Recent from talks
Contribute something
Nothing was collected or created yet.
Suicide
View on Wikipedia
| Suicide | |
|---|---|
 | |
| Le Suicidé by Édouard Manet, c. 1877 | |
| Specialty | Psychiatry, clinical psychology, clinical social work |
| Usual onset | 15–30 and 70+ years old[1] |
| Risk factors | Depression, previous attempts, bipolar disorder, autism, bereavement, breakups, divorce, loneliness, schizophrenia, personality disorders, anxiety disorders, alcoholism, chronic fatigue, chronic pain, crises, financial problems, mental disorders, physical disorders, substance abuse[2][3][4][5] |
| Prevention | Limiting access to methods of suicide, treating mental disorders and substance misuse, careful media reporting about suicide, improving social and economic conditions, improving behavior of others[2] |
| Frequency | 12 per 100,000 per year[6] |
| Deaths | 793,000 / 1.5% of deaths (2016)[7][8] |
| Suicide |
|---|
Suicide is the act of intentionally causing one's own death.[9]
Risk factors for suicide include mental disorders, neurodevelopmental disorders, physical disorders, and substance abuse.[2][3][5][10] Some suicides are impulsive acts driven by stress (such as from financial or academic difficulties), relationship problems (such as breakups or divorces), or harassment and bullying.[2][11][12] Those who have previously attempted suicide are at a higher risk for future attempts.[2] Effective suicide prevention efforts include limiting access to methods of suicide such as firearms, drugs, and poisons; treating mental disorders and substance abuse; careful media reporting about suicide; improving economic conditions;[2][13] and dialectical behaviour therapy (DBT).[14] Although crisis hotlines, like 988 in North America and 13 11 14 in Australia, are common resources, their effectiveness has not been well studied.[15][16]
Suicide is the 10th-leading cause of death worldwide,[3][6] accounting for about 1.5% of deaths.[8] In a given year, this is roughly 12 per 100,000 people.[6] Though suicides resulted in 828,000 deaths globally in 2015, up from 712,000 deaths in 1990, the age-standardized death rate decreased by 23.3%.[17][18] By gender, suicide rates are generally higher among men than women, ranging from 1.5 times higher in the developing world to 3.5 times higher in the developed world; in the Western world, non-fatal suicide attempts are more common among young people and women.[19] Suicide is generally most common among those over the age of 70; however, in certain countries, those aged between 15 and 30 are at the highest risk.[1] Europe had the highest rates of suicide by region in 2015.[20] There are an estimated 10 to 20 million non-fatal attempted suicides every year.[21] Non-fatal suicide attempts may lead to injury and long-term disabilities.[19] The most commonly adopted method of suicide varies from country to country and is partly related to the availability of effective means.[22] Assisted suicide, sometimes done when a person is in severe pain or facing an imminent death, is legal in many countries and increasing in numbers.[23][24]
Views on suicide have been influenced by broad existential themes such as religion, honor, and the meaning of life.[25][26] The Abrahamic religions traditionally consider suicide as an offense towards God due to belief in the sanctity of life.[27] During the samurai era in Japan, a form of suicide known as seppuku (腹切り, harakiri) was respected as a means of making up for failure or as a form of protest.[28] Suicide and attempted suicide, while previously illegal, are no longer so in most Western countries.[29] It remains a criminal offense in some countries.[30] In the 20th and 21st centuries, suicide has been used on rare occasions as a form of protest; it has also been committed while or after murdering others, a tactic that has been used both militarily and by terrorists.[31]
Suicide is often seen as a major catastrophe, causing significant grief to the deceased's relatives, friends and community members, and it is viewed negatively almost everywhere around the world.[32][33]
Definitions
[edit]Suicide, derived from Latin suicidium, is "the act of taking one's own life".[9][34] Attempted suicide, or non-fatal suicidal behavior, amounts to self-injury with at least some desire to end one's life that does not result in death.[35][36] Assisted suicide occurs when one individual helps another bring about their own death indirectly by providing either advice or the means to the end.[37] Euthanasia, more specifically voluntary euthanasia, is where another person takes a more active role in bringing about a person's death.[37]
Suicidal ideation is thoughts of ending one's life but not taking any active efforts to do so.[35] It may or may not involve exact planning or intent.[36] Suicidality is defined as "the risk of suicide, usually indicated by suicidal ideation or intent, especially as evident in the presence of a well-elaborated suicidal plan."[38]
In a murder–suicide (or homicide–suicide), the individual aims at taking the lives of others at the same time. A special case of this is extended suicide, where the murder is motivated by seeing the murdered persons as an extension of their self.[39] Suicide in which the reason is that the person feels that they are not part of society is known as egoistic suicide.[40]
The Centre for Suicide Prevention in Canada found that the normal verb in scholarly research and journalism for the act of suicide was commit, and argued for destigmatizing terminology related to suicide; in 2011, they published an article calling for changing the language used around suicide entitled "Suicide and language: Why we shouldn't use the 'C' word".[41][42] The American Psychological Association lists "committed suicide" as a term to avoid because it "frame[s] suicide as a crime."[43] Some advocacy groups recommend using the terms took his/her own life, died by suicide, or killed him/herself instead of committed suicide.[44][45][46] The Associated Press Stylebook recommends avoiding "committed suicide" except in direct quotes from authorities.[47] The Guardian and Observer style guides deprecate the use of "committed",[48] as does CNN.[49] Opponents of commit argue that it implies that suicide is criminal, sinful, or morally wrong.[50]
Pathophysiology
[edit]This section needs to be updated. (May 2024) |

There is no known unifying underlying pathophysiology for suicide;[19] it is believed to result from an interplay of behavioral, socio-economic and psychological factors.[22]
Low levels of brain-derived neurotrophic factor (BDNF) are directly associated with suicide[51] and indirectly associated through its role in major depression, post-traumatic stress disorder, schizophrenia and obsessive–compulsive disorder.[52] Post-mortem studies have found reduced levels of BDNF in the hippocampus and prefrontal cortex, in those with and without psychiatric conditions.[53] Serotonin, a brain neurotransmitter, is believed to be low in those who die by suicide.[54] This is partly based on evidence of increased levels of 5-HT2A receptors found after death.[55] Other evidence includes reduced levels of a breakdown product of serotonin, 5-hydroxyindoleacetic acid, in the cerebral spinal fluid.[56] However, direct evidence is hard to obtain.[55] Epigenetics, the study of changes in genetic expression in response to environmental factors which do not alter the underlying DNA, is also believed to play a role in determining suicide risk.[57]
Risk factors
[edit]Factors that affect the risk of suicide include mental disorders, drug misuse, psychological states, cultural, family and social situations, genetics, experiences of trauma or loss, and nihilism.[59][60][16] Mental disorders and substance misuse frequently co-exist.[61] Other risk factors include having previously attempted suicide,[19] the ready availability of a means to take one's life, a family history of suicide, or the presence of traumatic brain injury.[62] For example, suicide rates have been found to be greater in households with firearms than those without them.[63] Recent research examining 3,018 US counties found that "the distribution of suicide rates across US states corresponded to variations in [social determinants of health] cluster distribution in each state.[64]
Socio-economic problems such as unemployment, poverty, homelessness, and discrimination may trigger suicidal thoughts.[65][66] Suicide might be rarer in societies with high social cohesion and moral objections against suicide.[36] Genetics appears to account for between 38% and 55% of suicidal behaviors.[67] Suicides may also occur as a local cluster of cases.[68]
Most research does not distinguish between risk factors that lead to thinking about suicide and risk factors that lead to suicide attempts.[69][70] Risks for suicide attempt, rather than just thoughts of suicide, include a high pain tolerance and a reduced fear of death.[71]
Autism
[edit]Autistic individuals, on average, face more mental health and social challenges than non-autistic individuals, including higher rates of anxiety, depression, and social isolation.[72][73] They attempt and consider suicide more frequently than the general population.[74] Autistic people are about three times as likely as non-autistic people to attempt suicide.[75][76] Suicide is a leading cause of early death for autistic people without co-occurring learning disabilities.[77]
Environmental exposures
[edit]Some environmental exposures, including air pollution, intense sunlight, sunlight duration, hot weather, and high altitude, are associated with suicide.[78] There is a possible association between short-term PM10 exposure and suicide.[79][80] These factors might affect certain high-risk individuals more than others.[78]
The time of year may also affect suicide rates. There appears to be a decrease around Christmas,[81] but an increase in rates during spring and summer, which might be related to exposure to sunshine.[36] Another study found that the risk may be greater for males on their birthday.[82]
Genetics might influence rates of suicide. A family history of suicide, especially in the mother, affects children more than adolescents or adults.[83] Adoption studies have shown that this is the case for biological relatives, but not adopted relatives. This makes familial risk factors unlikely to be due to imitation.[36] Once mental disorders are accounted for, the estimated heritability rate is 36% for suicidal ideation and 17% for suicide attempts.[36] An evolutionary explanation for suicide is that it may improve inclusive fitness. This may occur if the person dying by suicide cannot have more children and takes resources away from relatives by staying alive. An objection to this explanation is that deaths by healthy adolescents likely do not increase inclusive fitness. Adaptation to a very different ancestral environment may be maladaptive in the current one.[84][85]
Media
[edit]
The media, including the Internet, plays an important role.[59][83] Certain depictions of suicide may increase its occurrence, with high-volume, prominent, repetitive coverage glorifying or romanticizing suicide having the most impact.[86] For example, about 15–40% of people leave a suicide note,[87] and media are discouraged from reporting the contents of that message. When detailed descriptions of how to kill oneself by a specific means are portrayed, this method of suicide can be imitated in vulnerable people.[22] This phenomenon has been observed in several cases after press coverage.[88][89] In a bid to reduce the adverse effect of media portrayals concerning suicide report, one of the effective methods is to educate journalists on how to report suicide news in a manner that might reduce that possibility of imitation and encourage those at risk to seek for help. When journalists follow certain reporting guidelines the risk of suicides can be decreased.[86] Getting buy-in from the media industry can be difficult, especially in the long term.[86]
This trigger of suicide contagion or copycat suicide is known as the "Werther effect", named after the protagonist in Goethe's The Sorrows of Young Werther who killed himself and then was emulated by many admirers of the book.[90] This risk is greater in adolescents who may romanticize death.[91] It appears that while news media has a significant effect, that of the entertainment media is equivocal.[92][93] It is unclear if searching for information about suicide on the Internet relates to the risk of suicide.[94] The opposite of the Werther effect is the proposed "Papageno effect", in which coverage of effective coping mechanisms may have a protective effect. The term is based upon a character in Mozart's opera The Magic Flute—fearing the loss of a loved one, he had planned to kill himself until his friends helped him out.[90] As a consequence, fictional portrayals of suicide, showing alternative consequences or negative consequences, might have a preventive effect,[95] for instance fiction might normalize mental health problems and encourage help-seeking.[96]
Medical conditions
[edit]There is an association between suicidality and physical health problems such as[97] chronic pain,[98] traumatic brain injury,[99] cancer,[100] chronic fatigue syndrome,[101] kidney failure (requiring hemodialysis), HIV, and systemic lupus erythematosus.[97] The diagnosis of cancer approximately doubles the subsequent frequency of suicide.[100] The prevalence of increased suicidality persisted after adjusting for depressive illness and alcohol abuse. Among people with more than one medical condition the frequency was particularly high. In Japan, health problems are listed as the primary justification for suicide.[102]
Sleep disturbances, such as insomnia[103] and sleep apnea, are risk factors for depression and suicide. In some instances, the sleep disturbances may be a risk factor independent of depression.[104] A number of other medical conditions may present with symptoms similar to mood disorders, including hypothyroidism, Alzheimer's, brain tumors, systemic lupus erythematosus, and adverse effects from a number of medications (such as beta blockers and steroids).[19]
Mental illness
[edit]Mental illness is present at the time of suicide 27% to more than 90% of the time.[105][19][106][107] Of those who have been hospitalized for suicidal behavior, the lifetime risk of suicide is 8.6%.[19][108] Comparatively, non-suicidal people hospitalized for affective disorders have a 4% lifetime risk of suicide.[108] Half of all people who die by suicide may have major depressive disorder; having this or one of the other mood disorders such as bipolar disorder increases the risk of suicide 20-fold.[109] Other conditions implicated include schizophrenia (14%), personality disorders (8%),[110][111] obsessive–compulsive disorder,[112] and post-traumatic stress disorder.[19]
Others estimate that about half of people who die by suicide could be diagnosed with a personality disorder, with borderline personality disorder being the most common.[113] About 5% of people with schizophrenia die of suicide.[114] Eating disorders are another high risk condition.[97] Around 22% to 50% of people with gender dysphoria have attempted suicide, however this greatly varies by region.[115][116][117][118][119]
Among approximately 80% of suicides, the individual has seen a physician within the year before their death,[120] including 45% within the prior month.[121] Approximately 25–40% of those who died by suicide had contact with mental health services in the prior year.[105][120] Antidepressants of the SSRI class appear to increase the frequency of suicide among children and young persons.[122] An unwillingness to get help for mental health problems also increases the risk.[68]
Occupational factors
[edit]Certain occupations carry an elevated risk of self-harm and suicide, such as military careers. Research in several countries has found that the rate of suicide among former armed forces personnel in particular,[123][124][125][126] and young veterans especially,[127][128][123] is markedly higher than that found in the general population. War veterans have a higher risk of suicide due in part to higher rates of mental illness, such as post-traumatic stress disorder, and physical health problems related to war.[129]
Previous attempts
[edit]A 2002 review of about 90 suicide related studies concluded that the risk of suicide following a previous attempt or self-harm is hundreds of times larger than in the general population.[130] A more recent study estimated that individuals with a history of suicide attempts are approximately 25 times more likely to die by suicide compared to the general population.[131] These findings makes a suicide attempt one of the strongest predictors of eventual suicide.[19]
Among the population that died by suicide, it is estimated that between 25% (up to a year prior)[130] to 40% [132] attempted suicide before. The likelihood of dying by suicide after the subsequent attempt depends on the means used, the age of the person and their gender.[132] Other risk factors such as substance use and mental health[131] impact likelihood of suicide after an attempt. High suicidal intent during previous attempts is another strong predictor.[133]
Time passed since the last attempt also plays a critical role. The first and the second year have the highest risk of suicide.[130][131] It is estimated that 1% die by suicide within a year of the first attempt,[19] and that about 90% of suicide survivors will not die of suicide.[134][97]
Psychosocial factors
[edit]A number of psychological factors increase the risk of suicide including: hopelessness, loss of pleasure in life, depression, anxiousness, agitation, rigid thinking, rumination, thought suppression, and poor coping skills.[109][83][135] A poor ability to solve problems, the loss of abilities one used to have, and poor impulse control also play a role.[109][84] In older adults, the perception of being a burden to others is important.[136] Those who have never married are also at greater risk.[19] Recent life stresses, such as a loss of a family member or friend or the loss of a job, might be a contributing factor.[109][68]
Certain personality factors, especially high levels of neuroticism and introvertedness, have been associated with suicide. This might lead to people who are isolated and sensitive to distress to be more likely to attempt suicide.[83] On the other hand, optimism has been shown to have a protective effect.[83] Other psychological risk factors include having few reasons for living and feeling trapped in a stressful situation.[83] Changes to the stress response system in the brain might be altered during suicidal states.[36] Specifically, changes in the polyamine system[137] and hypothalamic–pituitary–adrenal axis.[138]
Social isolation and the lack of social support has been associated with an increased risk of suicide.[83] Poverty is also a factor,[139] with heightened relative poverty compared to those around a person increasing suicide risk.[140] Over 200,000 farmers in India have died by suicide since 1997, partly due to issues of debt.[141] In China, suicide is three times as likely in rural regions as urban ones, partly, it is believed, due to financial difficulties in this area of the country.[142]
Being religious may reduce one's risk of suicide while beliefs that suicide is noble may increase it.[143][68][144] This has been attributed to the negative stance many religions take against suicide and to the greater connectedness religion may give.[143] Muslims, among religious people, appear to have a lower rate of suicide; however, the data supporting this is not strong.[30] There does not appear to be a difference in rates of attempted suicide.[30] Young women in the Middle East may have higher rates.[145]
Rational
[edit]
Rational suicide is the reasoned taking of one's own life.[146] However, some consider suicide as never being rational.[146]
Euthanasia and assisted suicide are accepted practices in a number of countries among those who have a poor quality of life without the possibility of getting better.[147][148] They are supported by the legal arguments for a right to die.[148]
The act of taking one's life for the benefit of others is known as altruistic suicide.[149] An example of this is an elder ending his or her life to leave greater amounts of food for the younger people in the community.[149] Suicide in some Inuit cultures has been seen as an act of respect, courage, or wisdom.[150]
A suicide attack is a political or religious action where an attacker carries out violence against others which they understand will result in their own death.[151] Some suicide bombers are motivated by a desire to obtain martyrdoms or are religiously motivated.[129] Kamikaze missions in the latter stages of World War II were carried out as a duty to a higher cause or moral obligation.[150] Murder–suicide is an act of homicide followed within a week by suicide of the person who carried out the act.[152]
Mass suicides are often performed under social pressure where members give up autonomy to a leader (see Notable cases below).[153] Mass suicides can take place with as few as two people, often referred to as a suicide pact.[154] In extenuating situations where continuing to live would be intolerable, some people use suicide as a means of escape.[155][156] Some inmates in Nazi concentration camps are known to have killed themselves during the Holocaust by deliberately touching the electrified fences.[157]
Self-harm
[edit]Non-suicidal self-harm is common with 18% of people engaging in self-harm over the course of their life.[158]: 1 Acts of self-harm are not usually suicide attempts and most who self-harm are not at high risk of suicide.[159] Some who self-harm, however, do still end their life by suicide, and risk for self-harm and suicide may overlap.[159] Individuals who have been identified as self-harming after being admitted to hospital are 68% (38–105%) more likely to die by suicide.[160]: 279
Substance misuse
[edit]
Substance misuse is the second most common risk factor for suicide after major depression and bipolar disorder.[161] Both chronic substance misuse as well as acute intoxication are associated.[61][162] When combined with personal grief, such as bereavement, the risk is further increased.[162] Substance misuse is also associated with mental health disorders.[61]
Most people are under the influence of sedative-hypnotic drugs (such as alcohol or benzodiazepines) when they die by suicide,[163] with alcoholism present in between 15% and 61% of cases.[61] Use of prescribed benzodiazepines is associated with an increased rate of suicide and attempted suicide. The pro-suicidal effects of benzodiazepines are suspected to be due to a psychiatric disturbance caused by side effects, such as disinhibition, or withdrawal symptoms.[10] Countries that have higher rates of alcohol use and a greater density of bars generally also have higher rates of suicide.[164] About 2.2–3.4% of those who have been treated for alcoholism at some point in their life die by suicide.[164] Alcoholics who attempt suicide are usually male, older, and have tried to take their own lives in the past.[61] Between 3 and 35% of deaths among those who use heroin are due to suicide (approximately fourteenfold greater than those who do not use).[165] In adolescents who misuse alcohol, neurological and psychological dysfunctions may contribute to the increased risk of suicide.[166]
The misuse of cocaine and methamphetamine has a high correlation with suicide.[61][167][168] In those who use cocaine, the risk is greatest during the withdrawal phase.[169] Those who used inhalants are also at significant risk with around 20% attempting suicide at some point and more than 65% considering it.[61] Smoking cigarettes is associated with risk of suicide.[170] There is little evidence as to why this association exists; however, it has been hypothesized that those who are predisposed to smoking are also predisposed to suicide, that smoking causes health problems which subsequently make people want to end their life, and that smoking affects brain chemistry causing a propensity for suicide.[170] Cannabis, however, does not appear to independently increase the risk.[61]
Other factors
[edit]Trauma is a risk factor for suicidality in both children[171] and adults.[83] Some may take their own lives to escape bullying or prejudice.[172] A history of childhood sexual abuse[173] and time spent in foster care are also risk factors.[174] Sexual abuse is believed to contribute to approximately 20% of the overall risk.[67] Significant adversity early in life has a negative effect on problem-solving skills and memory, both of which are implicated in suicidality.[36] According to a 2022 study, adverse childhood experiences maybe "associated with a two-fold higher odds" of anxiety disorders, depression and suicidality."[175]
Problem gambling is associated with increased suicidal ideation and attempts compared to the general population.[176] Between 12 and 24% of pathological gamblers attempt suicide.[177] The rate of suicide among their spouses is three times greater than that of the general population.[177] Other factors that increase the risk in problem gamblers include concomitant mental illness, alcohol, and drug misuse.[178]
Infection by the parasite Toxoplasma gondii, more commonly known as toxoplasmosis, has been linked with suicide risk. One explanation states that this is caused by altered neurotransmitter activity due to the immunological response.[36]
Community-level factors can also play a role. For example, a 2025 study found that a one-unit increase in local homicide rates was followed by a 3.6% rise in suicide rates the next year, suggesting that community-level violence may contribute to suicide risk.[179]
Dutch research by Lin Zhang focuses on the role of P2RX7 and the apoptosis of microglia in suicidal ideation.[184]
Prevention
[edit]Suicide prevention is a term used for the collective efforts to reduce the incidence of suicide through preventive measures. Protective factors for suicide include support, and access to therapy.[60] About 60% of people with suicidal thoughts do not seek help.[185] Reasons for not doing so include low perceived need, and wanting to deal with the problem alone.[185] Despite these high rates, there are few established treatments available for suicidal behavior.[83]
Reducing access to certain methods, such as access to firearms or toxins such as opioids and pesticides, can reduce risk of suicide by that method.[22][186][16][36] Reducing access to easily-accessible methods of suicide may make impulsive attempts less likely to succeed.[187] Other measures include reducing access to charcoal (for burning) and adding barriers on bridges and subway platforms.[22][188][16] Treatment of drug and alcohol addiction, depression, and those who have attempted suicide in the past, may also be effective.[186][16] Some have proposed reducing access to alcohol as a preventive strategy (such as reducing the number of bars).[61]

In young adults who have recently thought about suicide, cognitive behavioral therapy appears to improve outcomes.[189][83] School-based programs that increase mental health literacy and train staff have shown mixed results on suicide rates.[16] Economic development through its ability to reduce poverty may be able to decrease suicide rates.[139] Efforts to increase social connection, especially in elderly males, may be effective.[190] In people who have attempted suicide, following up on them might prevent repeat attempts.[191] Although crisis hotlines are common, there is little evidence to support or refute their effectiveness.[15][16] Preventing childhood trauma provides an opportunity for suicide prevention.[171] The World Suicide Prevention Day is observed annually on 10 September with the support of the International Association for Suicide Prevention and the World Health Organization.[192]
Diet
[edit]About 50% of people who die of suicide have a mood disorder such as major depression.[193][194] Sleep and diet may play a role in depression (major depressive disorder), and interventions in these areas may be an effective add-on to conventional methods.[195] Vitamin B2, B6 and B12 deficiency may cause depression in females.[196]
Risk of depression may be reduced with a healthy diet "high in fruits, vegetables, nuts, and legumes; moderate amounts of poultry, eggs, and dairy products; and only occasional red meat".[197][198] A balanced diet and the consumption of lots of water is essential for mental health. Consuming oily fish may also help as they contain omega-3 fats. Consuming too much refined carbohydrates (e.g., snack foods) may increase the risk of depression symptoms. The mechanism on how diet improves or worsens mental health is still not fully understood. Blood glucose levels alterations, inflammation, or effects on the gut microbiome have been suggested.[197]
Screening
[edit]IS PATH WARM [...] is an acronym [...] to assess [...] a potentially suicidal individual, (i.e., ideation, substance abuse, purposelessness, anger, feeling trapped, hopelessness, withdrawal, anxiety, recklessness, and mood).[199]
— American Association of Suicidology (2019)
There is little data on the effects of screening the general population on the ultimate rate of suicide.[200][201] Screening those who come to the emergency departments with injuries from self-harm have been shown to help identify suicide ideation and suicide intention. Psychometric tests such as the Beck Depression Inventory or the Geriatric Depression Scale for older people are being used.[202] As there is a high rate of people who test positive via these tools that are not at risk of suicide, there are concerns that screening may significantly increase mental health care resource utilization.[203] Assessing those at high risk, though, is recommended for.[19] Asking about suicidality does not appear to increase the risk.[19]
Treatment of mental illness
[edit]In those with mental health problems, a number of treatments may reduce the risk of suicide. Those who are actively suicidal may be admitted to psychiatric care either voluntarily or involuntarily.[19] Possessions that may be used to harm oneself are typically removed.[97] Some clinicians get patients to sign suicide prevention contracts where they agree to not harm themselves if released.[19] However, evidence does not support a significant effect from this practice.[19] If a person is at low risk, outpatient mental health treatment may be arranged.[97] Short-term hospitalization has not been found to be more effective than community care for improving outcomes in those with borderline personality disorder who are chronically suicidal.[204][205]
There is tentative evidence that psychotherapy, specifically dialectical behaviour therapy, reduces suicidality in adolescents[206] as well as in those with borderline personality disorder.[207] It may also be useful in decreasing suicide attempts in adults at high risk.[208]
There is controversy around the benefit-versus-harm of antidepressants.[59] In young persons, some antidepressants, such as SSRIs, appear to increase the risk of suicidality from 25 per 1000 to 40 per 1000.[209] In older persons, however, they may decrease the risk.[19] Lithium appears effective at lowering the risk in those with bipolar disorder and major depression to nearly the same levels as that of the general population.[210][211] Clozapine may decrease the thoughts of suicide in some people with schizophrenia.[212] Ketamine, which is a dissociative anaesthetic, seems to lower the rate of suicidal ideation.[213] In the United States, health professionals are legally required to take reasonable steps to try to prevent suicide.[214][215]
Caring letters
[edit]
The "Caring Letters" model of suicide prevention[216][217] involved mailing short letters that expressed the researchers' interest in the recipients without pressuring them to take any action. The intervention reduced deaths by suicide, as proven through a randomized controlled trial.[218] The technique involves letters sent from a researcher who had spoken at length with the recipient during a suicidal crisis.[217] The typewritten form letters were brief – sometimes as short as two sentences – personally signed by the researcher, and expressed interest in the recipient without making any demands.[217] They were initially sent monthly, eventually decreasing in frequency to quarterly letters; if the recipient wrote back, then an additional personal letter was mailed.[217]
Caring letters are inexpensive and either the only,[217] or one of very few,[216] approaches to suicide prevention that has been scientifically proven to work during the first years after a suicide attempt that resulted in hospitalization.
