "The association between glucose-dependent insulinotropic polypeptide and/or glucagon-like peptide-1 receptor agonist prescriptions and substance-related outcomes in patients with opioid and alcohol use disorders: A real-world data analysis". Addiction. 120 (2): 236–250. doi:10.1111/add.16679. ISSN 0965-2140. PMC 11707322. PMID 39415416.
- ^ Shareef F. "Weight loss drugs like Ozempic may help reduce overdose risks: Study". ABC News. Retrieved 18 October 2024.
- ^ a b Nestler EJ, Barrot M, Self DW (September 2001). "DeltaFosB: a sustained molecular switch for addiction". Proc. Natl. Acad. Sci. U.S.A. 98 (20): 11042–46. Bibcode:2001PNAS...9811042N. doi:10.1073/pnas.191352698. PMC 58680. PMID 11572966.
Although the ΔFosB signal is relatively long-lived, it is not permanent. ΔFosB degrades gradually and can no longer be detected in [the] brain after 1–2 months of drug withdrawal ... Indeed, ΔFosB is the longest-lived adaptation known to occur in [the] adult brain, not only in response to drugs of abuse, but to any other perturbation (that doesn't involve lesions) as well.
- ^ a b Jones S, Bonci A (2005). "Synaptic plasticity and drug addiction". Current Opinion in Pharmacology. 5 (1): 20–25. doi:10.1016/j.coph.2004.08.011. PMID 15661621.
- ^ a b Eisch AJ, Harburg GC (2006). "Opiates, psychostimulants, and adult hippocampal neurogenesis: Insights for addiction and stem cell biology". Hippocampus. 16 (3): 271–86. doi:10.1002/hipo.20161. PMID 16411230. S2CID 23667629.
- ^ Rang HP (2003). Pharmacology. Edinburgh: Churchill Livingstone. p. 596. ISBN 978-0-443-07145-4.
- ^ Kourrich S, Rothwell PE, Klug JR, Thomas MJ (2007). "Cocaine experience controls bidirectional synaptic plasticity in the nucleus accumbens". J. Neurosci. 27 (30): 7921–28. doi:10.1523/JNEUROSCI.1859-07.2007. PMC 6672735. PMID 17652583.
- ^ a b Kalivas PW, Volkow ND (August 2005). "The neural basis of addiction: a pathology of motivation and choice". The American Journal of Psychiatry. 162 (8): 1403–13. doi:10.1176/appi.ajp.162.8.1403. PMID 16055761.
- ^ a b Floresco SB, Ghods-Sharifi S (February 2007). "Amygdala-prefrontal cortical circuitry regulates effort-based decision making". Cerebral Cortex. 17 (2): 251–60. CiteSeerX 10.1.1.335.4681. doi:10.1093/cercor/bhj143. PMID 16495432.
- ^ Perry CJ, Zbukvic I, Kim JH, Lawrence AJ (October 2014). "Role of cues and contexts on drug-seeking behaviour". British Journal of Pharmacology. 171 (20): 4636–72. doi:10.1111/bph.12735. PMC 4209936. PMID 24749941.
- ^ a b c Volkow ND, Fowler JS, Wang GJ, Swanson JM, Telang F (2007). "Dopamine in drug abuse and addiction: results of imaging studies and treatment implications". Arch. Neurol. 64 (11): 1575–79. doi:10.1001/archneur.64.11.1575. PMID 17998440.
- ^ "Drugs, Brains, and Behavior: The Science of Addiction". National Institute on Drug Abuse. 6 July 2020.
- ^ "Understanding Drug Abuse and Addiction". National Institute on Drug Abuse. November 2012. Archived from the original on 16 August 2011. Retrieved 12 February 2015.
- ^ a b c Nestler EJ (October 2008). "Review. Transcriptional mechanisms of addiction: role of DeltaFosB". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 363 (1507): 3245–55. doi:10.1098/rstb.2008.0067. PMC 2607320. PMID 18640924.
Recent evidence has shown that ΔFosB also represses the c-fos gene that helps create the molecular switch – from the induction of several short-lived Fos family proteins after acute drug exposure to the predominant accumulation of ΔFosB after chronic drug exposure – cited earlier (Renthal et al. in press). The mechanism responsible for ΔFosB repression of c-fos expression is complex and is covered below. ...
Examples of validated targets for ΔFosB in nucleus accumbens ... GluR2 ... dynorphin ... Cdk5 ... NFκB ... c-Fos
Table 3 - ^ a b c d e f Berridge KC (April 2012). "From prediction error to incentive salience: mesolimbic computation of reward motivation". Eur. J. Neurosci. 35 (7): 1124–43. doi:10.1111/j.1460-9568.2012.07990.x. PMC 3325516. PMID 22487042.
Here I discuss how mesocorticolimbic mechanisms generate the motivation component of incentive salience. Incentive salience takes Pavlovian learning and memory as one input and as an equally important input takes neurobiological state factors (e.g. drug states, appetite states, satiety states) that can vary independently of learning. Neurobiological state changes can produce unlearned fluctuations or even reversals in the ability of a previously learned reward cue to trigger motivation. Such fluctuations in cue-triggered motivation can dramatically depart from all previously learned values about the associated reward outcome. ... Associative learning and prediction are important contributors to motivation for rewards. Learning gives incentive value to arbitrary cues such as a Pavlovian conditioned stimulus (CS) that is associated with a reward (unconditioned stimulus or UCS). Learned cues for reward are often potent triggers of desires. For example, learned cues can trigger normal appetites in everyone, and can sometimes trigger compulsive urges and relapse in individuals with addictions.
Cue-triggered 'wanting' for the UCS
A brief CS encounter (or brief UCS encounter) often primes a pulse of elevated motivation to obtain and consume more reward UCS. This is a signature feature of incentive salience.
Cue as attractive motivational magnets
When a Pavlovian CS+ is attributed with incentive salience it not only triggers 'wanting' for its UCS, but often the cue itself becomes highly attractive – even to an irrational degree. This cue attraction is another signature feature of incentive salience ... Two recognizable features of incentive salience are often visible that can be used in neuroscience experiments: (i) UCS-directed 'wanting' – CS-triggered pulses of intensified 'wanting' for the UCS reward; and (ii) CS-directed 'wanting' – motivated attraction to the Pavlovian cue, which makes the arbitrary CS stimulus into a motivational magnet. - ^ a b Malenka RC, Nestler EJ, Hyman SE (2009). Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (second ed.). New York: McGraw-Hill Medical. pp. 147–48, 366–67, 375–76. ISBN 978-0-07-148127-4.
VTA DA neurons play a critical role in motivation, reward-related behavior (Chapter 15), attention, and multiple forms of memory. This organization of the DA system, wide projection from a limited number of cell bodies, permits coordinated responses to potent new rewards. Thus, acting in diverse terminal fields, dopamine confers motivational salience ("wanting") on the reward itself or associated cues (nucleus accumbens shell region), updates the value placed on different goals in light of this new experience (orbital prefrontal cortex), helps consolidate multiple forms of memory (amygdala and hippocampus), and encodes new motor programs that will facilitate obtaining this reward in the future (nucleus accumbens core region and dorsal striatum). In this example, dopamine modulates the processing of sensorimotor information in diverse neural circuits to maximize the ability of the organism to obtain future rewards. ...
The brain reward circuitry that is targeted by addictive drugs normally mediates the pleasure and strengthening of behaviors associated with natural reinforcers, such as food, water, and sexual contact. Dopamine neurons in the VTA are activated by food and water, and dopamine release in the NAc is stimulated by the presence of natural reinforcers, such as food, water, or a sexual partner. ...
The NAc and VTA are central components of the circuitry underlying reward and memory of reward. As previously mentioned, the activity of dopaminergic neurons in the VTA appears to be linked to reward prediction. The NAc is involved in learning associated with reinforcement and the modulation of motoric responses to stimuli that satisfy internal homeostatic needs. The shell of the NAc appears to be particularly important to initial drug actions within reward circuitry; addictive drugs appear to have a greater effect on dopamine release in the shell than in the core of the NAc. ... If motivational drive is described in terms of wanting, and hedonic evaluation in terms of liking, it appears that wanting can be dissociated from liking and that dopamine may influence these phenomena differently. Differences between wanting and liking are confirmed in reports by humans with addictions, who state that their desire for drugs (wanting) increases with continued use even when pleasure (liking) decreases because of tolerance. - ^ a b c d Edwards S (2016). "Reinforcement principles for addiction medicine; from recreational drug use to psychiatric disorder". Neuroscience for Addiction Medicine: From Prevention to Rehabilitation - Constructs and Drugs. Progress in Brain Research. Vol. 223. pp. 63–76. doi:10.1016/bs.pbr.2015.07.005. ISBN 978-0-444-63545-7. PMID 26806771.
An important dimension of reinforcement highly relevant to the addiction process (and particularly relapse) is secondary reinforcement (Stewart, 1992). Secondary reinforcers (in many cases also considered conditioned reinforcers) likely drive the majority of reinforcement processes in humans. In the specific case of drug addiction, cues and contexts that are intimately and repeatedly associated with drug use will themselves become reinforcing ... A fundamental piece of Robinson and Berridge's incentive-sensitization theory of addiction posits that the incentive value or attractive nature of such secondary reinforcement processes, in addition to the primary reinforcers themselves, may persist and even become sensitized over time in league with the development of drug addiction (Robinson and Berridge, 1993).
- ^ a b Berridge KC, Kringelbach ML (May 2015). "Pleasure systems in the brain". Neuron. 86 (3): 646–664. doi:10.1016/j.neuron.2015.02.018. PMC 4425246. PMID 25950633.
- ^ a b c Walker DM, Cates HM, Heller EA, Nestler EJ (February 2015). "Regulation of chromatin states by drugs of abuse". Curr. Opin. Neurobiol. 30: 112–21. doi:10.1016/j.conb.2014.11.002. PMC 4293340. PMID 25486626.
Studies investigating general HDAC inhibition on behavioral outcomes have produced varying results but it seems that the effects are specific to the timing of exposure (either before, during or after exposure to drugs of abuse) as well as the length of exposure
- ^ "Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health" (PDF). Office of the Surgeon General. US Department of Health and Human Services. November 2016. pp. 35–37, 45, 63, 155, 317, 338. Retrieved 28 January 2017.
- ^ American Psychiatric Association (2013). "Substance-Related and Addictive Disorders" (PDF). American Psychiatric Publishing. pp. 1–2. Archived from the original (PDF) on 15 August 2015. Retrieved 8 April 2023.
Additionally, the diagnosis of dependence caused much confusion. Most people link dependence with "addiction" when in fact dependence can be a normal body response to a substance.
- ^ Petry NM, Rehbein F, Gentile DA, Lemmens JS, Rumpf HJ, Mößle T, et al. (September 2014). "An international consensus for assessing internet gaming disorder using the new DSM-5 approach". Addiction. 109 (9): 1399–406. doi:10.1111/add.12457. PMID 24456155.
- ^ Torres G, Horowitz JM (1999). "Drugs of abuse and brain gene expression". Psychosom Med. 61 (5): 630–50. CiteSeerX 10.1.1.326.4903. doi:10.1097/00006842-199909000-00007. PMID 10511013.
- ^ Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 16: Reinforcement and Addictive Disorders". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
The official diagnosis of drug addiction by the Diagnostic and Statistic Manual of Mental Disorders (2013), which uses the term substance use disorder, is flawed. Criteria used to make the diagnosis of substance use disorders include tolerance and somatic dependence/withdrawal, even though these processes are not integral to addiction as noted. It is ironic and unfortunate that the manual still avoids use of the term addiction as an official diagnosis, even though addiction provides the best description of the clinical syndrome.
- ^ a b c "International Classification of Diseases 11th revision – ICD-11. Disorders due to substance use or addictive behaviours". World Health Organization. Geneva. 2023. Retrieved 10 April 2023.
- ^ a b "International Classification of Diseases 11th revision – ICD-11. Disorders due to substance use". World Health Organization. Geneva. 2023. Retrieved 24 March 2023.
- ^ Koob GF, Powell P, White A (November 2020). "Addiction as a Coping Response: Hyperkatifeia, Deaths of Despair, and COVID-19". Am J Psychiatry. 177 (11): 1031–1037. doi:10.1176/appi.ajp.2020.20091375. PMID 33135468. S2CID 226233515.
- ^ a b c d Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D (August 2016). "Addictions Neuroclinical Assessment: A Neuroscience-Based Framework for Addictive Disorders". Biological Psychiatry. 80 (3): 179–189. doi:10.1016/j.biopsych.2015.10.024. PMC 4870153. PMID 26772405.
- ^ a b "Tobacco, Alcohol, Prescription medication, and other Substance use (TAPS) Tool". nida.nih.gov. Archived from the original on 14 August 2022. Retrieved 29 November 2022.
- ^ "About the CRAFFT – CRAFFT". Retrieved 3 December 2022.
- ^ a b c "Use the CRAFFT – CRAFFT". Retrieved 3 December 2022.
- ^ a b c Yudko E, Lozhkina O, Fouts A (March 2007). "A comprehensive review of the psychometric properties of the Drug Abuse Screening Test". Journal of Substance Abuse Treatment. 32 (2): 189–198. doi:10.1016/j.jsat.2006.08.002. PMID 17306727.
