Recent from talks
Contribute something
Nothing was collected or created yet.
Cannabis (drug)
View on Wikipedia
| Cannabis | |
|---|---|
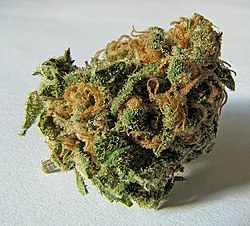
 Cannabis in the drying phase | |
| Pronunciation |
|
| Source plant(s) | Cannabis sativa, Cannabis indica, Cannabis ruderalis[a] |
| Part(s) of plant | Flower and fruit |
| Geographic origin | Central or South Asia |
| Active ingredients | Tetrahydrocannabinol, cannabidiol, cannabinol, tetrahydrocannabivarin |
| Main producers | Afghanistan, Canada, China, Colombia, India, Jamaica, Lebanon, Mexico, Morocco, Netherlands, Pakistan, Paraguay, Spain, Thailand, Turkey, United Kingdom, United States |
| Legal status |
|
| Part of a series on |
| Cannabis |
|---|
 |
Cannabis (/ˈkænəbɪs/),[2] commonly known as marijuana (/ˌmærəˈwɑːnə/),[3] weed, pot, and ganja, among other names, is a non-chemically uniform psychoactive drug from the Cannabis plant. Native to Central or South Asia, cannabis has been used as a drug for both recreational and entheogenic purposes and in various traditional medicines for centuries. Tetrahydrocannabinol (THC) is the main psychoactive component of cannabis, which is one of the 483 known compounds in the plant, including at least 65 other cannabinoids, such as cannabidiol (CBD). Cannabis can be used by smoking, vaporizing, within food, or as an extract.
Cannabis has various mental and physical effects, which include euphoria, altered states of mind and sense of time, difficulty concentrating, impaired short-term memory, impaired body movement (balance and fine psychomotor control), relaxation, and an increase in appetite. Onset of effects is felt within minutes when smoked, but may take up to 90 minutes when eaten (as orally consumed drugs must be digested and absorbed). The effects last for two to six hours, depending on the amount used. At high doses, mental effects can include anxiety, delusions (including ideas of reference), hallucinations, panic, paranoia, and psychosis. There is a strong relation between cannabis use and the risk of psychosis, though the direction of causality is debated.[4][5] Physical effects include increased heart rate, difficulty breathing, nausea, and behavioral problems in children whose mothers used cannabis during pregnancy; short-term side effects may also include dry mouth and red eyes. Long-term adverse effects may include addiction, decreased mental ability in those who started regular use as adolescents,[6] heart disease, chronic coughing, susceptibility to respiratory infections, and cannabinoid hyperemesis syndrome.[7]
Cannabis is mostly used recreationally or as a medicinal drug, although it may also be used for spiritual purposes. There is mixed and inconclusive evidence on the benefits of medical cannabis.[8] In 2013, between 128 and 232 million people used cannabis (2.7% to 4.9% of the global population between the ages of 15 and 65). It is the most commonly used largely-illegal drug in the world, with the highest use among adults in Zambia, the United States, Canada, and Nigeria. Since the 1970s, the potency of illicit cannabis has increased, with THC levels rising and CBD levels dropping.
Cannabis plants have been grown since at least the 3rd millennium BCE and there is evidence of it being smoked for its psychoactive effects around 500 BCE in the Pamir Mountains, Central Asia. Since the 14th century, cannabis has been subject to legal restrictions. The possession, use, and cultivation of cannabis has been illegal in most countries since the 20th century. In 2013, Uruguay became the first country to legalize recreational use of cannabis. Other countries to do so are Canada, Georgia, Germany, Luxembourg, Malta, South Africa, and Thailand. In the U.S., the recreational use of cannabis is legalized in 24 states, 3 territories, and the District of Columbia, though the drug remains federally illegal. In Australia, it is legalized only in the Australian Capital Territory.
Etymology
[edit]The origins of Cannabis are linked to a Scythian word.[9][10][11] The ancient Greeks may have learned of the use of cannabis, which they called κάνναβις, by observing Scythian funerals, during which cannabis was consumed.[10] In Akkadian, cannabis was known as qunubu (𐎯𐎫𐎠𐎭𐏂).[10] The word was adopted in to the Hebrew as qaneh bosem (קָנֶה בֹּשׂם).[10]
The Latin term cannabis derived from Greek evolved into Proto-Germanic *xan(a)paz, yielding various Germanic forms (Old Norse hampr, Old English hænep, Old Saxon hanup, Old High German hanaf) and ultimately modern British English "hemp."[12]
Uses
[edit]Medical
[edit]
Medical cannabis, or medical marijuana, refers to the use of herbal cannabis or its preparations to treat disease or improve symptoms. There is no single agreed-upon definition (e.g., cannabinoids derived from cannabis and synthetic cannabinoid analogs are also used).[13][14][15] The rigorous scientific study of cannabis as a medicine has been hampered by production restrictions and by the fact that it is classified as an illegal drug by many governments.[16]
Overall, there is mixed evidence on the benefits of cannabis-based medicines, frequent mild adverse effects, and generally low-to-moderate quality of evidence.[17]
There is some evidence suggesting cannabis can be used to reduce nausea and vomiting during chemotherapy, to improve appetite in people with HIV/AIDS, or to treat chronic pain and muscle spasms. Evidence for its use for other medical applications is insufficient for drawing conclusions about safety or efficacy.[18][19][20] There is evidence supporting the use of cannabis or its derivatives in the treatment of chemotherapy-induced nausea and vomiting, neuropathic pain, and multiple sclerosis. Lower levels of evidence support its use for AIDS wasting syndrome, epilepsy, rheumatoid arthritis, and glaucoma.[21]
The medical use of cannabis is legal only in a limited number of territories, including Canada,[22] Belgium, Australia, the Netherlands, New Zealand,[23][24] Spain, and many U.S. states. This usage generally requires a prescription, and distribution is usually done within a framework defined by local laws.[21]
Recreational
[edit]Being under the effects of cannabis is usually referred to as being "high".[25] Cannabis consumption has both psychoactive and physiological effects.[26] The "high" experience can vary widely, based (among other things) on the user's prior experience with cannabis, and the type of cannabis consumed.[27]: p647 When smoking cannabis, a euphoriant effect can occur within minutes of smoking.[28]: p104 Aside from a subjective change in perception and mood, the most common short-term physical and neurological effects include increased heart rate, increased appetite, impairment of short-term and working memory, and impairment of psychomotor coordination.[29][30]
Additional desired effects from consuming cannabis include relaxation, a general alteration of conscious perception, increased awareness of sensation, increased libido[31] and distortions in the perception of time and space. In some cases, cannabis can lead to dissociative states such as depersonalization[32][33] and derealization.[34]
Spiritual
[edit]Cannabis has held sacred status in several religions and has served as an entheogen – a chemical substance used in religious, shamanic, or spiritual contexts[35] – in the Indian subcontinent since the Vedic period. The earliest known reports regarding the sacred status of cannabis in the Indian subcontinent come from the Atharva Veda, estimated to have been composed sometime around 1400 BCE.[36] The Hindu god Shiva is described as a cannabis user, known as the "Lord of bhang".[37]: p19
In modern culture, the spiritual use of cannabis has been spread by the disciples of the Rastafari movement who use cannabis as a sacrament and as an aid to meditation.[36]
Consumption
[edit]Modes of consumption
[edit]
Many different ways to consume cannabis involve heat to decarboxylate THCA into THC;[38][39] common modes include:
- Smoking, involves burning and inhaling cannabinoids ("smoke") from small pipes, bongs (portable versions of hookahs with a water chamber), paper-wrapped joints, tobacco-leaf-wrapped blunts, or the like.[40]
- Vaporizing, heating various forms of cannabis to 165–190 °C (329–374 °F),[41] causing the active ingredients to form vapor without combustion of the plant material (the boiling point of THC is 157 °C (315 °F) at atmospheric pressure).[42]
- Edibles, adding cannabis as an ingredient to a wide variety of foods, including butter and baked goods. In India it is commonly consumed as the beverage bhang.
- Cannabis tea, prepared with attention to the lipophilic quality of THC, which is only slightly water-soluble (2.8 mg per liter),[43] often involving cannabis in a saturated fat.[44]
- Tincture of cannabis, sometimes known as green dragon, is an alcoholic cannabis concentrate.
- Capsules, typically containing cannabis oil, and other dietary supplement products, for which some 220 were approved in Canada in 2018.[22]
Consumption by country
[edit]| Substance | Best estimate |
Low estimate |
High estimate |
|---|---|---|---|
| Amphetamine- type stimulants |
34.16 | 13.42 | 55.24 |
| Cannabis | 192.15 | 165.76 | 234.06 |
| Cocaine | 18.20 | 13.87 | 22.85 |
| Ecstasy | 20.57 | 8.99 | 32.34 |
| Opiates | 19.38 | 13.80 | 26.15 |
| Opioids | 34.26 | 27.01 | 44.54 |
In 2013, between 128 and 232 million people used cannabis (2.7% to 4.9% of the global population between the ages of 15 and 65).[46] Cannabis is by far the most widely used illicit substance,[47] with the highest use among adults (as of 2018[update]) in Zambia, the United States, Canada, and Nigeria.[48]
United States
[edit]Between 1973 and 1978, eleven states decriminalized marijuana.[49] In 2001, Nevada reduced marijuana possession to a misdemeanor and since 2012, several other states have decriminalized and even legalized marijuana.[49]
In 2018, surveys indicated that almost half of the people in the United States had tried marijuana, 16% had used it in the past year, and 11% had used it in the past month.[50] In 2014, surveys said daily marijuana use amongst US college students had reached its highest level since records began in 1980, rising from 3.5% in 2007 to 5.9% in 2014 and had surpassed daily cigarette use.[51]
In the US, men are over twice as likely to use marijuana as women, and 18–29-year-olds are six times more likely to use as over-65-year-olds.[52] In 2015, a record 44% of the US population has tried marijuana in their lifetime, an increase from 38% in 2013 and 33% in 1985.[52]
Marijuana use in the United States is three times above the global average, but in line with other Western democracies. Forty-four percent of American 12th graders have tried the drug at least once, and the typical age of first-use is 16, similar to the typical age of first-use for alcohol but lower than the first-use age for other illicit drugs.[47]
A 2022 Gallup poll concluded Americans are smoking more marijuana than cigarettes for the first time.[53]
Adverse effects
[edit]Short-term
[edit]
Acute negative effects may include anxiety and panic, impaired attention and memory, an increased risk of psychotic symptoms,[b] the inability to think clearly, and an increased risk of accidents.[56][57][58] Cannabis impairs a person's driving ability, and THC was the illicit drug most frequently found in the blood of drivers who have been involved in vehicle crashes. Those with THC in their system are from three to seven times more likely to be the cause of vehicle crash than those who had not used either cannabis or alcohol.[59][60][c]
Some immediate undesired side effects include a decrease in short-term memory, dry mouth, impaired motor skills, reddening of the eyes,[63] dizziness, feeling tired and vomiting.[19] Some users may experience an episode of acute psychosis, which usually abates after six hours, but in rare instances, heavy users may find the symptoms continuing for many days.[64]
Legalization has increased the rates at which children are exposed to cannabis, particularly from edibles. While the toxicity and lethality of THC in children is not known, they are at risk for encephalopathy, hypotension, respiratory depression severe enough to require ventilation, somnolence and coma.[65][66]
Fatality
[edit]A systematic meta analysis showed that cannabis users double the chance of dying from heart disease. Cannabis users had a 29% higher risk of heart attack and a 20% higher risk of stroke than non-users.[67][68][69] There is an association between cannabis use and suicide, particularly in younger users.[70]
A 16-month survey of Oregon and Alaska emergency departments found a report of the death of an adult who had been admitted for acute cannabis toxicity.[71]
A recent study in 2025 suggests that individuals diagnosed with cannabis use disorder—characterized by an inability to stop using cannabis despite its negative effects—face a nearly threefold increase in mortality rates compared to those without the condition over a five-year period.[72] The research indicates that people with this disorder are ten times more likely to die by suicide than the general population.[73] Additionally, they have a higher risk of death from trauma, drug poisoning, and lung cancer. In a separate study researchers found an increase in schizophrenia and psychosis cases in Canada linked to cannabis use disorder following the drug's legalization.[74]
Long-term
[edit]
Psychological effects
[edit]A 2015 meta-analysis found that, although a longer period of abstinence was associated with smaller magnitudes of impairment, both retrospective and prospective memory were impaired in cannabis users. The authors concluded that some, but not all, of the deficits associated with cannabis use were reversible.[76] A 2012 meta-analysis found that deficits in most domains of cognition persisted beyond the acute period of intoxication, but was not evident in studies where subjects were abstinent for more than 25 days.[77] Few high quality studies have been performed on the long-term effects of cannabis on cognition, and the results were generally inconsistent.[78] Furthermore, effect sizes of significant findings were generally small.[77] One review concluded that, although most cognitive faculties were unimpaired by cannabis use, residual deficits occurred in executive functions.[79] Impairments in executive functioning are most consistently found in older populations, which may reflect heavier cannabis exposure, or developmental effects associated with adolescent cannabis use.[80] One review found three prospective cohort studies that examined the relationship between self-reported cannabis use and intelligence quotient (IQ). The study following the largest number of heavy cannabis users reported that IQ declined between ages 7–13 and age 38. Poorer school performance and increased incidence of leaving school early were both associated with cannabis use, although a causal relationship was not established.[81] Cannabis users demonstrated increased activity in task-related brain regions, consistent with reduced processing efficiency.[82]
A reduced quality of life is associated with heavy cannabis use, although the relationship is inconsistent and weaker than for tobacco and other substances.[83] The direction of cause and effect, however, is unclear.[83]
The long-term effects of cannabis are not clear.[19] There are concerns surrounding memory and cognition problems, risk of addiction, and the risk of schizophrenia in young people.[18]
Neuroimaging
[edit]Although global abnormalities in white matter and grey matter are not consistently associated with cannabis use,[84] reduced hippocampal volume is consistently found.[85] Amygdala abnormalities are sometimes reported, although findings are inconsistent.[86][87][88]
Cannabis use is associated with increased recruitment of task-related areas, such as the dorsolateral prefrontal cortex, which is thought to reflect compensatory activity due to reduced processing efficiency.[88][87][89] Cannabis use is also associated with downregulation of CB1 receptors. The magnitude of down regulation is associated with cumulative cannabis exposure, and is reversed after one month of abstinence.[81][90][91] There is limited evidence that chronic cannabis use can reduce levels of glutamate metabolites in the human brain.[92]
Cannabis dependence
[edit]About 9% of those who experiment with marijuana eventually become dependent according to DSM-IV (1994) criteria.[21] A 2013 review estimates daily use is associated with a 10–20% rate of dependence.[18] The highest risk of cannabis dependence is found in those with a history of poor academic achievement, deviant behavior in childhood and adolescence, rebelliousness, poor parental relationships, or a parental history of drug and alcohol problems.[93] Of daily users, about 50% experience withdrawal upon cessation of use (i.e. are dependent), characterized by sleep problems, irritability, dysphoria, and craving.[81] Cannabis withdrawal is less severe than withdrawal from alcohol.[94]
According to DSM-5 criteria, 9% of those who are exposed to cannabis develop cannabis use disorder, compared to 20% for cocaine, 23% for alcohol and 68% for nicotine. Cannabis use disorder in the DSM-5 involves a combination of DSM-IV criteria for cannabis abuse and dependence, plus the addition of craving, without the criterion related to legal troubles.[81]
Psychiatric
[edit]From a clinical perspective, two significant school of thought exists for psychiatric conditions associated with cannabis (or cannabinoids) use: transient, non-persistent psychotic reactions, and longer-lasting, persistent disorders that resemble schizophrenia. The former is formally known as acute cannabis-associated psychotic symptoms (CAPS).[95]
At an epidemiological level, a dose–response relationship exists between cannabis use and increased risk of psychosis and earlier onset of psychosis.[96][5][97][98][99] Although the epidemiological association is robust, evidence to prove a causal relationship is lacking.[100]
Cannabis may also increase the risk of depression, but insufficient research has been performed to draw a conclusion.[101][97] Cannabis use is associated with increased risk of anxiety disorders, although causality has not been established.[102]
A review in 2019 found that research was insufficient to determine the safety and efficacy of using cannabis to treat schizophrenia, psychosis, or other mental disorders.[103][104] Another found that cannabis during adolescence was associated with an increased risk of developing depression and suicidal behavior later in life, while finding no effect on anxiety.[105]
Physical
[edit]Heavy, long-term exposure to marijuana may have physical, mental, behavioral and social health consequences. It may be "associated with diseases of the liver (particularly with co-existing hepatitis C), lungs, heart, and vasculature".[106] A 2014 review found that while cannabis use may be less harmful than alcohol use, the recommendation to substitute it for problematic drinking was premature without further study.[107] Various surveys conducted between 2015 and 2019 found that many users of cannabis substitute it for prescription drugs (including opioids), alcohol, and tobacco; most of those who used it in place of alcohol or tobacco either reduced or stopped their intake of the latter substances.[108]
Cannabinoid hyperemesis syndrome (CHS) is a severe condition seen in some chronic cannabis users where they have repeated bouts of uncontrollable vomiting for 24–48 hours. Four cases of death have been reported as a result of CHS.[109][110]
A limited number of studies have examined the effects of cannabis smoking on the respiratory system.[111] Chronic heavy marijuana smoking is associated with respiratory infections,[112] coughing, production of sputum, wheezing, and other symptoms of chronic bronchitis.[56] The available evidence does not support a causal relationship between cannabis use and chronic obstructive pulmonary disease.[113] Short-term use of cannabis is associated with bronchodilation.[114] Other side effects of cannabis use include cannabinoid hyperemesis syndrome (CHS), a condition which involves recurrent nausea, cramping abdominal pain, and vomiting.[115]
Cannabis smoke contains thousands of organic and inorganic chemical compounds. This tar is chemically similar to that found in tobacco smoke,[116] and over fifty known carcinogens have been identified in cannabis smoke,[117] including; nitrosamines, reactive aldehydes, and polycyclic aromatic hydrocarbons, including benz[a]pyrene.[118] Cannabis smoke is also inhaled more deeply than tobacco smoke.[119] As of 2015[update], there is no consensus regarding whether cannabis smoking is associated with an increased risk of cancer.[120] Light and moderate use of cannabis is not believed to increase risk of lung or upper airway cancer. Evidence for causing these cancers is mixed concerning heavy, long-term use. In general there are far lower risks of pulmonary complications for regular cannabis smokers when compared with those of tobacco.[121] A 2015 review found an association between cannabis use and the development of testicular germ cell tumors (TGCTs), particularly non-seminoma TGCTs.[122] Another 2015 meta-analysis found no association between lifetime cannabis use and risk of head or neck cancer.[123] Combustion products are not present when using a vaporizer, consuming THC in pill form, or consuming cannabis foods.[124]
There is concern that cannabis may contribute to cardiovascular disease,[125] but as of 2018[update], evidence of this relationship was unclear.[126] Research in these events is complicated because cannabis is often used in conjunction with tobacco, and drugs such as alcohol and cocaine that are known to have cardiovascular risk factors.[127] Smoking cannabis has also been shown to increase the risk of myocardial infarction by 4.8 times for the 60 minutes after consumption.[128]
There is preliminary evidence that cannabis interferes with the anticoagulant properties of prescription drugs used for treating blood clots.[129] As of 2019[update], the mechanisms for the anti-inflammatory and possible pain relieving effects of cannabis were not defined, and there were no governmental regulatory approvals or clinical practices for use of cannabis as a drug.[104]
Emergency department visits
[edit]Emergency room (ER) admissions associated with cannabis use rose significantly from 2012 to 2016; adolescents from age 12–17 had the highest risk.[130] At one Colorado medical center following legalization, approximately two percent of ER admissions were classified as cannabis users. The symptoms of one quarter of these users were partially attributed to cannabis (a total of 2567 out of 449,031 patients); other drugs were sometimes involved. Of these cannabis admissions, one quarter were for acute psychiatric effects, primarily suicidal ideation, depression, and anxiety. An additional third of the cases were for gastrointestinal issues including cannabinoid hyperemesis syndrome.[131]
According to the United States Department of Health and Human Services, there were 455,000 emergency room visits associated with cannabis use in 2011. These statistics include visits in which the patient was treated for a condition induced by or related to recent cannabis use. The drug use must be "implicated" in the emergency department visit, but does not need to be the direct cause of the visit. Most of the illicit drug emergency room visits involved multiple drugs.[132] In 129,000 cases, cannabis was the only implicated drug.[132][21]
Reproductive health
[edit]Secondhand cannabis smoke
[edit]A 2022 study found that smoking cannabis using a bong can greatly increase background levels of fine particulate matter, a carcinogen, in an enclosed space such as a living room. After 15 minutes, mean levels of particulate matter were more than twice the Environmental Protection Agency hazardous air quality threshold, and after 140 minutes, the concentrations were four times greater than those generated by smoking tobacco using a cigarette or hookah. This suggests secondhand cannabis smoke from bongs may present a health risk to non-smokers.[134]
Pharmacology
[edit]Mechanism of action
[edit]THC is a weak partial agonist at CB1 receptors, while CBD is a CB1 receptor antagonist.[135][136] The CB1 receptor is found primarily in the brain as well as in some peripheral tissues, and the CB2 receptor is found primarily in peripheral tissues, but is also expressed in neuroglial cells.[137] THC appears to alter mood and cognition through its agonist actions on the CB1 receptors, which inhibit a secondary messenger system (adenylate cyclase) in a dose-dependent manner.