Methods
[edit]
The leading method of suicide varies among countries. The leading methods in different regions include hanging, pesticide poisoning, and firearms.[220] These differences are believed to be in part due to availability of the different methods.[22] A review of 56 countries found that hanging was the most common method in most of the countries,[220] accounting for 53% of male suicides and 39% of female suicides.[221]
Worldwide, 30% of suicides are estimated to occur from pesticide poisoning, most of which occur in the developing world.[2] The use of this method varies markedly from 4% in Europe to more than 50% in the Pacific region.[222] It is also common in Latin America due to the ease of access within the farming populations.[22] In many countries, drug overdoses account for approximately 60% of suicides among women and 30% among men.[223] Many are unplanned and occur during an acute period of ambivalence.[22] The death rate varies by method: firearms 80–90%, drowning 65–80%, hanging 60–85%, jumping 35–60%, charcoal burning 40–50%, pesticides 60–75%, and medication overdose 1.5–4.0%.[22] The most common attempted methods of suicide differ from the most common methods of completion; up to 85% of attempts are via drug overdose in the developed world.[97]
In China, the consumption of pesticides is the most common method.[224] In Japan, self-disembowelment known as seppuku (harakiri) still occurs;[224] however, hanging and jumping are the most common.[225] Jumping to one's death is common in both Hong Kong and Singapore at 50% and 80% respectively.[22] In Switzerland, firearms are the most frequent suicide method in young males, although this method has decreased since guns have become less common.[226][227] In the United States, 50% of suicides involve the use of firearms, with this method being somewhat more common in men (56%) than women (31%).[228] The next most common cause was hanging in males (28%) and self-poisoning in females (31%).[228] Together, hanging and poisoning constituted about 42% of U.S. suicides (as of 2017[update]).[228]
Epidemiology
[edit]
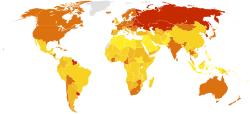
Approximately 1.4% of people die by suicide, a mortality rate of 11.6 per 100,000 persons per year.[6][19] Suicide resulted in 842,000 deaths in 2013 up from 712,000 deaths in 1990.[18] Rates of suicide have increased by 60% from the 1960s to 2012, with these increases seen primarily in the developing world.[3] Globally, as of 2008[update]/2009, suicide is the tenth leading cause of death.[3] For every suicide that results in death there are between 10 and 40 attempted suicides.[19]
Suicide rates differ significantly between countries and over time.[6] As a percentage of deaths in 2008 it was: Africa 0.5%, South-East Asia 1.9%, Americas 1.2% and Europe 1.4%.[6] Rates per 100,000 were: Australia 8.6, Canada 11.1, China 12.7, India 23.2, United Kingdom 7.6, United States 11.4 and South Korea 28.9.[230][231] It was ranked as the 10th leading cause of death in the United States in 2016 with about 45,000 cases that year.[232] Rates have increased in the United States in the last few years,[232] with about 49,500 people dying by suicide in 2022, the highest number ever recorded.[233] In the United States, about 650,000 people are seen in emergency departments yearly due to attempting suicide.[19] The United States rate among men in their 50s rose by nearly half in the decade 1999–2010.[234] Greenland, Lithuania, Japan, and Hungary have the highest rates of suicide.[6] Around 75% of suicides occur in the developing world.[2] The countries with the greatest absolute numbers of suicides are China and India, partly due to their large population size, accounting for over half the total.[6] In China, suicide is the 5th leading cause of death.[235]
An unofficial report estimated 5,000 suicides in Iran in 2022.[238]
Sex and gender
[edit]Globally as of 2012[update], death by suicide occurs about 1.8 times more often in males than females.[6][239] In the Western world, males die three to four times more often by means of suicide than do females.[6] This difference is even more pronounced in those over the age of 65, with tenfold more males than females dying by suicide.[240] Suicide attempts and self-harm are between two and four times more frequent among females.[19][241][242] Researchers have attributed the difference between suicide and attempted suicide among the sexes to males using more lethal means to end their lives.[240][243][244] However, separating intentional suicide attempts from non-suicidal self-harm is not currently done in places like the United States when gathering statistics at the national level.[245]
China has one of the highest female suicide rates in the world and is the only country where it is higher than that of men (ratio of 0.9).[6][235] In the Eastern Mediterranean, suicide rates are nearly equivalent between males and females.[6] The highest rate of female suicide is found in South Korea at 22 per 100,000, with high rates in South-East Asia and the Western Pacific generally.[6]
A number of reviews have found an increased risk of suicide among lesbian, gay, bisexual, and transgender people.[246][247] Among transgender persons, rates of attempted suicide are about 40% compared to a general population rate of 5%.[248][249] This is believed to in part be due to social stigmatisation.[250]
Age
[edit]
In many countries, the rate of suicide is highest in the middle-aged[252] or elderly.[22] The absolute number of suicides, however, is greatest in those between 15 and 29 years old, due to the number of people in this age group.[6] Worldwide, the average age of suicide is between age 30 and 49 for both men and women.[253] Suicidality is rare in children, but increases during the transition to adolescence.[254]
In the United States, the suicide death rate is greatest in Caucasian men older than 80 years, even though younger people more frequently attempt suicide.[19] It is the second most common cause of death in adolescents[59] and in young males is second only to accidental death.[252] In young males in the developed world, it is the cause of nearly 30% of mortality.[252] In the developing world rates are similar, but it makes up a smaller proportion of overall deaths due to higher rates of death from other types of trauma.[252] In South-East Asia, in contrast to other areas of the world, deaths from suicide occur at a greater rate in young females than elderly females.[6]
History
[edit]
In ancient Athens, a person who died by suicide without the approval of the state was denied the honors of a normal burial. The person would be buried alone, on the outskirts of the city, without a headstone or marker.[255] It was also common for the hand to be cut off the body and buried separately[256] - the hand (and the instrument used) being considered the perpetrator.[257] However, it was deemed to be an acceptable method to deal with military defeat.[258] In Ancient Rome, while suicide was initially permitted, it was later deemed a crime against the state due to its economic costs.[259] Aristotle condemned all forms of suicide while Plato was ambivalent.[260] In Rome, some reasons for suicide included volunteering death in a gladiator combat, guilt over murdering someone, to save the life of another, as a result of mourning, from shame from being raped, and as an escape from intolerable situations like physical suffering, military defeat, or criminal pursuit.[260]

Suicide came to be regarded as a sin in Christian Europe and was condemned at the Council of Arles (452) as the work of the Devil. In the Middle Ages, the Church had drawn-out discussions as to when the desire for martyrdom was suicidal, as in the case of martyrs of Córdoba. Despite these disputes and occasional official rulings, Catholic doctrine was not entirely settled on the subject of suicide until the later 17th century. A criminal ordinance issued by Louis XIV of France in 1670 was extremely severe, even for the times: the dead person's body was drawn through the streets, face down, and then hung or thrown on a garbage heap. Additionally, all of the person's property was confiscated.[261][262]
Attitudes towards suicide slowly began to shift during the Renaissance. John Donne's work Biathanatos contained one of the first modern defences of suicide, bringing proof from the conduct of Biblical figures, such as Jesus, Samson and Saul, and presenting arguments on grounds of reason and nature to sanction suicide in certain circumstances.[263]
The secularization of society that began during the Enlightenment questioned traditional religious attitudes (such as Christian views on suicide) toward suicide and brought a more modern perspective to the issue. David Hume denied that suicide was a crime as it affected no one and was potentially to the advantage of the individual. In his 1777 Essays on Suicide and the Immortality of the Soul he rhetorically asked, "Why should I prolong a miserable existence, because of some frivolous advantage which the public may perhaps receive from me?"[263] Hume's analysis was criticized by philosopher Philip Reed as being "uncharacteristically (for him) bad", since Hume took an unusually narrow conception of duty and his conclusion depended upon the suicide producing no harm to others – including causing no grief, feelings of guilt, or emotional pain to any surviving friends and family – which is almost never the case.[264] A shift in public opinion at large can also be discerned; The Times in 1786 initiated a spirited debate on the motion "Is suicide an act of courage?".[265]
By the 19th century, the act of suicide had shifted from being viewed as caused by sin to being caused by insanity in Europe.[262] Although suicide remained illegal during this period, it increasingly became the target of satirical comments, such as the Gilbert and Sullivan comic opera The Mikado, which satirized the idea of executing someone who had already killed himself.
By 1879, English law began to distinguish between suicide and homicide, although suicide still resulted in forfeiture of estate.[266] In 1882, the deceased were permitted daylight burial in England[267] and by the middle of the 20th century, suicide had become legal in much of the Western world. The term suicide first emerged shortly before 1700 to replace expressions on self-death which were often characterized as a form of self-murder in the West.[260]
Social and culture
[edit]Legislation
[edit]

Suicide is a crime in some parts of the world.[268] No country in Europe currently considers suicide or attempted suicide to be a crime.[269] However, it was in most Western European countries from the Middle Ages until at least the 19th century.[266] The Netherlands was the first country to legalize both physician-assisted suicide and euthanasia, which took effect in 2002, although only doctors are allowed to assist in either of them, and have to follow a protocol prescribed by Dutch law.[270] If such protocol is not followed, it is an offence punishable by law. In Germany, active euthanasia is illegal and anyone present during suicide may be prosecuted for failure to render aid in an emergency.[271] Switzerland has taken steps to legalize assisted suicide for the chronically mentally ill. The high court in Lausanne, Switzerland, in a 2006 ruling, granted an anonymous individual with longstanding psychiatric difficulties the right to end his own life.[272] England and Wales decriminalized suicide via the Suicide Act 1961 and the Republic of Ireland in 1993.[269] The word "commit" was used in reference to its being illegal, but many organisations have stopped it because of the negative connotation.[273][274]
In the United States, suicide is not illegal, but may be associated with penalties for those who attempt it.[269][better source needed] Physician-assisted suicide is legal in the state of Washington for people with terminal diseases.[275] In Oregon, people with terminal diseases may request medications to help end their lives.[276] Canadians who have attempted suicide may be barred from entering the United States. U.S. laws allow border guards to deny access to people who have a mental illness, including those with previous suicide attempts.[277][278][needs update]
In Australia, suicide is not a crime,[279] however it is a crime to counsel, incite, or aid and abet another in attempting to die by suicide, and the law explicitly allows any person to use "such force as may reasonably be necessary" to prevent another from taking their own life.[280] The Northern Territory of Australia briefly had legal physician-assisted suicide from 1996 to 1997.[281]
In India, suicide was illegal until 2014, and surviving family members used to face legal difficulties.[282][283] It remains a criminal offense in most Muslim-majority nations.[30]
In Malaysia, suicide per se is not a crime; however, attempted suicide is. Under Section 309 of the Penal Code, a person convicted of attempting suicide can be punished with imprisonment of up to one year, fined, or both. There are ongoing efforts to decriminalise attempted suicide, although rights groups and non-governmental organisations such as the local chapter of Befrienders say that progress has been slow.[284][285] Proponents of decriminalisation argue that suicide legislation may deter people from seeking help, and may even strengthen the resolve of would-be suicides to end their lives to avoid prosecution.[286] The first reading of a bill to repeal Section 309 of the Penal Code was tabled in Parliament in April 2023, bringing Malaysia one step closer towards decriminalising attempted suicide.[287]
Suicide became a trending crisis in North Korea in 2023; a secret order criminalized suicide as treason against the socialist state.[288]
Religious views
[edit]Christianity
[edit]Most forms of Christianity consider suicide sinful, based mainly on the writings of influential Christian thinkers of the Middle Ages, such as St. Augustine and St. Thomas Aquinas, but suicide was not considered a sin under the Byzantine Christian code of Justinian, for instance.[289][290] In Catholic and Orthodox doctrine, suicide is considered to be murder, violating the commandment "Thou shalt not kill," and historically neither church would even hold a burial service for a member that died by suicide, deeming it an act that condemned the person to hell, since they died in a state of mortal sin.[291] The basic idea being that life is a gift given by God which should not be spurned, and that suicide is against the "natural order" and thus interferes with God's master plan for the world.[292] However, according to the Catechism of the Catholic Church, it is believed that mental illness or grave fear of suffering diminishes the responsibility of the one committing suicide.[293]
Judaism
[edit]Judaism focuses on the importance of valuing this life, and as such, suicide is tantamount to denying God's goodness in the world. Despite this, under extreme circumstances when there has seemed no choice but to either be killed or forced to betray their religion, there are several accounts of Jews having died by suicide, either individually or in groups (see Holocaust, Masada, First French persecution of the Jews and York Castle for examples), and as a grim reminder there is even a prayer in the Jewish liturgy for "when the knife is at the throat", for those dying "to sanctify God's Name" (see Martyrdom). These acts have received mixed responses by Jewish authorities, regarded by some as examples of heroic martyrdom, while others state that it was wrong for them to take their own lives in anticipation of martyrdom.[294][better source needed]
Islam
[edit]Islamic religious views condemn suicide[30] and consider it haram. Hadith manuscripts state that suicide is unlawful and a sin,[30] and the Quran explicitly forbids it.[295][296] In Islamic countries, suicide is often stigmatized;[296] it is believed that those that successfully die by suicide are forbidden from entering Jannah.
Hinduism
[edit]
In Hinduism, suicide is generally disdained and is considered equally sinful as murdering another in contemporary Hindu society. Hindu Scriptures state that one who dies by suicide will become part of the spirit world, wandering earth until the time one would have otherwise died, had one not taken one's own life.[297] However, Hinduism accepts a man's right to end one's life through the non-violent practice of fasting to death, termed Prayopavesa;[298] but Prayopavesa is strictly restricted to people who have no desire or ambition left, and no responsibilities remaining in this life.[298]
Jainism
[edit]Jainism has a similar practice named Santhara. Sati, or self-immolation by widows, is a rare and illegal practice in Hindu society.[299]
Ainu
[edit]Within the Ainu religion, someone who dies by suicide is believed to become a ghost (tukap) who would haunt the living,[300] to come to fulfillment from which they were excluded during life.[301] Also, someone who insults another so they kill themselves is regarded as co-responsible for their death.[302] According to Norbert Richard Adami, this ethic exists due to the case that solidarity within the community is much more important to Ainu culture than it is to the Western world.[302]
Philosophy
[edit]A number of questions are raised within the philosophy of suicide, including what constitutes suicide, whether or not suicide can be a rational choice, and the moral permissibility of suicide.[303] Arguments as to acceptability of suicide in moral or social terms range from the position that the act is inherently immoral and unacceptable under any circumstances, to a regard for suicide as a sacrosanct right of anyone who believes they have rationally and conscientiously come to the decision to end their own lives, even if they are young and healthy.
Opponents to suicide include philosophers such as Augustine of Hippo, Thomas Aquinas,[303] Immanuel Kant[304] and, arguably, John Stuart Mill – Mill's focus on the importance of liberty and autonomy meant that he rejected choices which would prevent a person from making future autonomous decisions.[305] Others view suicide as a legitimate matter of personal choice. Supporters of this position maintain that no one should be forced to suffer against their will, particularly from conditions such as incurable disease, mental illness, and old age, with no possibility of improvement. They reject the belief that suicide is always irrational, arguing instead that it can be a valid last resort for those enduring major pain or trauma.[306] A stronger stance would argue that people should be allowed to autonomously choose to die regardless of whether they are suffering. Notable supporters of this school of thought include Scottish empiricist David Hume,[303] who accepted suicide so long as it did not harm or violate a duty to God, other people, or the self,[264] and American bioethicist Jacob Appel.[272][307]
Adverse attitudes
[edit]Society may have negative attitudes towards suicide, which can lead to suicidal people experiencing discrimination, stigmatization, exclusion, pathologization, and incarceration. They may be hospitalized or drugged without their consent, have difficulties in finding jobs or housing, and have their parental rights revoked. Suicide is not seen as a positive human right or a logical decision given circumstances. Suicidal people are not seen as having potentially valuable messages to convey.[308][309][310]
Advocacy
[edit]
Advocacy of suicide has occurred in many cultures and subcultures. The Japanese military during World War II encouraged and glorified kamikaze attacks, which were suicide attacks by military aviators from the Empire of Japan against Allied naval vessels in the closing stages of the Pacific Theater of World War II. Japanese society as a whole has been described as "suicide-tolerant"[312] (see Suicide in Japan).
Internet searches for information on suicide return webpages that, in a 2008 study, about 50% of the time provide information on suicide methods. A similar study found that 11% of sites encouraged suicide attempts.[313] There is some concern that such sites may push those already predisposed to attempt suicide. Some people form suicide pacts online, either with pre-existing friends or people they have recently encountered in chat rooms or message boards. The Internet, however, may also help prevent suicide by providing a social group for those who are isolated.[314]
Locations
[edit]Some landmarks have become known for high levels of suicide attempts.[315] These include China's Nanjing Yangtze River Bridge,[316] San Francisco's Golden Gate Bridge, Japan's Aokigahara Forest,[317] England's Beachy Head,[315] and Toronto's Bloor Street Viaduct.[318] As of 2010[update], the Golden Gate Bridge has had more than 1,300 suicides by jumping since its construction in 1937.[319] Many locations where suicide is common have constructed barriers to prevent it;[320] this includes the Luminous Veil in Toronto,[318] the Eiffel Tower in Paris, the West Gate Bridge in Melbourne, and Empire State Building in New York City.[320] They generally appear to be effective.[321]
Notable cases
[edit]An example of mass suicide is the 1978 Jonestown mass murder/suicide in which 909 members of the Peoples Temple, an American new religious movement led by Jim Jones, ended their lives by drinking grape Flavor Aid laced with cyanide and various prescription drugs.[322][323][324]
Thousands of Japanese civilians took their own lives in the last days of the Battle of Saipan in 1944, some jumping from "Suicide Cliff" and "Banzai Cliff".[325] The 1981 Irish hunger strikes, led by Bobby Sands, resulted in 10 deaths. The cause of death was recorded by the coroner as "starvation, self-imposed" rather than suicide; this was modified to simply "starvation" on the death certificates after protest from the dead strikers' families.[326] During World War II, Erwin Rommel was found to have foreknowledge of the 20 July plot on Hitler's life; he was threatened with public trial, execution, and reprisals on his family unless he killed himself.[327]
Other species
[edit]As suicide requires a wilful attempt to die, some feel it therefore cannot be said to occur in non-human animals.[258] Suicidal behavior has been observed in Salmonella seeking to overcome competing bacteria by triggering an immune system response against them.[328] Suicidal defenses by workers are also seen in the Brazilian ant Forelius pusillus, where a small group of ants leaves the security of the nest after sealing the entrance from the outside each evening.[329]
Pea aphids, when threatened by a ladybug, can explode themselves, scattering and protecting their brethren and sometimes even killing the ladybug; this form of suicidal altruism is known as autothysis.[330] Some species of termites (for example Globitermes sulphureus)[331] have soldiers that explode, covering their enemies with sticky goo.[332][331]
There have been anecdotal reports of dogs, horses, and dolphins killing themselves,[333] but little scientific study has been done regarding animal suicide.[334] Animal suicide is usually put down to romantic human interpretation and is not generally thought to be intentional. Some of the reasons animals are thought to unintentionally kill themselves include: psychological stress, infection by certain parasites or fungi, or disruption of a long-held social tie, such as the ending of a long association with an owner and thus not accepting food from another individual.[335]
See also
[edit]References
[edit]- ^ a b Preventing suicide: a global imperative. WHO. 2014. pp. 7, 20, 40. ISBN 978-92-4-156477-9.
- ^ a b c d e f g h "Suicide Fact sheet N°398". WHO. April 2016. Archived from the original on 4 March 2016. Retrieved 3 March 2016.
- ^ a b c d e Hawton K, van Heeringen K (April 2009). "Suicide". Lancet. 373 (9672): 1372–81. doi:10.1016/S0140-6736(09)60372-X. PMID 19376453. S2CID 208790312.
- ^ De La Vega D, Giner L, Courtet P (March 2018). "Suicidality in Subjects With Anxiety or Obsessive-Compulsive and Related Disorders: Recent Advances". Current Psychiatry Reports. 20 (4) 26. doi:10.1007/s11920-018-0885-z. ISSN 1523-3812. PMID 29594718. S2CID 4549236.
- ^ a b Richa S, Fahed M, Khoury E, Mishara B (2014). "Suicide in autism spectrum disorders". Archives of Suicide Research. 18 (4): 327–39. doi:10.1080/13811118.2013.824834. PMID 24713024. S2CID 25741716.
- ^ a b c d e f g h i j k l m n o Värnik P (March 2012). "Suicide in the world". International Journal of Environmental Research and Public Health. 9 (3): 760–71. doi:10.3390/ijerph9030760. PMC 3367275. PMID 22690161.
- ^ "Suicide across the world (2016)". World Health Organization. 27 September 2019. Archived from the original on 1 July 2004. Retrieved 16 October 2019.
- ^ a b Fazel S, Runeson B (January 2020). "Suicide". New England Journal of Medicine. 382 (3): 266–74. doi:10.1056/NEJMra1902944. PMC 7116087. PMID 31940700. S2CID 210332277.
- ^ a b Stedman's Medical Dictionary (28th ed.). Philadelphia: Lippincott Williams & Wilkins. 2006. ISBN 978-0-7817-3390-8.
- ^ a b Dodds TJ (March 2017). "Prescribed Benzodiazepines and Suicide Risk: A Review of the Literature". The Primary Care Companion for CNS Disorders. 19 (2). doi:10.4088/PCC.16r02037. PMID 28257172.
- ^ Bottino SM, Bottino CM, Regina CG, Correia AV, Ribeiro WS (March 2015). "Cyberbullying and adolescent mental health: systematic review". Cadernos de Saude Publica. 31 (3): 463–75. doi:10.1590/0102-311x00036114. PMID 25859714.
- ^ "Suicide rates rising across the U.S." CDC Online Newsroom. 11 April 2019. Retrieved 19 September 2019.
Relationship problems or loss, substance misuse; physical health problems; and job, money, legal or housing stress often contributed to risk for suicide.
- ^ Preventing Suicide A Resource for Media Professionals (PDF). World Health Organization. Department of Mental Health and Substance Abuse. 2008. ISBN 978-92-4-159707-4.
- ^ DeCou CR, Comtois KA, Landes SJ (January 2019). "Dialectical Behavior Therapy Is Effective for the Treatment of Suicidal Behavior: A Meta-Analysis". Behav Ther. 50 (1): 60–72. doi:10.1016/j.beth.2018.03.009. PMID 30661567. S2CID 58666001.
- ^ a b Sakinofsky I (June 2007). "The current evidence base for the clinical care of suicidal patients: strengths and weaknesses". Canadian Journal of Psychiatry. 52 (6 Suppl 1): 7S – 20S. doi:10.1177/07067437070526S102. PMID 17824349.
Other suicide prevention strategies that have been considered are crisis centers and hotlines, method control, and media education... There is minimal research on these strategies. Even though crisis centers and hotlines are used by suicidal youth, information about their impact on suicidal behavior is lacking.
- ^ a b c d e f g Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, et al. (July 2016). "Suicide prevention strategies revisited: 10-year systematic review". The Lancet. Psychiatry. 3 (7): 646–59. doi:10.1016/S2215-0366(16)30030-X. hdl:1854/LU-8509936. PMID 27289303.
Other approaches that need further investigation include gatekeeper training, education of physicians, and internet and helpline support.
- ^ Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.. For the number 828,000, see Table 5, line "Self-harm", second column (year 2015)
- ^ a b Naghavi M, Wang H, Lozano R, Davis A, Liang X, Zhou M, et al. (GBD 2013 Mortality and Causes of Death Collaborators) (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.. For the number 712,000, see Table 2, line "Self-harm", first column (year 1990)
- ^ a b c d e f g h i j k l m n o p q r s t u v Chang B, Gitlin D, Patel R (September 2011). "The depressed patient and suicidal patient in the emergency department: evidence-based management and treatment strategies". Emergency Medicine Practice. 13 (9): 1–23, quiz 23–4. PMID 22164363.