- ^ Han BH, Moore AA (February 2018). "Prevention and Screening of Unhealthy Substance Use by Older Adults". Clinics in Geriatric Medicine. 34 (1): 117–129. doi:10.1016/j.cger.2017.08.005. PMC 5718360. PMID 29129212.
- ^ Ali R, Meena S, Eastwood B, Richards I, Marsden J (September 2013). "Ultra-rapid screening for substance-use disorders: the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST-Lite)". Drug and Alcohol Dependence. 132 (1–2): 352–361. doi:10.1016/j.drugalcdep.2013.03.001. PMID 23561823.
- ^ a b "Drug abuse liability". Cambridge Cognition. Retrieved 9 March 2021.
- ^ National Institute on Drug Abuse (20 August 2020). "Commonly Used Drugs Charts". National Institute on Drug Abuse. Retrieved 9 March 2021.
- ^ Harwood HJ, Myers TG, Addiction NR (23 July 2004). Vaccines and Immunotherapies to Control Addiction in Minors: The Legal Framework. National Academies Press (US) – via National Center for Biotechnology Information.
- ^ "'Heavy' heroin vaccine provides hope for addiction treatment". Scripps Research. 30 July 2020.
- ^ "Experimental Opioid Vaccine Being Tested at Columbia". Columbia University Irving Medical Center. 1 July 2021.
- ^ Furfaro H (5 January 2022). "To fight opioid crisis, UW researchers take new shot at developing vaccine against addictive drugs". The Seattle Times.
- ^ "A Vaccine Against Addiction". Addiction Center. 12 January 2022.
- ^ American Addiction Centers Editorial Staff (4 January 2022) [December 29, 2016]. "Why Don't We Have Addiction Vaccines?". DrugAbuse.com.
- ^ Barbara Shine (October 2000). "Nicotine Vaccine Moves Toward Clinical Trials". National Institute on Drug Abuse. Archived from the original on 10 August 2006. Retrieved 19 September 2006.
- ^ "Nabi Biopharmaceuticals Website".
- ^ Hatsukami DK, Rennard S, Jorenby D, Fiore M, Koopmeiners J, de Vos A, et al. (2005). "Safety and immunogenicity of a nicotine conjugate vaccine in current smokers". Clinical Pharmacology & Therapeutics. 78 (5): 456–467. doi:10.1016/j.clpt.2005.08.007. PMID 16321612. S2CID 1218556.
- ^ Martell BA, Mitchell E, Poling J, Gonsai K, Kosten TR (July 2005). "Vaccine pharmacotherapy for the treatment of cocaine dependence". Biol. Psychiatry. 58 (2): 158–64. doi:10.1016/j.biopsych.2005.04.032. PMID 16038686. S2CID 22415520.
- ^ "Cocaine vaccine 'stops addiction'". BBC News. 14 June 2004. Retrieved 7 October 2009.
- ^ "CelticPharma: TA-NIC Nicotine Dependence". Archived from the original on 6 December 2009. Retrieved 27 October 2009.
- ^ "UW researcher explains new vaccine in the works to prevent opioid overdoses". KIRO 7. 19 September 2023.
- ^ Taylor SB, Lewis CR, Olive MF (February 2013). "The neurocircuitry of illicit psychostimulant addiction: acute and chronic effects in humans". Subst. Abuse Rehabil. 4: 29–43. doi:10.2147/SAR.S39684. PMC 3931688. PMID 24648786.
Initial drug use can be attributed to the ability of the drug to act as a reward (ie, a pleasurable emotional state or positive reinforcer), which can lead to repeated drug use and dependence.8,9 A great deal of research has focused on the molecular and neuroanatomical mechanisms of the initial rewarding or reinforcing effect of drugs of abuse. ... At present, no pharmacological therapy has been approved by the FDA to treat psychostimulant addiction. Many drugs have been tested, but none have shown conclusive efficacy with tolerable side effects in humans.172 ... A new emphasis on larger-scale biomarker, genetic, and epigenetic research focused on the molecular targets of mental disorders has been recently advocated.212 In addition, the integration of cognitive and behavioral modification of circuit-wide neuroplasticity (i.e., computer-based training to enhance executive function) may prove to be an effective adjunct-treatment approach for addiction, particularly when combined with cognitive enhancers.198,213–216 Furthermore, in order to be effective, all pharmacological or biologically based treatments for addiction need to be integrated into other established forms of addiction rehabilitation, such as CBT, individual and group psychotherapy, behavior-modification strategies, twelve-step programs, and residential treatment facilities.
- ^ Scott CG (July 2000). "Ethical Issues in Addiction Counseling". Rehabilitation Counseling Bulletin. 43 (4): 209–214. doi:10.1177/003435520004300405. ISSN 0034-3552. PMID 15714702. S2CID 28556555.
- ^ Chen CC, Yin SJ (October 2008). "Alcohol abuse and related factors in Asia". International Review of Psychiatry. 20 (5): 425–433. doi:10.1080/09540260802344075. PMID 19012127. S2CID 24571763.
- ^ Mak KK, Lai CM, Watanabe H, Kim DI, Bahar N, Ramos M, et al. (November 2014). "Epidemiology of internet behaviors and addiction among adolescents in six Asian countries". Cyberpsychology, Behavior and Social Networking. 17 (11): 720–728. doi:10.1089/cyber.2014.0139. PMID 25405785.
- ^ Slade T, Johnston A, Teesson M, Whiteford H, Burgess P, Pirkis J, et al. (May 2009). "The Mental Health of Australians 2: Substance Use Disorders in Australia" (PDF). Department of Health and Ageing, Canberra.
- ^ a b Australian Institute of Health and Welfare (AIHW) (2020). National Drug Strategy Household Survey 2019 (Report). doi:10.25816/E42P-A447.
- ^ Peacock A, Leung J, Larney S, Colledge S, Hickman M, Rehm J, et al. (October 2018). "Global statistics on alcohol, tobacco and illicit drug use: 2017 status report". Addiction. 113 (10): 1905–1926. doi:10.1111/add.14234. hdl:11343/283940. PMID 29749059. S2CID 13674349.
- ^ a b c d Merikangas KR, McClair VL (June 2012). "Epidemiology of Substance Use Disorders". Hum. Genet. 131 (6): 779–89. doi:10.1007/s00439-012-1168-0. PMC 4408274. PMID 22543841.
- ^ Manubay JM, Muchow C, Sullivan MA (March 2011). "Prescription drug abuse: epidemiology, regulatory issues, chronic pain management with narcotic analgesics". Primary Care. 38 (1): 71–90. doi:10.1016/j.pop.2010.11.006. PMC 3328297. PMID 21356422.
- ^ Substance Abuse and Mental Health Services Administration (2022). Key substance use and mental health indicators in the United States: Results from the 2021 National Survey on Drug Use and Health (Report). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved 24 March 2023.
- ^ a b c d e f "American Board of Medical Specialties recognizes the new subspecialty of addiction medicine" (PDF). American Board of Addiction Medicine. 14 March 2016. Archived from the original (PDF) on 21 March 2021. Retrieved 3 April 2016.
Sixteen percent of the non-institutionalized U.S. population age 12 and over – more than 40 million Americans – meets medical criteria for addiction involving nicotine, alcohol or other drugs. This is more than the number of Americans with cancer, diabetes or heart conditions. In 2014, 22.5 million people in the United States needed treatment for addiction involving alcohol or drugs other than nicotine, but only 11.6 percent received any form of inpatient, residential, or outpatient treatment. Of those who do receive treatment, few receive evidence-based care. (There is no information available on how many individuals receive treatment for addiction involving nicotine.)
Risky substance use and untreated addiction account for one-third of inpatient hospital costs and 20 percent of all deaths in the United States each year, and cause or contribute to more than 100 other conditions requiring medical care, as well as vehicular crashes, other fatal and non-fatal injuries, overdose deaths, suicides, homicides, domestic discord, the highest incarceration rate in the world and many other costly social consequences. The economic cost to society is greater than the cost of diabetes and all cancers combined. Despite these startling statistics on the prevalence and costs of addiction, few physicians have been trained to prevent or treat it. - ^ a b c Volkow N (31 March 2016). "A Major Step Forward for Addiction Medicine". National Institute on Drug Abuse. National Institutes of Health. Archived from the original on 5 April 2016. Retrieved 3 April 2016.
Only about 10 percent of the 21 million Americans who meet the need for care for an alcohol or drug use disorder receive any form of treatment, and much of the treatment available does not meet standards for evidence-based care. There are many attitudinal and systemic reasons for this treatment gap, including stigma against treating people with addictions and institutional barriers to providing or funding addiction treatment. ... A major milestone was reached on March 14, 2016, when the American Board of Medical Specialties (ABMS) formally announced recognition of the field of Addiction Medicine as a medical subspecialty. ... In a statement issued to mark this milestone, ABAM President Robert J. Sokol summed up its significance: 'This landmark event, more than any other, recognizes addiction as a preventable and treatable disease, helping to shed the stigma that has long plagued it. It sends a strong message to the public that American medicine is committed to providing expert care for this disease and services designed to prevent the risky substance use that precedes it.'
- ^ Gramlich J (26 October 2017). "Nearly half of Americans have a family member or close friend who's been addicted to drugs". Pew Research Center. Retrieved 14 January 2018.
- ^ "We were addicted to their pill, but they were addicted to the money". The Washington Post. Retrieved 22 July 2019.
- ^ Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, et al. (December 2015). "Prevalence of Marijuana Use Disorders in the United States Between 2001–2002 and 2012–2013". JAMA Psychiatry. 72 (12): 1235–1242. doi:10.1001/jamapsychiatry.2015.1858. PMC 5037576. PMID 26502112.
- ^ a b c d "Mental and substance use disorders in Canada". Statistics Canada. Government of Canada. 18 September 2013. Retrieved 8 November 2022.
- ^ "Drug addiction (substance use disorder) – Symptoms and causes". Mayo Clinic. Retrieved 8 November 2022.
- ^ a b "Mental Health and Addictions System Performance in Ontario: 2021 Scorecard". www.ices.on.ca. Retrieved 8 November 2022.
- ^ World Drug Report 2012 (PDF). United Nations Office on Drugs and Crime. June 2012. ISBN 978-92-1-148267-6.
- ^ Pacurucu-Castillo SF, Ordóñez-Mancheno JM, Hernández-Cruz A, Alarcón RD (April 2019). "World opioid and substance use epidemic: a Latin American perspective". Psychiatric Research and Clinical Practice. 1 (1): 32–8. doi:10.1176/appi.prcp.20180009. PMC 9175731. PMID 36101564.
- ^ Alexander, B. K., & Schweighofer, A. R. (1988). Defining" addiction.". Canadian psychology/psychologie canadienne, 29(2), 151.
- ^ a b Steverson (2020). Addiction reimagined: challenging views of an enduring social problem. Vernon Press. p. 206. ISBN 978-1-62273-953-0.
- ^ Gowing L, Ali R, Allsop S, Marsden J, Turf E, West E, et al. (2015). "Global statistics on addictive behaviours: 2014 status report" (PDF). Addiction. 110 (6): 904–919. doi:10.1111/add.12899. PMID 25963869.
- ^ Gilley (2018). "The new science of attention deficit hyperactivity disorder: news from the cutting edge of research science". Journal of Psychiatry and Psychiatric Disorders. 2 (3). doi:10.26502/jppd.2572-519X0043 (inactive 1 July 2025). S2CID 150196703.
{{cite journal}}: CS1 maint: DOI inactive as of July 2025 (link) - ^ Lee C, Ko A, Yang F (2018). "Association of DSM-5 betel-quid use disorder with oral potentially malignant disorder in 6 betel-quid endemic Asian populations". JAMA Psychiatry. 75 (3): 261–269. doi:10.1001/jamapsychiatry.2017.4307. PMC 5885949. PMID 29417149.
- ^ a b Sahithya B, Kashyap R (2020). "Sexual Addiction Disorder—a review with recent updates". Journal of Psychosexual Health. 4 (2): 95–101. doi:10.1177/26318318221081080. S2CID 248835855.
- ^ Destoop M, Morrens M, Coppens V, Dom G (2019). "Addiction, anhedonia, and comorbid mood disorder. A narrative review". Frontiers in Psychiatry. 10 311. doi:10.3389/fpsyt.2019.00311. PMC 6538808. PMID 31178763.
- ^ Crocq MA (December 2007). Thibaut F (ed.). "Historical and cultural aspects of man's relationship with addictive drugs". Dialogues in Clinical Neuroscience. 9 (4). Laboratoires Servier: 355–361. doi:10.31887/DCNS.2007.9.4/macrocq. OCLC 62869913. PMC 3202501. PMID 18286796. S2CID 12682928.
- ^ a b c Lemon R (2018). "Introduction: Addiction in (Early) Modernity". Addiction and Devotion in Early Modern England. Haney Foundation Series. Philadelphia: University of Pennsylvania Press. pp. 1–23. ISBN 978-0-8122-4996-5.
- ^ a b Rosenthal R, Faris S (February 2019). "The etymology and early history of 'addiction'". Addiction Research & Theory. 27 (5). Taylor & Francis: 437–449. doi:10.1080/16066359.2018.1543412. ISSN 1476-7392. S2CID 150418396.