Via CB1 receptor activation, THC indirectly increases dopamine release and produces psychotropic effects.[138] CBD also acts as an allosteric modulator of the μ- and δ-opioid receptors.[139] THC also potentiates the effects of the glycine receptors.[140] It is unknown if or how these actions contribute to the effects of cannabis.[141]
Pharmacokinetics
[edit]The high lipid-solubility of cannabinoids results in their persisting in the body for long periods of time.[142] Even after a single administration of THC, detectable levels of THC can be found in the body for weeks or longer (depending on the amount administered and the sensitivity of the assessment method).[142] Investigators have suggested that this is an important factor in marijuana's effects, perhaps because cannabinoids may accumulate in the body, particularly in the lipid membranes of neurons.[143]
Chemistry
[edit]Chemical composition
[edit]The main psychoactive component of cannabis is tetrahydrocannabinol (THC), which is formed via decarboxylation of tetrahydrocannabinolic acid (THCA) from the application of heat. Raw leaf is not psychoactive because the cannabinoids are in the form of carboxylic acids.[citation needed] THC is one of the 483 known compounds in the plant,[144] including at least 65 other cannabinoids,[145] such as cannabidiol (CBD).[58]
Detection in body fluids
[edit]THC and its major (inactive) metabolite, THC-COOH, can be measured in blood, urine, hair, oral fluid or sweat using chromatographic techniques as part of a drug use testing program or a forensic investigation of a traffic or other criminal offense.[64] The concentrations obtained from such analyses can often be helpful in distinguishing active use from passive exposure, elapsed time since use, and extent or duration of use. These tests cannot, however, distinguish authorized cannabis smoking for medical purposes from unauthorized recreational smoking.[146] Commercial cannabinoid immunoassays, often employed as the initial screening method when testing physiological specimens for marijuana presence, have different degrees of cross-reactivity with THC and its metabolites.[147] Urine contains predominantly THC-COOH, while hair, oral fluid and sweat contain primarily THC.[64] Blood may contain both substances, with the relative amounts dependent on the recency and extent of usage.[64]
The Duquenois–Levine test is commonly used as a screening test in the field, but it cannot definitively confirm the presence of cannabis, as a large range of substances have been shown to give false positives.[148] Researchers at John Jay College of Criminal Justice reported that dietary zinc supplements can mask the presence of THC and other drugs in urine.[149] However, a 2013 study conducted by researchers at the University of Utah School of Medicine refute the possibility of self-administered zinc producing false-negative urine drug tests.[150]
Varieties and strains
[edit]
CBD is a 5-HT1A receptor agonist, which is under laboratory research to determine if it has an anxiolytic effect.[151] It is often claimed that sativa strains provide a more stimulating psychoactive high while indica strains are more sedating with a body high.[152] However, this is disputed by researchers.[153]
A 2015 review found that the use of high CBD-to-THC strains of cannabis showed significantly fewer positive symptoms, such as delusions and hallucinations, better cognitive function and both lower risk for developing psychosis, as well as a later age of onset of the illness, compared to cannabis with low CBD-to-THC ratios.[154]
Psychoactive ingredients
[edit]According to the United Nations Office on Drugs and Crime (UNODC), "the amount of THC present in a cannabis sample is generally used as a measure of cannabis potency."[155] The three main forms of cannabis products are the flower/fruit, resin (hashish), and oil (hash oil). The UNODC states that cannabis often contains 5% THC content, resin "can contain up to 20% THC content", and that "Cannabis oil may contain more than 60% THC content."[155]
Studies have found that the potency of illicit cannabis has greatly increased since the 1970s, with THC levels rising and CBD levels dropping.[156][157][158] It is unclear, however, whether the increase in THC content has caused people to consume more THC or if users adjust based on the potency of the cannabis. It is likely that the higher THC content allows people to ingest less tar. At the same time, CBD levels in seized samples have lowered, in part because of the desire to produce higher THC levels and because more illegal growers cultivate indoors using artificial lights. This helps avoid detection but reduces the CBD production of the plant.[159]
Australia's National Cannabis Prevention and Information Centre (NCPIC) states that the buds (infructescences) of the female Cannabis plant contain the highest concentration of THC, followed by the leaves. The stalks and seeds have "much lower THC levels".[160] The UN states that the leaves can contain ten times less THC than the buds, and the stalks 100 times less THC.[155]
After revisions to cannabis scheduling in the UK, the government moved cannabis back from a class C to a class B drug. A purported reason was the appearance of high potency cannabis. They believe skunk accounts for between 70% and 80% of samples seized by police[161] (despite the fact that skunk can sometimes be incorrectly mistaken for all types of herbal cannabis).[162][163] Extracts such as hashish and hash oil typically contain more THC than high potency cannabis infructescences.[164]
Laced cannabis and synthetic cannabinoids
[edit]Hemp buds (or low-potency cannabis buds) laced with synthetic cannabinoids started to be sold as cannabis street drug in 2020.[165][166][167][168]
The short-term effects of cannabis can be altered if it has been laced with opioid drugs such as heroin or fentanyl.[169] The added drugs are meant to enhance the psychoactive properties, add to its weight, and increase profitability, despite the increased danger of overdose.[170][d]
Preparations
[edit]-
Dried flower buds (marijuana)
-
A gram of kief
-
Hashish
-
Hash oil
-
Infusion (dairy butter)
Marijuana
[edit]Marijuana or marihuana (herbal cannabis)[172] consists of the dried flowers and fruits and subtending leaves and stems of the female cannabis plant.[173][174][175][176] This is the most widely consumed form,[176] containing 3% to 20% THC,[177] with reports of up to 33% THC.[178] This is the stock material from which all other preparations are derived. Although herbal cannabis and industrial hemp derive from the same species and contain the psychoactive component (THC), they are distinct strains with unique biochemical compositions and uses. Hemp has lower concentrations of THC and higher concentrations of CBD, which gives lesser psychoactive effects.[179][180]
Kief
[edit]Kief is a powder, rich in trichomes,[181] which can be sifted from the leaves, flowers and fruits of cannabis plants and either consumed in powder form or compressed to produce cakes of hashish.[182] The word "kif" derives from colloquial Arabic كيف kēf/kīf, meaning pleasure.[183]
Hashish
[edit]
Hashish (also spelled hasheesh, hashisha, or simply hash) is a concentrated resin cake or ball produced from pressed kief, the detached trichomes and fine material that falls off cannabis fruits, flowers and leaves,[184] or from scraping the resin from the surface of the plants and rolling it into balls. It varies in color from black to golden brown depending upon purity and variety of cultivar it was obtained from.[185] It can be consumed orally or smoked, and is also vaporized, or 'vaped'.[186] The term "rosin hash" refers to a high quality solventless product obtained through heat and pressure.[187]
Tincture
[edit]Cannabinoids can be extracted from cannabis plant matter using high-proof spirits (often grain alcohol) to create a tincture, often referred to as "green dragon".[37]: p17 Nabiximols is a branded product name from a tincture manufacturing pharmaceutical company.[188]
Hash oil
[edit]Hash oil is a resinous matrix of cannabinoids obtained from the cannabis plant by solvent extraction,[189] formed into a hardened or viscous mass.[190] Hash oil can be the most potent of the main cannabis products because of its high level of psychoactive compound per its volume, which can vary depending on the plant's mix of essential oils and psychoactive compounds.[191] Butane and supercritical carbon dioxide hash oil have become popular in recent years.[192]
Infusions
[edit]There are many varieties of cannabis infusions owing to the variety of non-volatile solvents used.[193] The plant material is mixed with the solvent and then pressed and filtered to express the oils of the plant into the solvent. Examples of solvents used in this process are cocoa butter, dairy butter, cooking oil, glycerine, and skin moisturizers. Depending on the solvent, these may be used in cannabis foods or applied topically.[194]
Marihuana prensada
[edit]Marihuana prensada ('pressed marijuana') is a cannabis-derived product widespread among the lower classes of South America,[195] especially from the 90s. Locally it is known as "paraguayo" or "paragua", since its main producer is Paraguay.[196] Marijuana is dried and mixed with binding agents that make it toxic and highly harmful to health.[197] It is cut into the shape of bricks (ladrillos) and sold for a low price in Argentina, Brazil, Chile, Peru, Venezuela, and even the United States.[198]
History
[edit]Ancient history
[edit]
Cannabis is indigenous to Central or South Asia[199] and its uses for fabric and rope dates back to the Neolithic age in China and Japan.[200][201] It is unclear when cannabis first became known for its psychoactive properties. The oldest archeological evidence for the burning of cannabis was found in Romanian kurgans dated 3,500 BC, and scholars suggest that the drug was first used in ritual ceremonies by Proto-Indo-European tribes living in the Pontic-Caspian steppe during the Chalcolithic period, a custom they eventually spread throughout Western Eurasia during the Indo-European migrations.[202][203] Some research suggests that the ancient Indo-Iranian drug soma, mentioned in the Vedas, sometimes contained cannabis. This is based on the discovery of a basin containing cannabis in a shrine of the second millennium BC in Turkmenistan.[204]
Cannabis was known to the ancient Assyrians, who discovered its psychoactive properties through the Iranians.[205] Using it in some religious ceremonies, they called it qunubu (meaning "way to produce smoke"), a probable origin of the modern word cannabis.[206] The Iranians also introduced cannabis to the Scythians, Thracians and Dacians, whose shamans (the kapnobatai – "those who walk on smoke/clouds") burned cannabis infructescences to induce trance.[207] The plant was used in China before 2800 BC, and found therapeutic use in India by 1000 BC, where it was used in food and drink, including bhang.[208][209]

Cannabis has an ancient history of ritual use and has been used by religions around the world. It has been used as a drug for both recreational and entheogenic purposes and in various traditional medicines for centuries.[210][211][172] The earliest evidence of cannabis smoking has been found in the 2,500-year-old tombs of Jirzankal Cemetery in the Pamir Mountains in Western China, where cannabis residue were found in burners with charred pebbles possibly used during funeral rituals.[212][213] Hemp seeds discovered by archaeologists at Pazyryk suggest early ceremonial practices like eating by the Scythians occurred during the 5th to 2nd century BC, confirming previous historical reports by Herodotus.[214] It was used by Muslims in various Sufi orders as early as the Mamluk period, for example by the Qalandars.[215] Smoking pipes uncovered in Ethiopia and carbon-dated to around c. AD 1320 were found to have traces of cannabis.[216]
Modern history
[edit]Cannabis was introduced to the New World by the Spaniards in 1530–1545.[217][218][219] Following an 1836–1840 travel in North Africa and the Middle East, French physician Jacques-Joseph Moreau wrote on the psychological effects of cannabis use; he founded the Paris' Club des Hashischins in 1844.[220] In 1842, Irish physician William Brooke O'Shaughnessy, who had studied the drug while working as a medical officer in Bengal with the East India Company, brought a quantity of cannabis with him on his return to Britain, provoking renewed interest in the West.[221] Examples of classic literature of the period featuring cannabis include Les paradis artificiels (1860) by Charles Baudelaire and The Hasheesh Eater (1857) by Fitz Hugh Ludlow.

Cannabis was criminalized in some countries beginning in the 14th century and was illegal in most countries by the middle of the 20th century. The colonial government of Mauritius banned cannabis in 1840 over concerns on its effect on Indian indentured workers;[222] the same occurred in Singapore in 1870.[223] In the United States, the first restrictions on sale of cannabis came in 1906 (in the District of Columbia).[224] Canada criminalized cannabis in The Opium and Narcotic Drug Act, 1923,[225] before any reports of the use of the drug in Canada, but eventually legalized its consumption for recreational and medicinal purposes in 2018.[22]
In 1925, a compromise was made at an international conference in Geneva about the Second International Opium Convention that banned exportation of "Indian hemp" to countries that had prohibited its use, and requiring importing countries to issue certificates approving the importation and stating that the shipment was required "exclusively for medical or scientific purposes". It also required parties to "exercise an effective control of such a nature as to prevent the illicit international traffic in Indian hemp and especially in the resin".[226][227] In the United States in 1937, the Marihuana Tax Act was passed,[228] and prohibited the production of hemp in addition to cannabis.

In 1972, the Dutch government divided drugs into more- and less-dangerous categories, with cannabis being in the lesser category. Accordingly, possession of 30 grams (1.1 oz) or less was made a misdemeanor.[229] Cannabis has been available for recreational use in coffee shops since 1976.[230] Cannabis products are only sold openly in certain local "coffeeshops" and possession of up to 5 grams (0.18 oz) for personal use is decriminalized, however: the police may still confiscate it, which often happens in car checks near the border. Other types of sales and transportation are not permitted, although the general approach toward cannabis was lenient even before official decriminalization.[231][232][233]
In Uruguay, President Jose Mujica signed legislation to legalize recreational cannabis in December 2013, making Uruguay the first country in the modern era to legalize cannabis. In August 2014, Uruguay legalized growing up to six plants at home, as well as the formation of growing clubs (Cannabis social club), and a state-controlled marijuana dispensary regime.
As of 17 October 2018[update], when recreational use of cannabis was legalized in Canada, dietary supplements for human use and veterinary health products containing not more than 10 parts per million of THC extract were approved for marketing; Nabiximols (as Sativex) is used as a prescription drug in Canada.[22]
The United Nations' World Drug Report stated that cannabis "was the world's most widely produced, trafficked, and consumed drug in the world in 2010", and estimated between 128 million and 238 million users globally in 2015.[234][235]
Culture, legality and economics
[edit]Culture
[edit]
Cannabis has been one of the most used psychoactive drugs in the world since the late 20th century, following only tobacco and alcohol in popularity.[237] According to Vera Rubin, the use of cannabis has been encompassed by two major cultural complexes over time: a continuous, traditional folk stream, and a more circumscribed, contemporary configuration.[238] The former involves both sacred and secular use, and is usually based on small-scale cultivation: the use of the plant for cordage, clothing, medicine, food, and a "general use as an euphoriant and symbol of fellowship."[238][239] The second stream of expansion of cannabis use encompasses "the use of hemp for commercial manufacturers utilizing large-scale cultivation primarily as a fiber for mercantile purposes"; but it is also linked to the search for psychedelic experiences (which can be traced back to the formation of the Parisian Club des Hashischins).[239]
Legality
[edit]
See also countries that have legalized medical use of cannabis.
Since the beginning of the 20th century, most countries have enacted laws against the cultivation, possession or transfer of cannabis.[240] These laws have had an adverse effect on cannabis cultivation for non-recreational purposes, but there are many regions where handling of cannabis is legal or licensed. Many jurisdictions have lessened the penalties for possession of small quantities of cannabis so that it is punished by confiscation and sometimes a fine, rather than imprisonment, focusing more on those who traffic the drug on the black market.
In some areas where cannabis use had been historically tolerated, new restrictions were instituted, such as the closing of cannabis coffee shops near the borders of the Netherlands,[241] and closing of coffee shops near secondary schools in the Netherlands.[242] In Copenhagen, Denmark in 2014, mayor Frank Jensen discussed possibilities for the city to legalize cannabis production and commerce.[243]
Some jurisdictions use free voluntary or mandatory treatment programs for frequent known users. Simple possession can carry long prison terms in some countries, particularly in East Asia, where the sale of cannabis may lead to a sentence of life in prison or even execution. Political parties, non-profit organizations, and causes based on the legalization of medical cannabis or legalizing the plant entirely (with some restrictions) have emerged in such countries as China and Thailand.[244][245]
In December 2012, the U.S. state of Washington became the first state to officially legalize cannabis in a state law (Washington Initiative 502) (but still illegal by federal law),[246] with the state of Colorado following close behind (Colorado Amendment 64).[247] On 1 January 2013, the first cannabis "club" for private marijuana smoking (no buying or selling, however) was allowed for the first time in Colorado.[248] The California Supreme Court decided in May 2013 that local governments can ban medical cannabis dispensaries despite a state law in California that permits the use of cannabis for medical purposes. At least 180 cities across California have enacted bans in recent years.[249]
On 30 April 2024, the United States Department of Justice announced it would move to reclassify cannabis from a Schedule I to a Schedule III controlled substance.[250][251]
In December 2013, Uruguay became the first country to legalize growing, sale and use of cannabis.[252] After a long delay in implementing the retail component of the law, in 2017 sixteen pharmacies were authorized to sell cannabis commercially.[253] On 19 June 2018, the Canadian Senate passed a bill and the Prime Minister announced the effective legalization date as 17 October 2018.[22][254] Canada is the second country to legalize the drug.[255]
In November 2015, Uttarakhand became the first state of India to legalize the cultivation of hemp for industrial purposes.[256] Usage within the Hindu and Buddhist cultures of the Indian subcontinent is common, with many street vendors in India openly selling products infused with cannabis, and traditional medical practitioners in Sri Lanka selling products infused with cannabis for recreational purposes and well as for religious celebrations.[257] Indian laws criminalizing cannabis date back to the colonial period. India and Sri Lanka have allowed cannabis to be taken in the context of traditional culture for recreational/celebratory purposes and also for medicinal purposes.[257]
On 17 October 2015, Australian health minister Sussan Ley presented a new law that will allow the cultivation of cannabis for scientific research and medical trials on patients.[258]
On 17 October 2018, Canada legalized cannabis for recreational adult use[259] making it the second country in the world to do so after Uruguay and the first G7 nation.[260] This legalization comes with regulation similar to that of alcohol in Canada, age restrictions, limiting home production, distribution, consumption areas and sale times.[261] Laws around use vary from province to province including age limits, retail structure, and growing at home.[259] The Canadian Licensed Producer system aims to become the Gold Standard in the world for safe and secure cannabis production,[262] including provisions for a robust craft cannabis industry where many expect opportunities for experimenting with different strains.[263]
As the drug has increasingly been seen as a health issue instead of criminal behavior, cannabis has also been legalized or decriminalized in: Czech Republic,[264] Colombia,[265][266] Ecuador,[267][268][269] Portugal,[270] South Africa[271] and Canada.[22] Medical marijuana was legalized in Mexico in mid-2017 and legalized for recreational use in June 2021.[272][273][274]
Germany legalized cannabis for recreational use in April 2024.[275]
Legal status by country
[edit]As of 2022, Uruguay and Canada are the only countries that have fully legalized the cultivation, consumption and bartering of recreational cannabis nationwide.[276][277] In the United States, 24 states, 3 territories, and the District of Columbia have legalized the recreational use of cannabis – though the drug remains illegal at the federal level.[278] Laws vary from state to state when it comes to the commercial sale. Court rulings in Georgia and South Africa have led to the legalization of cannabis consumption, but not legal sales. A policy of limited enforcement has also been adopted in many countries, in particular Spain and the Netherlands where the sale of cannabis is tolerated at licensed establishments.[279][280] Contrary to popular belief, cannabis is not legal in the Netherlands,[281] but it has been decriminalized since the 1970s. In 2021, Malta was the first European Union member to legalize the use of cannabis for recreational purposes.[282] In Estonia, it is only legal to sell cannabis products with a THC content of less than 0.2%, although products may contain more cannabidiol.[283] Lebanon has recently become the first Arab country to legalize the plantation of cannabis for medical use.[284]
Penalties for illegal recreational use ranges from confiscation or small fines to jail time and even death.[285] In some countries, citizens can be punished if they have used the drug in another country, including Singapore and South Korea.[286][287]
Economics
[edit]Production
[edit]
Sinsemilla (Spanish for "without seed") is the dried, seedless (i.e. parthenocarpic) infructescences of female cannabis plants. Because THC production drops off once pollination occurs, the male plants (which produce little THC themselves) are eliminated before they shed pollen to prevent pollination, thus inducing the development of parthenocarpic fruits gathered in dense infructescences. Advanced cultivation techniques such as hydroponics, cloning, high-intensity artificial lighting, and the sea of green method are frequently employed as a response (in part) to prohibition enforcement efforts that make outdoor cultivation more risky.
"Skunk" refers to several named strains of potent cannabis, grown through selective breeding and sometimes hydroponics. It is a cross-breed of Cannabis sativa and C. indica (although other strains of this mix exist in abundance). Skunk cannabis potency ranges usually from 6% to 15% and rarely as high as 20%. The average THC level in coffee shops in the Netherlands is about 18–19%.[288]
The average levels of THC in cannabis sold in the United States rose dramatically between the 1970s and 2000.[289] This is disputed for various reasons, and there is little consensus as to whether this is a fact or an artifact of poor testing methodologies.[289] According to Daniel Forbes writing for slate.com, the relative strength of modern strains are likely skewed because undue weight is given to much more expensive and potent, but less prevalent, samples.[290] Some suggest that results are skewed by older testing methods that included low-THC-content plant material such as leaves in the samples, which are excluded in contemporary tests. Others believe that modern strains actually are significantly more potent than older ones.[289]
The main producing countries of cannabis are Afghanistan,[291] Canada,[292] China, Colombia,[293] India,[291] Jamaica,[291] Lebanon,[294] Mexico,[295] Morocco,[291] the Netherlands, Pakistan, Paraguay,[295] Spain,[291] Thailand, Turkey, the United Kingdom,[296] and the United States.[291]
Price
[edit]The price or street value of cannabis varies widely depending on geographic area and potency.[297] Prices and overall markets have also varied considerably over time.
- In 1997, cannabis was estimated to be overall the number four value crop in the US, and number one or two in many states, including California, New York, and Florida. This estimate is based on a value to growers of ~60% of retail value, or $3,000 per pound ($6,600/kg).[298]
- In 2006, cannabis was estimated to have been a $36 billion market.[299] This estimate has been challenged as exaggerated.[47] The UN World Drug Report (2008) estimated that 2006 street prices in the US and Canada ranged from about US$8.8 to $25 per gram (approximately $250 to $700 per ounce), depending on quality.[300] Typical U.S. retail prices were $10–15 per gram (approximately $280–420 per ounce).
- In 2017, the U.S. was estimated to constitute 90% of the worldwide $9.5 billion legal trade in cannabis.[301]
After some U.S. states legalized cannabis, street prices began to drop. In Colorado, the price of smokable buds (infructescences) dropped 40 percent between 2014 and 2019, from $200 per ounce to $120 per ounce ($7 per gram to $4.19 per gram).[302]
The European Monitoring Centre for Drugs and Drug Addiction reports that typical retail prices in Europe for cannabis varied from €2 to €20 per gram in 2008, with a majority of European countries reporting prices in the range €4–10.[303]
Cannabis as a gateway drug
[edit]The gateway hypothesis states that cannabis use increases the probability of trying "harder" drugs. The hypothesis has been hotly debated as it is regarded by some as the primary rationale for the United States prohibition on cannabis use.[304][305] A Pew Research Center poll found that political opposition to marijuana use was significantly associated with concerns about the health effects and whether legalization would increase cannabis use by children.[306]
Some studies state that while there is no proof for the gateway hypothesis,[307] young cannabis users should still be considered as a risk group for intervention programs.[308] Other findings indicate that hard drug users are likely to be poly-drug users, and that interventions must address the use of multiple drugs instead of a single hard drug.[309] Almost two-thirds of the poly drug users in the 2009–2010 Scottish Crime and Justice Survey used cannabis.[310]
The gateway effect may appear due to social factors involved in using any illegal drug. Because of the illegal status of cannabis, its consumers are likely to find themselves in situations allowing them to acquaint with individuals using or selling other illegal drugs.[311][312] Studies have shown that alcohol and tobacco may additionally be regarded as gateway drugs;[313] however, a more parsimonious explanation could be that cannabis is simply more readily available (and at an earlier age) than illegal hard drugs.[citation needed] In turn, alcohol and tobacco are typically easier to obtain at an earlier age than is cannabis (though the reverse may be true in some areas), thus leading to the "gateway sequence" in those individuals, since they are most likely to experiment with any drug offered.[304]
A related alternative to the gateway hypothesis is the common liability to addiction (CLA) theory. It states that some individuals are, for various reasons, willing to try multiple recreational substances. The "gateway" drugs are merely those that are (usually) available at an earlier age than the harder drugs. Researchers have noted in an extensive review that it is dangerous to present the sequence of events described in gateway "theory" in causative terms as this hinders both research and intervention.[314]
In 2020, the National Institute on Drug Abuse released a study backing allegations that marijuana is a gateway to harder drugs, though not for the majority of marijuana users.[315] The National Institute on Drug Abuse determined that marijuana use is "likely to precede use of other licit and illicit substances" and that "adults who reported marijuana use during the first wave of the survey were more likely than adults who did not use marijuana to develop an alcohol use disorder within 3 years; people who used marijuana and already had an alcohol use disorder at the outset were at greater risk of their alcohol use disorder worsening. Marijuana use is also linked to other substance use disorders including nicotine addiction."[315] It also reported that "These findings are consistent with the idea of marijuana as a "gateway drug". However, the majority of people who use marijuana do not go on to use other, "harder" substances. Also, cross-sensitization is not unique to marijuana. Alcohol and nicotine also prime the brain for a heightened response to other drugs and are, like marijuana, also typically used before a person progresses to other, more harmful substances."[315]
Research
[edit]Research on cannabis is challenging since the plant is illegal in most countries.[316][317][318][319][320] Research-grade samples of the drug are difficult to obtain for research purposes, unless granted under authority of national regulatory agencies, such as the US Food and Drug Administration.[321]
There are also other difficulties in researching the effects of cannabis. Many people who smoke cannabis also smoke tobacco.[322] This causes confounding factors, where questions arise as to whether the tobacco, the cannabis, or both that have caused a cancer. Another difficulty researchers have is in recruiting people who smoke cannabis into studies. Because cannabis is an illegal drug in many countries, people may be reluctant to take part in research, and if they do agree to take part, they may not say how much cannabis they actually smoke.[323]
See also
[edit]References
[edit]Footnotes
- ^ Pure varieties of C. ruderalis are rarely used for recreational purposes due to their negligible amounts of THC.[1]
- ^ Psychotic episodes are well-documented and typically resolve within minutes or hours, while symptoms may last longer.[54] The use of a single joint can temporarily induce some psychiatric symptoms.[55]
- ^ A 2016 review also found a statistically significant increase in crash risk associated with marijuana use, but noted that this risk was "of low to medium magnitude."[61] The increase in risk of motor vehicle crash for cannabis use is between 2 and 3 times relative to baseline, whereas that for comparable doses of alcohol is between 6 and 15 times.[62]
- ^ Advocates of legalizing marijuana for recreational use, such as former Illinois state Senator Heather Steans, say that legalizing it would help reduce such hazardous added drugs: "Over 95 percent are buying it on the black market. You don't know what you're buying. It's not a safe product. We've seen it laced with rat poison, fentanyl, all sorts of things. It's funding the cartels and other criminal activity."[171]
Citations
- ^ Cervantes, Jorge (2006). Marijuana Horticulture: The Indoor/Outdoor Medical Grower's Bible (5th ed.). Van Patten Publishing. pp. 12. ISBN 978-1-878823-23-6.
- ^ "cannabis noun – Definition, pictures, pronunciation and usage notes | Oxford Advanced Learner's Dictionary at OxfordLearnersDictionaries.com". www.oxfordlearnersdictionaries.com. Retrieved 10 November 2022.
- ^ "marijuana noun – Definition, pictures, pronunciation and usage notes | Oxford Advanced Learner's Dictionary at OxfordLearnersDictionaries.com". www.oxfordlearnersdictionaries.com. Retrieved 18 April 2019.
- ^ Myran, Daniel T.; Pugliese, Michael; Harrison, Lyndsay D.; Solmi, Marco; Anderson, Kelly K.; Fiedorowicz, Jess G.; Finkelstein, Yaron; Manuel, Doug; Taljaard, Monica; Webber, Colleen; Tanuseputro, Peter (3 February 2025). "Changes in Incident Schizophrenia Diagnoses Associated With Cannabis Use Disorder After Cannabis Legalization". JAMA Network Open. 8 (2): e2457868. doi:10.1001/jamanetworkopen.2024.57868. ISSN 2574-3805. PMC 11795325. PMID 39903464.
- ^ a b Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E (September 2016). "Meta-analysis of the Association Between the Level of Cannabis Use and Risk of Psychosis". Schizophrenia Bulletin. 42 (5): 1262–69. doi:10.1093/schbul/sbw003. PMC 4988731. PMID 26884547.
- ^ Shrivastava, Amresh; Johnston, Megan; Tsuang, Ming (2011). "Cannabis use and cognitive dysfunction". Indian Journal of Psychiatry. 53 (3): 187–191. doi:10.4103/0019-5545.86796. ISSN 0019-5545. PMC 3221171. PMID 22135433.
- ^ Gregory, Andrew; editor, Andrew Gregory Health (17 June 2025). "Cannabis use could double risk of heart deaths, study suggests". The Guardian.
{{cite web}}:|last2=has generic name (help) - ^ Pratt M, Stevens A, Thuku M, Butler C, Skidmore B, Wieland LS, Clemons M, Kanji S, Hutton B (December 2019). "Benefits and harms of medical cannabis: a scoping review of systematic reviews". Syst Rev (Systematic review). 8 (1) 320. doi:10.1186/s13643-019-1243-x. PMC 6905063. PMID 31823819.
- ^ Gray, Stephen (9 December 2016). Cannabis and Spirituality: An Explorer's Guide to an Ancient Plant Spirit Ally. Simon and Schuster. p. 69. ISBN 978-1-62055-584-2.
Cannabis is called kaneh bosem in Hebrew, which is now recognized as the Scythian word that Herodotus wrote as kánnabis (or cannabis).
- ^ a b c d Riegel, A.; Ellens, J.H. (2014). Seeking the Sacred with Psychoactive Substances: Chemical Paths to Spirituality and to God [2 volumes]. Psychology, Religion, and Spirituality. Bloomsbury Publishing. p. 80. ISBN 979-8-216-14310-9. Retrieved 3 June 2024.
- ^ Duncan, Perry M. (17 September 2020). Substance Use Disorders: A Biopsychosocial Perspective. Cambridge University Press. p. 441. ISBN 978-0-521-87777-0.
Cannabis is a Scythian word (Benet 1975).
- ^ Orel, Vladimir (2003). A Handbook of Germanic Etymology. Leiden: Brill. p. 159.
- ^ Murnion B (December 2015). "Medicinal cannabis". Australian Prescriber. 38 (6): 212–15. doi:10.18773/austprescr.2015.072. ISSN 0312-8008. PMC 4674028. PMID 26843715.
- ^ "What is medical marijuana?". National Institute of Drug Abuse. July 2015. Retrieved 19 April 2016.
The term medical marijuana refers to using the whole unprocessed marijuana plant or its basic extracts to treat a disease or symptom.
- ^ Backes M (2014). Cannabis Pharmacy: The Practical Guide to Medical Marijuana. Hachette Books. p. 46. ISBN 978-1-60376-334-9.
- ^ "Release the strains". Nature Medicine. 21 (9): 963. September 2015. doi:10.1038/nm.3946. PMID 26340110.