- ^ "Suicide rates per (100 000 population)". World Health Organization.
- ^ Bertolote JM, Fleischmann A (October 2002). "Suicide and psychiatric diagnosis: a worldwide perspective". World Psychiatry. 1 (3): 181–5. PMC 1489848. PMID 16946849.
- ^ a b c d e f g h i j k Yip PS, Caine E, Yousuf S, Chang SS, Wu KC, Chen YY (June 2012). "Means restriction for suicide prevention". Lancet. 379 (9834): 2393–9. doi:10.1016/S0140-6736(12)60521-2. PMC 6191653. PMID 22726520.
- ^ Montreal JE (16 October 2024). "'It's social murder' — is Canada's assisted dying a model or a warning?". www.thetimes.com.
- ^ Sydney Bruno Waterfield, Brussels | Josie Ensor, New York | Bernard Lagan (16 October 2024). "Where is assisted dying legal? How the rules worldwide compare". www.thetimes.com.
{{cite web}}: CS1 maint: multiple names: authors list (link) CS1 maint: numeric names: authors list (link) - ^ Tomer A (2013). Existential and Spiritual Issues in Death Attitudes. Psychology Press. p. 282. ISBN 978-1-136-67690-1.
- ^ Ritzer G, Stepnisky J, eds. (2011). The Wiley-Blackwell companion to major social theorists. Malden, MA: Wiley-Blackwell. p. 65. ISBN 978-1-4443-9660-7.
- ^ God, Religion, Science, Nature, Culture, and Morality. Archway Publishing. 2014. p. 254. ISBN 978-1-4808-1124-9.
- ^ Colt GH (1992). The enigma of suicide (1st Touchstone ed.). New York: Simon & Schuster. p. 139. ISBN 978-0-671-76071-7.
- ^ White T (2010). Working with suicidal individuals: a guide to providing understanding, assessment and support. London: Jessica Kingsley Publishers. p. 12. ISBN 978-1-84905-115-6.
- ^ a b c d e f Lester D (2006). "Suicide and islam". Archives of Suicide Research. 10 (1): 77–97. doi:10.1080/13811110500318489. PMID 16287698. S2CID 35754641.
- ^ Aggarwal N (2009). "Rethinking suicide bombing". Crisis. 30 (2): 94–7. doi:10.1027/0227-5910.30.2.94. PMID 19525169. S2CID 35560934.
- ^ Vaughan M. "The 'discovery' of suicide in Africa". BBC. Retrieved 16 June 2020.
- ^ "Suicide". World Health Organization. Retrieved 16 June 2020.
- ^ Issues in Law & Medicine, Volume 3. National Legal Center for the Medically Dependent & Disabled, Incorporated, and the Horatio R. Storer Foundation, Incorporated. 1987. p. 39.
- ^ a b Krug E (2002). World Report on Violence and Health. Vol. 1. Genève: World Health Organization. p. 185. ISBN 978-92-4-154561-7.
- ^ a b c d e f g h i j Turecki G, Brent DA (March 2016). "Suicide and suicidal behaviour". Lancet. 387 (10024): 1227–39. doi:10.1016/S0140-6736(15)00234-2. PMC 5319859. PMID 26385066.
- ^ a b Gullota TP, Bloom M (2002). Encyclopedia of Primary Prevention and Health Promotion. New York: Kluwer Academic/Plenum. p. 1112. ISBN 978-0-306-47296-1.
- ^ "suicidality". APA Dictionary of Psychology. Washington, DC: American Psychological Association. n.d. Retrieved 3 August 2023.
- ^ Lester D (2009). "Extended suicide". In Wasserman D, Wasserman C (eds.). Oxford textbook of suicidology. Oxford: Oxford University Press. pp. 134–36. doi:10.1093/med/9780198570059.003.0022. ISBN 978-0-19-857005-9.
- ^ Stein G, Wilkinson G (2007). Seminars in general adult psychiatry (2nd ed.). London: Gaskell. p. 144. ISBN 978-1-904671-44-2.
- ^ Olson R (2011). "Suicide and Language". Centre for Suicide Prevention. InfoExchange (3): 4. Archived from the original on 6 May 2012. Retrieved 15 May 2013.
- ^ Beaton S, Forster P, Maple M (February 2013). "Suicide and Language: Why we Shouldn't Use the 'C' Word". In Psych. 35 (1): 30–31. Archived from the original on 15 August 2014.
- ^ Inclusive Language Guidelines (PDF). Washington, D.C.: American Psychological Association. p. 19. Retrieved 13 February 2022.
- ^ Beck AT, Resnik HL, Lettieri DJ, eds. (1974). "Development of suicidal intent scales". The prediction of suicide. Bowie, MD: Charles Press. p. 41. ISBN 978-0-913486-13-9.
- ^ "Recommendations for Reporting on Suicide" (PDF). National Institute of Mental Health. 2001. Archived from the original (PDF) on 27 April 2013. Retrieved 15 May 2013.
- ^ "Reporting Suicide and Self Harm". Time To Change. 2008. Archived from the original on 14 January 2016. Retrieved 2 January 2016.
- ^ @apstylebook (18 May 2017). "Avoid "committed suicide" except in direct quotes from authorities. Alternatives: "killed himself," "took her own life," "died by suicide."" (Tweet) – via Twitter.
- ^ "Guardian and Observer style guide: S". The Guardian. 4 May 2021.
- ^ Ravitz J (11 June 2018). "The words to say -- and not to say -- about suicide". CNN.
- ^ Ball PB (2005). "The Power of words". Canadian Association of Suicide Prevention. Archived from the original on 13 May 2013. Retrieved 16 May 2013.
- ^ Pjevac M, Pregelj P (October 2012). "Neurobiology of suicidal behaviour". Psychiatria Danubina. 24 (Suppl 3): S336-41. PMID 23114813.
- ^ Sher L (2011). "The role of brain-derived neurotrophic factor in the pathophysiology of adolescent suicidal behavior". International Journal of Adolescent Medicine and Health. 23 (3): 181–5. doi:10.1515/ijamh.2011.041. PMID 22191181. S2CID 25684743.
- ^ Sher L (May 2011). "Brain-derived neurotrophic factor and suicidal behavior". QJM. 104 (5): 455–8. doi:10.1093/qjmed/hcq207. PMID 21051476.
- ^ Yanowitch R, Coccaro EF (2011). "The neurochemistry of human aggression". Aggression. Advances in Genetics. Vol. 75. Elsevier. pp. 151–69. doi:10.1016/b978-0-12-380858-5.00005-8. ISBN 978-0-12-380858-5. PMID 22078480.
- ^ a b Dwivedi Y (2012). The neurobiological basis of suicide. Boca Raton, FL: Taylor & Francis/CRC Press. p. 166. ISBN 978-1-4398-3881-5.
- ^ Stein G, Wilkinson G (2007). Seminars in general adult psychiatry (2nd ed.). London: Gaskell. p. 145. ISBN 978-1-904671-44-2.
- ^ Autry AE, Monteggia LM (November 2009). "Epigenetics in suicide and depression". Biological Psychiatry. 66 (9): 812–3. doi:10.1016/j.biopsych.2009.08.033. PMC 2770810. PMID 19833253.
- ^ Petrosky E, Ertl A, Sheats KJ, Wilson R, Betz CJ, Blair JM (December 2020). "Surveillance for Violent Deaths - National Violent Death Reporting System, 34 States, Four California Counties, the District of Columbia, and Puerto Rico, 2017". MMWR. Surveillance Summaries. 69 (8): 1–37. doi:10.15585/mmwr.ss6908a1. PMC 7713989. PMID 33270620.
- ^ a b c d Hawton K, Saunders KE, O'Connor RC (June 2012). "Self-harm and suicide in adolescents". Lancet. 379 (9834): 2373–82. doi:10.1016/S0140-6736(12)60322-5. PMID 22726518. S2CID 151486181.
- ^ a b "Suicide Risk and Protective Factors|Suicide|Violence Prevention|Injury Center|CDC". www.cdc.gov. 25 April 2019. Retrieved 29 July 2019.
- ^ a b c d e f g h i Vijayakumar L, Kumar MS, Vijayakumar V (May 2011). "Substance use and suicide". Current Opinion in Psychiatry. 24 (3): 197–202. doi:10.1097/YCO.0b013e3283459242. PMID 21430536. S2CID 206143129.
- ^ Simpson G, Tate R (December 2007). "Suicidality in people surviving a traumatic brain injury: prevalence, risk factors and implications for clinical management". Brain Injury. 21 (13–14): 1335–51. doi:10.1080/02699050701785542. PMID 18066936. S2CID 24562104.
- ^ Miller M, Azrael D, Barber C (April 2012). "Suicide mortality in the United States: the importance of attending to method in understanding population-level disparities in the burden of suicide". Annual Review of Public Health. 33: 393–408. doi:10.1146/annurev-publhealth-031811-124636. PMID 22224886.
- ^ Xiao Y, Meng Y, Brown TT, Tsai AC, Snowden LR, Chow JC, Pathak J, Mann JJ (12 May 2025). "Machine learning to investigate policy-relevant social determinants of health and suicide rates in the United States". Nature Mental Health. 3 (6): 675–684. doi:10.1038/s44220-025-00424-4. ISSN 2731-6076.
- ^ Qin P, Agerbo E, Mortensen PB (April 2003). "Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: a national register-based study of all suicides in Denmark, 1981–1997". The American Journal of Psychiatry. 160 (4): 765–72. doi:10.1176/appi.ajp.160.4.765. hdl:10818/17040. PMID 12668367. S2CID 25133734.
- ^ Centers for Disease Control Prevention (CDC) (May 2013). "Suicide among adults aged 35-64 years--United States, 1999-2010". MMWR. Morbidity and Mortality Weekly Report. 62 (17): 321–5. PMC 4604925. PMID 23636024.
- ^ a b Brent DA, Melhem N (June 2008). "Familial transmission of suicidal behavior". The Psychiatric Clinics of North America. 31 (2): 157–77. doi:10.1016/j.psc.2008.02.001. PMC 2440417. PMID 18439442.
- ^ a b c d "Suicide Risk and Protective Factors|Suicide|Violence Prevention|Injury Center|CDC". www.cdc.gov. 25 April 2019. Retrieved 17 June 2019.
- ^ May AM, Klonsky ED (2016). "What Distinguishes Suicide Attempters From Suicide Ideators? A Meta-Analysis of Potential Factors". Clinical Psychology: Science and Practice. 23 (1): 5–20. doi:10.1111/cpsp.12136. S2CID 35079333.
- ^ Klonsky ED, May AM (February 2014). "Differentiating suicide attempters from suicide ideators: a critical frontier for suicidology research". Suicide & Life-Threatening Behavior. 44 (1): 1–5. doi:10.1111/sltb.12068. PMID 24313594.
- ^ Klonsky ED, Qiu T, Saffer BY (January 2017). "Recent advances in differentiating suicide attempters from suicide ideators". Current Opinion in Psychiatry. 30 (1): 15–20. doi:10.1097/YCO.0000000000000294. PMID 27798483. S2CID 21053071.
- ^ Lai MC, Kassee C, Besney R, Bonato S, Hull L, Mandy W, Szatmari P, Ameis SH (2019). "Prevalence of co-occurring mental health diagnoses in the autism population: a systematic review and meta-analysis" (PDF). The Lancet Psychiatry. 6 (10). Elsevier BV: 819–829. doi:10.1016/s2215-0366(19)30289-5. ISSN 2215-0366. PMID 31447415. Retrieved 8 May 2025.
- ^ "Social difficulties in autism spectrum disorder". KU SOE. 22 May 2023. Retrieved 8 May 2025.
- ^ Zahid S, Upthegrove R (July 2017). "Suicidality in Autistic Spectrum Disorders" (PDF). Crisis. 38 (4): 237–246. doi:10.1027/0227-5910/a000458. PMID 28468556. S2CID 10644601.
- ^ Blanchard A, Chihuri S, DiGuiseppi CG, Li G (1 October 2021). "Risk of Self-harm in Children and Adults With Autism Spectrum Disorder: A Systematic Review and Meta-analysis". JAMA Network Open. 4 (10): e2130272. doi:10.1001/jamanetworkopen.2021.30272. ISSN 2574-3805. PMC 8527356. PMID 34665237.
- ^ Santomauro DF, Hedley D, Sahin E, Brugha TS, Naghavi M, Vos T, Whiteford HA, Ferrari AJ, Stokes MA (November 2024). "The global burden of suicide mortality among people on the autism spectrum: A systematic review, meta-analysis, and extension of estimates from the Global Burden of Disease Study 2021". Psychiatry Research. 341 116150. doi:10.1016/j.psychres.2024.116150. ISSN 1872-7123. PMID 39197224.
- ^ Newell, V., Phillips, L., Jones, C. et al. A systematic review and meta-analysis of suicidality in autistic and possibly autistic people without co-occurring intellectual disability. Molecular Autism 14, 12 (2023). https://doi.org/10.1186/s13229-023-00544-7
- ^ a b Cornelius SL, Berry T, Goodrich AJ, Shiner B, Riblet NB (23 July 2021). "The Effect of Meteorological, Pollution, and Geographic Exposures on Death by Suicide: A Scoping Review". International Journal of Environmental Research and Public Health. 18 (15): 7809. doi:10.3390/ijerph18157809. ISSN 1660-4601. PMC 8345465. PMID 34360101.
- ^ Go TH, Kim MH, Choi YY, Han J, Kim C, Kang DR (3 January 2024). "The short-term effect of ambient particulate matter on suicide death". Environmental Health (meta-analysis). 23 (1). Springer Science and Business Media LLC: 3. Bibcode:2024EnvHe..23....3G. doi:10.1186/s12940-023-01042-2. ISSN 1476-069X. PMC 10763266. PMID 38169380.
- ^ Braithwaite I, Zhang S, Kirkbride JB, Osborn DP, Hayes JF (December 2019). "Air Pollution (Particulate Matter) Exposure and Associations with Depression, Anxiety, Bipolar, Psychosis and Suicide Risk: A Systematic Review and Meta-Analysis". Environmental Health Perspectives. 127 (12) 126002. Bibcode:2019EnvHP.127l6002B. doi:10.1289/EHP4595. PMC 6957283. PMID 31850801.
- ^ Carley S, Hamilton M (November 2004). "Best evidence topic report. Suicide at christmas". Emergency Medicine Journal. 21 (6): 716–7. doi:10.1136/emj.2004.019703. PMC 1726490. PMID 15496706.
- ^ Williams A, While D, Windfuhr K, Bickley H, Hunt IM, Shaw J, et al. (2011). "Birthday blues: examining the association between birthday and suicide in a national sample". Crisis. 32 (3): 134–42. doi:10.1027/0227-5910/a000067. PMID 21616762.
- ^ a b c d e f g h i j O'Connor RC, Nock MK (June 2014). "The psychology of suicidal behaviour". The Lancet. Psychiatry. 1 (1): 73–85. doi:10.1016/S2215-0366(14)70222-6. PMID 26360404.
- ^ a b Joiner TE, Brown JS, Wingate LR (2005). "The psychology and neurobiology of suicidal behavior". Annual Review of Psychology. 56: 287–314. doi:10.1146/annurev.psych.56.091103.070320. PMID 15709937. S2CID 42500507.
- ^ Confer JC, Easton JA, Fleischman DS, Goetz CD, Lewis DM, Perilloux C, Buss DM (1 January 2010). "Evolutionary psychology. Controversies, questions, prospects, and limitations". The American Psychologist. 65 (2): 110–26. CiteSeerX 10.1.1.601.8691. doi:10.1037/a0018413. PMID 20141266.
- ^ a b c Bohanna I, Wang X (2012). "Media guidelines for the responsible reporting of suicide: a review of effectiveness". Crisis. 33 (4): 190–8. doi:10.1027/0227-5910/a000137. PMID 22713977. S2CID 1262883.
- ^ Gilliland B, James R (8 May 2012). Crisis intervention strategies (7th ed.). Belmont, CA: Brooks/Cole. p. 215. ISBN 978-1-111-18677-7. Archived from the original on 3 October 2015.
- ^ Exeter DJ, Boyle PJ (August 2007). "Does young adult suicide cluster geographically in Scotland?". Journal of Epidemiology and Community Health. 61 (8): 731–6. doi:10.1136/jech.2006.052365. PMC 2653005. PMID 17630375.
- ^ Gould MS, Wallenstein S, Davidson L (1989). "Suicide clusters: a critical review". Suicide & Life-Threatening Behavior. 19 (1): 17–29. doi:10.1111/j.1943-278X.1989.tb00363.x. PMID 2652386.
- ^ a b Sisask M, Värnik A (January 2012). "Media roles in suicide prevention: a systematic review". International Journal of Environmental Research and Public Health. 9 (1): 123–38. doi:10.3390/ijerph9010123. PMC 3315075. PMID 22470283.
- ^ Stack S (April 2005). "Suicide in the media: a quantitative review of studies based on non-fictional stories". Suicide and Life-Threatening Behavior. 35 (2): 121–33. doi:10.1521/suli.35.2.121.62877. PMID 15843330. S2CID 21353878.
- ^ Pirkis J (July 2009). "Suicide and the media". Psychiatry. 8 (7): 269–71. doi:10.1016/j.mppsy.2009.04.009.
- ^ Shrivastava A, Kimbrell M, Lester D (2012). Suicide from a global perspective: psychosocial approaches. New York: Nova Science Publishers. pp. 115–18. ISBN 978-1-61470-965-7.
- ^ Mok K, Jorm AF, Pirkis J (August 2015). "Suicide-related Internet use: A review". The Australian and New Zealand Journal of Psychiatry. 49 (8): 697–705. doi:10.1177/0004867415569797. hdl:11343/58519. PMID 25698810. S2CID 26744237.
- ^ Scalvini M, Rigamonti F (October 2017). "Why we must defend suicide in fiction". BMJ. 359 j4743. doi:10.1136/bmj.j4743. PMID 29046321. S2CID 22599053.
- ^ Scalvini M (18 June 2020). "13 Reasons Why: can a TV show about suicide be 'dangerous'? What are the moral obligations of a producer?". Media, Culture & Society. 42 (7–8): 1564–1574. doi:10.1177/0163443720932502. hdl:1765/128013. ISSN 0163-4437.
- ^ a b c d e f g Tintinalli, Judith E. (2010). Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine (Tintinalli)). New York: McGraw-Hill Companies. pp. 1940–46. ISBN 978-0-07-148480-0.
- ^ Manthorpe J, Iliffe S (December 2010). "Suicide in later life: public health and practitioner perspectives". International Journal of Geriatric Psychiatry. 25 (12): 1230–1238. doi:10.1002/gps.2473. PMID 20104515. S2CID 23697880.
- ^ Simpson GK, Tate RL (August 2007). "Preventing suicide after traumatic brain injury: implications for general practice". The Medical Journal of Australia. 187 (4): 229–232. doi:10.5694/j.1326-5377.2007.tb01206.x. PMID 17708726. S2CID 44454339. Archived from the original on 10 September 2011.
- ^ a b Anguiano L, Mayer DK, Piven ML, Rosenstein D (July–August 2012). "A literature review of suicide in cancer patients". Cancer Nursing. 35 (4): E14 – E26. doi:10.1097/NCC.0b013e31822fc76c. PMID 21946906. S2CID 45874503.
- ^ Chu L, Elliott M, Stein E, Jason LA (May 2021). "Identifying and Managing Suicidality in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Healthcare. 9 (6): 629. doi:10.3390/healthcare9060629. PMC 8227525. PMID 34070367.
- ^ Yip PS (2008). Suicide in Asia: causes and prevention. Hong Kong: Hong Kong University Press. p. 11. ISBN 978-962-209-943-2.
- ^ Ribeiro JD, Pease JL, Gutierrez PM, Silva C, Bernert RA, Rudd MD, Joiner TE (February 2012). "Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military". Journal of Affective Disorders. 136 (3): 743–50. doi:10.1016/j.jad.2011.09.049. PMID 22032872.
- ^ Bernert RA, Joiner TE, Cukrowicz KC, Schmidt NB, Krakow B (September 2005). "Suicidality and sleep disturbances". Sleep. 28 (9): 1135–41. doi:10.1093/sleep/28.9.1135. PMID 16268383.
- ^ a b University of Manchester Centre for Mental Health and Risk. "The National Confidential Inquiry into Suicide and Homicide by People with Mental Illness" (PDF). Archived from the original (PDF) on 14 July 2012. Retrieved 25 July 2012.
- ^ Stone DM, Simon TR, Fowler KA, Kegler SR, Yuan K, Holland KM, et al. (June 2018). "Vital Signs: Trends in State Suicide Rates – United States, 1999–2016 and Circumstances Contributing to Suicide – 27 States, 2015". MMWR. Morbidity and Mortality Weekly Report. 67 (22): 617–624. doi:10.15585/mmwr.mm6722a1. PMC 5991813. PMID 29879094.
- ^ Arsenault-Lapierre G, Kim C, Turecki G (November 2004). "Psychiatric diagnoses in 3275 suicides: a meta-analysis". BMC Psychiatry. 4 (1) 37. doi:10.1186/1471-244X-4-37. PMC 534107. PMID 15527502.
- ^ a b Bostwick JM, Pankratz VS (December 2000). "Affective disorders and suicide risk: a reexamination". The American Journal of Psychiatry. 157 (12): 1925–32. doi:10.1176/appi.ajp.157.12.1925. PMID 11097952.
- ^ a b c d Kutcher S, Chehil S (2012). Suicide Risk Management A Manual for Health Professionals (2nd ed.). Chicester: John Wiley & Sons. pp. 30–33. ISBN 978-1-119-95311-1.
- ^ Pompili M, Girardi P, Ruberto A, Tatarelli R (2005). "Suicide in borderline personality disorder: a meta-analysis". Nordic Journal of Psychiatry. 59 (5): 319–24. doi:10.1080/08039480500320025. PMID 16757458. S2CID 27142497.
- ^ Bertolote JM, Fleischmann A, De Leo D, Wasserman D (2004). "Psychiatric diagnoses and suicide: revisiting the evidence". Crisis. 25 (4): 147–55. doi:10.1027/0227-5910.25.4.147. PMID 15580849. S2CID 13331602.
- ^ Angelakis I, Gooding P, Tarrier N, Panagioti M (July 2015). "Suicidality in obsessive compulsive disorder (OCD): a systematic review and meta-analysis". Clinical Psychology Review. 39: 1–15. doi:10.1016/j.cpr.2015.03.002. PMID 25875222.
- ^ Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M (2004). "Borderline personality disorder". Lancet. 364 (9432): 453–461. doi:10.1016/S0140-6736(04)16770-6. PMID 15288745. S2CID 54280127.
Between 40% and 65% of individuals who commit suicide meet criteria for a personality disorder, with borderline personality disorder being the most commonly associated.
- ^ van Os J, Kapur S (August 2009). "Schizophrenia" (PDF). Lancet. 374 (9690): 635–645. doi:10.1016/S0140-6736(09)60995-8. PMID 19700006. S2CID 208792724. Archived from the original (PDF) on 23 June 2013. Retrieved 22 January 2013.
- ^ Cheung A, Zwickl S (23 March 2021). "Why have nearly half of transgender Australians attempted suicide?". Pursuit. Melbourne, Australia: University of Melbourne. Retrieved 26 August 2022.
- ^ "Transgender people and suicide". Centre for Suicide Prevention. Retrieved 26 August 2022.
- ^ Biggs M (February 2022). "Suicide by Clinic-Referred Transgender Adolescents in the United Kingdom". Archives of Sexual Behavior. 51 (2): 685–690. doi:10.1007/s10508-022-02287-7. PMC 8888486. PMID 35043256.
- ^ "Suicide risk in transgender and gender diverse people". National Elf Service. 13 July 2021. Retrieved 26 August 2022.
- ^ "Study Shows Shocking Rates of Attempted Suicide Among Trans Teens". Human Rights Campaign. 12 September 2018. Retrieved 26 August 2022.
- ^ a b Pirkis J, Burgess P (December 1998). "Suicide and recency of health care contacts. A systematic review". The British Journal of Psychiatry. 173 (6): 462–74. doi:10.1192/bjp.173.6.462. PMID 9926074. S2CID 43144463.
- ^ Luoma JB, Martin CE, Pearson JL (June 2002). "Contact with mental health and primary care providers before suicide: a review of the evidence". The American Journal of Psychiatry. 159 (6): 909–16. doi:10.1176/appi.ajp.159.6.909. PMC 5072576. PMID 12042175.
- ^ Sharma T, Guski LS, Freund N, Gøtzsche PC (January 2016). "Suicidality and aggression during antidepressant treatment: systematic review and meta-analyses based on clinical study reports". BMJ. 352: i65. doi:10.1136/bmj.i65. PMC 4729837. PMID 26819231.