- ^ "Alcohol". Online Etymology Dictionary.
- ^ Institute of Medicine (1996). Pathways of Addiction: Opportunities in Drug Abuse Research. Washington: National Academies Press.
- ^ Bettinardi-Angres K, Angres DH (July 2010). Alexander M (ed.). "Understanding the Disease of Addiction". Journal of Nursing Regulation. 1 (2). Elsevier on behalf of the National Council of State Boards of Nursing: 31–37. doi:10.1016/S2155-8256(15)30348-3. ISSN 2155-8256. S2CID 143289528.
- ^ Appel PW, Ellison AA, Jansky HK, Oldak R (2004). "Barriers to enrollment in drug abuse treatment and suggestions for reducing them: opinions of drug injecting street outreach clients and other system stakeholders". The American Journal of Drug and Alcohol Abuse. 30 (1): 129–153. doi:10.1081/ada-120029870. PMID 15083558. S2CID 20193011.
- ^ Megranahan K, Lynskey MT (February 2018). "Do creative arts therapies reduce substance misuse? A systematic review". The Arts in Psychotherapy. 57: 50–58. doi:10.1016/j.aip.2017.10.005. ISSN 0197-4556.
- ^ Moore RW, W (1 December 1983). "Art therapy with substance abusers: A review of the literature". The Arts in Psychotherapy. 10 (4): 251–260. doi:10.1016/0197-4556(83)90026-6. ISSN 0197-4556.
- ^ North American Drama Therapy Association (2016), Drama therapy with addictions populations
- ^ Waller D, Mahony J, eds. (9 December 1998). Treatment of Addiction: Current Issues for Arts Therapists. Routledge. doi:10.4324/9780203132395. ISBN 978-0-203-13239-5.
- ^ Kaufman GH (1 July 1981). "Art therapy with the addicted". Journal of Psychoactive Drugs. 13 (4). Taylor & Francis: 353–360. doi:10.1080/02791072.1981.10471892. PMID 7040619.
- ^ Waller D, Mahony J, eds. (9 December 1998). Treatment of Addiction: Current Issues for Arts Therapists. Routledge. doi:10.4324/9780203132395. ISBN 978-0-203-13239-5.
- ^ a b c d e f g Schmanke L (2015). "Art Therapy and Substance Abuse". The Wiley Handbook of Art Therapy. John Wiley & Sons, Ltd. pp. 361–374. doi:10.1002/9781118306543.ch35. ISBN 978-1-118-30654-3.
- ^ a b c Schmanke L (2019). "Art Therapy Applications and Substance Abuse". Art and Expressive Therapies within the Medical Model (1st ed.). Routledge. pp. 177–187. doi:10.4324/9780429400087-16. ISBN 978-0-367-02340-9. S2CID 208386296.
- ^ Chiang M, Reid-Varley WB, Fan X (May 2019). "Creative art therapy for mental illness". Psychiatry Research. 275: 129–136. doi:10.1016/j.psychres.2019.03.025. PMID 30901671. S2CID 78090920.
- ^ Dickson C (June 2007). "An evaluation study of art therapy provision in a residential Addiction Treatment Programme (ATP)". International Journal of Art Therapy. 12 (1): 17–27. doi:10.1080/17454830701265220. ISSN 1745-4832. S2CID 72987664.
- ^ Matto H, Corcoran J, Fassler, A (January 2003). "Integrating solution-focused and art therapies for substance abuse treatment: guidelines for practice". The Arts in Psychotherapy. 30 (5): 265–272. doi:10.1016/j.aip.2003.08.003. ISSN 0197-4556.
- ^ a b Megranahan K, Lynskey MT (February 2018). "Do creative arts therapies reduce substance misuse? A systematic review". The Arts in Psychotherapy. 57: 50–58. doi:10.1016/j.aip.2017.10.005. ISSN 0197-4556.
- ^ a b c Rockwell P, Dunham M (January 2006). "The Utility of the Formal Elements Art Therapy Scale in Assessment for Substance Use Disorder". Art Therapy. 23 (3): 104–111. doi:10.1080/07421656.2006.10129625. ISSN 0742-1656. S2CID 5541133.
- ^ Francis D, Kaiser D, Deaver SP (22 April 2011). "Representations of Attachment Security in the Bird's Nest Drawings of Clients with Substance Abuse Disorders". Art Therapy. 20 (3). Routledge: 125–137. doi:10.1080/07421656.2003.10129571. ISSN 0742-1656. S2CID 142341708. Retrieved 4 December 2022.
- ^ Ball SA, Legow NE (November 1996). "Attachment theory as a working model for the therapist transitioning from early to later recovery substance abuse treatment". The American Journal of Drug and Alcohol Abuse. 22 (4). Taylor & Francis: 533–547. doi:10.3109/00952999609001679. PMID 8911591.
- ^ a b Holt ES, Kaiser DH (January 2001). "Indicators of Familial Alcoholism in Children's Kinetic Family Drawings". Art Therapy. 18 (2): 89–95. doi:10.1080/07421656.2001.10129751. ISSN 0742-1656. S2CID 141669979.
- ^ Ashford RD, Brown AM, Curtis B (August 2018). "Systemic barriers in substance use disorder treatment: A prospective qualitative study of professionals in the field". Drug and Alcohol Dependence. 189: 62–69. doi:10.1016/j.drugalcdep.2018.04.033. PMID 29883870. S2CID 47011510.
- ^ Barry CL, McGinty EE, Pescosolido BA, Goldman HH (October 2014). "Stigma, discrimination, treatment effectiveness, and policy: public views about drug addiction and mental illness". Psychiatric Services. 65 (10): 1269–1272. doi:10.1176/appi.ps.201400140. PMC 4285770. PMID 25270497.
- ^ Feldman N (2020), Philly Council bill to block supervised injection sites advances - WHYY, retrieved 14 December 2022
- ^ Drug Enforcement Administration (2018), Implementation of the Provision of the Comprehensive Addiction and Recovery Act of 2016 Relating to the Dispensing of Narcotic Drugs for Opioid Use Disorder, retrieved 14 December 2022
- ^ Sattler, S., Escande, A., Racine, É., Göritz, A. (2017): Public Stigma towards People with Drug Addiction: A Factorial Survey. Journal of Studies on Alcohol and Drugs 78: 415-425. doi:10.15288/jsad.2017.78.415
- ^ Reichert, J., Martins, K. F., Taylor, B., & del Pozo, B. (2023). Police Knowledge, Attitudes, and Beliefs About Opioid Addiction Treatment and Harm Reduction: A Survey of Illinois Officers. Journal of Drug Issues, 55(2), 239-259. https://doi.org/10.1177/00220426231212567
- ^ Whipple, C. R., Kaynak, Ö., Kruis, N. E., D. Silesky, M., Bonnevie, E., Smyser, J., … Kensinger, W. S. (2024). Challenging public stigma: the impact of a statewide social media campaign to reduce opioid use disorder stigma. Drugs: Education, Prevention and Policy, 1–10. https://doi.org/10.1080/09687637.2024.2416583
- ^ Sattler, S., Zolala, F., Baneshi, R., Ghasemi, J., Amirzadeh, S. (2021): Public Stigma towards Female and Male Opioid and Heroin Users. An Experimental Test of Attribution Theory and the Familiarity Hypothesis. Frontiers in Public Health 9: 652876. doi.org/10.3389/fpubh.2021.652876.
- ^ a b c Henningfield JE, Dowell ML, Santora PB (2010). Addiction and art. Baltimore: Johns Hopkins University Press. ISBN 978-1-4214-0023-5. OCLC 794700340.
- ^ a b Dingman DA, Zibalese-Crawford, M (April 2021). "Reducing Substance Use Related Stigma through Expressions of Artwork". Journal of Alcohol & Drug Education. 65 (1). American Alcohol & Drug Information Foundation: 29–39. ISSN 0090-1482.
- ^ Skelly J (2015). "Alternative Paths: Mapping Addiction in Contemporary Art by Landon Mackenzie, Rebecca Belmore, Manasie Akpaliapik, and Ron Noganosh". Journal of Canadian Studies. 49 (2). University of Toronto Press: 268–295, 356. doi:10.3138/jcs.49.2.268. ISSN 0021-9495. S2CID 148421461.
- ^ a b Paivinen H, Bade S (June 2008). "Voice: challenging the stigma of addiction; a nursing perspective". The International Journal on Drug Policy. 19 (3): 214–219. doi:10.1016/j.drugpo.2008.02.011. PMID 18439812.
- ^ Rau BL (September 2014). "The Oxford Handbook of Evidence-Based Management, Rousseau DM 2012. 432 pages, hardcover. New York, NY: Oxford University Press". Academy of Management Learning & Education. 13 (3): 485–487. doi:10.5465/amle.2013.0309. ISSN 1537-260X.
- ^ Daley DC (December 2013). "Family and social aspects of substance use disorders and treatment". Journal of Food and Drug Analysis. 21 (4): S73 – S76. doi:10.1016/j.jfda.2013.09.038. PMC 4158844. PMID 25214748.
- ^ Saad M, de Medeiros R, Mosini AC (October 2017). "Are We Ready for a True Biopsychosocial-Spiritual Model? The Many Meanings of "Spiritual"". Medicines. 4 (4): 79. doi:10.3390/medicines4040079. PMC 5750603. PMID 29088101.
- ^ Farmer P, Kleinman A, Kim J, Basilico M, eds. (31 December 2019). Reimagining Global Health: An Introduction. University of California Press. doi:10.1525/9780520954632. ISBN 978-0-520-95463-2. S2CID 168489288.
- ^ Weakland JH (October 1961). "The Essence of Anthropological Education". American Anthropologist. 63 (5): 1094–1097. doi:10.1525/aa.1961.63.5.02a00130. ISSN 0002-7294.
- ^ Bourgois P (23 December 2002). In Search of Respect: Selling Crack in El Barrio. Structural Analysis in the Social Sciences (2 ed.). Cambridge University Press. doi:10.1017/cbo9780511808562. ISBN 978-0-521-01711-4.
- ^ a b c d e f g h i j k l m n o p Singer M (October 2012). "Anthropology and addiction: an historical review". Addiction. 107 (10): 1747–1755. doi:10.1111/j.1360-0443.2012.03879.x. PMID 22962955.
- ^ a b c d Heath DB (September 1958). "Drinking patterns of the Bolivian Camba". Quarterly Journal of Studies on Alcohol. 19 (3): 491–508. doi:10.15288/qjsa.1958.19.491. PMID 13579177.
- ^ Heath DB (January 1995). "Changes in Drinking Patterns in Bolivian Cultures: A Cautionary Tale About Historical Approaches". Addiction Research. 2 (3): 307–318. doi:10.3109/16066359509005215. ISSN 1058-6989.
- ^ Burraway J (October 2020). "Addiction". In Stein F, Diemberger H, Stasch R, Robbins J, Sanchez A, Lazar S, Candea M (eds.). Open Encyclopedia of Anthropology. doi:10.29164/20addiction. S2CID 241689890.
- ^ Preble E, Casey JJ (January 1969). "Taking Care of Business—The Heroin User's Life on the Street". International Journal of the Addictions. 4 (1): 1–24. doi:10.3109/10826086909061998. ISSN 0020-773X.
- ^ a b Golub A, Johnson BD, Dunlap E (May 2005). "Subcultural evolution and illicit drug use". Addiction Research & Theory. 13 (3): 217–229. doi:10.1080/16066350500053497. PMC 3690817. PMID 23805068.
- ^ Falk, Richard; Kim, Samuel S. (2019-08-15). The War System: An Interdisciplinary Approach. Routledge. ISBN 978-1-000-23507-4
- ^ "Bandura, Albert: Social Learning Theory", Encyclopedia of Criminological Theory, 2455 Teller Road, Thousand Oaks California 91320 United States: SAGE Publications, Inc., 2010, retrieved 2023-11-09
- ^ Smith, Mark A. (2021-02-01). "Social Learning and Addiction". Behavioural Brain Research. 398: 112954. doi:10.1016/j.bbr.2020.112954 ISSN 0166-4328
- ^ Brinthaupt, Thomas M.; Lipka, Richard P. (1994-10-11). Changing the Self: Philosophies, Techniques, and Experiences. State University of New York Press. ISBN 978-0-7914-9754-8
- ^ a b Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 1: Basic Principles of Neuropharmacology". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 4. ISBN 978-0-07-148127-4.
Drug abuse and addiction exact an astoundingly high financial and human toll on society through direct adverse effects, such as lung cancer and hepatic cirrhosis, and indirect adverse effects –for example, accidents and AIDS – on health and productivity.
- ^ "Economic consequences of drug abuse" (PDF). International Narcotics Control Board Report: 2013 (PDF). United Nations – International Narcotics Control Board. 2013. ISBN 978-92-1-148274-4. Retrieved 28 September 2018.
- ^ "Overdose Death Rates". National Institute on Drug Abuse. 9 August 2018. Retrieved 17 September 2018.
- ^ "Overdose Deaths Accelerating During Covid-19". Centers For Disease Control Prevention. 18 December 2020. Retrieved 10 February 2021.
Further reading
[edit]- Pelchat ML (March 2009). "Food Addiction in Humans". The Journal of Nutrition. 139 (3): 620–622. doi:10.3945/jn.108.097816. PMID 19176747.