- ^ Pratt M, Stevens A, Thuku M, Butler C, Skidmore B, Wieland LS, Clemons M, Kanji S, Hutton B (December 2019). "Benefits and harms of medical cannabis: a scoping review of systematic reviews". Syst Rev (Systematic review). 8 (1) 320. doi:10.1186/s13643-019-1243-x. PMC 6905063. PMID 31823819.
- ^ a b c Borgelt LM, Franson KL, Nussbaum AM, Wang GS (February 2013). "The pharmacologic and clinical effects of medical cannabis". Pharmacotherapy. 33 (2): 195–209. CiteSeerX 10.1.1.1017.1935. doi:10.1002/phar.1187. PMID 23386598. S2CID 8503107.
- ^ a b c Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, Keurentjes JC, Lang S, Misso K, Ryder S, Schmidlkofer S, Westwood M, Kleijnen J (23 June 2015). "Cannabinoids for Medical Use: A Systematic Review and Meta-analysis". JAMA. 313 (24): 2456–73. doi:10.1001/jama.2015.6358. hdl:10757/558499. PMID 26103030.
- ^ Jensen B, Chen J, Furnish T, Wallace M (October 2015). "Medical Marijuana and Chronic Pain: a Review of Basic Science and Clinical Evidence". Current Pain and Headache Reports. 19 (10) 50. doi:10.1007/s11916-015-0524-x. PMID 26325482. S2CID 9110606.
- ^ a b c d Volkow ND, Baler RD, Compton WM, Weiss SR (June 2014). "Adverse health effects of marijuana use". The New England Journal of Medicine. 370 (23): 2219–27. doi:10.1056/NEJMra1402309. PMC 4827335. PMID 24897085.
- ^ a b c d e f "Health products containing cannabis or for use with cannabis: Guidance for the Cannabis Act, the Food and Drugs Act, and related regulations". Government of Canada. 11 July 2018. Retrieved 19 October 2018.
- ^ Ainge Roy, Eleanor (11 December 2018). "New Zealand passes laws to make medical marijuana widely available". The Guardian. Retrieved 20 January 2019.
- ^ Schulz, Chris (30 June 2022). "You can get actual weed from the doctor now". The Spinoff.
- ^ Ernest Small (2016). Cannabis: A Complete Guide. CRC Press. ISBN 978-1-315-35059-2.
- ^ Onaivi ES, Sugiura T, Di Marzo V (2005). Endocannabinoids: The Brain and Body's Marijuana and Beyond. Taylor & Francis. p. 58. ISBN 978-0-415-30008-7.
- ^ Curran, H. Valerie; Morgan, Celia J.A. (2014). "Desired and Undesired Effects of Cannabis on the Human Mind and Psychological Well-Being". In Pertwee, Roger G. (ed.). Handbook of Cannabis. Oxford University Press.
- ^ Ashton, C.Heather (2001). "Pharmacology and Effects of Cannabis: A Brief Review". British Journal of Psychiatry. 178 (2): 101–06. doi:10.1192/bjp.178.2.101. PMID 11157422. S2CID 15918781.
- ^ Mathre ML, ed. (1997). Cannabis in Medical Practice: A Legal, Historical, and Pharmacological Overview of the Therapeutic Use of Marijuana. University of Virginia Medical Center. pp. 144–. ISBN 978-0-7864-8390-7.
- ^ Riedel G, Davies SN (2005). "Cannabinoid function in learning, memory and plasticity". Cannabinoids. Handbook of Experimental Pharmacology. Vol. 168. pp. 445–77. doi:10.1007/3-540-26573-2_15. ISBN 978-3-540-22565-2. PMID 16596784.
- ^ Osborne GB, Fogel C (2008). "Understanding the motivations for recreational marijuana use among adult Canadians" (PDF). Substance Use & Misuse. 43 (3–4): 539–72, discussion 573–79, 585–87. doi:10.1080/10826080701884911. PMID 18365950. S2CID 31053594.
- ^ "Medication-Associated Depersonalization Symptoms". Medscape.
- ^ Shufman E, Lerner A, Witztum E (April 2005). "[Depersonalization after withdrawal from cannabis usage]" (PDF). Harefuah (in Hebrew). 144 (4): 249–51, 303. PMID 15889607. Archived from the original (PDF) on 30 April 2005.
- ^ Johnson BA (February 1990). "Psychopharmacological effects of cannabis". British Journal of Hospital Medicine. 43 (2): 114–16, 118–20, 122. PMID 2178712.
- ^ Souza RS, Albuquerque UP, Monteiro JM, de Amorim EL (2008). "Brazilian Archives of Biology and Technology – Jurema-Preta (Mimosa tenuiflora [Willd.] Poir.): a review of its traditional use, phytochemistry and pharmacology". Brazilian Archives of Biology and Technology. 51 (5): 937–47. doi:10.1590/S1516-89132008000500010.
- ^ a b Courtwright D (2001). Forces of Habit: Drugs and the Making of the Modern World. Harvard University Press. ISBN 978-0-674-00458-0.
- ^ a b Iversen LL (2000). The Science of Marijuana. Oxford University Press. ISBN 978-0-19-515110-7.
- ^ Golub A (2012). The Cultural/Subcultural Contexts of Marijuana Use at the Turn of the Twenty-First Century. Routledge. p. 82. ISBN 978-1-136-44627-6.
- ^ "Why Does Cannabis Have to be Heated?". patriotcare.org. Archived from the original on 14 February 2022. Retrieved 30 May 2020.
- ^ Tasman A, Kay J, Lieberman JA, First MB, Maj M (2011). Psychiatry. John Wiley & Sons. p. 9. ISBN 978-1-119-96540-4.
- ^ Rosenthal E (2002). Ask Ed: Marijuana Gold: Trash to Stash. Perseus Books Group. p. 15. ISBN 978-1-936807-02-4.
- ^ "Cannabis and Cannabis Extracts: Greater Than the Sum of Their Parts?" (PDF). Cannabis-med.org. Archived from the original (PDF) on 22 June 2017. Retrieved 7 April 2014.
- ^ Dronabinol from PubChem
- ^ Gieringer D, Rosenthal E (2008). Marijuana medical handbook: practical guide to therapeutic uses of marijuana. QUICK AMER Publishing Company. p. 182. ISBN 978-0-932551-86-3.
- ^ "Annual prevalence of use of drugs, by region and globally, 2016". World Drug Report 2018. United Nations Office on Drugs and Crime. 2018. Retrieved 7 July 2018.
- ^ "Status and Trend Analysis of Illict [sic] Drug Markets" (PDF). World Drug Report 2015. p. 23. Retrieved 26 June 2015.
- ^ a b c Caulkins JP, Hawken A, Kilmer B, Kleiman MA (2012). Marijuana Legalization: What Everyone Needs to Know. Oxford University Press. p. 16. ISBN 978-0-19-991373-2.
- ^ "UNODC Statistics Online". data.unodc.org. Retrieved 9 September 2018.
- ^ a b Joshua CD (2015). "The business of getting high: head shops, countercultural capitalism, and the marijuana legalization movement". The Sixties. 8: 27–49. doi:10.1080/17541328.2015.1058480. hdl:11603/7422. S2CID 142795620.
- ^ "6 facts about marijuana". 22 November 2018. Retrieved 24 September 2020.
- ^ "Daily marijuana use among college students highest since 1980". The University Record.
- ^ a b McCarthy, Justin (22 July 2015). "More Than Four in 10 Americans Say They Have Tried Marijuana". Gallup.
- ^ "For the first time, Americans are smoking more marijuana than cigarettes, poll finds". cbsnews.com.
- ^ "Sativex Oral Mucosal Spray Public Assessment Report. Decentralized Procedure" (PDF). United Kingdom Medicines and Healthcare Products Regulatory Agency. p. 93. Retrieved 7 May 2015.
There is clear evidence that recreational cannabis can produce a transient toxic psychosis in larger doses or in susceptible individuals, which is said to characteristically resolve within a week or so of absence (Johns 2001). Transient psychotic episodes as a component of acute intoxication are well-documented (Hall et al 1994)
- ^ Hunt, Katie (17 March 2020). "Single cannabis joint linked with temporary psychiatric symptoms, review finds". CNN. Retrieved 21 March 2020.
- ^ a b Hall W, Solowij N (November 1998). "Adverse effects of cannabis". Lancet. 352 (9140): 1611–16. doi:10.1016/S0140-6736(98)05021-1. PMID 9843121. S2CID 16313727.
- ^ Oltmanns T, Emery R (2015). Abnormal Psychology. New Jersey: Pearson. p. 294. ISBN 978-0-205-97074-2.
- ^ a b D'Souza DC, Sewell RA, Ranganathan M (October 2009). "Cannabis and psychosis/schizophrenia: human studies". European Archives of Psychiatry and Clinical Neuroscience. 259 (7): 413–31. doi:10.1007/s00406-009-0024-2. PMC 2864503. PMID 19609589.
- ^ Abuse, National Institute on Drug. "Does marijuana use affect driving?". www.drugabuse.gov. Retrieved 18 December 2019.
- ^ Li MC, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, Li G (4 October 2011). "Marijuana use and motor vehicle crashes". Epidemiologic Reviews. 34 (1): 65–72. doi:10.1093/epirev/mxr017. PMC 3276316. PMID 21976636.
- ^ Rogeberg O, Elvik R (August 2016). "The effects of cannabis intoxication on motor vehicle collision revisited and revised". Addiction. 111 (8): 1348–59. doi:10.1111/add.13347. PMID 26878835.
- ^ Hall W (January 2015). "What has research over the past two decades revealed about the adverse health effects of recreational cannabis use?" (PDF). Addiction. 110 (1): 19–35. doi:10.1111/add.12703. PMID 25287883.
- ^ Hall W, Pacula RL (2003). Cannabis Use and Dependence: Public Health and Public Policy. Cambridge University Press. p. 38. ISBN 978-0-521-80024-2.
- ^ a b c d Barceloux DG (2012). "Chapter 60: Marijuana (Cannabis sativa L.) and synthetic cannabinoids". Medical Toxicology of Drug Abuse: Synthesized Chemicals and Psychoactive Plants. John Wiley & Sons. pp. 910–. ISBN 978-1-118-10605-1. Retrieved 14 July 2013.
- ^ Wong, Kei U.; Baum, Carl R. (November 2019). "Acute Cannabis Toxicity". Pediatric Emergency Care. 35 (11): 799–804. doi:10.1097/PEC.0000000000001970. ISSN 0749-5161. PMID 31688799. S2CID 207897219.
- ^ Claudet, Isabelle; Le Breton, Mathilde; Bréhin, Camille; Franchitto, Nicolas (April 2017). "A 10-year review of cannabis exposure in children under 3-years of age: do we need a more global approach?". European Journal of Pediatrics. 176 (4): 553–56. doi:10.1007/s00431-017-2872-5. ISSN 1432-1076. PMID 28210835. S2CID 11639790.
- ^ "New study shows marijuana doubles your risk of cardiovascular death". National Geographic Society. Archived from the original on 18 June 2025.
- ^ "Marijuana use dramatically increases risk of dying from heart attacks and stroke, large study finds". CNN. 17 June 2025.
- ^ Storck W, Elbaz M, Vindis C, et alCardiovascular risk associated with the use of cannabis and cannabinoids: a systematic review and meta-analysisHeart Published Online First: 17 June 2025. doi: 10.1136/heartjnl-2024-325429
- ^ Shamabadi A, Ahmadzade A, Pirahesh K, Hasanzadeh A, Asadigandomani H (December 2023). "Suicidality risk after using cannabis and cannabinoids: An umbrella review". Dialogues Clin Neurosci. 25 (1): 50–63. doi:10.1080/19585969.2023.2231466. PMC 10334849. PMID 37427882. S2CID 259499926.
- ^ Takakuwa KM, Schears RM (February 2021). "The emergency department care of the cannabis and synthetic cannabinoid patient: a narrative review". Int J Emerg Med (Review). 14 (1) 10. doi:10.1186/s12245-021-00330-3. PMC 7874647. PMID 33568074.
- ^ Rabin, Roni Caryn (6 February 2025). "Marijuana Dependence Linked to Higher Risk of Death". The New York Times. ISSN 0362-4331. Retrieved 8 February 2025.
- ^ Myran, Daniel T.; Pugliese, Michael; McDonald, André J.; Xiao, Jennifer; Fischer, Benedikt; Finkelstein, Yaron; Tanuseputro, Peter; Firth, Joseph; Pakpour, Amir; Hsu, Chih-Wei; Chang, Wing-Chung; Solmi, Marco (6 February 2025). "Cannabis Use Disorder Emergency Department Visits and Hospitalizations and 5-Year Mortality". JAMA Network Open. 8 (2): e2457852. doi:10.1001/jamanetworkopen.2024.57852. ISSN 2574-3805. PMC 11803479. PMID 39913138.
- ^ Myran, Daniel T.; Pugliese, Michael; Harrison, Lyndsay D.; Solmi, Marco; Anderson, Kelly K.; Fiedorowicz, Jess G.; Finkelstein, Yaron; Manuel, Doug; Taljaard, Monica; Webber, Colleen; Tanuseputro, Peter (4 February 2025). "Changes in Incident Schizophrenia Diagnoses Associated With Cannabis Use Disorder After Cannabis Legalization". JAMA Network Open. 8 (2): e2457868. doi:10.1001/jamanetworkopen.2024.57868. ISSN 2574-3805. PMC 11795325. PMID 39903464.
- ^ Nutt D, King LA, Saulsbury W, Blakemore C (March 2007). "Development of a rational scale to assess the harm of drugs of potential misuse". Lancet. 369 (9566): 1047–53. doi:10.1016/s0140-6736(07)60464-4. PMID 17382831. S2CID 5903121.
- ^ Schoeler T, Kambeitz J, Behlke I, Murray R, Bhattacharyya S (January 2016). "The effects of cannabis on memory function in users with and without psychotic disorder: findings from a combined meta-analysis". Psychological Medicine. 46 (1): 177–88. doi:10.1017/S0033291715001646. PMID 26353818. S2CID 23749219.
- ^ a b Schreiner AM, Dunn ME (October 2012). "Residual effects of cannabis use on neurocognitive performance after prolonged abstinence: a meta-analysis". Experimental and Clinical Psychopharmacology. 20 (5): 420–29. doi:10.1037/a0029117. PMID 22731735. S2CID 207618350.
Therefore, results indicate evidence for small neurocognitive effects that persist after the period of acute intoxication...As hypothesized, the meta-analysis conducted on studies eval- uating users after at least 25 days of abstention found no residual effects on cognitive performance...These results fail to support the idea that heavy cannabis use may result in long-term, persistent effects on neuropsychological functioning.
- ^ Gonzalez R, Carey C, Grant I (November 2002). "Nonacute (residual) neuropsychological effects of cannabis use: a qualitative analysis and systematic review". Journal of Clinical Pharmacology. 42 (S1): 48S – 57S. doi:10.1002/j.1552-4604.2002.tb06003.x. PMID 12412836. S2CID 37826919.
- ^ Crean RD, Crane NA, Mason BJ (March 2011). "An evidence based review of acute and long-term effects of cannabis use on executive cognitive functions". Journal of Addiction Medicine. 5 (1): 1–8. doi:10.1097/ADM.0b013e31820c23fa. PMC 3037578. PMID 21321675.
Cannabis appears to continue to exert impairing effects in executive functions even after 3 weeks of abstinence and beyond. While basic attentional and working memory abilities are largely restored, the most enduring and detectable deficits are seen in decision-making, concept formation and planning.
- ^ Broyd SJ, van Hell HH, Beale C, Yücel M, Solowij N (April 2016). "Acute and Chronic Effects of Cannabinoids on Human Cognition-A Systematic Review". Biological Psychiatry. 79 (7): 557–67. doi:10.1016/j.biopsych.2015.12.002. PMID 26858214. S2CID 9858298.
- ^ a b c d Curran HV, Freeman TP, Mokrysz C, Lewis DA, Morgan CJ, Parsons LH (May 2016). "Keep off the grass? Cannabis, cognition and addiction" (PDF). Nature Reviews. Neuroscience. 17 (5): 293–306. doi:10.1038/nrn.2016.28. hdl:10871/24746. PMID 27052382. S2CID 1685727. Archived from the original (PDF) on 22 September 2017. Retrieved 27 December 2018.
- ^ Ganzer F, Bröning S, Kraft S, Sack PM, Thomasius R (June 2016). "Weighing the Evidence: A Systematic Review on Long-Term Neurocognitive Effects of Cannabis Use in Abstinent Adolescents and Adults". Neuropsychology Review. 26 (2): 186–222. doi:10.1007/s11065-016-9316-2. PMID 27125202. S2CID 4335379.
- ^ a b Goldenberg M, IsHak WW, Danovitch I (January 2017). "Quality of life and recreational cannabis use". The American Journal on Addictions. 26 (1): 8–25. doi:10.1111/ajad.12486. PMID 28000973. S2CID 40707053.
- ^ Hampton WH, Hanik I, Olson IR (2019). "[Substance Abuse and White Matter: Findings, Limitations, and Future of Diffusion Tensor Imaging Research]". Drug and Alcohol Dependence. 197 (4): 288–298. doi:10.1016/j.drugalcdep.2019.02.005. PMC 6440853. PMID 30875650.
Given that [the human] central nervous system is an intricately balanced, complex network of billions of neurons and supporting cells, some might imagine that extrinsic substances could cause irreversible brain damage. Our review paints a less gloomy picture of the substances reviewed, however. Following prolonged abstinence, abusers of alcohol (Pfefferbaum et al., 2014) or opiates (Wang et al., 2011) have white matter microstructure that is not significantly different from nonusers. There was also no evidence that the white matter microstructural changes observed in longitudinal studies of cannabis, nicotine, or cocaine were completely irreparable. It is therefore possible that, at least to some degree, abstinence can reverse effects of substance abuse on white matter. The ability of white matter to "bounce back" very likely depends on the level and duration of abuse, as well as the substance being abused.
- ^ Yücel, M; Lorenzetti, V; Suo, C; Zalesky, A; Fornito, A; Takagi, M J; Lubman, D I; Solowij, N (January 2016). "Hippocampal harms, protection and recovery following regular cannabis use". Translational Psychiatry. 6 (1): e710–. doi:10.1038/tp.2015.201. PMC 5068875. PMID 26756903.
- ^ Rocchetti M, Crescini A, Borgwardt S, Caverzasi E, Politi P, Atakan Z, Fusar-Poli P (November 2013). "Is cannabis neurotoxic for the healthy brain? A meta-analytical review of structural brain alterations in non-psychotic users". Psychiatry and Clinical Neurosciences. 67 (7): 483–92. doi:10.1111/pcn.12085. PMID 24118193. S2CID 8245635.
- ^ a b Batalla A, Bhattacharyya S, Yücel M, Fusar-Poli P, Crippa JA, Nogué S, Torrens M, Pujol J, Farré M, Martin-Santos R (2013). "Structural and functional imaging studies in chronic cannabis users: a systematic review of adolescent and adult findings". PLOS ONE. 8 (2) e55821. Bibcode:2013PLoSO...855821B. doi:10.1371/journal.pone.0055821. PMC 3563634. PMID 23390554.
The most consistently reported brain alteration was reduced hippocampal volume which was shown to persist even after several months of abstinence in one study and also to be related to the amount of cannabis use Other frequently reported morphological brain alterations related to chronic cannabis use were reported in the amygdala the cerebellum and the frontal cortex...These findings may be interpreted as reflecting neuroadaptation, perhaps indicating the recruitment of additional regions as a compensatory mechanism to maintain normal cognitive performance in response to chronic cannabis exposure, particularly within the prefrontal cortex area.
- ^ a b Weinstein A, Livny A, Weizman A (2016). "Brain Imaging Studies on the Cognitive, Pharmacological and Neurobiological Effects of Cannabis in Humans: Evidence from Studies of Adult Users". Current Pharmaceutical Design. 22 (42): 6366–79. doi:10.2174/1381612822666160822151323. PMID 27549374.
1) The studies reviewed so far demonstrated that chronic cannabis use has been associated with a volume reduction of the hippocampus...3) The overall conclusion arising from these studies is that recent cannabis users may experience subtle neurophysiological deficits while performing on working memory tasks, and that they compensate for these deficits by "working harder" by using additional brain regions to meet the demands of the task.
- ^ Blest-Hopley G, Giampietro V, Bhattacharyya S (May 2018). "Residual effects of cannabis use in adolescent and adult brains – A meta-analysis of fMRI studies" (PDF). Neuroscience and Biobehavioral Reviews. 88: 26–41. doi:10.1016/j.neubiorev.2018.03.008. PMID 29535069. S2CID 4402954.
This may reflect the multitude of cognitive tasks employed by the various studies included in these meta-analyses, all of which involved performing a task thereby requiring the participant to reorient their attention and attempt to solve the problem at hand and suggest that greater engagement of this region indicates less efficient cognitive performance in cannabis users in general, irrespective of their age.
- ^ Parsons LH, Hurd YL (October 2015). "Endocannabinoid signalling in reward and addiction". Nature Reviews. Neuroscience. 16 (10): 579–94. doi:10.1038/nrn4004. PMC 4652927. PMID 26373473.
- ^ Zehra A, Burns J, Liu CK, Manza P, Wiers CE, Volkow ND, Wang GJ (March 2018). "Cannabis Addiction and the Brain: a Review". Journal of Neuroimmune Pharmacology. 13 (4): 438–52. doi:10.1007/s11481-018-9782-9. PMC 6223748. PMID 29556883.
- ^ Colizzi M, McGuire P, Pertwee RG, Bhattacharyya S (May 2016). "Effect of cannabis on glutamate signalling in the brain: A systematic review of human and animal evidence". Neuroscience and Biobehavioral Reviews. 64: 359–81. doi:10.1016/j.neubiorev.2016.03.010. PMID 26987641. S2CID 24043856.
- ^ Hall W, Degenhardt L (October 2009). "Adverse health effects of non-medical cannabis use". Lancet. 374 (9698): 1383–91. doi:10.1016/s0140-6736(09)61037-0. PMID 19837255. S2CID 31616272.
- ^ Subbaraman MS (2014). "Can cannabis be considered a substitute medication for alcohol?". Alcohol and Alcoholism. 49 (3): 292–98. doi:10.1093/alcalc/agt182. PMC 3992908. PMID 24402247.
- ^ Schoeler, Tabea; Baldwin, Jessie R.; Martin, Ellen; Barkhuizen, Wikus; Pingault, Jean-Baptiste (3 June 2024). "Assessing rates and predictors of cannabis-associated psychotic symptoms across observational, experimental and medical research". Nature Mental Health. 2 (7): 865–876. doi:10.1038/s44220-024-00261-x. ISSN 2731-6076. PMC 11236708. PMID 39005547.
- ^ Leweke FM, Mueller JK, Lange B, Rohleder C (April 2016). "Therapeutic Potential of Cannabinoids in Psychosis". Biological Psychiatry. 79 (7): 604–12. doi:10.1016/j.biopsych.2015.11.018. PMID 26852073. S2CID 24160677.
Epidemiological data indicate a strong relationship between cannabis use and psychosis and schizophrenia beyond transient intoxication with an increased risk of any psychotic outcome in individuals who had ever used cannabis
- ^ a b Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, Lewis G (July 2007). "Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review" (PDF). Lancet. 370 (9584): 319–28. doi:10.1016/S0140-6736(07)61162-3. PMID 17662880. S2CID 41595474.
- ^ Semple DM, McIntosh AM, Lawrie SM (March 2005). "Cannabis as a risk factor for psychosis: systematic review". Journal of Psychopharmacology. 19 (2): 187–94. doi:10.1177/0269881105049040. PMID 15871146. S2CID 44651274.
- ^ Large M, Sharma S, Compton MT, Slade T, Nielssen O (June 2011). "Cannabis use and earlier onset of psychosis: a systematic meta-analysis". Archives of General Psychiatry. 68 (6): 555–61. doi:10.1001/archgenpsychiatry.2011.5. PMID 21300939.
- ^ McLaren JA, Silins E, Hutchinson D, Mattick RP, Hall W (January 2010). "Assessing evidence for a causal link between cannabis and psychosis: a review of cohort studies". The International Journal on Drug Policy. 21 (1): 10–19. doi:10.1016/j.drugpo.2009.09.001. PMID 19783132.
The contentious issue of whether cannabis use can cause serious psychotic disorders that would not otherwise have occurred cannot be answered based on the existing data
- ^ Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, Rehm J (March 2014). "The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies". Psychological Medicine. 44 (4): 797–810. doi:10.1017/S0033291713001438. PMID 23795762. S2CID 36763290.
- ^ Kedzior KK, Laeber LT (May 2014). "A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population – a meta-analysis of 31 studies". BMC Psychiatry. 14 136. doi:10.1186/1471-244X-14-136. PMC 4032500. PMID 24884989.
- ^ Black, Nicola; Stockings, Emily; Campbell, Gabrielle; Tran, Lucy T.; Zagic, Dino; Hall, Wayne D.; Farrell, Michael; Degenhardt, Louisa (December 2019). "Cannabinoids for the treatment of mental disorders and symptoms of mental disorders: a systematic review and meta-analysis". The Lancet. Psychiatry. 6 (12): 995–1010. doi:10.1016/S2215-0366(19)30401-8. PMC 6949116. PMID 31672337.
- ^ a b VanDolah, Harrison J.; Bauer, Brent A.; Mauck, Karen F. (September 2019). "Clinicians' Guide to Cannabidiol and Hemp Oils". Mayo Clinic Proceedings. 94 (9): 1840–51. doi:10.1016/j.mayocp.2019.01.003. PMID 31447137.
- ^ Gobbi, Gabriella; Atkin, Tobias; Zytynski, Tomasz; Wang, Shouao; Askari, Sorayya; Boruff, Jill; Ware, Mark; Marmorstein, Naomi; Cipriani, Andrea; Dendukuri, Nandini; Mayo, Nancy (13 February 2019). "Cannabis Use in Adolescence and Risk of Depression, Anxiety, and Suicidality in Young Adulthood". JAMA Psychiatry. 76 (4): 426–34. doi:10.1001/jamapsychiatry.2018.4500. PMC 6450286. PMID 30758486.
- ^ Gordon AJ, Conley JW, Gordon JM (December 2013). "Medical consequences of marijuana use: a review of current literature". Current Psychiatry Reports. 15 (12) 419. doi:10.1007/s11920-013-0419-7. PMID 24234874. S2CID 29063282.