- ^ a b Australian Institute of Health and Welfare (29 September 2021). "Serving and ex-serving Australian Defence Force members who have served since 1985: suicide monitoring 2001 to 2019". aihw.gov.au. Archived from the original on 26 August 2022. Retrieved 26 August 2022.
- ^ Department of National Defence (11 May 2022). "2021 Report on Suicide Mortality in the Canadian Armed Forces (1995 to 2020)". www.canada.ca. Archived from the original on 30 August 2022. Retrieved 30 August 2022.
- ^ Simkus K, Hall A, Heber A, VanTil L (18 June 2020). "Veteran Suicide Mortality Study: Follow-up period from 1976 to 2014". Ottawa, ON: Veterans Affairs Canada. Archived from the original on 30 August 2022. Retrieved 30 August 2022.
- ^ US Department of Veterans Affairs (Office of Mental Health and Suicide Prevention) (September 2021). "2001-2019 National Suicide Data Appendix". va.gov. Retrieved 30 August 2022.
- ^ Kapur N, While D, Blatchley N, Bray I, Harrison K (March 2009). Hotopf M (ed.). "Suicide after leaving the UK armed forces--a cohort study". PLOS Medicine. 6 (3) e26. doi:10.1371/journal.pmed.1000026. PMC 2650723. PMID 19260757.
- ^ Jones M, Jones N, Burdett H, Bergman BP, Fear NT, Wessely S, Rona RJ (April 2021). "Do Junior Entrants to the UK Armed Forces have worse outcomes than Standard Entrants?" (PDF). BMJ Military Health. 169 (3): 218–224. doi:10.1136/bmjmilitary-2021-001787. PMID 33879526. S2CID 233313427. Archived from the original (PDF) on 8 October 2022. Retrieved 8 September 2022.
- ^ a b Rozanov V, Carli V (July 2012). "Suicide among war veterans". International Journal of Environmental Research and Public Health. 9 (7): 2504–19. doi:10.3390/ijerph9072504. PMC 3407917. PMID 22851956.
- ^ a b c Owens D, Horrocks J, House A (2002). "Fatal and non-fatal repetition of self-harm: Systematic review". British Journal of Psychiatry. 181 (3): 193–199. doi:10.1192/bjp.181.3.193. ISSN 0007-1250. PMID 12204922.
- ^ a b c Parra-Uribe I, Blasco-Fontecilla H, Garcia-Parés G, Martínez-Naval L, Valero-Coppin O, Cebrià-Meca A, Oquendo MA, Palao-Vidal D (2017). "Risk of re-attempts and suicide death after a suicide attempt: A survival analysis". BMC Psychiatry. 17 (1): 163. doi:10.1186/s12888-017-1317-z. ISSN 1471-244X. PMC 5415954. PMID 28472923.
- ^ a b Bostwick JM, Pabbati C, Geske JR, McKean AJ (1 November 2016). "Suicide Attempt as a Risk Factor for Completed Suicide: Even More Lethal Than We Knew". American Journal of Psychiatry. 173 (11): 1094–1100. doi:10.1176/appi.ajp.2016.15070854. ISSN 0002-953X. PMC 5510596. PMID 27523496.
- ^ Suominen K, Isometsä E, Ostamo A, Lönnqvist J (20 April 2004). "Level of suicidal intent predicts overall mortality and suicide after attempted suicide: a 12-year follow-up study". BMC Psychiatry. 4 (1): 11. doi:10.1186/1471-244X-4-11. ISSN 1471-244X. PMC 415554. PMID 15099401.
- ^ "Attempters' Longterm Survival". Means Matter. 11 September 2012. Retrieved 1 November 2024.
- ^ Bostwick JM, Rackley SJ (June 2007). "Completed suicide in medical/surgical patients: who is at risk?". Current Psychiatry Reports. 9 (3): 242–6. doi:10.1007/s11920-007-0026-6. PMID 17521522. S2CID 7093281.
- ^ Van Orden K, Conwell Y (June 2011). "Suicides in late life". Current Psychiatry Reports. 13 (3): 234–41. doi:10.1007/s11920-011-0193-3. PMC 3085020. PMID 21369952.
- ^ Turecki G (December 2013). "Polyamines and suicide risk". Molecular Psychiatry. 18 (12): 1242–3. doi:10.1038/mp.2013.153. PMC 5293538. PMID 24166408.
- ^ Nemeroff CB, Owens MJ, Bissette G, Andorn AC, Stanley M (June 1988). "Reduced corticotropin releasing factor binding sites in the frontal cortex of suicide victims". Archives of General Psychiatry. 45 (6): 577–9. doi:10.1001/archpsyc.1988.01800300075009. PMID 2837159. S2CID 23574459.
- ^ a b Stark CR, Riordan V, O'Connor R (2011). "A conceptual model of suicide in rural areas". Rural and Remote Health. 11 (2): 1622. PMID 21702640.
- ^ Daly M (September 2012). "Relative Status and Well-Being: Evidence from U.S. Suicide Deaths" (PDF). Federal Reserve Bank of San Francisco, Working Paper Series: 01–52. doi:10.24148/wp2012-16. Archived (PDF) from the original on 19 October 2012.
- ^ Lerner G (5 January 2010). "Activist: Farmer suicides in India linked to debt, globalization". CNN World. Archived from the original on 16 January 2013. Retrieved 13 February 2013.
- ^ Law S, Liu P (February 2008). "Suicide in China: unique demographic patterns and relationship to depressive disorder". Current Psychiatry Reports. 10 (1): 80–6. doi:10.1007/s11920-008-0014-5. PMID 18269899. S2CID 24474367.
- ^ a b Koenig HG (May 2009). "Research on religion, spirituality, and mental health: a review" (PDF). Canadian Journal of Psychiatry. 54 (5): 283–91. doi:10.1177/070674370905400502. PMID 19497160. S2CID 14523984. Archived (PDF) from the original on 6 April 2015.
- ^ Zuckerman P (2007). Martin M (ed.). The Cambridge Companion to Atheism. Cambridge Univ. Press. pp. 58–59. ISBN 978-0-521-60367-6.
Concerning suicide rates, religious nations fare better than secular nations. According to the 2003 World Health Organization's report on international male suicides rates, of the top ten nations with the highest male suicide rates, all but one (Sri Lanka) are strongly irreligious nations with high levels of atheism. Of the top remaining nine nations leading the world in male suicide rates, all are former Soviet/Communist nations, such as Belarus, Ukraine, and Latvia. Of the bottom ten nations with the lowest male suicide rates, all are highly religious nations with statistically insignificant levels of organic atheism.
- ^ Rezaeian M (2010). "Suicide among young Middle Eastern Muslim females". Crisis. 31 (1): 36–42. doi:10.1027/0227-5910/a000005. PMID 20197256.
- ^ a b Loue S (2008). Encyclopedia of aging and public health: with 19 tables. New York: Springer. p. 696. ISBN 978-0-387-33753-1.
- ^ Conejero I, Olié E, Courtet P, Calati R (2018). "Suicide in older adults: current perspectives". Clinical Interventions in Aging. 13: 691–699. doi:10.2147/CIA.S130670. PMC 5916258. PMID 29719381.
- ^ a b Calabrò RS, Naro A, De Luca R, Russo M, Caccamo L, Manuli A, et al. (2016). "The Right to Die in Chronic Disorders of Consciousness: Can We Avoid the Slippery Slope Argument?". Innovations in Clinical Neuroscience. 13 (11–12): 12–24. PMC 5300707. PMID 28210521.
- ^ a b Moody HR (2010). Aging: concepts and controversies (6th ed.). Los Angeles: Pine Forge Press. p. 158. ISBN 978-1-4129-6966-6.
- ^ a b Hales RE, Simon RI (2012). The American Psychiatric Publishing textbook of suicide assessment and management (2nd ed.). Washington, DC: American Psychiatric Pub. p. 714. ISBN 978-1-58562-414-0.
- ^ Sobh T (2010). Innovations and advances in computer sciences and engineering (Online-Ausg. ed.). Dordrecht: Springer Verlag. p. 503. ISBN 978-90-481-3658-2.
- ^ Eliason S (2009). "Murder-suicide: a review of the recent literature". The Journal of the American Academy of Psychiatry and the Law. 37 (3): 371–6. PMID 19767502.
- ^ Kornblum W, Smith CD (31 January 2011). Sociology in a changing world (9th ed.). Belmont, CA: Wadsworth Cengage Learning. p. 27. ISBN 978-1-111-30157-6.
- ^ Campbell RJ (2004). Campbell's psychiatric dictionary (8th ed.). Oxford: Oxford University Press. p. 636. ISBN 978-0-19-515221-0.
- ^ Veatch RM (1997). Medical ethics (2nd ed.). Sudbury, MA: Jones and Bartlett. p. 292. ISBN 978-0-86720-974-7.
- ^ Warburton N (2004). The Basics - Philosophy (4th ed.). New York: Routledge. p. 21. ISBN 978-0-415-32773-2.
- ^ Gutman Y, Berenbaum M (1998). Anatomy of the Auschwitz death camp (1st ed.). Bloomington: Publ. in association with the United States Holocaust Memorial Museum, Washington, D.C. by Indiana University Press. p. 400. ISBN 978-0-253-20884-2.
- ^ Plener PL, Schumacher TS, Munz LM, Groschwitz RC (2015). "The longitudinal course of non-suicidal self-injury and deliberate self-harm: a systematic review of the literature". Borderline Personality Disorder and Emotion Dysregulation. 2 (1): 2. doi:10.1186/s40479-014-0024-3. PMC 4579518. PMID 26401305.
- ^ a b Greydanus DE, Shek D (September 2009). "Deliberate self-harm and suicide in adolescents". The Keio Journal of Medicine. 58 (3): 144–151. doi:10.2302/kjm.58.144. hdl:10397/4495. PMID 19826208.
- ^ Chan MK, Bhatti H, Meader N, Stockton S, Evans J, O'Connor RC, et al. (October 2016). "Predicting suicide following self-harm: systematic review of risk factors and risk scales". The British Journal of Psychiatry. 209 (4): 277–283. doi:10.1192/bjp.bp.115.170050. PMID 27340111. S2CID 3428927.
- ^ Levin JD, Culkin J, Perrotto RS (2001). Introduction to chemical dependency counseling. Northvale, NJ: Jason Aronson. pp. 150–52. ISBN 978-0-7657-0289-0.
- ^ a b Fadem B (2004). Behavioral science in medicine. Philadelphia: Lippincott Williams & Wilkins. p. 217. ISBN 978-0-7817-3669-5.
- ^ Youssef NA, Rich CL (2008). "Does acute treatment with sedatives/hypnotics for anxiety in depressed patients affect suicide risk? A literature review". Annals of Clinical Psychiatry. 20 (3): 157–69. doi:10.1080/10401230802177698. PMID 18633742.
- ^ a b Sher L (January 2006). "Alcohol consumption and suicide". QJM. 99 (1): 57–61. doi:10.1093/qjmed/hci146. PMID 16287907.
- ^ Darke S, Ross J (November 2002). "Suicide among heroin users: rates, risk factors and methods". Addiction. 97 (11): 1383–94. doi:10.1046/j.1360-0443.2002.00214.x. PMID 12410779. S2CID 11619947.
- ^ Sher L (2007). "Functional magnetic resonance imaging in studies of the neurobiology of suicidal behavior in adolescents with alcohol use disorders". International Journal of Adolescent Medicine and Health. 19 (1): 11–8. doi:10.1515/ijamh.2007.19.1.11. PMID 17458319. S2CID 42672912.
- ^ Darke S, Kaye S, McKetin R, Duflou J (May 2008). "Major physical and psychological harms of methamphetamine use". Drug and Alcohol Review. 27 (3): 253–62. doi:10.1080/09595230801923702. PMID 18368606. S2CID 39592475.
- ^ Moçambique M, Hoffmann A, Roglio VS, Kessler F, Dalbosco C, Schuch JB, Pechansky F (24 June 2022). "Prevalence of suicide in cocaine users accessing health services: A systematic review and meta-analysis". Brazilian Journal of Psychiatry. 44 (4): 441–8. doi:10.47626/1516-4446-2021-2207. PMC 9375660. PMID 35751594.
- ^ Ayd FJ (2000). Lexicon of psychiatry, neurology, and the neurosciences (2nd ed.). Philadelphia [u.a.]: Lippincott Williams & Wilkins. p. 256. ISBN 978-0-7817-2468-5.
- ^ a b Hughes JR (December 2008). "Smoking and suicide: a brief overview". Drug and Alcohol Dependence. 98 (3): 169–78. doi:10.1016/j.drugalcdep.2008.06.003. PMC 2585177. PMID 18676099.
- ^ a b Ports KA, Merrick MT, Stone DM, Wilkins NJ, Reed J, Ebin J, Ford DC (September 2017). "Adverse Childhood Experiences and Suicide Risk: Toward Comprehensive Prevention". American Journal of Preventive Medicine. 53 (3): 400–403. doi:10.1016/j.amepre.2017.03.015. PMC 5603224. PMID 28483301.
- ^ Cox WT, Abramson LY, Devine PG, Hollon SD (September 2012). "Stereotypes, Prejudice, and Depression: The Integrated Perspective". Perspectives on Psychological Science. 7 (5): 427–49. doi:10.1177/1745691612455204. PMID 26168502. S2CID 1512121.
- ^ Wegman HL, Stetler C (October 2009). "A meta-analytic review of the effects of childhood abuse on medical outcomes in adulthood". Psychosomatic Medicine. 71 (8): 805–12. doi:10.1097/PSY.0b013e3181bb2b46. PMID 19779142. S2CID 25054003.
- ^ Oswald SH, Heil K, Goldbeck L (June 2010). "History of maltreatment and mental health problems in foster children: a review of the literature". Journal of Pediatric Psychology. 35 (5): 462–72. doi:10.1093/jpepsy/jsp114. PMID 20007747.
- ^ Sahle BW, Reavley NJ, Li W, Morgan AJ, Yap MB, Reupert A, Jorm AF (October 2022). "The association between adverse childhood experiences and common mental disorders and suicidality: an umbrella review of systematic reviews and meta-analyses" (PDF). Eur Child Adolesc Psychiatry. 31 (10): 1489–1499. doi:10.1007/s00787-021-01745-2. PMID 33638709. S2CID 232065964.
- ^ Pallanti S, Rossi NB, Hollander E (2006). "11. Pathological Gambling". In Hollander E, Stein DJ (eds.). Clinical manual of impulse-control disorders. American Psychiatric Pub. p. 253. ISBN 978-1-58562-136-1.
- ^ a b Oliveira MP, Silveira DX, Silva MT (June 2008). "[Pathological gambling and its consequences for public health]". Revista de Saude Publica. 42 (3): 542–9. doi:10.1590/S0034-89102008005000026. PMID 18461253.
- ^ Hansen M, Rossow I (January 2008). "[Gambling and suicidal behaviour]". Tidsskrift for den Norske Laegeforening. 128 (2): 174–6. PMID 18202728.
- ^ Semenza DC (29 July 2025). "Local homicides increase suicide in US counties". Social Science & Medicine. 382 118406. doi:10.1016/j.socscimed.2025.118406. PMID 40935491.
- ^ Takken W (10 September 2025). "Twee tv-programma's tonen wat er gebeurt als de dood uit de lucht komt vallen". NRC (in Dutch). Retrieved 10 September 2025.
- ^ Focus, NPO2, 9 September 2025, 21:00 CEST.
- ^ Zhang L, Lucassen PJ, Salta E, Verhaert PD, Swaab DF (2022). "Hippocampal neuropathology in suicide: Gaps in our knowledge and opportunities for a breakthrough". Neuroscience and Biobehavioral Reviews. 132: 542–552. doi:10.1016/j.neubiorev.2021.12.023. ISSN 1873-7528. PMID 34906612.
- ^ Zhang L (2023). Molecular pathology of suicide: A postmortem study (PDF) (dr. thesis). University of Amsterdam. hdl:11245.1/da6f5dee-5a73-4602-ac84-a3789e966fed.
- ^ [180][181][182][183]
- ^ a b Bruffaerts R, Demyttenaere K, Hwang I, Chiu WT, Sampson N, Kessler RC, et al. (July 2011). "Treatment of suicidal people around the world". The British Journal of Psychiatry. 199 (1): 64–70. doi:10.1192/bjp.bp.110.084129. PMC 3167419. PMID 21263012.
- ^ a b "Suicide prevention". WHO Sites: Mental Health. World Health Organization. 31 August 2012. Archived from the original on 1 July 2004. Retrieved 13 January 2013.
- ^ Miller M, Hemenway D (September 2008). "Guns and suicide in the United States". The New England Journal of Medicine. 359 (10): 989–91. doi:10.1056/NEJMp0805923. PMID 18768940. S2CID 35738851.
- ^ Cox GR, Owens C, Robinson J, Nicholas A, Lockley A, Williamson M, et al. (March 2013). "Interventions to reduce suicides at suicide hotspots: a systematic review". BMC Public Health. 13 214. doi:10.1186/1471-2458-13-214. PMC 3606606. PMID 23496989.
- ^ Robinson J, Hetrick SE, Martin C (January 2011). "Preventing suicide in young people: systematic review". The Australian and New Zealand Journal of Psychiatry. 45 (1): 3–26. doi:10.3109/00048674.2010.511147. PMID 21174502. S2CID 24708914.
- ^ Fässberg MM, van Orden KA, Duberstein P, Erlangsen A, Lapierre S, Bodner E, et al. (March 2012). "A systematic review of social factors and suicidal behavior in older adulthood". International Journal of Environmental Research and Public Health. 9 (3): 722–45. doi:10.3390/ijerph9030722. PMC 3367273. PMID 22690159.
- ^ Luxton DD, June JD, Comtois KA (January 2013). "Can postdischarge follow-up contacts prevent suicide and suicidal behavior? A review of the evidence". Crisis. 34 (1): 32–41. doi:10.1027/0227-5910/a000158. PMID 22846445. S2CID 25181980.
- ^ "World Suicide Prevention Day −10 September, 2013". IASP. Archived from the original on 4 November 2013. Retrieved 29 October 2013.
- ^ Barlow DH, Durand VM (2005). Abnormal Psychology. Wadsworth Publishing Company. pp. 248–249. ISBN 978-0-534-63356-1.
- ^ Bachmann S (6 July 2018). "Epidemiology of Suicide and the Psychiatric Perspective". International Journal of Environmental Research and Public Health. 15 (7): 1425. doi:10.3390/ijerph15071425. PMC 6068947. PMID 29986446.
Half of all completed suicides are related to depressive and other mood disorders
- ^ Lopresti AL, Hood SD, Drummond PD (May 2013). "A review of lifestyle factors that contribute to important pathways associated with major depression: diet, sleep and exercise" (PDF). Journal of Affective Disorders. 148 (1): 12–27. doi:10.1016/j.jad.2013.01.014. PMID 23415826. S2CID 22218602. Archived (PDF) from the original on 9 January 2017.
- ^ Wu Y, Zhang L, Li S, Zhang D (29 April 2021). "Associations of dietary vitamin B1, vitamin B2, vitamin B6, and vitamin B12 with the risk of depression: a systematic review and meta-analysis". Nutrition Reviews. 80 (3). Oxford University Press (OUP): 351–366. doi:10.1093/nutrit/nuab014. ISSN 0029-6643. PMID 33912967.
- ^ a b c "Food, drink and mental health". healthdirect. Retrieved 25 August 2023.
- ^ "How to Boost Mental Health Through Better Nutrition". Psychiatry.org. 18 April 2023. Retrieved 25 May 2024.
- ^ Young M (2020). "Assessment and Goal Setting". Learning the Art of Helping: Building Blocks and Techniques. Pearson. p. 195.
[And] was developed by the American Association of Suicidology (2019) to gauge suicidal risk (see also Juhnke, Granello, & Lebrón-Striker, 2007)
- ^ Williams SB, O'Connor EA, Eder M, Whitlock EP (April 2009). "Screening for child and adolescent depression in primary care settings: a systematic evidence review for the US Preventive Services Task Force". Pediatrics. 123 (4): e716-35. doi:10.1542/peds.2008-2415. PMID 19336361. S2CID 8881023.
- ^ LeFevre ML (May 2014). "Screening for suicide risk in adolescents, adults, and older adults in primary care: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 160 (10): 719–26. doi:10.7326/M14-0589. PMID 24842417.
- ^ Clinard MB, Meier RF (2008). Sociology of deviant behavior (14th ed.). Belmont, CA: Wadsworth Cengage Learning. p. 169. ISBN 978-0-495-81167-1.
- ^ Horowitz LM, Ballard ED, Pao M (October 2009). "Suicide screening in schools, primary care and emergency departments". Current Opinion in Pediatrics. 21 (5): 620–7. doi:10.1097/MOP.0b013e3283307a89. PMC 2879582. PMID 19617829.
- ^ Paris J (June 2004). "Is hospitalization useful for suicidal patients with borderline personality disorder?". Journal of Personality Disorders. 18 (3): 240–7. doi:10.1521/pedi.18.3.240.35443. PMID 15237044. S2CID 28921269.
- ^ Goodman M, Roiff T, Oakes AH, Paris J (February 2012). "Suicidal risk and management in borderline personality disorder". Current Psychiatry Reports. 14 (1): 79–85. doi:10.1007/s11920-011-0249-4. PMID 22113831. S2CID 7261201.
- ^ Canadian Agency for Drugs Technologies in Health (CADTH) (2010). "Dialectical behaviour therapy in adolescents for suicide prevention: systematic review of clinical-effectiveness". CADTH Technology Overviews. 1 (1): e0104. PMC 3411135. PMID 22977392.
- ^ Stoffers JM, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K (August 2012). Lieb K (ed.). "Psychological therapies for people with borderline personality disorder". The Cochrane Database of Systematic Reviews. 8 (8) CD005652. doi:10.1002/14651858.CD005652.pub2. PMC 6481907. PMID 22895952.
- ^ O'Connor E, Gaynes BN, Burda BU, Soh C, Whitlock EP (May 2013). "Screening for and treatment of suicide risk relevant to primary care: a systematic review for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 158 (10): 741–54. doi:10.7326/0003-4819-158-10-201305210-00642. PMID 23609101.
- ^ Hetrick SE, McKenzie JE, Cox GR, Simmons MB, Merry SN (November 2012). Hetrick SE (ed.). "Newer generation antidepressants for depressive disorders in children and adolescents". The Cochrane Database of Systematic Reviews. 11 (9) CD004851. doi:10.1002/14651858.CD004851.pub3. hdl:11343/59246. PMC 8786271. PMID 23152227.
- ^ Baldessarini RJ, Tondo L, Hennen J (2003). "Lithium treatment and suicide risk in major affective disorders: update and new findings". The Journal of Clinical Psychiatry. 64 (Suppl 5): 44–52. PMID 12720484.
- ^ Cipriani A, Hawton K, Stockton S, Geddes JR (June 2013). "Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis". BMJ. 346 (jun27 4) f3646. doi:10.1136/bmj.f3646. PMID 23814104.
- ^ Wagstaff A, Perry C (2003). "Clozapine: in prevention of suicide in patients with schizophrenia or schizoaffective disorder". CNS Drugs. 17 (4): 273–80, discussion 281–3. doi:10.2165/00023210-200317040-00004. PMID 12665398.
- ^ Rajkumar R, Fam J, Yeo EY, Dawe GS (September 2015). "Ketamine and suicidal ideation in depression: Jumping the gun?". Pharmacological Research. 99: 23–35. doi:10.1016/j.phrs.2015.05.003. PMID 25982932.
- ^ Caldwell BE (September–October 2013). "Whose Conscience Matters?" (PDF). Family Therapy Magazine (page 22). American Association for Marriage and Family Therapy (AAMFT). Archived from the original (PDF) on 22 January 2018. Retrieved 22 January 2018.
- ^ Bellah v. Greenson (Court case). California First District Court of Appeals. 6 June 1978. Retrieved 22 January 2018 – via Findlaw.
- ^ a b Luxton DD, Thomas EK, Chipps J, Relova RM, Brown D, McLay R, Lee TT, Nakama H, Smolenski DJ (March 2014). "Caring letters for suicide prevention: implementation of a multi-site randomized clinical trial in the U.S. military and Veteran Affairs healthcare systems". Contemporary Clinical Trials. 37 (2): 252–260. doi:10.1016/j.cct.2014.01.007. ISSN 1559-2030. PMID 24473106.
- ^ a b c d e Nock MK (8 May 2014). The Oxford Handbook of Suicide and Self-Injury. Oxford University Press. p. 375. ISBN 978-0-19-020914-8.
- ^ Cherkis J (15 November 2018). "The Best Way To Save People From Suicide". The Huffington Post. Retrieved 29 November 2018.
- ^ Grinshteyn E, Hemenway D (March 2016). "Violent Death Rates: The US Compared with Other High-income OECD Countries, 2010". The American Journal of Medicine. 129 (3): 266–73. doi:10.1016/j.amjmed.2015.10.025. PMID 26551975.
- ^ a b Ajdacic-Gross V, Weiss MG, Ring M, Hepp U, Bopp M, Gutzwiller F, Rössler W (September 2008). "Methods of suicide: international suicide patterns derived from the WHO mortality database". Bulletin of the World Health Organization. 86 (9): 726–32. doi:10.2471/BLT.07.043489. PMC 2649482. PMID 18797649.