- Gordon HW (April 2016). "Laterality of Brain Activation for Risk Factors of Addiction". Current Drug Abuse Reviews. 9 (1): 1–18. doi:10.2174/1874473709666151217121309. PMC 4811731. PMID 26674074.
- Szalavitz M (2016). Unbroken Brain. St. Martin's Press. ISBN 978-1-250-05582-8.
- Courtwright DT (2019). The Age of Addiction: How Bad Habits Became Big Business. Cambridge, Massachusetts: Harvard University Press. ISBN 978-0-674-24822-9.
External links
[edit]- "The Science of Addiction: Genetics and the Brain". learn.genetics.utah.edu. Learn.Genetics – University of Utah.
- Why do our brains get addicted? – a TEDMED 2014 talk by Nora Volkow, the director of the National Institute on Drug Abuse at NIH.
Kyoto Encyclopedia of Genes and Genomes (KEGG) signal transduction pathways:
Addiction
View on GrokipediaDefinition and Core Concepts
Signs and Symptoms
Addiction manifests through behavioral, psychological, and physiological signs indicating compulsive engagement with a substance or behavior despite adverse consequences. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), outlines 11 criteria for substance use disorders (SUDs), applicable over a 12-month period, where the presence of two or three symptoms indicates mild severity, four or five moderate, and six or more severe.[10] These criteria emphasize impaired control, social impairment, risky use, and pharmacological indicators.[11] Behavioral signs include using the substance in larger amounts or over longer periods than intended; persistent unsuccessful efforts to reduce or control use; spending excessive time obtaining, using, or recovering from the substance; giving up important social, occupational, or recreational activities; and continuing use despite persistent or recurrent social or interpersonal problems caused or exacerbated by the substance.[12] Recurrent use in hazardous situations, such as driving while intoxicated, and failure to fulfill major role obligations at work, school, or home further characterize behavioral impairment.[13] For behavioral addictions like gambling disorder, analogous signs involve preoccupation with the activity, needing to escalate involvement for satisfaction, unsuccessful attempts to control participation, and risking significant relationships or opportunities due to the behavior.[14] Psychological symptoms encompass strong cravings or urges to use the substance, often triggered by cues, alongside emotional dysregulation such as irritability or anxiety during abstinence attempts.[15] Comorbid mental health issues, including depression and anxiety, frequently co-occur, exacerbating the cycle of use as a maladaptive coping mechanism, though causality varies.[16] Physiological signs primarily involve tolerance, defined as needing markedly increased amounts to achieve the desired effect or diminished effect with continued use, and withdrawal, manifesting as clinically significant distress or impairment upon cessation, such as tremors, sweating, nausea, or seizures depending on the substance.[17] These symptoms underscore physical dependence but are not required for diagnosis, as behavioral criteria suffice in early stages.[10] In severe cases, chronic use leads to observable health deterioration, including weight loss, poor hygiene, and organ damage specific to the substance, like liver cirrhosis from alcohol.[18]Conceptual Models: Disease, Choice, and Hybrids
The disease model of addiction posits that substance use disorders and behavioral addictions constitute a chronic, relapsing brain disease characterized by compulsive engagement despite adverse consequences, driven by neuroadaptations in reward, stress, and self-control circuits.[19] This framework, advanced by the National Institute on Drug Abuse since the 1990s, draws on neuroimaging evidence such as positron emission tomography (PET) scans revealing reduced dopamine receptor availability and metabolic deficits in prefrontal cortex regions among individuals with cocaine dependence compared to controls.[5] Longitudinal studies indicate persistent brain alterations post-abstinence, with recovery rates of 40-60% correlating to partial neuroplasticity rather than full reversal, supporting the view of addiction as a progressive pathology akin to hypertension or diabetes.[6] Proponents argue this model destigmatizes addiction by emphasizing biological causality over moral failing, yet empirical critiques highlight its limitations: it fails to account for high spontaneous remission rates (e.g., 80-90% of heroin users quit within 10 years without formal treatment) and overlooks volitional control evident in controlled use by some addicts.[20] Furthermore, the model has not yielded novel biomarkers or superior treatments beyond existing pharmacotherapies, and some data suggest it may inadvertently reinforce helplessness by implying irreversible impairment.[8] In contrast, the choice model frames addiction as a series of rational or near-rational decisions shaped by behavioral economics principles, where substance use reflects preferences weighted by immediate rewards, delayed costs, and environmental constraints rather than pathological compulsion.[21] Experimental evidence from delay discounting tasks shows that individuals with addiction exhibit steeper devaluation of future outcomes (e.g., preferring $50 today over $100 in a week at rates 2-3 times higher than non-addicts), but this trait is not unique to addiction and responds to incentives like contingency management, where voucher-based rewards increase abstinence rates by 40-60% in cocaine users.[22] Population surveys confirm that drug consumption inversely correlates with access barriers, such as price hikes reducing alcohol intake by 10-20% per 10% cost increase, and many addicts intermittently abstain or moderate use based on situational costs, challenging notions of involuntariness.[23] Critics of this model, often from neurobiological perspectives, contend it underemphasizes heritable vulnerabilities (e.g., twin studies estimating 50% genetic influence on alcoholism liability) and cue-induced cravings that mimic compulsion in animal models.[24] Nonetheless, real-world data on recovery—such as 75% of problem gamblers quitting without intervention—underscore agency, with behavioral interventions leveraging choice architecture (e.g., nudges toward alternatives) outperforming disease-centric approaches in cost-effectiveness.[25] Hybrid models seek to reconcile these views by integrating neurobiological vulnerabilities with decision-making processes, positing that addiction emerges from interactions between predisposing brain changes (e.g., genetic polymorphisms in dopamine genes increasing reward sensitivity) and learned choices amplified by environmental cues.[26] For instance, computational frameworks model addiction as heightened goal-directed choice under negative reinforcement, where stress exacerbates discounting but interventions targeting both neural plasticity (e.g., via cognitive training) and incentives yield synergistic effects, as seen in trials combining naltrexone with behavioral economics yielding 50% higher retention than either alone.[27] These approaches acknowledge empirical dualities: brain imaging reveals sensitization in ventral striatum persisting for months, yet functional recovery aligns with deliberate abstinence choices, with meta-analyses of 50+ studies showing hybrid therapies (e.g., motivational interviewing plus pharmacotherapy) achieving 20-30% better long-term outcomes than unimodal treatments.[28] By avoiding determinism, hybrids align with causal evidence of multifactorial etiology—heritability explains initiation risk but environment and agency drive persistence and remission—offering a pragmatic basis for policy emphasizing prevention through choice-enhancing structures alongside medical support.[29]Classification and Types
Substance Use Disorders
Substance use disorders (SUDs) encompass a range of conditions defined by the recurrent use of alcohol or other drugs that causes clinically significant impairment or distress, as outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).[30] Diagnosis requires the presence of at least two of eleven specified criteria occurring within a 12-month period, including using larger amounts or over longer periods than intended, persistent unsuccessful efforts to reduce or control use, excessive time spent obtaining or recovering from the substance, cravings, failure to fulfill major role obligations, continued use despite social or interpersonal problems, reduction or abandonment of important activities, recurrent use in hazardous situations, tolerance, and withdrawal symptoms.[31] Severity is graded as mild (2-3 criteria), moderate (4-5 criteria), or severe (6 or more criteria), reflecting the intensity of physiological dependence and behavioral disruption.[32] SUDs are classified primarily by the specific substance involved, with distinct diagnostic categories for each major class of psychoactive agents.[33] The DSM-5 recognizes ten classes: alcohol; caffeine; cannabis; phencyclidine and other hallucinogens; inhalants; opioids; sedatives, hypnotics, or anxiolytics; stimulants (including amphetamines and cocaine); tobacco; and other (or unknown) substances.[34] Common examples include alcohol use disorder, characterized by heavy drinking leading to tolerance and withdrawal; opioid use disorder, marked by compulsive use of prescription painkillers or heroin despite risks of overdose; and cannabis use disorder, involving problematic marijuana use interfering with daily functioning.[35] Stimulant use disorders, such as those involving cocaine or methamphetamine, often feature intense euphoria followed by crashes, contributing to cycles of bingeing and withdrawal.[36] In the United States, SUDs are highly prevalent, with the 2023 National Survey on Drug Use and Health indicating that millions of individuals aged 12 and older meet diagnostic criteria, including approximately 27.9 million with alcohol use disorder and 8.9 million with opioid use disorder.[37][38][39] These disorders frequently co-occur with other mental health conditions and exhibit shared neurobiological underpinnings, such as alterations in dopamine-mediated reward pathways, though classification emphasizes behavioral and symptomatic patterns over etiology.[1] Effective identification relies on standardized criteria to differentiate SUDs from mere recreational use or isolated incidents of misuse.[40]Behavioral Addictions
Behavioral addictions, also termed process addictions, refer to compulsive patterns of engagement in non-substance-related rewarding activities that persist despite adverse consequences, mirroring core features of substance use disorders such as impaired control, tolerance, and withdrawal-like symptoms.[41] These conditions activate similar neural reward pathways, particularly involving dopamine release in the mesolimbic system, as evidenced by functional neuroimaging studies showing overlapping hypofrontality and sensitization in the ventral striatum for both behavioral and substance addictions.[42] [43] Empirical support includes longitudinal data indicating persistence over time, with one 5-year study of individuals with behavioral addictions finding remission rates comparable to substance dependencies but highlighting higher relapse risks without intervention.[44] The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published in 2013, formally recognizes gambling disorder as the sole behavioral addiction within its Substance-Related and Addictive Disorders chapter, based on criteria including recurrent engagement leading to distress or impairment, with nine diagnostic thresholds out of eleven shared with substance use disorders.[45] Internet gaming disorder is provisionally listed in Section III for further research, requiring endorsement of at least five of nine criteria such as preoccupation, withdrawal symptoms like irritability upon cessation, and jeopardizing relationships or opportunities, with prevalence estimates ranging from 0.3% to 1.0% in general populations and up to 3.3% in meta-analyses, higher among males (8.5%) than females (3.5%).[46] [47] Gambling disorder prevalence varies by context, with systematic reviews reporting 2.7% to 11.1% problematic gambling among online gamblers as of 2024 data.[48] Other proposed behavioral addictions, such as compulsive sexual behavior or excessive shopping, lack formal DSM-5 classification due to insufficient empirical validation distinguishing them from impulse-control disorders, though shared neurobiological markers like altered serotonin and dopamine signaling suggest partial overlap.[49] Biochemical and genetic studies reinforce similarities, including reduced monoamine oxidase B activity in platelets akin to substance users, but critics argue that behavioral variants often reflect volitional failures or environmental reinforcements rather than inexorable disease progression, as physical dependence is absent and remission can occur without specialized treatment in milder cases.[50] [49] Treatment approaches, including cognitive-behavioral therapy and opioid antagonists like naltrexone, show modest efficacy for gambling and gaming, with response rates of 40-60% in randomized trials, underscoring causal roles for disrupted prefrontal inhibition over purely hedonic pursuit.[51]Overlaps with Compulsive Behaviors
Addiction and compulsive behaviors exhibit significant overlaps, particularly in their manifestation as repetitive actions performed despite adverse consequences, with compulsivity recognized as a core transdiagnostic dimension linking substance use disorders, behavioral addictions, and conditions like obsessive-compulsive disorder (OCD).[52] [53] Empirical studies highlight that both involve impaired inhibitory control and habit formation, often measured through dimensional phenotypes of impulsivity and compulsivity that predict vulnerability across these domains.[54] For instance, individuals with addictive behaviors frequently display elevated compulsivity scores on validated scales, akin to those in OCD, suggesting shared underlying mechanisms rather than categorical distinctions.[50] Neurobiologically, overlaps center on dysfunction in reward-processing circuitry, including attenuated dopamine release in the ventral striatum and orbitofrontal cortex, which impairs the integration of punishment signals with ongoing behavior in both addiction and OCD compulsions.[55] Functional imaging studies demonstrate that compulsive drug-seeking in addiction mirrors the inflexible repetition in OCD, with both linked to hyperactivity in cortico-striatal-thalamo-cortical loops that prioritize habit over flexible goal-directed action.[56] However, addiction compulsions often retain a stronger goal-directed component driven by negative reinforcement (e.g., relief from withdrawal), contrasting with OCD's primary motivation of anxiety reduction, though recent evidence indicates reward-driven elements in OCD compulsions as well.[52] [23] Clinically, these overlaps manifest in high comorbidity rates; for example, OCD patients show elevated risks for substance use disorders, with shared genetic and environmental factors contributing to co-occurring repetitive behaviors.[57] [58] Compulsive traits, such as persistence in maladaptive habits, may predispose individuals to addiction escalation, as evidenced by longitudinal studies tracking trait compulsivity as a predictor of transition from voluntary use to inflexible patterns.[59] Yet, debates persist on the primacy of compulsion in addiction: while habit theories posit a shift to stimulus-response driven actions, empirical data from decision-making tasks reveal that even severe addiction involves deliberate choice under distress, challenging pure compulsivity models.[60] [21] Distinctions arise in motivational substrates and neurochemical profiles; addiction compulsions are frequently tied to mesolimbic dopamine sensitization from repeated exposure, whereas OCD involves broader serotonergic dysregulation, though convergent frontal-striatal hypoactivation underscores partial overlap.[52] Treatment implications include targeting shared compulsivity via cognitive-behavioral interventions that enhance inhibitory control, with evidence from randomized trials showing efficacy for both domains through exposure-response prevention adapted for addictive cues.[53] This dimensional approach supports viewing compulsivity not as addiction's defining feature but as a modifiable overlap facilitating integrated therapeutic strategies.[61]Neurobiological Foundations