- ^ Subbaraman MS (8 January 2014). "Can cannabis be considered a substitute medication for alcohol?". Alcohol and Alcoholism. 49 (3): 292–98. doi:10.1093/alcalc/agt182. PMC 3992908. PMID 24402247.
- ^ Armentano, Paul (5 February 2019). "Marijuana access is associated with decreased use of alcohol, tobacco and other prescription drugs". The Hill.
- ^ Nourbakhsh, Mahra; Miller, Angela; Gofton, Jeff; Jones, Graham; Adeagbo, Bamidele (2019). "Cannabinoid Hyperemesis Syndrome: Reports of Fatal Cases". Journal of Forensic Sciences. 64 (1): 270–74. doi:10.1111/1556-4029.13819. ISSN 1556-4029. PMID 29768651. S2CID 21718690.
- ^ Rudavsky, Shari. "He loved weed. Then the vomiting began. Months later, he died". USA Today. Retrieved 2 August 2021.
- ^ Maisto S, Galizio M, Connors G (2014). Drug Use and Abuse. Cengage Learning. p. 278. ISBN 978-1-305-17759-8.
- ^ "Commonly Abused Drugs Charts: Marijuana (Cannabis)". National Institute on Drug Abuse, US National Institutes of Health. 22 July 2019. Retrieved 20 January 2020.
- ^ Owen KP, Sutter ME, Albertson TE (February 2014). "Marijuana: respiratory tract effects". Clinical Reviews in Allergy & Immunology. 46 (1): 65–81. doi:10.1007/s12016-013-8374-y. PMID 23715638. S2CID 23823391.
- ^ Tetrault JM, Crothers K, Moore BA, Mehra R, Concato J, Fiellin DA (February 2007). "Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review". Archives of Internal Medicine. 167 (3): 221–28. doi:10.1001/archinte.167.3.221. PMC 2720277. PMID 17296876.
- ^ Sorensen CJ, DeSanto K, Borgelt L, Phillips KT, Monte AA (March 2017). "Cannabinoid Hyperemesis Syndrome: Diagnosis, Pathophysiology, and Treatment-a Systematic Review". Journal of Medical Toxicology. 13 (1): 71–87. doi:10.1007/s13181-016-0595-z. PMC 5330965. PMID 28000146.
- ^ Hashibe M, Straif K, Tashkin DP, Morgenstern H, Greenland S, Zhang ZF (April 2005). "Epidemiologic review of marijuana use and cancer risk". Alcohol. 35 (3): 265–75. doi:10.1016/j.alcohol.2005.04.008. PMID 16054989.
- ^ "Does smoking cannabis cause cancer?". Cancer Research UK. 20 September 2010. Archived from the original on 29 July 2012. Retrieved 9 January 2013.
- ^ Tashkin, Donald (March 1997). "Effects of marijuana on the lung and its immune defenses". UCLA School of Medicine. Retrieved 23 June 2012.
- ^ Gates P, Jaffe A, Copeland J (July 2014). "Cannabis smoking and respiratory health: consideration of the literature". Respirology. 19 (5): 655–62. doi:10.1111/resp.12298. PMID 24831571. S2CID 29423964.
- ^ Huang YH, Zhang ZF, Tashkin DP, Feng B, Straif K, Hashibe M (January 2015). "An epidemiologic review of marijuana and cancer: an update". Cancer Epidemiology, Biomarkers & Prevention. 24 (1): 15–31. doi:10.1158/1055-9965.EPI-14-1026. PMC 4302404. PMID 25587109.
- ^ Tashkin DP (June 2013). "Effects of marijuana smoking on the lung". Annals of the American Thoracic Society. 10 (3): 239–47. doi:10.1513/annalsats.201212-127fr. PMID 23802821. S2CID 20615545.
- ^ Gurney J, Shaw C, Stanley J, Signal V, Sarfati D (November 2015). "Cannabis exposure and risk of testicular cancer: a systematic review and meta-analysis". BMC Cancer. 15 (1) 897. doi:10.1186/s12885-015-1905-6. PMC 4642772. PMID 26560314.
- ^ de Carvalho MF, Dourado MR, Fernandes IB, Araújo CT, Mesquita AT, Ramos-Jorge ML (December 2015). "Head and neck cancer among marijuana users: a meta-analysis of matched case-control studies". Archives of Oral Biology. 60 (12): 1750–55. doi:10.1016/j.archoralbio.2015.09.009. PMID 26433192.
- ^ Loflin M, Earleywine M (2015). "No smoke, no fire: What the initial literature suggests regarding vapourized cannabis and respiratory risk". Canadian Journal of Respiratory Therapy. 51 (1): 7–9. PMC 4456813. PMID 26078621.
- ^ Riecher-Rössler A (2014). Comorbidity of Mental and Physical Disorders. Karger Medical and Scientific Publishers. p. 88. ISBN 978-3-318-02604-7.
- ^ Ravi D, Ghasemiesfe M, Korenstein D, Cascino T, Keyhani S (February 2018). "Associations Between Marijuana Use and Cardiovascular Risk Factors and Outcomes: A Systematic Review". Annals of Internal Medicine. 168 (3): 187–94. doi:10.7326/M17-1548. PMC 6157910. PMID 29357394.
- ^ Thomas G, Kloner RA, Rezkalla S (January 2014). "Adverse cardiovascular, cerebrovascular, and peripheral vascular effects of marijuana inhalation: what cardiologists need to know". The American Journal of Cardiology. 113 (1): 187–90. doi:10.1016/j.amjcard.2013.09.042. PMID 24176069.
- ^ Franz CA, Frishman WH (9 February 2016). "Marijuana Use and Cardiovascular Disease". Cardiology in Review. 24 (4): 158–62. doi:10.1097/CRD.0000000000000103. PMID 26886465. S2CID 205566342.
- ^ Greger, Jessica; Bates, Vernice; Mechtler, Laszlo; Gengo, Fran (2020). "A review of cannabis and interactions with anticoagulant and antiplatelet agents". The Journal of Clinical Pharmacology. 60 (4): 432–38. doi:10.1002/jcph.1557. PMID 31724188. S2CID 208019237.
- ^ Shen, Jay J.; Shan, Guogen; Kim, Pearl C.; Yoo, Ji Won; Dodge-Francis, Carolee; Lee, Yong-Jae (2019). "Trends and Related Factors of Cannabis-Associated Emergency Department Visits in the United States: 2006–2014". Journal of Addiction Medicine. 13 (3): 193–200. doi:10.1097/ADM.0000000000000479. ISSN 1932-0620. PMID 30418337. S2CID 53286585.
- ^ Shelton, Shelby K.; Mills, Eleanor; Saben, Jessica L.; Devivo, Michael; Williamson, Kayla; Abbott, Diana; Hall, Katelyn E.; Monte, Andrew A. (2020). "Why do patients come to the emergency department after using cannabis?". Clinical Toxicology. 58 (6): 453–59. doi:10.1080/15563650.2019.1657582. ISSN 1556-9519. PMC 7073292. PMID 31526057.
- ^ a b "National Estimates of Drug-Related Emergency Department Visits" (PDF). Drug Abuse Warning Network. U.S. Department of Health and Human Services. 2011. Archived from the original (PDF) on 4 April 2015. Retrieved 8 May 2015.
- ^ Hayer S, Mandelbaum AD, Watch L, Ryan KS, Hedges MA, Manuzak JA, Easley CA, Schust DJ, Lo JO (July 2023). "Cannabis and Pregnancy: A Review". Obstet Gynecol Surv. 78 (7): 411–428. doi:10.1097/OGX.0000000000001159. PMC 10372687. PMID 37480292.
- ^ Nguyen, Patton Khuu; Hammond, S. Katharine (30 March 2022). "Fine Particulate Matter Exposure From Secondhand Cannabis Bong Smoking". JAMA. 5 (3): e224744. doi:10.1001/jamanetworkopen.2022.4744. PMC 8968464. PMID 35353170.
- ^ Bow, Eric (2016). "The Structure–Function Relationships of Classical Cannabinoids: CB1/CB2 Modulation". Perspectives in Medicinal Chemistry. 8 PMC.S32171: 17–39. doi:10.4137/PMC.S32171. PMC 4927043. PMID 27398024.
- ^ Thomas, A (2007). "Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro". Br J Pharmacol. 150 (5): 613–623. doi:10.1038/sj.bjp.0707133. PMC 2189767. PMID 17245363.
- ^ Wilson RI, Nicoll RA (April 2002). "Endocannabinoid signaling in the brain". Science. 296 (5568): 678–82. Bibcode:2002Sci...296..678W. doi:10.1126/science.1063545. PMID 11976437. S2CID 21573145.
- ^ Oleson EB, Cheer JF (August 2012). "A brain on cannabinoids: the role of dopamine release in reward seeking". Cold Spring Harbor Perspectives in Medicine. 2 (8) a012229. doi:10.1101/cshperspect.a012229. PMC 3405830. PMID 22908200.
- ^ Kathmann M, Flau K, Redmer A, Tränkle C, Schlicker E (February 2006). "Cannabidiol is an allosteric modulator at mu- and delta-opioid receptors". Naunyn-Schmiedeberg's Archives of Pharmacology. 372 (5): 354–61. doi:10.1007/s00210-006-0033-x. PMID 16489449. S2CID 4877869.
- ^ Hejazi N, Zhou C, Oz M, Sun H, Ye JH, Zhang L (March 2006). "Delta9-tetrahydrocannabinol and endogenous cannabinoid anandamide directly potentiate the function of glycine receptors". Molecular Pharmacology. 69 (3): 991–97. doi:10.1124/mol.105.019174. PMID 16332990. S2CID 21801428.
- ^ Xiong W, Cheng K, Cui T, Godlewski G, Rice KC, Xu Y, Zhang L (May 2011). "Cannabinoid potentiation of glycine receptors contributes to cannabis-induced analgesia". Nature Chemical Biology. 7 (5): 296–303. doi:10.1038/nchembio.552. PMC 3388539. PMID 21460829.
- ^ a b Hall W, Pacula RL (2003). Cannabis Use and Dependence: Public Health and Public Policy. Cambridge University Press. p. 15. ISBN 978-0-521-80024-2.
- ^ Hollister LE, et al. (March 1986). "Health aspects of cannabis". Pharma Review. 38 (38): 1–20. doi:10.1016/S0031-6997(25)06862-0. PMID 3520605. Archived from the original on 15 April 2013. Retrieved 17 February 2011.
- ^ Russo EB (2013). Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential. Routledge. p. 28. ISBN 978-1-136-61493-4.
- ^ Newton DE (2013). Marijuana: a reference handbook. Santa Barbara, Calif.: ABC-CLIO. p. 7. ISBN 978-1-61069-149-9.
- ^ Baselt RC (2008). Disposition of Toxic Drugs and Chemicals in Man. Biomedical Publications. pp. 1513–18. ISBN 978-0-9626523-7-0.
- ^ Shaw LM, Kwong TC (2001). The Clinical Toxicology Laboratory: Contemporary Practice of Poisoning Evaluation. Amer. Assoc. for Clinical Chemistry. p. 51. ISBN 978-1-890883-53-9.
- ^ "The Non-Specificity of the Duquenois-Levine Field Test for Marijuana". ResearchGate.
- ^ Venkatratnam A, Lents NH (July 2011). "Zinc reduces the detection of cocaine, methamphetamine, and THC by ELISA urine testing". Journal of Analytical Toxicology. 35 (6): 333–40. doi:10.1093/anatox/35.6.333. PMID 21740689.
- ^ Lin CN, Strathmann FG (10 July 2013). "Elevated urine zinc concentration reduces the detection of methamphetamine, cocaine, THC and opiates in urine by EMIT". Journal of Analytical Toxicology. 37 (9): 665–69. doi:10.1093/jat/bkt056. PMID 23843421.
- ^ Joy JE, Watson SJ, Benson JA (1999). Marijuana and Medicine: Assessing The Science Base. Washington, D.C.: National Academy of Sciences Press. Bibcode:1999nap..book.6376I. doi:10.17226/6376. ISBN 978-0-585-05800-9. PMID 25101425.
- ^ Elliott S. "The Ultimate Guide on Indicas vs. Sativas". Herb. Retrieved 22 June 2018.
- ^ Piomelli D, Russo EB (2016). "The Cannabis sativa Versus Cannabis indica Debate: An Interview with Ethan Russo, MD". Cannabis and Cannabinoid Research. 1 (1): 44–46. doi:10.1089/can.2015.29003.ebr. PMC 5576603. PMID 28861479.
- ^ Iseger TA, Bossong MG (March 2015). "A systematic review of the antipsychotic properties of cannabidiol in humans". Schizophrenia Research. 162 (1–3): 153–61. doi:10.1016/j.schres.2015.01.033. PMID 25667194. S2CID 3745655.
- ^ a b c "Why Does Cannabis Potency Matter?". United Nations Office on Drugs and Crime. 29 June 2009.
- ^ "Cannabis strength soars over past half century". ScienceDaily. 16 November 2020.
- ^ ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC (2016). "Changes in Cannabis Potency Over the Last 2 Decades (1995–2014): Analysis of Current Data in the United States". Biological Psychiatry. 79 (7): 613–619. doi:10.1016/j.biopsych.2016.01.004. PMC 4987131. PMID 26903403.
- ^ Cascini F, Aiello C, Di Tanna G (March 2012). "Increasing delta-9-tetrahydrocannabinol (Δ-9-THC) content in herbal cannabis over time: systematic review and meta-analysis". Current Drug Abuse Reviews. 5 (1): 32–40. doi:10.2174/1874473711205010032. PMID 22150622. S2CID 24350419.
- ^ Smith D (17 January 2014). "Cannabis and memory loss: dude, where's my CBD?". The Guardian.
- ^ "Cannabis Potency". National Cannabis Prevention and Information Centre. Archived from the original on 6 December 2011. Retrieved 13 December 2011.
- ^ "BBC: Cannabis laws to be strengthened. May 2008 20:55 UK". BBC News. 7 May 2008. Retrieved 20 September 2010.
- ^ Di Forti M, Morgan C, Dazzan P, Pariante C, Mondelli V, Marques TR, Handley R, Luzi S, et al. (December 2009). "High-potency cannabis and the risk of psychosis". The British Journal of Psychiatry. 195 (6): 488–91. doi:10.1192/bjp.bp.109.064220. PMC 2801827. PMID 19949195.
- ^ Hope, Christopher (6 February 2008). "Use of extra strong 'skunk' cannabis soars". The Daily Telegraph. London. Archived from the original on 10 January 2022.
- ^ Doweiko H (2011). Concepts of Chemical Dependency. Cengage Learning. p. 124. ISBN 978-1-133-17081-5.
- ^ "Fake Hanf: Ein Drogentrend schwappt in die Schweiz – was du darüber wissen musst". Watson (in German).
- ^ "Fake Hanf: Tödliches Marihuana hat bereits 61 Menschen getötet". Watson (in German).
- ^ "Fake Hanf mit synthetischen Cannabinoiden besprüht". drugcom (in German).
- ^ "Tödlicher Fake Hanf – Chemisch behandelte Hanfblüten – niemand kann sie erkennen". Schweizer Radio und Fernsehen (SRF) (in German). 14 August 2020.
- ^ "Growing Array of Street Drugs Now Laced with Fentanyl", MedPageToday, 17 July 2018
- ^ "Is the opioid epidemic now the fentanyl epidemic?" Archived 18 December 2018 at the Wayback Machine, The Baltimore Sun, 7 December 2018
- ^ "Medical officials oppose effort to legalize recreational use of marijuana", State Journal-Register, (Springfield, IL), 15 December 2018
- ^ a b Spanish Word Histories and Mysteries: English Words That Come From Spanish. Houghton Mifflin Harcourt. 2007. p. 142. ISBN 978-0-547-35021-9.
- ^ Potter G, Bouchard M, Decorte T (2013). World Wide Weed: Global Trends in Cannabis Cultivation and its Control (revised ed.). Ashgate Publishing, Ltd. p. 17. ISBN 978-1-4094-9438-6.
- ^ Hall W, Pacula RL (2003). Cannabis Use and Dependence: Public Health and Public Policy. Cambridge University Press. p. 13. ISBN 978-0-521-80024-2.
- ^ United Nations Office on Drugs and Crime (2009). Recommended Methods for the Identification and Analysis of Cannabis and Cannabis Products. United Nations Publications. p. 15. ISBN 978-92-1-148242-3.
- ^ a b Houck MM (2015). Forensic Chemistry. Elsevier Science. p. 131. ISBN 978-0-12-800624-5.
- ^ Adler PA, Adler P, O'Brien PK (2012). Drugs and the American Dream: An Anthology. John Wiley & Sons. pp. 330–. ISBN 978-0-470-67027-9.
- ^ Mosher CJ, Akins SM (2013). Drugs and Drug Policy: The Control of Consciousness Alteration. Sage Publications. p. 17. ISBN 978-1-4833-2188-2.
- ^ "Hemp Facts". Naihc.org. Archived from the original on 27 November 2012. Retrieved 9 January 2013.
- ^ Earleywine, Mitch (2002). Understanding Marijuana: A New Look at the Scientific Evidence. Oxford University Press. p. 3. ISBN 978-0-19-988143-7.
- ^ Rosenthal E (2002). Ask Ed: Marijuana Gold: Trash to Stash. QUICK AMER Publishing Company. p. 116. ISBN 978-0-932551-52-8.
- ^ "Kief". Cannabis Culture. Cannabisculture.com. 9 March 2005. Archived from the original on 5 June 2009. Retrieved 2 January 2010.
- ^ Bukszpan D (2012). Is That a Word?: From AA to ZZZ, the Weird and Wonderful Language of SCRABBLE. Chronicle Books. p. 94. ISBN 978-1-4521-0824-7.
- ^ "Hashish". dictionary.reference.com.
- ^ Slade, Desmond; Mehmedic, Zlato; Chandra, Suman; ElSohly, Mahmoud (2012). "Is cannabis becoming more potent?". In Castle, David; Murray, Robin M.; Cyril D'Souza, Deepak (eds.). Marijuana and Madness (Second Edition). Cambridge University Press. p. 35.
- ^ Goldberg R (2012). Drugs Across the Spectrum (7th ed.). Cengage Learning. p. 255. ISBN 978-1-133-59416-1.
- ^ Alchimia Blog, Rosin Hash
- ^ Cohen JA, Rudick RA (2011). Multiple Sclerosis Therapeutics. Cambridge University Press. p. 670. ISBN 978-1-139-50237-5.
- ^ King LA (2009). Forensic Chemistry of Substance Misuse: A Guide to Drug Control. Royal Society of Chemistry. p. 78. ISBN 978-0-85404-178-7.
- ^ "Dabs – marijuana's explosive secret". CNBC. 24 February 2014. Retrieved 28 February 2014.
- ^ World Drug Report. United Nations Publications. 2009. p. 98. ISBN 978-92-1-148240-9.
- ^ Alison Hallett for Wired. 20 February 2013 Hash Oil is Blowing Up Across the U.S. – Literally
- ^ Kintz P (2014). Toxicological Aspects of Drug-Facilitated Crimes. Elsevier Science. p. 141. ISBN 978-0-12-416969-2.
- ^ McDonough E (2012). The Official High Times Cannabis Cookbook: More Than 50 Irresistible Recipes That Will Get You High. Chronicle Books. p. 17. ISBN 978-1-4521-0133-0.
- ^ Sociedad de Psiquiatría y Neurología de la infancia y la Adolescencia (2016). Marihuana: Consensos y evidencias sobre su impacto en la salud (in Spanish). Editorial Forja. p. 35. ISBN 978-956-338-260-0. Retrieved 17 July 2021.
- ^ Trejos Rosero, Luis Fernando (2016). Fronteras: fuentes de conflicto y cooperación (in Spanish). Luis Fernando Trejos Rosero, Universidad del Norte. Departamento de Ciencia Política y Relaciones Internacionales. Barranquilla, Colombia. pp. 111. ISBN 978-958-741-689-3. OCLC 979988717.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Stuardo, S. (5 September 2015). "Marihuana prensada: El lado negro de la hierba canábica". BioBioChile (in Spanish). Retrieved 17 June 2021.
- ^ Wicht, J. J. (1991). Por un Perú mejor: exposiciones y debates del Primer Programa de Alta Especialización para Parlamentarios (in Spanish). Universidad del Pacífico. Centro de Investigación, Asociación Acción y Pensamiento Democrático (Lima, Peru), Konrad-Adenauer-Stiftung. Internationales Institut. p. 206. Retrieved 17 June 2021.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ ElSohly MA (2007). Marijuana and the Cannabinoids. Springer. p. 19. ISBN 978-1-59259-947-9.
- ^ Stafford PG, Bigwood J (1992). Psychedelics Encyclopedia. Ronin Publishing. p. 157. ISBN 978-0-914171-51-5.
- ^ Barber EJ (1992). Prehistoric Textiles: The Development of Cloth in the Neolithic and Bronze Ages with Special Reference to the Aegean. Princeton University Press. p. 17.
- ^ Anthony, David W. (2007). The Horse, the Wheel, and Language: How Bronze-Age Riders from the Eurasian Steppes Shaped the Modern World. Princeton University Press. p. 362. ISBN 978-0-691-05887-0.
- ^ Ellens, J. Harold (2014). Seeking the Sacred with Psychoactive Substances: Chemical Paths to Spirituality and to God. ABC-CLIO. pp. 24, 31. ISBN 978-1-4408-3088-4.
- ^ Rudgley R (1998). "Soma". The Encyclopedia of Psychoactive Substances. Little, Brown and Company. ISBN 978-0-349-11127-8.
- ^ Franck M (1997). Marijuana Grower's Guide. Red Eye Press. p. 3. ISBN 978-0-929349-03-9.
- ^ Rubin VD (1976). Cannabis and Culture. Campus Verlag. p. 305. ISBN 978-3-593-37442-0.
- ^ Cunliffe BW (2001). The Oxford Illustrated History of Prehistoric Europe. Oxford University Press. p. 405. ISBN 978-0-19-285441-4.
- ^ Schultes, Richard Evans (1976). Hallucinogenic Plants. Illustrated by Elmer W. Smith. New York: Golden Press. p. 34. ISBN 978-0-307-24362-1.
- ^ Staelens, Stefanie (10 March 2015). "The Bhang Lassi Is How Hindus Drink Themselves High for Shiva". Vice.com. Retrieved 10 August 2017.
- ^ Vij (2012). Textbook Of Forensic Medicine And Toxicology: Principles And Practice. Elsevier India. p. 672. ISBN 978-81-312-1129-8.See also article on Marijuana as a word.
- ^ Shorter Oxford English Dictionary (6th ed.), Oxford University Press, 2007, ISBN 978-0-19-920687-2
- ^ Ren M, Tang Z, Wu X, Spengler R, Jiang H, Yang Y, Boivin N (June 2019). "The origins of cannabis smoking: Chemical residue evidence from the first millennium BCE in the Pamirs". Science Advances. 5 (6) eaaw1391. Bibcode:2019SciA....5.1391R. doi:10.1126/sciadv.aaw1391. PMC 6561734. PMID 31206023.
- ^ Donahue, Michelle (12 June 2019). "Earliest evidence for cannabis smoking discovered in ancient tombs". National Geographic. Archived from the original on 13 June 2019.
- ^ Walton RP (1938). Marijuana, America's New Drug Problem. JB Lippincott. p. 6.
- ^ Taymiyya I (2001). Le haschich et l'extase (in French). Beyrouth: Albouraq. ISBN 978-2-84161-174-4.
- ^ Rubin V (1975). Cannabis and Culture. Walter de Gruyter. pp. 77–. ISBN 978-3-11-081206-0.
Cannabis Smoking in 13th-14th Century Ethiopia: Chemical Evidence
- ^ Booth, Martin (2004). Cannabis: A History. Picador. p. 38.
- ^ David E. Newton (2017). Marijuana: A Reference Handbook, 2nd Edition. p. 325.
- ^ Eileen Konieczny, Lauren Wilson (2018). Healing with CBD.
- ^ Pilkington, Mark (27 July 2005). "Clouds of smoke". The Guardian. Retrieved 10 November 2022.
- ^ Iversen LL (2007). The Science of Marijuana. Oxford University Press. pp. 110–. ISBN 978-0-19-988693-7.
- ^ A Collection of the Laws of Mauritius and Its Dependencies. By the authority of the Government. 1867. pp. 541–.
- ^ Bunyapraphatsōn N (1999). Medicinal and poisonous plants. Backhuys Publishers. p. 169. ISBN 978-90-5782-042-7.
- ^ "Statement of Dr. William C. Woodward". Drug library. Retrieved 20 September 2010.
The District of Columbia law, insofar as it relates to Cannabis, is a part of an act passed by Congress in 1906 entitled "An act to regulate the practice of pharmacy and the sale of poisons in the District of Columbia, and for other purposes", approved May 17, 1906, and originally published as 34 Statutes, 175, which is now to be found in the District Code, section 191 and following. It limits the sale of Cannabis, its derivatives and its preparations to pharmacists and persons who are authorized assistants to pharmacists.
- ^ The Opium and Narcotic Drug Act, 1923, S.C. 1923, c. 22
- ^ Willoughby WW (1925). "Opium as an international problem". Baltimore: The Johns Hopkins Press. Retrieved 20 September 2010.
- ^ Opium as an international problem: the Geneva conferences – Westel Woodbury Willoughby at Google Books
- ^ Pub. L. 75–238, 50 Stat. 551, enacted August 2, 1937
- ^ Booth M (2004). Cannabis: A History. Picador. p. 338. ISBN 978-0-312-42494-7.
- ^ Michael Tonry (2015). Crime and Justice. A Review of Research. Vol. 44. University of Chicago Press. pp. 261–. ISBN 978-0-226-34102-6.
- ^ Use drop-down menu on site to view Netherlands entry.), Eldd.emcdda.europa.eu, archived from the original on 7 May 2010, retrieved 17 February 2011
- ^ Drugs Policy in the Netherlands, Ukcia.org, archived from the original on 2 August 2017, retrieved 17 February 2011
- ^ "Amsterdam Will Ban Tourists from Pot Coffee Shops". Atlantic Wire. 27 May 2011. Archived from the original on 28 May 2011. Retrieved 23 June 2011.