- ^ O'Connor RC, Platt S, Gordon J, eds. (1 June 2011). International Handbook of Suicide Prevention: Research, Policy and Practice. John Wiley and Sons. p. 34. ISBN 978-1-119-99856-3.
- ^ Gunnell D, Eddleston M, Phillips MR, Konradsen F (December 2007). "The global distribution of fatal pesticide self-poisoning: systematic review". BMC Public Health. 7 357. doi:10.1186/1471-2458-7-357. PMC 2262093. PMID 18154668.
- ^ Geddes J, Price J, McKnight R, Gelder M, Mayou R (5 January 2012). Psychiatry (4th ed.). Oxford: Oxford University Press. p. 62. ISBN 978-0-19-923396-0.
- ^ a b Krug E (2002). World Report on Violence and Health. Vol. 1. Genève: World Health Organization. p. 196. ISBN 978-92-4-154561-7.
- ^ Yoshioka E, Hanley SJ, Kawanishi Y, Saijo Y (February 2016). "Time trends in method-specific suicide rates in Japan, 1990–2011". Epidemiology and Psychiatric Sciences. 25 (1): 58–68. doi:10.1017/S2045796014000675. PMC 6998669. PMID 25373686.
- ^ Reisch T, Steffen T, Habenstein A, Tschacher W (September 2013). "Change in suicide rates in Switzerland before and after firearm restriction resulting from the 2003 "Army XXI" reform". The American Journal of Psychiatry. 170 (9): 977–84. doi:10.1176/appi.ajp.2013.12091256. PMID 23897090. S2CID 8405876.
- ^ Eshun S, Gurung RA (2009). Culture and mental health sociocultural influences, theory, and practice. Chichester: Wiley-Blackwell. p. 301. ISBN 978-1-4443-0581-4. Archived from the original on 3 October 2015.
- ^ a b c "Suicide – Mental Health Statistics". National Institute of Mental Health. April 2019. Retrieved 15 October 2019.
- ^ a b Fox K, Shveda K, Croker N, Chacon M (26 November 2021). "How US gun culture stacks up with the world". CNN. Archived from the original on 21 December 2023. Article updated October 26, 2023. CNN cites data source: Institute for Health Metrics and Evaluation (Global Burden of Disease 2019), UN Population Division.
- ^ "Deaths estimates for 2008 by cause for WHO Member States". World Health Organization. Archived from the original on 11 November 2009. Retrieved 10 February 2013.
- ^ "Suicide rates Data by country". who.int. Archived from the original on 15 October 2015. Retrieved 23 November 2014.
- ^ a b "Suicide rates rising across the U.S." CDC Newsroom. 7 June 2018. Retrieved 11 October 2018.
- ^ "Suicides in the U.S. reached all-time high in 2022, CDC data shows". NBC News. 10 August 2023. Retrieved 11 August 2023.
- ^ "CDC finds suicide rates among middle-aged adults increased from 1999 to 2010". Centers for Disease Control and Prevention. 2 May 2013. Archived from the original on 21 June 2013. Retrieved 15 July 2013.
- ^ a b Weiyuan C (December 2009). "Women and suicide in rural China". Bulletin of the World Health Organization. 87 (12): 888–9. doi:10.2471/BLT.09.011209. PMC 2789367. PMID 20454475.
- ^ "Death rate from suicides". Our World in Data. Retrieved 4 March 2020.
- ^ "Share of deaths from suicide". Our World in Data. Retrieved 4 March 2020.
- ^ "میزان خودکشی در ایران طی یک دهه گذشته، بیش از ۴۰درصد رشد کرده". etemadonline.com (in Persian). Retrieved 28 December 2023.
- ^ "Estimates for 2000–2012". WHO. Retrieved 24 August 2016.
- ^ a b Sue D, Sue DW, Sue S, Sue D (1 January 2012). Understanding abnormal behavior (Tenth [student] ed.). Belmont, CA: Wadsworth/Cengage Learning. p. 255. ISBN 978-1-111-83459-3. Archived from the original on 30 October 2015.
- ^ Stern TA, Fava M, Wilens TE, Rosenbaum JF (2015). Massachusetts General Hospital Comprehensive Clinical Psychiatry (2 ed.). Elsevier Health Sciences. p. 589. ISBN 978-0-323-32899-9. Archived from the original on 14 September 2016.
- ^ Krug EG (2002). World Report on Violence and Health. World Health Organization. p. 191. ISBN 978-92-4-154561-7. Archived from the original on 14 September 2016.
- ^ Osváth P, Voros V, Fekete SA (2010). "Gender Issues in Suicide Risk Assessment". In Kumar U, Mandal MK (eds.). Suicidal Behaviour: Assessment of People-At-Risk. SAGE Publications India. p. 139. ISBN 978-81-321-0499-5. Retrieved 4 March 2017.
- ^ Ellis L, Hershberger S, Pellis S, Field E, Wersinger S, Pellis S, Geary D, Palmer C, Hoyenga K, Hetsroni A, Karadi K (2013). Sex Differences: Summarizing More than a Century of Scientific Research. Psychology Press. p. 387. ISBN 978-1-136-87493-2. Archived from the original on 5 March 2017. Retrieved 4 March 2017.
- ^ "Suicide Statistics". American Foundation for Suicide Prevention (AFSP). 16 February 2016. Archived from the original on 2 September 2016. Retrieved 3 September 2016.
- ^ Haas AP, Eliason M, Mays VM, Mathy RM, Cochran SD, D'Augelli AR, et al. (2011). "Suicide and suicide risk in lesbian, gay, bisexual, and transgender populations: review and recommendations". Journal of Homosexuality. 58 (1): 10–51. doi:10.1080/00918369.2011.534038. PMC 3662085. PMID 21213174.
- ^ "Suicide Attempts among Transgender and Gender Non-Conforming Adults" (PDF). January 2014. Retrieved 28 April 2018.
- ^ Williams A (April 2017). "Risk factors for suicide in the transgender community". European Psychiatry. 41: S894. doi:10.1016/j.eurpsy.2017.01.1820. S2CID 149086762.
- ^ Virupaksha HG, Muralidhar D, Ramakrishna J (2016). "Suicide and Suicidal Behavior among Transgender Persons". Indian Journal of Psychological Medicine. 38 (6): 505–509. doi:10.4103/0253-7176.194908. PMC 5178031. PMID 28031583.
- ^ "Reports" (PDF). 2011. Archived from the original (PDF) on 8 September 2014. Retrieved 25 July 2016.
- ^ "Suicide rates by age". Our World in Data. Retrieved 4 March 2020.
- ^ a b c d Pitman A, Krysinska K, Osborn D, King M (June 2012). "Suicide in young men". Lancet. 379 (9834): 2383–92. doi:10.1016/S0140-6736(12)60731-4. PMID 22726519. S2CID 193711.
- ^ "Summary tables of mortality estimates by cause, age and sex, globally and by region, 2000–2016". World Health Organization. 2018. Retrieved 21 December 2018.
- ^ Glenn CR, Kleiman EM, Kellerman J, Pollak O, Cha CB, Esposito EC, et al. (March 2020). "Annual Research Review: A meta-analytic review of worldwide suicide rates in adolescents". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 61 (3): 294–308. doi:10.1111/jcpp.13106. PMID 31373003. S2CID 199380438.
- ^ Szasz T (1999). Fatal freedom: the ethics and politics of suicide. Westport, CT: Praeger. p. 11. ISBN 978-0-275-96646-1.
- ^ Battin MP (2015). The ethics of suicide: historical sources. Oxford; New York: Oxford University Press. p. 2. ISBN 978-0-19-938580-5.
- ^ Naiden FS (May 2015). "The Sword Did It: A Greek Explanation for Suicide". The Classical Quarterly. 65 (1): 85–95. doi:10.1017/S0009838814000858. ISSN 0009-8388.
- ^ a b Maris R (2000). Comprehensive textbook of suicidology. New York [u.a.]: Guilford Press. pp. 97–103. ISBN 978-1-57230-541-0.
- ^ Dickinson MR, Leming GE (2 September 2010). Understanding dying, death, and bereavement (7th ed.). Belmont, CA: Wadsworth Cengage Learning. p. 290. ISBN 978-0-495-81018-6.
- ^ a b c Minois G (2001). History of Suicide: Voluntary Death in Western Culture (Johns Hopkins University ed.). Baltimore: Johns Hopkins University Press. ISBN 978-0-8018-6647-0.
- ^ Pickering WS, Walford G (2000). Durkheim's Suicide: a century of research and debate (1. publ. ed.). London: Routledge. p. 69. ISBN 978-0-415-20582-5. Archived from the original on 2 April 2016.
- ^ a b Maris R (2000). Comprehensive textbook of suicidology. New York: Guilford Press. p. 540. ISBN 978-1-57230-541-0.
- ^ a b Suicide. Stanford Encyclopedia of Philosophy. 2017.
- ^ a b Reed P (30 December 2020). "Suicide and its Discontents". In Timmerman T, Cholbi M (eds.). Exploring the Philosophy of Death and Dying: Classical and Contemporary Perspectives. Routledge. ISBN 978-1-000-21674-5.
- ^ Backscheider PR, Ingrassia C (2008). A Companion to the Eighteenth-Century English Novel and Culture. John Wiley & Sons. p. 530. ISBN 978-1-4051-5450-5.
- ^ a b Paperno I (1997). Suicide as a cultural institution in Dostoevsky's Russia. Ithaca: Cornell university press. p. 60. ISBN 978-0-8014-8425-4. Archived from the original on 28 September 2015.
- ^ St John-Stevas N (2002). Life, Death and the Law: Law and Christian Morals in England and the United States. Beard Books. p. 233. ISBN 978-1-58798-113-5.
- ^ Smith JC, Hogan B, Ormerod DC, Ormerod D (2011). Smith & Hogan's criminal law (13th ed.). Oxford: Oxford Univ. Press. p. 583. ISBN 978-0-19-958649-3.
- ^ a b c McLaughlin C (2007). Suicide-related behaviour understanding, caring and therapeutic responses. Chichester: John Wiley & Sons. p. 24. ISBN 978-0-470-51241-8.
- ^ "Dutch 'mercy killing law' passed". 11 April 2001. Retrieved 27 February 2019.
- ^ "German politician Roger Kusch helped elderly woman to die". Times Online. 2 July 2008. Archived from the original on 1 June 2010.
- ^ a b Appel JM (May 2007). "A suicide right for the mentally ill? A Swiss case opens a new debate". The Hastings Center Report. 37 (3): 21–3. doi:10.1353/hcr.2007.0035. PMID 17649899. S2CID 28038414.
- ^ Holt, Gerry."When suicide was illegal" Archived 7 February 2014 at the Wayback Machine. BBC News. 3 August 2011. Accessed 11 August 2011.
- ^ "Guardian & Observer style guide". Guardian website. The Guardian. 31 December 2015. Archived from the original on 19 October 2013. Retrieved 29 November 2011.
- ^ "Chapter 70.245 RCW, The Washington death with dignity act". Washington State Legislature. Archived from the original on 8 July 2010.
- ^ "Oregon Revised Statute – 127.800 s.1.01. Definitions". Oregon State Legislature. Archived from the original on 7 October 2015.
- ^ "CBCNews.ca Mobile". Cbc.ca. 1 February 1999. Archived from the original on 7 August 2014. Retrieved 6 August 2014.
- ^ Adams C (15 April 2014). "US border suicide profiling must stop: Report". globalnews.ca. Archived from the original on 8 August 2014. Retrieved 7 August 2014.
- ^ Lanham D, Bartal BF, Evans RC, Wood D (2006). Criminal laws in Australia. Annandale, N.S.W.: The Federation Press. p. 229. ISBN 978-1-86287-558-6.
- ^ Costa M, Duffy M (1991). Labor, prosperity and the nineties: beyond the bonsai economy (2nd ed.). Sydney: Federation Press. p. 315. ISBN 978-1-86287-060-4.
- ^ Putnam CE (2002). Hospice or hemlock?: searching for heroic compassion. Westport, CT: Praeger. p. 143. ISBN 978-0-89789-921-5.
- ^ Dogra M, Srivastava S (1 January 2012). Climate change and disease dynamics in India. New Delhi: The Energy and Resources Institute. p. 256. ISBN 978-81-7993-412-8. Archived from the original on 28 September 2015.
- ^ "Govt decides to repeal Section 309 from IPC; attempt to suicide no longer a crime". Zee News. 10 December 2014. Archived from the original on 15 May 2015. Retrieved 10 December 2014.
- ^ "Why so long to decriminalise suicide, says Befrienders". Free Malaysia Today. 19 June 2022.
- ^ "Decision on decriminalising suicide attempts in Malaysia lie with cabinet: Khairy". Channel News Asia. 28 September 2022.
- ^ "Malaysia's Pathway to the Decriminalisation of Suicides: Students' Opinion and Discussions (pdf)". academia.edu. 27 December 2020.
- ^ "As decriminalisation nears, a brief look at how suicide became a crime in Malaysia". Malay Mail. 7 April 2023.
- ^ Zitser J. "Kim Jong Un orders North Koreans to stop killing themselves after number of suicides skyrocketed". Business Insider. Retrieved 12 June 2023.
- ^ Roth R. "Suicide & Euthanasia – a Biblical Perspective". Acu-cell.com. Archived from the original on 18 April 2009. Retrieved 6 May 2009.
- ^ "Norman N. Holland, Literary Suicides: A Question of Style". Clas.ufl.edu. Archived from the original on 28 May 2009. Retrieved 6 May 2009.
- ^ "Is suicide a sin?". 28 October 2014. Retrieved 14 April 2022.
- ^ "Catechism of the Catholic Church – Part 3 Section 2 Chapter 2 Article 5". Scborromeo.org. 1 June 1941. Archived from the original on 25 April 2009. Retrieved 6 May 2009.
- ^ "Catechism of the Catholic Church – Part 3 Section 2 Chapter 2 Article 5". Scborromeo.org. 1 June 1941. Archived from the original on 25 April 2009. Retrieved 6 May 2009.
- ^ "Euthanasia and Judaism: Jewish Views of Euthanasia and Suicide". ReligionFacts.com. Archived from the original on 6 May 2006. Retrieved 16 September 2008.
- ^ "Surah An-Nisa - 29". Quran.com. Retrieved 25 February 2023.
- ^ a b Gearing RE, Lizardi D (September 2009). "Religion and suicide". Journal of Religion and Health. 48 (3): 332–41. doi:10.1007/s10943-008-9181-2. PMID 19639421. S2CID 30494312.
- ^ Hindu Website. Hinduism and suicide Archived 7 May 2008 at the Wayback Machine
- ^ a b "Hinduism – Euthanasia and Suicide". BBC. 25 August 2009. Archived from the original on 25 February 2009.
- ^ "India wife dies on husband's pyre". 22 August 2006. Retrieved 30 June 2019.
- ^ Takako Yamada: The Worldview of the Ainu. Nature and Cosmos Reading from Language, p. 25–37, p. 123.
- ^ Norbert Richard Adami: Religion und Schaminismus der Ainu auf Sachalin (Karafuto), Bonn 1989, p. 45.
- ^ a b Adami: Religion und Schaminismus der Ainu auf Sachalin (Karafuto), p. 79, p. 119.
- ^ a b c "Suicide". Suicide (Stanford Encyclopedia of Philosophy). Plato.stanford.edu. 2017. Retrieved 6 May 2009.
- ^ Kant, Immanuel. (1785) Kant: The Metaphysics of Morals, M. Gregor (trans.), Cambridge: Cambridge University Press, 1996. ISBN 978-0-521-56673-5. p. 177.
- ^ Safranek John P (1998). "Autonomy and Assisted Suicide: The Execution of Freedom". The Hastings Center Report. 28 (4): 32–36. doi:10.2307/3528611. JSTOR 3528611. PMID 9762538.
- ^ Whiting R (2001). A natural right to die: twenty-three centuries of debate. Praeger. pp. 13–17. ISBN 0-313-31474-8.
- ^ Smith WJ (August 2007). "Death on Demand: The assisted-suicide movement sheds its fig leaf". NRL News. 34 (8): 18. Archived from the original on 16 April 2021. Retrieved 25 July 2020.
- ^ "A Q&A with Alexandre Baril". 31 May 2023.
- ^ "Don't Say It's Selfish: Suicide Is Not a Choice". www.nationwidechildrens.org.
- ^ Suicidism has been described as "an oppressive system (stemming from non-suicidal perspectives) functioning at the normative, discursive, medical, legal, social, political, economic, and epistemic levels in which suicidal people experience multiple forms of injustice and violence..."Baril A (2020). "Suicidism: A new theoretical framework to conceptualize suicide from an anti-oppressive perspective". Disability Studies Quarterly. 40 (3): 1–41. doi:10.18061/dsq.v40i3.7053. Archived from the original on 12 December 2020. Retrieved 2 January 2021.
- ^ "The Suicide". The Walters Art Museum. Archived from the original on 16 January 2013.
- ^ Ozawa-de Silva C (December 2008). "Too lonely to die alone: internet suicide pacts and existential suffering in Japan". Culture, Medicine and Psychiatry. 32 (4): 516–51. doi:10.1007/s11013-008-9108-0. PMID 18800195. S2CID 145475668.
- ^ Luxton DD, June JD, Fairall JM (May 2012). "Social Media and Suicide: A Public Health Perspective". American Journal of Public Health. 102 (Suppl 2): S195 – S200. doi:10.2105/AJPH.2011.300608. ISSN 0090-0036. PMC 3477910. PMID 22401525.
- ^ Durkee T, Hadlaczky G, Westerlund M, Carli V (October 2011). "Internet pathways in suicidality: a review of the evidence". International Journal of Environmental Research and Public Health. 8 (10): 3938–52. doi:10.3390/ijerph8103938. PMC 3210590. PMID 22073021.
- ^ a b Picard D, Robinson M (28 November 2012). Emotion in motion: tourism, affect and transformation. Farnham, Surrey: Ashgate. p. 176. ISBN 978-1-4094-2133-7.
- ^ "A voice of reason on Yangtze bridge". The National. 8 July 2008. Retrieved 16 October 2019.
- ^ Robinson P, Heitmann S, Dieke PU (2010). Research themes for tourism. Oxfordshire [etc.]: CABI. p. 172. ISBN 978-1-84593-684-6.
- ^ a b Dennis R (2008). Cities in modernity: representations and productions of metropolitan space, 1840–1930 (Repr. ed.). Cambridge [u.a.]: Cambridge Univ. Press. p. 20. ISBN 978-0-521-46841-1.
- ^ McDougall T, Armstrong M, Trainor G (2010). Helping children and young people who self-harm: an introduction to self-harming and suicidal behaviours for health professionals. Abingdon, Oxon: Routledge. p. 23. ISBN 978-0-415-49913-2.
- ^ a b Bateson J (2008). Building hope: leadership in the nonprofit world. Westport, CT: Praeger. p. 180. ISBN 978-0-313-34851-8.
- ^ Miller D (2011). Child and Adolescent Suicidal Behavior: School-Based Prevention, Assessment, and Intervention. Guilford Press. p. 46. ISBN 978-1-60623-997-1.
- ^ Hall 1987, p.282
- ^ "Alternative Considerations of Jonestown and Peoples Temple". San Diego State University. Archived from the original on 20 February 2011. Retrieved 10 November 2011.
- ^ "1978:Mass Suicide Leaves 900 Dead Archived 2012-11-04 at the Wayback Machine". Retrieved 9 November 2011.
- ^ John Toland, The Rising Sun: The Decline and Fall of the Japanese Empire 1936–1945, Random House, 1970, p. 519
- ^ O'Keeffe TM (1984). "Suicide and Self-Starvation". Philosophy. 59 (229): 349–363. doi:10.1017/S0031819100069941. JSTOR 3750951. S2CID 154281192.
- ^ Watson B (2007). Exit Rommel: The Tunisian Campaign, 1942–43. Stackpole Books. p. 170. ISBN 978-0-8117-3381-6.
- ^ Chang K (25 August 2008). "In Salmonella Attack, Taking One for the Team". The New York Times. Archived from the original on 5 August 2017.
- ^ Tofilski A, Couvillon MJ, Evison SE, Helanterä H, Robinson EJ, Ratnieks FL (November 2008). "Preemptive defensive self-sacrifice by ant workers" (PDF). The American Naturalist. 172 (5): E239-43. Bibcode:2008ANat..172E.239T. doi:10.1086/591688. PMID 18928332. S2CID 7052340. Archived (PDF) from the original on 27 November 2009.
- ^ O'Hanlon L (10 March 2010). "Animal Suicide Sheds Light on Human Behavior". Discovery News. Archived from the original on 25 July 2010.
- ^ a b Bordereau C, Robert A, Van Tuyen V, Peppuy A (1 August 1997). "Suicidal defensive behaviour by frontal gland dehiscence in Globitermes sulphureus Haviland soldiers (Isoptera)". Insectes Sociaux. 44 (3): 289–97. doi:10.1007/s000400050049. ISSN 1420-9098. S2CID 19770804.
- ^ "Life In The Undergrowth". BBC.
- ^ Nobel J (19 March 2010). "Do Animals Commit Suicide? A Scientific Debate". Time. Archived from the original on 22 March 2010.
- ^ Stoff DM, Mann JJ (December 1997). "Suicide research. Overview and introduction". Annals of the New York Academy of Sciences. 836 (1): 1–11. Bibcode:1997NYASA.836....1S. doi:10.1111/j.1749-6632.1997.tb52352.x. PMID 9616791. S2CID 31876340.
- ^ Hogenboom M (6 July 2016). "Many animals seem to kill themselves, but it is not suicide". BBC. Archived from the original on 26 February 2017. Retrieved 20 July 2017.
Further reading
[edit]- Gambotto A (2004). The Eclipse: A Memoir of Suicide. Australia: Broken Ankle Books. ISBN 978-0-9751075-1-5.
- Goeschel C (2009). Suicide in Nazi Germany. Oxford University Press. ISBN 978-0-19-953256-8.
External links
[edit]- Preventing suicide: a global imperative (PDF). WHO. 2014. ISBN 978-92-4-156477-9.