Reward Circuitry and Neurotransmitters
The brain's reward circuitry, centered on the mesolimbic dopamine pathway, processes natural reinforcers such as food and social interaction by releasing dopamine from neurons in the ventral tegmental area (VTA) to the nucleus accumbens (NAc) and prefrontal cortex.[62] This pathway mediates incentive salience and motivation, with phasic dopamine bursts signaling reward prediction errors to reinforce behaviors.[63] Addictive substances hijack this system by acutely elevating dopamine levels in the NAc, far exceeding natural rewards, which fosters compulsive drug-seeking through enhanced reinforcement learning.[64] Chronic exposure leads to neuroadaptations, including reduced dopamine receptor density and blunted responses to non-drug rewards, contributing to anhedonia and dependence; these include durable alterations in brain structure, particularly in prefrontal and limbic regions, impairing executive functions such as memory, decision-making, and impulse control.[65][13] Dopamine's primary role involves D1 and D2 receptor subtypes in the striatum, where overstimulation drives sensitization of reward signals and habit formation via direct and indirect pathways.[66] Positron emission tomography (PET) studies reveal decreased dopamine transporter availability and receptor binding in addicts, correlating with prolonged abstinence and relapse vulnerability.[65] Beyond dopamine, glutamate from cortical inputs to the NAc facilitates synaptic plasticity, strengthening drug-associated cues through long-term potentiation (LTP), a process amplified in addiction.[67] GABAergic interneurons in the VTA modulate dopamine neuron firing, with drug-induced disinhibition enhancing burst activity.[68] Endogenous opioids interact with dopamine systems to amplify hedonic "liking," particularly via mu-opioid receptors in the NAc shell, while serotonin influences impulse control and mood regulation in addiction trajectories.[69] Norepinephrine contributes to arousal and stress responses that exacerbate craving.[68] At the molecular level, repeated drug exposure induces accumulation of ΔFosB, a stable transcription factor in the NAc, which alters gene expression to promote dendritic spine growth and behavioral sensitization, persisting weeks after cessation and serving as a molecular switch for addiction vulnerability.[70] This ΔFosB-mediated plasticity underscores causal mechanisms linking acute reward to chronic compulsion across substances.[71]Sensitization, Tolerance, and Dependence
Tolerance refers to a progressive decrease in a drug's effect following repeated administration, necessitating higher doses to achieve the initial response.[72] This phenomenon arises through cellular and molecular adaptations, including receptor desensitization, downregulation of neurotransmitter receptors (e.g., opioid receptor internalization in chronic opioid use), and enhanced drug metabolism.[73] In substance use disorders, tolerance primarily affects rewarding effects like euphoria, contributing to dose escalation and heightened overdose risk, as seen in opioid tolerance where mu-opioid receptor signaling diminishes via G-protein uncoupling.[74] Physical dependence manifests as physiological adaptations to chronic drug exposure, resulting in withdrawal symptoms upon abrupt cessation or dose reduction, often severe and contributing to the chronic, relapsing nature of addiction as a brain disease.[75][13] These adaptations include homeostatic changes in neurotransmitter systems, such as upregulated cAMP signaling in opioid dependence, which drives negative reinforcement to alleviate dysphoric states like anxiety or pain during withdrawal; such neuroadaptations also heighten the risk of comorbid mental disorders, including depression, anxiety, and psychosis.[76][77] Dependence differs from addiction, as it can occur without compulsive use, but in addiction contexts, withdrawal aversion sustains drug-seeking behavior, particularly in substances like alcohol and benzodiazepines where GABAergic adaptations predominate.[78] Sensitization, conversely, involves augmented behavioral responses to drugs or drug-associated cues over time, often termed reverse tolerance.[79] This is mediated by neuroplasticity in the mesolimbic dopamine pathway, where repeated psychostimulant exposure hypersensitizes dopamine release in the nucleus accumbens, enhancing incentive salience—attributing motivational value to drug cues and promoting craving and relapse.[80] A key molecular driver is the transcription factor ΔFosB, which accumulates in the nucleus accumbens following chronic drug use due to its stability and resistance to degradation, upregulating genes that amplify sensitivity to rewards and diminish sensitivity to natural reinforcers.[81] [82] Experimental overexpression of ΔFosB in rodents increases cocaine self-administration and conditioned place preference, underscoring its causal role in sensitized drug-seeking.[83] These processes coexist paradoxically in addiction: tolerance to acute pharmacological effects co-occurs with sensitization to motivational cues, while dependence enforces continued use via withdrawal avoidance, collectively perpetuating the cycle of compulsive consumption and high relapse risk in this chronic disorder.[84] Neuroimaging evidence confirms altered striatal dopamine signaling in dependent individuals, with sensitized responses correlating to cue-reactivity and poor treatment outcomes.[66]Genetic and Epigenetic Influences
Twin and family studies estimate the heritability of substance use disorders (SUDs) at 30-80%, with many converging on 40-60% of variance attributable to genetic factors across substances like alcohol, nicotine, and opioids.[85] For alcohol use disorder specifically, twin studies report heritability around 50%.[86] Genome-wide association studies (GWAS) have identified polygenic contributions, with risk variants mapping to over 60 genes, including DRD2 encoding the dopamine D2 receptor, alongside loci involved in neurotransmitter signaling and neurodevelopment.[86] Candidate gene approaches highlight polymorphisms such as the A1 allele of DRD2 (Taq1A), which reduces receptor density and is associated with heightened reward sensitivity and increased risk for addiction to alcohol, cocaine, and opioids in multiple cohorts.[88] Variants in COMT, which regulates dopamine catabolism via catechol-O-methyltransferase, influence prefrontal cortex function and have been linked to impulsive traits and vulnerability to substances like methamphetamine and alcohol.[89] These associations underscore how genetic variations in reward circuitry genes can predispose individuals to dysregulated reinforcement learning, though effect sizes are modest and require environmental triggers for phenotypic expression. Epigenetic modifications, including DNA methylation, histone acetylation/methylation, and non-coding RNA activity, enable drug-induced changes in gene expression without altering DNA sequence, facilitating persistent neuroadaptations in addiction.[90][91] Chronic exposure to psychostimulants or opioids often hypermethylates promoters of dopamine-related genes like Drd2 in the nucleus accumbens, suppressing expression and contributing to tolerance and craving.[92] Histone modifications, such as increased H3K9 acetylation, enhance transcription of plasticity genes in reward pathways, while reduced methylation promotes maladaptive synaptic strengthening. The transcription factor ΔFosB exemplifies epigenetic persistence: repeated drug administration induces its accumulation in striatal neurons, where its stability (half-life >8 weeks) drives downstream gene programs for hypersensitivity to rewards and relapse propensity, even after abstinence.[81] This mechanism integrates genetic predisposition with experiential inputs, as early-life stress or drug history can prime epigenetic marks that amplify later vulnerability, highlighting causal interplay between inherited traits and modifiable chromatin states in addiction trajectories.[93]Etiology and Risk Factors
Heritability and Genetic Vulnerabilities
Heritability estimates for substance use disorders, derived from twin, family, and adoption studies, typically range from 40% to 60%, indicating that genetic factors account for a substantial portion of vulnerability while environmental influences explain the remainder.[85] For alcohol use disorder specifically, meta-analyses of twin and adoption data report heritability around 50%, with similar figures for other substances like tobacco (up to 70%) and opioids.[94] [95] These estimates arise from comparisons of concordance rates in monozygotic versus dizygotic twins, where shared genetics amplify risk, though shared environments can confound results if not modeled appropriately. Behavioral addictions, such as gambling disorder, show comparable heritability (around 50%), suggesting overlapping genetic liabilities across addictive phenotypes.[85] Genome-wide association studies (GWAS) reveal that addiction vulnerability is polygenic, involving thousands of common variants with small effect sizes rather than rare high-impact mutations. A unitary "addiction risk factor" has been identified through multivariate analyses, representing a shared genetic predisposition across substances like alcohol, cannabis, opioids, and tobacco, distinct from substance-specific loci.[96] Polygenic risk scores (PRS) derived from these GWAS predict not only disorder onset but also progression milestones, such as earlier initiation of use or escalation to dependence, explaining up to 5-10% of variance in European-ancestry cohorts.[97] Key implicated pathways include dopaminergic reward signaling (e.g., variants near DRD2 and CHRNA5 genes), glutamatergic neurotransmission, and stress-response systems like the HPA axis, which modulate impulsivity and reinforcement sensitivity.[98] Genetic vulnerabilities interact with environmental triggers, amplifying risk in carriers of high PRS who face adversity, though main effects persist independently. Adoption studies disentangle these by showing elevated risk in biological relatives of affected individuals raised in non-affected homes, underscoring causal genetic roles over purely cultural transmission. Limited evidence suggests ancestry-specific effects, with PRS performance varying across populations due to linkage disequilibrium differences, necessitating diverse genomic data for broader applicability.[99] Overall, while no single gene confers determinism, cumulative polygenic burden objectively elevates susceptibility, informing precision prevention without negating individual agency in modifiable environments.[96]Environmental and Developmental Contributors
Environmental exposures during critical developmental periods can elevate the risk of addiction later in life, though outcomes depend on interactions with genetic predispositions and protective factors. Prenatal exposure to maternal substance use, for instance, has been associated with heightened vulnerability to substance use disorders in offspring; a 2024 study found that prenatal alcohol exposure alters reward processing pathways, increasing the likelihood of drug addiction in exposed individuals. Similarly, prenatal illicit drug exposure correlates with elevated risks of neurodevelopmental impairments that may predispose to addiction, including attention-deficit/hyperactivity disorder and other conditions linked to impulsivity.[100][101] Adverse childhood experiences (ACEs), such as abuse, neglect, household dysfunction, or witnessing violence, exhibit a dose-response relationship with subsequent substance use disorders. Individuals with four or more ACEs face up to 12 times the risk of alcoholism and seven times the risk of illicit drug use compared to those with none, according to longitudinal data from the CDC's ACE Study and subsequent analyses. These effects persist into adulthood even after controlling for socioeconomic status and other confounders, with specific patterns like childhood maltreatment showing stronger links to illicit drug disorders in males. Family environments marked by parental substance use further compound this risk; children of parents with substance use disorders are two to four times more likely to develop similar issues, mediated by modeling, genetic transmission, and disrupted caregiving.[102][103][104] Adolescence represents a particularly sensitive developmental window for addiction vulnerability due to ongoing maturation of the brain's reward circuitry, including heightened dopamine sensitivity and prefrontal cortex underdevelopment, which amplify impulsivity and reward-seeking. Initiation of substance use during this period—often influenced by peer pressure, availability, and social norms—dramatically increases the odds of progression to dependence; for example, early adolescent drug exposure triples the lifetime risk of addiction compared to adult onset. Peer groups and neighborhood disadvantage, such as high-crime areas with easy substance access, independently predict initiation and escalation, with studies showing that adolescents in disordered environments report 1.5 to 2 times higher rates of heavy use.[105][106][107] Socioeconomic factors like poverty and low educational attainment also contribute, correlating with 36% higher odds of substance abuse among those below the federal poverty line, potentially through chronic stress, limited access to resources, and co-occurring adversities. However, affluent environments can foster certain risks, such as increased alcohol and marijuana use among high-SES youth due to permissive norms and availability. These environmental contributors underscore the importance of early interventions targeting modifiable risks, though empirical evidence emphasizes their probabilistic rather than deterministic nature.[108][109]Comorbid Psychiatric Conditions
Individuals with substance use disorders exhibit markedly elevated rates of comorbid psychiatric conditions, with lifetime prevalence estimates indicating that over 50% of those seeking treatment for addiction also meet criteria for at least one other mental disorder.[110] Among specific populations, such as those with opioid use disorder, the current prevalence of any non-opioid substance use disorder comorbidity reaches 59.5%, often alongside psychiatric issues like mood and anxiety disorders.[111] These co-occurrences extend to behavioral addictions, where meta-analyses reveal significant associations with conditions such as depression, anxiety, ADHD, and alcohol abuse in cases of internet addiction.[112] Mood disorders, particularly major depressive disorder and bipolar disorder, represent the most prevalent psychiatric comorbidities in addiction. In treatment-seeking individuals with drug use disorders (excluding alcohol), approximately 26% concurrently experience mood disorders, with bipolar disorder appearing in 16% of substance dependence cases.[110][113] Longitudinal evidence supports a bidirectional relationship, wherein alcohol use disorder doubles the risk of subsequent major depressive disorder, and vice versa, suggesting shared vulnerability factors rather than unidirectional causation in many instances.[114] Anxiety disorders, including generalized anxiety, panic disorder, and post-traumatic stress disorder (PTSD), co-occur at rates of 26% in drug use disorder populations and up to 41% for panic disorder in certain addiction cohorts.[110][115] The self-medication hypothesis posits that individuals may use substances to alleviate anxiety symptoms, yet empirical data from prospective studies indicate reciprocal influences, with anxiety predisposing to addiction initiation and chronic substance use exacerbating anxiety severity.[116] PTSD, in particular, shows strong links, appearing in 4-40% of cases depending on trauma exposure and substance type.[117] Attention-deficit/hyperactivity disorder (ADHD) demonstrates robust comorbidity with addiction, with meta-analyses confirming increased risk of substance use disorders among adolescents with ADHD, oppositional defiant disorder, and conduct disorder.[118] Personality disorders, especially cluster B types like antisocial and borderline, are frequent, contributing to impulsive behaviors that perpetuate addictive cycles.[117] Schizophrenia-spectrum disorders appear in about 11% of substance dependence patients, often complicating differential diagnosis due to substance-induced psychotic symptoms.[113] The bidirectional dynamics challenge simplistic models like primary addiction with secondary psychiatric effects or vice versa; instead, shared neurobiological pathways, such as dysregulated reward and stress systems, underlie many co-occurrences, as evidenced by genetic overlap and environmental triggers amplifying both.[119] Treatment outcomes worsen with untreated comorbidity, underscoring the need for integrated assessments, though causal inference remains limited by confounding factors in observational data.[120]Diagnosis and Assessment