- ^ Dockterman E (29 June 2012). "Marijuana Now the Most Popular Drug in the World". Time NewsFeed. Time Inc. Retrieved 16 March 2013.
- ^ "Factsheet". World Drug Report 2017. United Nation Office on Drugs and Crime (UNODC).
- ^ Ayyagari S (2007). ""Hori Hai": A Festival of Colours!! (review)". Asian Music. 38 (2). Johns Hopkins University Press: 151–53. doi:10.1353/amu.2007.0029. S2CID 192201145.
- ^ Rubin, 1975. p. 1
- ^ a b Rubin, 1975. p. 3
- ^ a b Rubin, 1975. p. 4
- ^ Levinson D (2002). Encyclopedia of Crime and Punishment. Sage Publications. p. 572. ISBN 978-0-7619-2258-2.
- ^ "Many Dutch coffee shops close as liberal policies change, Exaptica". Expatica.com. 27 November 2007. Archived from the original on 29 April 2011. Retrieved 20 September 2010.
- ^ "43 Amsterdam coffee shops to close door", Radio Netherlands, Friday 21 November 2008 Archived 2 December 2008 at the Wayback Machine
- ^ O'Sullivan F (3 March 2014). "Why the Mayor of Copenhagen Wants to Get Into the Marijuana Business". Bloomberg.com. Retrieved 23 January 2018.
- ^ Johnston I (5 January 2014). "As cannabis is widely legalised, China cashes in on an unprecedented boom". Independent. Retrieved 23 January 2018.
- ^ Liljas P (3 June 2017). "Could Thailand, which gave world the bong, legalise cannabis for medicinal use? After failed war on drugs, attitudes have softened". Post Magazine. Retrieved 23 January 2018.
- ^ "Marijuana goes legal in Washington state amid mixed messages". Reuters. 7 December 2012. Archived from the original on 24 September 2015. Retrieved 14 December 2012.
- ^ Duke A (8 November 2012). "2 states legalize pot, but don't 'break out the Cheetos' yet". CNN.com. Retrieved 2 January 2013.
- ^ "Marijuana clubs ring in new year in Colorado as legalized pot smoking begins". Abcnews.go.com. 1 January 2013. Retrieved 2 January 2013.
- ^ Mintz H (6 May 2013). "Medical pot: California Supreme Court allows cities to ban weed dispensaries". Marin Independent Journal. Archived from the original on 2 November 2013.
- ^ "US drug control agency will move to reclassify marijuana in a historic shift, AP sources say". AP News. 30 April 2024. Retrieved 30 April 2024.
- ^ "Biden administration plans to drastically change federal rules on marijuana". USA TODAY. Retrieved 30 April 2024.
- ^ Baker V (11 December 2013). "Marijuana laws around the world: what you need to know". The Guardian.
- ^ Castaldi, Malena (19 July 2017). "Uruguay pharmacies start selling cannabis straight to consumers". Reuters. Montevideo.
- ^ Scotti, Monique (20 June 2018). "Marijuana to be legal in Canada starting October 17, Trudeau confirms".
- ^ Sapra, Bani (20 June 2018). "Canada becomes second nation in the world to legalize marijuana". CNN.
- ^ "Uttarakhand To Become First Indian State To Legalise Cannabis Cultivation". Indiatimes. 27 November 2015. Retrieved 12 March 2017.
- ^ a b "South Asia Regional Profile Report" (PDF). UNODC.
- ^ Alchimia Blog, Medical marijuana news, December 2015
- ^ a b Butler, Patrick (17 October 2018). "Cannabis is legal in Canada – here's what you need to know". CBC. Retrieved 1 November 2018.
- ^ Sapra, Bani (20 June 2018). "Canada becomes second nation in the world to legalize marijuana". CNN. Retrieved 1 November 2018.
- ^ "Cannabis Act (S.C. 2018, c. 16)". Justice Canada. Government of Canada. Archived from the original on 25 March 2022. Retrieved 24 November 2018.
- ^ "This Application Seems Rigorous. Are All These Hoops Necessary?". LicensedProducersCanada.com. 5 July 2018. Retrieved 1 November 2018.
- ^ "Will Craft Cannabis Growers in Canada Succeed Like Craft Brewers?". LicensedProducersCanada.com. October 2018. Retrieved 1 November 2018.
- ^ Parliament of the Czech Republic (1998), Explanatory Report to Act No. 112/1998 Coll., which amends the Act No. 140/1961 Coll., the Criminal Code, and the Act No. 200/1990 Coll., on misdemeanors (in Czech), Prague
{{citation}}: CS1 maint: location missing publisher (link) "Podle čl. 36 Jednotné úmluvy o omamných látkách ze dne 31. března 1961 (č. 47/1965 Sb.) se signatáři zavazují k trestnímu postihu tam uvedených forem nakládání s drogami včetně jejich držby. Návrh upouští od dosavadní beztrestnosti držby omamných a psychotropních látek a jedů pro svoji potřebu. Dosavadní beztrestnost totiž eliminuje v řadě případů možnost postihu dealerů a distributorů drog." - ^ Castaneda JG (31 March 2012). "The summit of muted intentions". aljazeera.com.
- ^ "Congreso aprobó, en último debate, uso medicinal de la marihuana". 25 May 2016.
- ^ "Dosis máximas de droga para consumo ya están vigentes" Archived 24 June 2013 at the Wayback Machine at El Comercio.com.
- ^ "Ecuador: Aprueban tenencia de drogas para consumo" Archived 25 June 2013 at the Wayback Machine at El Nuevo Herald
- ^ "Ecuador could regulate the drug industry". Archived from the original on 24 June 2013.
- ^ "Drug policy profiles – Portugal" (PDF). 1 June 2011. Retrieved 5 February 2017.
- ^ Lindeque, Mia. "Dagga users celebrate following ConCourt ruling on private use". Retrieved 3 November 2018.
- ^ Williams, Sean (28 April 2019). "Mexico Aims to Legalize Recreational Marijuana Before October". The Motley Fool. Retrieved 29 April 2019.
- ^ Vélez, Manuel (17 October 2009). "Ley de Narcomenudeo". El Pensador. Archived from the original on 27 March 2012. Retrieved 29 September 2016.
- ^ "Mexico marijuana: Top court decriminalises recreational use of cannabis". BBC News. 28 June 2021. Archived from the original on 20 January 2024.
- ^ "Germany becomes largest EU country to legalize cannabis for recreational use". Le Monde.fr. 1 April 2024. Retrieved 19 April 2024.
- ^ Ross, Selena (6 June 2018). "All eyes on Canada as first G7 nation prepares to make marijuana legal". The Guardian. Retrieved 10 July 2018.
- ^ Sapra, Bani (20 June 2018). "Canada becomes second nation in the world to legalize marijuana". CNN.
- ^ "Marijuana Overview". National Conference of State Legislatures. Archived from the original on 24 June 2018. Retrieved 29 August 2019.
- ^ Smith, Tasha (5 June 2018). ""New Amsterdam" No More? Spain's Cannabis Clubs Fight to Stay Open". Merry Jane. Retrieved 23 August 2018.
- ^ Haines, Gavin (21 February 2017). "Everything you need to know about marijuana smoking in the Netherlands". The Telegraph. Archived from the original on 10 January 2022. Retrieved 22 July 2018.
- ^ "The Legal Situation of Cannabis in the Netherlands". Strain Insider. 20 May 2020. Archived from the original on 18 June 2020. Retrieved 2 June 2020.
- ^ Bubola, Emma (15 December 2021). "Malta Becomes First E.U. Country to Legalize Marijuana". The New York Times. Archived from the original on 28 December 2021.
- ^ Massa, Silja (29 June 2019). "Kevytkannabis saapui Viroon – Suomalaisturistin ei kannata ostaa tuliaisiksi Virossa laillisia tuotteita". Yle (in Finnish). Retrieved 25 September 2022.
- ^ "Lebanon legalizes cannabis farming for medicinal use". Reuters. 21 April 2020.
- ^ "Is Weed Legal in Japan? And Other Vacation Info for Cannabis Users". 6 February 2020.
- ^ "Here are the absolute worst places on earth to be caught with weed". thegrowthop.
- ^ "Bong arm of the law: South Korea says it will arrest citizens who smoke weed in Canada". TheGuardian.com. 23 October 2018.
- ^ "World Drug Report 2006". United Nations Office on Drugs and Crime. Ch. 2.3.
- ^ a b c Turco, Bucky (25 September 2017). "Why is Weed Getting More Potent". Gizmodo.
- ^ Forbes D (19 November 2002). "The Myth of Potent Pot". Slate.com.
- ^ a b c d e f United Nations. "World Drug Report 2013" (PDF). United Nations Office on Drugs and Crime. Retrieved 13 December 2014.
- ^ "Medical Use of Marijuana". Health Canada. Retrieved 12 January 2015.
- ^ "New Colombia Resources Inc Subsidiary, Sannabis, Produces First Batch of Medical Marijuana Based Products in Colombia to Fill Back Orders". prnewswire.com (Press release). PR Newswire. Retrieved 12 January 2015.
- ^ Moussaoui R (25 November 2013). "Lebanon cannabis trade thrives in shadow of Syrian war". AFP.
- ^ a b Garelli SL (25 November 2008). "Mexico, Paraguay top pot producers, U.N. report says". CNN International. Retrieved 28 September 2013.
- ^ Jackman, Robert (12 January 2019). "How Britain became the world's largest exporter of medical marijuana". The Spectator. Retrieved 27 December 2019.
- ^ "Cannabis: Wholesale, street prices and purity levels" (PDF). UNODC.org. 2005. Retrieved 9 January 2013.
- ^ "Report on U.S. Domestic Marijuana Production". NORML. Archived from the original on 26 December 2009. Retrieved 2 January 2010.
- ^ "Marijuana Called Top U.S. Cash Crop". 2008 ABCNews Internet Ventures. 20 December 2006.
- ^ United Nations Office on Drugs and Crime (2008). World drug report (PDF). United Nations Publications. p. 268. ISBN 978-92-1-148229-4.
- ^ Sharma, Rakesh (25 June 2019). "How Federal Legalization Could Transform The US Cannabis Market". Investopedia. Retrieved 24 July 2019.
- ^ Hughes, Trevor (23 May 2019). "As marijuana prices drop, growers push 'organic' cannabis – with a higher price tag". USA Today. Retrieved 24 July 2019.
- ^ European Monitoring Centre for Drugs and Drug Addiction (2008). Annual report: the state of the drugs problem in Europe (PDF). Luxembourg: Office for Official Publications of the European Communities. p. 38. ISBN 978-92-9168-324-6. Archived from the original (PDF) on 25 April 2013. Retrieved 1 July 2009.
- ^ a b "RAND study casts doubt on claims that marijuana acts as a "gateway" to the use of cocaine and heroin". RAND Corporation. 2 December 2002. Archived from the original on 4 November 2006.
- ^ "Public Views of Marijuana – Legalization, Decriminalization, Concerns". Pew Research Center for the People and the Press. 2 April 2014.
- ^ Mosher CJ, Akins S (2007). Drugs and Drug Policy: The Control of Consciousness Alteration. Sage Publications. p. 18. ISBN 978-0-7619-3007-5.
- ^ Saitz R (18 February 2003). "Is marijuana a gateway drug?". Journal Watch. 2003 (218): 1. Archived from the original on 10 July 2003.
- ^ Degenhardt L, Coffey C, Carlin JB, Moran P, Patton GC (August 2007). "Who are the new amphetamine users? A 10-year prospective study of young Australians". Addiction. 102 (8): 1269–79. doi:10.1111/j.1360-0443.2007.01906.x. PMID 17624977.
- ^ "3 The Experience of Drug Users". 2009/10 Scottish Crime and Justice Survey: Drug Use. The Scottish Government. 21 January 2011. Retrieved 5 November 2013.
- ^ Morral AR, McCaffrey DF, Paddock SM (December 2002). "Reassessing the marijuana gateway effect". Addiction. 97 (12): 1493–504. doi:10.1046/j.1360-0443.2002.00280.x. PMID 12472629. S2CID 2833456.
- ^ "Marijuana Policy Project – FAQ". Archived from the original on 22 June 2008.
- ^ Torabi MR, Bailey WJ, Majd-Jabbari M (September 1993). "Cigarette smoking as a predictor of alcohol and other drug use by children and adolescents: evidence of the "gateway drug effect"". The Journal of School Health. 63 (7): 302–06. doi:10.1111/j.1746-1561.1993.tb06150.x. PMID 8246462.
- ^ Vanyukov MM, Tarter RE, Kirillova GP, Kirisci L, Reynolds MD, Kreek MJ, Conway KP, Maher BS, Iacono WG, Bierut L, Neale MC, Clark DB, Ridenour TA (June 2012). "Common liability to addiction and "gateway hypothesis": theoretical, empirical and evolutionary perspective". Drug and Alcohol Dependence (Review). 123 (Suppl 1): S3–17. doi:10.1016/j.drugalcdep.2011.12.018. PMC 3600369. PMID 22261179.
- ^ a b c "Marijuana Research Report:Is marijuana a gateway drug?". National Institute on Drug Abuse. July 2020. Retrieved 7 November 2020.
- ^ "Marijuana Research: Current restrictions on marijuana research are absurd". Scientific American. 22 November 2004. Archived from the original on 7 November 2010. Retrieved 15 January 2013.
- ^ Ponto LL (May 2006). "Challenges of marijuana research". Brain. 129 (Pt 5): 1081–83. doi:10.1093/brain/awl092. PMID 16627464.
- ^ Jha A (31 May 2012). "Ecstasy and cannabis should be freely available for study, says David Nutt". The Guardian. Retrieved 15 January 2013.
- ^ "Medical Marijuana Policy in the United States". Stanford.edu. 15 May 2012. Retrieved 15 January 2013.
- ^ Conaboy C (19 October 2012). "Research into marijuana's medical benefits limited; scientists cite challenge of studying an illegal drug". Boston Globe. Archived from the original on 21 October 2012. Retrieved 15 January 2013.
- ^ "FDA and Cannabis: Research and Drug Approval Process". US Food and Drug Administration. 14 January 2020. Retrieved 21 January 2020.
- ^ Peters EN, Budney AJ, Carroll KM (August 2012). "Clinical correlates of co-occurring cannabis and tobacco use: a systematic review". Addiction. 107 (8): 1404–17. doi:10.1111/j.1360-0443.2012.03843.x. PMC 3377777. PMID 22340422.
- ^ "Does smoking cannabis cause cancer?". Cancer Research UK (CRUK). 30 August 2017. Archived from the original on 19 December 2013. Retrieved 26 December 2013.
Further reading
[edit]- Booth, Martin (2004). Cannabis: A History. Picador. ISBN 978-0-312-42494-7.
- Drake, Bill (2002). The Marijuana Food Handbook: A Guide for the Sensuous Connoisseur. Ronin Publishing. ISBN 978-0-914171-99-7.
- Grinspoon, Lester (1994). Marihuana Reconsidered. Quick American Archives. ISBN 978-0-932551-13-9.
External links
[edit] Media related to Cannabis at Wikimedia Commons
Media related to Cannabis at Wikimedia Commons The dictionary definition of marijuana at Wiktionary
The dictionary definition of marijuana at Wiktionary- "Cannabis". European Union Drugs Agency (EUDA).
Cannabis (drug)
View on GrokipediaEtymology and Classification
Etymology
The English term "cannabis" derives from the Latin cannabis, adopted in the 18th century to denote the hemp plant, which traces back to the Ancient Greek kánnabis (κάνναβις), referring to hemp fibers or the plant itself.[11] This Greek word is attested as early as the 5th century BCE and is posited to originate from a Scythian or Thracian loanword, spoken by ancient nomadic peoples of the Eurasian steppes who cultivated and used the plant for its psychoactive properties. In Neo-Assyrian Akkadian, cannabis was known as qunnabu (𒋆𒄣𒌦𒈾𒁍), referring to a plant used as a source of oil, fiber, and medicine during the 1st millennium BC, likely a loanword from Scythian due to historical contacts between the Neo-Assyrians and Scythians.[12] Linguistic evidence suggests the root may connect to Proto-Indo-European forms related to "cane" or "reed," reflecting the plant's fibrous stem, though direct etymological links remain speculative due to limited Scythian textual records.[13] In historical contexts, kánnabis primarily denoted industrial hemp (Cannabis sativa) for rope and textiles, as evidenced by Greek and Roman agricultural texts, but by the 19th century, "cannabis" in English medical literature specifically referenced psychoactive extracts like hashish or Indian hemp resin, distinguishing it from non-intoxicating fiber varieties.[11] The term's adoption in scientific nomenclature occurred in 1728 with Carl Linnaeus's classification of the genus Cannabis, formalizing its botanical identity amid growing recognition of its dual utility in fiber production and medicinal or recreational intoxication.[14] Unlike the later American slang "marijuana," which emerged around 1910 from Mexican Spanish influences and carried stigmatizing connotations tied to anti-immigrant campaigns, "cannabis" retained a neutral, scholarly tone rooted in classical linguistics.[15]Botanical and Taxonomic Classification
Cannabis belongs to the genus Cannabis in the family Cannabaceae, order Rosales.[16] The family also includes the genus Humulus (hops), sharing morphological and chemical similarities such as glandular trichomes producing resins.[16] Taxonomically, the genus is monotypic according to many botanists, comprising a single species Cannabis sativa L., described by Carl Linnaeus in 1753 based on European hemp varieties.[16] However, classifications vary, with some recognizing three species—C. sativa, C. indica Lam. (described in 1785 from Indian specimens), and C. ruderalis Janisch. (described in 1924 from Russian wild populations)—while others treat indica and ruderalis as subspecies or varieties within C. sativa due to interbreeding capabilities and genetic overlap.[16] Morphological distinctions underpin much of the taxonomic debate, though genetic analyses often support a single species with ecotypes adapted to different environments.[16] C. sativa subsp. sativa typically exhibits tall stature (up to 6 meters), narrow leaflets, and low-THC fiber production suited to temperate climates, whereas subsp. indica features shorter plants (1-3 meters), broader leaflets, and higher cannabinoid content adapted to subtropical regions. C. ruderalis is characterized by dwarf growth (under 1 meter), minimal branching, and auto-flowering traits independent of photoperiod, originating from ruderal habitats in Central Asia and Eastern Europe.[16] These forms hybridize readily, producing intermediate phenotypes, which challenges strict species boundaries and aligns with clinal variation rather than discrete taxa.[16] Botanically, Cannabis plants are annual herbs with erect, often branched stems bearing palmate leaves of 3-11 serrated leaflets arranged alternately.[17] The plants are predominantly dioecious, with male flowers in loose panicles and female flowers in compact spikes or bracts clustered at nodes, though monoecious cultivars exist for agricultural purposes.[17] Fruits are achenes containing a single seed, and the plant's resinous glandular trichomes on leaves, stems, and inflorescences produce cannabinoids and terpenes central to its pharmacological profile.[18] Native to Central Asia, Cannabis exhibits high phenotypic plasticity influenced by photoperiod, soil, and cultivation, enabling adaptation across latitudes from 30° to 55° N.[17]Chemistry and Pharmacology
Chemical Composition
Cannabis contains over 550 chemical compounds, including more than 100 phytocannabinoids, over 120 terpenoids, and various flavonoids, phenols, hydrocarbons, sugars, and other secondary metabolites.[19][20][21] Phytocannabinoids are terpenophenolic compounds (C21) unique to the genus Cannabis, biosynthesized via the polyketide pathway from precursors like geranyl pyrophosphate and olivetolic acid, with Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD) as the principal variants.[22][19] THC, typically comprising 1-25% of dried inflorescence mass in high-THC cultivars, binds CB1 receptors to produce psychoactive effects, whereas CBD, often 0-20% in concentration, lacks such affinity and exhibits anti-inflammatory properties in preclinical models.[22][23] Other notable cannabinoids include cannabigerol (CBG), cannabinol (CBN), and cannabichromene (CBC), present in trace amounts (<1%) and derived from acidic precursors like THCA and CBDA that decarboxylate upon heating.[22][21] Terpenoids, volatile hydrocarbons synthesized via the mevalonate pathway, dominate the essential oil fraction (up to 5% by weight) and include monoterpenes like β-myrcene (often 30-50% of total), β-caryophyllene, and limonene, alongside sesquiterpenes such as α-humulene.[20][24] These compounds contribute to strain-specific aromas—earthy from myrcene, spicy from caryophyllene—and may enhance cannabinoid bioavailability or modulate receptor activity, though human evidence remains limited.[24][22] Flavonoids, numbering around 20-30 including unique cannflavins A-C, glycosides like vitexin, and orientin, comprise 0.1-1% of dry weight and demonstrate antioxidant and anti-inflammatory effects in vitro, potentially synergizing with cannabinoids.[20][22] Additional constituents encompass phenolic compounds (e.g., stilbenes), alkaloids (in minor quantities), and polysaccharides, with overall profiles varying by chemotype, cultivation environment, and harvest timing—female flowers yielding up to 30% cannabinoids by dry mass versus <1% in leaves or seeds.[20][24] Analytical methods like gas chromatography-mass spectrometry confirm these distributions, revealing hemp varieties (<0.3% THC) prioritize CBD over THC.[20][21]Pharmacokinetics
Cannabis pharmacokinetics describe the absorption, distribution, metabolism, and elimination (ADME) of cannabinoids—most prominently Δ⁹-tetrahydrocannabinol (THC) and cannabidiol (CBD)—across different routes of administration. Because commercial and medical products vary widely in THC/CBD content, formulation, and delivery device, quantitative PK parameters (e.g., bioavailability, time to peak) show substantial between-study and between-person variability.[3][25] Absorption and bioavailability. Route of administration strongly influences onset and peak exposure. With inhalation (smoking or vaporization), systemic exposure occurs rapidly, and peak blood concentrations are typically reached within minutes; reported bioavailability spans a wide range because it depends on inhalation topography (puff volume, breath-hold), device characteristics, and THC concentration.[3] With oral ingestion (edibles, capsules), absorption is slower and more variable, and peak concentrations commonly occur hours after dosing; variability is influenced by formulation, food intake, gastric emptying, and extensive first-pass metabolism.[26] Oromucosal/sublingual products can yield intermediate onset and exposure in some studies, but many “tincture” use patterns involve partial swallowing, producing a mixed oromucosal–oral profile; consequently, reported bioavailability and onset estimates depend on formulation and administration technique.[25] Distribution. THC is highly lipophilic, distributing rapidly into well-perfused tissues (including brain) and partitioning into adipose tissue, which can prolong terminal elimination and contribute to prolonged detectability of metabolites—especially with frequent use. High plasma protein binding has been reported, but measured free concentrations and tissue kinetics vary across individuals and study methods.[3][25] Metabolism and interactions. THC is metabolized primarily in the liver via cytochrome P450 enzymes (commonly including CYP2C9 and CYP3A4), producing 11-hydroxy-THC (an active metabolite that can contribute to psychoactive effects, particularly after oral dosing) and downstream metabolites such as THC-COOH, which is inactive but commonly measured in biological testing. Conjugation (e.g., glucuronidation) contributes importantly to clearance of THC metabolites.[27] CBD is metabolized by overlapping pathways and can inhibit or compete for some CYP enzymes in vitro and in clinical drug–drug interaction studies; the magnitude of any CBD–THC interaction (and interactions with other medications) depends on dose, formulation, timing, and co-administered drugs.[25] Elimination and “detection windows.” THC and its metabolites show multi-compartment kinetics: an initial phase of redistribution and decline followed by a slower terminal phase reflecting release from tissues. Reported half-life estimates therefore vary with sampling duration, frequency of use, and the analyte measured (THC vs metabolites). Excretion occurs via both feces and urine, with proportions varying by study design and metabolite form. Importantly, prolonged urinary detection of metabolites—especially THC-COOH—reflects metabolite kinetics and assay sensitivity/cutoffs and should not be interpreted as evidence of ongoing intoxication or impairment.[26][3]Mechanism of Action
The primary intoxicating effects of cannabis are largely attributed to Δ⁹-tetrahydrocannabinol (THC), which acts as a partial agonist at cannabinoid receptors—especially CB1—within the endocannabinoid system.[3] CB1 receptors are highly expressed in the central nervous system and are distributed across multiple brain regions (including cortex, hippocampus, basal ganglia, cerebellum, and others), consistent with cannabis effects on cognition, motor coordination, and reward-related processes. CB2 receptors are expressed prominently in immune and peripheral tissues, and are also detectable in the nervous system under some conditions; their role in the typical acute intoxicating effects of cannabis appears less central than CB1-mediated signaling.[28] Endogenous cannabinoids such as anandamide and 2-arachidonoylglycerol (2-AG) normally act as retrograde neuromodulators that help regulate synaptic transmission. THC can engage the same receptor system, altering neuronal excitability and synaptic signaling, although THC differs from endogenous ligands in pharmacokinetic profile and receptor activation dynamics.[29] At the cellular level, CB1 receptors couple primarily to Gi/o proteins, which can inhibit adenylyl cyclase and reduce cyclic AMP signaling, and modulate additional pathways (including MAPK/ERK) depending on cell type and context.[3] CB1 activation typically reduces presynaptic calcium influx and can increase potassium conductance, producing presynaptic inhibition of neurotransmitter release in many circuits.[30] Because CB1 receptors are present on multiple neuronal populations, cannabis can influence release of several neurotransmitters (including GABA and glutamate, among others), with downstream effects that vary by brain region and network state rather than producing a uniform increase or decrease in any single transmitter across the brain.[30] These receptor- and circuit-level actions are understood to contribute to acute cannabis effects such as intoxication, altered perception, and short-term impairments in attention and memory, but mapping from receptor signaling to specific subjective experiences (e.g., “euphoria”) remains indirect and depends on dose, route of administration, prior exposure (tolerance), and individual susceptibility.[5] Cannabidiol (CBD) has low direct agonist activity at CB1/CB2 at typical concentrations and is often described as acting through multiple indirect mechanisms. Proposed effects include modulation of endocannabinoid signaling (e.g., via effects on endocannabinoid metabolism or uptake) and receptor-level modulation (including allosteric effects reported in some experimental systems), though the magnitude and relevance of these mechanisms in humans depend on dose and formulation.[31] CBD also interacts with non-cannabinoid targets (e.g., 5-HT1A and TRP channels) in experimental studies; these actions may contribute to certain therapeutic effects of purified CBD, but are not generally regarded as the primary basis of cannabis intoxication, which is dominated by THC acting at CB1.[32] Claims that “minor cannabinoids” and terpenes produce clinically meaningful synergy via an “entourage effect” are hypotheses supported mainly by in vitro studies, animal models, and limited human data, and evidence remains insufficient to conclude that such synergy reliably amplifies or shapes intoxication or therapeutic outcomes across products and users.[3]Acute Effects
Desired Short-Term Effects
Users commonly seek cannabis for its acute psychoactive effects, which are predominantly attributed to delta-9-tetrahydrocannabinol (THC) binding to cannabinoid receptors in the brain, resulting in dopamine release and subjective experiences of euphoria and relaxation.[33] [34] These effects typically onset within minutes of inhalation or 30-90 minutes of oral ingestion, peaking at 10-30 minutes for smoking and lasting 2-3 hours.[35] Low to moderate doses often produce a "high" characterized by feelings of well-being, tranquility, and mood elevation, with users reporting reduced inhibitions and enhanced enjoyment of sensory stimuli.[36] [37] Altered perception is another frequently desired outcome, including distortions in time sense—where minutes feel extended—and heightened sensory acuity, such as intensified colors, sounds, tastes, and tactile sensations.[34] [38] These perceptual shifts contribute to reported increases in creativity and introspection, though empirical validation of creativity enhancement remains subjective and inconsistent across studies.[35] Social effects like increased sociability, laughter, and decreased anxiety in social settings are also sought, particularly with strains higher in THC relative to cannabidiol (CBD), which may modulate intensity.[35] [39] Physiological effects aligned with user desires include appetite stimulation, often termed "the munchies," driven by THC's action on hypothalamic endocannabinoid systems, and mild sedation promoting relaxation without full impairment in low doses.[1] [40] However, the desirability of these effects varies by individual factors such as tolerance, set, setting, and dosage; higher doses can shift toward less desired outcomes, underscoring a biphasic response profile where low THC levels (e.g., 2.5-5 mg) are more reliably rewarding.[36] [41] User surveys and self-reports consistently prioritize these effects as motivations for recreational use, with euphoria and relaxation cited in over 70% of initiation reasons in epidemiological data.[37]Adverse Short-Term Effects
Acute cannabis intoxication commonly impairs cognitive functions, including attention, memory, and executive function, with meta-analytic evidence showing decreases in episodic verbal memory and working memory performance during intoxication.[42][43] Recent use within 24 hours disrupts thinking, coordination, movement, and time perception, particularly in youth and adults.[44] These effects stem from THC's interference with hippocampal and prefrontal cortex activity, leading to short-term deficits that resolve upon cessation but recur with repeated acute exposure.[45] Psychological adverse effects include heightened anxiety, panic attacks, and paranoia, especially with high-THC strains or in inexperienced users.[46] In susceptible individuals, acute use can precipitate transient psychotic symptoms such as hallucinations or delusions, with rates of cannabis-associated psychotic experiences reported in up to 20-30% of heavy users in clinical samples.[46][45] These episodes are typically self-limiting but may unmask underlying vulnerabilities, with higher potency products elevating risk.[47] Cardiovascular responses involve dose-dependent tachycardia, with heart rates increasing by 20-50% shortly after inhalation or ingestion, alongside orthostatic hypotension and potential supine hypertension.[48] Blood pressure rises immediately post-use, straining the system in those with preexisting conditions.[49] Smoking exacerbates respiratory irritation, causing cough, phlegm, and bronchospasm within minutes.[45] Psychomotor impairment heightens accident risk, with cannabis linked to doubled odds of motor vehicle crashes due to slowed reaction times and distorted perception.[50][47] Other somatic effects encompass dry mouth, conjunctival injection, and nausea, particularly from edibles where delayed onset leads to overconsumption.[45] Severity varies by dose, route, tolerance, and individual factors like age and genetics, though empirical data underscore consistent acute risks across populations.[51]Long-Term Health Effects