- Freakonomics podcast: The Suicide Paradox
Suicide
View on GrokipediaDefinitions and Classification
Core Definitions
Suicide is defined as death caused by self-directed injurious behavior with any intent to die as a result of the behavior.[3] This definition, employed by the National Institute of Mental Health (NIMH), highlights the centrality of deliberate intent, which differentiates suicide from accidental self-injury or externally inflicted harm.[3] Similarly, the Centers for Disease Control and Prevention (CDC) describes suicide as death resulting from injuring oneself with the intent to die, a formulation that underscores the purposeful nature of the act in public health surveillance and classification systems.[1] Medically, suicide constitutes the fatal outcome of purposeful self-inflicted harm aimed at terminating life, often confirmed through forensic investigation, including psychological autopsies that reconstruct evidence of suicidal ideation, planning, or prior attempts when direct testimony is unavailable.[8] The World Health Organization (WHO) aligns with this framework in its global reporting, treating suicide as deliberate self-killing and estimating over 720,000 annual deaths worldwide under this criterion, though underreporting due to stigma or misclassification as accidents complicates precise enumeration in many regions.[2][9] Legally, suicide is characterized as the intentional taking of one's own life by one's own agency, typically requiring volition and mental capacity; acts by individuals deemed insane or coerced may be reclassified to avoid equating them with autonomous choice, varying by jurisdiction in statutes addressing insurance exclusions or criminal assistance to suicide.[10][11] In both medical and legal domains, intent is inferred from circumstantial evidence such as suicide notes, method lethality, or behavioral history, as direct proof is often posthumous and probabilistic rather than absolute.[10][8]Distinctions from Related Behaviors
Non-suicidal self-injury (NSSI) involves the deliberate destruction of one's own body tissue without suicidal intent, typically serving functions such as emotional regulation, interpersonal influence, or sensation-seeking, whereas suicide requires the explicit aim of causing death.[12] NSSI often results in superficial wounds, like cutting or burning, and is more prevalent among adolescents and young adults, with lifetime prevalence rates estimated at 17-18% in non-clinical samples, but it carries an elevated risk for future suicidal behavior due to shared underlying vulnerabilities like impulsivity or borderline personality traits.[13] In contrast, suicidal acts prioritize lethality, such as through hanging or firearms, reflecting a primary intent to end life rather than temporary relief.[14] Parasuicide, or deliberate self-harm without genuine suicidal intent, differs from completed or attempted suicide by lacking the core motivation of death; it may represent a cry for help, impulsive gesture, or manipulation, often involving low-lethality methods like minor overdoses that are survivable.[15] Empirical data indicate that parasuicidal acts are more common in females and linked to situational stressors, with repetition rates up to 20-30% within a year, but they do not equate to suicide attempts where death is earnestly pursued.[16] Distinguishing these relies on clinical assessment of intent, as ambiguous cases complicate epidemiology; for instance, some overdoses may blend elements, but suicide demands verifiable evidence of fatal purpose over mere self-injury.[17] Euthanasia and assisted suicide diverge from standard suicide in their relational and contextual elements: euthanasia entails a third party, such as a physician, actively administering a lethal agent to end suffering, often in terminal illness, while assisted suicide provides the means (e.g., prescribing lethal drugs) for the individual to self-administer.[18] These practices are typically framed within medical ethics for rational, non-psychiatric decisions, legalized in jurisdictions like the Netherlands since 2002, with annual cases numbering around 4% of deaths there, contrasting suicide's unilateral, often impulsive nature amid mental health crises.[19] Suicide lacks external facilitation and is not contingent on prognosis or consent protocols, frequently involving untreated depression or acute despair rather than end-of-life autonomy.[20] Self-sacrifice, including martyrdom, entails forfeiting life for ideological, communal, or altruistic gains, such as preserving group honor or advancing a cause, rather than escaping personal torment central to most suicides.[21] Historical examples, like soldierly self-immolation in battle or religious martyrdom, emphasize external validation and legacy, with psychological drivers rooted in duty or transcendence, differing from suicide's inward focus on individual cessation.[22] Empirical distinctions arise in intent assessment: self-sacrifice anticipates posthumous benefit, as in documented cases of ideological extremism where actors perceive empowerment through death, whereas suicide correlates with hopelessness scales showing diminished future orientation.[23]Rational vs. Irrational Suicide
The debate over rational versus irrational suicide centers on whether ending one's life can constitute a reasoned decision free from distortion by mental impairment or transient states, or if it invariably reflects flawed judgment. Philosophers like David Hume contended that suicide may be rational when it alleviates irremediable suffering without violating duties to self, society, or providence, arguing that it parallels permissible acts like medical intervention to hasten recovery rather than an affront to divine order.[24] This view posits rationality in cases of terminal illness or profound, unrelievable pain where continued existence yields net harm, emphasizing individual autonomy over imposed preservation of life.[25] In contrast, psychiatric perspectives predominantly classify suicide as irrational, attributing it to underlying mental disorders that impair cognitive evaluation of alternatives and future prospects. Empirical studies indicate that over 90% of suicides involve diagnosable conditions such as depression or substance use disorders, which distort risk-benefit assessments and often respond to treatment, rendering the act non-volitional in a fully rational sense.[26] Psychotherapists have proposed criteria for potential rational suicide, including decisional competence, absence of coercion or impulsivity, exploration of alternatives, and irreversible suffering, yet such cases remain exceedingly rare, with most professionals estimating fewer than 1% of suicides meet these thresholds due to pervasive influence of psychopathology.[27] [28] Critics of rational suicide arguments highlight that even in non-terminal scenarios, psychogenic pain—though subjective—is biochemically real and frequently amenable to intervention, challenging claims of inevitability.[29] Professional bodies like the American Psychiatric Association deem assistance in non-terminal rational suicide unethical, underscoring that rationality requires undistorted foresight, which mental illness precludes, and that societal emphasis on prevention aligns with evidence of post-crisis regret or recovery in survivors.[30] While cultural examples, such as Stoic self-slaughter in antiquity, illustrate perceived honor in chosen death, modern data reveal impulsivity in up to 50% of attempts, further eroding notions of premeditated rationality across broad populations.[31]Epidemiology
Global and Regional Trends
The global age-standardized suicide mortality rate declined by nearly 40% over the three decades prior to 2021, falling from approximately 15 deaths per 100,000 population to 9 per 100,000.[32] This equates to an estimated 727,000 suicide deaths in 2021, representing the third leading cause of death among individuals aged 15-29 years worldwide, with males exhibiting rates more than twice those of females (12.3 versus 5.9 per 100,000).[33] The decline reflects improvements in prevention efforts, socioeconomic development, and access to mental health interventions in various regions, though underreporting remains prevalent due to stigma, cultural taboos, and legal prohibitions on suicide in many countries, potentially underestimating true rates by up to 100% in low-income settings.[2] Despite the overall downward trajectory, progress has been uneven, with a 12% reduction observed from 8.23 per 100,000 in 2013 to 7.24 per 100,000 in 2020, but persistent high burdens in certain demographics and areas.[34] Regionally, suicide rates exhibit substantial variation, influenced by factors such as economic development, cultural norms, and healthcare infrastructure. In Eastern Europe, age-standardized rates reached 19.2 per 100,000 in 2021, the highest globally, attributed to historical socioeconomic disruptions, alcohol consumption patterns, and limited mental health resources.00006-4/fulltext) Southern sub-Saharan Africa followed with 16.1 per 100,000, where crude rates are elevated due to younger populations and vulnerabilities like poverty and conflict, though age-adjusted figures may be lower than in high-income regions when accounting for demographics.00006-4/fulltext) In contrast, the WHO Western Pacific and European Regions report comparatively higher rates than African or American regions in some analyses, with Western Pacific rates often exceeding 10 per 100,000 due to rapid urbanization stresses and varying access to lethal means.[35]| WHO Region | Approximate Age-Standardized Rate (per 100,000, recent estimates) | Key Trend Notes |
|---|---|---|
| Europe | 10-12 | Stable to declining, but high in Eastern subregions00006-4/fulltext) |
| Western Pacific | 8-11 | Declining overall, with urban-rural disparities[35] |
| Africa | 11-16 (higher in southern areas) | Underreporting common; linked to socioeconomic factors00006-4/fulltext) |
| Americas | 7-9 | Declines in some countries, rises in others like the U.S.[5] |
| South-East Asia | 8-10 | Moderate declines, but high absolute numbers due to population size[2] |
| Eastern Mediterranean | 6-8 | Lower rates, influenced by cultural and religious prohibitions[36] |
Demographic Patterns
Globally, suicide rates are substantially higher among males than females, with men dying by suicide at more than twice the rate of women. In 2021, the age-standardized global suicide rate was 12.3 per 100,000 for males compared to 5.6 per 100,000 for females, according to World Health Organization estimates derived from vital registration and verbal autopsy data.[39] [36] This disparity persists across most regions, though it widens in high-income countries; for instance, in the United States in 2023, the rate for males was nearly four times that for females (22.8 per 100,000 versus 5.9 per 100,000).[3] Males' higher lethality often stems from methods like firearms or hanging, which have lower survival rates compared to overdoses more common among females.[40] Age patterns vary by sex and region, but globally, suicide rates tend to increase with age, peaking among older adults. The World Health Organization reports that suicide is the third leading cause of death for individuals aged 15–29, yet rates are highest among those 65 and older, at approximately 15.99 per 100,000—significantly elevated compared to younger groups.[2] [41] In the U.S., per 2022 Centers for Disease Control and Prevention data, the highest rates among males occur in those aged 75 and older, while for females, peaks are in the 45–64 age group (8.6 per 100,000).[3] [4] These trends reflect cumulative risk factors such as chronic illness, isolation, and loss of social roles in later life, though underreporting due to stigma may skew younger age data in low-resource settings.[42] Regionally, 73% of global suicides occur in low- and middle-income countries, where rates exceed those in high-income nations despite lower overall reporting.[2] The highest national rates include Greenland (59.6 per 100,000), Guyana (31.3 per 100,000), and Lithuania (27.9 per 100,000), often linked to rural isolation, alcohol use, and limited mental health access.[37] In contrast, rates are lower in regions like Southern Europe and parts of Latin America. Within countries like the U.S., rural areas show 17.3 per 100,000 versus 11.2 in urban areas, highlighting geographic disparities tied to economic and service access.[43] In the U.S., racial and ethnic patterns reveal elevated rates among American Indian/Alaska Native populations (27.1 per 100,000 overall in recent data), followed by non-Hispanic Whites (17.6 per 100,000), with non-Hispanic Black and Hispanic rates lower but rising among youth.[44] [3] American Indian/Alaska Native males face the highest burden at 35.3 per 100,000.[3] Socioeconomic status inversely correlates with rates worldwide; lower income, unemployment, and social isolation predict higher risk, with hazard ratios increasing as economic position declines.[45] [46] This holds across ethnic groups and ages, though disparities may be underestimated in data from biased or incomplete registries.[47]Temporal and Occupational Variations
Suicide rates exhibit seasonal patterns in many populations, with peaks often observed in spring and early summer, particularly in Northern Hemisphere countries. A multi-country analysis found greater seasonal effects among females and the elderly compared to males and younger individuals, attributing variations to factors like photoperiod and temperature. However, patterns differ by demographics; for instance, U.S. youth aged 15-24 show autumn peaks (September-October) and summer troughs, potentially linked to school schedules. Globally, suicide attempts and self-harm presentations to emergency departments also tend to peak in spring and summer.[48][49][50][51] Short-term temporal fluctuations include diurnal and weekly cycles. Suicides frequently occur in the early morning or morning hours, especially among middle-aged males, with peaks noted on Mondays in some datasets. Midnight peaks appear in young and middle-aged male suicides in Japan over 41 years of observation. Weekly patterns show elevated risk on Mondays and New Year's Day across multiple countries, though weekend and Christmas effects vary geographically.[52][53][54][55] Long-term historical trends reveal a global decline in age-standardized suicide rates, from 14.0 per 100,000 in 2000 to 9.0 per 100,000 in 2019, with 746,000 deaths estimated in 2021. In the United States, rates rose 37% from 2000 to 2018 before a 5% dip through 2020, rebounding to prior highs by 2022, reflecting over 539,810 deaths from 2011 to 2022. These shifts correlate with economic, social, and mental health service access changes, though causal links require further empirical scrutiny beyond correlational data.[56][57][5][58] Occupational variations show elevated suicide rates in manual and high-risk professions, often tied to physical demands, isolation, access to lethal means, and economic instability. In the U.S., working-age suicide rates increased 33% over two decades ending 2021, with farming, fishing, and forestry workers at 84.5 per 100,000—the highest overall—and construction and extraction at 49.4 per 100,000 for males. Among males, top groups include agricultural scientists (173.1 per 100,000) and logging workers. Females in construction and extraction also face high rates (25.5 per 100,000). These disparities persist across datasets, underscoring needs for targeted interventions in industries with limited mental health support.[59][60][61][62]| Occupational Group (U.S., 2021) | Suicide Rate per 100,000 (Males) | Suicide Rate per 100,000 (Overall or Females where noted) |
|---|---|---|
| Farming, Fishing, Forestry | - | 84.5 |
| Construction and Extraction | 49.4 | 25.5 (females) |
| Agricultural/Food Scientists | 173.1 | - |
| Logging Workers | High (specific rate not isolated) | - |
Etiology and Risk Factors
Genetic and Biological Factors
Twin and family studies indicate a moderate genetic contribution to suicidal behavior, with heritability estimates ranging from 30% to 55%.[63][64] A 2007 systematic review of twin studies concluded that genetic factors significantly influence liability for suicide, independent of shared environment in many cases.[65] Family history of completed suicide independently elevates risk, with odds ratios approximately 2.5 to 3.0 after controlling for psychiatric illness.[66][67] Genome-wide association studies (GWAS) have identified multiple genetic loci associated with suicide attempts and ideation, though individual variants confer small effect sizes and no single gene has been definitively established as causal.[64] A 2023 meta-analysis of over 22 million individuals pinpointed 12 genome-wide significant loci for suicide attempt, implicating pathways related to neuronal development and psychiatric comorbidities.[68] Candidate genes such as those involved in serotonergic signaling (e.g., SLC6A4) show inconsistent associations across studies, highlighting the polygenic nature of risk.[69] Biological markers include dysregulation in the serotonergic system, evidenced by lower cerebrospinal fluid levels of 5-hydroxyindoleacetic acid (5-HIAA), a serotonin metabolite, in suicide completers compared to controls.[69] The hypothalamic-pituitary-adrenal (HPA) axis exhibits hyperactivity in some suicidal individuals, correlating with elevated cortisol responses to stress, though blunted activity has been observed in attempters with psychopathology.[70][71] Neuroimaging reveals structural alterations, such as reduced gray matter volume in the prefrontal cortex and anterior cingulate, and functional connectivity disruptions in emotion regulation networks among those with suicidal behavior.[72] These findings suggest impaired inhibitory control and heightened impulsivity as underlying mechanisms, though results vary by study population and methodology.[73]Psychiatric and Neurobiological Contributors
Psychiatric disorders are among the strongest predictors of suicide, with meta-analyses indicating that individuals diagnosed with any mental disorder face an odds ratio of 13.1 for suicide compared to those without.[6] Approximately 49% of suicide decedents in the United States have a known diagnosed mental health condition, though this figure may underestimate due to underdiagnosis or absence in the remaining cases.[74] Major depressive disorder (MDD) exhibits one of the highest associations, with affected individuals showing significantly elevated risk across multiple studies.[75] Bipolar disorder and schizophrenia spectrum disorders also confer substantial risk, often exceeding that of unipolar depression in lifetime prevalence among completers.[76] Borderline personality disorder and other personality disorders further amplify vulnerability, with suicide rates up to 10% in clinical populations.[77] These associations persist even after controlling for comorbidities, underscoring a direct causal pathway rather than mere correlation, as evidenced by prospective cohort data linking disorder onset to subsequent suicidal acts.[78] Anxiety disorders, including post-traumatic stress disorder, contribute independently, though their risk is moderated by co-occurring depression.[75] Schizophrenia elevates risk through chronic psychosis and negative symptoms, with meta-analyses reporting odds ratios around 20 for suicide in early-course patients.[76] Notably, while psychiatric diagnoses cluster in suicide cases, their absence in roughly half of completers highlights multifactorial etiology, including acute stressors absent formal illness criteria.[74] Neurobiologically, dysregulation of the serotonergic system is a core feature, with postmortem and cerebrospinal fluid studies revealing reduced serotonin metabolite (5-HIAA) levels in suicide attempters, particularly those with impulsive acts.[79] This deficit correlates with impaired prefrontal inhibition of aggressive impulses, as low serotonin facilitates disinhibition in limbic regions.[70] The hypothalamic-pituitary-adrenal (HPA) axis shows hyperactivity in many cases, marked by elevated cortisol responses to stress, which exacerbates emotional dysregulation and hopelessness.[80] However, blunted HPA reactivity appears in chronic attempters, suggesting adaptive exhaustion that impairs stress coping and heightens lethality.[71] Neuroimaging reveals structural alterations, including reduced gray matter volume in the prefrontal cortex and anterior cingulate, regions critical for emotion regulation and decision-making.[72] Functional MRI studies demonstrate amygdala hyperreactivity to negative stimuli in suicide ideators, coupled with diminished connectivity to regulatory prefrontal areas.[73] These changes, observed across disorders like MDD and bipolar, precede attempts and predict recurrence, independent of symptom severity alone.[81] Dopaminergic and noradrenergic imbalances further contribute, with elevated norepinephrine in suicidal states linking to agitation and arousal.[79] Inflammation markers, such as elevated cytokines, correlate with these neural shifts, implying a role for neuroimmune activation in vulnerability.[82]Substance Use and Comorbidities
Substance use disorders (SUDs) are strongly associated with elevated suicide risk, with psychological autopsy studies indicating that 19% to 63% of suicide decedents suffered from SUDs, predominantly alcohol use disorder (AUD).[83] Adults with SUDs were nearly four times more likely to seriously consider suicide and three times more likely to plan or attempt it in 2020, compared to those without SUDs.[84] All categories of SUDs, including alcohol, cannabis, opioids, cocaine, and other drugs, correlate with increased suicide mortality in population-based cohorts, with adjusted odds ratios ranging from 2.0 for other drug use disorders to higher for specific substances after controlling for demographics and other risk factors.[85] Alcohol use disorder exhibits one of the strongest links, with individuals diagnosed with AUD showing a lifetime prevalence of attempted suicide around 40%.[86] Lifetime suicide rates among those with AUD reach 3.54% for women and 3.94% for men, versus 0.29% and 0.76% in the general population, respectively, based on Swedish registry data spanning decades.[87] Acute alcohol intoxication at the time of death is common in suicides, impairing judgment and impulsivity control, while chronic AUD contributes through neurotoxic effects and social isolation.[88] Opioid use disorders confer particularly high risk, with affected individuals 14 times more likely to die by suicide than the general population; standardized mortality ratios for suicide among opioid users approximate 5.46.[89][90] Estimates suggest 25% to 50% of all suicides involve alcohol or drug dependence, with opioids implicated in a subset of overdose suicides that may blur intentionality boundaries.[91][92] Psychiatric comorbidities amplify these risks, as SUDs frequently co-occur with mood disorders like major depression, where men with comorbid depression and AUD face a 16.2% long-term suicide risk.[93] AUD alone elevates suicidality odds by 86%, but conjunction with other psychiatric conditions such as anxiety or bipolar disorder intensifies vulnerability through shared neurobiological pathways, including serotonin dysregulation and heightened impulsivity.[94] Tobacco use disorder, often comorbid with other SUDs, independently raises suicide risk, while polysubstance use patterns further escalate lethality by compounding cognitive impairments and withdrawal states that precipitate acute crises.[95] Causal evidence from longitudinal studies supports SUDs as both precursors and precipitants, distinct from mere correlation, though reverse causation (e.g., self-medication of underlying distress) requires disentangling via first-episode analyses.[96]| Substance | Key Suicide Risk Metric | Source |
|---|---|---|
| Alcohol Use Disorder | Lifetime attempt prevalence: ~40%; Suicide rate: 3.5-3.9% | [86] [87] |
| Opioid Use Disorder | 14x increased suicide mortality odds; SMR ~5.46 | [89] [90] |
| General SUDs | 19-63% prevalence in suicide decedents; 4x ideation risk | [83] [84] |
Psychosocial and Environmental Influences
Childhood adversities, including abuse, neglect, and household dysfunction, significantly elevate suicide risk in adulthood. Individuals with four or more adverse childhood experiences (ACEs) face odds of suicide attempts approximately 30 times higher than those without such exposures. These effects persist through mediating pathways like reduced resilience and heightened mental distress, with long-term childhood difficulties linked to 21% higher odds of suicidal ideation or planning.[97][98] Social isolation and loneliness independently contribute to suicidality, with meta-analyses indicating a fivefold increase in suicide mortality risk among affected individuals, particularly pronounced in men.[99] Living alone exacerbates this vulnerability, especially when comorbid with depression or anxiety, as evidenced by cohort studies showing elevated suicide rates in such arrangements.[100] Interpersonal factors like divorce and exposure to others' suicides further amplify risk, acting as precipitating stressors in susceptible populations.[101] Lower socioeconomic status correlates with higher suicide rates, with hazard ratios demonstrating a gradient where decreasing economic position yields progressively elevated risks; for instance, the lowest income quintile exhibits rates up to several times higher than the highest.[45] Unemployment exerts a causal influence, with each 1% rise in unemployment rates associated with 2-3% higher suicide rates across countries, particularly impacting men aged 40-64.[102][103] Economic downturns, such as the Great Recession, intensified these patterns in regions with weaker social protections, underscoring the role of financial hardship in precipitating suicidal outcomes.[104] Justice system involvement and foster care placement also emerge as social-environmental risks, tied to structural disadvantages that compound individual vulnerabilities.[101] Despite profound hopelessness, psychosocial protective factors often avert suicide. Suicidal impulses are typically transient and subside after the acute crisis passes. Fear of physical pain or a failed attempt leading to further suffering deters action. Concerns about causing emotional distress to loved ones, including family, friends, and pets, provide significant barriers. Residual hope for improvement, religious beliefs, and last-moment help-seeking, such as contacting crisis services, further contribute to survival. Survivor testimonies highlight these elements: "I thought of my mother and couldn't do that to her"; "The pain of dying seemed worse than continuing to live"; "My dog looked at me and I couldn't abandon it"; "I called a helpline and talking changed my perspective"; "The moment passed and the next day things looked different."Pathophysiology
Neurochemical Mechanisms
Dysregulation of the serotonin system represents a core neurochemical feature in suicidal behavior, with postmortem studies of suicide victims revealing decreased serotonin (5-HT) and its metabolite 5-hydroxyindoleacetic acid (5-HIAA) levels in the brainstem.[105] Low cerebrospinal fluid 5-HIAA concentrations have been linked to heightened suicide risk, particularly in impulsive acts, independent of underlying psychiatric diagnosis.[106] Additionally, increased binding of 5-HT2A receptors in the prefrontal cortex has been observed in suicide completers, suggesting altered serotonergic signaling that impairs impulse control and mood regulation.[79] The 5-HT1A autoreceptor, which modulates serotonin release, appears pivotal, as its dysfunction may lower the threshold for translating suicidal ideation into action.[106] Noradrenergic and dopaminergic systems also exhibit perturbations associated with suicidality. Norepinephrine dysfunction, second only to serotonin in research attention, manifests in altered locus coeruleus activity and receptor binding changes in suicide victims' brains, contributing to deficits in arousal, attention, and stress response.[107] Elevated norepinephrine levels have been noted in specific suicide subtypes, such as carbon monoxide poisoning cases, alongside increased dopamine, potentially reflecting acute hyperarousal or compensatory mechanisms.[108] Dopamine dysregulation, implicated in reward processing and impulsivity, interacts with serotonin to influence coping capacity during suicidal crises, with evidence from pharmacological and postmortem data indicating reduced dopaminergic activity in mood disorders linked to suicide.[109] The hypothalamic-pituitary-adrenal (HPA) axis, central to stress responsivity, shows hyperactivity or blunting in suicidal individuals, with meta-analyses confirming elevated cortisol levels correlated with suicidal behavior, varying by age and modulated by childhood adversity.[110] Blunted HPA reactivity in attempters may impair adaptive stress responses, increasing vulnerability, while chronic hypercortisolemia exacerbates neurotoxicity in regions like the hippocampus.[71] This aligns with the stress-diathesis model, where trait-like HPA alterations interact with environmental stressors to precipitate suicide.[111] Imbalances in excitatory and inhibitory neurotransmission further contribute, with glutamatergic hyperactivity and GABAergic deficits observed in suicide brains. Reduced GABA concentrations or receptor binding in forebrain regions like the frontal cortex and amygdala have been documented in depressed suicide victims, diminishing inhibitory control over aggressive or impulsive drives.[112] Glutamate dysregulation, potentially via NMDA receptor overactivation, promotes excitotoxicity, while neuroinflammation—evidenced by elevated cytokines like interleukin-6—activates the kynurenine pathway, yielding neurotoxic quinolinic acid that depletes serotonin and exacerbates glutamate toxicity.[113][114] These mechanisms underscore a multifactorial neurochemical diathesis, where interconnected deficits amplify risk under stress.[115]Brain Structure and Function