Diagnostic Frameworks
The primary diagnostic frameworks for addiction, encompassing both substance use disorders and certain behavioral addictions, are outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) published by the American Psychiatric Association and the International Classification of Diseases, Eleventh Revision (ICD-11) issued by the World Health Organization.[121][122] In DSM-5-TR, substance use disorders (SUDs) are diagnosed based on a single disorder spectrum replacing prior distinctions between abuse and dependence, requiring at least two of eleven criteria within a 12-month period for a mild diagnosis (2-3 symptoms), escalating to severe (6 or more).[11] These criteria include: substance taken in larger amounts or over longer periods than intended; persistent desire or unsuccessful efforts to cut down or control use; excessive time spent obtaining, using, or recovering from the substance; cravings or strong urges; recurrent use resulting in failure to fulfill major role obligations at work, school, or home; continued use despite persistent social or interpersonal problems caused or exacerbated by the substance; giving up or reducing important social, occupational, or recreational activities due to use; recurrent use in hazardous situations; continued use despite knowledge of physical or psychological problems likely caused or exacerbated by the substance; tolerance, defined as needing markedly increased amounts or diminished effect with continued use; and withdrawal symptoms or using the substance to relieve or avoid them. Severity is graded as mild, moderate, or severe based on symptom count, with specifiers for early/sustained remission or controlled environment; the framework extends to behavioral addictions like gambling disorder, which shares similar criteria adapted to non-substance contexts, such as preoccupation, tolerance, and chasing losses.[11] A novel addition in DSM-5 was the explicit inclusion of craving as a diagnostic criterion, supported by empirical validation across substances like alcohol, tobacco, and opioids, though its standalone predictive value for disorder progression remains debated in longitudinal studies.[123] ICD-11 classifies disorders due to substance use under a unified category emphasizing dependence as the core diagnosis, defined by a strong internal drive to use the substance, impaired control over use (e.g., onset, frequency, quantity, termination despite intent), and physiological features like tolerance or withdrawal, requiring at least two of these three elements over a 12-month period (or shorter if continuous).[124] This simplifies prior ICD-10 criteria by condensing six elements into three paired domains, aiming for greater clinical utility and alignment with neurobiological evidence of dysregulated reward and control circuits.[125] Unlike DSM-5's polysubstance flexibility, ICD-11 mandates substance-specific diagnoses and excludes legal problems as a criterion, focusing instead on functional impairments; it also categorizes gambling and gaming disorders as addictive behaviors outside substance use, requiring similar evidence of impaired control and harm continuation.[126] Diagnostic concordance between DSM-5 and ICD-11 for alcohol and cannabis dependence is high (kappa >0.8 in community samples), though DSM-5 yields slightly higher prevalence due to its broader symptom set.[127] These frameworks prioritize observable behavioral, cognitive, and physiological indicators over subjective self-reports alone, reflecting causal mechanisms like reinforced habit formation and neuroadaptation, but they face criticism for potential overpathologization of non-clinical use patterns and underemphasis on volitional factors in early-stage maladaptive behaviors.[128] Peer-reviewed analyses highlight that while both systems correlate with functional outcomes like treatment need, DSM-5's dimensional approach may better capture severity gradients supported by neuroimaging and genetic data, whereas ICD-11's categorical structure aligns more closely with global public health metrics.[129] Neither framework equates addiction solely to a "brain disease" model without integrating environmental contingencies, and ongoing revisions incorporate evidence from large-scale cohort studies showing variable progression rates influenced by genetic vulnerabilities.[130]Screening Instruments and Tools
Screening instruments for addiction, particularly substance use disorders (SUDs), consist of brief, standardized questionnaires designed to detect risky or problematic use in non-clinical or primary care settings, facilitating referral for further assessment rather than providing a formal diagnosis. These tools typically rely on self-reported behaviors and consequences, with validation against clinical criteria such as those in the DSM-5, though they exhibit varying sensitivity and specificity depending on population and substance.[131][132] The Alcohol Use Disorders Identification Test (AUDIT), developed by the World Health Organization in 1989 and updated as AUDIT-C (a three-item version), screens for hazardous drinking, harmful use, and dependence through 10 questions on consumption, dependence symptoms, and alcohol-related problems, with scores ranging from 0-40; a score of 8 or higher indicates hazardous or harmful use in men, and 4 or higher in women. Validation studies confirm its high internal consistency (Cronbach's alpha ≈0.80-0.90) and criterion validity against DSM criteria, outperforming shorter tools like CAGE for detecting at-risk drinking in primary care, though it may underperform in populations with low prevalence or cultural differences in reporting.[133][134][135] For non-alcohol drugs, the Drug Abuse Screening Test (DAST), available in 10- or 20-item versions since 1982, employs yes/no responses to assess drug-related problems excluding alcohol, with a score of 6 or higher on DAST-10 suggesting substantial issues; it demonstrates good reliability (test-retest r>0.70) and validity in distinguishing drug abusers from non-abusers, correlating with DSM diagnoses, though sensitivity decreases for milder use. The CAGE questionnaire, adapted as CAGE-AID for alcohol and illicit drugs since the 1990s, uses four items (Cut down, Annoyed, Guilty, Eye-opener) to flag dependence, with two or more positive responses indicating potential problems; it offers quick administration but lower sensitivity for hazardous use compared to AUDIT, performing better for severe dependence in validation against structured interviews.[136][137][138] Polysubstance and broader SUD screening incorporates tools like the Screening, Brief Intervention, and Referral to Treatment (SBIRT) framework's Brief Screener for Alcohol, Tobacco, and other Drugs (BSTAD), a five-item tool validated for adolescents and adults to triage risk levels, or the Substance Abuse Subtle Screening Inventory (SASSI-3), which includes subtle validity scales to detect denial, showing high accuracy (AUC>0.90) in clinical samples. DSM-5-aligned checklists, such as the 11-item SUD criteria questionnaire, quantify symptoms like tolerance and withdrawal over the past year for diagnostic severity, with scores of 2-3 indicating mild disorder; these exhibit strong inter-rater reliability but require clinician administration for full assessment. Limitations across tools include reliance on honest self-reporting, potential under-detection in dissimulating individuals, and reduced validity in non-Western or comorbid psychiatric populations, necessitating corroboration with biological markers or collateral reports where feasible.[131][139][140]Prevention Approaches
Biological and Early Intervention Strategies
Biological strategies for addiction prevention emphasize identifying neurobiological and genetic vulnerabilities to enable targeted risk mitigation prior to substance exposure. Advances in genetic testing, such as the Genetic Addiction Risk Score (GARS), assess polymorphisms in dopaminergic genes including DRD2, DRD1, and OPRM1 within the brain reward cascade, yielding a risk score that correlates with addiction severity and predicts vulnerability to reward deficiency syndrome-linked behaviors.[141] Studies indicate a positive predictive value of approximately 74% for the DRD2 A1 variant in forecasting addiction risk, supporting its use in high-risk families to guide personalized prevention plans like enhanced monitoring or pro-dopamine lifestyle modifications.[141] However, these tests are probabilistic, with heritability estimates for substance use disorders ranging from 40-60% across substances, necessitating integration with environmental and behavioral assessments to avoid over-reliance on genetics alone.[142] Pharmacological prophylaxis remains underdeveloped for primary prevention, as current medications like naltrexone or buprenorphine are primarily evidenced for treating established dependence rather than preempting onset in vulnerable individuals.[143] Neurobiological insights, such as altered dopamine signaling and metabolic differences observable via PET imaging, inform research into potential preventive agents but lack robust clinical trial support for routine use in at-risk populations without prior exposure.[143] Early intervention strategies target adolescents and youth with identified risks, such as familial history or early experimentation, through evidence-based programs that address developmental windows of vulnerability. Family-based interventions, endorsed by the Community Preventive Services Task Force based on 60 U.S. studies, significantly reduce substance initiation and use: for instance, cannabis initiation by 36.6%, alcohol use by 33.8%, and prescription drug misuse initiation by 58.1%.[144] These programs, typically for ages 10-14, incorporate components like parental rule-setting, monitoring, and communication skills training, delivered via home visits, group sessions, or digital modules by trained professionals.[144] School- and community-based early interventions, including brief motivational interviewing and skill-training, further bolster prevention by reducing alcohol and illicit drug use in at-risk youth through personalized feedback on risks and coping strategies.[145] Multisystemic therapy, which holistically addresses family, peer, and school factors, has demonstrated reductions in substance use among adolescents with behavioral risks, emphasizing causal pathways like poor parental supervision.[145] When combined with genetic risk profiling, these approaches enable stratified prevention, prioritizing high-vulnerability individuals for intensive support to interrupt progression to dependence.[142]Policy and Education Measures
Fiscal policies, such as excise taxes on tobacco, alcohol, and sugary beverages, have demonstrated effectiveness in reducing consumption levels, with studies showing consistent price elasticity leading to lower use, particularly among youth and price-sensitive populations.[146] [147] For tobacco, a 10% increase in price is associated with a 4-5% reduction in demand, contributing to declines in smoking initiation and prevalence.[148] Similarly, alcohol taxation strategies, including minimum unit pricing, correlate with reduced overall consumption and alcohol-related harms in population-level analyses.[149] Regulatory policies restricting availability and access further support prevention efforts. The minimum legal drinking age (MLDA) of 21 in the United States has been linked to lower rates of youth alcohol consumption, traffic fatalities, and alcohol use disorders, with estimates indicating up to a 13 percentage point reduction in drinking probability among those under 21 compared to lower MLDA jurisdictions.[150] [151] Advertising restrictions and sales bans on substances like tobacco to minors have also contributed to delayed onset of use, as evidenced by longitudinal data from implemented policies.[152] Education measures emphasize school- and community-based programs that build resistance skills, normative beliefs, and decision-making abilities rather than didactic or fear-based approaches. Meta-analyses of universal school-based interventions indicate small but significant reductions in substance initiation, with effect sizes around 0.10-0.20 for alcohol and drug use, particularly when programs are interactive and developmentally timed during transitions like middle school.[153] [154] Examples of evidence-supported curricula include Project Towards No Drug Abuse (TND), which targets high-risk high school students and has shown sustained reductions in tobacco, alcohol, and marijuana use through cognitive-behavioral techniques.[155] In contrast, programs like D.A.R.E., relying on lectures and "just say no" messaging, exhibited no long-term effects on drug use at 10-year follow-ups and minimal impact even short-term.[156] [157] Public awareness campaigns, while less potent standalone, can reinforce education by correcting misperceptions about peer norms and risks, with meta-reviews finding modest effects on intentions to use when integrated with school efforts, though standalone mass media shows limited behavioral change.[158] Comprehensive policies combining fiscal, regulatory, and educational elements yield the strongest outcomes, as seen in community-wide initiatives reducing youth substance use by addressing multiple risk factors.[159] [160]Treatment Modalities
Pharmacotherapies and Their Mechanisms