Physical Health Consequences
Evidence on long-term physical health outcomes is drawn mainly from observational studies (cross-sectional surveys, cohorts, and case-control designs), supplemented by clinical statements and smaller mechanistic or imaging studies. Interpretation is limited by heterogeneous definitions of “cannabis/marijuana” (smoked vs vaporized vs ingested), frequent co-use with tobacco and alcohol (including blunts/spliffs), incomplete adjustment for other substances and baseline health, and reliance on self-report. In some settings, “cannabis” exposure may also be misclassified if respondents include synthetic cannabinoids or products with contaminants, which can have different toxicology.[9] [52] Regular cannabis smoking is consistently associated with symptoms of chronic bronchitis (e.g., chronic cough and phlegm), and cessation is likely to reduce these symptoms. Evidence syntheses also describe airway epithelial injury and inflammatory changes among smokers in histologic studies, but the clinical significance of biopsy findings is not fully established and is complicated by tobacco co-use in many samples.[53] [54] CT-based studies in heavy users report higher frequencies of airway inflammatory changes and emphysema patterns (e.g., paraseptal emphysema) compared with nonsmokers, but conclusions are limited by small samples, selection effects (imaging is often obtained for clinical reasons), and concomitant cigarette smoking in many cannabis-smoking cohorts.[54] By contrast with tobacco, evidence is unclear or inconsistent on whether cannabis smoking alone causes chronic obstructive pulmonary disease (COPD) or accelerates long-term decline in lung function to the same extent as tobacco; longitudinal findings are mixed and often constrained by exposure measurement and confounding.[9] [52] Reports of bullous lung disease and pneumothorax among young cannabis smokers exist largely as case reports/series, and reviews caution against treating these as definitive evidence of causation.[54] Large observational analyses report that cannabis use—particularly more frequent use—is associated with higher odds of cardiovascular events. One large U.S. survey-based analysis reported that daily cannabis use was associated with ~25% higher odds of myocardial infarction and ~42% higher odds of stroke compared with non-use (adjusted estimates), while emphasizing that self-reported exposure/outcomes and observational design preclude causal inference.[55] [56] Small physiological studies have reported endothelial dysfunction in regular users (including in some “otherwise healthy” samples), but these studies are typically cross-sectional and do not by themselves demonstrate accelerated atherosclerosis or predict event rates.[57] Scientific statements note plausible acute mechanisms (e.g., sympathetic activation, hemodynamic effects) and report associations with arrhythmias and ischemic events, but also emphasize uncertainties due to co-use, comorbidity, and limited prospective data.[48] The relationship between cannabis and cancer remains inconclusive overall, largely because relatively few studies cleanly separate cannabis smoking from tobacco smoking and because exposure measurement is often imprecise. A major evidence review found moderate evidence of no statistical association between cannabis smoking and lung or head-and-neck cancers, alongside limited evidence for an association with certain testicular cancer outcomes in some studies.[58] Later systematic and umbrella reviews have similarly emphasized limitations from confounding (especially tobacco), selection, and exposure misclassification, yielding uncertain conclusions for most cancer sites.[59] [60] For males, systematic reviews and clinical guidance summarize studies reporting associations between cannabis use and altered semen parameters (e.g., concentration, motility, morphology), but findings are heterogeneous and commonly observational, with potential confounding by tobacco, alcohol, other drug use, and health behaviors. These results are therefore typically framed as possible reproductive risk rather than established causation.[61] [62] For females, evidence linking cannabis use to fertility-related outcomes is also mixed and varies by endpoint and study population; some findings come from assisted reproduction cohorts and/or in vitro experiments (e.g., THC exposure effects on embryo-related measures), which may not generalize to natural conception.[63] [61] Broad claims that cannabis “suppresses immune function” are not well established in humans. Evidence reviews describe immunomodulatory effects in experimental systems, but conclude that human clinical implications (including infection susceptibility) remain uncertain and context-dependent.[64] [65] Regarding other chronic outcomes, a long-running cohort reported an association between longer-term cannabis use and periodontal disease, while finding limited evidence of broad associations with other midlife physical morbidities in the same cohort context; these findings remain sensitive to exposure definition and confounding.[66]Mental Health Risks Including Psychosis and Schizophrenia
Heavy or frequent cannabis use is associated with a higher risk of later psychotic outcomes, including psychotic disorders and schizophrenia-spectrum diagnoses, in epidemiologic studies; meta-analyses commonly report elevated relative risks for regular/heavy users compared with non-users, though estimates vary by study design and case definition.[67][68] Many syntheses describe a dose–response pattern, with stronger associations among daily or near-daily users; some multi-site studies also report higher risk estimates among users of high-tetrahydrocannabinol (“high-potency”) products, while noting that potency measures and product categories differ across settings and over time.[69][70] Interpretation is constrained by the observational nature of much of the literature and by exposure measurement limits. “Cannabis/marijuana use” in surveys may include smoked products mixed with tobacco (e.g., blunts/spliffs), variable routes (smoking, vaping, edibles), and varying THC/CBD composition; many studies also face incomplete control for other substance use, comorbidity, and social determinants. Misclassification is also possible where “cannabis” includes synthetic cannabinoids or contaminated products, which may have different psychosis risk profiles.[71][72] Prospective cohort studies can provide evidence of temporal ordering (cannabis use preceding onset of psychotic symptoms or diagnosis) and can adjust for baseline symptoms and familial factors, but they cannot fully exclude residual confounding or reverse causation.[73][74] Reverse causation remains a recognized concern because individuals experiencing prodromal symptoms may be more likely to initiate or escalate cannabis use (including for self-management of distress, insomnia, or anxiety). Some longitudinal analyses that control for baseline psychopathology and related liabilities still find an association consistent with cannabis acting as a contributory factor in at least a subset of cases, but causal attribution remains inferential rather than definitive at the individual level.[75][76] “Cannabis-induced psychosis” (acute psychotic symptoms temporally linked to intoxication or use) has been studied in registry and clinical samples; for example, Danish registry analyses reported increasing recorded incidence over time. Such trends are difficult to interpret because they may reflect changes in product potency, patterns of use, diagnostic practices, and service contact, as well as changes in underlying risk.[77] Follow-up studies of people presenting with cannabis-associated or substance-induced psychosis report that a substantial minority later receive a schizophrenia diagnosis (often on the order of one-third to one-half in some cohorts), but progression estimates vary with diagnostic criteria, follow-up duration, continued substance use, and selection into treatment.[78][79] Population-attributable fraction (PAF) analyses have estimated the proportion of schizophrenia cases statistically attributable to cannabis use disorder (CUD) under explicit causal assumptions. For example, a large Ontario, Canada cohort analysis reported an increase in the PAF of CUD associated with schizophrenia after legalization, while emphasizing that PAFs depend on model assumptions, measurement of exposure, and stability of diagnosis practices over time.[80] Danish registry-based modeling similarly estimated that a non-trivial proportion of schizophrenia cases among males could be preventable in the absence of CUD, explicitly framed as counterfactual estimates that assume causality and depend on registry definitions and confounding control.[81] Mechanistic accounts emphasize that Δ⁹-tetrahydrocannabinol acts at CB1 receptors in cortical–striatal circuits, and experimental studies show that THC can produce transient psychotomimetic effects in some individuals; neurobiological models frequently discuss modulation of dopamine signaling as a plausible pathway, without implying that cannabis exposure alone is sufficient to cause schizophrenia.[82] Gene–environment interaction hypotheses (e.g., candidate variants in COMT and AKT1 genes) have been reported in some studies, including experimental challenge paradigms, but effect sizes and replication have been variable, and the clinical utility of these candidates remains uncertain.[83] Meta-analyses report that cannabis users who develop psychosis may present with earlier age at onset than non-users by a small number of years on average, though this finding may be influenced by shared risk factors and earlier help-seeking.[84] Among individuals with established schizophrenia or psychotic disorders, continued cannabis use is associated with higher relapse risk and poorer outcomes in several observational studies; however, interpretation is complicated by confounding (e.g., illness severity, medication adherence, and comorbid substance use).[85]Cognitive and Neurodevelopmental Impacts
Research on cannabis and cognition draws primarily on cross-sectional comparisons, longitudinal cohorts, and neuroimaging, with relatively few designs that can decisively separate cannabis effects from pre-existing differences. Across studies, interpretation is complicated by (i) heterogeneous measures of “cannabis/marijuana” exposure (route, THC:CBD composition, potency, frequency, and whether use is mixed with tobacco), (ii) frequent polysubstance use (especially nicotine and alcohol), (iii) baseline differences in cognition, mental health, and education that can precede use, and (iv) the possibility that some “cannabis” reports include synthetic cannabinoids or contaminated products with different neuropsychiatric profiles.[86][87][88] Adult cognition: Meta-analyses and reviews generally find that frequent or heavy cannabis use is associated with lower performance on some cognitive tasks—often most consistently in domains such as learning, memory, attention, and aspects of executive function—but effect sizes are typically small to modest and vary with age of onset, intensity and duration of use, comorbidity, and the length of abstinence before testing.[86][87][88] A recurring finding in quantitative syntheses is that cognitive differences are smaller when assessments require longer abstinence periods, which is consistent with partial recovery and/or with residual intoxication/withdrawal influencing test performance in some studies.[89][90] Neuroimaging studies report group differences in task-related activation among frequent users, including during working-memory tasks. For example, a large 2025 fMRI analysis reported lower activation during a working-memory task among participants with a history of heavy lifetime use; however, such findings are correlational and task-specific, and they do not on their own establish enduring impairment because activation differences can reflect recent use, tolerance/withdrawal state, compensatory recruitment, comorbidity, or other unmeasured factors.[91] Structural MRI findings are also mixed. Some studies report associations between heavy long-term use and smaller hippocampal volumes or other morphometric differences, while other studies find limited or no differences after stronger control for confounding and exposure measurement.[89][90] Accordingly, most evidence summaries describe the adult literature as supporting associations between heavy use and modest cognitive/neurobiological differences, while emphasizing uncertainty about causality and reversibility.[86][89] Adolescents and neurodevelopment: Because adolescence involves substantial neurodevelopmental change, many studies focus on whether early initiation or heavy use is linked to differences in cortical and white-matter measures. Some longitudinal MRI cohorts report associations between adolescent cannabis use and trajectories such as cortical thinning or altered maturation in frontal regions; however, the direction of effect is contested because baseline brain and behavioral differences can precede initiation, and co-use (notably nicotine) is common.[92][93] Functional MRI meta-analyses similarly report altered activation patterns in youth users during executive-function tasks, but these results are sensitive to abstinence, psychiatric comorbidity, and selection into use.[94] IQ and long-term cognitive change: The Dunedin cohort reported that persistent, adolescent-onset cannabis use was associated with a larger decline in neuropsychological performance (including an average IQ decline reported in that cohort) by adulthood, with stronger associations among heavier and more persistent users.[95] Subsequent analyses using genetically informed or co-twin approaches, and later longitudinal syntheses, have found that associations with IQ change are often substantially attenuated after controlling for shared familial factors and pre-use differences, and that estimated average changes—when detectable—tend to be modest.[96][97] Recent large analyses reporting minimal or no IQ decline in relation to lifetime use have reinforced that conclusions depend heavily on study design, timing of cognitive assessment relative to use, and control of confounding.[98] Overall, evidence summaries commonly characterize the IQ literature as suggestive of risk in early-onset, heavy, and persistent use, but not definitive for causal IQ loss across users.[86][96] Prenatal exposure: Prenatal cannabis exposure is biologically plausible as a developmental influence because the endocannabinoid system is involved in neurodevelopmental processes. However, human evidence is observational and highly confounding-sensitive (e.g., concurrent tobacco/alcohol use, socioeconomic factors, maternal mental health, and indications for use). Cohort and registry studies have reported associations between prenatal exposure and some early-life neurobehavioral outcomes (e.g., attention and inhibitory-control measures), but effect estimates vary and often attenuate with stronger confounder control; findings for later neurodevelopmental diagnoses (e.g., ADHD or autism-related outcomes) have been inconsistent across studies and analytic specifications.[99][100][101] Animal models demonstrate that cannabinoid exposure can affect neurodevelopmental pathways, but translation to human outcomes and real-world exposure patterns remains uncertain.[102] Judgments about causality therefore remain inferential, and most reviews emphasize that the strongest concerns center on heavy, frequent, early-onset use and on prenatal exposure contexts where confounding cannot be confidently excluded.[86][89][100]Dependence and Addiction
Addiction Mechanisms and Prevalence
Mechanistic accounts of cannabis dependence draw on preclinical reward-circuit research, human laboratory studies, neuroimaging, and epidemiologic/clinical diagnostic surveys; these literatures differ in what they can support about causality. Delta-9-tetrahydrocannabinol (THC) acts primarily at cannabinoid type 1 (CB1) receptors, which are widely expressed in the central nervous system and modulate neurotransmitter release (including GABAergic and glutamatergic signaling). In animal models and translational frameworks, CB1-mediated modulation can influence mesolimbic reward circuitry, but the extent to which cannabis dependence in humans is mediated by a dopamine mechanism analogous to other substance use disorders remains uncertain, with reviews noting mixed findings and methodological limitations across studies.[103] With repeated heavy use, tolerance and withdrawal can occur and are part of the diagnostic construct of cannabis use disorder (CUD). Human PET studies have reported reduced CB1 receptor availability in regular/heavy users, with evidence that CB1 measures can partly recover after sustained abstinence; these findings are commonly interpreted as neuroadaptations associated with frequent exposure, while not uniquely specific to compulsive use in every individual.[104] Functional neuroimaging studies of frequent/heavy users have also reported altered reward-related responses (including reduced striatal activation in some paradigms), but such findings are correlational and may reflect tolerance, recent use/withdrawal state, comorbidity, and co-use of other substances, in addition to (or instead of) enduring addiction-related changes.[42] CUD is defined in DSM-5 by clinically significant impairment or distress with ≥2 of 11 criteria (e.g., unsuccessful efforts to cut down, tolerance, withdrawal) occurring within a 12-month period.[33] Prevalence estimates vary by population, timeframe, and diagnostic method. U.S. national survey reporting for 2023 estimated that 6.8% of people aged 12 or older (19.2 million) met criteria for past-year marijuana use disorder, with the highest percentage among ages 18–25.[105] Public-health summaries also note that a substantial minority of people who use cannabis develop CUD, with risk increasing with earlier initiation and more frequent use; one federal summary communicates approximate risks on the order of ~1 in 10 among adult users and ~1 in 6 among those who start before age 18, while emphasizing that risk is not uniform across users.[106] For medical-cannabis populations, a 2024 systematic review and meta-analysis estimated CUD prevalence around 25% (with wide uncertainty across included studies), underscoring that medical-context use does not preclude problematic patterns and that prevalence depends strongly on case definition and sampling frame.[107] Across these sources, an important interpretive limitation is that many estimates rely on self-report and survey instruments that can be affected by underreporting, differences in product potency and patterns of use, and shifts in diagnostic thresholds or measurement approaches over time; consequently, prevalence and mechanism claims are best stated as ranges and associations rather than as precise, universally applicable figures.[105][106]Withdrawal and Dependence Symptoms
Problematic, impairing cannabis use is diagnosed as cannabis use disorder (CUD) in DSM-5, requiring a maladaptive pattern of cannabis use leading to clinically significant impairment or distress and meeting at least 2 of 11 criteria within a 12-month period, including loss of control, social or role impairment, hazardous use, continued use despite problems, and pharmacological features such as tolerance or withdrawal. Severity is specified as mild (2–3 criteria), moderate (4–5), or severe (≥6 criteria).[33] Population prevalence estimates depend on the sampling frame, survey instrument, and case definition. Meta-analytic syntheses of population surveys report past-year CUD prevalence of approximately 2–3% and lifetime prevalence of approximately 6–7%, though rates rise to around 22% among individuals who have ever used cannabis and may reach 25% among those using cannabis for medicinal purposes, with substantial heterogeneity across jurisdictions, time periods, methods, and operationalizations of use and disorder.[108][109][110] Dependence involves neuroadaptations in the endocannabinoid system, such as downregulation of CB1 receptors following chronic THC exposure, which correlate with tolerance and the need for escalating doses to achieve prior effects in heavy users.[111] Cannabis withdrawal syndrome is recognized in DSM-5 and may occur after abrupt cessation or marked reduction following prolonged heavy use (often daily or near-daily for weeks to months). DSM-5 requires ≥3 symptoms developing within about 1 week—irritability/anger/aggression, nervousness or anxiety, sleep difficulty (e.g., insomnia, disturbing dreams), decreased appetite or weight loss, restlessness, depressed mood, abdominal pain, tremors, sweating, fever/chills or shakiness, or headache—that cause significant distress or impairment and are not better explained by another medical or mental disorder or by withdrawal from another substance.[112][113] A key interpretive issue is that some individuals use cannabis to self-manage symptoms such as anxiety, insomnia, chronic pain, or mood issues. In such cases, symptom worsening after cessation may reflect recurrence or rebound of the underlying condition, or changes in concurrent medication or substance use, rather than cannabis-induced withdrawal, requiring consideration of baseline history, timing, and alternative explanations rather than assuming causation from temporal association alone.- Most common symptoms: Across clinical syntheses, frequently reported features include irritability/anger, anxiety, sleep disturbance (including vivid dreams), depressed mood, and reduced appetite, with physical symptoms reported less consistently and more commonly in heavier users or treatment samples.[114][115]
- Onset and duration: Symptoms often begin within 1–2 days after cessation, peak around days 2–6, and typically improve within 1–2 weeks, though sleep problems and cravings can persist longer, particularly with heavy use, comorbidity, or concurrent withdrawal from tobacco or other substances.[116]
- Prevalence: Meta-analytic estimates suggest clinically significant withdrawal is reported by roughly half of regular users, with higher rates in treatment-seeking samples, reflecting heavier exposure, selection effects, co-use patterns, and potential self-medication of underlying conditions.[117][112]
Medical Applications
FDA-Approved and Evidence-Based Uses
The U.S. Food and Drug Administration (FDA) has approved four cannabinoid-based medications for narrow therapeutic indications, all involving purified isolates or synthetic analogs rather than crude cannabis extracts or plant material. These approvals stem from clinical trials demonstrating efficacy and safety for specific conditions, primarily supported by randomized controlled trials (RCTs). Dronabinol (Marinol capsules and Syndros oral solution), a synthetic form of delta-9-tetrahydrocannabinol (THC), received FDA approval in 1985 for treating nausea and vomiting associated with cancer chemotherapy in patients unresponsive to conventional antiemetics, and in 1992 for anorexia with weight loss in patients with acquired immune deficiency syndrome (AIDS).[120][121] Nabilone (Cesamet), a synthetic cannabinoid analogous to THC, was approved in 1985 for refractory chemotherapy-induced nausea and vomiting (CINV), with evidence from RCTs showing superior antiemetic effects compared to placebo, though comparable to some other agents like metoclopramide.[122][123] Epidiolex, a purified oral cannabidiol (CBD) solution derived from cannabis, marks the first FDA-approved cannabis-derived drug, authorized in June 2018 for seizures in patients aged two years and older with Lennox-Gastaut syndrome or Dravet syndrome, rare epileptic encephalopathies.[124] Its approval was based on three pivotal RCTs involving over 500 patients, which reported median seizure reductions of 39-42% versus 14-17% with placebo, with expansions in 2019 and 2020 to include tuberous sclerosis complex-related seizures.[124][120] Systematic reviews affirm moderate-quality evidence for CBD's antiseizure effects in these refractory pediatric epilepsies, though benefits are less clear for other seizure types or adults.[123] Beyond these approvals, evidence-based uses supported by systematic reviews and meta-analyses include CINV management, where cannabinoids outperform placebo in reducing vomiting episodes (odds ratio 3.82 for complete response) across 23 RCTs, though head-to-head trials show no superiority over active comparators like ondansetron.[123][125] For chronic neuropathic pain, meta-analyses of 16 RCTs indicate modest pain relief (mean difference -0.46 on a 0-10 scale) with THC-dominant products, but evidence quality is low due to small sample sizes, short durations, and high dropout rates from adverse effects.[126][123] No FDA-approved cannabis products exist for pain, multiple sclerosis spasticity, or other common indications despite state-level access, as broader reviews highlight inconsistent benefits, publication bias risks, and insufficient high-quality data for whole-plant cannabis.[47][127] Rescheduling of cannabis to Schedule III in 2024 acknowledges potential medical utility but does not confer FDA endorsement for unapproved forms or expand indications.[128][129]Unsubstantiated Claims and Empirical Limitations
Numerous commercial and anecdotal claims assert that cannabis or its derivatives, such as cannabidiol (CBD), can cure or effectively treat serious conditions including cancer, Alzheimer's disease, and a wide array of chronic pains, despite lacking robust clinical validation.[121] [130] For instance, marketing materials for CBD products frequently promote efficacy against over 125 health issues, with cancer cited in 87.2% of such unsubstantiated promotions, often relying on preclinical animal data or patient testimonials that fail to demonstrate causality in human trials.[130] The U.S. Food and Drug Administration (FDA) has repeatedly issued warnings against these claims, noting that only specific purified cannabinoids like Epidiolex (for rare epilepsies) and dronabinol (for chemotherapy-induced nausea) have undergone rigorous approval processes, while crude cannabis extracts or unstandardized products do not.[131] [132] Empirical limitations in cannabis research stem from methodological shortcomings, including a predominance of small-scale, short-duration observational studies prone to self-reporting biases and confounding variables like concurrent use of other substances or placebo effects.[133] Systematic reviews, such as those by Cochrane, highlight insufficient high-quality randomized controlled trials (RCTs) for most proposed uses; for chronic neuropathic pain, evidence remains limited to moderate at best, with no clear superiority over placebo in large, long-term datasets, and increased dropout rates due to adverse effects.[134] [135] Similarly, claims for cancer symptom relief or tumor regression lack support from adequately powered trials, as most data derive from case reports or undercontrolled studies unable to isolate cannabis effects from standard therapies.[136] [137] Regulatory constraints, including Schedule I classification under U.S. federal law until recent partial rescheduling, have historically impeded large-scale RCTs by restricting access to standardized materials, though state-level programs have yielded real-world data plagued by variability in product potency and patient selection biases.[138] Industry-funded research often amplifies positive outcomes while underreporting harms, contributing to overstated efficacy narratives that diverge from independent meta-analyses showing inconsistent benefits outweighed by risks in non-FDA-approved contexts.[139] Overall, the translation from in vitro or animal models to human efficacy remains poor, underscoring the need for pharmacology-specific trials differentiating cannabinoids rather than treating cannabis holistically.[125]Risks in Therapeutic Contexts
Cannabis and cannabinoids prescribed for therapeutic purposes, such as chronic pain management or chemotherapy-induced nausea, carry risks of adverse events that occur more frequently than with placebo in randomized controlled trials, including dizziness (odds ratio 4.6), dry mouth (3.7), nausea (2.7), fatigue (3.1), and somnolence (4.4).[123] Serious adverse events, though less common, are also elevated, with overall adverse event prevalence estimated at 26% (95% CI 13.2-41.2%) among medical users for chronic pain, albeit with very low certainty evidence due to study heterogeneity and reporting biases.[140] These effects stem from cannabinoids' interaction with the endocannabinoid system, which can disrupt homeostasis in ways not fully mitigated by controlled dosing.[125] Psychiatric risks are particularly pronounced in therapeutic contexts for patients with preexisting vulnerabilities, as THC can exacerbate anxiety, paranoia, or induce transient psychosis, with evidence indicating heightened harm potential in those with psychotic disorders or adolescents.[141][72] Meta-analyses link regular medical cannabis exposure to worsened mental health outcomes, including increased schizophrenia risk proportional to usage intensity, challenging assumptions of safety in psychiatric comorbidities.[47] Dependence develops in approximately 25% (95% CI 18-33%) of medicinal cannabis users, with higher rates (29% per DSM-5 criteria) among those using it in the past 6-12 months, driven by frequent dosing schedules that mirror recreational patterns of tolerance and withdrawal.[142][107] Cardiovascular effects include acute tachycardia and hypotension from THC, alongside associations with myocardial infarction (odds ratio 1.29) and stroke (1.20) in users, with therapeutic regimens involving chronic administration potentially amplifying these via endothelial dysfunction or arrhythmogenic potential.[143][55] Systematic reviews report rhythm abnormalities, syncope, and myocardial ischemia as emerging concerns in medical marijuana users, particularly edibles which delay onset and increase dosing errors leading to cardiovascular symptoms in 8% of emergency visits versus 3% for inhalants.[144][145] Cognitive impairments, such as reduced executive function and memory, persist with prolonged therapeutic use, supported by umbrella reviews of observational data showing converging evidence of harm despite short-term trial limitations.[47]| Common Adverse Effects in Therapeutic Trials | Odds Ratio vs. Placebo | Source |