Neuroimaging studies have identified structural alterations in the brains of individuals with suicidal behavior, particularly reductions in gray matter volume in the prefrontal cortex (PFC). Postmortem and MRI-based volumetric analyses reveal decreased PFC volume, including the orbitofrontal and ventromedial regions, in suicide attempters compared to controls, potentially impairing executive functions such as decision-making and impulse inhibition.[116][117] These findings are consistent across mood disorders, where smaller PFC volumes correlate with higher suicide risk, though causality remains unestablished due to confounding factors like chronic illness duration.[118] Hippocampal subfield volumes also show deviations in suicide attempters with major depressive disorder (MDD), including enlarged bilateral hippocampal fissures and reduced overall volume in some cohorts, suggesting atrophy linked to stress-induced glucocorticoid effects.[119][120] Amygdala structural changes are less consistent but include increased right amygdala volume in certain psychiatric populations with suicide history, potentially contributing to heightened emotional reactivity.[121] White matter integrity disruptions, particularly in frontal-subcortical tracts, further indicate impaired connectivity underlying suicidal ideation.[122] Functionally, resting-state fMRI demonstrates aberrant connectivity in suicide-prone individuals, such as hyperconnectivity in the frontoparietal network and reduced PFC-amygdala coupling, which may reflect deficient top-down regulation of threat responses.[123] Task-based fMRI reveals cognitive deficits, including diminished activation in the dorsolateral PFC during emotion processing tasks, aligning with impaired inhibitory control observed in behavioral studies.[72] Positron emission tomography (PET) studies highlight dysfunctional serotonin 1A receptor binding in the PFC and midbrain, with elevated autoreceptor density in suicide victims, suggesting reduced serotonergic tone that exacerbates impulsivity without directly altering gross structure.[124] These functional anomalies persist even after controlling for depression severity, pointing to suicide-specific neural signatures, though replication across larger samples is needed due to methodological heterogeneity.[125]Acute Triggers and Impulsivity
Acute triggers of suicide involve proximal stressors that precipitate the act amid preexisting vulnerabilities, often interacting via a stress-diathesis model where acute events overwhelm coping in predisposed individuals.[126] Empirical data identify common precipitants such as interpersonal conflicts (e.g., arguments or relationship terminations), financial crises, legal issues, and sudden losses including bereavement or job dismissal.[127][128] These acute interpersonal stressors, coupled with diminished social connectedness, correlate with elevated risks of suicidal ideation, attempts, and completions.[129] Diagnosis of acute stress reaction independently elevates completed suicide rates tenfold relative to the general population, underscoring the causal potency of immediate physiological and emotional dysregulation.[130] In adolescents and young adults, maladaptive biological responses to such stressors—such as blunted cortisol reactivity or heightened amygdala activation—may directly underpin acute suicidal crises, representing a failure of adaptive stress buffering rather than mere chronic buildup.[131][132] Acute emotional distress from these triggers, including abrupt symptom worsening or novel conflicts occurring minutes to days prior, frequently signals imminent risk, with evidence linking them to both ideation and lethal outcomes independent of baseline psychopathology.[133][128] Impulsivity amplifies the lethality of these triggers, with 24% of attempters acting on sudden urges without extended planning, and up to 48% reporting impelled actions driven by immediate inclinations rather than premeditation.[134][135] Impulsive attempts characterize younger, unmarried individuals more often, and correlate with higher Barratt Impulsiveness Scale scores (e.g., mean 85.03 in attempters vs. 8.22 in non-attempters on suicide risk measures).[135][136] While trait impulsivity does not always distinguish impulsive from deliberate acts, state-dependent impulsivity—exacerbated by acute intoxication, agitation, or aggression—facilitates rapid escalation from trigger to behavior, serving as a key proximal risk modifier.[137][138] This interplay manifests in low-preparation acts, where brief ideation (e.g., under 10 minutes) precedes many attempts and completions, emphasizing impulsivity's role in bridging chronic diathesis to acute execution; systematic reviews confirm such behaviors as impulsive across definitions, often tied to aggression and poor distress tolerance.[139][140] In clinical contexts, impulsivity emerges as a marker for adolescent inpatient risk, with higher scores predicting attempts amid stressors.[141]Methods
Primary Methods and Their Lethality
The primary methods of suicide worldwide include hanging, firearms discharge, and poisoning, with variations by region influenced by method availability. Hanging, strangulation, and suffocation collectively account for about 48% of global suicide deaths, predominant in low- and middle-income countries due to minimal barriers to access. Firearms are the leading method in high-income nations like the United States, comprising over 50% of suicides there, while pesticide poisoning is common in agricultural regions of Asia and Africa.[142][143][4] Lethality, measured as case fatality rate (CFR)—the proportion of suicide acts resulting in death—differs markedly by method, with more violent or rapid interventions yielding higher rates. A meta-analysis of studies on suicide acts (fatal and non-fatal) found firearms to have the highest CFR at 89.7%, followed closely by hanging or suffocation at 84.5%. Drowning ranks third at 80.4%, while less immediate methods like jumping from heights (46.7%) and gas poisoning (56.6%) are comparably lower. Drug or chemical poisoning generally exhibits the lowest lethality, often below 5-10%, due to potential for timely medical reversal.[144][145][144]| Method | Case Fatality Rate (%) | Notes |
|---|---|---|
| Firearms | 89.7 | Highest lethality; prevalent in regions with high gun ownership.[144][146] |
| Hanging/Suffocation | 84.5 | Globally most common; requires no specialized tools.[144][142] |
| Drowning | 80.4 | Less frequent but highly fatal if uninterrupted.[144] |
| Gas Poisoning | 56.6 | Includes vehicle exhaust; declining with catalytic converters.[144] |
| Jumping from Heights | 46.7 | Urban settings increase access.[144] |
| Pesticide Poisoning | 10-20 | Varies by ingestion volume and antidote availability. (Note: Cited for data point only, not overall reliability) |
Geographic and Temporal Shifts
Suicide methods display pronounced geographic variations, largely determined by the availability of lethal means and cultural practices. Hanging predominates globally as the leading method, comprising over 50% of suicides in most countries and exceeding 80% among males in Eastern European nations such as Lithuania.[143] Firearms account for the majority of suicides in the United States, reaching 60.6% for males and 35.7% for females, with notably lower prevalence in regions with stringent gun controls like Asia and Europe.[143] Pesticide ingestion prevails in agrarian areas of Asia, such as the Republic of Korea (37.5% males, 42.8% females), and Latin America, including El Salvador (86.2% males, 95.1% females), reflecting easy access in rural settings.[143] Drug poisoning is more frequent in Northern Europe and the United Kingdom, while jumping from heights is prominent in densely urbanized areas like Hong Kong (43.3% males, 47.5% females).[143] These patterns underscore how method choice correlates with local access rather than universal preference, with hanging serving as a ubiquitous fallback where other means are restricted.[143] Temporal shifts in suicide methods have been driven by regulatory interventions altering means availability, often resulting in declines in specific poisoning subtypes without full substitution to equally lethal alternatives. In the United Kingdom, suicides by carbon monoxide from coal gas plummeted following the gradual replacement with non-toxic natural gas between the 1960s and 1970s, contributing to an overall reduction in poisoning deaths. Similarly, restrictions on highly toxic pesticides have yielded substantial drops: in Sri Lanka, pesticide suicides fell from 37.4 per 100,000 in 1995 to 11.2 per 100,000 in 2009 after import bans and safer alternatives; in South Korea, paraquat regulations in 2011–2012 reduced pesticide-specific rates; and in Finland, limiting parathion access in the 1960s lowered both poisoning and total suicide mortality.[149][150] Systematic reviews confirm that poison restrictions across 26 countries correlate with method-specific declines, typically without equivalent rises in other methods, thereby lowering overall suicide rates.[151] Concurrently, hanging has risen as a substitute in multiple nations amid poisoning reductions, though not always offsetting the net decrease in lethality. In Norway, male hanging suicides increased at an average annual rate of 1.0% over 44 years ending in 2014.[152] Cyprus saw hanging rise to 49.2% of all suicides by 2017–2020, up from prior decades. In the United States, hanging and asphyxiation surged among adolescents from 1999 to 2020, becoming the predominant method in this group.[153] Japan experienced a similar uptick in hanging post-1979, intensifying after the 1990s economic downturn.[154] These trends highlight hanging's accessibility and high lethality, positioning it as the default in settings where restricted methods previously dominated, yet overall suicide mortality has declined in many contexts due to incomplete substitution.[151]Access and Restriction Impacts
Restriction of access to highly lethal suicide methods has demonstrated effectiveness in reducing overall suicide rates, particularly by interrupting impulsive acts where the availability of means influences completion rates. Empirical studies indicate that limiting such access provides a temporal buffer during acute crises, decreasing method-specific fatalities without substantial substitution to alternative methods.[155][156] This approach leverages the observation that many suicide attempts occur with minimal planning, and denial of preferred means often results in survival rather than switching to equally lethal options.[157] In jurisdictions with greater firearm availability, suicide rates by gunshot are markedly elevated, with household presence of firearms correlating to an 86% usage rate in home suicides versus 6% in non-firearm homes. States permitting easier gun access exhibit higher firearm suicide deaths, comprising over half of total firearm fatalities in the U.S. as of 2020. Handgun ownership specifically elevates self-inflicted gunshot risk eightfold for men and twelvefold for women, underscoring the causal link between access and lethality given the 90% fatality rate of firearm attempts.[158][159][160][161] Physical barriers on bridges and high structures similarly curtail jumping suicides, with installations yielding near-elimination of site-specific incidents and minimal displacement to nearby locations. For instance, barriers have proven highly effective across multiple evaluations, reducing fatalities without corresponding rises elsewhere, as evidenced by pre- and post-installation data from various bridges.[162][163][164] Bans on highly hazardous pesticides in agricultural regions have substantially lowered poisoning suicides, with reductions ranging from 28% to 92% in affected countries like Sri Lanka, India, and China, particularly among youth and females. These restrictions decreased method-specific mortality—for example, a 60.5% drop in standardized pesticide suicide rates in one studied area from 2006 to 2018—while overall suicide attempts persisted but with lower lethality, confirming limited substitution effects.[165][166][167][151]Prevention and Intervention
Therapeutic and Pharmacological Approaches
Cognitive behavioral therapy (CBT), particularly adaptations like CBT for suicide prevention (CBT-SP), targets suicidal ideation and behaviors by addressing cognitive distortions, hopelessness, and problem-solving deficits.[168] Meta-analyses indicate CBT reduces recurrent suicidal behavior among adults by approximately half in the six months post-treatment, with odds ratios around 0.5, though effect sizes for ideation are small (Hedges' g ≈ 0.2-0.3).[169] [170] In adolescents, suicide-focused CBT variants show efficacy in reducing attempts, supported by randomized trials demonstrating lower reattempt rates compared to treatment as usual.[171] However, evidence for long-term suicide mortality reduction remains limited, with most data derived from proxy outcomes like ideation or attempts rather than deaths.[172] Dialectical behavior therapy (DBT), originally developed for borderline personality disorder, emphasizes emotion regulation, distress tolerance, and chain analysis of suicidal behaviors. Randomized controlled trials in high-risk adolescents report DBT halves the odds of repeat suicide attempts versus supportive therapy, with sustained reductions in self-harm up to one year follow-up.[173] Meta-analyses confirm DBT's superiority in decreasing suicidal behaviors across adults and youth, though impacts on ideation may be less pronounced than on acts.[174] Efficacy depends on treatment fidelity, as therapist adherence correlates with outcome improvements, including fewer hospitalizations.[175] Limitations include resource intensity, with full DBT requiring group and individual sessions, potentially limiting scalability in non-specialized settings.[176] Pharmacologically, lithium demonstrates robust anti-suicidal effects in mood disorders, particularly bipolar, with observational and trial data showing 60-80% reductions in suicide risk independent of mood stabilization.[177] A 2021 randomized trial found adjunctive lithium delayed repeat suicide-related events in patients with recent attempts, though overall event rates remained high.[178] Antidepressants, especially SSRIs, are linked to fewer attempts in meta-analyses of ecological and cohort studies, but randomized trials are underpowered for mortality endpoints and show mixed results on ideation.[179] Ketamine and esketamine offer rapid relief, with intravenous ketamine reducing suicidal ideation within hours in major depression (response rates 50-70% at 24 hours), per systematic reviews and RCTs.[180] [181] A 2024 meta-analysis confirmed ketamine's moderate effect on ideation in treatment-resistant cases (SMD ≈ -0.7), though sustained benefits require repeated dosing and monitoring for side effects like dissociation.[182] Clozapine shows promise in schizophrenia-related suicidality, reducing attempts by up to 25% in long-term use.[177] Overall, pharmacological interventions excel in acute risk but lack definitive proof of mortality prevention, with confounding from underlying disorders and potential iatrogenic risks like initial activation in antidepressants.[183] Integrated approaches combining therapy and medication yield additive benefits in reducing attempts, as evidenced by multimodal trials.[184]Means Restriction and Public Policy
Means restriction encompasses public policies that limit access to highly lethal suicide methods, predicated on evidence that many suicide attempts occur impulsively and that reducing availability of such means decreases overall suicide mortality by preventing completions while allowing opportunities for intervention.[185] Empirical studies indicate these interventions can reduce suicide rates by 30-50% in affected populations, with limited full substitution to equivalently lethal alternatives due to differences in method lethality.[186] An umbrella review of means restriction strategies confirms effectiveness across common methods like pesticides, firearms, and jumping sites, though outcomes vary by implementation rigor and cultural context.[187] In the United Kingdom, the phased replacement of toxic coal gas with non-lethal natural gas from the 1960s to 1970s exemplifies successful means restriction; coal gas suicides, which accounted for about one-third of total suicides, fell to zero, contributing to a 33% overall decline in suicide rates from 1963 to 1975 without corresponding increases in other methods.[188] Similarly, Sri Lanka's sequential bans on highly toxic pesticides starting in 1995 reduced pesticide self-poisoning—previously over 70% of suicides—leading to a 70% drop in national suicide rates by 2015, averting an estimated 93,000 deaths, despite some rise in hanging as a substitute method.[189][190] Structural barriers on high bridges demonstrate localized efficacy; the Golden Gate Bridge's 2024 installation of suicide deterrent nets correlated with a 73% reduction in bridge suicides within the first year, aligning with prior analyses projecting 286 lives saved over 20 years at high cost-effectiveness.[191][192] Comparable barriers on other structures, such as Norway's Tromsø Bridge, have similarly curtailed jumping suicides by over 80% at those sites.[193] Firearm restrictions represent a contentious policy domain, with U.S. state-level studies associating stricter licensing, waiting periods, and storage laws with 5-10% lower firearm suicide rates, given firearms' 90% lethality compared to other methods.[194][161] For instance, analyses of laws regulating handgun purchaser age and concealed carry permits link them to reduced overall suicide rates, particularly among youth, though debates persist over confounding factors like rural-urban divides and cultural gun ownership norms.[195][196] Internationally, Australia's 1996 National Firearms Agreement, including buybacks, preceded a sustained decline in firearm suicides without method substitution elevating total rates. Pharmaceutical policies, such as blister packaging of analgesics and limits on pack sizes, have lowered overdose suicides in countries like the UK and Australia by 20-30%, reducing impulsive access. Public policy implementation often involves balancing efficacy against rights concerns, with evidence favoring targeted restrictions on lethal means over broad prohibitions, as supported by systematic reviews emphasizing population-level impacts without evidence of displaced epidemics.[197][187]Screening, Education, and Community Strategies
Screening for suicide risk typically occurs in healthcare, educational, and community settings using brief, validated instruments to identify individuals warranting further assessment. The Ask Suicide-Screening Questions (ASQ), a four-item tool developed by the National Institute of Mental Health, can be administered in approximately 20 seconds and has demonstrated sensitivity in detecting youth at risk in emergency departments and primary care.[198] The Columbia-Suicide Severity Rating Scale (C-SSRS), available in triage versions, evaluates ideation severity, intent, and behavior through a series of questions suitable for children, adolescents, and adults, with validation across diverse populations including clinical and non-clinical contexts.[199] [200] Other tools, such as the Patient Health Questionnaire-9 (PHQ-9) modified for adolescents, incorporate suicide-specific items to gauge depressive symptoms linked to risk.[200] These instruments prioritize brevity and accessibility but require follow-up clinical evaluation, as false positives can occur without contextual assessment.[201] Education strategies focus on building awareness of risk factors, warning signs, and help-seeking behaviors, often implemented in schools and through public campaigns. School-based programs, such as those evaluated in randomized trials, have shown large effect sizes in improving students' knowledge of suicide warning signs and attitudes toward intervention, though reductions in attempts remain inconsistent across studies.[202] [203] For instance, pupil-led education in high schools outperformed teacher training in one analysis by enhancing peer recognition of distress.[203] Public awareness campaigns, like those conducted in Nagoya, Japan, have correlated with temporary declines in suicide counts post-implementation, attributed to increased help-seeking, but long-term impacts on rates are debated due to confounding factors such as economic conditions.[204] These efforts emphasize destigmatizing discussions of suicide without promoting ideation, though evidence from meta-analyses indicates stronger outcomes for knowledge gains than behavioral changes like reduced ideation.[205] Community strategies encompass gatekeeper training, coalitions, and crisis response networks to foster early intervention outside formal healthcare. Gatekeeper programs, such as Question, Persuade, Refer (QPR), train laypersons including teachers, clergy, and family members to identify warning signs, ask direct questions about suicidal intent, and connect individuals to resources; participants report heightened self-efficacy and referral intentions immediately post-training.[206] [207] Systematic reviews confirm improvements in knowledge and stigma reduction, with brief formats effective for broad dissemination, though sustained behavioral referral rates require reinforcement like role-playing.[208] [209] Community coalitions, as outlined in the U.S. National Strategy for Suicide Prevention updated in 2024, promote integrated approaches including local data surveillance and equity-focused outreach, aiming to address disparities in high-risk groups.[210] Crisis hotlines and peer support networks provide immediate, non-judgmental access, with evidence from population-level interventions suggesting they enhance coping and reduce isolation, particularly when embedded in comprehensive plans.[211] These strategies rely on voluntary participation and cultural adaptation, with effectiveness hinging on community buy-in rather than top-down mandates.[212]Evidence on Effectiveness and Limitations
Means restriction strategies, such as barriers on bridges and restrictions on access to firearms or pesticides, demonstrate robust empirical evidence of effectiveness in reducing suicide rates. Population-level interventions, including the detoxification of domestic gas in the United Kingdom during the 1960s and 1970s, correlated with a 30-50% decline in overall suicide rates without substitution to other methods.[213] Similarly, pesticide regulations in Sri Lanka from 1995 onward averted an estimated 13,666 suicides by 2007.[214] An umbrella review of 45 studies confirmed that restricting access to highly lethal methods like firearms and high-rise buildings significantly lowers method-specific and overall suicide mortality, with effects persisting over time.[187] Therapeutic interventions, particularly cognitive behavioral therapy (CBT), show moderate evidence for reducing suicidal ideation and re-attempts in high-risk populations. A network meta-analysis of 54 randomized controlled trials indicated an 87% probability that CBT outperforms other psychotherapies in preventing suicide re-attempts, with moderate-quality evidence.[215] However, effects on completed suicides remain less consistent, as many trials are underpowered for rare outcomes like death.[216] Pharmacological approaches, such as lithium for mood disorders, yield stronger data; meta-analyses of observational and randomized studies report up to an 80% reduction in suicide risk among bipolar patients on long-term lithium, independent of mood stabilization effects.[217] Antidepressants exhibit mixed results, with meta-analyses suggesting reduced attempts in adults but elevated risks in adolescents, prompting regulatory warnings.[218] Despite these findings, limitations pervade the evidence base for suicide prevention. Systematic reviews highlight heterogeneous study designs, small sample sizes, and reliance on surrogate outcomes like ideation rather than completed suicides, which occur infrequently and complicate randomized trials.[203] Many interventions, including hotlines and general screening programs, lack rigorous empirical support, with meta-analyses showing negligible effects on mortality.[219] Publication bias and short follow-up periods further undermine claims of broad efficacy, as initial reductions in attempts may not translate to sustained declines in deaths.[220] Barriers such as treatment non-adherence, access disparities, and clinician underestimation of risk also limit real-world impact, underscoring the need for causal, long-term evaluations over correlational data.[221]Rational Suicide and Euthanasia
Conceptual Foundations
Rational suicide refers to the deliberate termination of one's life by a mentally competent individual, grounded in realistic assessments of one's circumstances, enduring values, and fundamental interests, often to alleviate irremediable suffering or profound loss of autonomy.[222][223] This concept distinguishes itself from impulsive or pathological self-destruction by requiring decision-making capacity free from transient distortions like acute depression or external coercion, emphasizing instead a sustained, reflective choice aligned with the agent's long-term worldview.[224][28] Central to the notion are criteria such as autonomy—the right to self-governance over one's body and fate—and competence, defined as the ability to comprehend relevant information, deliberate rationally, and communicate a consistent preference without undue influence.[225][226] Rationality further demands a realistic appraisal of alternatives, acknowledging that while suffering may be subjective, the decision must weigh evidence-based prospects for relief against the finality of death, rejecting appeals to mere emotional states as insufficient justification.[223] Philosophically, this framework draws on principles of self-ownership and the absence of absolute duties to preserve life, challenging traditional prohibitions that equate all suicide with moral or psychiatric failure.[227][228] Euthanasia intersects with rational suicide when the latter's logic extends to third-party assistance, positing that competent individuals facing terminal conditions or intractable pain retain the prerogative to enlist aid in dying, thereby preserving agency amid physical incapacity.[19] Unlike unassisted rational suicide, which relies solely on personal agency, euthanasia introduces conceptual tensions around beneficence, non-maleficence, and societal roles in facilitating death, often framed as voluntary active euthanasia (direct administration by another) or physician-assisted suicide (provision of lethal means for self-use).[229][20] This distinction underscores that rational suicide prioritizes individual volition without intermediary moral hazards, while euthanasia demands safeguards against slippery slopes toward non-voluntary applications, rooted in empirical observations of decision-making under duress.[230][231]Arguments For and Against
Proponents of rational suicide argue that competent individuals possess an inherent right to self-determination over their lives, including the decision to end them when facing unbearable suffering or loss of dignity, grounded in the philosophical principle of personal autonomy.[232] This view posits that denying such choice infringes on bodily sovereignty, akin to consenting to one's own fate in extremis, as exemplified in historical philosophical defenses where suicide preserves agency against inevitable decline.[232] For euthanasia, advocates extend this to assisted means for those physically unable to act alone, citing empirical cases in jurisdictions like the Netherlands where, by 2022, over 8,000 annual procedures addressed refractory pain or neurodegenerative diseases, with safeguards purportedly ensuring voluntariness.[233] Relief from suffering forms a core empirical justification, asserting that advanced palliative care fails in 5-10% of terminal cases involving multidimensional distress—physical, psychological, and existential—where continued existence equates to torture without meaningful quality.[233] Studies from Belgium indicate that euthanasia patients often report autonomy and dignity as primary motivations, with 77% citing "unbearable suffering" in 2021 reports, arguing that prohibition forces needless prolongation of agony, contravening beneficence.[234] Philosophically, this aligns with utilitarian reasoning that ending suffering maximizes overall welfare, provided capacity assessments confirm rationality over transient despair.[28] Opponents counter with the sanctity of life doctrine, a deontological stance holding human existence as intrinsically valuable and inviolable, rendering intentional self-termination or assistance morally impermissible regardless of consent or suffering, as it equates to devaluing human worth.[232] This perspective, rooted in ethical traditions emphasizing life's inherent purpose, warns that rational suicide rarely attains true rationality, with evidence showing 90% of suicidal ideation linked to treatable mental disorders like depression, even in non-terminal cases among the elderly.[222] [235] The slippery slope argument highlights empirical risks of expansion post-legalization: in the Netherlands, initial 2002 criteria for unbearable suffering in terminal illness broadened by 2023 to include psychiatric conditions and dementia, with cases rising from 1,882 to 8,720 annually, including non-voluntary applications on incompetent patients via advance directives.[236] [237] Similarly, Oregon's assisted suicide law, enacted 1997, saw eligibility extend beyond six-month prognosis limits in practice, with 367 deaths in 2022 amid concerns over unaddressed comorbidities like untreated depression in 40% of cases.[238] Critics argue this fosters coercion vulnerabilities—economic pressures or family burdens—undermining safeguards, as vulnerability assessments prove unreliable, with 25% of Dutch cases involving social isolation factors.[233] [239] Such expansions suggest logical erosion: justifying autonomy for suffering implies permissibility for lesser thresholds, eroding protections for the disabled or depressed.[240]Empirical and Ethical Controversies
Empirical analyses of euthanasia practices in jurisdictions like the Netherlands and Belgium reveal expansions beyond initial terminal illness criteria, with cases increasing for chronic, non-terminal, and psychiatric conditions. In the Netherlands, euthanasia notifications for patients whose suffering was largely due to psychiatric disorders rose to 138 in 2023, up 20% from 115 in 2022, representing a small but growing fraction of total cases amid overall euthanasia deaths reaching approximately 9,068 that year.[241] Similarly, Belgium has permitted euthanasia for non-terminal illnesses since its 2002 law, with debates persisting over its prevalence, estimated in some analyses to include a notable subset of cases not strictly limited to end-stage disease.[242] These shifts have fueled slippery slope concerns, as practices have broadened from voluntary euthanasia for competent adults with unbearable physical suffering to include psychiatric disorders and, in Belgium since 2014, minors of any age under strict conditions, with two such cases reported by 2016.[243][244][245] Proponents of legalization often cite studies finding no empirical slippery slope, arguing that due care criteria are largely adhered to and non-voluntary euthanasia rates have not surged post-legalization.[246][234] However, critics highlight that initial safeguards—such as restricting to terminal cancer patients—have eroded, with Dutch data showing progression to chronic illnesses and youth under 24 requesting medical aid in dying for mental disorders surging from 10 cases in 2012 to 74 in 2020.[247][248] Regret and withdrawal data remain sparse but indicate that about 25% of euthanasia requests in the Netherlands are withdrawn, often due to improved mental states or alternative support, while denied requests have preceded suicides in documented cases, raising questions about assessment accuracy.[249][250] Among psychiatric candidates, depression features as the primary diagnosis in roughly 35% of cases, with 70% having multiple diagnoses, complicating claims of irremediable suffering independent of treatable conditions.[251] Ethically, rational suicide debates center on whether requests reflect autonomous choice or impaired judgment, particularly when depression—potentially underdiagnosed or undertreated—drives the desire for death, as symptoms like hopelessness may masquerade as reasoned evaluation rather than transient illness.[252] Autonomy arguments emphasize patient sovereignty over enduring suffering, provided decisions are uncoerced and informed, yet opponents contend that true voluntariness is elusive amid familial, economic, or societal pressures, especially for vulnerable groups like the disabled or elderly, where subtle coercion could erode protections against abuse.[26][253] Safeguards against manipulation exist in theory, such as multiple consultations, but empirical gaps in verifying enduring competence persist, with some analyses questioning whether psychiatric euthanasia equates to endorsing suicide prevention failures as policy.[254][255] Broader concerns include physician moral distress, with 25% reporting regret post-participation due to lingering doubts about the patient's agency.[256] These tensions underscore causal risks: legalizing rational suicide may inadvertently normalize ending life for reversible despair, prioritizing individual preference over societal duties to alleviate suffering through care rather than cessation.[257]History