Pharmacotherapies for addiction primarily target the neurobiological underpinnings of substance use disorders, including dysregulation of dopamine reward pathways, withdrawal symptoms, and cue-induced craving, though efficacy varies by substance class and individual factors. For opioid use disorder (OUD), three FDA-approved medications—methadone, buprenorphine, and naltrexone—demonstrate robust evidence in reducing illicit opioid use, overdose mortality, and transmission of infectious diseases like HIV and hepatitis C. Methadone, a full mu-opioid receptor agonist, occupies receptors to alleviate withdrawal and suppress craving while providing cross-tolerance to other opioids, administered in opioid treatment programs with daily dosing starting at 20-30 mg and titrated to 60-120 mg to minimize diversion risks. Buprenorphine, a partial mu-opioid agonist with high receptor affinity and a ceiling effect on respiratory depression, similarly mitigates withdrawal and euphoria from short-acting opioids, often combined with naloxone (as Suboxone) to deter misuse via injection, with induction doses of 2-4 mg sublingual followed by maintenance at 8-24 mg daily. Naltrexone, a mu-opioid antagonist, blocks euphoric effects of opioids to prevent relapse, available as daily oral (50 mg) or extended-release intramuscular injection (380 mg monthly), requiring detoxification prior to initiation to avoid precipitated withdrawal.[161][162][163] For alcohol use disorder (AUD), pharmacotherapies focus on reducing heavy drinking days and promoting abstinence by modulating glutamate-GABA imbalance or aversive responses. Naltrexone (50 mg oral daily or 380 mg monthly injection) acts as an opioid antagonist to blunt alcohol-induced dopamine release in the nucleus accumbens, decreasing craving and relapse risk by approximately 20-30% in meta-analyses of randomized trials. Acamprosate (666 mg three times daily) stabilizes hyperglutamatergic states post-withdrawal by antagonizing NMDA receptors and modulating calcium channels, sustaining abstinence longer in patients with severe dependence, though evidence is stronger when combined with psychosocial support. Disulfiram (250 mg daily under supervision) inhibits aldehyde dehydrogenase, leading to acetaldehyde accumulation and unpleasant symptoms upon alcohol consumption, serving as an aversive deterrent effective in adherent patients but limited by non-compliance and cardiovascular risks. Emerging agents like topiramate (up to 300 mg daily), which enhances GABA and inhibits glutamate, show promise in reducing drinks per day via off-label use, supported by network meta-analyses.[164][165][166] Nicotine dependence treatments leverage partial agonism or replacement to counteract nicotinic acetylcholine receptor (nAChR) upregulation and withdrawal dysphoria. Nicotine replacement therapies (NRT), including transdermal patches (7-21 mg/day), gum (2-4 mg), or lozenges, deliver controlled nicotine doses to taper dependence, doubling quit rates over placebo in Cochrane reviews by easing withdrawal and allowing behavioral adaptation. Varenicline (1 mg twice daily after titration), a selective partial agonist at α4β2 nAChRs, stimulates dopamine release to alleviate craving while competitively blocking full agonist effects from smoking, yielding 2-3 times higher abstinence rates at 6-12 months compared to NRT or bupropion. Bupropion sustained-release (150 mg twice daily), a norepinephrine-dopamine reuptake inhibitor, attenuates withdrawal irritability and weight gain via antidepressant effects, with efficacy comparable to NRT in diverse populations.[167][168][169] For psychostimulant use disorders like cocaine or methamphetamine dependence, no FDA-approved pharmacotherapies exist as of 2025, with trials of agents such as modafinil, amphetamine-like stimulants, or dopamine modulators showing inconsistent reductions in use or craving, often failing primary endpoints in phase III studies due to heterogeneous neuroadaptations and high placebo responses. Contingency management paired with off-label prescriptions like methylphenidate has demonstrated modest retention benefits in comorbid ADHD cases, but broader evidence underscores the need for novel targets beyond monoamine modulation. Behavioral addictions, such as gambling disorder, lack dedicated approvals but employ opioid antagonists like naltrexone (50 mg daily) to interrupt reward sensitization, with randomized trials indicating reduced urges in subsets of patients, though meta-analyses reveal limited overall efficacy without therapy integration and highlight risks of overgeneralizing substance models to non-pharmacological compulsions.[170][171][172]Psychosocial and Behavioral Interventions
Psychosocial and behavioral interventions encompass a range of non-pharmacological approaches aimed at modifying maladaptive thoughts, behaviors, and social environments to support recovery from substance use disorders (SUDs). These methods emphasize skill-building, motivation enhancement, and contingency reinforcement to foster abstinence or reduced use, often delivered in individual, group, or family formats. Empirical evidence indicates moderate efficacy overall, with effects typically strongest in the short term (1-6 months post-treatment) and varying by substance and intervention type.[173][174] Cognitive behavioral therapy (CBT) targets cognitive distortions and habitual behaviors linked to substance use through structured techniques like functional analysis and coping skills training. A systematic review of meta-analyses found CBT yields small to moderate reductions in substance use compared to inactive controls, with effect sizes diminishing over longer follow-ups beyond 6 months.[175] Another meta-analysis confirmed CBT's efficacy for alcohol and other drug use disorders, producing small-to-moderate improvements in abstinence and use frequency, though outcomes are enhanced when combined with pharmacotherapy.[176] Limitations include high attrition rates and challenges in maintaining gains without ongoing support, as relapse often occurs due to unaddressed environmental cues.[177] Contingency management (CM) employs operant conditioning principles, providing tangible rewards (e.g., vouchers or prizes) contingent on verified abstinence, typically via urine toxicology. This approach demonstrates robust efficacy, particularly for stimulants and opioids, outperforming standard care in promoting sustained abstinence up to one year post-treatment in multiple randomized trials.[178] A review of studies on medication-assisted treatment patients showed CM increased end-of-treatment abstinence in 64% of trials, though long-term effects wane without continued reinforcement due to cost and logistical barriers.[179] Critics note potential ethical concerns over incentivizing behavior, yet evidence supports its causal role in behavior change via positive reinforcement.[180] Motivational interviewing (MI), a client-centered technique to resolve ambivalence and enhance intrinsic motivation, shows short-term benefits in reducing substance use when compared to no intervention.[181] Integrated MI with CBT has been associated with higher abstinence rates through 6 months in group settings for SUD patients.[182] However, effects are modest and primarily preparatory, best suited for engaging treatment-resistant individuals rather than as standalone long-term therapy.[183] Twelve-step facilitation programs, modeled on Alcoholics Anonymous principles, promote abstinence through peer support, spiritual components, and step-based self-examination. A Cochrane meta-analysis of 27 studies found participation linked to increased abstinence days and reduced drinks per occasion for alcohol use disorder, comparable to other behavioral therapies.[184] Effectiveness is attributed to ongoing mutual aid rather than initial facilitation, with attendance predicting better outcomes independently of baseline severity.[185] Evidence is stronger for alcohol than other substances, and self-selection biases in observational data necessitate caution in causal attribution.[186] Behavioral couples therapy (BCT) addresses interpersonal dynamics by involving partners in sessions to improve communication and reduce enabling behaviors. Meta-analytic evidence indicates BCT superior to individual therapies in enhancing relationship satisfaction and abstinence rates, particularly for alcohol and opioid use.[187] Relapse prevention, an extension of CBT focusing on high-risk situations, similarly shows cross-substance efficacy but requires integration with other modalities for durability.[173] Across interventions, real-world implementation faces challenges like access disparities and variable therapist fidelity, underscoring the need for tailored, evidence-monitored application.[174]Abstinence vs. Harm Reduction: Evidence and Critiques
Abstinence-based treatments prioritize complete cessation of substance use as the primary goal, often through programs such as Alcoholics Anonymous (AA), 12-step facilitation (TSF), therapeutic communities (TCs), and contingency management (CM), which reinforce sobriety via behavioral incentives.[188] These approaches assume that sustained abstinence is necessary to disrupt the cycle of addiction and restore normal functioning, drawing on evidence that partial reduction in use often fails to prevent relapse due to neuroadaptations like tolerance and craving.[189] Randomized controlled trials (RCTs) of manualized AA/TSF interventions have demonstrated improved rates of continuous abstinence compared to other clinical treatments, with participants achieving higher percentages of abstinence days over 1-2 years.[188] Long-term residential TCs, particularly for opioid dependence, have shown reductions in drug abuse and antisocial behavior, with effect sizes indicating sustained benefits beyond 12 months for those completing the program.[190] Abstinence pathways are associated with greater overall functioning and well-being, even if not requisite for all, as moderate use often correlates with poorer psychosocial outcomes.[191] Harm reduction strategies, by contrast, focus on minimizing immediate risks such as overdose, infectious disease transmission, and social harms without mandating abstinence, including opioid agonist therapies (OAT) like methadone or buprenorphine, needle-syringe programs, and supervised consumption sites.[192] These interventions have empirical support for short-term outcomes: OAT reduces overdose mortality and opioid-related acute care utilization compared to non-medication treatments or no intervention, with cohort studies showing 50-70% lower overdose rates during treatment.[193] Needle exchange programs decrease HIV and hepatitis C incidence among injectors by 30-50% in evaluated implementations, while safe injection facilities correlate with localized drops in fatal overdoses.[194] Contingency management within harm reduction frameworks yields moderate reductions in substance use (standardized mean difference of -0.47) relative to treatment as usual.[195] Comparative evidence reveals trade-offs, with limited head-to-head meta-analyses showing minimal differences in overall impact between abstinence-based and harm reduction approaches versus standard care in populations like the homeless, though abstinence interventions often edge out in achieving zero use.[196] For opioids, abstinence-based care without maintenance medications carries higher short-term overdose risk due to rapid tolerance loss upon cessation, potentially exceeding risks of untreated states, as evidenced by elevated post-discharge mortality in detox-only programs.[197] Long-term, however, sustained abstinence—achievable in subsets with factors like later onset age and strong social support—links to lower relapse and better quality of life than ongoing substitution, where dropout rates exceed 50% annually and many remain physiologically dependent.[189] Critiques of harm reduction highlight its potential to prolong addiction by normalizing continued use and reducing incentives for full cessation, as substitution therapies may foster indefinite reliance on agonists, with some analyses noting no superior long-term abstinence rates over behavioral abstinence programs.[198] Opponents argue it underemphasizes personal agency and causal drivers like impaired self-control, potentially enabling use under utilitarian pretexts while sidelining evidence that total abstinence better addresses underlying neuropathology.[199] Sources advocating harm reduction, often from public health institutions, may reflect biases favoring incrementalism over rigorous recovery metrics, overlooking data where abstinence-focused care yields durable outcomes in motivated cohorts.[200] Abstinence models face criticism for inaccessibility, as abrupt cessation elevates acute risks and dropout, with success rates under 20% in some outpatient settings without adjunct pharmacotherapy, ignoring heterogeneous addiction severities where initial harm minimization stabilizes patients for later abstinence attempts.[201] Yet, empirical prioritization of abstinence aligns with causal realism, as partial harm mitigation rarely reverses addiction's progressive trajectory without full disruption, supported by longitudinal data favoring zero-use endpoints for sustained remission.[202] Integrated models, blending elements, show promise but require scrutiny of outcome definitions, as "recovery" metrics in harm reduction literature sometimes conflate harm avoidance with true desistance.[203]Epidemiology and Prevalence
Global and Demographic Patterns
In 2023, an estimated 316 million people worldwide aged 15-64 used drugs at least once in the past year, equating to a global prevalence of 5.8% in that age group, with the number of individuals experiencing drug use disorders rising 13% over the prior decade despite population growth.[204] Alcohol contributes substantially to this burden, causing 2.6 million deaths annually or 4.7% of all global deaths, while drug use disorders account for over 600,000 deaths yearly, with total alcohol- and drug-attributable mortality exceeding 3 million, predominantly among males.[205] Regional variations are pronounced: annual cannabis use prevalence reaches 4.5% in the Americas and 3.6% in Oceania, compared to 1.1% in Asia; opioids affect 1.3% in the Near and Middle East/Southwest Asia versus under 0.5% in Africa; and cocaine use is highest at 1.4% in the Americas.[204] Only 8.1% of those with drug use disorders received treatment in 2023, highlighting gaps in global access.[206] Demographic patterns reveal consistent gender disparities, with males exhibiting higher rates of substance involvement across substances and regions; for instance, women are lifetime abstainers from alcohol more frequently than men in all WHO regions, and drug-related deaths skew heavily male.[207] [205] Age trends show peak prevalence of substance use disorders in early adulthood, particularly ages 18-25, where risks for initiation and dependence are elevated due to neurodevelopmental vulnerabilities and social exposures, though disorders persist into later life with male-female gaps narrowing after age 70.[208] Lifetime prevalence of drug use disorders averages 3.5% globally but varies sharply by country, from 0.2% in low-use nations like Iraq to 8.4% in high-prevalence settings like the United States.[209] Behavioral addictions follow similar patterns but with sparser global data. Gambling disorder past-year prevalence ranges from 0.1% to 5.8% among adults, serving as a proxy for problematic gambling, with harms affecting 11.9% of men versus 5.5% of women worldwide; adolescent rates can reach 4-21.9% among online gamblers.[210] [211] Internet gaming disorder affects 0.3-1.0% of the general population, disproportionately impacting adolescents and young males.[46] Racial and ethnic differences, more documented in high-income contexts, indicate elevated adolescent substance risks among Native Americans, multiracial individuals, whites, and Hispanics compared to other groups, influenced by socioeconomic and cultural factors rather than inherent traits.[212] Overall, these patterns underscore causal roles of availability, cultural norms, and biological sex differences in vulnerability, with limited cross-national data on behavioral forms complicating comprehensive estimates.[209]Trends in Specific Substances and Behaviors