|---|---|---|
| Dizziness | 4.6 | JAMA 2017 meta-analysis[123] |
| Dry Mouth | 3.7 | JAMA 2017 meta-analysis[123] |
| Nausea | 2.7 | JAMA 2017 meta-analysis[123] |
| Fatigue | 3.1 | JAMA 2017 meta-analysis[123] |
| Somnolence | 4.4 | JAMA 2017 meta-analysis[123] |
Non-Medical Uses
Recreational Use Patterns
Cannabis recreational use is most prevalent among adults aged 18-25, with global past-year usage rates peaking in this demographic at around 10-15% in many regions, though rates vary widely by country and legal status.[147] Men report higher frequency and quantity of use compared to women, often citing increased appetite and enthusiasm as effects, while women more commonly experience appetite suppression and dysphoria.[148] In the United States, approximately 42% of adults aged 19-30 reported past-year use in 2023, with 29% in the past month and 10% daily (defined as use on 20 or more days per month).[149] Overall, 52.5 million Americans, or 19% of the population aged 12 and older, used cannabis at least once in the past year as of 2023 data.[150] In Canada, past-year recreational use stood at 22% among those aged 15 and older in 2021, five years after legalization, with 6% reporting daily or near-daily consumption, unchanged from 2023 levels but up from 5% pre-legalization in 2018.[151] Post-legalization trends show an initial spike in use followed by stabilization or slight decline, with increased normalization of attitudes but no sustained rise in heavy use among former non-users.[152][153] Globally, annual prevalence hovers at 2.5-5% of the adult population, equating to roughly 147-228 million users, with highest rates in North America (up to 21.9% in the US) and parts of West Africa and Oceania exceeding 10%.[154][155][156] Use patterns differ by socioeconomic factors, with higher prevalence among unmarried individuals and those with lower education levels in surveyed populations; racial variations exist, such as elevated rates among non-Hispanic Black adults in some US cohorts.[157] Occasional use (1-11 days per month) dominates, comprising over 80% of users in national surveys, while daily use remains below 10% but has risen modestly in legalized markets.[158] Legalization correlates with shifts toward regulated sourcing and diverse products, though illicit markets persist, supplying 40-70% of users in Canada post-2018.[159][160]Spiritual and Religious Contexts
Cannabis has been employed in spiritual and religious rituals across various ancient cultures, with archaeological and textual evidence indicating its use for inducing altered states during ceremonies. Greek historian Herodotus, writing around 440 BCE, described Scythian nomads in Central Asia performing post-funeral purification rites by inhaling cannabis smoke in enclosed tents, throwing hemp seeds onto hot stones to produce vapors that elicited shouts of joy and apparent euphoria.[161] This account aligns with 2019 archaeological findings from a 2500-year-old Jirzankal cemetery in western China, where residue analysis of wooden braziers revealed high-THC cannabis burned intentionally for its psychoactive effects, likely in funerary or shamanic contexts among local Indo-Iranian groups akin to Scythians.[162] In Hinduism, cannabis, prepared as bhang—a beverage of cannabis leaves, milk, and spices—holds ritual significance tied to Lord Shiva, revered as the "Lord of Bhang" in legends where the plant soothed him after consuming poison during the churning of the ocean.[163] Devotees consume bhang during festivals like Maha Shivratri to emulate Shiva's ascetic meditation and attain spiritual insight, a practice documented in texts from around 1000 BCE and persisting in India and Nepal.[164] This entheogenic role emphasizes cannabis as one of five sacred plants for mystic inspiration, though its use is confined to specific rites rather than daily devotion.[165] Rastafarianism, emerging in Jamaica in the 1930s, regards cannabis—termed ganja or holy herb—as a sacrament essential for reasoning sessions called groundations, where it facilitates meditation, biblical interpretation, and connection to Jah (God).[166] Adherents cite passages like Psalms 104:14 and Revelation 22:2 to justify its divine origin for healing and enlightenment, integrating it into daily spiritual practice despite legal challenges.[167] Archaeological evidence from a 760 BCE Judahite shrine at Tel Arad in Israel revealed cannabis residues on altars, suggesting its burning in cultic rituals possibly for psychoactive effects, though interpretations remain debated and not universally accepted as confirmatory of widespread religious use.[168] Similarly, hypotheses linking "kaneh-bosem" in Exodus 30:23's holy anointing oil to cannabis lack definitive linguistic or chemical consensus, with traditional translations favoring calamus.[169] In ancient Chinese Taoism, cannabis (ma) appeared in shamanic texts like the Wu Yao Jing for inducing visions of immortality, reserved for religious elites, but empirical evidence for routine entheogenic application is sparse compared to medicinal records.[170] Indigenous American uses post-date European introduction, with limited pre-Columbian evidence, underscoring cannabis's primary historical entheogenic roles in Eurasian traditions.Consumption Methods and Preparations
Traditional Consumption Methods
Archaeological evidence from the Jirzankal Cemetery in the Pamir Mountains of western China reveals the earliest known instance of cannabis smoking, dating to around 500 BCE, where mourners burned high-THC cannabis in wooden braziers to inhale psychoactive fumes during funerary rituals.[162] This method involved placing cannabis atop heated stones or embers, producing vapors for communal inhalation, as corroborated by chemical residue analysis showing elevated levels of THC and related compounds compared to wild varieties.[171] In ancient Central Asia, Scythian nomads employed a similar vaporization technique, as recorded by Herodotus in the 5th century BCE: they erected small tent-like structures, heated stones within, and cast cannabis seeds or flowers onto them, inhaling the resulting smoke during purification ceremonies following funerals or burials.[172] This practice, evidenced by residue in artifacts and ethnographic parallels, predates widespread pipe use and highlights early selective breeding for potent strains.[161] In the Indian subcontinent, bhang—a preparation from cannabis leaves, flowers, and sometimes seeds—has been consumed orally since at least the Vedic period, with documented ritual use by the 8th century CE in Hindu texts associating it with Shiva.[164] Traditional preparation involves grinding the plant material into a paste, soaking it in hot milk or water to extract cannabinoids, straining through cloth, and blending with spices, nuts, sugar, and yogurt or milk to form drinks like thandai or lassi, often ingested during festivals such as Holi for purported euphoric and devotional effects.[173][174] In the Middle East and Islamic world, hashish emerged around 900 CE as a concentrated resin extract, traditionally produced by hand-rubbing live cannabis plants to collect trichomes (charas) or sieving dried material, then compressing into blocks for smoking in pipes or ingestion in foods and beverages.[175] Sufi orders disseminated its use for mystical experiences, inhaling vapors or consuming orally despite theological debates, with preparation methods emphasizing purity of resin to maximize psychoactive potency. These techniques, rooted in agrarian practices, prioritized non-combustive collection to preserve terpenes and cannabinoids.[176]Processed Forms and Modern Preparations
Processed forms of cannabis encompass concentrates derived primarily from glandular trichomes, which contain high levels of cannabinoids like THC and terpenes, yielding products with potencies often exceeding 50% THC by weight compared to 10-25% in raw flower. [177][178] These include both traditional mechanical separations and modern extraction techniques designed to isolate active compounds efficiently. Kief represents the simplest processed form, consisting of sifted trichomes collected as a fine, powdery residue from dried cannabis flowers using mesh screens; it typically contains 50% or more THC and can be used directly for smoking or further processed. [179] Hashish, or hash, compresses kief or sieved resin into blocks or balls, a method dating back centuries but refined today via dry-sifting or ice-water agitation to produce bubble hash, which separates trichomes through cold water and bubble bags for purer results. [180][181] Solventless modern variants like rosin apply heat and pressure—often 150-220°F and thousands of pounds per square inch—to flower or hash, squeezing out resin without chemicals, resulting in a sticky extract preserving natural terpenes. [182] Solvent-based extractions dominate contemporary production for their scalability and high yields. Butane hash oil (BHO) employs liquid butane to dissolve cannabinoids from plant material, followed by purging to remove the solvent, producing forms like shatter—a brittle, translucent glass-like concentrate—or wax and crumble with THC levels of 60-90%. [178][183] Supercritical CO2 extraction uses pressurized carbon dioxide above its critical point (around 88°F and 1,070 psi) as a tunable solvent, extracting oils suitable for further refinement into distillates, which are nearly pure THC isolates used in vapes. [184] Ethanol extraction, another common method, soaks biomass in cold ethanol to capture compounds before winterization to remove waxes, yielding versatile oils. [182] Modern preparations extend beyond concentrates to infused products for alternative consumption. Edibles incorporate decarboxylated cannabis extracts or fats like cannabutter—made by simmering ground flower in butter to bind THC to lipids—into foods such as brownies or gummies, with effects onsetting in 30-120 minutes and lasting 4-8 hours due to hepatic metabolism converting THC to the more potent 11-hydroxy-THC. [185] Tinctures dissolve extracts in alcohol or carrier oils like MCT for sublingual or oral use, offering precise dosing via droppers and faster absorption (15-45 minutes) than edibles while avoiding inhalation. [186] Vape preparations heat distillates or full-spectrum oils in cartridges to 350-450°F, vaporizing cannabinoids for inhalation without combustion byproducts, popular for discretion and rapid onset within minutes. [187] These forms prioritize potency, flavor preservation, and method-specific bioavailability, though extraction residuals in solvent methods necessitate rigorous testing for safety. [188]
Varieties and Production
Natural Strains and Genetic Variations
Cannabis displays extensive genetic diversity resulting from millennia of adaptation to varied climates and geographies, primarily within the species Cannabis sativa L. as supported by taxonomic and genomic evidence. Traditional morphological classifications distinguish C. sativa (tall, lax-branching plants with narrow leaflets from temperate and equatorial regions), C. indica (compact, bushy forms with broad leaflets from subtropical highlands), and C. ruderalis (short, weedy variants from steppe environments), but empirical data from genome-wide analyses reveal no reproductive barriers or fixed genetic discontinuities warranting separate species status.31379-X)[17] Instead, these align as subspecies or varieties under C. sativa, with C. sativa subsp. sativa encompassing fiber hemp and drug-type variants, and subsp. indica covering narcotic landraces, per classifications proposed by Small in 1979 and refined through phylogenetic studies.[189][14] Natural strains, known as landraces, embody this variation as regionally stabilized populations shaped by natural selection without human hybridization, originating from centers like South Asia, the Middle East, and Africa. Sativa landraces, such as those from Thailand (high-THC, energizing profiles) or Durban, South Africa (narrow leaves, resinous buds adapted to hot climates), typically exhibit photoperiod-sensitive flowering and elevated tetrahydrocannabinol (THC) levels exceeding 10-15% in wild forms, alongside lower cannabidiol (CBD).[190][191] Indica landraces from Afghanistan or Hindu Kush regions feature shorter statures (1-2 meters), dense branching for cold tolerance, and cannabinoid ratios favoring sedation, with THC:CBD often around 1:1 in traditional accessions documented in ethnobotanical collections since the 1970s.[190] Ruderalis strains from Russia and Kazakhstan, documented in Soviet-era surveys, are autoflowering due to a recessive genetic trait independent of day length, reaching maturity in 8-10 weeks but yielding under 5% THC, reflecting adaptation to short growing seasons.[191][192] Genetic variations manifest in cannabinoid synthase loci (e.g., THCAS and CBDAS genes), terpene synthases, and morphological traits like leaflet serration or internode length, with studies of over 300 accessions showing principal component analysis clustering by origin rather than strict indica-sativa binaries.[193] For instance, high-altitude indica landraces exhibit upregulated genes for UV-protective flavonoids, while equatorial sativas prioritize heat-dissipating volatiles, as evidenced by metabolomic profiling of preserved seeds from 1920s-1950s germplasm banks. Rare mutations, such as duckfoot (broadened leaflets) or sugar leaves (increased resin glands), occur sporadically in wild populations but do not define strains, underscoring cannabis's outcrossing dioecious nature that promotes heterozygosity over fixation.[194] These natural profiles form the genetic foundation for modern cultivars, though extensive breeding has diluted pure landrace traits, with genomic sequencing of feral populations confirming ongoing introgression from escaped hybrids.[193]Cultivation Practices and Synthetic Alternatives
Cannabis cultivation primarily involves propagating Cannabis sativa or C. indica plants from seeds or cuttings, with photoperiod-sensitive varieties requiring an 18-hour light/6-hour dark cycle during vegetative growth (typically 4-8 weeks) to promote stem and leaf development, followed by a 12-hour light/12-hour dark cycle to induce flowering (8-10 weeks).[195] Autoflowering strains, derived from C. ruderalis genetics, bypass photoperiod dependence and complete cycles in 8-12 weeks regardless of light schedule, enabling multiple harvests annually in controlled settings.[196] Plants are dioecious, producing male and female flowers separately, though feminized seeds or removal of males prevent pollination and maximize female bud production containing cannabinoids like THC.[197] Outdoor cultivation relies on natural sunlight in temperate climates, yielding 600-750 grams per plant under optimal conditions (e.g., Mediterranean summers with 14+ hours daylight), but is vulnerable to weather, pests, and seasonal limits, often harvested in late summer to fall.[198] Indoor methods, using artificial lights like high-intensity discharge lamps or LEDs, allow year-round production in controlled environments, with hydroponic systems—where roots are suspended in nutrient-enriched water—accelerating vegetative growth by up to 1.5 times compared to soil, due to direct oxygen and nutrient delivery, potentially yielding 100-250 grams per plant indoors.[199][200] Hydroponics offers precise pH (5.5-6.5) and electrical conductivity control for nutrient uptake, reducing water use by 90% versus soil, but demands constant monitoring to avoid root rot or deficiencies, contrasting soil's forgiving microbial buffering and natural pest resistance at the cost of slower maturation and lower yields.[201] Greenhouse hybrids combine natural light with supplemental controls, balancing cost and output for commercial scales exceeding 1 kg per plant outdoors with advanced training like topping or SCROG nets.[202] Synthetic alternatives to natural cannabis encompass lab-produced cannabinoids designed to activate CB1 receptors like THC, but often with higher affinity and altered pharmacokinetics, leading to intensified effects. Developed initially in the 1970s-1990s for pharmacological research—such as Raphael Mechoulam's analogs or John W. Huffman's JWH series at Clemson University—these compounds, including JWH-018 (first synthesized in 1990s), emerged as recreational substitutes around 2004 via products like "Spice," sprayed onto inert herbs to mimic smoking cannabis while evading early bans on plant-derived THC.[203][204] Unlike variable natural profiles (e.g., 5-30% THC in bred strains), synthetics like AM-2201 or UR-144 exhibit potencies 10-100 times greater, correlating with elevated risks of acute toxicity, including tachycardia, seizures, and psychosis, as documented in emergency data from 2010s outbreaks where metabolites persisted longer than THC.[205][206] These synthetics, structurally diverse (classical like HU-210 resembling THC versus non-classical indoles), proliferated as "legal highs" post-2008 amid tightening natural cannabis laws, but empirical evidence shows inconsistent dosing on commercial products, with adulterants amplifying harms absent in regulated plant cultivation; for instance, JWH-018 binds irreversibly to receptors, unlike THC's partial agonism, contributing to dependency and withdrawal not equivalently observed in natural use.[207][203] Therapeutic pursuits, such as nabiximols (synthetic THC-CBD mix approved in 2010 for spasticity), remain narrow and prescription-bound, while unregulated variants drive public health burdens, with U.S. poison center calls surging 20-fold from 2010-2015, underscoring their unreliability as substitutes.[208][209]Historical Development
Ancient and Traditional History
Archaeological evidence indicates cannabis originated in Central Asia, with paleobotanical remains dating to approximately 11,700 years ago near the Altai Mountains, initially utilized for fiber production.[165] The earliest confirmed psychoactive use occurred around 2500 years ago in the Jirzankal Cemetery in the Pamir Mountains of western China, where mourners burned high-THC cannabis in wooden braziers during funerary rituals, as evidenced by chemical analysis of residues showing elevated tetrahydrocannabinol levels compared to wild varieties.[162][171] In ancient China, cannabis was documented in Emperor Shen Nung's pharmacopeia circa 2800 BC for medicinal applications, including pain relief and as an anesthetic, alongside its roles in fiber for textiles and ropes.[163] By the 5th century BC, Greek historian Herodotus described Scythian nomads in Central Asia inhaling cannabis smoke through heated stones in small tents for ritual purification following burials, a practice corroborated by later archaeological finds of similar paraphernalia.[210][161] In the Indian subcontinent, the Atharva Veda (circa 2000–1400 BC) references cannabis as one of five sacred plants, portraying it as a source of happiness and liberation, often prepared as bhang—a beverage infused with leaves and consumed in religious contexts associated with Shiva.[164] Traditional uses extended to Africa via ancient trade routes, arriving at least 1,000 years ago in regions like Madagascar and the Mediterranean coast, where indigenous groups such as the Khoisan employed it for ceremonial and medicinal purposes.[211][212] Cannabis spread to the Middle East, with hashish production emerging in areas like Morocco by early modern periods, building on ancient fiber and seed uses.[213]Modern Prohibition and Scientific Discovery
In the early 20th century, cannabis prohibition emerged in the United States amid growing concerns over recreational use associated with Mexican immigrants following the 1910 Mexican Revolution, leading to state-level bans beginning with California's 1913 law prohibiting possession and sale.[214] By 1931, 29 states had enacted outright prohibitions, often justified by reports of marijuana-induced violence and psychosis, though Federal Bureau of Narcotics commissioner Harry Anslinger amplified unsubstantiated claims of widespread harm to advocate for federal action.[214] The Marihuana Tax Act of 1937 imposed prohibitive taxes and regulations on cannabis transfer, effectively criminalizing non-medical possession and cultivation nationwide, despite limited empirical evidence of its dangers compared to alcohol or tobacco at the time.[215] Internationally, cannabis entered treaty-based control with the 1925 Geneva Opium Conference, where the League of Nations first regulated its export for non-medical purposes, marking the onset of global prohibition frameworks.[216] This evolved into the 1961 United Nations Single Convention on Narcotic Drugs, which classified cannabis alongside heroin and cocaine, mandating signatory nations to prohibit production and trade except for limited medical or scientific uses, influencing widespread criminalization despite varying cultural acceptance in regions like India and Jamaica.[217] In the U.S., the 1970 Controlled Substances Act reinforced domestic prohibition by scheduling cannabis as a Schedule I substance, denoting high abuse potential and no accepted medical value, a classification that persisted amid the "War on Drugs" escalation under subsequent administrations.[215] Scientific inquiry into cannabis persisted amid prohibition, with Israeli chemist Raphael Mechoulam isolating and elucidating the structure of delta-9-tetrahydrocannabinol (THC), its primary psychoactive compound, in 1964 at the Hebrew University of Jerusalem, enabling precise pharmacological study.[218] This breakthrough, derived from hashish samples, contradicted blanket assertions of cannabis's uniform toxicity by identifying specific cannabinoids responsible for effects, though U.S. research remained constrained by federal restrictions requiring special approvals.[219] Further advances in the 1980s and 1990s revealed the endocannabinoid system, including the cloning of the CB1 receptor in 1990, discovery of the endogenous ligand anandamide in 1992, and 2-arachidonoylglycerol (2-AG) in 1995, demonstrating cannabis's interaction with innate neural regulatory pathways involved in pain, appetite, and mood.[220] These findings, primarily from non-U.S. labs due to domestic barriers, underscored cannabis's therapeutic potential while highlighting prohibition's role in delaying clinical trials and empirical data collection on risks like dependency and cognitive impairment.[165] Despite biases in prohibition-era advocacy—such as Anslinger's reliance on anecdotal hysteria over controlled studies—subsequent research affirmed moderate acute harms, including impaired psychomotor function and psychosis risk in vulnerable users, without evidence equating it to opiates' lethality.[221]Recent Legalization and Policy Shifts
In the United States, Colorado and Washington voters approved recreational cannabis legalization initiatives in November 2012, marking the first such state-level reforms, with regulated sales beginning in January 2014 in Colorado.[215] By 2025, recreational use has been legalized in 24 states plus the District of Columbia, alongside medical programs in 38 states.[222] Federally, the Biden administration initiated proceedings in May 2024 to reschedule cannabis from Schedule I to Schedule III under the Controlled Substances Act, following a recommendation from the Department of Health and Human Services that acknowledged its medical uses and lower abuse potential relative to heroin or LSD, though the process remains ongoing amid administrative reviews and potential shifts under the incoming Trump administration.[223] [224] Canada enacted the Cannabis Act on October 17, 2018, becoming the second country after Uruguay to legalize recreational cannabis nationwide, permitting adults to possess up to 30 grams of dried cannabis and cultivate up to four plants per household.[225] In Europe, Germany implemented the Cannabis Act on April 1, 2024, allowing adults over 18 to possess up to 25 grams in public and 50 grams at home, as well as cultivate up to three plants privately or join nonprofit cannabis social clubs for distribution starting July 1, 2024, though commercial sales remain prohibited and consumption is banned near schools.[226] [227] This made Germany the largest EU nation to partially legalize recreational use, influencing debates in neighboring countries like the Netherlands and France, where policy remains focused on decriminalization or medical access without full recreational markets.[228] Other notable shifts include Thailand's decriminalization of cannabis in June 2022, the first in Asia, leading to widespread dispensaries but prompting regulatory tightening in 2024 due to increased youth access concerns.[229] Malta legalized recreational possession and cultivation for adults in December 2021, with limited home grow and no commercial framework.[225] Globally, over 40 countries permit medical cannabis by 2025, but recreational legalization remains confined to a handful of jurisdictions, with international treaties like the UN Single Convention on Narcotic Drugs still classifying cannabis as a Schedule I substance, complicating harmonization efforts.[230] These reforms have been driven by arguments over reducing black market violence, generating tax revenue—such as Colorado's $2.4 billion since 2014—and addressing disproportionate enforcement on minorities, though critics highlight potential increases in impaired driving and adolescent use without corresponding reductions in overall prohibition-era harms.[215] [231]Legal Status and Regulation
International Frameworks
The principal international framework regulating cannabis is the Single Convention on Narcotic Drugs of 1961, as amended by the 1972 Protocol, which consolidates prior treaties and requires parties to limit cannabis cultivation, production, manufacture, export, import, distribution, trade, and use to exclusively medical and scientific purposes.[232] Under this treaty, cannabis and cannabis resin are listed in Schedule I, signifying substances with a high potential for abuse and limited accepted medical utility at the time of adoption, necessitating strict controls including licensing and record-keeping for any permitted activities.[233] As of 2021, approximately 95 percent of United Nations member states, or 186 parties, have ratified or acceded to the convention, binding them to its provisions unless reservations are specified.[234] [217] In December 2020, the United Nations Commission on Narcotic Drugs (CND) voted to remove cannabis and cannabis resin from Schedule IV of the 1961 Convention, which had previously categorized them alongside substances deemed to have no therapeutic value and posing exceptional risks, thereby acknowledging potential medical applications while retaining Schedule I status for the plant and resin containing delta-9-tetrahydrocannabinol (THC).[235] [236] This adjustment followed World Health Organization recommendations, including the exclusion from scheduling of preparations containing cannabidiol (CBD) with no more than 0.2 percent THC, though the cannabis plant itself remains controlled due to THC content.[237] The 1971 Convention on Psychotropic Substances complements this by scheduling synthetic THC and certain cannabinoids, but natural cannabis derivatives fall primarily under the 1961 framework. The 1988 United Nations Convention Against Illicit Traffic in Narcotic Drugs and Psychotropic Substances further strengthens enforcement by mandating criminal penalties for unauthorized production, possession, purchase, sale, and trafficking of cannabis, including precursor controls and extradition provisions, with over 190 parties as of 2023. Compliance is overseen by the International Narcotics Control Board (INCB), which issues quotas for licit production and reports inconsistencies, such as national recreational legalization efforts that strain treaty obligations by expanding beyond medical allowances. As of 2025, no amendments have altered cannabis's core scheduling despite ongoing WHO reviews and national divergences, maintaining the conventions' emphasis on prohibition outside narrow exceptions.[238]National Variations Including United States
Cannabis regulations exhibit significant national variations, ranging from outright prohibition to full legalization for recreational and medical use. Uruguay pioneered nationwide recreational legalization in December 2013, establishing a state-regulated market for adults over 18, including home cultivation limits and pharmacy sales.[239] Canada followed with federal recreational legalization on October 17, 2018, via the [Cannabis Act](/page/Cannabis Act), permitting possession of up to 30 grams and home growing of four plants, though provinces manage distribution.[240] Other nations with recreational legalization include Malta (2021, allowing possession and nonprofit clubs), Luxembourg (2023, personal cultivation and possession), Germany (April 2024, possession up to 25 grams and home growing, with commercial sales pending), and Georgia (2018 decriminalization with constitutional protection for personal use).[241] [240] Thailand decriminalized cannabis in June 2022 as the first Asian country, enabling widespread cultivation and sales, but by June 2025, the government proposed recriminalization of recreational use due to unregulated proliferation and youth access concerns, restricting it primarily to medical purposes.[242] [243] In contrast, many countries maintain strict prohibitions or limited medical access. Portugal decriminalized all drugs, including cannabis, in 2001, treating possession under 25 grams as an administrative offense with health-focused interventions rather than criminal penalties.[244] The Netherlands employs a policy of gedoogbeleid (tolerance), allowing sales of up to 5 grams in licensed coffeeshops since the 1970s, though cultivation remains illegal, creating a gray market.[225] Medical cannabis is authorized in over 40 countries globally, often under stringent prescriptions, but recreational use faces barriers in Asia and the Middle East, where penalties include severe imprisonment or death in nations like Singapore and Saudi Arabia.[245] In the United States, cannabis remains federally illegal under the Controlled Substances Act of 1970, classified as a Schedule I drug with no accepted medical use and high abuse potential, though the Department of Health and Human Services recommended rescheduling to Schedule III in August 2023, acknowledging moderate dependence risk and medical applications; as of October 2025, the DEA has not finalized this shift, leaving interstate commerce and banking restricted. [246] State-level reforms diverge sharply: 24 states and the District of Columbia have legalized recreational use as of mid-2025, typically allowing possession of 1-2 ounces for adults 21 and older, with regulated sales generating over $30 billion annually in tax revenue.[10] [247] An additional 14 states permit medical-only programs, while 40 states overall authorize some medical access, often limited to low-THC products or specific conditions like epilepsy.[248] Decriminalization prevails in seven states, reducing penalties to fines for small amounts, but full prohibition persists in Idaho, Wyoming, and Kansas, where possession can yield felony charges.[10] This federal-state tension results in enforcement discretion, with rare federal interventions in legal states post-2013 Cole Memorandum (rescinded 2018 but informally observed), yet persistent challenges in taxation, research, and veteran access due to federal barriers.[246] Legislative efforts, such as the MORE Act reintroduced in August 2025 to remove cannabis from federal schedules, face partisan hurdles amid a divided Congress.[249]Effects of Decriminalization and Legalization