Ancient and Pre-Modern Eras
In ancient Egypt, documented instances of suicide were infrequent, with one of the earliest known suicide notes dating to around 1900 BCE, penned by a man expressing anguish over rejection by his lover's family despite his offerings.[258] Literary and historical records provide scattered examples, such as officials or lovers ending their lives amid personal crises, but archaeological evidence remains sparse, indicating it was not normalized or prevalent.[259] In Mesopotamia, self-inflicted death appears even less attested, though elite retainer sacrifices—where servants were killed to accompany rulers to the afterlife—reflect a cultural acceptance of coerced death for hierarchical continuity, distinct from voluntary suicide.[260] Ancient Greek attitudes toward suicide varied across philosophical schools and literary depictions. Deniers, emphasizing societal disruption, opposed it broadly, while proponents allowed it in cases of incurable pain or dishonor.[261] Tragedies by Sophocles and Euripides portrayed suicides as responses to madness, shame, or heroic despair, such as Ajax's self-stabbing after humiliation or Heracles' death following torment by Hera.[262] Prevention was prioritized over condemnation, viewing it as a controllable impulse rather than inherently shameful. Roman views elevated suicide as an act of agency and virtue, particularly for free citizens facing defeat, trial, or enslavement.[263] Notable examples include Cato the Younger slashing his veins in 46 BCE to defy Julius Caesar and Seneca ordering his forced suicide in 65 CE under Nero, both framed as stoic assertions of autonomy.[264] Lucretia's stabbing in response to rape around 509 BCE symbolized civic honor, inspiring republican ideals. Slaves and certain outcasts faced restrictions, underscoring its privilege as a marker of status. In ancient India, practices like sati—widows self-immolating on husbands' pyres—emerged as ritually sanctioned, often altruistic acts tied to dharma, though texts like the Manusmriti prohibited general self-killing.[265] Jauhar, mass suicides by Rajput women during sieges to evade capture, exemplified collective honor preservation from medieval periods onward. Ascetic traditions permitted sallekhana, voluntary fasting to death for spiritual purification, distinguishing it from impulsive suicide. Feudal Japan institutionalized seppuku among samurai by the 12th century as a means to atone for failure or restore family honor, involving ritual disembowelment followed by decapitation. This contrasted with broader East Asian views, where Confucian emphasis on filial piety generally discouraged self-harm, though isolated honorable deaths occurred in Chinese annals. Pre-modern shifts under Abrahamic dominance imposed prohibitions. Judaism rejected suicide as violating the sanctity of life granted by God, with Talmudic rulings equating it to murder.[266] Early Christianity, drawing from Augustine's 5th-century condemnation as theft from God, entrenched it as a mortal sin barring salvation. In medieval Europe, canon law denied Christian burial to suicides, while secular authorities confiscated goods and permitted public shaming or mutilation of corpses, reflecting fears of demonic influence.[267][268] Islam paralleled this, deeming suicide a grave offense against Allah's will, punishable eternally in hadiths. These frameworks supplanted pagan rationales for self-killing, prioritizing communal and divine order over individual resolve.19th to 20th Century Developments
During the 19th century, suicide rates appeared to rise across Europe, particularly between 1860 and 1880, coinciding with improved vital registration systems that enabled more accurate enumeration through coroners' inquests and official statistics in countries like England and Wales starting from 1861.[269][270] This empirical data collection facilitated the first large-scale analyses, revealing patterns such as higher male rates peaking at 28 per 100,000 in England during the 1890s, and prompted a reconceptualization of suicide from a criminal or sinful act to a social or pathological condition.[271] Émile Durkheim's 1897 book Suicide utilized these statistics from European nations to argue that suicide rates inversely correlated with social integration, categorizing them into egoistic (low integration), altruistic (excessive integration), anomic (normative deregulation), and fatalistic (excessive regulation) types, thereby founding suicide as a subject of sociological inquiry independent of individual psychology.[272][273] In psychiatry, early 19th-century French alienists like Jean-Étienne Esquirol framed suicide as a symptom of monomania or partial insanity, broadening the insanity defense in legal contexts and contributing to the medicalization of the act, though lay juries often determined verdicts rather than medical experts.[274] By the early 20th century, Sigmund Freud's 1917 essay "Mourning and Melancholia" advanced a psychoanalytic model, positing suicide as an internalized aggression stemming from ambivalence toward lost love objects, where the ego attacks itself as a surrogate, resolving the paradox of self-directed hostility.[275][276] This theory influenced subsequent psychiatric views, emphasizing unconscious conflicts over purely somatic or environmental factors, though it lacked empirical validation through controlled studies. Legal attitudes evolved unevenly; while suicide remained a felony in England until the Suicide Act of 1961 decriminalized attempts, 19th-century reforms softened punishments by expanding insanity pleas and allowing daytime burials from 1882, reflecting secularization amid rising reported incidents.[277][274] The 20th century saw attempted suicide increasingly treated as a psychiatric emergency rather than a crime, with institutional responses in places like Queensland, Australia, integrating community oversight by 1950, though self-harm methods like cut-throats persisted as concerns into the 1930s due to their lethality and social visibility.[278][279] These shifts laid groundwork for mid-century suicide prevention efforts, influenced by Durkheim's legacy, prioritizing social and clinical interventions over punitive measures.[273]Contemporary Shifts Post-2000
Globally, suicide rates have declined by approximately 35% since 2000, with the age-standardized rate falling from around 13 per 100,000 in 2000 to about 9 per 100,000 by 2019, according to World Health Organization estimates, reflecting improvements in some low- and middle-income countries through interventions like pesticide restrictions and economic development.[280] [281] However, this trend masks regional variations, including persistent or rising rates in parts of Europe and North America, where socioeconomic factors, mental health service gaps, and cultural shifts have counteracted broader gains.[282] In the United States, suicide rates rose steadily by 30-35% from 10.4 per 100,000 in 2000 to a peak of 14.2 per 100,000 in 2018, before a temporary dip to 13.5 in 2020 amid COVID-19 lockdowns, rebounding to over 14 per 100,000 by 2022, with more than 49,000 deaths recorded in 2023.[4] [5] This increase has disproportionately affected middle-aged men, linked to factors such as economic stagnation following the 2008 recession, the opioid epidemic peaking in the 2010s, and social isolation, though causal mechanisms remain debated with empirical evidence pointing to multifactorial drivers rather than singular psychiatric explanations.[283] Among youth, adolescent suicide rates climbed across all methods from 1999 to 2020, with a 95% surge for ages 10-14 and notable rises for females using suffocation, coinciding temporally with widespread smartphone adoption and social media proliferation around 2012, which studies associate with heightened risks through mechanisms like cyberbullying, sleep disruption, and exposure to self-harm content, though direct causation requires further longitudinal validation.[153] [284] [283] Shifts in suicide methods post-2000 reflect adaptations to availability and lethality, with hanging and suffocation overtaking poisoning in many high-income settings due to restrictions on toxic substances like pesticides and carbon monoxide, while firearm use remained dominant in the US, accounting for over half of male suicides by the 2010s.[285] [286] Means restriction policies, such as Sri Lanka's 1990s-2000s bans on highly toxic pesticides extended into broader enforcement, demonstrated effectiveness in reducing overall rates without full method substitution, averting an estimated 20-30% of potential deaths in affected populations.[213] [151] In response, public health strategies evolved toward infrastructure changes, including bridge barriers and firearm storage counseling, alongside digital interventions to curb online contagion, though overall efficacy has been uneven, with US rates persisting amid debates over underlying social and economic contributors.[283]Cultural and Religious Perspectives
Abrahamic Religions
In Judaism, suicide is prohibited as a violation of the sanctity of life, which is viewed as belonging to God rather than the individual. Although the Torah contains no explicit command against self-killing, rabbinic authorities derive the ban from verses such as Genesis 9:5, which demands accountability for shedding one's own blood, interpreting the prohibition against murder (Exodus 20:13) to encompass self-destruction.[266] The Talmud does not directly forbid it but implies condemnation through discussions of life's divine ownership, with post-Talmudic texts like Semahot reinforcing that the body is merely entrusted by God, precluding self-harm or termination.[287] [288] Rare historical exceptions appear in cases of imminent forced transgression of severe commandments, such as idolatry or sexual violation during persecution, as in the martyrdoms of figures like the mother and seven sons in 2 Maccabees (accepted in some Jewish traditions), but these are distinguished from despair-driven acts and not endorsed as normative.[289] Christian doctrine uniformly condemns suicide as a grave sin against God's sovereignty over human life. Early Church Fathers, particularly Augustine of Hippo in The City of God (Book I, circa 413–426 CE), argued that it contravenes the Sixth Commandment ("Thou shalt not kill," Exodus 20:13) by usurping divine authority and failing to love oneself as a neighbor (Mark 12:31), even in cases of suffering or shame.[290] This view solidified through Church councils and canon law, equating suicide with self-murder and barring ecclesiastical burial until reforms in the 19th–20th centuries allowed pastoral discretion for mental distress.[291] Distinctions persist between suicide and martyrdom, where death results from fidelity to faith under persecution rather than self-initiated escape, as exemplified by early Christian saints facing execution. Protestant traditions, drawing from the same scriptural base, generally echo this prohibition, though some Reformers like Luther emphasized God's mercy potentially overriding human judgment on eternal fate.[292] In Islam, suicide constitutes a major sin (kaba'ir), explicitly forbidden in the Quran (4:29: "Do not kill yourselves or one another") and elaborated in hadith as meriting eternal punishment in Hellfire replicating the method of death—such as perpetual stabbing for one who stabs himself.[293] The Prophet Muhammad warned that "he who commits suicide by throttling shall keep on throttling himself in the Fire," underscoring its gravity as despair against divine decree, with no redemptive exceptions even under duress.[294] This stance reflects the belief that life is a trust (amanah) from Allah, to be preserved until natural death, barring entry to Paradise for the perpetrator absent repentance before death, though ultimate judgment rests with God.[295] Martyrdom in defensive jihad differs fundamentally, as it involves combat against aggressors rather than self-inflicted harm for personal relief.[296]Eastern Traditions
In Hinduism, suicide is generally prohibited as a violation of ahimsa (non-violence) and the duty to preserve life across reincarnations, with texts like the Manusmriti equating it to murder and prescribing penalties such as wandering as a ghost for years.[297] However, exceptions existed for religiously motivated acts, including sati (widow self-immolation on her husband's funeral pyre, practiced historically until banned by British colonial law in 1829 and reinforced in independent India in 1987) and prayopavesa (voluntary fasting by the terminally ill or ascetics under strict ritual conditions).[298] These were viewed as paths to spiritual merit rather than despair-driven suicide, though modern Hindu interpretations overwhelmingly condemn all forms due to karmic repercussions and ethical evolution.[299] Jainism distinguishes sallekhana (or santhara), a voluntary fast unto death by gradually reducing food and water intake, as a non-violent spiritual purification rather than suicide, undertaken by ascetics or laypersons facing inevitable death to shed karma and attachments.[300] Documented since at least the 5th century BCE in texts like the Acaranga Sutra, it requires guru approval, mental resolve, and detachment from worldly ties, with an estimated 200-300 cases annually in India as of 2015, though courts have occasionally challenged it legally as akin to suicide.[301] Proponents argue it aligns with ahimsa by avoiding harm to self or others through sudden violence, contrasting with impulsive self-killing.[302] Buddhist doctrine, rooted in the first precept against taking life, views ordinary suicide as generating negative karma due to attachment, anger, or delusion, potentially leading to rebirth in lower realms, as exemplified in the Vinaya texts where monks who self-immolate face expulsion.[303] Yet, for enlightened arhats (those free of defilements), self-ending may be neutral or meritorious, as in the case of the monk Godhula's scriptural suicide to aid others, though such instances are rare and not prescriptive for laypersons.[304] Theravada and Mahayana traditions emphasize enduring suffering for enlightenment, with historical self-immolations in China (e.g., during 1960s protests) blending protest and devotion but diverging from core precepts.[305] In Chinese traditions, Confucianism permits suicide as a means to uphold ren (humaneness) and virtue, such as jingjie (remonstrative suicide to protest injustice) or to avoid dishonor, as seen in historical figures like Qu Yuan (c. 340–278 BCE) who drowned himself in loyalty to his ideals, influencing rates where intellectuals faced execution.[306] Taoism adopts a more fluid stance, viewing death as natural transformation akin to seasonal change, with texts like the Zhuangzi (4th century BCE) portraying voluntary death by enlightened sages as harmonious release from bodily constraints, though not endorsing despair-motivated acts.[307] Japanese samurai culture ritualized seppuku (disembowelment with a wakizashi blade, often followed by decapitation by a second), emerging in the 12th century amid feudal wars as a code of honor under bushido, influenced by Zen Buddhism's emphasis on detachment and Shinto purity.[308] Performed by over 1,000 recorded instances during the Sengoku period (1467–1603), it restored family name or evaded capture, with the 1663 Yamaga Sokō treatise codifying procedures; post-Meiji Restoration (1868), it persisted until Emperor Hirohito's 1945 ban amid WWII kamikaze extensions.[309] Modern views frame it as cultural relic, not endorsement of suicide.[310]Secular and Philosophical Views
In ancient Stoic philosophy, suicide was regarded as a permissible rational choice under specific conditions, such as when life becomes incompatible with virtue or involves intolerable suffering. Seneca, in his Letters to Lucilius, argued that the wise person may exit life voluntarily if circumstances prevent eudaimonia, viewing death as neither good nor evil but indifferent, with suicide serving as an "open door" to escape unendurable pain or tyranny.[311] Epictetus echoed this, permitting self-killing only in extreme cases like enslavement or loss of autonomy, emphasizing control over one's end rather than passive endurance.[312] During the Enlightenment, David Hume challenged prevailing prohibitions in his 1783 essay Of Suicide, contending that it violates no duties to society, self-preservation, or providence, as individuals possess sovereignty over their lives akin to property rights. Hume reasoned that suicide could alleviate greater harms, dismissing religious objections by arguing even divine order allows rational self-exit when life yields net misery.[24] In contrast, Immanuel Kant categorically opposed suicide in his Lectures on Ethics (circa 1770s-1790s), asserting it contravenes the categorical imperative by treating the self as a means to end suffering rather than an end in itself, thus undermining rational autonomy and moral law. Kant viewed it as self-degradation below animal instinct, permissible only hypothetically to preserve rationality in dire threats like torture.[313] Nineteenth-century thinker Friedrich Nietzsche reframed suicide positively in works like Twilight of the Idols (1889), praising the "free death" chosen at one's peak as an affirmation of will to power, while decrying Christian denaturalization of it as weakness. He saw contemplation of suicide as consoling through dark periods, enabling endurance, but advocated timing it for maximal life-affirmation rather than despair.[314] In the twentieth century, existentialists like Albert Camus in The Myth of Sisyphus (1942) posed suicide as the fundamental philosophical question amid life's absurdity, ultimately rejecting it in favor of defiant rebellion through living fully despite meaninglessness. Jean-Paul Sartre, emphasizing radical freedom, implicitly opposed suicide as an evasion of authentic responsibility, though his framework allowed autonomy in facing nausea and contingency. Utilitarian perspectives vary: act-utilitarians like Jeremy Bentham (1748-1832) might endorse suicide if it maximizes pleasure minus pain for the individual and society, such as terminating prolonged agony without dependents' undue burden. Rule-utilitarians, however, often caution against general permission, citing empirical risks of impulsive acts increasing overall harm, as evidenced by higher regret in attempts versus completions.[315] Modern secular ethics, drawing from these traditions, prioritize autonomy and harm minimization, with debates centering on rational capacity—suicide deemed permissible for competent adults in irremediable suffering but discouraged amid treatable mental illness, per evidence from longitudinal studies showing 90% of survivors do not reattempt.[316]Legal Frameworks
Decriminalization and Regulation
In common law jurisdictions, suicide was historically treated as a felony, with successful suicide forfeiting the perpetrator's goods to the crown and burial denied Christian rites, while attempted suicide constituted a misdemeanor punishable by imprisonment or pillory.[277] This framework stemmed from medieval ecclesiastical and secular prohibitions viewing self-killing as usurping divine authority over life. Decriminalization gained momentum in the 20th century as medical understandings of mental illness supplanted moral condemnation, recognizing attempts as symptoms of treatable conditions rather than willful crimes.[317] The Suicide Act 1961 marked a pivotal reform in England and Wales, explicitly abrogating the common law rule criminalizing suicide and ensuring that survivors of attempts faced no prosecution.[318] In the United States, suicide derived from English common law but was progressively eliminated from state statutes, with the last decriminalizations occurring in New Jersey in 1971, North Carolina and North Dakota in 1973, and Washington in 1976; today, no state imposes criminal penalties for attempts alone.[319] These shifts reflected broader civil rights advancements and empirical observations that criminal sanctions deterred help-seeking without reducing rates.[320] Globally, attempted suicide remains a criminal offense in approximately 23 countries as of 2023, primarily in regions like sub-Saharan Africa, the Middle East, and parts of Asia, where penalties range from fines to imprisonment up to three years, often under penal codes labeling it as "abetting one's own death."[321] Notable recent decriminalizations include India via the Mental Healthcare Act of 2017, which repealed Section 309 of the Indian Penal Code, and Guyana in 1998, driven by advocacy highlighting how criminalization stigmatizes survivors and burdens mental health systems.[322] In these jurisdictions, enforcement varies, but data indicate no correlation between criminalization and lower suicide rates, as socioeconomic factors dominate incidence.[323] Post-decriminalization regulations emphasize prevention and intervention over punishment. Assisting or encouraging suicide is prohibited in most nations, such as under Section 2 of the UK's Suicide Act 1961, which carries up to 14 years' imprisonment to safeguard vulnerable individuals from coercion.[324] Following an attempt, civil mechanisms prevail, including mandatory mental health evaluations and potential involuntary hospitalization under criteria like imminent danger to self, as in U.S. statutes modeled on standards like California's Lanterman-Petris-Short Act (1967), which authorizes 72-hour holds for assessment.[10] These protocols prioritize empirical risk assessment via standardized tools, though critics argue they can infringe autonomy without clear causal reductions in recidivism.[325] Coroners' inquests classify completed suicides as non-criminal deaths, informing public health data but excluding punitive elements.[326]Assisted Suicide Laws
Assisted suicide, defined as the act of intentionally providing a person with the means or knowledge to commit suicide, with the explicit intention of enabling that act, is permitted under specific legal frameworks in a limited number of jurisdictions worldwide. These laws typically restrict eligibility to mentally competent adults experiencing unbearable physical suffering from incurable conditions, often requiring multiple medical assessments, waiting periods, and reporting to authorities to prevent abuse. Empirical data from jurisdictions with longstanding laws, such as the Netherlands, indicate steady increases in cases since legalization, with 9,068 euthanasia and assisted suicide deaths reported in 2023, representing 5% of all deaths, though safeguards aim to ensure voluntariness.[327][328][329] In Europe, the Netherlands was the first country to explicitly legalize both euthanasia and assisted suicide through the Termination of Life on Request and Assisted Suicide (Review Procedures) Act of April 1, 2002, allowing it for patients aged 12 and older with unbearable suffering that cannot be alleviated, subject to review by regional committees. Belgium followed with similar legislation on September 28, 2002, extending to psychiatric conditions since 2014, with 2,966 cases in 2022 comprising 2.5% of deaths. Switzerland permits assisted suicide under Article 115 of its Penal Code since 1942, exempting it from punishment if not motivated by selfish reasons, enabling non-profit organizations like Dignitas to assist both residents and foreigners without requiring terminal illness, provided the patient self-administers the lethal substance; approximately 1,200 foreigners sought assistance there in 2023. Other European nations include Austria, where a 2022 constitutional court ruling decriminalized it for unbearable suffering; Germany, following a 2020 Federal Constitutional Court decision allowing organized assistance without prosecution; Luxembourg since 2009; and Spain, which legalized both euthanasia and assisted suicide in March 2021 for serious, incurable illnesses causing intolerable suffering.[330][331][332]| Jurisdiction | Year Effective | Eligibility Criteria | Key Safeguards |
|---|---|---|---|
| Netherlands | 2002 | Unbearable suffering (physical or mental), no age minimum for children under parental consent | Two physicians' approval, independent review committee |
| Belgium | 2002 | Unbearable psychological or physical suffering from serious disorder | Two doctors, waiting period, federal commission review |
| Switzerland | 1942 (de facto) | No terminal illness required; self-administration mandatory | Not for selfish motives; physician consultation optional |
| Canada | 2016 (expanded 2021) | Grievous, irremediable condition causing intolerable suffering; includes non-terminal since expansion | Two independent assessments, 10-day reflection period (waivable) |
| Oregon (US) | 1997 | Terminal illness with <6 months prognosis, age 18+ | Two oral requests, written request, two physicians' confirmation |
| Australia (Victoria) | 2019 | Terminal illness <6 months, unbearable suffering | Multiple approvals, mandatory reporting |
International Variations
As of 2024, attempted suicide remains a criminal offense in 23 countries, including the Bahamas, Bangladesh, Brunei Darussalam, Guyana, Kenya (prior to its 2025 decriminalization), Malaysia, Nigeria, Pakistan, Papua New Guinea, Sierra Leone, Singapore, South Korea, Sri Lanka, Trinidad and Tobago, and several others predominantly in Africa and Asia, where penalties can include fines, imprisonment up to three years, or corporal punishment.[335] In nations adhering to Sharia law, such as Brunei and parts of Nigeria and Pakistan, suicide attempts may incur additional religious-based sanctions, including potential death penalties under strict interpretations, though enforcement varies.[336] These laws often stem from colonial-era penal codes or religious doctrines that view self-harm as a moral or societal transgression, contrasting with the decriminalization trend in over 170 countries, driven by human rights arguments and recognition that criminalization hinders prevention efforts.[337] Recent reforms include Kenya's High Court ruling on January 9, 2025, striking down Section 226 of its Penal Code as unconstitutional, and the United Arab Emirates' 2025 amendments removing criminal penalties for attempts while maintaining prohibitions on facilitation.[338][339] Legal frameworks for assisted suicide and euthanasia exhibit greater variation, with permissive regimes in approximately 15 jurisdictions as of mid-2023, primarily in Europe, North America, and Oceania, while remaining strictly prohibited elsewhere.[340] In the Netherlands, euthanasia and physician-assisted suicide have been legal since 2002 for patients experiencing unbearable suffering with no prospect of improvement, regardless of terminal status, with over 8,000 cases annually by 2022 under strict procedural safeguards including second medical opinions.[341] Belgium legalized both in 2002, extending eligibility to minors with parental consent since 2014 and to psychiatric conditions, reporting around 2,900 euthanasia deaths in 2022.[342] Switzerland permits assisted suicide since 1942 under organizations like Dignitas, without residency requirements, attracting international cases but prohibiting direct euthanasia.[334] Canada authorized medical assistance in dying (MAiD) in 2016, expanding in 2021 to non-terminal patients with grievous and irremediable conditions, resulting in 13,000 deaths in 2022, though debates persist over safeguards amid rising utilization.[343] In contrast, assisting suicide carries severe penalties in most jurisdictions, such as up to 14 years imprisonment in England, Wales, and Northern Ireland, or life sentences in some U.S. states and many Islamic countries like Saudi Arabia, where it is equated with murder under religious law.[334] Australia demonstrates subnational variation, with voluntary assisted dying legalized in all six states by 2022-2025 but not federally, featuring residency requirements and terminal illness criteria in most.[331] Latin American exceptions include Colombia's 1997 Constitutional Court decriminalization of euthanasia for terminal patients, expanded in 2021 to non-terminal cases, though implementation lags due to regulatory gaps.[344] These divergences reflect cultural, religious, and ethical priorities: permissive laws often emphasize autonomy and suffering relief in secular contexts, while prohibitions prioritize sanctity of life, with empirical data showing no consistent spike in overall suicide rates post-legalization in jurisdictions like the Netherlands.[345]| Region | Criminalization of Attempts | Assisted Dying Status |
|---|---|---|
| Europe (select) | Decriminalized in most (e.g., EU nations) | Legal in Netherlands, Belgium, Switzerland, Spain (2021), Portugal (decriminalized 2023)[346] |
| North America | Decriminalized | Legal in Canada (federal); U.S. states like Oregon (1997), varying by jurisdiction[343] |
| Asia/Middle East | Criminal in ~10 countries (e.g., Malaysia, UAE pre-2025) | Prohibited; exceptions rare (e.g., Japan decriminalized assistance in some contexts but no formal euthanasia)[339] |
| Africa | Criminal in several (e.g., Nigeria, Sierra Leone) | Prohibited universally[335] |
| Oceania | Decriminalized | Legal in New Zealand (2021), Australian states[331] |
.jpg/250px-Édouard_Manet_-_Le_Suicidé_(ca._1877).jpg)
.jpg)




![Death rate from suicide per 100,000 as of 2017[236]](http://upload.wikimedia.org/wikipedia/commons/thumb/0/01/Death_rate_from_suicides_%28IHME_%281990_to_2016%29%29%2C_OWID.svg/330px-Death_rate_from_suicides_%28IHME_%281990_to_2016%29%29%2C_OWID.svg.png)
![Share of deaths from suicide, 2017[237]](http://upload.wikimedia.org/wikipedia/commons/thumb/6/6a/Share_of_deaths_from_suicide%2C_OWID.svg/330px-Share_of_deaths_from_suicide%2C_OWID.svg.png)