Opioid use disorder has seen dramatic increases in overdose mortality driven primarily by synthetic opioids such as fentanyl, with U.S. drug overdose deaths doubling from 16.25 per 100,000 population in 2015 to 32.76 per 100,000 in 2023.[213] Provisional data indicate a 23% decline in total overdose deaths to 80,499 in 2024, attributed to interventions like naloxone distribution and fentanyl test strips, though opioid-involved fatalities remain elevated compared to pre-pandemic levels.[214] [215] Stimulant use disorders, encompassing methamphetamine and cocaine, have exhibited rising overdose trends, with methamphetamine-involved deaths surging from 547 in 1999 to 34,855 in 2023, yielding a mortality rate increase from 0.20 to 12.13 per 100,000.[216] Cocaine-involved overdose rates climbed from 4.5 per 100,000 in 2018 to 8.6 in 2023, often co-occurring with opioids in 43.1% of cases from 2021 to mid-2024.[217] Past-year misuse affected 10.2 million U.S. individuals aged 12 and older in 2022, reflecting polysubstance patterns and limited effective pharmacotherapies.[218] Cannabis use has expanded post-legalization, with U.S. past-year prevalence reaching 25% (62 million people aged 12+) in 2022, up from prior decades.[219] In legalized states, frequent use among non-college young adults rose by 2 percentage points to 14%, with overall youth current use increasing from 11.54% in 2020 to 15.11% in 2022.[220] [221] Cannabis dependence rates have followed suit, though evidence on causality remains mixed due to self-selection in legalization adopters.[222] Alcohol use disorder affects approximately 400 million people globally (7% of adults aged 15+), with stable but persistent prevalence; incident cases among working-age adults totaled 51.3 million in 2021.[223] [224] In the U.S., alcohol-attributable deaths rose 70% over the past decade to 51,191 in 2022, linked to increased binge drinking (24% past-month among adults).[225] [226] Tobacco and nicotine addiction trends show declining combustible cigarette use but persistent challenges from vaping, with 1 in 5 adults worldwide still addicted as of 2025.[227] U.S. youth e-cigarette use dropped significantly in recent years, yet remains the most common tobacco product among high schoolers, with nearly 30% of users vaping daily in 2024 and nicotine's adolescent brain effects heightening addiction risk.[228] [229] Among behavioral addictions, gambling disorder prevalence stands at about 1% severe cases in U.S. adults (2.5 million), with a 33% surge in help-seeking post-sports betting legalization in 2018.[230] [231] Globally, 11.9% of men and 5.5% of women report gambling-related harm.[211] Internet gaming disorder affects a small proportion overall per WHO estimates, though meta-analyses indicate 10.4% prevalence among young adults, with rates varying widely (0.7–27.5%) by region and measurement.[232] [233]Historical Development
Early Theories and Shifts in Paradigm
In ancient Greek philosophy, excessive indulgence in substances was conceptualized as akrasia, or weakness of the will, wherein individuals knowingly act against their better judgment due to lack of self-control, as articulated by Aristotle in his Nicomachean Ethics.[234] Aristotle linked this to the virtue of temperance (sophrosyne), emphasizing moderation in appetites for food, drink, and pleasure as essential for eudaimonia, or human flourishing; failure to achieve this balance was seen as a moral deficiency rather than an involuntary condition.[235] This perspective framed habitual overconsumption not as a disease but as a failure of rational agency, influencing subsequent Western views on intemperance as a character flaw amenable to ethical training.[236] Throughout much of history, particularly in Judeo-Christian traditions and up to the early 20th century, the dominant moral model portrayed addiction as a sin or ethical lapse, attributing compulsive substance use to personal vice, lack of willpower, or demonic influence, which justified punitive responses like shaming or incarceration.[1] This model, reinforced by 19th-century temperance movements in the United States and Europe, viewed alcoholics and drug users as morally culpable, with organizations like the Woman's Christian Temperance Union advocating prohibition as a societal remedy for individual failings; empirical data from the era, such as rising alcohol-related crime rates, was often invoked to support claims of widespread moral decay.[237] Critics of this paradigm, however, noted its tendency to overlook environmental factors like poverty or trauma, though proponents argued it underscored personal responsibility, aligning with causal accounts where choice initiates and sustains habitual use.[238] A significant paradigm shift occurred in the mid-20th century with the medicalization of addiction, epitomized by E. M. Jellinek's 1952 paper and 1960 book The Disease Concept of Alcoholism, which proposed alcoholism as a progressive disease characterized by loss of control, physical dependence, and distinct phases (e.g., prodromal, crucial, chronic).[239] Jellinek's typology, drawing on survey data from Alcoholics Anonymous members, differentiated "gamma" alcoholism (acquired increased tissue tolerance and withdrawal) from other forms, framing it as a treatable biopsychosocial illness rather than mere moral weakness, thereby reducing stigma and promoting rehabilitation over punishment.[240] This model gained traction through institutions like the American Medical Association's 1956 endorsement of alcoholism as a disease, shifting policy toward therapeutic interventions; however, detractors highlighted methodological flaws in Jellinek's data, such as self-selected samples, questioning its universality while acknowledging its role in destigmatizing treatment-seeking.[241] Subsequent refinements incorporated neurobiological evidence, but early adopters emphasized multifactorial causality over purely volitional explanations.[242]Modern Research Milestones
In 1954, James Olds and Peter Milner demonstrated that rats would repeatedly self-administer electrical stimulation to specific brain regions, such as the septal area, revealing the existence of neural circuits underlying reward and reinforcement, which laid the groundwork for understanding addiction as involving hijacked natural reward pathways.[243] This discovery shifted paradigms from purely behavioral views toward neurobiological mechanisms, showing that direct activation of these circuits produces profound motivation akin to drug-seeking behaviors.[244] Subsequent research in the 1960s and 1970s established self-administration paradigms for drugs in animals, confirming that substances like opioids and cocaine sustain operant responding through reinforcement, mirroring human addiction patterns and emphasizing pharmacological specificity in reward circuit activation.[245] By the late 1970s, studies identified the mesolimbic dopamine pathway—from the ventral tegmental area to the nucleus accumbens—as central to drug reward, with psychostimulants acutely elevating dopamine levels to drive reinforcement learning and habit formation.[246] In the 1990s, positron emission tomography (PET) imaging by Nora Volkow and colleagues provided direct evidence of neuroadaptations in human addicts, revealing reduced dopamine D2 receptor availability and altered brain glucose metabolism in cocaine users compared to controls, linking chronic drug use to prefrontal cortex hypoactivity and impaired impulse control.[247] These findings supported the brain disease model of addiction, portraying it as a disorder of dysregulated decision-making circuits rather than mere moral failing.[5] Molecular investigations advanced in the early 2000s with the identification of ΔFosB, a transcription factor that accumulates in the nucleus accumbens after repeated drug exposure, acting as a sustained "molecular switch" to promote long-term neural adaptations favoring addiction vulnerability over acute responses.[82] Overexpression of ΔFosB in animal models enhances sensitivity to drug rewards and escalates intake, while its persistence post-abstinence explains relapse propensity.[81] Twin and adoption studies from the 1980s onward quantified addiction's heritability at approximately 40-60% across substances, with meta-analyses confirming genetic influences on liability independent of environmental factors like family transmission.[248] Recent genome-wide association studies, such as a 2023 NIH analysis, uncovered shared genetic loci across substance use disorders, indicating common polygenic risks that modulate reward sensitivity and impulsivity.[249] These milestones collectively underscore addiction's multifactorial etiology, integrating genetic predispositions with neuroplastic changes induced by drug exposure.[86]Societal Implications and Debates
Policy, Stigma, and Personal Agency
Drug policies addressing addiction have historically oscillated between punitive enforcement and public health-oriented approaches, with empirical outcomes favoring the latter in reducing harms without increasing prevalence. In the United States, the War on Drugs, initiated by President Richard Nixon in 1971, prioritized criminalization, leading to mass incarceration where drug offenses accounted for one-fifth of the prison population—or approximately 456,000 individuals—by 2018, yet states with higher imprisonment rates showed no corresponding reductions in drug problems, and national overdose deaths surged from 6,000 in 1980 to over 100,000 annually by 2021.[250] [251] In contrast, Portugal's 2001 decriminalization of personal possession of all drugs treated use as an administrative rather than criminal matter, redirecting resources to dissuasion commissions and treatment; this resulted in a 95% drop in drug-related HIV infections from 2001 to 2012, overdose deaths falling from 80 per million in 2001 to 3 per million by 2019, and no significant rise in overall drug use, though critics note modest increases in youth experimentation.[252] [253] These outcomes underscore that coercive policies exacerbate incarceration disparities—disproportionately affecting Black Americans, who comprised 24% of drug arrests in 2020 despite similar usage rates across races—while decriminalization correlates with improved health metrics through voluntary engagement.[254] Stigma associated with addiction, often manifesting as moral judgment or perceptions of weakness, impedes recovery by deterring treatment-seeking and fostering isolation, with longitudinal studies indicating that individuals experiencing high public or internalized stigma are less likely to initiate care and more prone to dropout, relapse, and poorer long-term outcomes.[255] [256] For instance, anticipation of stigmatization contributes to hiding substance use, delaying interventions, and exacerbating comorbidities like depression, as evidenced in multinational surveys where stigma reduced willingness to engage medical help.[257] Health professionals' own biases further compound this, with reviews showing persistent stigmatizing attitudes toward substance use disorders that undermine therapeutic alliances, though interventions like stigma-reduction training have shown limited efficacy in altering clinical behaviors.[258] While some theoretical critiques posit that stigma might incentivize self-control by imposing social costs, empirical data predominantly link it to barriers rather than motivators, particularly in contexts where the disease model dominates narratives but fails to address volitional aspects.[238] Debates on personal agency in addiction challenge the prevailing chronic brain disease model, which frames it as an involuntary, progressive pathology, by highlighting evidence of self-directed remission and responsiveness to incentives. Critics including Gene Heyman contend that addiction functions as a disorder of choice, where users weigh costs and benefits akin to economic decision-making, supported by laboratory data showing addicts forgo drugs under high-value alternatives and population surveys revealing high remission rates independent of neurobiological permanence.[259] Neuroscientist Marc Lewis argues against the disease label, positing addiction as maladaptive learning via neuroplasticity that individuals can unlearn through effort and environmental shifts, rather than irreversible hijacking, with recovery involving agency-driven rewiring rather than mere symptom management.[259] Similarly, Stanton Peele emphasizes contextual factors and willpower, critiquing the model for disempowering users by implying helplessness, despite evidence that over 50% of those with alcohol or drug problems—up to 81.8% for alcohol dependence—achieve natural recovery without treatment or self-help, often triggered by life changes like employment or relationships that alter perceived rewards.[260] [261] These findings, drawn from epidemiological cohorts, indicate that while biological vulnerabilities exist, agency plays a causal role, as most users (90% for tobacco, 75% for alcohol) never develop dependence and many exit voluntarily when contingencies shift, countering narratives that overlook self-efficacy in favor of deterministic pathology.[262] [263] Academic endorsement of the disease model may reflect funding incentives from pharmaceutical interests, yet undiluted analysis prioritizes data showing addiction's reversibility through personal resolve over chronic incurability.Cultural Narratives and Media Influence
Cultural narratives surrounding addiction have historically oscillated between viewing it as a moral failing attributable to weak character or lack of willpower and a chronic brain disease beyond individual control.[238] The moral model, prevalent in earlier eras, emphasized personal responsibility and choice, often leading to punitive responses, while the disease model, gaining traction since the late 20th century through advocacy by organizations like Alcoholics Anonymous and medical bodies, frames addiction as a progressive, relapsing condition akin to other illnesses, thereby aiming to destigmatize it by shifting blame from the individual to neurobiological factors.[264] However, empirical evidence challenges the universality of the disease narrative, as studies indicate that 50-75% of individuals with alcohol dependence achieve remission without formal treatment, often through self-directed changes motivated by life events or internal resolve, underscoring elements of agency absent in rigid disease portrayals.[265][263] Media representations significantly shape these narratives, frequently amplifying the disease model while reinforcing stereotypes that hinder nuanced understanding. In film and television, addiction is often depicted as either glamorized rebellion—associating substance use with creativity or social allure, as seen in portrayals of rock stars or artists—or as tragic downfall, emphasizing helplessness and relapse over successful self-recovery.[266] Reality shows like Intervention, which premiered in 2005 and ran for 25 seasons, humanize addicts by showcasing family dynamics and treatment entries, potentially fostering empathy and altering viewer perceptions toward viewing addiction as treatable rather than purely volitional; surveys of viewers report increased awareness of addiction's severity and support for intervention strategies.[267] Yet, such formats can sensationalize chaos and failure, with episodes highlighting dramatic relapses (occurring in about 80% of featured cases post-treatment), which may perpetuate a fatalistic view that downplays the prevalence of untreated remission documented in longitudinal studies.[268] Social media and news outlets further influence perceptions, often normalizing or stigmatizing use based on framing. Platforms like Instagram and TikTok expose youth to content glamorizing alcohol and drugs, correlating with positive attitudes and initiation; a 2023 review found higher exposure linked to permissive norms, with 70% of analyzed posts depicting substance use without negative consequences.[269] News coverage, meanwhile, frequently employs stigmatizing language—labeling individuals as "junkies" or focusing on crime—intensifying public moral judgment; experimental studies show that exposure to such portrayals increases stigma and reduces policy support for harm reduction, while images of recovery lower pity-driven biases.[270][271] Critiques note that mainstream media, influenced by institutional ties to treatment industries, underreports natural recovery rates—estimated at 75-81% for alcohol dependence in some cohorts—favoring narratives that prioritize professional intervention over evidence of self-efficacy.[272] This selective emphasis risks eroding personal agency, as lay inferences of moral responsibility diminish under disease-centric framings, potentially discouraging proactive behavioral changes.[273]References
- https://learn.genetics.[utah](/page/Utah).edu/content/addiction/genes/