Decriminalization of cannabis possession for personal use, as implemented in Portugal in July 2001, has been associated with stable or declining rates of overall drug use, including cannabis, without evidence of significant increases in prevalence among the general population or youth. Lifetime cannabis use among adults remained around 7-10% post-decriminalization, comparable to pre-policy levels, while problematic use and related health harms decreased due to expanded treatment access and reduced stigma. Drug-related arrests and incarcerations dropped sharply, with administrative panels handling cases instead of courts, contributing to lower HIV transmission rates among injectors and fewer overdose deaths overall, though cannabis-specific health metrics showed minimal shifts. Critics note persistent challenges with addiction treatment delivery, attributing some ongoing issues to implementation rather than the policy itself.[250][251][252] In jurisdictions pursuing full legalization of recreational cannabis production and sales, such as Colorado following voter approval in November 2012, arrests for marijuana possession fell by over 50% by 2019, with juvenile marijuana-related arrests declining 42% from 599 to 349 per 100,000 youth between 2012 and 2019. Tax revenues from legal sales exceeded $2 billion cumulatively by 2023, funding schools and infrastructure, though black market activity persisted due to lower prices and variety. Cannabis use prevalence among adults increased modestly in some states, but youth use rates (ages 12-17) showed no statistically significant rise in national surveys post-legalization, despite concerns over increased potency and accessibility.[253][254] Legalization has yielded mixed outcomes on public safety metrics. In Colorado and Washington, major crime rates exhibited no sustained increases attributable to legalization, with some analyses finding minimal effects on violent or property crimes. However, traffic fatalities rose in a lagged pattern after retail sales began, with studies reporting up to a 52% increase in driver mortality rates in legalized states, linked to higher THC-impaired driving detection. Meta-analyses indicate recreational access correlates with elevated emergency department visits for cannabis-related disorders, including a 20% rise in Canada post-2018 legalization.[255][256][257] Canada's nationwide legalization in October 2018 shifted market dynamics, with legal sales capturing approximately 78% of expenditures by 2023, reducing illegal sources from over 50% to 24%, though daily cannabis use edged up from 5% to 6% among adults. Youth (15-17) use remained stable at around 20%, but young adults (18-24) reported higher frequency, alongside increased hospitalizations for cannabis poisoning. Substitution effects on opioids are inconclusive; while medical cannabis laws reduced opioid deaths in some U.S. states, recreational legalization showed no clear decline and potential increases in fentanyl-related mortality in adopting jurisdictions. Uruguay's 2013 legalization sold over 10 million grams legally by 2023, trimming black market profits by an estimated $30 million annually, yet consumer preference for unregulated strains limited full displacement, with grey markets emerging due to regulatory constraints on quality and potency.[258][151][259]| Jurisdiction | Key Effect | Metric (Pre- vs. Post-Policy) | Source |
|---|---|---|---|
| Portugal (Decrim. 2001) | Drug use prevalence | Stable (no major increase) | [250] |
| Colorado (Legal. 2012) | Juvenile arrests | -42% (2012-2019) | [253] |
| Canada (Legal. 2018) | Legal market share | 78% by 2023 | [258] |
| Uruguay (Legal. 2013) | Black market profit reduction | ~$30M/year | [260] |
Economic Aspects
Production and Supply Chains
Cannabis production primarily involves cultivating Cannabis sativa or Cannabis indica plants for their psychoactive flowers, which are harvested, dried, and processed into various forms such as dried buds, concentrates, or edibles. Global illicit production occurs in countries with favorable climates, including Mexico, Morocco, Afghanistan, and Paraguay, where outdoor cultivation dominates due to low costs and large land availability, though exact yields are difficult to quantify due to underreporting and enforcement challenges.[263] In contrast, legal production in jurisdictions like Canada, the United States (e.g., California and Colorado), and Israel emphasizes controlled environments, with Canada emerging as a leading exporter of medical cannabis flower and extracts as of 2024.[264] Cultivation methods vary between outdoor, indoor, and hybrid greenhouse systems. Outdoor growing, common in illicit operations in subtropical regions, yields 0.5 to 1 kg per plant over 4-6 months but is vulnerable to weather, pests, and detection.[265] Indoor methods, prevalent in legal markets for year-round production and quality control, use artificial lighting (e.g., LEDs or HPS) and hydroponics, achieving higher THC potency but at energy costs up to five times those of outdoor per gram produced, with typical yields of 0.4-0.6 grams per watt of light.[266] Greenhouse hybrids balance costs and control, enabling multiple harvests annually in legal facilities.[267] Post-harvest processing in both chains involves trimming, drying (reducing moisture to 10-15%), curing, and sometimes extraction via solvents like butane for oils or CO2 for safer concentrates. Legal processing adheres to standards ensuring pesticide-free products and lab testing for contaminants, reducing risks like arsenic found in 44% of illicit samples versus 18% in regulated ones.[268] Illicit processing often skips testing, leading to variable potency and adulteration.[269] Illicit supply chains rely on decentralized networks: small-scale farmers supply mid-level processors and traffickers, who use smuggling routes (e.g., Mexican cartels via land borders to the U.S.) to evade interdiction, sustaining dominance in prohibitive markets due to lower prices from avoiding taxes.[270] Legal chains are segmented and traceable: licensed cultivators sell to manufacturers for processing, then to wholesalers/distributors under strict inventory tracking (e.g., via METRC in U.S. states), culminating in retail dispensaries, though high regulatory costs hinder competition with black markets.[270][271] As of 2024, UNODC reports persistent illicit flows despite legalization expansions, with organized groups adapting to exploit regulatory gaps.[272]Market Dynamics and Pricing
The global cannabis market, encompassing both medical and recreational segments, is projected to reach approximately US$70.71 billion in revenue by 2025, driven primarily by expanding legalization in North America and emerging markets elsewhere.[273] In the United States, the market is anticipated to grow from USD 36.94 billion in 2024 to USD 91.10 billion by 2033, with adult-use sales contributing significantly amid ongoing state-level expansions.[274] This growth reflects surging demand from medical prescriptions and recreational consumers, tempered by supply increases from licensed cultivation. Pricing in legal markets varies widely by jurisdiction due to differences in taxation, production costs, and regulatory compliance. In the US, wholesale spot prices averaged $1,048 per pound ($2.31 per gram) as of early 2025, with retail flower prices ranging from $74 per ounce in oversupplied states like California to over $300 per ounce in newer markets such as New Jersey and Connecticut.[275] [276] High taxes—often exceeding 30-40% in states like Washington and Illinois—elevate legal retail prices, making them 20-50% higher than black market equivalents, where sellers avoid compliance costs and offer untaxed product at lower rates.[277] [278] Market dynamics are characterized by oversupply in mature legal states, leading to price compression and consolidation among producers. Legalization has flooded markets with supply, reducing average prices by up to 70% in some areas since initial rollouts, as economies of scale and competition erode margins for cultivators.[277] [279] However, persistent black market dominance—estimated to capture 50-70% of total US consumption in states like California—stems from price disparities, federal illegality limiting interstate trade, and consumer preference for unregulated potency without testing mandates.[280] [281] Demand elasticity remains high, with higher THC concentrations commanding premiums (e.g., 20-30% uplift for top-shelf strains), while bulk purchases and lower-potency flower depress averages.[282] Black market persistence disrupts legal dynamics by undercutting prices and diverting tax revenue, estimated at billions annually in lost state funds.[283] Efforts to erode illicit supply through enforcement have yielded mixed results, as smuggling and home cultivation adapt to legal availability, maintaining downward pressure on overall pricing.[284] In contrast, emerging markets experience initial price spikes from scarcity and hype, followed by stabilization as supply chains mature.[285] Federal policy uncertainty, including banking restrictions, further hampers legal scalability, prolonging black market viability.[277]Societal and Cultural Dimensions
Cultural Representations and Norms
In Hinduism, cannabis has held sacramental status for millennia, often associated with the deity Shiva and consumed as bhang—a preparation of cannabis leaves mixed with milk and spices—during festivals like Holi and Maha Shivaratri to induce spiritual insight and devotion.[164][165] This practice, documented in ancient texts such as the Atharva Veda around 1500 BCE, reflects norms of ritualistic use for mystical elevation rather than recreation, persisting among sadhus (ascetic holy men) in India and Nepal. In Rastafarianism, originating in Jamaica in the 1930s, cannabis—termed ganja—serves as a sacrament to foster meditation, unity, and connection to Jah (God), integral to communal nyabinghi ceremonies and symbolized in reggae music by figures like Bob Marley.[286] Ancient civilizations integrated cannabis into spiritual and funerary rites, with Scythian nomads (circa 400 BCE) inhaling its vapors in tents for purification rituals, as described by Herodotus, while African shamans employed it for divination and healing.[287][288] These uses underscore symbolic roles as a bridge to the divine or ancestors, contrasting with later Western prohibitions that imposed norms of deviance.[289] In Western popular culture, early 20th-century representations emphasized peril, as in the 1936 film Reefer Madness, which depicted cannabis inducing violence and insanity to support U.S. prohibition efforts amid racialized fears targeting Mexican immigrants and Black jazz musicians.[290] By the 1960s counterculture, it symbolized rebellion against authority in literature (e.g., Beat Generation works by Allen Ginsberg) and music, with reggae and rock genres normalizing it as a tool for creativity and anti-establishment ethos.[291][292] Contemporary media often portrays cannabis through the "stoner" archetype—lazy, unmotivated, and disheveled—reinforcing stereotypes that associate users with lower productivity, particularly among males and minorities, though legalization since the 2010s has spurred nuanced depictions in films like Pineapple Express (2008) and music across hip-hop and indie genres, contributing to destigmatization.[293][294][295] Social norms have shifted accordingly, with subcultures viewing it as a wellness aid or identity marker resisting mainstream conformity, while broader acceptance correlates with reduced perceptions of moral failing in surveys post-legalization.[296][297] Persistent stigmas, however, link it to dependency and cognitive impairment, challenging claims of harmlessness amid evidence of varied outcomes by dosage and user demographics.[298]Public Health Implications and Youth Exposure
Public health discussions of cannabis focus on outcomes that appear more common among frequent or heavy use patterns, particularly when use involves high-THC products, early initiation, or co-use with other substances. Interpretation is limited by heterogeneous definitions of “cannabis/marijuana” across surveys and studies (including smoked products mixed with tobacco, edibles and concentrates, varying THC/CBD composition, and different modes of use), and by the possibility that some self-reported “cannabis” exposures include synthetic cannabinoids or contaminated products with different toxicology. These measurement issues complicate comparisons across time and jurisdictions and can bias risk estimates in either direction.[299][300] Psychosis and schizophrenia-spectrum outcomes: Epidemiologic syntheses generally report that heavier cannabis use is associated with higher odds of psychotic outcomes, with effect sizes varying by outcome definition (psychotic symptoms vs diagnosed disorder), population, and confounder control. Some longitudinal and multi-site studies report dose–response patterns, including larger relative risks among daily users and among users reporting high-THC preparations; however, these designs remain vulnerable to residual confounding (including tobacco and other drug use), reverse causation (prodromal symptoms preceding escalation), and differential ascertainment of diagnosis and treatment. Accordingly, statements about “doubling” or “fivefold” risks are best presented as estimates reported in particular studies rather than as universal effects.[299][300][301] Physical health and health-service use: When cannabis is smoked, long-term use is consistently associated with chronic bronchitis–type respiratory symptoms; evidence for other long-term physical outcomes varies by endpoint and study design. Some population-level analyses report associations between cannabis use and higher rates of emergency department visits or hospitalization, but such outcomes are non-specific and can reflect confounding by comorbidity, polysubstance use, socioeconomic factors, and differences in healthcare-seeking behavior.[302] Dependence and high-intensity use: A subset of people who use cannabis develop cannabis use disorder (CUD), with higher conditional risk among early-onset and frequent users; estimates vary by timeframe, diagnostic method, and sampling frame.[51] Trends toward wider availability of high-THC products in some regulated markets have raised concern that higher THC exposure per use episode may increase the likelihood of acute adverse effects (including severe intoxication episodes and cannabinoid hyperemesis syndrome in susceptible individuals) and may increase the probability of developing CUD among those who use frequently. However, potency trends and “average THC” estimates vary substantially by product category, jurisdiction, and testing method, so claims about specific percentage changes over time should be tied to clearly defined surveillance datasets.[303][304][305] Other mental health outcomes: Systematic reviews examining anxiety, depression, and suicidality commonly conclude that associations exist in observational data, but the strength of causal inference is limited by confounding (including underlying psychiatric vulnerability), measurement error in exposure, and co-use of alcohol, nicotine, and other drugs. Where reviews or quasi-experimental designs argue for a contributory role of cannabis, that conclusion should be stated as interpretive and conditional on the assumptions of the included studies rather than as settled causation.[306] Adolescents and neurodevelopment: Because adolescence involves rapid neurodevelopmental change, many studies examine whether early initiation or frequent use is associated with cognitive or neuroimaging differences. Meta-analyses of neuroimaging studies in youth report group differences (e.g., in gray matter measures or functional connectivity) and cognitive performance differences (executive function, memory, attention), but these findings are heterogeneous and sensitive to abstinence duration, psychiatric comorbidity, baseline cognitive differences, and tobacco/nicotine co-use. Claims that deficits “persist even after abstinence” should therefore be presented cautiously and, where possible, linked to studies with well-defined abstinence verification and appropriate controls.[94][42] Longitudinal cohorts have reported associations between early, persistent use and poorer cognitive or educational outcomes, including IQ-related measures in some studies; however, genetically informed and co-twin designs often attenuate these associations, underscoring that causality remains inferential and likely varies by intensity of exposure and individual vulnerability.[307][308] Post-legalization youth exposure: Surveillance findings after legalization have been mixed. Some jurisdictions report stable or declining prevalence of adolescent past-month use, while others report changes in initiation, frequency, or modes of use (e.g., concentrates or edibles). Differences across studies often reflect variation in the regulatory environment, product availability, measurement instruments, and timing relative to implementation. As a result, claims of uniform increases in youth use or initiation after legalization are not well supported across settings; changes, where observed, should be described with explicit jurisdiction, age group, time window, and outcome definition.[309][310][311] Separate from prevalence trends, many analyses note that perceived risk and commercial marketing practices may influence youth attitudes and product selection, though estimating causal effects of marketing is methodologically challenging and context-dependent.[312]Key Controversies
Gateway Drug Debate
The gateway drug hypothesis posits that cannabis use serves as an entry point to the use of more dangerous illicit substances, such as cocaine, heroin, or methamphetamine, by increasing the likelihood of progression through altered brain reward pathways, social networks in illicit markets, or desensitization to drug-taking behaviors.[313] This idea gained prominence in the 1970s from observational patterns where cannabis typically precedes harder drugs in user histories, with U.S. National Longitudinal Survey of Youth data indicating that cannabis users are several times more likely to later try other illicit drugs compared to non-users.[314] Proponents argue this sequence implies causation, potentially via neurobiological changes like enhanced dopamine sensitivity that prime users for stronger stimulants or opioids.[315] However, rigorous empirical scrutiny, including twin and longitudinal studies, reveals primarily correlational rather than causal links, attributable to common underlying risk factors such as genetic predispositions, personality traits like impulsivity, or environmental influences like peer groups and socioeconomic stressors that predispose individuals to polysubstance experimentation regardless of starting substance.[316] Twin studies, which control for shared genetics and family environment, consistently find no independent causal effect of cannabis initiation on subsequent hard drug use; for instance, a 2023 University of Colorado analysis of thousands of twins across states with varying cannabis policies showed that cannabis use did not predict harder drug involvement beyond shared liabilities, and in some cases correlated with reduced alcohol-related problems.[317] Similarly, a multivariate twin study from Australia and the U.S. decomposed variance in cannabis and other drug use, attributing covariation to heritable factors rather than sequential causation.[318] Post-legalization data further undermines causal claims, as states implementing recreational cannabis access since 2012, such as Colorado and Washington, have not observed surges in hard drug use disorders or overdose rates attributable to increased cannabis prevalence; a 2023 study of U.S. adults found no rise in other illicit drug use or substance use disorders following legalization, with cannabis often substituting for alcohol or opioids in some cohorts.[319] Meta-analyses of longitudinal cohorts, including a 20-year New Zealand study, confirm that while early cannabis use associates with elevated risk (e.g., 10-20% progression probability in high-risk groups), this diminishes when adjusting for confounders like tobacco initiation or mental health comorbidities, suggesting availability and cultural norms drive sequences more than pharmacological gateways.[320] Critics of the hypothesis, drawing from causal realism, emphasize that prohibiting cannabis may inadvertently funnel users into unregulated markets where harder drugs are co-marketed, whereas regulated access reduces such exposures without escalating progression.[321] Overall, while associations persist, evidence favors a "common liability" model over strict gateway causation, informing policy debates on decriminalization without presuming inevitable escalation.[322]Disparities in Enforcement and Social Costs
Enforcement of cannabis prohibition in the United States has exhibited significant racial disparities, with Black individuals arrested for marijuana possession at rates substantially higher than White individuals despite comparable usage patterns. According to an analysis of FBI Uniform Crime Reporting data from 2001 to 2010, Black people were on average 3.73 times more likely to be arrested for marijuana possession than White people nationwide, even though national surveys indicate similar lifetime and past-year usage rates across racial groups.[323] This disparity persisted into the 2010s, with Black arrest rates reaching 3.6 times those of Whites in a 2018 review of state-level data, unaffected by variations in actual consumption prevalence.[324] These uneven enforcement patterns correlate with broader policing priorities in urban areas where minority populations predominate, leading to higher detection rates for low-level possession offenses among Black and Hispanic communities. A Bureau of Justice Statistics examination of drug arrests found that Blacks accounted for 40% of drug violation arrests while comprising only 13% of self-reported drug users, highlighting a mismatch between offense prevalence and enforcement outcomes that amplifies collateral consequences like felony records and employment barriers.[325] Even in jurisdictions with decriminalization or legalization, such as certain states post-2010, racial arrest gaps have lingered, with Black individuals facing 3.64 times the possession arrest likelihood compared to Whites as of recent years, underscoring institutional inertia in law enforcement practices.[326] The social costs of these enforcement disparities extend beyond immediate arrests to long-term community harms, including disproportionate incarceration and economic disruption in affected demographics. Annual U.S. expenditures on marijuana law enforcement alone have been estimated at $7.6 billion in criminal justice costs, encompassing policing, prosecution, and incarceration for primarily non-violent offenses that yield minimal deterrence against use.[327] This fiscal burden, drawn from taxpayer funds, diverts resources from other public priorities while contributing to cycles of poverty through barriers to housing, education, and jobs for those with cannabis-related convictions, effects that compound in minority communities due to higher conviction rates.[328] Prohibition's social toll also manifests in lost productivity and family separations, with hundreds of thousands of annual arrests—over 200,000 for possession in 2023 per FBI data—disrupting lives without proportionally reducing availability or consumption.[329] Economists have projected that shifting from prohibition to regulation could reclaim $7.7 billion yearly in enforcement savings, alongside forgone tax revenue, illustrating the inefficiency of current approaches that prioritize punishment over evidence-based alternatives.[328] These costs, empirically tied to policy rather than inherent drug risks, have fueled arguments for reform, though persistent disparities suggest enforcement reforms lag behind legal changes.[330]Myths of Harmlessness vs. Causal Realities
Public discussion sometimes characterizes cannabis as “harmless” or as comparable to a benign herbal remedy. Scientific and clinical assessments instead emphasize that risks vary substantially by dose, frequency, product type (THC/CBD content; concentrates vs flower), route of administration, age at onset, and individual vulnerability, and that “cannabis/marijuana” in surveys may also encompass heterogeneous exposures (including smoked products mixed with tobacco, unregulated vape products, and—by misclassification in some settings—synthetic cannabinoids or contaminated products with different toxicology). These factors complicate simple comparisons across substances and across jurisdictions.[150] cannabis use disorder (CUD): A subset of people who use cannabis meet DSM-5 criteria for CUD (e.g., impaired control, continued use despite problems, tolerance, and/or withdrawal). National surveys and clinical syntheses typically report that risk is higher among frequent users, and that conditional prevalence estimates depend strongly on the population sampled (general population vs treatment-seeking), the timeframe (past-month vs past-year), and the diagnostic instrument used. For this reason, commonly cited “one in ten” or “three in ten” summaries should be presented as approximate and context-dependent rather than as universal rates.[150][331][332] Psychosis-related outcomes: Epidemiologic evidence consistently reports an association between more frequent cannabis use and higher odds of psychotic outcomes, with many meta-analyses describing a dose–response pattern and higher risk estimates among daily users and among those using higher-THC products. However, causal interpretation remains inferential because studies vary in confounder control (including tobacco and other drug use), and reverse causation (prodromal symptoms preceding escalation) can contribute to observed associations. Mechanistic accounts (including THC effects on CB1-mediated signaling and downstream dopamine-related pathways) are frequently discussed as plausible contributors, but do not on their own establish that cannabis exposure is sufficient to cause schizophrenia in the absence of other vulnerabilities.[8][333][82] Cognition and long-term functioning: Reviews and longitudinal studies report that heavy or persistent cannabis use is associated with worse performance on some neuropsychological measures (e.g., learning, memory, aspects of executive function), but effect sizes are often small to modest and sensitive to abstinence duration, baseline cognitive differences, comorbidity, and polysubstance use. IQ-change findings are contested: some cohorts report larger declines concentrated among persistent, early-onset heavy users, whereas genetically informed or co-twin designs can attenuate these associations, suggesting an important role for shared familial or premorbid factors. Neuroimaging studies reporting altered task-related activation in heavy users are correlational and do not, by themselves, establish lasting impairment, because activation differences may reflect recent use, withdrawal state, compensatory recruitment, or selection effects.[95][334][91] Respiratory and cardiovascular outcomes: For smoked cannabis, evidence syntheses consistently report an association with chronic bronchitis–type symptoms (e.g., cough, sputum production). Histologic and inflammatory airway changes have been described in smokers, but inference about long-term structural lung damage and infection susceptibility is limited by confounding (especially tobacco) and by reliance on clinical or convenience samples in parts of the literature.[335][336] Cardiovascular research includes observational studies reporting associations between cannabis use and adverse events (e.g., myocardial infarction and stroke) and physiological studies reporting endothelial-function differences; however, effect estimates vary and remain sensitive to exposure definition, co-use, and underlying risk profiles. Mechanistic explanations (e.g., sympathetic stimulation, hemodynamic changes, prothrombotic pathways) are typically presented as hypothesized contributors rather than definitive causal chains.[55][337][338] Overall, evidence reviews generally conclude that cannabis-related harms are not uniform across users and products, and that the strongest concerns in many syntheses cluster around early initiation, frequent/heavy use, and high-THC exposure, while emphasizing that many prominent claims rest on observational data and thus warrant careful framing of uncertainty.[150][8][55]References
- https://en.wiktionary.org/wiki/%CE%BA%CE%AC%CE%BD%CE%BD%CE%B1%CE%B2%CE%B9%CF%82
.jpg/250px-Cannabis_Drying_out_the_crop_(16558794823).jpg)
.jpg/2000px-Cannabis_Drying_out_the_crop_(16558794823).jpg)




